Case Study: Comprehensive Health Assessment of Type 2 Diabetes
VerifiedAdded on 2022/08/18
|13
|4422
|15
Case Study
AI Summary
This case study presents a comprehensive health assessment of a 69-year-old male, Elio, diagnosed with type 2 diabetes for five years. The assessment encompasses his medical history, including symptoms, previous treatments, and lifestyle factors such as diet and exercise. It details his physical examination findings, including vital signs, and lab results like blood glucose levels, lipid panels, and A1C. The study analyzes the data, revealing uncontrolled diabetes, hyperlipidemia, hypertension, and peripheral neuropathy. Based on these findings, the case study proposes a health plan, including dietary recommendations, weight management strategies, and the importance of patient education for effective self-care and improved disease management. The role of the nurse practitioner in guiding Elio's care is emphasized, highlighting the prioritization of health concerns and the development of tailored treatment plans.

Running Head: COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
Name of the Student:
Name of the University:
Author Note:
COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

1COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
Introduction:
Nursing's specialist function (Rolfe, 2014) in the treatment and education of people with diabetes
has been in operation for over 30 years. Diabetes screening by clinicians has expanded into a number of
health-care environments outside the medical bedside. Nursing have played an important role in the
diabetes team management framework between the disciplines engaged with diabetes training. This was
well demonstrated by the success of nurse practitioners in planning and providing life-management care
for diabetes in the Diabetes Prevention and Complications Trial (DCCT). Not only did these nurse
managers conduct management duties that were essential to the DCCT results, but they often engaged
actively in patient treatment. The advent and rapid development of specialized nursing practice over the
past 20 years has broadened the dimension of patient treatment, integrating elements of both nursing and
medical care while retaining the functions of teaching and counselling. Once applicable to chronic disease
control, both the frameworks of clinical nurse specialist (CNS) and nurse practitioner (NP) establish
improved patient-provider partnerships under which self-care instruction and treatment are offered within
the framework of state management of the disorder. (Greenwood ET AL, 2017), states in his paper, an
analysis of diabetes self-management education (Greenwood et al,2017) concerns where awareness may
increase but most health conditions still minimally change when continuing care becomes part of an
education programme. By the very definition of their field of work, specialized specialist nurses
successfully integrate knowledge and training into their service delivery. Operating in the position of
mentor, experienced nurses in practice holistically evaluate the interests in patients with an appreciation
of the key function of patients in promoting and sustaining their own safety and wellbeing.
Advanced professional nurses (Williams et al, 2016) closely examine the personal histories of
individuals when performing examinations and undertake centered clinical assessments. After conclusion
of tests, specialized practicing nurses define performance priorities in collaboration with patients, and
develop effective treatment strategies. A study of the self-help coping capabilities and application /
Introduction:
Nursing's specialist function (Rolfe, 2014) in the treatment and education of people with diabetes
has been in operation for over 30 years. Diabetes screening by clinicians has expanded into a number of
health-care environments outside the medical bedside. Nursing have played an important role in the
diabetes team management framework between the disciplines engaged with diabetes training. This was
well demonstrated by the success of nurse practitioners in planning and providing life-management care
for diabetes in the Diabetes Prevention and Complications Trial (DCCT). Not only did these nurse
managers conduct management duties that were essential to the DCCT results, but they often engaged
actively in patient treatment. The advent and rapid development of specialized nursing practice over the
past 20 years has broadened the dimension of patient treatment, integrating elements of both nursing and
medical care while retaining the functions of teaching and counselling. Once applicable to chronic disease
control, both the frameworks of clinical nurse specialist (CNS) and nurse practitioner (NP) establish
improved patient-provider partnerships under which self-care instruction and treatment are offered within
the framework of state management of the disorder. (Greenwood ET AL, 2017), states in his paper, an
analysis of diabetes self-management education (Greenwood et al,2017) concerns where awareness may
increase but most health conditions still minimally change when continuing care becomes part of an
education programme. By the very definition of their field of work, specialized specialist nurses
successfully integrate knowledge and training into their service delivery. Operating in the position of
mentor, experienced nurses in practice holistically evaluate the interests in patients with an appreciation
of the key function of patients in promoting and sustaining their own safety and wellbeing.
Advanced professional nurses (Williams et al, 2016) closely examine the personal histories of
individuals when performing examinations and undertake centered clinical assessments. After conclusion
of tests, specialized practicing nurses define performance priorities in collaboration with patients, and
develop effective treatment strategies. A study of the self-help coping capabilities and application /
2COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
adaptation to lifestyle of patients is integrated into original records, clinical assessments and treatment
plans. Many experienced practicing nurses (NPs, CNSs, nurse midwives, and nurse anesthetists) can
administer and change prescription under their local healthcare administrative body's prescriptive
jurisdiction. All 50 states currently have a sort of prescriptive authority for nurses in advanced practice.
A crucial benefit of treatment for diabetes-individuals is the ability of prescribe and change
medications. It is a vital element in caring for people with type I diabetes, and taking care of patients with
type 2 diabetes who have a number of comorbidities, all of which must be monitored for successful
effects of the disease, is becoming especially important. The role of experienced clinical nurses in
diabetes has led dramatically to better results in the treatment of type 2 diabetes, specialist diabetes foot
care services, diabetes control during breastfeeding, and the care of juvenile type 1 diabetic patients and
their parents. Several reports have recorded the efficacy of nurses with specialized experience in
addressing specific primary care (Dunphy et al, 2015) concerns. Nursing Practitioner treatment has been
correlated with a high degree of quality for users of the health services. The paper below discussed and
illustrates the clinical role of advanced practice nurse while handling and managing of a patient named,
Elio who had been suffering from type II diabetes. Additionally the paper focuses on synthesizing the
findings and diagnostic data to recommend the health and clinical decision making priorities for Elio.
Case Presentation:
Medical History:
Elio is a former 69-year-old guy with type 2 diabetes (American Diabetes Association, 2018)
with a 5-year past. While diagnosed in 1997, he had signs 2 years before diagnosis suggesting
hyperglycemia. He had history of fasting blood glucose showing levels of 118–127 mg / dl, which he
identified as suggestive of "borderline diabetes." He also remembered previous nocturia events consistent
with massive spaghetti meals and Italian pastries. He was recommended to lose weight ("at least 10 lb.")
adaptation to lifestyle of patients is integrated into original records, clinical assessments and treatment
plans. Many experienced practicing nurses (NPs, CNSs, nurse midwives, and nurse anesthetists) can
administer and change prescription under their local healthcare administrative body's prescriptive
jurisdiction. All 50 states currently have a sort of prescriptive authority for nurses in advanced practice.
A crucial benefit of treatment for diabetes-individuals is the ability of prescribe and change
medications. It is a vital element in caring for people with type I diabetes, and taking care of patients with
type 2 diabetes who have a number of comorbidities, all of which must be monitored for successful
effects of the disease, is becoming especially important. The role of experienced clinical nurses in
diabetes has led dramatically to better results in the treatment of type 2 diabetes, specialist diabetes foot
care services, diabetes control during breastfeeding, and the care of juvenile type 1 diabetic patients and
their parents. Several reports have recorded the efficacy of nurses with specialized experience in
addressing specific primary care (Dunphy et al, 2015) concerns. Nursing Practitioner treatment has been
correlated with a high degree of quality for users of the health services. The paper below discussed and
illustrates the clinical role of advanced practice nurse while handling and managing of a patient named,
Elio who had been suffering from type II diabetes. Additionally the paper focuses on synthesizing the
findings and diagnostic data to recommend the health and clinical decision making priorities for Elio.
Case Presentation:
Medical History:
Elio is a former 69-year-old guy with type 2 diabetes (American Diabetes Association, 2018)
with a 5-year past. While diagnosed in 1997, he had signs 2 years before diagnosis suggesting
hyperglycemia. He had history of fasting blood glucose showing levels of 118–127 mg / dl, which he
identified as suggestive of "borderline diabetes." He also remembered previous nocturia events consistent
with massive spaghetti meals and Italian pastries. He was recommended to lose weight ("at least 10 lb.")
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
at the time of clinical diagnosis but no further intervention was taken. Post being referred to
diabetes specialist center by his family practitioner, Elio was recorded of recent weight gain, suboptimal
regulation of diabetes and foot discomfort. He's been attempting to shed weight and increasing his
exercise without results for the past 6 months. He also begun on glyburide (Diabeta), 2.5 mg each
morning but avoided taking it in late in the afternoon due to lightheadedness, frequently followed by
nausea and a sense of moderate irritation. Elio also requires 10 mg of atorvastatin (Lipitor) regular for
hypercholesterolemia (strong LDL cholesterol, weak HDL cholesterol and lower triglyceride). He has
endured this medication and he complies to the normal routine. In an effort to boost his diabetes
management he has even ingested gymnema sylvestre, chromium picolinate, and a "pancreas elixir" over
the last 6 months. However, h He discontinued such treatments because no good effects were shown. On
speaking to him it came to the light that at home, he doesn't quite monitor his blood sugar levels and
shares skepticism whether this treatment will help him gain regulation of his diabetes. "What do the
figures say about me?"says Elio. "The doctor realizes the glucose are still very heavy."
Comprehensive Other Findings in relation to Elio:
Elio further notes that he "was never ill a day in my career." Recently, he sold his company and
was very involved in a number of charitable organisations. He stays with his 48-year-old partner, and has
two children together. While his mother and father suffered from type 2 diabetes, A.B. Has little
understanding about self-care treatment about diabetes, and claims he doesn't understand whether he has
diabetes because he rarely consumes sugar. His wife has persuaded him in the past to cure his diabetes
with natural treatments and weight-loss supplements, so she also searches the internet for the new cures
for diabetes. In the preceding year, Elio started gaining weight and was weighed as 22 lb. He has become
more physically involved following retirement, playing golf once per week, planting, but have been
unable to reduce more than 2–3 lb. He also informed that he never saw a nutritionist and was not trained
in blood glucose self-monitoring (BGMS). The history of Elio's lifestyle shows disproportionate
consumption of carbs in sandwich and noodles types. His regular meals are 2 cups of cooked pasta with
at the time of clinical diagnosis but no further intervention was taken. Post being referred to
diabetes specialist center by his family practitioner, Elio was recorded of recent weight gain, suboptimal
regulation of diabetes and foot discomfort. He's been attempting to shed weight and increasing his
exercise without results for the past 6 months. He also begun on glyburide (Diabeta), 2.5 mg each
morning but avoided taking it in late in the afternoon due to lightheadedness, frequently followed by
nausea and a sense of moderate irritation. Elio also requires 10 mg of atorvastatin (Lipitor) regular for
hypercholesterolemia (strong LDL cholesterol, weak HDL cholesterol and lower triglyceride). He has
endured this medication and he complies to the normal routine. In an effort to boost his diabetes
management he has even ingested gymnema sylvestre, chromium picolinate, and a "pancreas elixir" over
the last 6 months. However, h He discontinued such treatments because no good effects were shown. On
speaking to him it came to the light that at home, he doesn't quite monitor his blood sugar levels and
shares skepticism whether this treatment will help him gain regulation of his diabetes. "What do the
figures say about me?"says Elio. "The doctor realizes the glucose are still very heavy."
Comprehensive Other Findings in relation to Elio:
Elio further notes that he "was never ill a day in my career." Recently, he sold his company and
was very involved in a number of charitable organisations. He stays with his 48-year-old partner, and has
two children together. While his mother and father suffered from type 2 diabetes, A.B. Has little
understanding about self-care treatment about diabetes, and claims he doesn't understand whether he has
diabetes because he rarely consumes sugar. His wife has persuaded him in the past to cure his diabetes
with natural treatments and weight-loss supplements, so she also searches the internet for the new cures
for diabetes. In the preceding year, Elio started gaining weight and was weighed as 22 lb. He has become
more physically involved following retirement, playing golf once per week, planting, but have been
unable to reduce more than 2–3 lb. He also informed that he never saw a nutritionist and was not trained
in blood glucose self-monitoring (BGMS). The history of Elio's lifestyle shows disproportionate
consumption of carbs in sandwich and noodles types. His regular meals are 2 cups of cooked pasta with
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
home-made sauce and 3 to 4 slices of toasted bread. He also have "a piece or two" of buttered toast or
olive oil throughout the day. Additionally, he He also consumes, at meals and as snacks, eight to ten bits
of fresh fruit a day. He informed that he loves chicken and shrimp which is typically eaten with a
spaghetti followed tomato or cream sauce. His wife tried to make him grilled meats pure but he
considered them "crass." Every evening he enjoys eight glasses of red wine with dinner. He had quit
smoking more than 10 years earlier and claimed it was more than fifty bucks around the time when the
price of tobacco had peaked.
Medical Records:
Elio's diagnostic records at the approved diabetic clinic demonstrate that his hemoglobin A1c
(A1C) has seldom been < 8%. His blood pressure in the nearby senior center screening clinic was
calculated at 150/70, 148/92 and 166/88 mmHg on different times over the past year. Elio claimed that as
part of his primary care tests he had neither undergone a foot evaluation nor was he trained in preventive
foot treatment. While he was advised that his blood pressure was "up a bit," he was not conscious about
the need for overall cardiovascular and renal wellbeing to sustain his blood pressure at around 130/80
mmHg. His medical reports, though, still show that he has not undergone surgery or hospitalization, his
immunizations are up-to-date, and he has remained relatively well for several years in total.
Physical Examination:
Elio on his arrival to the clinic was immediately taken by the diagnostic team to conduct all the
necessary examinations that would help in understanding his case in a much better and clear way. The
tests that were conducted included with the checking of the primary vital stats, which included with the
checking of his weight, pressure. The full chart of the physical examination that had been conducted is
supplied below:
1. Fasting capillary glucose: 166 mg/dl
2. Weight: 178 lb; height: 5′2″; body mass index (BMI): 32.6 kg/m2
home-made sauce and 3 to 4 slices of toasted bread. He also have "a piece or two" of buttered toast or
olive oil throughout the day. Additionally, he He also consumes, at meals and as snacks, eight to ten bits
of fresh fruit a day. He informed that he loves chicken and shrimp which is typically eaten with a
spaghetti followed tomato or cream sauce. His wife tried to make him grilled meats pure but he
considered them "crass." Every evening he enjoys eight glasses of red wine with dinner. He had quit
smoking more than 10 years earlier and claimed it was more than fifty bucks around the time when the
price of tobacco had peaked.
Medical Records:
Elio's diagnostic records at the approved diabetic clinic demonstrate that his hemoglobin A1c
(A1C) has seldom been < 8%. His blood pressure in the nearby senior center screening clinic was
calculated at 150/70, 148/92 and 166/88 mmHg on different times over the past year. Elio claimed that as
part of his primary care tests he had neither undergone a foot evaluation nor was he trained in preventive
foot treatment. While he was advised that his blood pressure was "up a bit," he was not conscious about
the need for overall cardiovascular and renal wellbeing to sustain his blood pressure at around 130/80
mmHg. His medical reports, though, still show that he has not undergone surgery or hospitalization, his
immunizations are up-to-date, and he has remained relatively well for several years in total.
Physical Examination:
Elio on his arrival to the clinic was immediately taken by the diagnostic team to conduct all the
necessary examinations that would help in understanding his case in a much better and clear way. The
tests that were conducted included with the checking of the primary vital stats, which included with the
checking of his weight, pressure. The full chart of the physical examination that had been conducted is
supplied below:
1. Fasting capillary glucose: 166 mg/dl
2. Weight: 178 lb; height: 5′2″; body mass index (BMI): 32.6 kg/m2
5COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
3. Blood pressure: lying, right arm 154/96 mmHg; sitting, right arm 140/90 mmHg
4. Pulse: 88 bpm; respirations 20 per minute
5. Thyroid: nonpalpable
6. Eyes: Corrective glasses, illumination and housing receptive pupils, Fundi-clear, no arteriovenous
nicking, no retinopathy
7. Lungs: clear to auscultation
8. Heart: Rate and rhythm regular, no murmurs or gallops
9. Neurological assessment: Weakened sensation of vibration to the forefoot, lacking ankle reflexes,
monofilament (5.07 Semmes-Weinstein) felt only above the knee.
10. Vascular assessment: no carotid bruits; femoral, popliteal, and dorsalis pedis pulses 2+ bilaterally
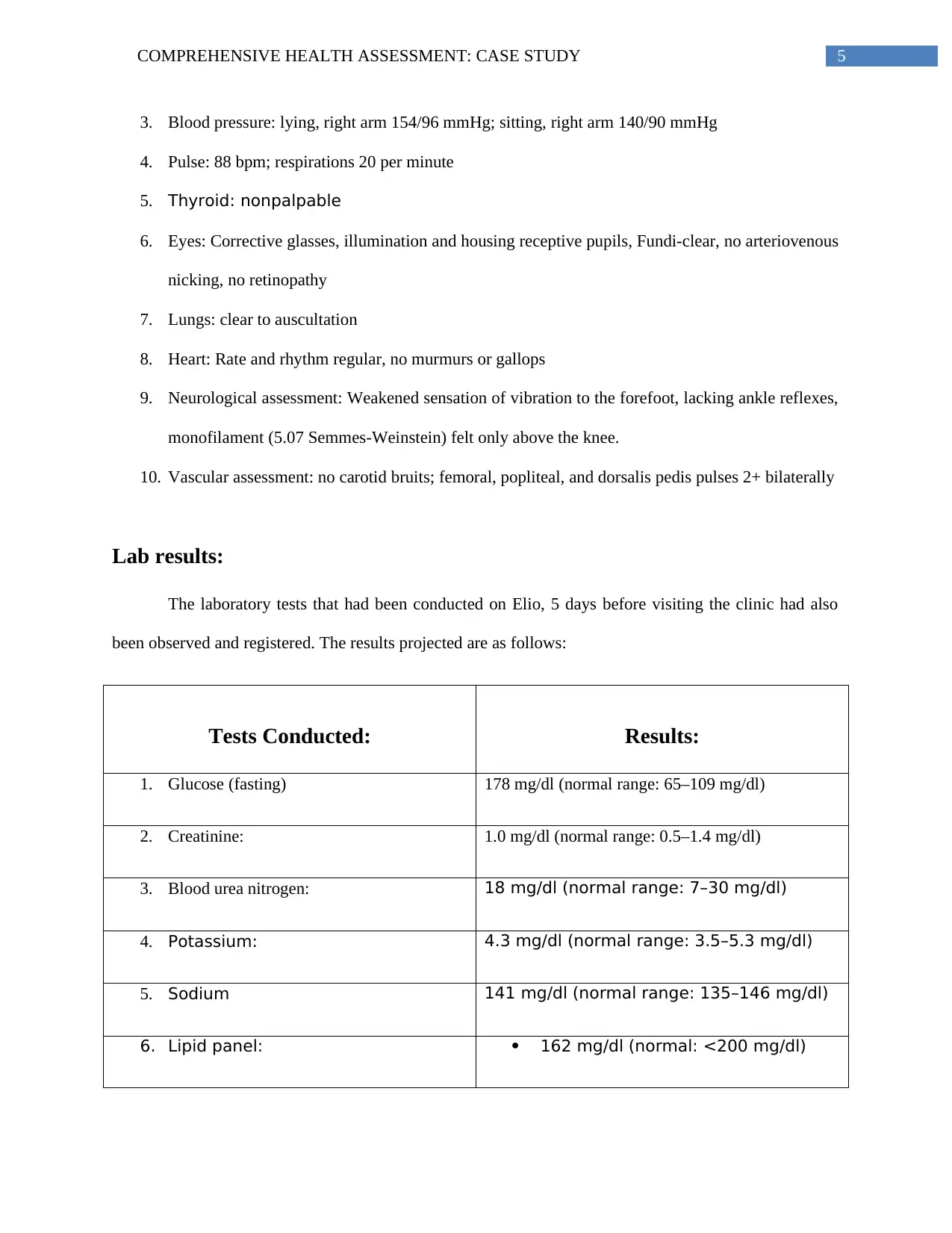
Lab results:
The laboratory tests that had been conducted on Elio, 5 days before visiting the clinic had also
been observed and registered. The results projected are as follows:
Tests Conducted: Results:
1. Glucose (fasting) 178 mg/dl (normal range: 65–109 mg/dl)
2. Creatinine: 1.0 mg/dl (normal range: 0.5–1.4 mg/dl)
3. Blood urea nitrogen: 18 mg/dl (normal range: 7–30 mg/dl)
4. Potassium: 4.3 mg/dl (normal range: 3.5–5.3 mg/dl)
5. Sodium 141 mg/dl (normal range: 135–146 mg/dl)
6. Lipid panel: 162 mg/dl (normal: <200 mg/dl)
3. Blood pressure: lying, right arm 154/96 mmHg; sitting, right arm 140/90 mmHg
4. Pulse: 88 bpm; respirations 20 per minute
5. Thyroid: nonpalpable
6. Eyes: Corrective glasses, illumination and housing receptive pupils, Fundi-clear, no arteriovenous
nicking, no retinopathy
7. Lungs: clear to auscultation
8. Heart: Rate and rhythm regular, no murmurs or gallops
9. Neurological assessment: Weakened sensation of vibration to the forefoot, lacking ankle reflexes,
monofilament (5.07 Semmes-Weinstein) felt only above the knee.
10. Vascular assessment: no carotid bruits; femoral, popliteal, and dorsalis pedis pulses 2+ bilaterally
Lab results:
The laboratory tests that had been conducted on Elio, 5 days before visiting the clinic had also
been observed and registered. The results projected are as follows:
Tests Conducted: Results:
1. Glucose (fasting) 178 mg/dl (normal range: 65–109 mg/dl)
2. Creatinine: 1.0 mg/dl (normal range: 0.5–1.4 mg/dl)
3. Blood urea nitrogen: 18 mg/dl (normal range: 7–30 mg/dl)
4. Potassium: 4.3 mg/dl (normal range: 3.5–5.3 mg/dl)
5. Sodium 141 mg/dl (normal range: 135–146 mg/dl)
6. Lipid panel: 162 mg/dl (normal: <200 mg/dl)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
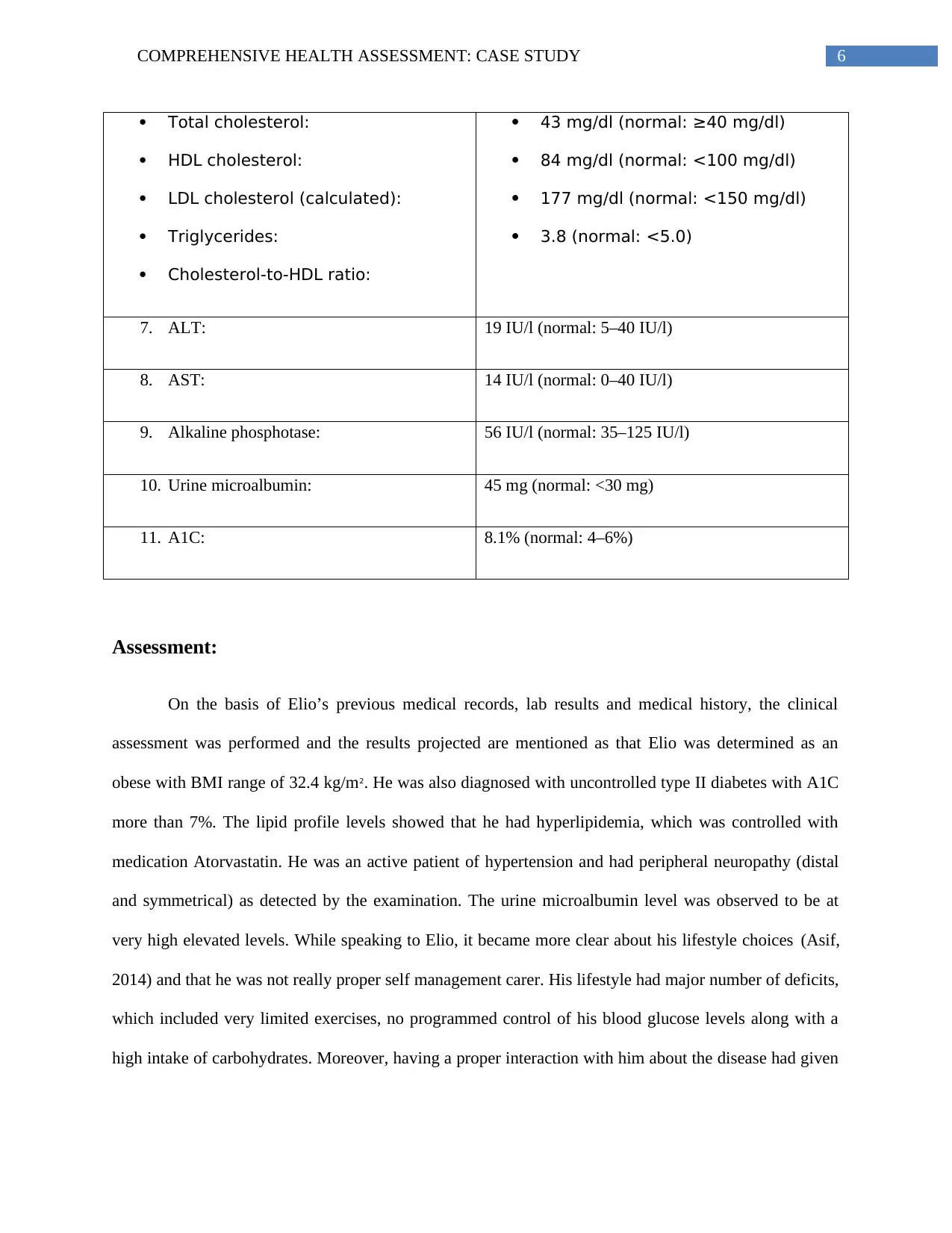
Total cholesterol:
HDL cholesterol:
LDL cholesterol (calculated):
Triglycerides:
Cholesterol-to-HDL ratio:
43 mg/dl (normal: ≥40 mg/dl)
84 mg/dl (normal: <100 mg/dl)
177 mg/dl (normal: <150 mg/dl)
3.8 (normal: <5.0)
7. ALT: 19 IU/l (normal: 5–40 IU/l)
8. AST: 14 IU/l (normal: 0–40 IU/l)
9. Alkaline phosphotase: 56 IU/l (normal: 35–125 IU/l)
10. Urine microalbumin: 45 mg (normal: <30 mg)
11. A1C: 8.1% (normal: 4–6%)
Assessment:
On the basis of Elio’s previous medical records, lab results and medical history, the clinical
assessment was performed and the results projected are mentioned as that Elio was determined as an
obese with BMI range of 32.4 kg/m2. He was also diagnosed with uncontrolled type II diabetes with A1C
more than 7%. The lipid profile levels showed that he had hyperlipidemia, which was controlled with
medication Atorvastatin. He was an active patient of hypertension and had peripheral neuropathy (distal
and symmetrical) as detected by the examination. The urine microalbumin level was observed to be at
very high elevated levels. While speaking to Elio, it became more clear about his lifestyle choices (Asif,
2014) and that he was not really proper self management carer. His lifestyle had major number of deficits,
which included very limited exercises, no programmed control of his blood glucose levels along with a
high intake of carbohydrates. Moreover, having a proper interaction with him about the disease had given
Total cholesterol:
HDL cholesterol:
LDL cholesterol (calculated):
Triglycerides:
Cholesterol-to-HDL ratio:
43 mg/dl (normal: ≥40 mg/dl)
84 mg/dl (normal: <100 mg/dl)
177 mg/dl (normal: <150 mg/dl)
3.8 (normal: <5.0)
7. ALT: 19 IU/l (normal: 5–40 IU/l)
8. AST: 14 IU/l (normal: 0–40 IU/l)
9. Alkaline phosphotase: 56 IU/l (normal: 35–125 IU/l)
10. Urine microalbumin: 45 mg (normal: <30 mg)
11. A1C: 8.1% (normal: 4–6%)
Assessment:
On the basis of Elio’s previous medical records, lab results and medical history, the clinical
assessment was performed and the results projected are mentioned as that Elio was determined as an
obese with BMI range of 32.4 kg/m2. He was also diagnosed with uncontrolled type II diabetes with A1C
more than 7%. The lipid profile levels showed that he had hyperlipidemia, which was controlled with
medication Atorvastatin. He was an active patient of hypertension and had peripheral neuropathy (distal
and symmetrical) as detected by the examination. The urine microalbumin level was observed to be at
very high elevated levels. While speaking to Elio, it became more clear about his lifestyle choices (Asif,
2014) and that he was not really proper self management carer. His lifestyle had major number of deficits,
which included very limited exercises, no programmed control of his blood glucose levels along with a
high intake of carbohydrates. Moreover, having a proper interaction with him about the disease had given
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

7COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
a clear idea that Elio had a very poor knowledge about his diagnosed diseases and that he needed proper
education to practice self care and management.
Analysis and Synthesis of the Findings to determine a perfect health plan as a Nurse
Practitioner:
The first duty of the nurse that delivered medical services was to pick and organize the medical
treatment to resolve the most urgent health-care concerns (Edvardsson, Watt & Pearce, 2017). While Elio
claimed that his desire to lose some weight was his primary motivation to pursue advanced diabetes
treatment, he still wanted to tackle his accelerated rates of glucose and his hypertension at the initial visit.
The patient and his wife decided first step was a recommendation to a dietitian. Elio also admitted that he
had no nutritional guidance (MacLeod et al, 2017) to aid him maintain weight reduction, and that he was
overweight and "embarrassing" at present. He acknowledged that big amounts of bread and pasta
impaired his glucose regulation and decided to continue enhancing food management by rising his
serving size by one-third throughout the week prior to his nutritional appointment. Weight reduction will
also be a major first step toward raising the blood pressure. As a nurse, the first step conducted was to
book an appointment for Elio to undergo a nutrition therapy session (Ekong & Kavookjian, 2016)
from a registered dietician (RD). The therapy was mainly focused on loss of weight and ways to
implement better control of diabetes. The RD also recommended that the patient maintain a diet (Sami et
al., 2017) log reporting his food consumption at meals and snacks over the following week. She told the
patient to seek to guess portion amounts, too. While his physical activity had improved after he retired, it
was relatively intermittent and reliant on conditions. He discovered after some reflection that a week or
more would often pass without any meaningful type of exercise, and that much of his exercise was
seasonal.
Elio's wife proposed during the continuing conversation that the two of them could walk after
breakfast each morning. He also thought that the safest option for having adequate exercise in inclement
a clear idea that Elio had a very poor knowledge about his diagnosed diseases and that he needed proper
education to practice self care and management.
Analysis and Synthesis of the Findings to determine a perfect health plan as a Nurse
Practitioner:
The first duty of the nurse that delivered medical services was to pick and organize the medical
treatment to resolve the most urgent health-care concerns (Edvardsson, Watt & Pearce, 2017). While Elio
claimed that his desire to lose some weight was his primary motivation to pursue advanced diabetes
treatment, he still wanted to tackle his accelerated rates of glucose and his hypertension at the initial visit.
The patient and his wife decided first step was a recommendation to a dietitian. Elio also admitted that he
had no nutritional guidance (MacLeod et al, 2017) to aid him maintain weight reduction, and that he was
overweight and "embarrassing" at present. He acknowledged that big amounts of bread and pasta
impaired his glucose regulation and decided to continue enhancing food management by rising his
serving size by one-third throughout the week prior to his nutritional appointment. Weight reduction will
also be a major first step toward raising the blood pressure. As a nurse, the first step conducted was to
book an appointment for Elio to undergo a nutrition therapy session (Ekong & Kavookjian, 2016)
from a registered dietician (RD). The therapy was mainly focused on loss of weight and ways to
implement better control of diabetes. The RD also recommended that the patient maintain a diet (Sami et
al., 2017) log reporting his food consumption at meals and snacks over the following week. She told the
patient to seek to guess portion amounts, too. While his physical activity had improved after he retired, it
was relatively intermittent and reliant on conditions. He discovered after some reflection that a week or
more would often pass without any meaningful type of exercise, and that much of his exercise was
seasonal.
Elio's wife proposed during the continuing conversation that the two of them could walk after
breakfast each morning. He also thought that the safest option for having adequate exercise in inclement
8COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
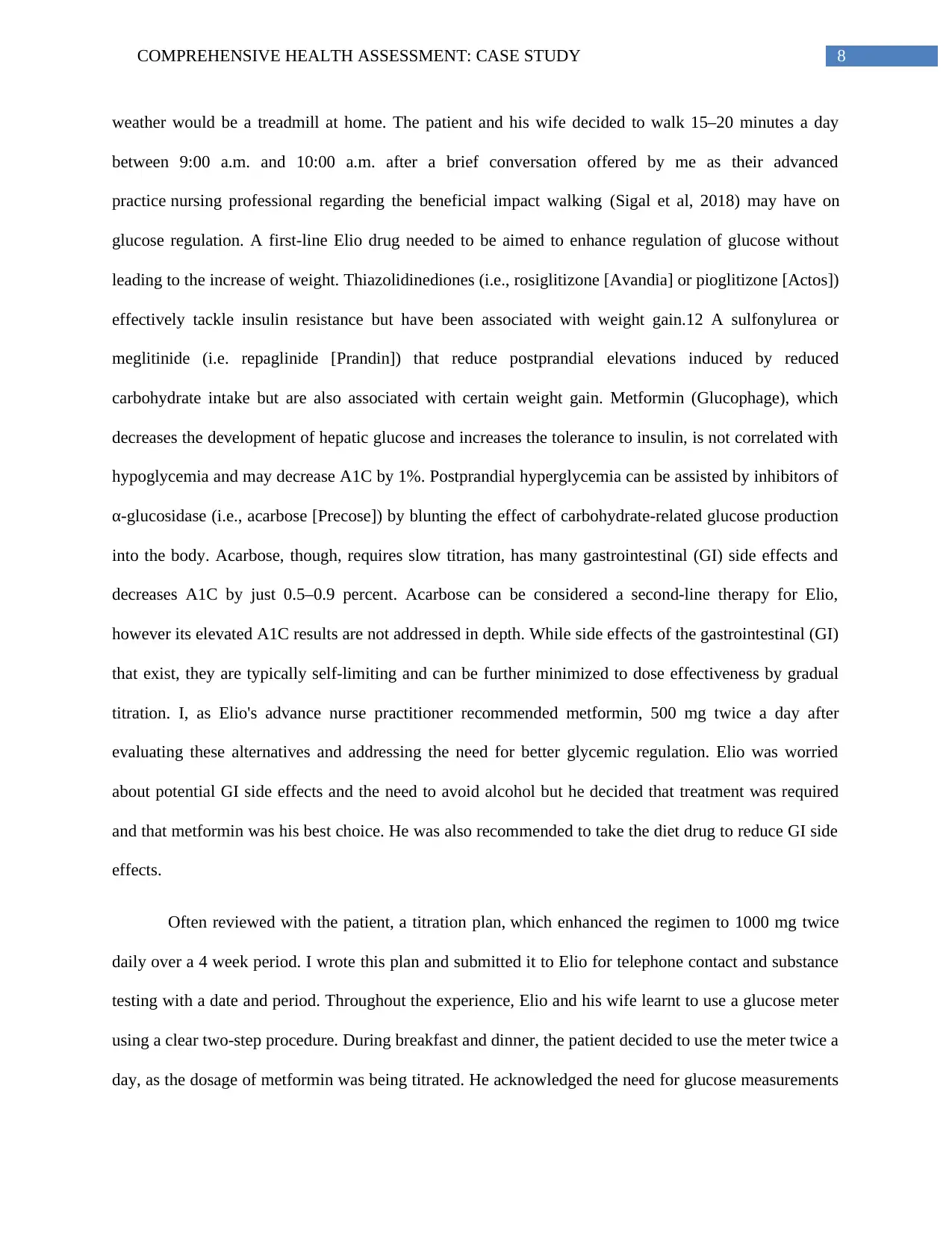
weather would be a treadmill at home. The patient and his wife decided to walk 15–20 minutes a day
between 9:00 a.m. and 10:00 a.m. after a brief conversation offered by me as their advanced
practice nursing professional regarding the beneficial impact walking (Sigal et al, 2018) may have on
glucose regulation. A first-line Elio drug needed to be aimed to enhance regulation of glucose without
leading to the increase of weight. Thiazolidinediones (i.e., rosiglitizone [Avandia] or pioglitizone [Actos])
effectively tackle insulin resistance but have been associated with weight gain.12 A sulfonylurea or
meglitinide (i.e. repaglinide [Prandin]) that reduce postprandial elevations induced by reduced
carbohydrate intake but are also associated with certain weight gain. Metformin (Glucophage), which
decreases the development of hepatic glucose and increases the tolerance to insulin, is not correlated with
hypoglycemia and may decrease A1C by 1%. Postprandial hyperglycemia can be assisted by inhibitors of
α-glucosidase (i.e., acarbose [Precose]) by blunting the effect of carbohydrate-related glucose production
into the body. Acarbose, though, requires slow titration, has many gastrointestinal (GI) side effects and
decreases A1C by just 0.5–0.9 percent. Acarbose can be considered a second-line therapy for Elio,
however its elevated A1C results are not addressed in depth. While side effects of the gastrointestinal (GI)
that exist, they are typically self-limiting and can be further minimized to dose effectiveness by gradual
titration. I, as Elio's advance nurse practitioner recommended metformin, 500 mg twice a day after
evaluating these alternatives and addressing the need for better glycemic regulation. Elio was worried
about potential GI side effects and the need to avoid alcohol but he decided that treatment was required
and that metformin was his best choice. He was also recommended to take the diet drug to reduce GI side
effects.
Often reviewed with the patient, a titration plan, which enhanced the regimen to 1000 mg twice
daily over a 4 week period. I wrote this plan and submitted it to Elio for telephone contact and substance
testing with a date and period. Throughout the experience, Elio and his wife learnt to use a glucose meter
using a clear two-step procedure. During breakfast and dinner, the patient decided to use the meter twice a
day, as the dosage of metformin was being titrated. He acknowledged the need for glucose measurements
weather would be a treadmill at home. The patient and his wife decided to walk 15–20 minutes a day
between 9:00 a.m. and 10:00 a.m. after a brief conversation offered by me as their advanced
practice nursing professional regarding the beneficial impact walking (Sigal et al, 2018) may have on
glucose regulation. A first-line Elio drug needed to be aimed to enhance regulation of glucose without
leading to the increase of weight. Thiazolidinediones (i.e., rosiglitizone [Avandia] or pioglitizone [Actos])
effectively tackle insulin resistance but have been associated with weight gain.12 A sulfonylurea or
meglitinide (i.e. repaglinide [Prandin]) that reduce postprandial elevations induced by reduced
carbohydrate intake but are also associated with certain weight gain. Metformin (Glucophage), which
decreases the development of hepatic glucose and increases the tolerance to insulin, is not correlated with
hypoglycemia and may decrease A1C by 1%. Postprandial hyperglycemia can be assisted by inhibitors of
α-glucosidase (i.e., acarbose [Precose]) by blunting the effect of carbohydrate-related glucose production
into the body. Acarbose, though, requires slow titration, has many gastrointestinal (GI) side effects and
decreases A1C by just 0.5–0.9 percent. Acarbose can be considered a second-line therapy for Elio,
however its elevated A1C results are not addressed in depth. While side effects of the gastrointestinal (GI)
that exist, they are typically self-limiting and can be further minimized to dose effectiveness by gradual
titration. I, as Elio's advance nurse practitioner recommended metformin, 500 mg twice a day after
evaluating these alternatives and addressing the need for better glycemic regulation. Elio was worried
about potential GI side effects and the need to avoid alcohol but he decided that treatment was required
and that metformin was his best choice. He was also recommended to take the diet drug to reduce GI side
effects.
Often reviewed with the patient, a titration plan, which enhanced the regimen to 1000 mg twice
daily over a 4 week period. I wrote this plan and submitted it to Elio for telephone contact and substance
testing with a date and period. Throughout the experience, Elio and his wife learnt to use a glucose meter
using a clear two-step procedure. During breakfast and dinner, the patient decided to use the meter twice a
day, as the dosage of metformin was being titrated. He acknowledged the need for glucose measurements
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

9COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
to monitor drug choice and determine the results of his dietary adjustments, but he thought it wasn't going
to be "one thing forever." While both the severity of hypertension and the occurrence of
microalbuminuria recommended the usage of an ACE inhibitor, the medical decision to wait until the
next doctor visit would help assess the need for antihypertensive care and also give the patient and his
wife opportunity to examine the benefit of this pharmacotherapy integration. They also had the chance to
read several posts about the dangers of avoiding diabetes. Nevertheless, both the individual and his wife
shared a deep willingness to concentrate their attention on diet and physical activity improvements.
Moreover, I was able to inform Elio and his wife about the importance of foot care in diabetic patients
and also further, explained the loss of peripheral neuropathy, which indicated that he will have to be more
diligent in testing his feet for every kind of skin abnormalities induced by improperly fitted boots worn
throughout exercise.
Conclusion:
Advanced practicing nurses are best qualified for having an active part in training and treating
individuals with diabetes medicinally. The integration of nursing knowledge and teaching and coaching
experience improves treatment provision in a manner that is both cost-cutting and effective. The case
study discussed states that as a nursing practitioner, Elio was assured that the nursing care plan would be
discussed with him and that he will be well informed about the alterations of his case. The concept of
mutual accountability for health-care performance is implicit in the position of advanced professional
nurses. This nurse-patient relationship not only enhances treatment but also reinforces the position of the
patient as the self-manager. Moreover, involving Elio, in deciding and discussing the changes can help in
better analysis of the diagnostics and protocol, along with facilitating the continuation of care and keep
the pathways to openly communicate with the patient openly.
to monitor drug choice and determine the results of his dietary adjustments, but he thought it wasn't going
to be "one thing forever." While both the severity of hypertension and the occurrence of
microalbuminuria recommended the usage of an ACE inhibitor, the medical decision to wait until the
next doctor visit would help assess the need for antihypertensive care and also give the patient and his
wife opportunity to examine the benefit of this pharmacotherapy integration. They also had the chance to
read several posts about the dangers of avoiding diabetes. Nevertheless, both the individual and his wife
shared a deep willingness to concentrate their attention on diet and physical activity improvements.
Moreover, I was able to inform Elio and his wife about the importance of foot care in diabetic patients
and also further, explained the loss of peripheral neuropathy, which indicated that he will have to be more
diligent in testing his feet for every kind of skin abnormalities induced by improperly fitted boots worn
throughout exercise.
Conclusion:
Advanced practicing nurses are best qualified for having an active part in training and treating
individuals with diabetes medicinally. The integration of nursing knowledge and teaching and coaching
experience improves treatment provision in a manner that is both cost-cutting and effective. The case
study discussed states that as a nursing practitioner, Elio was assured that the nursing care plan would be
discussed with him and that he will be well informed about the alterations of his case. The concept of
mutual accountability for health-care performance is implicit in the position of advanced professional
nurses. This nurse-patient relationship not only enhances treatment but also reinforces the position of the
patient as the self-manager. Moreover, involving Elio, in deciding and discussing the changes can help in
better analysis of the diagnostics and protocol, along with facilitating the continuation of care and keep
the pathways to openly communicate with the patient openly.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
References:
American Diabetes Association. (2014). Diagnosis and classification of diabetes mellitus. Diabetes
care, 37(Supplement 1), S81-S90.
American Diabetes Association. (2016). Standards of medical care in diabetes—2016 abridged for
primary care providers. Clinical diabetes: a publication of the American Diabetes
Association, 34(1), 3.
American Diabetes Association. (2018). 11. Older adults: standards of medical care in diabetes—
2018. Diabetes Care, 41(Supplement 1), S119-S125.
American Diabetes Association. (2018). 4. Lifestyle management: standards of medical care in diabetes—
2018. Diabetes Care, 41(Supplement 1), S38-S50.
Asif, M. (2014). The prevention and control the type-2 diabetes by changing lifestyle and dietary
pattern. Journal of education and health promotion, 3.
Dunphy, L. M., Winland-Brown, J., Porter, B., & Thomas, D. (2015). Primary care: Art and science of
advanced practice nursing. FA Davis.
Edvardsson, D., Watt, E., & Pearce, F. (2017). Patient experiences of caring and person‐centredness are
associated with perceived nursing care quality. Journal of advanced nursing, 73(1), 217-227.
Ekong, G., & Kavookjian, J. (2016). Motivational interviewing and outcomes in adults with type 2
diabetes: a systematic review. Patient education and counseling, 99(6), 944-952.
Evert, A. B., Boucher, J. L., Cypress, M., Dunbar, S. A., Franz, M. J., Mayer-Davis, E. J., ... & Yancy, W.
S. (2014). Nutrition therapy recommendations for the management of adults with
diabetes. Diabetes care, 37(Supplement 1), S120-S143.
References:
American Diabetes Association. (2014). Diagnosis and classification of diabetes mellitus. Diabetes
care, 37(Supplement 1), S81-S90.
American Diabetes Association. (2016). Standards of medical care in diabetes—2016 abridged for
primary care providers. Clinical diabetes: a publication of the American Diabetes
Association, 34(1), 3.
American Diabetes Association. (2018). 11. Older adults: standards of medical care in diabetes—
2018. Diabetes Care, 41(Supplement 1), S119-S125.
American Diabetes Association. (2018). 4. Lifestyle management: standards of medical care in diabetes—
2018. Diabetes Care, 41(Supplement 1), S38-S50.
Asif, M. (2014). The prevention and control the type-2 diabetes by changing lifestyle and dietary
pattern. Journal of education and health promotion, 3.
Dunphy, L. M., Winland-Brown, J., Porter, B., & Thomas, D. (2015). Primary care: Art and science of
advanced practice nursing. FA Davis.
Edvardsson, D., Watt, E., & Pearce, F. (2017). Patient experiences of caring and person‐centredness are
associated with perceived nursing care quality. Journal of advanced nursing, 73(1), 217-227.
Ekong, G., & Kavookjian, J. (2016). Motivational interviewing and outcomes in adults with type 2
diabetes: a systematic review. Patient education and counseling, 99(6), 944-952.
Evert, A. B., Boucher, J. L., Cypress, M., Dunbar, S. A., Franz, M. J., Mayer-Davis, E. J., ... & Yancy, W.
S. (2014). Nutrition therapy recommendations for the management of adults with
diabetes. Diabetes care, 37(Supplement 1), S120-S143.
11COMPREHENSIVE HEALTH ASSESSMENT: CASE STUDY
Greenwood, D. A., Gee, P. M., Fatkin, K. J., & Peeples, M. (2017). A systematic review of reviews
evaluating technology-enabled diabetes self-management education and support. Journal of
diabetes science and technology, 11(5), 1015-1027.
Inzucchi, S. E., Bergenstal, R. M., Buse, J. B., Diamant, M., Ferrannini, E., Nauck, M., ... & Matthews,
D. R. (2015). Management of hyperglycaemia in type 2 diabetes, 2015: a patient-centred
approach. Update to a position statement of the American Diabetes Association and the European
Association for the Study of Diabetes. Diabetologia, 58(3), 429-442.
Kleinpell, R., Scanlon, A., Hibbert, D., Ganz, F., East, L., Fraser, D., ... & Beauchesne, M. (2014).
Addressing issues impacting advanced nursing practice worldwide. Online J Issues Nurs, 19(2),
5.
MacLeod, J., Franz, M. J., Handu, D., Gradwell, E., Brown, C., Evert, A., ... & Robinson, M. (2017).
Academy of Nutrition and Dietetics nutrition practice guideline for type 1 and type 2 diabetes in
adults: nutrition intervention evidence reviews and recommendations. Journal of the Academy of
Nutrition and Dietetics, 117(10), 1637-1658.
Morilla-Herrera, J. C., Garcia-Mayor, S., Martín-Santos, F. J., Uttumchandani, S. K., Campos, Á. L.,
Bautista, J. C., & Morales-Asencio, J. M. (2016). A systematic review of the effectiveness and
roles of advanced practice nursing in older people. International journal of nursing studies, 53,
290-307.
Odgers‐Jewell, K., Ball, L. E., Kelly, J. T., Isenring, E. A., Reidlinger, D. P., & Thomas, R. (2017).
Effectiveness of group‐based self‐management education for individuals with Type 2 diabetes: a
systematic review with meta‐analyses and meta‐regression. Diabetic Medicine, 34(8), 1027-1039.
Rolfe, G. (2014). Understanding advanced nursing practice. Nursing times, 110(27), 20-23.
Greenwood, D. A., Gee, P. M., Fatkin, K. J., & Peeples, M. (2017). A systematic review of reviews
evaluating technology-enabled diabetes self-management education and support. Journal of
diabetes science and technology, 11(5), 1015-1027.
Inzucchi, S. E., Bergenstal, R. M., Buse, J. B., Diamant, M., Ferrannini, E., Nauck, M., ... & Matthews,
D. R. (2015). Management of hyperglycaemia in type 2 diabetes, 2015: a patient-centred
approach. Update to a position statement of the American Diabetes Association and the European
Association for the Study of Diabetes. Diabetologia, 58(3), 429-442.
Kleinpell, R., Scanlon, A., Hibbert, D., Ganz, F., East, L., Fraser, D., ... & Beauchesne, M. (2014).
Addressing issues impacting advanced nursing practice worldwide. Online J Issues Nurs, 19(2),
5.
MacLeod, J., Franz, M. J., Handu, D., Gradwell, E., Brown, C., Evert, A., ... & Robinson, M. (2017).
Academy of Nutrition and Dietetics nutrition practice guideline for type 1 and type 2 diabetes in
adults: nutrition intervention evidence reviews and recommendations. Journal of the Academy of
Nutrition and Dietetics, 117(10), 1637-1658.
Morilla-Herrera, J. C., Garcia-Mayor, S., Martín-Santos, F. J., Uttumchandani, S. K., Campos, Á. L.,
Bautista, J. C., & Morales-Asencio, J. M. (2016). A systematic review of the effectiveness and
roles of advanced practice nursing in older people. International journal of nursing studies, 53,
290-307.
Odgers‐Jewell, K., Ball, L. E., Kelly, J. T., Isenring, E. A., Reidlinger, D. P., & Thomas, R. (2017).
Effectiveness of group‐based self‐management education for individuals with Type 2 diabetes: a
systematic review with meta‐analyses and meta‐regression. Diabetic Medicine, 34(8), 1027-1039.
Rolfe, G. (2014). Understanding advanced nursing practice. Nursing times, 110(27), 20-23.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





