NURBN 3018: Peer Teaching Plan on Type 1 Diabetes Management
VerifiedAdded on 2022/09/07
|8
|1744
|17
Practical Assignment
AI Summary
This assignment presents a comprehensive teaching plan designed for nursing students, focusing on the management of type 1 diabetes. The plan, developed for a 12-minute teaching session, outlines specific lesson objectives, targeting patient education on self-management techniques. It details the session's structure, including a welcome, group activities, individual tasks, visual aids, and evaluation methods. The plan incorporates various learning modalities such as auditory, visual, logic, social, verbal, physical, and tactile approaches to cater to diverse learning styles. It emphasizes the importance of patient education during discharge, particularly on blood glucose monitoring, medication, nutrition, and risk reduction. The plan also includes a detailed evaluation component, assessing student understanding through active participation and individual tasks. The assignment concludes with a statement on group collaboration, highlighting the roles and contributions of each team member. References to relevant research papers are also included to support the strategies used in the teaching plan.

Running head: LEADERSHIP FOR CLINICAL PRACTICE 1
LEADERSHIP FOR CLINICAL PRACTICE
Student’s Names
Institutional Affiliation
LEADERSHIP FOR CLINICAL PRACTICE
Student’s Names
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

LEADERSHIP FOR CLINICAL PRACTICE 2
Leadership for Clinical Practice
Type 1 diabetes is a life- long ailment that is caused by a high sugar level in the blood. The body is able to generate insulin which can cause
complication over a period of time. It often causes damages of kidneys, eye and nerves which can lead to stroke. Patient education is a
fundamental aspect during discharge to reduce readmissions and complications (Peter et al., 2015). Thus the ultimate goal for a discharge plan
especially for the patient with type I diabetes is to well equip the patient with appropriate survival skills that will enable him to manage and be
responsible for his personal welfare. The key aspect of a transition plan is self- management education. In addition, it has also been noted that
inpatient education has an impact on the early discharge of the patient (Shin, Park & Kim, 2015). They are 3 phases of patient education that
comprise of continuing education, depth education and survival or acute education. All these types of education empower the diabetes patient on
areas such as foot care, nutrition, physical activity, medication and risk reduction. The basis of education is to maintain glycaemia, avoid
diabetes crisis and manage medicine.
The teaching sessions are guided by the learning theories such as behaviourism, cognitivism, constructivism and humanism. These theories
provide illustrations on the manner individuals are able to acquire organize, deploy knowledge and skills. On the other hand, the learning styles
that would be effective during discharge plan comprise of auditory learning, visual learning, logic learning, social learning, verbal learning and
physical learning.
Leadership for Clinical Practice
Type 1 diabetes is a life- long ailment that is caused by a high sugar level in the blood. The body is able to generate insulin which can cause
complication over a period of time. It often causes damages of kidneys, eye and nerves which can lead to stroke. Patient education is a
fundamental aspect during discharge to reduce readmissions and complications (Peter et al., 2015). Thus the ultimate goal for a discharge plan
especially for the patient with type I diabetes is to well equip the patient with appropriate survival skills that will enable him to manage and be
responsible for his personal welfare. The key aspect of a transition plan is self- management education. In addition, it has also been noted that
inpatient education has an impact on the early discharge of the patient (Shin, Park & Kim, 2015). They are 3 phases of patient education that
comprise of continuing education, depth education and survival or acute education. All these types of education empower the diabetes patient on
areas such as foot care, nutrition, physical activity, medication and risk reduction. The basis of education is to maintain glycaemia, avoid
diabetes crisis and manage medicine.
The teaching sessions are guided by the learning theories such as behaviourism, cognitivism, constructivism and humanism. These theories
provide illustrations on the manner individuals are able to acquire organize, deploy knowledge and skills. On the other hand, the learning styles
that would be effective during discharge plan comprise of auditory learning, visual learning, logic learning, social learning, verbal learning and
physical learning.
LEADERSHIP FOR CLINICAL PRACTICE 3
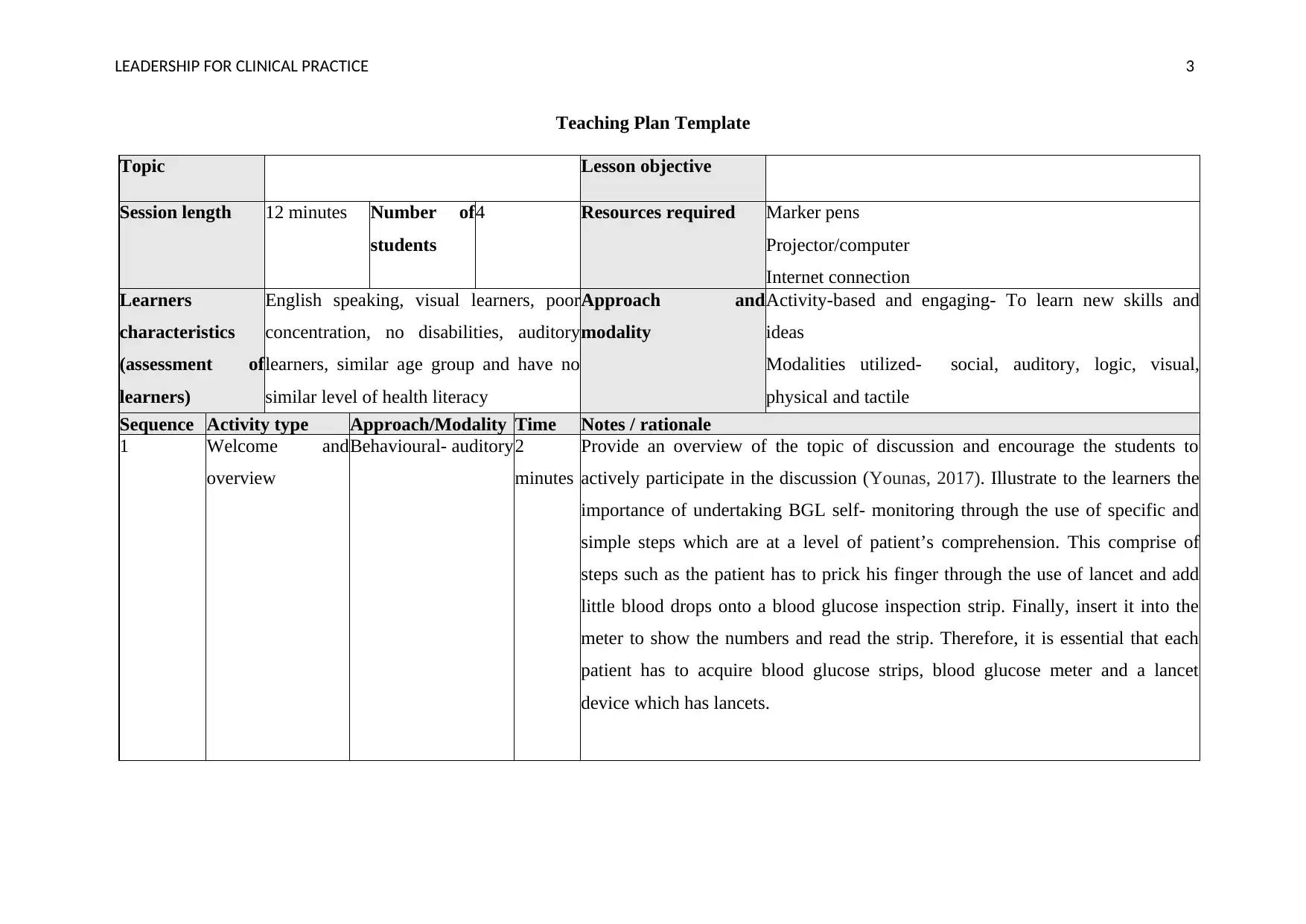
Teaching Plan Template
Topic Lesson objective
Session length 12 minutes Number of
students
4 Resources required Marker pens
Projector/computer
Internet connection
Learners
characteristics
(assessment of
learners)
English speaking, visual learners, poor
concentration, no disabilities, auditory
learners, similar age group and have no
similar level of health literacy
Approach and
modality
Activity-based and engaging- To learn new skills and
ideas
Modalities utilized- social, auditory, logic, visual,
physical and tactile
Sequence Activity type Approach/Modality Time Notes / rationale
1 Welcome and
overview
Behavioural- auditory2
minutes
Provide an overview of the topic of discussion and encourage the students to
actively participate in the discussion (Younas, 2017). Illustrate to the learners the
importance of undertaking BGL self- monitoring through the use of specific and
simple steps which are at a level of patient’s comprehension. This comprise of
steps such as the patient has to prick his finger through the use of lancet and add
little blood drops onto a blood glucose inspection strip. Finally, insert it into the
meter to show the numbers and read the strip. Therefore, it is essential that each
patient has to acquire blood glucose strips, blood glucose meter and a lancet
device which has lancets.
Teaching Plan Template
Topic Lesson objective
Session length 12 minutes Number of
students
4 Resources required Marker pens
Projector/computer
Internet connection
Learners
characteristics
(assessment of
learners)
English speaking, visual learners, poor
concentration, no disabilities, auditory
learners, similar age group and have no
similar level of health literacy
Approach and
modality
Activity-based and engaging- To learn new skills and
ideas
Modalities utilized- social, auditory, logic, visual,
physical and tactile
Sequence Activity type Approach/Modality Time Notes / rationale
1 Welcome and
overview
Behavioural- auditory2
minutes
Provide an overview of the topic of discussion and encourage the students to
actively participate in the discussion (Younas, 2017). Illustrate to the learners the
importance of undertaking BGL self- monitoring through the use of specific and
simple steps which are at a level of patient’s comprehension. This comprise of
steps such as the patient has to prick his finger through the use of lancet and add
little blood drops onto a blood glucose inspection strip. Finally, insert it into the
meter to show the numbers and read the strip. Therefore, it is essential that each
patient has to acquire blood glucose strips, blood glucose meter and a lancet
device which has lancets.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LEADERSHIP FOR CLINICAL PRACTICE 4
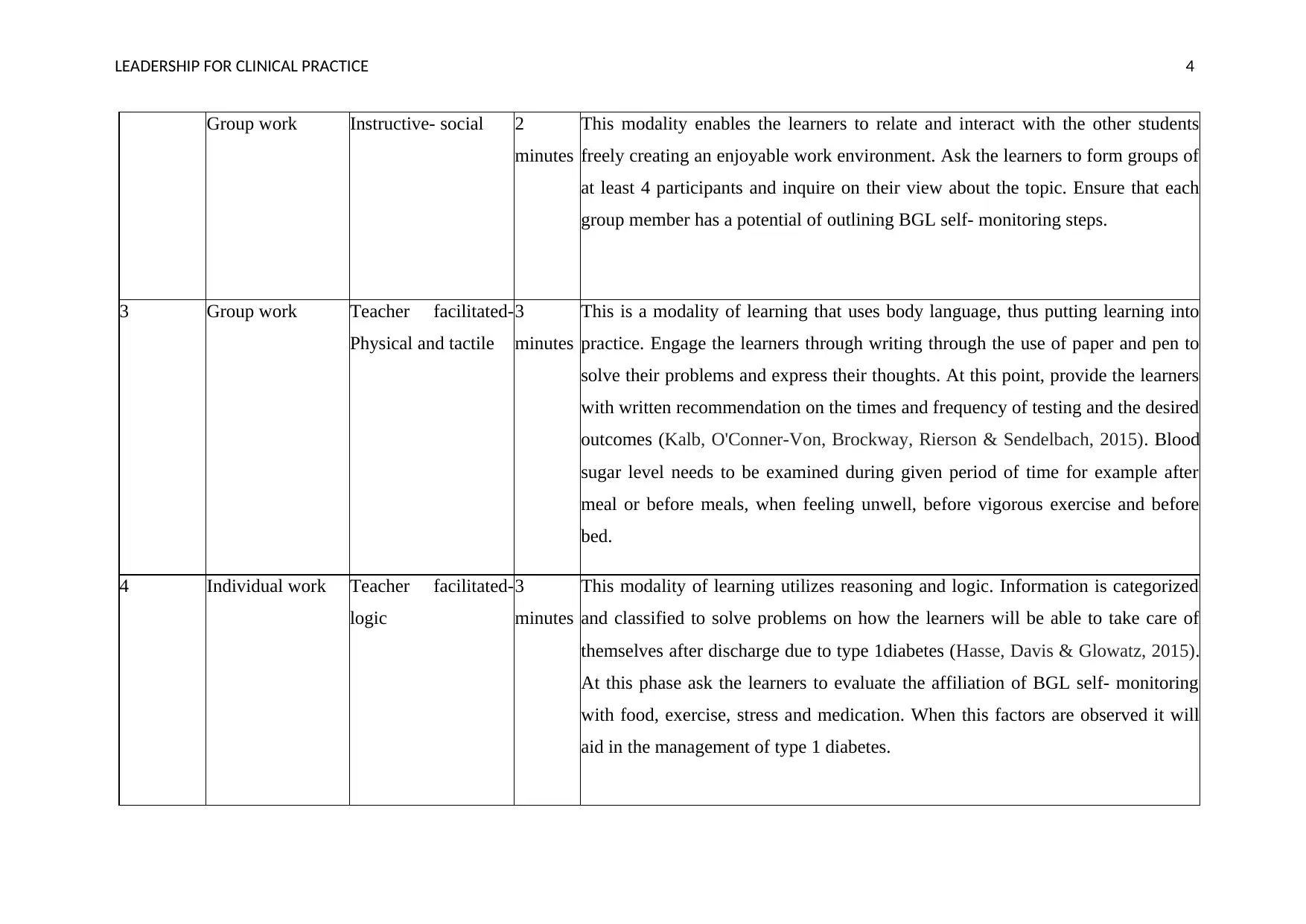
Group work Instructive- social 2
minutes
This modality enables the learners to relate and interact with the other students
freely creating an enjoyable work environment. Ask the learners to form groups of
at least 4 participants and inquire on their view about the topic. Ensure that each
group member has a potential of outlining BGL self- monitoring steps.
3 Group work Teacher facilitated-
Physical and tactile
3
minutes
This is a modality of learning that uses body language, thus putting learning into
practice. Engage the learners through writing through the use of paper and pen to
solve their problems and express their thoughts. At this point, provide the learners
with written recommendation on the times and frequency of testing and the desired
outcomes (Kalb, O'Conner-Von, Brockway, Rierson & Sendelbach, 2015). Blood
sugar level needs to be examined during given period of time for example after
meal or before meals, when feeling unwell, before vigorous exercise and before
bed.
4 Individual work Teacher facilitated-
logic
3
minutes
This modality of learning utilizes reasoning and logic. Information is categorized
and classified to solve problems on how the learners will be able to take care of
themselves after discharge due to type 1diabetes (Hasse, Davis & Glowatz, 2015).
At this phase ask the learners to evaluate the affiliation of BGL self- monitoring
with food, exercise, stress and medication. When this factors are observed it will
aid in the management of type 1 diabetes.
Group work Instructive- social 2
minutes
This modality enables the learners to relate and interact with the other students
freely creating an enjoyable work environment. Ask the learners to form groups of
at least 4 participants and inquire on their view about the topic. Ensure that each
group member has a potential of outlining BGL self- monitoring steps.
3 Group work Teacher facilitated-
Physical and tactile
3
minutes
This is a modality of learning that uses body language, thus putting learning into
practice. Engage the learners through writing through the use of paper and pen to
solve their problems and express their thoughts. At this point, provide the learners
with written recommendation on the times and frequency of testing and the desired
outcomes (Kalb, O'Conner-Von, Brockway, Rierson & Sendelbach, 2015). Blood
sugar level needs to be examined during given period of time for example after
meal or before meals, when feeling unwell, before vigorous exercise and before
bed.
4 Individual work Teacher facilitated-
logic
3
minutes
This modality of learning utilizes reasoning and logic. Information is categorized
and classified to solve problems on how the learners will be able to take care of
themselves after discharge due to type 1diabetes (Hasse, Davis & Glowatz, 2015).
At this phase ask the learners to evaluate the affiliation of BGL self- monitoring
with food, exercise, stress and medication. When this factors are observed it will
aid in the management of type 1 diabetes.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LEADERSHIP FOR CLINICAL PRACTICE 5
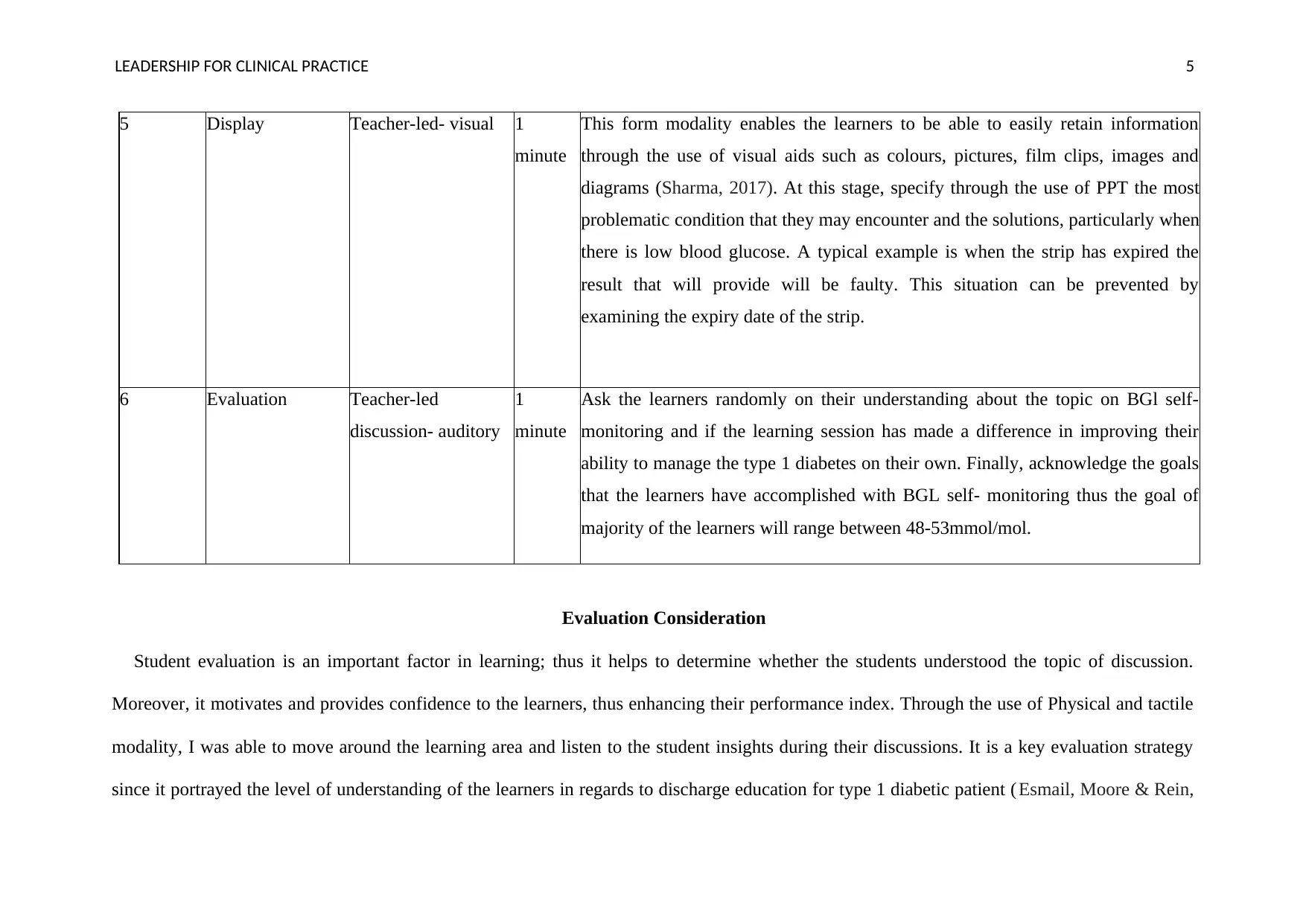
5 Display Teacher-led- visual 1
minute
This form modality enables the learners to be able to easily retain information
through the use of visual aids such as colours, pictures, film clips, images and
diagrams (Sharma, 2017). At this stage, specify through the use of PPT the most
problematic condition that they may encounter and the solutions, particularly when
there is low blood glucose. A typical example is when the strip has expired the
result that will provide will be faulty. This situation can be prevented by
examining the expiry date of the strip.
6 Evaluation Teacher-led
discussion- auditory
1
minute
Ask the learners randomly on their understanding about the topic on BGl self-
monitoring and if the learning session has made a difference in improving their
ability to manage the type 1 diabetes on their own. Finally, acknowledge the goals
that the learners have accomplished with BGL self- monitoring thus the goal of
majority of the learners will range between 48-53mmol/mol.
Evaluation Consideration
Student evaluation is an important factor in learning; thus it helps to determine whether the students understood the topic of discussion.
Moreover, it motivates and provides confidence to the learners, thus enhancing their performance index. Through the use of Physical and tactile
modality, I was able to move around the learning area and listen to the student insights during their discussions. It is a key evaluation strategy
since it portrayed the level of understanding of the learners in regards to discharge education for type 1 diabetic patient ( Esmail, Moore & Rein,
5 Display Teacher-led- visual 1
minute
This form modality enables the learners to be able to easily retain information
through the use of visual aids such as colours, pictures, film clips, images and
diagrams (Sharma, 2017). At this stage, specify through the use of PPT the most
problematic condition that they may encounter and the solutions, particularly when
there is low blood glucose. A typical example is when the strip has expired the
result that will provide will be faulty. This situation can be prevented by
examining the expiry date of the strip.
6 Evaluation Teacher-led
discussion- auditory
1
minute
Ask the learners randomly on their understanding about the topic on BGl self-
monitoring and if the learning session has made a difference in improving their
ability to manage the type 1 diabetes on their own. Finally, acknowledge the goals
that the learners have accomplished with BGL self- monitoring thus the goal of
majority of the learners will range between 48-53mmol/mol.
Evaluation Consideration
Student evaluation is an important factor in learning; thus it helps to determine whether the students understood the topic of discussion.
Moreover, it motivates and provides confidence to the learners, thus enhancing their performance index. Through the use of Physical and tactile
modality, I was able to move around the learning area and listen to the student insights during their discussions. It is a key evaluation strategy
since it portrayed the level of understanding of the learners in regards to discharge education for type 1 diabetic patient ( Esmail, Moore & Rein,
LEADERSHIP FOR CLINICAL PRACTICE 6
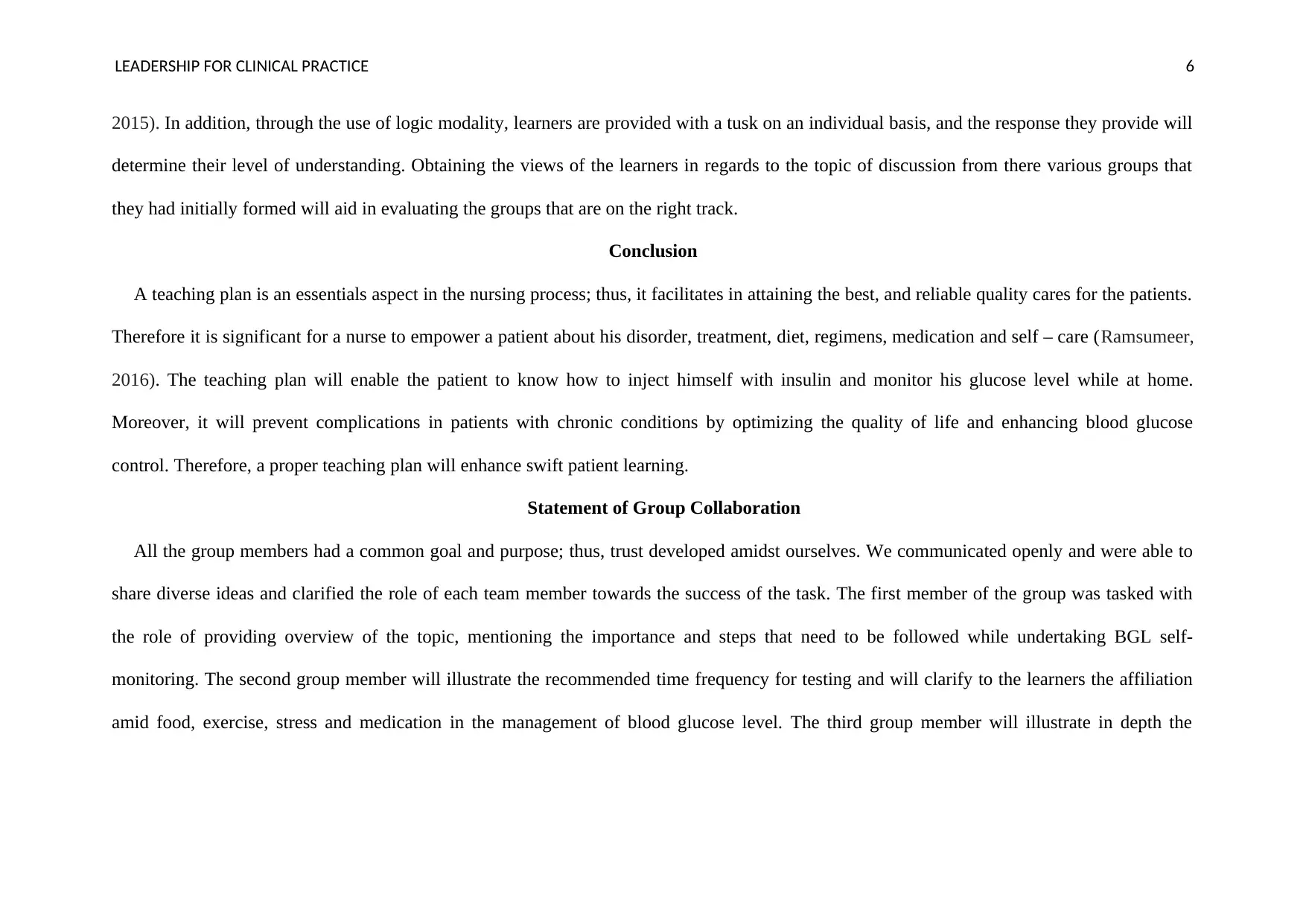
2015). In addition, through the use of logic modality, learners are provided with a tusk on an individual basis, and the response they provide will
determine their level of understanding. Obtaining the views of the learners in regards to the topic of discussion from there various groups that
they had initially formed will aid in evaluating the groups that are on the right track.
Conclusion
A teaching plan is an essentials aspect in the nursing process; thus, it facilitates in attaining the best, and reliable quality cares for the patients.
Therefore it is significant for a nurse to empower a patient about his disorder, treatment, diet, regimens, medication and self – care (Ramsumeer,
2016). The teaching plan will enable the patient to know how to inject himself with insulin and monitor his glucose level while at home.
Moreover, it will prevent complications in patients with chronic conditions by optimizing the quality of life and enhancing blood glucose
control. Therefore, a proper teaching plan will enhance swift patient learning.
Statement of Group Collaboration
All the group members had a common goal and purpose; thus, trust developed amidst ourselves. We communicated openly and were able to
share diverse ideas and clarified the role of each team member towards the success of the task. The first member of the group was tasked with
the role of providing overview of the topic, mentioning the importance and steps that need to be followed while undertaking BGL self-
monitoring. The second group member will illustrate the recommended time frequency for testing and will clarify to the learners the affiliation
amid food, exercise, stress and medication in the management of blood glucose level. The third group member will illustrate in depth the
2015). In addition, through the use of logic modality, learners are provided with a tusk on an individual basis, and the response they provide will
determine their level of understanding. Obtaining the views of the learners in regards to the topic of discussion from there various groups that
they had initially formed will aid in evaluating the groups that are on the right track.
Conclusion
A teaching plan is an essentials aspect in the nursing process; thus, it facilitates in attaining the best, and reliable quality cares for the patients.
Therefore it is significant for a nurse to empower a patient about his disorder, treatment, diet, regimens, medication and self – care (Ramsumeer,
2016). The teaching plan will enable the patient to know how to inject himself with insulin and monitor his glucose level while at home.
Moreover, it will prevent complications in patients with chronic conditions by optimizing the quality of life and enhancing blood glucose
control. Therefore, a proper teaching plan will enhance swift patient learning.
Statement of Group Collaboration
All the group members had a common goal and purpose; thus, trust developed amidst ourselves. We communicated openly and were able to
share diverse ideas and clarified the role of each team member towards the success of the task. The first member of the group was tasked with
the role of providing overview of the topic, mentioning the importance and steps that need to be followed while undertaking BGL self-
monitoring. The second group member will illustrate the recommended time frequency for testing and will clarify to the learners the affiliation
amid food, exercise, stress and medication in the management of blood glucose level. The third group member will illustrate in depth the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LEADERSHIP FOR CLINICAL PRACTICE 7
challenges that the patients may encounter and the solutions. Furthermore, he will acknowledge the goals that the patients have achieved with
BGL self- monitoring.
challenges that the patients may encounter and the solutions. Furthermore, he will acknowledge the goals that the patients have achieved with
BGL self- monitoring.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LEADERSHIP FOR CLINICAL PRACTICE 8
References
Esmail, L., Moore, E., & Rein, A. (2015). Evaluating patient and stakeholder engagement in research: moving from theory to practice. Journal
of comparative effectiveness research, 4(2), 133-145.
Hasse, A. M., Davis, A., & Glowatz, T. (2015). Development of a diabetes learning needs assessment tool to promote an individualized
predischarge patient education plan. The Journal of Continuing Education in Nursing, 46(11), 484-486.
Kalb, K. A., O'Conner-Von, S. K., Brockway, C., Rierson, C. L., & Sendelbach, S. (2015). Evidence-based teaching practice in nursing
education: Faculty perspectives and practices. Nursing education perspectives, 36(4), 212-219.
Peter, D., Robinson, P., Jordan, M., Lawrence, S., Casey, K., & Salas-Lopez, D. (2015). Reducing readmissions using teach-back: enhancing
patient and family education. JONA: The Journal of Nursing Administration, 45(1), 35-42.
Ramsumeer, S. (2016). A plan for the implementation and evaluation of diet education in type 2 diabetes.
Sharma, R. K. (2017). Emerging innovative teaching strategies in nursing. JOJ Nurs Health Care, 1(2).
Shin, S., Park, J. H., & Kim, J. H. (2015). Effectiveness of patient simulation in nursing education: a meta-analysis. Nurse education
today, 35(1), 176-182.
Younas, A. (2017). The nursing process and patient teaching. Nursing Made Incredibly Easy, 15(6), 13-16.
References
Esmail, L., Moore, E., & Rein, A. (2015). Evaluating patient and stakeholder engagement in research: moving from theory to practice. Journal
of comparative effectiveness research, 4(2), 133-145.
Hasse, A. M., Davis, A., & Glowatz, T. (2015). Development of a diabetes learning needs assessment tool to promote an individualized
predischarge patient education plan. The Journal of Continuing Education in Nursing, 46(11), 484-486.
Kalb, K. A., O'Conner-Von, S. K., Brockway, C., Rierson, C. L., & Sendelbach, S. (2015). Evidence-based teaching practice in nursing
education: Faculty perspectives and practices. Nursing education perspectives, 36(4), 212-219.
Peter, D., Robinson, P., Jordan, M., Lawrence, S., Casey, K., & Salas-Lopez, D. (2015). Reducing readmissions using teach-back: enhancing
patient and family education. JONA: The Journal of Nursing Administration, 45(1), 35-42.
Ramsumeer, S. (2016). A plan for the implementation and evaluation of diet education in type 2 diabetes.
Sharma, R. K. (2017). Emerging innovative teaching strategies in nursing. JOJ Nurs Health Care, 1(2).
Shin, S., Park, J. H., & Kim, J. H. (2015). Effectiveness of patient simulation in nursing education: a meta-analysis. Nurse education
today, 35(1), 176-182.
Younas, A. (2017). The nursing process and patient teaching. Nursing Made Incredibly Easy, 15(6), 13-16.
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



