An Analysis of Anatomy, Physiology & Pathophysiology of Diabetes
VerifiedAdded on 2023/06/10
|18
|3872
|198
Essay
AI Summary
This essay provides a detailed analysis of diabetes mellitus, covering the anatomy and physiology of glucose metabolism, the role of insulin and glucagon, and the pathophysiological changes occurring in type 1, type 2, and gestational diabetes. It discusses the symptoms associated with each type and explores potential problems in nursing care, such as hypoglycemia and hyperglycemia. The essay also addresses factors affecting self-esteem in diabetic individuals, issues in diabetes care delivery, environmental and social factors contributing to diabetes in Australia, and the roles of organizations like the NDSS and Diabetes Australia in supporting diabetes care. Desklib offers a platform to access this and many other solved assignments for students.

Running head: DIABETES
Diabetes
Name of the Student
Name of the University
Author Note
Diabetes
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
DIABETES
Part 1: Questions and Answers
Answer 1
Two factors that affects the self of a person with diabetes mellitus include obese or
over-weight body and physically fit people in the vicinity. Due to the obesity body weight a
person suffering from diabetes is suppose to a different diet from others like while others are
enjoy food to their content, a diabetes person is only restricted to salads this create frustration
and low self-esteem causing difficulty in self management of diabetes mellitus. Diabetic
people are asked to do physical exercise however, viewing physically fit people and their
high fitness level of gym creates low self-esteem and thereby generating barrier in self
management (Reyes et al. 2017).
Answer 2
Three issues related to the diabetic care delivery are client specific, political and
cultural issues. For example, people from different cultural background (Australian
aboriginals or Torres Strait Islanders), have different dietary habits and spiritual values and
hence the care plan needs to adjusted accordingly (Pottie et al. 2013). Client specific factors
include co-morbidity with other associated disease (high blood pressure or cardiac problems)
and while procuring the care plan the co-morbidities must be taken into consideration.
Political factors like political unrest creates stress at times leads to diabetes and thus care plan
need to be adjusted accordingly (Monk and Buysse 2013).
Answer 3
Environmental factors contributing to diabetes mellitus in the Australian general
population include increase rate of air and noise pollution along with decrease in greenery
and less free space for walkability (Dendup et al. 2018). Social factors contributing to
DIABETES
Part 1: Questions and Answers
Answer 1
Two factors that affects the self of a person with diabetes mellitus include obese or
over-weight body and physically fit people in the vicinity. Due to the obesity body weight a
person suffering from diabetes is suppose to a different diet from others like while others are
enjoy food to their content, a diabetes person is only restricted to salads this create frustration
and low self-esteem causing difficulty in self management of diabetes mellitus. Diabetic
people are asked to do physical exercise however, viewing physically fit people and their
high fitness level of gym creates low self-esteem and thereby generating barrier in self
management (Reyes et al. 2017).
Answer 2
Three issues related to the diabetic care delivery are client specific, political and
cultural issues. For example, people from different cultural background (Australian
aboriginals or Torres Strait Islanders), have different dietary habits and spiritual values and
hence the care plan needs to adjusted accordingly (Pottie et al. 2013). Client specific factors
include co-morbidity with other associated disease (high blood pressure or cardiac problems)
and while procuring the care plan the co-morbidities must be taken into consideration.
Political factors like political unrest creates stress at times leads to diabetes and thus care plan
need to be adjusted accordingly (Monk and Buysse 2013).
Answer 3
Environmental factors contributing to diabetes mellitus in the Australian general
population include increase rate of air and noise pollution along with decrease in greenery
and less free space for walkability (Dendup et al. 2018). Social factors contributing to
2
DIABETES
diabetes mellitus in the Australian general population include high rate of health inequality,
lack of employment among the aboriginals and associated lifestyle factors like unhealthy diet,
lack of physical exercise and substance abuse (Australian Institute of Health and Welfare
2016).
Answer 4
The high rates of diabetes mellitus experience by the Australian aboriginals and
Torres Strait Islanders (ATSI) because the ATSI resides under the poor social determinants of
health. Poor social determinants of health like poor individual life style factors, lack of proper
sanitation, unhealthy diet, substance abuse, lack of employment and stress lead to high rate of
occurrence of diabetes mellitus among the ATSI (Australian Institute of Health and Welfare
2016).
Answer 5
National Diabetes Services Scheme (NDSS) aims to increase the lifespan of people
living with diabetes in order to understand and promote self-management their condition. An
Australian citizens living with diabetes or non-Australians from another country that shares
health agreements with Australia are able to register under the NDSS. NDSS provide
different diabetes prevention program across different cultural group while increasing
diabetes awareness (NDSS 2017).
Answer 6
Diabetes Australia is a national body that was established in the year 1984 for the
people affected with all types of diabetes and those at high risk of developing diabetes.
Diabetes Australia is committed in reducing the overall impact of diabetes from the
Australian population via providing active leadership, prevention and management. They also
work in close association with the physicians and community members and thereby helping
DIABETES
diabetes mellitus in the Australian general population include high rate of health inequality,
lack of employment among the aboriginals and associated lifestyle factors like unhealthy diet,
lack of physical exercise and substance abuse (Australian Institute of Health and Welfare
2016).
Answer 4
The high rates of diabetes mellitus experience by the Australian aboriginals and
Torres Strait Islanders (ATSI) because the ATSI resides under the poor social determinants of
health. Poor social determinants of health like poor individual life style factors, lack of proper
sanitation, unhealthy diet, substance abuse, lack of employment and stress lead to high rate of
occurrence of diabetes mellitus among the ATSI (Australian Institute of Health and Welfare
2016).
Answer 5
National Diabetes Services Scheme (NDSS) aims to increase the lifespan of people
living with diabetes in order to understand and promote self-management their condition. An
Australian citizens living with diabetes or non-Australians from another country that shares
health agreements with Australia are able to register under the NDSS. NDSS provide
different diabetes prevention program across different cultural group while increasing
diabetes awareness (NDSS 2017).
Answer 6
Diabetes Australia is a national body that was established in the year 1984 for the
people affected with all types of diabetes and those at high risk of developing diabetes.
Diabetes Australia is committed in reducing the overall impact of diabetes from the
Australian population via providing active leadership, prevention and management. They also
work in close association with the physicians and community members and thereby helping
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
DIABETES
to reduce the adverse health impact of diabetes in a comprehensive rate (Diabetes Australia
2017).
Answer 7
Diabetes management via general practitioner (GP) mainly involves proper control
and maintenance of the blood cholesterol level and plasma concentration of HDL, LDL,
triglycerides. GP also takes into account the rate of physical activity, cigarette and alcohol
consumption and blood pressure level (Diabetes Australia 2012).
Answer 8
The role of an endocrinologist is to manage diabetes based on the control and co-
ordination of the endocrine system. They most help in the proper regulation of the insulin
hormone secreted from the pancreatic beta cells (American Diabetes Association 2017).
Answer 9
National Association of Diabetes Centres (NADC) is involved both directly and
indirectly in diabetes care and services. It aim in exploring the mechanisms and subsequent
implementation of the strategies directed towards the improving the standard of care of
diabetic people or people who are at in increased risk of developing diabetes. It also helps to
generates diabetes awareness via providing disease education along with proper support in
primary care and policy development for successful management of the disease (NDAC
2017).
Answer 10
In order to identify the family or carer’s understanding and involvement in a person’s
diabetes care, I would first access his or her level of knowledge in disease management and
disease progress. According to Mendenhall et al. (2012), proper knowledge and disease
DIABETES
to reduce the adverse health impact of diabetes in a comprehensive rate (Diabetes Australia
2017).
Answer 7
Diabetes management via general practitioner (GP) mainly involves proper control
and maintenance of the blood cholesterol level and plasma concentration of HDL, LDL,
triglycerides. GP also takes into account the rate of physical activity, cigarette and alcohol
consumption and blood pressure level (Diabetes Australia 2012).
Answer 8
The role of an endocrinologist is to manage diabetes based on the control and co-
ordination of the endocrine system. They most help in the proper regulation of the insulin
hormone secreted from the pancreatic beta cells (American Diabetes Association 2017).
Answer 9
National Association of Diabetes Centres (NADC) is involved both directly and
indirectly in diabetes care and services. It aim in exploring the mechanisms and subsequent
implementation of the strategies directed towards the improving the standard of care of
diabetic people or people who are at in increased risk of developing diabetes. It also helps to
generates diabetes awareness via providing disease education along with proper support in
primary care and policy development for successful management of the disease (NDAC
2017).
Answer 10
In order to identify the family or carer’s understanding and involvement in a person’s
diabetes care, I would first access his or her level of knowledge in disease management and
disease progress. According to Mendenhall et al. (2012), proper knowledge and disease
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
DIABETES
education of the family member of a diabetes patient helps to increase the overall
involvement of that carer in the therapy plan.
Answer 11
Proper knowledge and understanding of the family or carer in person’s diabetic care
helps to implement effective family based interventions for diabetes management. According
to Baig et al. (2015), family involvement and family based interventions help to improve the
self-efficacy, reduction in disease burden and increase in the overall self-management of the
disease.
DIABETES
education of the family member of a diabetes patient helps to increase the overall
involvement of that carer in the therapy plan.
Answer 11
Proper knowledge and understanding of the family or carer in person’s diabetic care
helps to implement effective family based interventions for diabetes management. According
to Baig et al. (2015), family involvement and family based interventions help to improve the
self-efficacy, reduction in disease burden and increase in the overall self-management of the
disease.

5
DIABETES
Part 2: Essay
Introduction
Diabetes mellitus, commonly known as diabetes and is defined as group of metabolic
disorders which are characterised by high level of blood glucose concentration for a prolong
period of time due to malfunction in insulin metabolism and secretion. There are two types of
diabetes, type 1, type 2 diabetes and gestational diabetes. The common symptoms of diabetes
include high blood sugar or glucose level, frequent urination, increased hunger and thrust
along with body weight imbalance. According to the National Health Survey conducted by
the Australian Bureau of Statistics at least 1.2 million people who are aged over 2 years are
diagnosed with diabetes in Australia. The prevalence of diabetes has doubled in Australia
during the tenure of 2004 to 2014 and have showed high rate of occurrence among the
aboriginals and the Torres Strait Islanders (Australian Government Department of Health
2016). The following essay aims to analyse the anatomy and physiology associated with the
development of diabetes. The essay also aims to throw light over the pathophysiological
changes occurring during different types of diabetes and the associated complication of
diabetes. The essay thus will help the readers to get a rough overview of diabetes.
About Diabetes
Anatomy of physiology of glucose metabolism and absorption
Role of pancreas in glucose metabolism and absorption
Glucose metabolism occurs through glycolysis. In glycolysis single molecule of
glucose is broken down via a series of enzyme-catalyzed reactions in order to yield two
molecules of three carbon compounds known as pyruvate along with the release of energy in
the form of ATP. When the blood glucose level is low, islet of Langerhans in the pancreas
DIABETES
Part 2: Essay
Introduction
Diabetes mellitus, commonly known as diabetes and is defined as group of metabolic
disorders which are characterised by high level of blood glucose concentration for a prolong
period of time due to malfunction in insulin metabolism and secretion. There are two types of
diabetes, type 1, type 2 diabetes and gestational diabetes. The common symptoms of diabetes
include high blood sugar or glucose level, frequent urination, increased hunger and thrust
along with body weight imbalance. According to the National Health Survey conducted by
the Australian Bureau of Statistics at least 1.2 million people who are aged over 2 years are
diagnosed with diabetes in Australia. The prevalence of diabetes has doubled in Australia
during the tenure of 2004 to 2014 and have showed high rate of occurrence among the
aboriginals and the Torres Strait Islanders (Australian Government Department of Health
2016). The following essay aims to analyse the anatomy and physiology associated with the
development of diabetes. The essay also aims to throw light over the pathophysiological
changes occurring during different types of diabetes and the associated complication of
diabetes. The essay thus will help the readers to get a rough overview of diabetes.
About Diabetes
Anatomy of physiology of glucose metabolism and absorption
Role of pancreas in glucose metabolism and absorption
Glucose metabolism occurs through glycolysis. In glycolysis single molecule of
glucose is broken down via a series of enzyme-catalyzed reactions in order to yield two
molecules of three carbon compounds known as pyruvate along with the release of energy in
the form of ATP. When the blood glucose level is low, islet of Langerhans in the pancreas
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
DIABETES
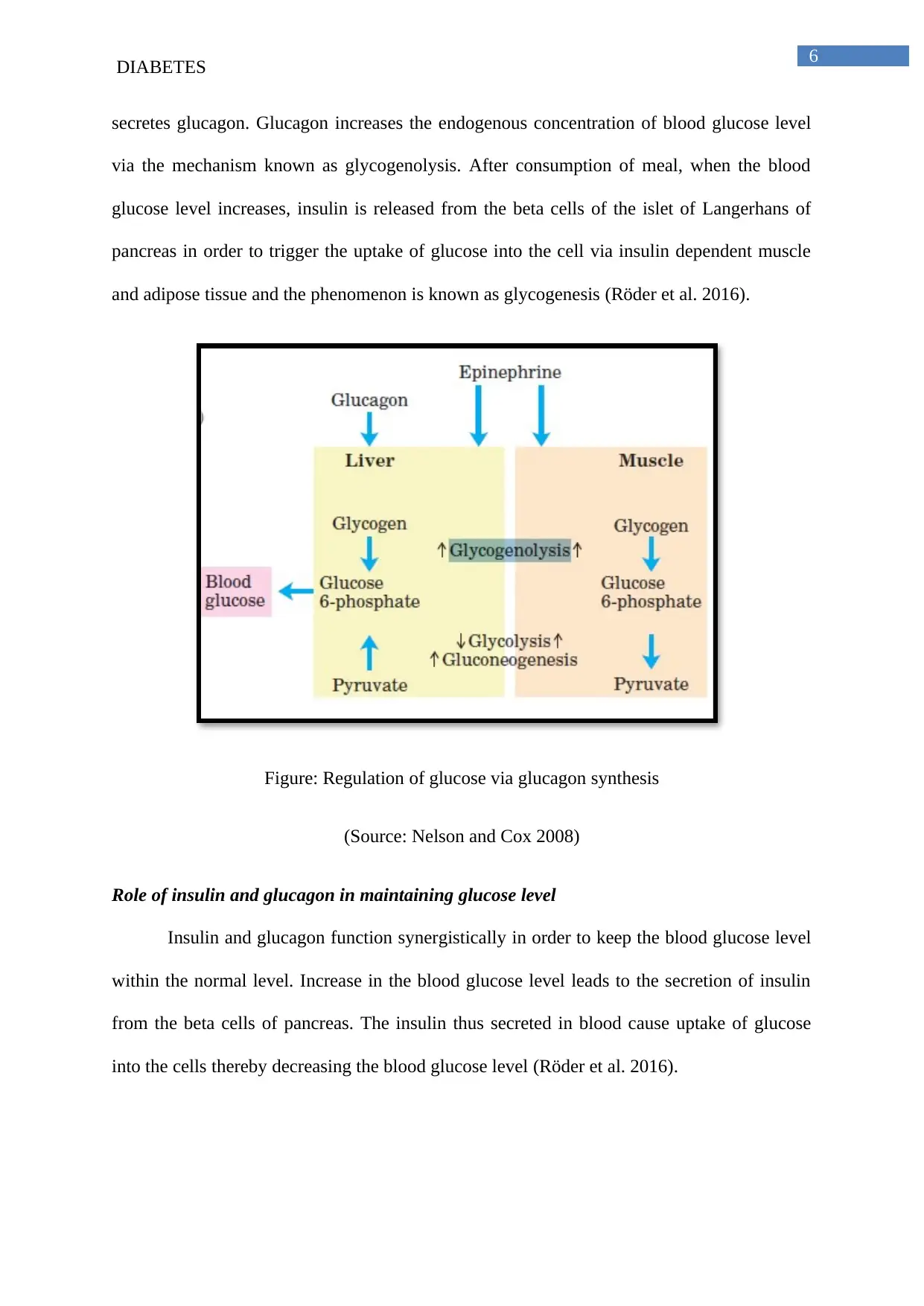
secretes glucagon. Glucagon increases the endogenous concentration of blood glucose level
via the mechanism known as glycogenolysis. After consumption of meal, when the blood
glucose level increases, insulin is released from the beta cells of the islet of Langerhans of
pancreas in order to trigger the uptake of glucose into the cell via insulin dependent muscle
and adipose tissue and the phenomenon is known as glycogenesis (Röder et al. 2016).
Figure: Regulation of glucose via glucagon synthesis
(Source: Nelson and Cox 2008)
Role of insulin and glucagon in maintaining glucose level
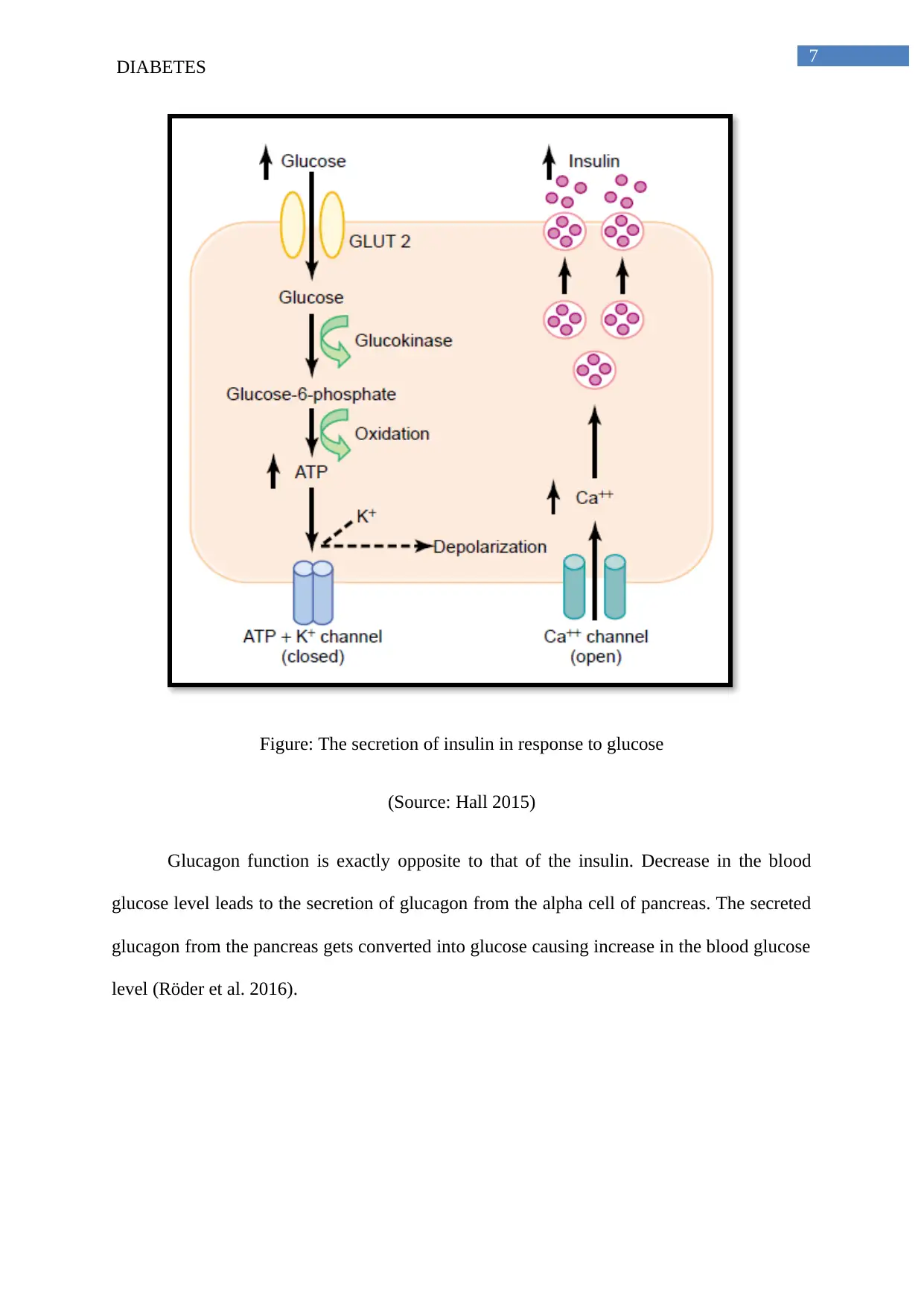
Insulin and glucagon function synergistically in order to keep the blood glucose level
within the normal level. Increase in the blood glucose level leads to the secretion of insulin
from the beta cells of pancreas. The insulin thus secreted in blood cause uptake of glucose
into the cells thereby decreasing the blood glucose level (Röder et al. 2016).
DIABETES
secretes glucagon. Glucagon increases the endogenous concentration of blood glucose level
via the mechanism known as glycogenolysis. After consumption of meal, when the blood
glucose level increases, insulin is released from the beta cells of the islet of Langerhans of
pancreas in order to trigger the uptake of glucose into the cell via insulin dependent muscle
and adipose tissue and the phenomenon is known as glycogenesis (Röder et al. 2016).
Figure: Regulation of glucose via glucagon synthesis
(Source: Nelson and Cox 2008)
Role of insulin and glucagon in maintaining glucose level
Insulin and glucagon function synergistically in order to keep the blood glucose level
within the normal level. Increase in the blood glucose level leads to the secretion of insulin
from the beta cells of pancreas. The insulin thus secreted in blood cause uptake of glucose
into the cells thereby decreasing the blood glucose level (Röder et al. 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
DIABETES
Figure: The secretion of insulin in response to glucose
(Source: Hall 2015)
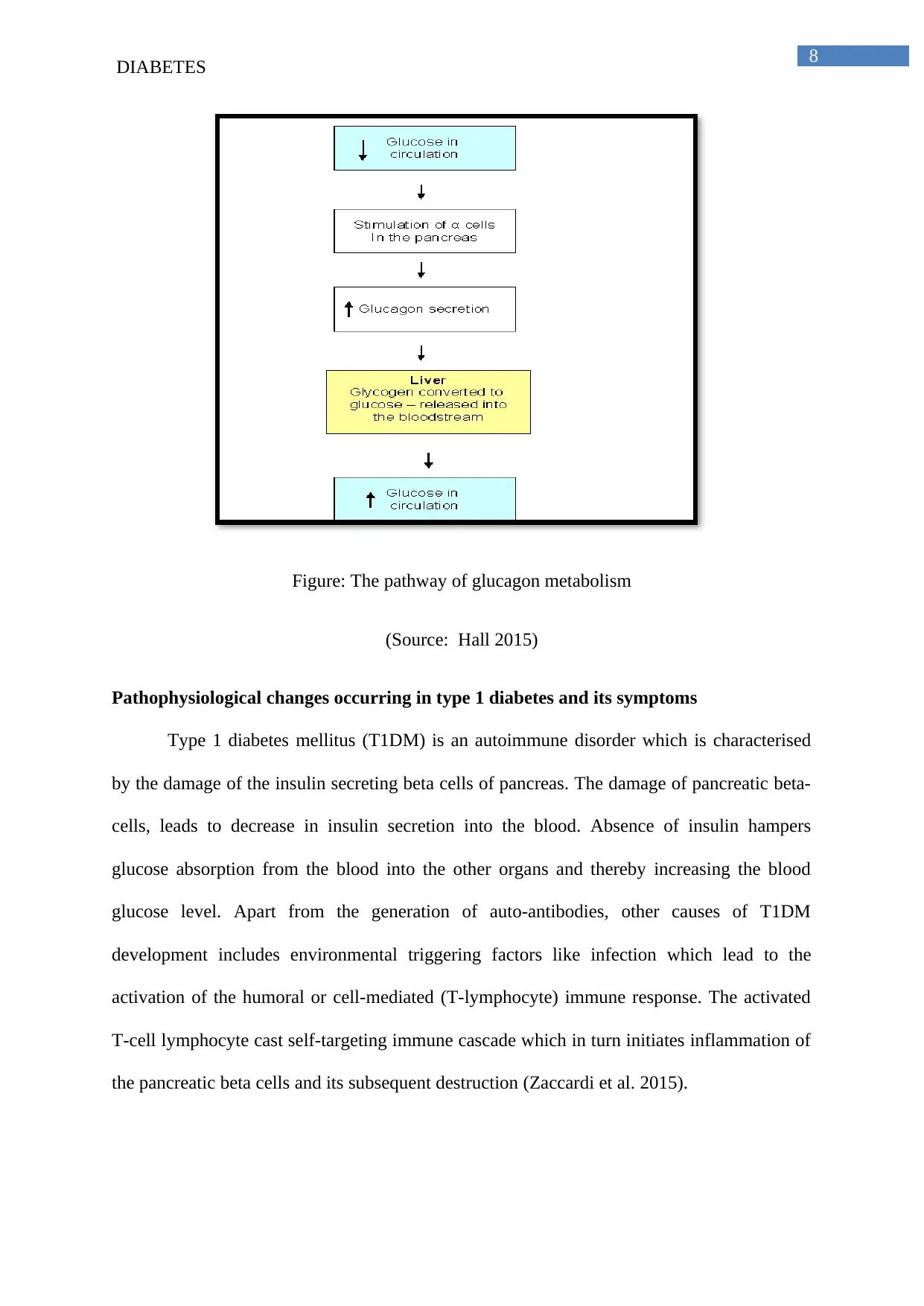
Glucagon function is exactly opposite to that of the insulin. Decrease in the blood
glucose level leads to the secretion of glucagon from the alpha cell of pancreas. The secreted
glucagon from the pancreas gets converted into glucose causing increase in the blood glucose
level (Röder et al. 2016).
DIABETES
Figure: The secretion of insulin in response to glucose
(Source: Hall 2015)
Glucagon function is exactly opposite to that of the insulin. Decrease in the blood
glucose level leads to the secretion of glucagon from the alpha cell of pancreas. The secreted
glucagon from the pancreas gets converted into glucose causing increase in the blood glucose
level (Röder et al. 2016).
8
DIABETES
Figure: The pathway of glucagon metabolism
(Source: Hall 2015)
Pathophysiological changes occurring in type 1 diabetes and its symptoms
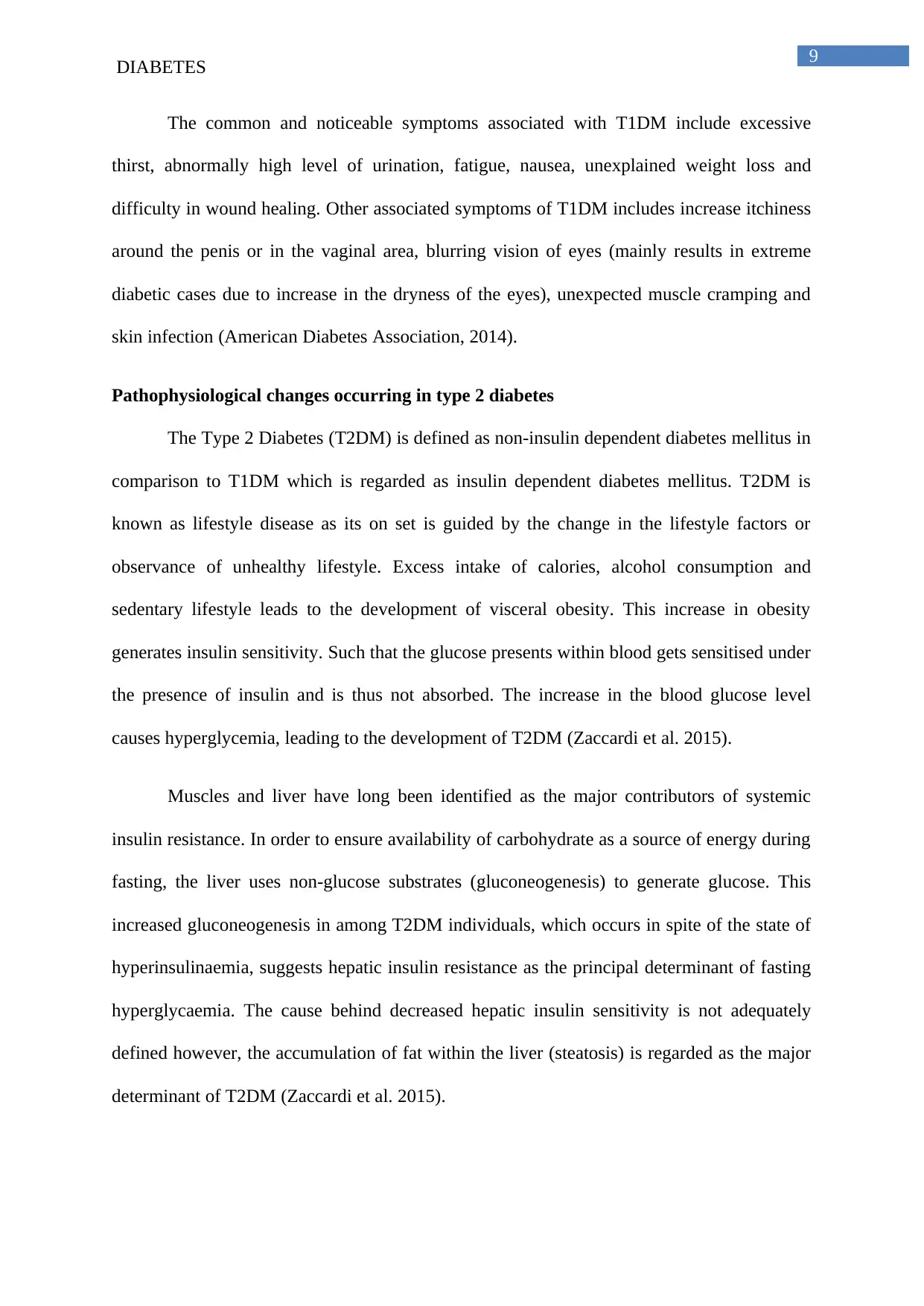
Type 1 diabetes mellitus (T1DM) is an autoimmune disorder which is characterised
by the damage of the insulin secreting beta cells of pancreas. The damage of pancreatic beta-
cells, leads to decrease in insulin secretion into the blood. Absence of insulin hampers
glucose absorption from the blood into the other organs and thereby increasing the blood
glucose level. Apart from the generation of auto-antibodies, other causes of T1DM
development includes environmental triggering factors like infection which lead to the
activation of the humoral or cell-mediated (T-lymphocyte) immune response. The activated
T-cell lymphocyte cast self-targeting immune cascade which in turn initiates inflammation of
the pancreatic beta cells and its subsequent destruction (Zaccardi et al. 2015).
DIABETES
Figure: The pathway of glucagon metabolism
(Source: Hall 2015)
Pathophysiological changes occurring in type 1 diabetes and its symptoms
Type 1 diabetes mellitus (T1DM) is an autoimmune disorder which is characterised
by the damage of the insulin secreting beta cells of pancreas. The damage of pancreatic beta-
cells, leads to decrease in insulin secretion into the blood. Absence of insulin hampers
glucose absorption from the blood into the other organs and thereby increasing the blood
glucose level. Apart from the generation of auto-antibodies, other causes of T1DM
development includes environmental triggering factors like infection which lead to the
activation of the humoral or cell-mediated (T-lymphocyte) immune response. The activated
T-cell lymphocyte cast self-targeting immune cascade which in turn initiates inflammation of
the pancreatic beta cells and its subsequent destruction (Zaccardi et al. 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
DIABETES
The common and noticeable symptoms associated with T1DM include excessive
thirst, abnormally high level of urination, fatigue, nausea, unexplained weight loss and
difficulty in wound healing. Other associated symptoms of T1DM includes increase itchiness
around the penis or in the vaginal area, blurring vision of eyes (mainly results in extreme
diabetic cases due to increase in the dryness of the eyes), unexpected muscle cramping and
skin infection (American Diabetes Association, 2014).
Pathophysiological changes occurring in type 2 diabetes
The Type 2 Diabetes (T2DM) is defined as non-insulin dependent diabetes mellitus in
comparison to T1DM which is regarded as insulin dependent diabetes mellitus. T2DM is
known as lifestyle disease as its on set is guided by the change in the lifestyle factors or
observance of unhealthy lifestyle. Excess intake of calories, alcohol consumption and
sedentary lifestyle leads to the development of visceral obesity. This increase in obesity
generates insulin sensitivity. Such that the glucose presents within blood gets sensitised under
the presence of insulin and is thus not absorbed. The increase in the blood glucose level
causes hyperglycemia, leading to the development of T2DM (Zaccardi et al. 2015).
Muscles and liver have long been identified as the major contributors of systemic
insulin resistance. In order to ensure availability of carbohydrate as a source of energy during
fasting, the liver uses non-glucose substrates (gluconeogenesis) to generate glucose. This
increased gluconeogenesis in among T2DM individuals, which occurs in spite of the state of
hyperinsulinaemia, suggests hepatic insulin resistance as the principal determinant of fasting
hyperglycaemia. The cause behind decreased hepatic insulin sensitivity is not adequately
defined however, the accumulation of fat within the liver (steatosis) is regarded as the major
determinant of T2DM (Zaccardi et al. 2015).
DIABETES
The common and noticeable symptoms associated with T1DM include excessive
thirst, abnormally high level of urination, fatigue, nausea, unexplained weight loss and
difficulty in wound healing. Other associated symptoms of T1DM includes increase itchiness
around the penis or in the vaginal area, blurring vision of eyes (mainly results in extreme
diabetic cases due to increase in the dryness of the eyes), unexpected muscle cramping and
skin infection (American Diabetes Association, 2014).
Pathophysiological changes occurring in type 2 diabetes
The Type 2 Diabetes (T2DM) is defined as non-insulin dependent diabetes mellitus in
comparison to T1DM which is regarded as insulin dependent diabetes mellitus. T2DM is
known as lifestyle disease as its on set is guided by the change in the lifestyle factors or
observance of unhealthy lifestyle. Excess intake of calories, alcohol consumption and
sedentary lifestyle leads to the development of visceral obesity. This increase in obesity
generates insulin sensitivity. Such that the glucose presents within blood gets sensitised under
the presence of insulin and is thus not absorbed. The increase in the blood glucose level
causes hyperglycemia, leading to the development of T2DM (Zaccardi et al. 2015).
Muscles and liver have long been identified as the major contributors of systemic
insulin resistance. In order to ensure availability of carbohydrate as a source of energy during
fasting, the liver uses non-glucose substrates (gluconeogenesis) to generate glucose. This
increased gluconeogenesis in among T2DM individuals, which occurs in spite of the state of
hyperinsulinaemia, suggests hepatic insulin resistance as the principal determinant of fasting
hyperglycaemia. The cause behind decreased hepatic insulin sensitivity is not adequately
defined however, the accumulation of fat within the liver (steatosis) is regarded as the major
determinant of T2DM (Zaccardi et al. 2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
DIABETES
Pathophysiological changes occurring in gestational mellitus
The pathophysiology of gestational diabetes mellitus is still unknown. One of the
principal aspects of the pathophysiology of gestational diabetes mellitus is insulin resistance.
Under this condition, the cells of the body fail to respond to the hormone insulin in usual
manner. Numerous pregnancy hormones are thought to hamper the normal function of
insulin. The pregnancy hormones mimic and bind to the insulin receptor and thereby
interfering with the glucose uptake. The glucose mainly present within the blood crosses the
placenta through GLUT1 carrier in order to propagate to foetus. Lack of proper treatment of
gestational diabetes causes overexposure of foetus to glucose. Excess of glucose causes
increase in insulin production within the foetus leading to overgrowth of the foetus in
comparison to the normal gestational age (Baz, Riveline and Gautier 2015).
Problems associated while procuring nursing care to a person with diabetes
Hypoglycemia
Hypoglycemia is a condition where the blood glucose level decrease below the
normal range (72mg/dL) and mostly arises due to improper dosage of diabetes medication.
The early signs and symptoms of hypoglycemia include sweating, fatigue and dizziness and
can be fatal if not treated early (Seaquist et al. 2013).
Hyperglycemia
Hyperglycemia is a pathological condition that is defined by high blood sugar level. It
is defined as the hallmark sign of T1DM and T2DM. Apart from diabetes high level of blood
sugar also occurs during the conditions like Cushing syndrome, pancreatic cancer and under
certain medication which generates insulin resistance. The main symptoms of hyperglycemia
include frequent excretion of dilute urine and increased level of thirst. Hyperglycemia if not
DIABETES
Pathophysiological changes occurring in gestational mellitus
The pathophysiology of gestational diabetes mellitus is still unknown. One of the
principal aspects of the pathophysiology of gestational diabetes mellitus is insulin resistance.
Under this condition, the cells of the body fail to respond to the hormone insulin in usual
manner. Numerous pregnancy hormones are thought to hamper the normal function of
insulin. The pregnancy hormones mimic and bind to the insulin receptor and thereby
interfering with the glucose uptake. The glucose mainly present within the blood crosses the
placenta through GLUT1 carrier in order to propagate to foetus. Lack of proper treatment of
gestational diabetes causes overexposure of foetus to glucose. Excess of glucose causes
increase in insulin production within the foetus leading to overgrowth of the foetus in
comparison to the normal gestational age (Baz, Riveline and Gautier 2015).
Problems associated while procuring nursing care to a person with diabetes
Hypoglycemia
Hypoglycemia is a condition where the blood glucose level decrease below the
normal range (72mg/dL) and mostly arises due to improper dosage of diabetes medication.
The early signs and symptoms of hypoglycemia include sweating, fatigue and dizziness and
can be fatal if not treated early (Seaquist et al. 2013).
Hyperglycemia
Hyperglycemia is a pathological condition that is defined by high blood sugar level. It
is defined as the hallmark sign of T1DM and T2DM. Apart from diabetes high level of blood
sugar also occurs during the conditions like Cushing syndrome, pancreatic cancer and under
certain medication which generates insulin resistance. The main symptoms of hyperglycemia
include frequent excretion of dilute urine and increased level of thirst. Hyperglycemia if not
11
DIABETES
treated on time may result in emergency condition known as ketacidosis (Inzucchi, et al.
2015).
Ketoacidosis
Ketacidosis is a life-threatening complications arising out of T1DM and occurs when
the blood plasma concentration of ketones are high due to lack of insulin. The main signs of
ketoacidosis include confusion, dehydration, nausea, vomiting and abdominal pain. Increase
in the risk factor of ketoacidosis during the treatment of T1DM mostly arises from stressor of
higher dosage of insulin. Proper monitoring of the blood glucose level and the level of insulin
intake helps to prevent the chance of developing ketoacidosis (Erondu et al. 2015).
Hyper osmolar non-ketonic coma
It is also commonly known as hyperglycaemic state which is characterised as a fatal
condition with abnormally high level of glucose. Having high blood sugar level for an
extended period of time increases the susceptibility of developing hyper osmolar non-ketonic
coma. It is mainly common among the older adults suffering from diabetes and can lead to
coma if not treated with cautions (Pasquel and Umpierrez 2014).
Diabetic retinopathy
High blood sugar level for a prolong period of time cause diabetic retinopathy. Under
this condition high level of blood sugar cause damage to the blood vessels of retina and
thereby causing change in vision. There are two stages of diabetic retinopathy, non-
proliferative diabetic retinopathy and proliferative diabetic retinopathy (Mohammedi et al.
2016).
Infection
High blood sugar level increases the risk of infection. Moreover, high level of blood
sugar slows down the process of healing and thereby increasing the vulnerability of the
DIABETES
treated on time may result in emergency condition known as ketacidosis (Inzucchi, et al.
2015).
Ketoacidosis
Ketacidosis is a life-threatening complications arising out of T1DM and occurs when
the blood plasma concentration of ketones are high due to lack of insulin. The main signs of
ketoacidosis include confusion, dehydration, nausea, vomiting and abdominal pain. Increase
in the risk factor of ketoacidosis during the treatment of T1DM mostly arises from stressor of
higher dosage of insulin. Proper monitoring of the blood glucose level and the level of insulin
intake helps to prevent the chance of developing ketoacidosis (Erondu et al. 2015).
Hyper osmolar non-ketonic coma
It is also commonly known as hyperglycaemic state which is characterised as a fatal
condition with abnormally high level of glucose. Having high blood sugar level for an
extended period of time increases the susceptibility of developing hyper osmolar non-ketonic
coma. It is mainly common among the older adults suffering from diabetes and can lead to
coma if not treated with cautions (Pasquel and Umpierrez 2014).
Diabetic retinopathy
High blood sugar level for a prolong period of time cause diabetic retinopathy. Under
this condition high level of blood sugar cause damage to the blood vessels of retina and
thereby causing change in vision. There are two stages of diabetic retinopathy, non-
proliferative diabetic retinopathy and proliferative diabetic retinopathy (Mohammedi et al.
2016).
Infection
High blood sugar level increases the risk of infection. Moreover, high level of blood
sugar slows down the process of healing and thereby increasing the vulnerability of the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





