Food Consumption Analysis: Cardiovascular Disease and Diet Solutions
VerifiedAdded on 2023/05/29
|25
|27721
|367
Homework Assignment
AI Summary
This assignment solution is based on a review article from the Journal of the American College of Cardiology, focusing on the relationship between food consumption and cardiovascular disease (CVD). It addresses the impact of the globalized food system on dietary patterns and potential policy solutions. The analysis covers the development of the modern food system, the effects of various macronutrients and foods on CVD, and the necessary changes to the food system to address diet-related public health problems. The assignment likely involves analyzing a person's diet, comparing it against recommended guidelines, identifying key nutrients, and calculating the energy provided by each food group to assess overall dietary health in relation to CVD risk. It also involves comparing dietary intakes with the Australian Guide to Healthy Eating.
THE PRESENT AND FUTURE
STATE-OF-THE-ART REVIEW
Food Consumption and its Impact
on Cardiovascular Disease:
Importance of Solutions Focused on
the Globalized Food System
A Report From the Workshop Convened by the
World Heart Federation
Sonia S. Anand, MD, PHD,*y Corinna Hawkes, PHD,z Russell J. de Souza, SCD, RD,x Andrew Mente, PHD,y
Mahshid Dehghan, PHD,y Rachel Nugent, PHD,k Michael A. Zulyniak, PHD,* Tony Weis, PHD,{
Adam M. Bernstein, MD,# Ronald M. Krauss, MD,** Daan Kromhout, MPH, PHD,yy
David J.A. Jenkins, MD, P HD, DSC,zzxx Vasanti Malik, SCD,kk Miguel A. Martinez-Gonzalez, MPH, MD, PHD,{{
Dariush Mozaffarian, MD, DRPH,## Salim Yusuf, MD, DPHIL ,y Walter C. Willett, MD, DRPH,{{ Barry M. Popkin, PHD***
ABSTRACT
Major scholars in the field, on the basis of a 3-day consensus, created an in-depth review of current knowledge on the
role of diet in cardiovascular disease (CVD), the changing global food system and global dietary patterns, and potential
policy solutions. Evidence from different countries and age/race/ethnicity/socioeconomic groups suggesting the health
effects studies of foods, macronutrients, and dietary patterns on CVD appear to be far more consistent though regional
knowledge gaps are highlighted. Large gaps in knowledge about the association of macronutrients to CVD in low-
and middle-income countries particularly linked with dietary patterns are reviewed. Our understanding of foods and
macronutrients in relationship to CVD is broadly clear; however, major gaps exist both in dietary pattern research and
ways to change diets and food systems. On the basis of the current evidence, the traditional Mediterranean-type diet,
including plant foods and emphasis on plant protein sources provides a well-tested healthy dietary pattern to reduce
CVD. (J Am Coll Cardiol 2015;66:1590–614) © 2015 by the American College of Cardiology Foundation.
From the *Department of Medicine,McMaster University,Hamilton, Ontario, Canada;yPopulation Health Research Institute,
Hamilton Health Sciences and McMaster University, Hamilton, Ontario, Canada; zCentre for Food Policy, City University, London,
J O U R N A LO F T H E A M E R I C A N C O L L E G E O FC A R D I O L O G Y V O L . 6 6 , N O . 1 4 ,2 0 1 5
ª 2 0 1 5 B Y T H E A M E R I C A N C O L L E G E O FC A R D I O L O G Y F O U N D A T I O N I S S N 0 7 3 5 - 1 0 9 7 / $ 3 6 . 0 0
P U B L I S H E D B Y E L S E V I E R I N C . h t t p : / / d x . d o i . o r g / 1 0 . 1 0 1 6 / j . j a c c . 2 0 1 5 . 0 7 . 0 5 0
STATE-OF-THE-ART REVIEW
Food Consumption and its Impact
on Cardiovascular Disease:
Importance of Solutions Focused on
the Globalized Food System
A Report From the Workshop Convened by the
World Heart Federation
Sonia S. Anand, MD, PHD,*y Corinna Hawkes, PHD,z Russell J. de Souza, SCD, RD,x Andrew Mente, PHD,y
Mahshid Dehghan, PHD,y Rachel Nugent, PHD,k Michael A. Zulyniak, PHD,* Tony Weis, PHD,{
Adam M. Bernstein, MD,# Ronald M. Krauss, MD,** Daan Kromhout, MPH, PHD,yy
David J.A. Jenkins, MD, P HD, DSC,zzxx Vasanti Malik, SCD,kk Miguel A. Martinez-Gonzalez, MPH, MD, PHD,{{
Dariush Mozaffarian, MD, DRPH,## Salim Yusuf, MD, DPHIL ,y Walter C. Willett, MD, DRPH,{{ Barry M. Popkin, PHD***
ABSTRACT
Major scholars in the field, on the basis of a 3-day consensus, created an in-depth review of current knowledge on the
role of diet in cardiovascular disease (CVD), the changing global food system and global dietary patterns, and potential
policy solutions. Evidence from different countries and age/race/ethnicity/socioeconomic groups suggesting the health
effects studies of foods, macronutrients, and dietary patterns on CVD appear to be far more consistent though regional
knowledge gaps are highlighted. Large gaps in knowledge about the association of macronutrients to CVD in low-
and middle-income countries particularly linked with dietary patterns are reviewed. Our understanding of foods and
macronutrients in relationship to CVD is broadly clear; however, major gaps exist both in dietary pattern research and
ways to change diets and food systems. On the basis of the current evidence, the traditional Mediterranean-type diet,
including plant foods and emphasis on plant protein sources provides a well-tested healthy dietary pattern to reduce
CVD. (J Am Coll Cardiol 2015;66:1590–614) © 2015 by the American College of Cardiology Foundation.
From the *Department of Medicine,McMaster University,Hamilton, Ontario, Canada;yPopulation Health Research Institute,
Hamilton Health Sciences and McMaster University, Hamilton, Ontario, Canada; zCentre for Food Policy, City University, London,
J O U R N A LO F T H E A M E R I C A N C O L L E G E O FC A R D I O L O G Y V O L . 6 6 , N O . 1 4 ,2 0 1 5
ª 2 0 1 5 B Y T H E A M E R I C A N C O L L E G E O FC A R D I O L O G Y F O U N D A T I O N I S S N 0 7 3 5 - 1 0 9 7 / $ 3 6 . 0 0
P U B L I S H E D B Y E L S E V I E R I N C . h t t p : / / d x . d o i . o r g / 1 0 . 1 0 1 6 / j . j a c c . 2 0 1 5 . 0 7 . 0 5 0
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

T here is much controversy surrounding the
optimal diet for cardiovascular health. Data
relating diet to cardiovascular diseases
(CVDs) has predominantly been generated from
high-income countries (HIC), but >80% of CVD
deaths occur in low- and middle-income countries
(LMIC). Relatively sparse data on diet and CVD exist
from these countries though new data sources are
rapidly emerging (1,2). Noncommunicable diseases
are forecasted to increase substantially in LMIC
because of lifestyle transitions associated with in-
creasing urbanization, economic development, and
globalization. The Global Burden of Disease study
cites diet as a major factor behind the rise in hyper-
tension, diabetes, obesity, and other CVD compo-
nents (3). There are an estimated >500 million
obese (4,5) and close to 2 billion overweight or obese
individuals worldwide (6). Furthermore, unhealthy
dietary patterns have negative environmental im-
pacts, notably on climate change.
Poor quality diets are high in refined grains and
added sugars, salt, unhealthy fats, and animal-source
foods; and low in whole grains, fruits, vegetables,
legumes, fish, and nuts. They are often high in pro-
cessed food products—typically packaged and often
ready to consume—and light on whole foods and freshly
prepared dishes. These unhealthy diets are facilitated
by modern food environments, a problem that is
likely to become more widespread as food environ-
ments in LMIC shift to resemble those of HIC (5,7,8).
In this paper, we summarize the evidence relating
food to CVD, and the powerful forces that underpin
the creation of modern food environments—what we
call the global food system—to emphasize the impor-
tance of identifying systemic solutions to diet-related
health outcomes. We do this in the context of
increasing global attention to the importance
of improving food systems by the interna-
tional development and nutrition community
(9–11). Although the “food system” may seem
remote to a clinician sitting in an office seeing
a patient, its impact on the individuals they
are trying to treat are very real. This paper is on
the basis of a World Heart Federation inter-
national workshop to review the state of
knowledge on this topic. This review of diet,
dietary patterns, and CVD is not on the basis of
new systematic reviews or meta-analyses but
represents a careful review of many published
meta-analyses, seminal primary studies, and
recent research by the scholars who partici-
pated in the Consensus conference.
This paper presents: 1) an overview of the
development of the modern, globalized food
system and its implications for the food
supply; 2) a consensus on the evidence
relating various macronutrients and foods to
CVD and its related comorbidities; and 3) an
outline of how changes to the global food
system can address current diet-related pub-
lic health problems, and simultaneously have bene-
ficial impacts on climate change.
THE CHANGING FOOD SYSTEM AND
FOOD SUPPLY AND IMPLICATIONS FOR
DIETS AND THE ENVIRONMENT
THE DEVELOPMENT OF THE MODERN, GLOBALIZED
FOOD SYSTEM. Food systems were once dominated
by local production for local markets, with relatively
little processing before foods reached the household
(Online Appendix, Box 1) (12). In contrast, the modern
A B B R E V I A T I O N S
A N D A C R O N Y M S
CHD =coronary heart disease
CI = confidence interval
CVD = cardiovascular disease
GI =glycemic index
GL = glycemic load
HDL-C = high-density
lipoprotein cholesterol
HIC = high-income countries
LDL-C = low-density
lipoprotein cholesterol
LMIC = low- and middle-
income countries
MI =myocardial infarction
OR = odds ratio
RCT = randomized controlled
trial
RR = relative risk
SSB =sugar-sweetened
beverage
T2DM =type 2 diabetes
mellitus
Barilla, Unilever Canada, Solae, Oldways, Kellogg’s, Quaker Oats, Procter & Gamble, Coca-Cola, NuVal Griffin Hospital, Abbott, the
Canola Council of Canada, Dean Foods, the California Strawberry Commission, Haine Celestial, and the Alpro Foundation; has
J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5 Anand et al.
O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4 Diet, Cardiovascular Disease, and the Food System
1591
optimal diet for cardiovascular health. Data
relating diet to cardiovascular diseases
(CVDs) has predominantly been generated from
high-income countries (HIC), but >80% of CVD
deaths occur in low- and middle-income countries
(LMIC). Relatively sparse data on diet and CVD exist
from these countries though new data sources are
rapidly emerging (1,2). Noncommunicable diseases
are forecasted to increase substantially in LMIC
because of lifestyle transitions associated with in-
creasing urbanization, economic development, and
globalization. The Global Burden of Disease study
cites diet as a major factor behind the rise in hyper-
tension, diabetes, obesity, and other CVD compo-
nents (3). There are an estimated >500 million
obese (4,5) and close to 2 billion overweight or obese
individuals worldwide (6). Furthermore, unhealthy
dietary patterns have negative environmental im-
pacts, notably on climate change.
Poor quality diets are high in refined grains and
added sugars, salt, unhealthy fats, and animal-source
foods; and low in whole grains, fruits, vegetables,
legumes, fish, and nuts. They are often high in pro-
cessed food products—typically packaged and often
ready to consume—and light on whole foods and freshly
prepared dishes. These unhealthy diets are facilitated
by modern food environments, a problem that is
likely to become more widespread as food environ-
ments in LMIC shift to resemble those of HIC (5,7,8).
In this paper, we summarize the evidence relating
food to CVD, and the powerful forces that underpin
the creation of modern food environments—what we
call the global food system—to emphasize the impor-
tance of identifying systemic solutions to diet-related
health outcomes. We do this in the context of
increasing global attention to the importance
of improving food systems by the interna-
tional development and nutrition community
(9–11). Although the “food system” may seem
remote to a clinician sitting in an office seeing
a patient, its impact on the individuals they
are trying to treat are very real. This paper is on
the basis of a World Heart Federation inter-
national workshop to review the state of
knowledge on this topic. This review of diet,
dietary patterns, and CVD is not on the basis of
new systematic reviews or meta-analyses but
represents a careful review of many published
meta-analyses, seminal primary studies, and
recent research by the scholars who partici-
pated in the Consensus conference.
This paper presents: 1) an overview of the
development of the modern, globalized food
system and its implications for the food
supply; 2) a consensus on the evidence
relating various macronutrients and foods to
CVD and its related comorbidities; and 3) an
outline of how changes to the global food
system can address current diet-related pub-
lic health problems, and simultaneously have bene-
ficial impacts on climate change.
THE CHANGING FOOD SYSTEM AND
FOOD SUPPLY AND IMPLICATIONS FOR
DIETS AND THE ENVIRONMENT
THE DEVELOPMENT OF THE MODERN, GLOBALIZED
FOOD SYSTEM. Food systems were once dominated
by local production for local markets, with relatively
little processing before foods reached the household
(Online Appendix, Box 1) (12). In contrast, the modern
A B B R E V I A T I O N S
A N D A C R O N Y M S
CHD =coronary heart disease
CI = confidence interval
CVD = cardiovascular disease
GI =glycemic index
GL = glycemic load
HDL-C = high-density
lipoprotein cholesterol
HIC = high-income countries
LDL-C = low-density
lipoprotein cholesterol
LMIC = low- and middle-
income countries
MI =myocardial infarction
OR = odds ratio
RCT = randomized controlled
trial
RR = relative risk
SSB =sugar-sweetened
beverage
T2DM =type 2 diabetes
mellitus
Barilla, Unilever Canada, Solae, Oldways, Kellogg’s, Quaker Oats, Procter & Gamble, Coca-Cola, NuVal Griffin Hospital, Abbott, the
Canola Council of Canada, Dean Foods, the California Strawberry Commission, Haine Celestial, and the Alpro Foundation; has
J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5 Anand et al.
O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4 Diet, Cardiovascular Disease, and the Food System
1591
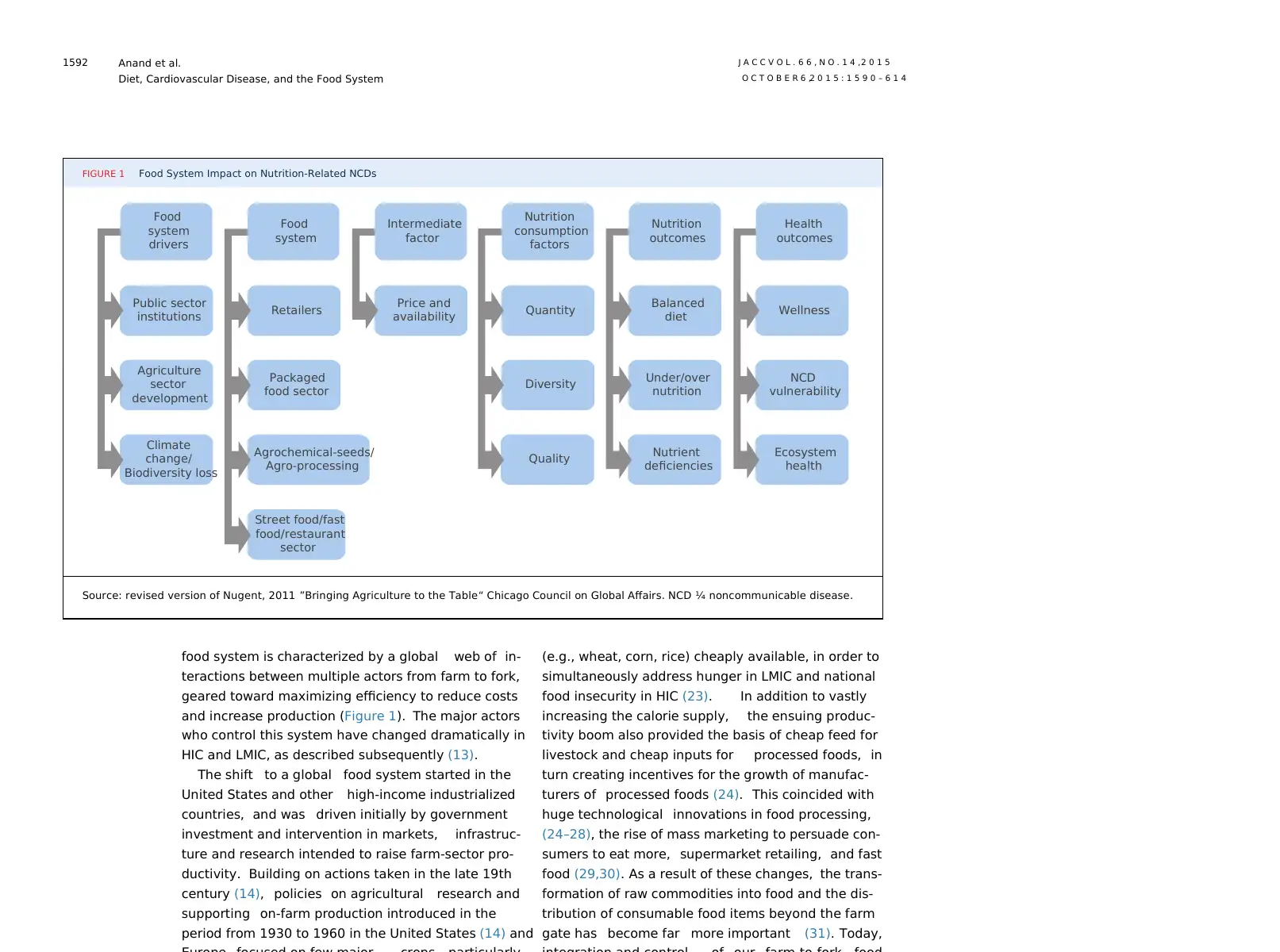
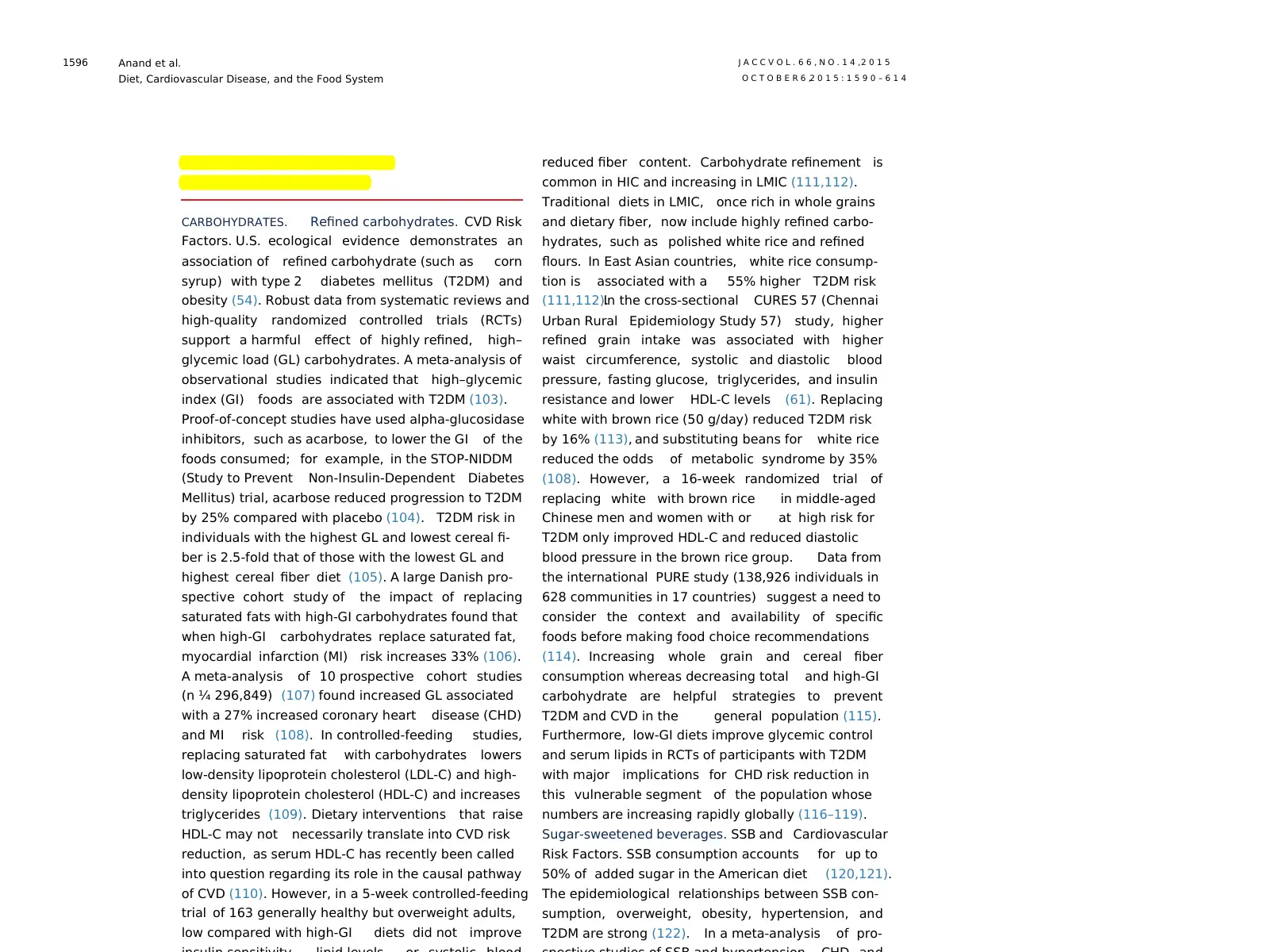
food system is characterized by a global web of in-
teractions between multiple actors from farm to fork,
geared toward maximizing efficiency to reduce costs
and increase production (Figure 1). The major actors
who control this system have changed dramatically in
HIC and LMIC, as described subsequently (13).
The shift to a global food system started in the
United States and other high-income industrialized
countries, and was driven initially by government
investment and intervention in markets, infrastruc-
ture and research intended to raise farm-sector pro-
ductivity. Building on actions taken in the late 19th
century (14), policies on agricultural research and
supporting on-farm production introduced in the
period from 1930 to 1960 in the United States (14) and
(e.g., wheat, corn, rice) cheaply available, in order to
simultaneously address hunger in LMIC and national
food insecurity in HIC (23). In addition to vastly
increasing the calorie supply, the ensuing produc-
tivity boom also provided the basis of cheap feed for
livestock and cheap inputs for processed foods, in
turn creating incentives for the growth of manufac-
turers of processed foods (24). This coincided with
huge technological innovations in food processing,
(24–28), the rise of mass marketing to persuade con-
sumers to eat more, supermarket retailing, and fast
food (29,30). As a result of these changes, the trans-
formation of raw commodities into food and the dis-
tribution of consumable food items beyond the farm
gate has become far more important (31). Today,
FIGURE 1 Food System Impact on Nutrition-Related NCDs
Food
system
drivers
Food
system
Intermediate
factor
Nutrition
consumption
factors
Nutrition
outcomes
Health
outcomes
Public sector
institutions Retailers Price and
availability Quantity Balanced
diet Wellness
Agriculture
sector
development
Packaged
food sector Diversity Under/over
nutrition
NCD
vulnerability
Climate
change/
Biodiversity loss
Agrochemical-seeds/
Agro-processing
Street food/fast
food/restaurant
sector
Quality Nutrient
deficiencies
Ecosystem
health
Source: revised version of Nugent, 2011 ”Bringing Agriculture to the Table“ Chicago Council on Global Affairs. NCD ¼ noncommunicable disease.
Anand et al. J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5
Diet, Cardiovascular Disease, and the Food System O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4
1592
teractions between multiple actors from farm to fork,
geared toward maximizing efficiency to reduce costs
and increase production (Figure 1). The major actors
who control this system have changed dramatically in
HIC and LMIC, as described subsequently (13).
The shift to a global food system started in the
United States and other high-income industrialized
countries, and was driven initially by government
investment and intervention in markets, infrastruc-
ture and research intended to raise farm-sector pro-
ductivity. Building on actions taken in the late 19th
century (14), policies on agricultural research and
supporting on-farm production introduced in the
period from 1930 to 1960 in the United States (14) and
(e.g., wheat, corn, rice) cheaply available, in order to
simultaneously address hunger in LMIC and national
food insecurity in HIC (23). In addition to vastly
increasing the calorie supply, the ensuing produc-
tivity boom also provided the basis of cheap feed for
livestock and cheap inputs for processed foods, in
turn creating incentives for the growth of manufac-
turers of processed foods (24). This coincided with
huge technological innovations in food processing,
(24–28), the rise of mass marketing to persuade con-
sumers to eat more, supermarket retailing, and fast
food (29,30). As a result of these changes, the trans-
formation of raw commodities into food and the dis-
tribution of consumable food items beyond the farm
gate has become far more important (31). Today,
FIGURE 1 Food System Impact on Nutrition-Related NCDs
Food
system
drivers
Food
system
Intermediate
factor
Nutrition
consumption
factors
Nutrition
outcomes
Health
outcomes
Public sector
institutions Retailers Price and
availability Quantity Balanced
diet Wellness
Agriculture
sector
development
Packaged
food sector Diversity Under/over
nutrition
NCD
vulnerability
Climate
change/
Biodiversity loss
Agrochemical-seeds/
Agro-processing
Street food/fast
food/restaurant
sector
Quality Nutrient
deficiencies
Ecosystem
health
Source: revised version of Nugent, 2011 ”Bringing Agriculture to the Table“ Chicago Council on Global Affairs. NCD ¼ noncommunicable disease.
Anand et al. J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5
Diet, Cardiovascular Disease, and the Food System O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4
1592
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
revolutionized the entire sector in many regions
(13,42). Retailing has been transformed in LMIC
through the growth of supermarkets (18,38–41).
Although this process originated with companies in
industrialized countries looking for growth in foreign
markets, companies based in LMIC are now also
investing back into HIC.
carbohydrates—refined grains and added sugars.
Rapidly increasing production of starchy staples com-
bined with processing technologies mean that refined
flour is increasingly dominant in diets. White bread, for
example, once rarely consumed in Latin America,
became widespread after the introduction of high-
yield wheat varieties. In Asia, white rice became
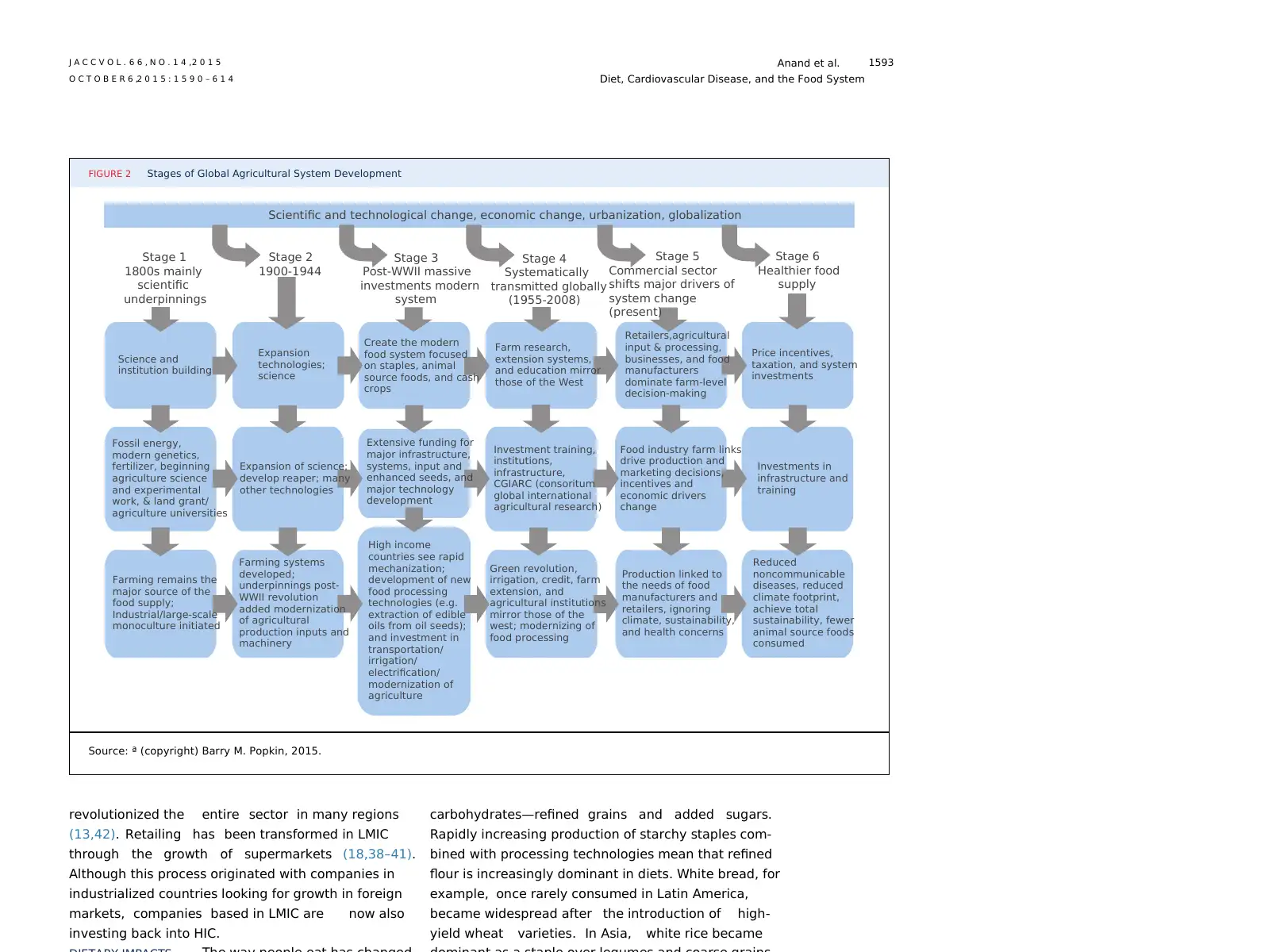
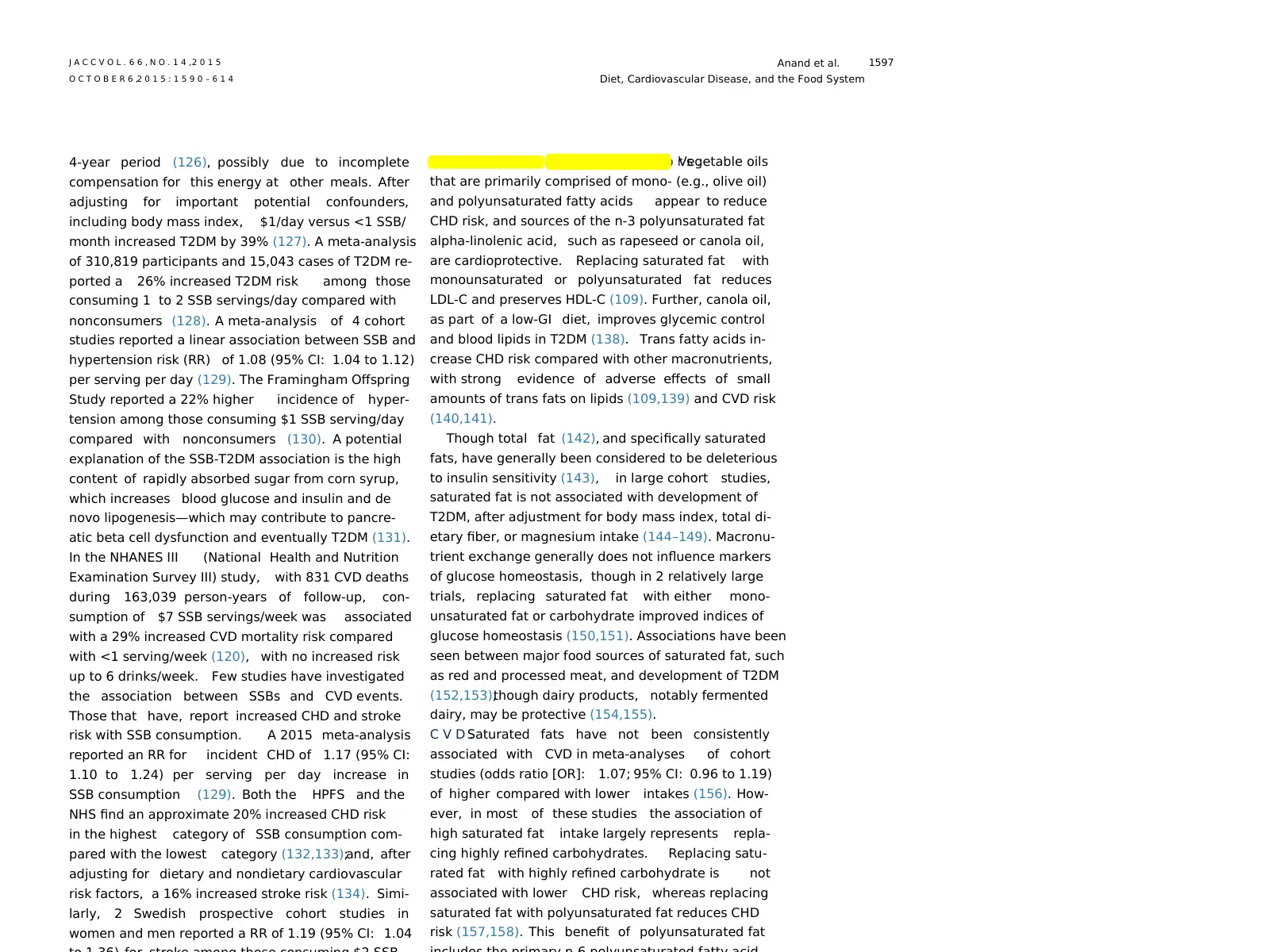
FIGURE 2 Stages of Global Agricultural System Development
Scientific and technological change, economic change, urbanization, globalization
Stage 1
1800s mainly
scientific
underpinnings
Stage 2
1900-1944
Stage 3
Post-WWII massive
investments modern
system
Stage 4
Systematically
transmitted globally
(1955-2008)
Stage 5
Commercial sector
shifts major drivers of
system change
(present)
Stage 6
Healthier food
supply
Price incentives,
taxation, and system
investments
Retailers,agricultural
input & processing,
businesses, and food
manufacturers
dominate farm-level
decision-making
Farm research,
extension systems,
and education mirror
those of the West
Create the modern
food system focused
on staples, animal
source foods, and cash
crops
Expansion
technologies;
science
Science and
institution building
Fossil energy,
modern genetics,
fertilizer, beginning
agriculture science
and experimental
work, & land grant/
agriculture universities
Expansion of science;
develop reaper; many
other technologies
Extensive funding for
major infrastructure,
systems, input and
enhanced seeds, and
major technology
development
Investment training,
institutions,
infrastructure,
CGIARC (consoritum
global international
agricultural research)
Food industry farm links
drive production and
marketing decisions,
incentives and
economic drivers
change
Investments in
infrastructure and
training
Reduced
noncommunicable
diseases, reduced
climate footprint,
achieve total
sustainability, fewer
animal source foods
consumed
Production linked to
the needs of food
manufacturers and
retailers, ignoring
climate, sustainability,
and health concerns
Green revolution,
irrigation, credit, farm
extension, and
agricultural institutions
mirror those of the
west; modernizing of
food processing
High income
countries see rapid
mechanization;
development of new
food processing
technologies (e.g.
extraction of edible
oils from oil seeds);
and investment in
transportation/
irrigation/
electrification/
modernization of
agriculture
Farming systems
developed;
underpinnings post-
WWII revolution
added modernization
of agricultural
production inputs and
machinery
Farming remains the
major source of the
food supply;
Industrial/large-scale
monoculture initiated
Source: ª (copyright) Barry M. Popkin, 2015.
J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5 Anand et al.
O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4 Diet, Cardiovascular Disease, and the Food System
1593
(13,42). Retailing has been transformed in LMIC
through the growth of supermarkets (18,38–41).
Although this process originated with companies in
industrialized countries looking for growth in foreign
markets, companies based in LMIC are now also
investing back into HIC.
carbohydrates—refined grains and added sugars.
Rapidly increasing production of starchy staples com-
bined with processing technologies mean that refined
flour is increasingly dominant in diets. White bread, for
example, once rarely consumed in Latin America,
became widespread after the introduction of high-
yield wheat varieties. In Asia, white rice became
FIGURE 2 Stages of Global Agricultural System Development
Scientific and technological change, economic change, urbanization, globalization
Stage 1
1800s mainly
scientific
underpinnings
Stage 2
1900-1944
Stage 3
Post-WWII massive
investments modern
system
Stage 4
Systematically
transmitted globally
(1955-2008)
Stage 5
Commercial sector
shifts major drivers of
system change
(present)
Stage 6
Healthier food
supply
Price incentives,
taxation, and system
investments
Retailers,agricultural
input & processing,
businesses, and food
manufacturers
dominate farm-level
decision-making
Farm research,
extension systems,
and education mirror
those of the West
Create the modern
food system focused
on staples, animal
source foods, and cash
crops
Expansion
technologies;
science
Science and
institution building
Fossil energy,
modern genetics,
fertilizer, beginning
agriculture science
and experimental
work, & land grant/
agriculture universities
Expansion of science;
develop reaper; many
other technologies
Extensive funding for
major infrastructure,
systems, input and
enhanced seeds, and
major technology
development
Investment training,
institutions,
infrastructure,
CGIARC (consoritum
global international
agricultural research)
Food industry farm links
drive production and
marketing decisions,
incentives and
economic drivers
change
Investments in
infrastructure and
training
Reduced
noncommunicable
diseases, reduced
climate footprint,
achieve total
sustainability, fewer
animal source foods
consumed
Production linked to
the needs of food
manufacturers and
retailers, ignoring
climate, sustainability,
and health concerns
Green revolution,
irrigation, credit, farm
extension, and
agricultural institutions
mirror those of the
west; modernizing of
food processing
High income
countries see rapid
mechanization;
development of new
food processing
technologies (e.g.
extraction of edible
oils from oil seeds);
and investment in
transportation/
irrigation/
electrification/
modernization of
agriculture
Farming systems
developed;
underpinnings post-
WWII revolution
added modernization
of agricultural
production inputs and
machinery
Farming remains the
major source of the
food supply;
Industrial/large-scale
monoculture initiated
Source: ª (copyright) Barry M. Popkin, 2015.
J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5 Anand et al.
O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4 Diet, Cardiovascular Disease, and the Food System
1593
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
United States packaged and processed food supply,
over 75% of foods, have some form of added sugar
(60). With urbanization there is some evidence to
show that refined carbohydrate consumption is
increasing, whereas consumption of traditional
grains (i.e., millet, maize) is decreasing in LMIC
(61,62).
A second key change has been the increasing
intake of vegetable oils, including processed vege-
table oils, and a decline in consumption of animal fats
(2,63). This was initially driven by rising production
of soybeans in the United States, later in Argentina
and Brazil, and then palm oil in East Asia. Oilseeds are
now among the most widely traded crops, and are
also processed to create margarines and vegetable
shortenings and into partially hydrogenated fats and
bleached deodorized oils for use in processed foods
(Online Appendix, Box 2). Between 1958 and 1996,a
major global shift occurred in the amount and types
of available fats, with soybean, palm, and rapeseed/
canola oils replacing butter, tallow, and lard. From
1958 to 1962, soybean, palm, and rapeseed/canola oils
represented 20% of the 29 million metric tons of fat
produced globally per year, whereas butter, lard, and
tallow represented 37%. By 1996 to 2001, these oils
accounted for 52% of the 103 million metric tons of fat
produced globally per year, whereas butter, lard, and
tallow contributed 20% (64). This has implications for
consumption of fatty acids. Palm oil (deodorized) has
become an increasing source of saturated fatty acids;
and partially hydrogenated fats are the main source
of trans fatty acids. Between 1990 and 2010, global
saturated fat, dietary cholesterol, and trans fat in-
takes remained stable (trans fats going down in HIC
and up in LMIC), whereas n-6, seafood n-3, and plant
n-3 fat intakes each increased (65). Vegetable oil
consumption remains 2 times higher in HIC than in
LMIC. However, trans fat consumption is very high in
many LMIC although decreasing markedly in HIC. In
India, for example, vanaspati, a vegetable ghee used
A third key change has been the increasing
global consumption of meat, which has been made
economically feasible by subsidized production of
crops for animal feed—most importantly corn and
soybeans (soybean oil is a byproduct of soymeal
production for animals) (66–69). At very low levels
of intake animal food consumption may not induce
harm, providing high-quality protein and iron,
whereas excess animal food intake in HIC may
be linked to adverse health outcomes, particularly
from processed meats (70). Meat consumption has
increased considerably worldwide, and there is sub-
stantially greater production of meat in HIC than in
LMIC (71). North and South America, Europe, and
Australia/New Zealand have the highest meat intake,
whereas Asia and Africa have the lowest (72,73).
Processed meats (which refers to post-butchering
modifications of foods such as curing, smoking, or
addition of sodium nitrate), account for 35.8% of all
meat consumed in HIC (unpublished data from the
PURE [Prospective Urban and Rural Epidemiological]
study) (71).
Dietary consumption patterns of other protein
sources have been mixed. Between 1973 and 1997,
dairy consumption per capita (kilograms) increased
in LMIC by w48% and is projected to almost double
(93% increase) by 2020. On average, fish consump-
tion is 2 to 3 times higher in HIC than LMIC (74),
although with marked heterogeneity within income
categories. China has the highest per-capita con-
sumption of fish in the world, followed by Oceania,
North America, and Europe (74). Globally, although
there has been little or no increase in sea fish con-
sumption per capita since the 1960s, catches per year
have risen exponentially (75) and freshwater fish
intake has increased during this time (71). Eggs are
similarly consumed in higher quantities (2 to 6 times
per week) in HIC relative to LMIC, with a 14% decline
in consumption in HIC observed between 1980 and
2000, and no change was observed in LMIC (76). The
Anand et al. J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5
Diet, Cardiovascular Disease, and the Food System O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4
1594
over 75% of foods, have some form of added sugar
(60). With urbanization there is some evidence to
show that refined carbohydrate consumption is
increasing, whereas consumption of traditional
grains (i.e., millet, maize) is decreasing in LMIC
(61,62).
A second key change has been the increasing
intake of vegetable oils, including processed vege-
table oils, and a decline in consumption of animal fats
(2,63). This was initially driven by rising production
of soybeans in the United States, later in Argentina
and Brazil, and then palm oil in East Asia. Oilseeds are
now among the most widely traded crops, and are
also processed to create margarines and vegetable
shortenings and into partially hydrogenated fats and
bleached deodorized oils for use in processed foods
(Online Appendix, Box 2). Between 1958 and 1996,a
major global shift occurred in the amount and types
of available fats, with soybean, palm, and rapeseed/
canola oils replacing butter, tallow, and lard. From
1958 to 1962, soybean, palm, and rapeseed/canola oils
represented 20% of the 29 million metric tons of fat
produced globally per year, whereas butter, lard, and
tallow represented 37%. By 1996 to 2001, these oils
accounted for 52% of the 103 million metric tons of fat
produced globally per year, whereas butter, lard, and
tallow contributed 20% (64). This has implications for
consumption of fatty acids. Palm oil (deodorized) has
become an increasing source of saturated fatty acids;
and partially hydrogenated fats are the main source
of trans fatty acids. Between 1990 and 2010, global
saturated fat, dietary cholesterol, and trans fat in-
takes remained stable (trans fats going down in HIC
and up in LMIC), whereas n-6, seafood n-3, and plant
n-3 fat intakes each increased (65). Vegetable oil
consumption remains 2 times higher in HIC than in
LMIC. However, trans fat consumption is very high in
many LMIC although decreasing markedly in HIC. In
India, for example, vanaspati, a vegetable ghee used
A third key change has been the increasing
global consumption of meat, which has been made
economically feasible by subsidized production of
crops for animal feed—most importantly corn and
soybeans (soybean oil is a byproduct of soymeal
production for animals) (66–69). At very low levels
of intake animal food consumption may not induce
harm, providing high-quality protein and iron,
whereas excess animal food intake in HIC may
be linked to adverse health outcomes, particularly
from processed meats (70). Meat consumption has
increased considerably worldwide, and there is sub-
stantially greater production of meat in HIC than in
LMIC (71). North and South America, Europe, and
Australia/New Zealand have the highest meat intake,
whereas Asia and Africa have the lowest (72,73).
Processed meats (which refers to post-butchering
modifications of foods such as curing, smoking, or
addition of sodium nitrate), account for 35.8% of all
meat consumed in HIC (unpublished data from the
PURE [Prospective Urban and Rural Epidemiological]
study) (71).
Dietary consumption patterns of other protein
sources have been mixed. Between 1973 and 1997,
dairy consumption per capita (kilograms) increased
in LMIC by w48% and is projected to almost double
(93% increase) by 2020. On average, fish consump-
tion is 2 to 3 times higher in HIC than LMIC (74),
although with marked heterogeneity within income
categories. China has the highest per-capita con-
sumption of fish in the world, followed by Oceania,
North America, and Europe (74). Globally, although
there has been little or no increase in sea fish con-
sumption per capita since the 1960s, catches per year
have risen exponentially (75) and freshwater fish
intake has increased during this time (71). Eggs are
similarly consumed in higher quantities (2 to 6 times
per week) in HIC relative to LMIC, with a 14% decline
in consumption in HIC observed between 1980 and
2000, and no change was observed in LMIC (76). The
Anand et al. J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5
Diet, Cardiovascular Disease, and the Food System O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4
1594
Total production of tree nuts in 2012 was 3.5 million
metric tons, a 5.5% increase from 2011. World con-
sumption of tree nuts in 2011 exceeded 3 million
metric tons (81).
A fourth key change is the marked growth of pur-
chases of all packaged foods and beverages (all cate-
gories of processing). This process is accelerating
across all LMIC markets (13,82,83). For example,
58% of calories consumed by Mexicans come from
packaged foods and beverages, which is similar
throughout the Americas (83) and even within the
United States (66%) (65,84). The proportion for China
is 28.5% and rising rapidly (36,82,83). The component
of snack foods that is “ultra-processed” (i.e., ready to
eat) varies depending on the method of measurement
but is increasing wherever it is studied at all income
levels (50,85,86). The shift to ultra-processed foods
has not just affected the food available for consump-
tion but also the way food is consumed (87). The way
people eat has changed greatly across the globe and the
pace of change is quickening. Snacking and snack
foods have grown in frequency and number (43–48);
eating frequency has increased; away-from-home
eating in restaurants, in fast food outlets, and from
take-out meals is increasing dramatically in LMIC;
both at home and away-from-home eating increa-
singly involve fried and processed food (47); and
the overall proportion of highly processed food in diets
has grown (50,51).
A fifth trend noted previously in relation to the
added sugar change is the shift in the way LMIC are
experiencing a marked increase in added sugar in
beverages. In the 1985 to 2005 period extensive added
sugar intake occurred across HIC (55) but more
recently large increases have occurred in LMIC,
particularly in consumption of SSBs and ultra-
processed foods (56–59). Today in the U.S. packaged
and processed food supply, >75% of foods have some
form of added sugar (60).
In addition, fruit and vegetable intake has re-
reported consuming fruits and vegetables 5 or more
times per day (91).
Although all of these changes across LMIC display
great heterogeneity (92), the global food system has
clearly reached all corners of the LMIC urban and
rural sector and major shifts in diets appear to be
accelerating.
IMPLICATIONS FOR ENVIRONMENTAL IMPACTS. The
modern food system is a major force in a range of
serious environmental problems, including climate
change (as a leading source of greenhouse gas emis-
sions, including carbon dioxide, methane, and nitrous
oxide), the loss of biodiversity, the strain on fresh-
water resources, and the release of persistent toxins,
excess nitrates and phosphates (from fertilizer and
concentrated livestock operations, causing wide-
spread problems of eutrophication), and animal phar-
maceutical residues into waterways (12,93–95).
The major causes are beef and other large animals
for greenhouse gas and the metabolic losses associ-
ated with shifting the product of nearly one-third of
the world’s arable land to concentrated animals,
which effectively magnifies the resource budgets and
pollution loads of industrial monocultures (34). The
expansion of low-input agriculture and extensive
ranching are also major factors in deforestation,
which bear heavily on both climate change (as carbon
is released from vegetation and soils and sequestra-
tion capacity diminishes) and biodiversity loss.
In addition to being a major force in many envi-
ronmental problems, world agriculture is also ex-
tremely vulnerable to climate change, biodiversity
loss, declining freshwater availability, and the inevi-
table limits of nonrenewable resources (e.g., fossil
energy, high-grade phosphorous) although vulnera-
bility is highly uneven on a world scale (96). Many of
the world’s poorest-regions are poised to be most
adversely affected by rising average temperatures,
aridity, and water stress, as well as through increas-
ingly severe extreme weather events such as drought
J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5 Anand et al.
O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4 Diet, Cardiovascular Disease, and the Food System
1595
metric tons, a 5.5% increase from 2011. World con-
sumption of tree nuts in 2011 exceeded 3 million
metric tons (81).
A fourth key change is the marked growth of pur-
chases of all packaged foods and beverages (all cate-
gories of processing). This process is accelerating
across all LMIC markets (13,82,83). For example,
58% of calories consumed by Mexicans come from
packaged foods and beverages, which is similar
throughout the Americas (83) and even within the
United States (66%) (65,84). The proportion for China
is 28.5% and rising rapidly (36,82,83). The component
of snack foods that is “ultra-processed” (i.e., ready to
eat) varies depending on the method of measurement
but is increasing wherever it is studied at all income
levels (50,85,86). The shift to ultra-processed foods
has not just affected the food available for consump-
tion but also the way food is consumed (87). The way
people eat has changed greatly across the globe and the
pace of change is quickening. Snacking and snack
foods have grown in frequency and number (43–48);
eating frequency has increased; away-from-home
eating in restaurants, in fast food outlets, and from
take-out meals is increasing dramatically in LMIC;
both at home and away-from-home eating increa-
singly involve fried and processed food (47); and
the overall proportion of highly processed food in diets
has grown (50,51).
A fifth trend noted previously in relation to the
added sugar change is the shift in the way LMIC are
experiencing a marked increase in added sugar in
beverages. In the 1985 to 2005 period extensive added
sugar intake occurred across HIC (55) but more
recently large increases have occurred in LMIC,
particularly in consumption of SSBs and ultra-
processed foods (56–59). Today in the U.S. packaged
and processed food supply, >75% of foods have some
form of added sugar (60).
In addition, fruit and vegetable intake has re-
reported consuming fruits and vegetables 5 or more
times per day (91).
Although all of these changes across LMIC display
great heterogeneity (92), the global food system has
clearly reached all corners of the LMIC urban and
rural sector and major shifts in diets appear to be
accelerating.
IMPLICATIONS FOR ENVIRONMENTAL IMPACTS. The
modern food system is a major force in a range of
serious environmental problems, including climate
change (as a leading source of greenhouse gas emis-
sions, including carbon dioxide, methane, and nitrous
oxide), the loss of biodiversity, the strain on fresh-
water resources, and the release of persistent toxins,
excess nitrates and phosphates (from fertilizer and
concentrated livestock operations, causing wide-
spread problems of eutrophication), and animal phar-
maceutical residues into waterways (12,93–95).
The major causes are beef and other large animals
for greenhouse gas and the metabolic losses associ-
ated with shifting the product of nearly one-third of
the world’s arable land to concentrated animals,
which effectively magnifies the resource budgets and
pollution loads of industrial monocultures (34). The
expansion of low-input agriculture and extensive
ranching are also major factors in deforestation,
which bear heavily on both climate change (as carbon
is released from vegetation and soils and sequestra-
tion capacity diminishes) and biodiversity loss.
In addition to being a major force in many envi-
ronmental problems, world agriculture is also ex-
tremely vulnerable to climate change, biodiversity
loss, declining freshwater availability, and the inevi-
table limits of nonrenewable resources (e.g., fossil
energy, high-grade phosphorous) although vulnera-
bility is highly uneven on a world scale (96). Many of
the world’s poorest-regions are poised to be most
adversely affected by rising average temperatures,
aridity, and water stress, as well as through increas-
ingly severe extreme weather events such as drought
J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5 Anand et al.
O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4 Diet, Cardiovascular Disease, and the Food System
1595
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
MACRONUTRIENTS, FOODS,
AND CVD RISK FACTORS
CARBOHYDRATES. Refined carbohydrates. CVD Risk
Factors. U.S. ecological evidence demonstrates an
association of refined carbohydrate (such as corn
syrup) with type 2 diabetes mellitus (T2DM) and
obesity (54). Robust data from systematic reviews and
high-quality randomized controlled trials (RCTs)
support a harmful effect of highly refined, high–
glycemic load (GL) carbohydrates. A meta-analysis of
observational studies indicated that high–glycemic
index (GI) foods are associated with T2DM (103).
Proof-of-concept studies have used alpha-glucosidase
inhibitors, such as acarbose, to lower the GI of the
foods consumed; for example, in the STOP-NIDDM
(Study to Prevent Non-Insulin-Dependent Diabetes
Mellitus) trial, acarbose reduced progression to T2DM
by 25% compared with placebo (104). T2DM risk in
individuals with the highest GL and lowest cereal fi-
ber is 2.5-fold that of those with the lowest GL and
highest cereal fiber diet (105). A large Danish pro-
spective cohort study of the impact of replacing
saturated fats with high-GI carbohydrates found that
when high-GI carbohydrates replace saturated fat,
myocardial infarction (MI) risk increases 33% (106).
A meta-analysis of 10 prospective cohort studies
(n ¼ 296,849) (107) found increased GL associated
with a 27% increased coronary heart disease (CHD)
and MI risk (108). In controlled-feeding studies,
replacing saturated fat with carbohydrates lowers
low-density lipoprotein cholesterol (LDL-C) and high-
density lipoprotein cholesterol (HDL-C) and increases
triglycerides (109). Dietary interventions that raise
HDL-C may not necessarily translate into CVD risk
reduction, as serum HDL-C has recently been called
into question regarding its role in the causal pathway
of CVD (110). However, in a 5-week controlled-feeding
trial of 163 generally healthy but overweight adults,
low compared with high-GI diets did not improve
reduced fiber content. Carbohydrate refinement is
common in HIC and increasing in LMIC (111,112).
Traditional diets in LMIC, once rich in whole grains
and dietary fiber, now include highly refined carbo-
hydrates, such as polished white rice and refined
flours. In East Asian countries, white rice consump-
tion is associated with a 55% higher T2DM risk
(111,112).In the cross-sectional CURES 57 (Chennai
Urban Rural Epidemiology Study 57) study, higher
refined grain intake was associated with higher
waist circumference, systolic and diastolic blood
pressure, fasting glucose, triglycerides, and insulin
resistance and lower HDL-C levels (61). Replacing
white with brown rice (50 g/day) reduced T2DM risk
by 16% (113), and substituting beans for white rice
reduced the odds of metabolic syndrome by 35%
(108). However, a 16-week randomized trial of
replacing white with brown rice in middle-aged
Chinese men and women with or at high risk for
T2DM only improved HDL-C and reduced diastolic
blood pressure in the brown rice group. Data from
the international PURE study (138,926 individuals in
628 communities in 17 countries) suggest a need to
consider the context and availability of specific
foods before making food choice recommendations
(114). Increasing whole grain and cereal fiber
consumption whereas decreasing total and high-GI
carbohydrate are helpful strategies to prevent
T2DM and CVD in the general population (115).
Furthermore, low-GI diets improve glycemic control
and serum lipids in RCTs of participants with T2DM
with major implications for CHD risk reduction in
this vulnerable segment of the population whose
numbers are increasing rapidly globally (116–119).
Sugar-sweetened beverages. SSB and Cardiovascular
Risk Factors. SSB consumption accounts for up to
50% of added sugar in the American diet (120,121).
The epidemiological relationships between SSB con-
sumption, overweight, obesity, hypertension, and
T2DM are strong (122). In a meta-analysis of pro-
Anand et al. J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5
Diet, Cardiovascular Disease, and the Food System O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4
1596
AND CVD RISK FACTORS
CARBOHYDRATES. Refined carbohydrates. CVD Risk
Factors. U.S. ecological evidence demonstrates an
association of refined carbohydrate (such as corn
syrup) with type 2 diabetes mellitus (T2DM) and
obesity (54). Robust data from systematic reviews and
high-quality randomized controlled trials (RCTs)
support a harmful effect of highly refined, high–
glycemic load (GL) carbohydrates. A meta-analysis of
observational studies indicated that high–glycemic
index (GI) foods are associated with T2DM (103).
Proof-of-concept studies have used alpha-glucosidase
inhibitors, such as acarbose, to lower the GI of the
foods consumed; for example, in the STOP-NIDDM
(Study to Prevent Non-Insulin-Dependent Diabetes
Mellitus) trial, acarbose reduced progression to T2DM
by 25% compared with placebo (104). T2DM risk in
individuals with the highest GL and lowest cereal fi-
ber is 2.5-fold that of those with the lowest GL and
highest cereal fiber diet (105). A large Danish pro-
spective cohort study of the impact of replacing
saturated fats with high-GI carbohydrates found that
when high-GI carbohydrates replace saturated fat,
myocardial infarction (MI) risk increases 33% (106).
A meta-analysis of 10 prospective cohort studies
(n ¼ 296,849) (107) found increased GL associated
with a 27% increased coronary heart disease (CHD)
and MI risk (108). In controlled-feeding studies,
replacing saturated fat with carbohydrates lowers
low-density lipoprotein cholesterol (LDL-C) and high-
density lipoprotein cholesterol (HDL-C) and increases
triglycerides (109). Dietary interventions that raise
HDL-C may not necessarily translate into CVD risk
reduction, as serum HDL-C has recently been called
into question regarding its role in the causal pathway
of CVD (110). However, in a 5-week controlled-feeding
trial of 163 generally healthy but overweight adults,
low compared with high-GI diets did not improve
reduced fiber content. Carbohydrate refinement is
common in HIC and increasing in LMIC (111,112).
Traditional diets in LMIC, once rich in whole grains
and dietary fiber, now include highly refined carbo-
hydrates, such as polished white rice and refined
flours. In East Asian countries, white rice consump-
tion is associated with a 55% higher T2DM risk
(111,112).In the cross-sectional CURES 57 (Chennai
Urban Rural Epidemiology Study 57) study, higher
refined grain intake was associated with higher
waist circumference, systolic and diastolic blood
pressure, fasting glucose, triglycerides, and insulin
resistance and lower HDL-C levels (61). Replacing
white with brown rice (50 g/day) reduced T2DM risk
by 16% (113), and substituting beans for white rice
reduced the odds of metabolic syndrome by 35%
(108). However, a 16-week randomized trial of
replacing white with brown rice in middle-aged
Chinese men and women with or at high risk for
T2DM only improved HDL-C and reduced diastolic
blood pressure in the brown rice group. Data from
the international PURE study (138,926 individuals in
628 communities in 17 countries) suggest a need to
consider the context and availability of specific
foods before making food choice recommendations
(114). Increasing whole grain and cereal fiber
consumption whereas decreasing total and high-GI
carbohydrate are helpful strategies to prevent
T2DM and CVD in the general population (115).
Furthermore, low-GI diets improve glycemic control
and serum lipids in RCTs of participants with T2DM
with major implications for CHD risk reduction in
this vulnerable segment of the population whose
numbers are increasing rapidly globally (116–119).
Sugar-sweetened beverages. SSB and Cardiovascular
Risk Factors. SSB consumption accounts for up to
50% of added sugar in the American diet (120,121).
The epidemiological relationships between SSB con-
sumption, overweight, obesity, hypertension, and
T2DM are strong (122). In a meta-analysis of pro-
Anand et al. J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5
Diet, Cardiovascular Disease, and the Food System O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4
1596
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4-year period (126), possibly due to incomplete
compensation for this energy at other meals. After
adjusting for important potential confounders,
including body mass index, $1/day versus <1 SSB/
month increased T2DM by 39% (127). A meta-analysis
of 310,819 participants and 15,043 cases of T2DM re-
ported a 26% increased T2DM risk among those
consuming 1 to 2 SSB servings/day compared with
nonconsumers (128). A meta-analysis of 4 cohort
studies reported a linear association between SSB and
hypertension risk (RR) of 1.08 (95% CI: 1.04 to 1.12)
per serving per day (129). The Framingham Offspring
Study reported a 22% higher incidence of hyper-
tension among those consuming $1 SSB serving/day
compared with nonconsumers (130). A potential
explanation of the SSB-T2DM association is the high
content of rapidly absorbed sugar from corn syrup,
which increases blood glucose and insulin and de
novo lipogenesis—which may contribute to pancre-
atic beta cell dysfunction and eventually T2DM (131).
In the NHANES III (National Health and Nutrition
Examination Survey III) study, with 831 CVD deaths
during 163,039 person-years of follow-up, con-
sumption of $7 SSB servings/week was associated
with a 29% increased CVD mortality risk compared
with <1 serving/week (120), with no increased risk
up to 6 drinks/week. Few studies have investigated
the association between SSBs and CVD events.
Those that have, report increased CHD and stroke
risk with SSB consumption. A 2015 meta-analysis
reported an RR for incident CHD of 1.17 (95% CI:
1.10 to 1.24) per serving per day increase in
SSB consumption (129). Both the HPFS and the
NHS find an approximate 20% increased CHD risk
in the highest category of SSB consumption com-
pared with the lowest category (132,133);and, after
adjusting for dietary and nondietary cardiovascular
risk factors, a 16% increased stroke risk (134). Simi-
larly, 2 Swedish prospective cohort studies in
women and men reported a RR of 1.19 (95% CI: 1.04
FATS AND OILS. C V D r i s k f a c t o r s .Vegetable oils
that are primarily comprised of mono- (e.g., olive oil)
and polyunsaturated fatty acids appear to reduce
CHD risk, and sources of the n-3 polyunsaturated fat
alpha-linolenic acid, such as rapeseed or canola oil,
are cardioprotective. Replacing saturated fat with
monounsaturated or polyunsaturated fat reduces
LDL-C and preserves HDL-C (109). Further, canola oil,
as part of a low-GI diet, improves glycemic control
and blood lipids in T2DM (138). Trans fatty acids in-
crease CHD risk compared with other macronutrients,
with strong evidence of adverse effects of small
amounts of trans fats on lipids (109,139) and CVD risk
(140,141).
Though total fat (142), and specifically saturated
fats, have generally been considered to be deleterious
to insulin sensitivity (143), in large cohort studies,
saturated fat is not associated with development of
T2DM, after adjustment for body mass index, total di-
etary fiber, or magnesium intake (144–149). Macronu-
trient exchange generally does not influence markers
of glucose homeostasis, though in 2 relatively large
trials, replacing saturated fat with either mono-
unsaturated fat or carbohydrate improved indices of
glucose homeostasis (150,151). Associations have been
seen between major food sources of saturated fat, such
as red and processed meat, and development of T2DM
(152,153),though dairy products, notably fermented
dairy, may be protective (154,155).
C V D .Saturated fats have not been consistently
associated with CVD in meta-analyses of cohort
studies (odds ratio [OR]: 1.07; 95% CI: 0.96 to 1.19)
of higher compared with lower intakes (156). How-
ever, in most of these studies the association of
high saturated fat intake largely represents repla-
cing highly refined carbohydrates. Replacing satu-
rated fat with highly refined carbohydrate is not
associated with lower CHD risk, whereas replacing
saturated fat with polyunsaturated fat reduces CHD
risk (157,158). This benefit of polyunsaturated fat
J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5 Anand et al.
O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4 Diet, Cardiovascular Disease, and the Food System
1597
compensation for this energy at other meals. After
adjusting for important potential confounders,
including body mass index, $1/day versus <1 SSB/
month increased T2DM by 39% (127). A meta-analysis
of 310,819 participants and 15,043 cases of T2DM re-
ported a 26% increased T2DM risk among those
consuming 1 to 2 SSB servings/day compared with
nonconsumers (128). A meta-analysis of 4 cohort
studies reported a linear association between SSB and
hypertension risk (RR) of 1.08 (95% CI: 1.04 to 1.12)
per serving per day (129). The Framingham Offspring
Study reported a 22% higher incidence of hyper-
tension among those consuming $1 SSB serving/day
compared with nonconsumers (130). A potential
explanation of the SSB-T2DM association is the high
content of rapidly absorbed sugar from corn syrup,
which increases blood glucose and insulin and de
novo lipogenesis—which may contribute to pancre-
atic beta cell dysfunction and eventually T2DM (131).
In the NHANES III (National Health and Nutrition
Examination Survey III) study, with 831 CVD deaths
during 163,039 person-years of follow-up, con-
sumption of $7 SSB servings/week was associated
with a 29% increased CVD mortality risk compared
with <1 serving/week (120), with no increased risk
up to 6 drinks/week. Few studies have investigated
the association between SSBs and CVD events.
Those that have, report increased CHD and stroke
risk with SSB consumption. A 2015 meta-analysis
reported an RR for incident CHD of 1.17 (95% CI:
1.10 to 1.24) per serving per day increase in
SSB consumption (129). Both the HPFS and the
NHS find an approximate 20% increased CHD risk
in the highest category of SSB consumption com-
pared with the lowest category (132,133);and, after
adjusting for dietary and nondietary cardiovascular
risk factors, a 16% increased stroke risk (134). Simi-
larly, 2 Swedish prospective cohort studies in
women and men reported a RR of 1.19 (95% CI: 1.04
FATS AND OILS. C V D r i s k f a c t o r s .Vegetable oils
that are primarily comprised of mono- (e.g., olive oil)
and polyunsaturated fatty acids appear to reduce
CHD risk, and sources of the n-3 polyunsaturated fat
alpha-linolenic acid, such as rapeseed or canola oil,
are cardioprotective. Replacing saturated fat with
monounsaturated or polyunsaturated fat reduces
LDL-C and preserves HDL-C (109). Further, canola oil,
as part of a low-GI diet, improves glycemic control
and blood lipids in T2DM (138). Trans fatty acids in-
crease CHD risk compared with other macronutrients,
with strong evidence of adverse effects of small
amounts of trans fats on lipids (109,139) and CVD risk
(140,141).
Though total fat (142), and specifically saturated
fats, have generally been considered to be deleterious
to insulin sensitivity (143), in large cohort studies,
saturated fat is not associated with development of
T2DM, after adjustment for body mass index, total di-
etary fiber, or magnesium intake (144–149). Macronu-
trient exchange generally does not influence markers
of glucose homeostasis, though in 2 relatively large
trials, replacing saturated fat with either mono-
unsaturated fat or carbohydrate improved indices of
glucose homeostasis (150,151). Associations have been
seen between major food sources of saturated fat, such
as red and processed meat, and development of T2DM
(152,153),though dairy products, notably fermented
dairy, may be protective (154,155).
C V D .Saturated fats have not been consistently
associated with CVD in meta-analyses of cohort
studies (odds ratio [OR]: 1.07; 95% CI: 0.96 to 1.19)
of higher compared with lower intakes (156). How-
ever, in most of these studies the association of
high saturated fat intake largely represents repla-
cing highly refined carbohydrates. Replacing satu-
rated fat with highly refined carbohydrate is not
associated with lower CHD risk, whereas replacing
saturated fat with polyunsaturated fat reduces CHD
risk (157,158). This benefit of polyunsaturated fat
J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5 Anand et al.
O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4 Diet, Cardiovascular Disease, and the Food System
1597
cardiac deaths and nonfatal CHD (163), whereas the
PREDIMED (Prevención con Dieta Mediterránea) RCT
found that a Mediterranean diet (50 g/day extra virgin
olive oil) reduced CVD events by 30% over a 5-year
period (164).
Palm oil is the dominant fat globally and is rela-
tively high in saturated fat. On the basis of controlled-
feeding studies examining changes in blood lipids,
replacing palm oil with unsaturated fatty acids would
be expected to lower CHD risk (109), but palm oil
would be preferred to partially hydrogenated oils
high in trans fatty acids. Few studies have directly
compared palm oil with other oils for CHD risk. One
large case-control study in Costa Rica found that
soybean oil consumption was associated with lower
acute MI risk compared with palm oil consumption
(165).
S u m m a r y o ff a t sa n d o i l s .Compared with satu-
rated fat, vegetable oils rich in polyunsaturated fats
reduce the TC:HDL-C (total cholesterol:HDL-C) ratio
and CHD incidence; inclusion of n-3 fatty acids
(alpha-linolenic acid) with the vegetable oils is
important for CHD prevention. The effect of
replacing saturated fat with carbohydrate on CHD
risk appears to depend on the quality of the carbo-
hydrate. Prospective studies consistently indicate
adverse effects of trans fats on CHD. Effects of
monounsaturated fat from plant sources require
further study; extra virgin olive oil appears to re-
duce CVD.
PROTEIN SOURCES. M e a t s .Nutrients and CVD Risk
Factors. Meat is rich in protein, iron, zinc, and B
vitamins, but can also contain significant amounts
of cholesterol and saturated fatty acids, which
raise LDL-C and lower triglyceride (157). A high
red meat intake (rich in heme iron), increases
endogenous formation of N-nitroso compounds in
the gastrointestinal tract that are associated with
increased epithelial proliferation, oxidative stress,
and iron-induced hypoxia signaling (166–168).
content and N-nitroso compounds, also implicated in
colorectal cancer (167). The evidence suggests that
processed meat consumption increases CHD risk,
whereas unprocessed meat consumption has a small
or no association with CHD, mainly when compared
with refined starch and sugar. Both unprocessed and
processed red meats are associated with greater CVD
risk compared with poultry, fish, or vegetable protein
sources. Both types of meat are associated with
higher T2DM risk, although gram for gram the effect
size is notably larger for processed meats.
LMIC. Data relating meat consumption to CVD risk in
LMIC is limited. A recent pooled analysis of data
from 296,721 individuals from Asian countries (i.e.,
Bangladesh, mainland China, Japan, Korea, and
Taiwan) found no association between red meat and
poultry consumption and CVD, cancer mortality, or
all-cause mortality (173). Red meat intake is generally
much lower in these areas than in HIC however, and
current consumption does not likely reflect long-
term patterns.
D a i r y .CVD Risk Factors. The consumption of dairy
products has been associated with weight loss in
small studies (174), but the overall published data
does not confirm an important effect on body weight.
However, increased low-fat dairy consumption is
associated with lower LDL-C, triglycerides, plasma
insulin, insulin resistance, waist circumference, body
mass index, possibly blood pressure; and reduced
diabetes risk (174–182). In a large meta-analysis of
cohort studies (13,000 incident cases), and the EPIC
InterAct (European Prospective Investigation into
Cancer and Nutrition) case-cohort study (12,000
incident cases), fermented dairy (i.e., yogurt,
cheese, and thick fermented milk), but not total
dairy, was inversely associated with T2DM (155,183).
In a meta-analysis of prospective cohort studies,
milk consumption was inversely associated with
total CVD in a small subset of studies with few
cases, but using a larger body of data with more
Anand et al. J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5
Diet, Cardiovascular Disease, and the Food System O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4
1598
PREDIMED (Prevención con Dieta Mediterránea) RCT
found that a Mediterranean diet (50 g/day extra virgin
olive oil) reduced CVD events by 30% over a 5-year
period (164).
Palm oil is the dominant fat globally and is rela-
tively high in saturated fat. On the basis of controlled-
feeding studies examining changes in blood lipids,
replacing palm oil with unsaturated fatty acids would
be expected to lower CHD risk (109), but palm oil
would be preferred to partially hydrogenated oils
high in trans fatty acids. Few studies have directly
compared palm oil with other oils for CHD risk. One
large case-control study in Costa Rica found that
soybean oil consumption was associated with lower
acute MI risk compared with palm oil consumption
(165).
S u m m a r y o ff a t sa n d o i l s .Compared with satu-
rated fat, vegetable oils rich in polyunsaturated fats
reduce the TC:HDL-C (total cholesterol:HDL-C) ratio
and CHD incidence; inclusion of n-3 fatty acids
(alpha-linolenic acid) with the vegetable oils is
important for CHD prevention. The effect of
replacing saturated fat with carbohydrate on CHD
risk appears to depend on the quality of the carbo-
hydrate. Prospective studies consistently indicate
adverse effects of trans fats on CHD. Effects of
monounsaturated fat from plant sources require
further study; extra virgin olive oil appears to re-
duce CVD.
PROTEIN SOURCES. M e a t s .Nutrients and CVD Risk
Factors. Meat is rich in protein, iron, zinc, and B
vitamins, but can also contain significant amounts
of cholesterol and saturated fatty acids, which
raise LDL-C and lower triglyceride (157). A high
red meat intake (rich in heme iron), increases
endogenous formation of N-nitroso compounds in
the gastrointestinal tract that are associated with
increased epithelial proliferation, oxidative stress,
and iron-induced hypoxia signaling (166–168).
content and N-nitroso compounds, also implicated in
colorectal cancer (167). The evidence suggests that
processed meat consumption increases CHD risk,
whereas unprocessed meat consumption has a small
or no association with CHD, mainly when compared
with refined starch and sugar. Both unprocessed and
processed red meats are associated with greater CVD
risk compared with poultry, fish, or vegetable protein
sources. Both types of meat are associated with
higher T2DM risk, although gram for gram the effect
size is notably larger for processed meats.
LMIC. Data relating meat consumption to CVD risk in
LMIC is limited. A recent pooled analysis of data
from 296,721 individuals from Asian countries (i.e.,
Bangladesh, mainland China, Japan, Korea, and
Taiwan) found no association between red meat and
poultry consumption and CVD, cancer mortality, or
all-cause mortality (173). Red meat intake is generally
much lower in these areas than in HIC however, and
current consumption does not likely reflect long-
term patterns.
D a i r y .CVD Risk Factors. The consumption of dairy
products has been associated with weight loss in
small studies (174), but the overall published data
does not confirm an important effect on body weight.
However, increased low-fat dairy consumption is
associated with lower LDL-C, triglycerides, plasma
insulin, insulin resistance, waist circumference, body
mass index, possibly blood pressure; and reduced
diabetes risk (174–182). In a large meta-analysis of
cohort studies (13,000 incident cases), and the EPIC
InterAct (European Prospective Investigation into
Cancer and Nutrition) case-cohort study (12,000
incident cases), fermented dairy (i.e., yogurt,
cheese, and thick fermented milk), but not total
dairy, was inversely associated with T2DM (155,183).
In a meta-analysis of prospective cohort studies,
milk consumption was inversely associated with
total CVD in a small subset of studies with few
cases, but using a larger body of data with more
Anand et al. J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5
Diet, Cardiovascular Disease, and the Food System O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4
1598
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
T2DM (RR: 0.65; 95% CI: 0.49 to 0.85) than
nonconsumers (185).
E g g .CVD Risk Factors. Eggs are a relatively in-
expensive and low-calorie source of protein, folate,
and B vitamins (186). Eggs are also a source of
dietary cholesterol (a medium egg contains approxi-
mately 225 mg of cholesterol) (187). A meta-analysis
showed that eggs increase TC, HDL-C, and TC:HDL-C
(188), but 5 RCTs subsequently reported that egg
consumption did not significantly alter these para-
meters (189–191)or endothelial function (192,193).No
RCT has tested the effect of egg consumption on CVD
events. In a meta-analysis (194) of 16 prospective cohort
studies (90,735 participants) (191), egg consumption
was not associated with overall CVD or CHD, stroke, or
CHD or stroke mortality; but was associated with T2DM.
Overall, consumption of eggs in moderation (1 egg/day)
is likely neutral for CVD. However, relative to other
protein-rich foods that lower LDL cholesterol, such as
whole grains and nuts, eggs would likely increase
CVD risk.
LMIC. Unpublished data from 3 large international
studies, PURE (Prospective Urban and Rural Epide-
miological Study), ONTARGET (Ongoing Telmisartan
Alone and in Combination with Ramipril Global
Endpoint Trial), and INTERHEART (a global study of
risk factors for acute myocardial infarction), with
collectively 200,000 individuals and 22,000 CVD
events from regions including China, India, and Af-
rica, show that moderate egg consumption appears to
be neutral or protective against CVD. However, sig-
nificant variations exist across regions, with a benefit
of daily egg consumption in China but possible harm
in South Asia.
F i s h .CVD Risk Factors. Fish are a source of protein,
vitamin D, multiple B vitamins, essential amino
acids, and trace elements; and the long-chain
omega-3 (n-3) fatty acids docosahexaenoic acid and
eicosapentaenoic acid (195,196), though amounts
vary over 10-fold across seafood species. Fatty
explanations include differences in the amounts and
types of fish consumed, cooking methods, and
background fish consumption. Fifteen of the 16
cohort studies (with 1 exception) (199) were con-
ducted in North America and European countries,
where deep-frying fish is common. The DART-1 (Diet
and Reinfarction) trials, a secondary prevention trial
and DART-2, in men with stable angina, are the only
randomized trial of fish intake and CVD outcomes.
They arrive at opposite conclusions. In the DART-1
trial, fish lowered all-cause mortality and trended
toward reducing CVD events after 2 years (194). In
the DART-2 trial oily fish did not affect all-cause
mortality or CVD events after 3 to 9 years, and
increased sudden cardiac death, largely confined to
the subgroup given fish oil capsules (200). Differ-
ential behavioral change or CVD stage may explain
the discrepancy (201). Follow-up of the DART-1 trial
at 5 years also showed increased rates of CVD in the
fish/fish oil group that did not persist through the
10-year assessment (202). We know of no primary
prevention trial on fish intake and CVD outcomes,
but a meta-analysis of fish oil supplement RCTs is
neutral (203).
Low-Income Countries and HIC. Mostof the data indi-
cating that fish is protective comes from studies
in HIC (204–208). Unpublished data from 3 large
international studies (PURE, ONTARGET, and
INTERHEART) reflect considerable heterogeneity in
the association between fish intake and CVD out-
comes. In the PURE study fish intake was inversely
associated with CVD outcomes in South America,
China, North America, and Europe (RR: 0.76 to
0.84) but positively associated in South Asia (RR:
1.97). However, no associations between fish con-
sumption and CVD outcomes were observed in a
high-risk secondary population in the ONTARGET
study. The INTERHEART study found fish intake
beneficial in North America and Europe (RR: 0.73;
95% CI: 0.62 to 0.87) but harmful in the Middle
J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5 Anand et al.
O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4 Diet, Cardiovascular Disease, and the Food System
1599
nonconsumers (185).
E g g .CVD Risk Factors. Eggs are a relatively in-
expensive and low-calorie source of protein, folate,
and B vitamins (186). Eggs are also a source of
dietary cholesterol (a medium egg contains approxi-
mately 225 mg of cholesterol) (187). A meta-analysis
showed that eggs increase TC, HDL-C, and TC:HDL-C
(188), but 5 RCTs subsequently reported that egg
consumption did not significantly alter these para-
meters (189–191)or endothelial function (192,193).No
RCT has tested the effect of egg consumption on CVD
events. In a meta-analysis (194) of 16 prospective cohort
studies (90,735 participants) (191), egg consumption
was not associated with overall CVD or CHD, stroke, or
CHD or stroke mortality; but was associated with T2DM.
Overall, consumption of eggs in moderation (1 egg/day)
is likely neutral for CVD. However, relative to other
protein-rich foods that lower LDL cholesterol, such as
whole grains and nuts, eggs would likely increase
CVD risk.
LMIC. Unpublished data from 3 large international
studies, PURE (Prospective Urban and Rural Epide-
miological Study), ONTARGET (Ongoing Telmisartan
Alone and in Combination with Ramipril Global
Endpoint Trial), and INTERHEART (a global study of
risk factors for acute myocardial infarction), with
collectively 200,000 individuals and 22,000 CVD
events from regions including China, India, and Af-
rica, show that moderate egg consumption appears to
be neutral or protective against CVD. However, sig-
nificant variations exist across regions, with a benefit
of daily egg consumption in China but possible harm
in South Asia.
F i s h .CVD Risk Factors. Fish are a source of protein,
vitamin D, multiple B vitamins, essential amino
acids, and trace elements; and the long-chain
omega-3 (n-3) fatty acids docosahexaenoic acid and
eicosapentaenoic acid (195,196), though amounts
vary over 10-fold across seafood species. Fatty
explanations include differences in the amounts and
types of fish consumed, cooking methods, and
background fish consumption. Fifteen of the 16
cohort studies (with 1 exception) (199) were con-
ducted in North America and European countries,
where deep-frying fish is common. The DART-1 (Diet
and Reinfarction) trials, a secondary prevention trial
and DART-2, in men with stable angina, are the only
randomized trial of fish intake and CVD outcomes.
They arrive at opposite conclusions. In the DART-1
trial, fish lowered all-cause mortality and trended
toward reducing CVD events after 2 years (194). In
the DART-2 trial oily fish did not affect all-cause
mortality or CVD events after 3 to 9 years, and
increased sudden cardiac death, largely confined to
the subgroup given fish oil capsules (200). Differ-
ential behavioral change or CVD stage may explain
the discrepancy (201). Follow-up of the DART-1 trial
at 5 years also showed increased rates of CVD in the
fish/fish oil group that did not persist through the
10-year assessment (202). We know of no primary
prevention trial on fish intake and CVD outcomes,
but a meta-analysis of fish oil supplement RCTs is
neutral (203).
Low-Income Countries and HIC. Mostof the data indi-
cating that fish is protective comes from studies
in HIC (204–208). Unpublished data from 3 large
international studies (PURE, ONTARGET, and
INTERHEART) reflect considerable heterogeneity in
the association between fish intake and CVD out-
comes. In the PURE study fish intake was inversely
associated with CVD outcomes in South America,
China, North America, and Europe (RR: 0.76 to
0.84) but positively associated in South Asia (RR:
1.97). However, no associations between fish con-
sumption and CVD outcomes were observed in a
high-risk secondary population in the ONTARGET
study. The INTERHEART study found fish intake
beneficial in North America and Europe (RR: 0.73;
95% CI: 0.62 to 0.87) but harmful in the Middle
J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5 Anand et al.
O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4 Diet, Cardiovascular Disease, and the Food System
1599
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

In observational studies (133,217–220)and RCTs
(164,221–223),a Mediterranean diet including nuts
lowers CVD risk. However, no RCTs have assessed the
effects of nut consumption alone on CVD events.
Taken together, the published data from observa-
tional studies and clinical trials support nuts for
lowering CVD risk.
LMIC. Unpublished data from the PURE cohort
indicate that nut consumption is very low in LMIC
(60% of individuals consume #1 nut serving/week).
No associations between nut consumption and
CVD outcomes are seen at this low level.
L e g u m e s .CVD Risk Factors. In observational studies
and RCTs consumption of legumes improves CVD risk
factors, such as waist circumference, cholesterol,
blood pressure, C-reactive protein, glucose; and is
protective against T2DM (224–231). A meta-analysis of
26 RCTs (1,037 participants) found that 130 g legumes/
day (w1 serving) reduced LDL-C by 0.17 mmol/l (95%
CI: –0.25 to –0.09) (228). Legumes also reduce systolic
blood pressure (by 2 mm Hg) and lowered mean
arterial pressure (231) in a meta-analysis of 8 RCTs.
A legume-rich diet reduced HbA1c (–0.3%; 95% CI:
–1.4% to –0.1%) in an RCT in participants with
diabetes (226).
CVD. In a meta-analysis of 5 observational studies,
100 g of legumes 4 times/week is inversely
associated with CHD (RR: 0.86; 95% CI: 0.78 to 0.94)
(232). However, that study and another meta-
analysis of 8 prospective cohort studies found no
association between legumes and diabetes (207) or
stroke (232,233). A large prospective study of 2
cohorts of U.S. health professionals found a 45%
increased risk of ischemic stroke per daily serving of
legumes (RR: 1.45; 95% CI: 1.06 to 2.00) (234). This
suggests that although legumes are valuable to
reduce CHD risk, more research is required to
understand their impact on total stroke risk.
LMIC. In a cohort of Chinese men and women, soy
(the primary legume consumed in China) was
protein were less likely to develop CHD (RR:
0.25; 95% CI: 0.10 to 0.63) than were those
consuming #4.5 g/day (238).
S u m m a r y o f m a j o r p r o t e i n s o u r c e s .Reducing red
meats, especially processed meats, and increasing
fish, nuts, legumes, and possibly fermented dairy
products are likely beneficial. Sustainability issues
discussed in this paper must also be addressed spe-
cifically in relation to meat, fish, and dairy foods
(12,34,239–241).
FRUITS AND VEGETABLES. C V D r i s k f a c t o r s .In the
DASH RCT, higher intake of fruits and vegetables,
either as part of a typical Western diet or the DASH
eating plan, reduced blood pressure, TC, LDL-C, and
HDL-C without affecting triglycerides (242). A meta-
analysis of 3 prospective cohorts (3,415 cases) found
high adherence to the DASH eating reduced T2DM
risk by 27% (243). A strong evidence base from
observational studies indicates that high consump-
tion of vegetables and fruits reduces CHD and
stroke (196).
C V D i n H I C a n d L M I C .Large global studies and
systematic reviews of prospective cohorts generally
support a protective role of fruits and vegetables
against CVD (244–246). In the global INTERSTROKE
study (3,000 stroke cases and 3,000 control cases),
compared with fewer than 1 serving per day, 1
serving of fruit was protective against stroke (OR:
0.61; 95% CI: 0.50 to 0.73), but the benefits were
not clear with higher consumption of up to 3 serv-
ings/day of vegetables was not (OR: 0.91; 95% CI:
0.75 to 1.10) (244). A meta-analysis of 20 prospec-
tive cohort studies (16,981 stroke events) found that
fruit and vegetable consumption was associated
with decreased stroke risk (RR: 0.79; 95% CI: 0.75 to
0.84 for highest vs. lowest categories), as were
fruits (RR: 0.77; 95% CI: 0.71 to 0.84) and vegeta-
bles (RR: 0.86; 95% CI: 0.79 to 0.93) separately
(245). In unpublished INTERHEART study data a
Anand et al. J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5
Diet, Cardiovascular Disease, and the Food System O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4
1600
(164,221–223),a Mediterranean diet including nuts
lowers CVD risk. However, no RCTs have assessed the
effects of nut consumption alone on CVD events.
Taken together, the published data from observa-
tional studies and clinical trials support nuts for
lowering CVD risk.
LMIC. Unpublished data from the PURE cohort
indicate that nut consumption is very low in LMIC
(60% of individuals consume #1 nut serving/week).
No associations between nut consumption and
CVD outcomes are seen at this low level.
L e g u m e s .CVD Risk Factors. In observational studies
and RCTs consumption of legumes improves CVD risk
factors, such as waist circumference, cholesterol,
blood pressure, C-reactive protein, glucose; and is
protective against T2DM (224–231). A meta-analysis of
26 RCTs (1,037 participants) found that 130 g legumes/
day (w1 serving) reduced LDL-C by 0.17 mmol/l (95%
CI: –0.25 to –0.09) (228). Legumes also reduce systolic
blood pressure (by 2 mm Hg) and lowered mean
arterial pressure (231) in a meta-analysis of 8 RCTs.
A legume-rich diet reduced HbA1c (–0.3%; 95% CI:
–1.4% to –0.1%) in an RCT in participants with
diabetes (226).
CVD. In a meta-analysis of 5 observational studies,
100 g of legumes 4 times/week is inversely
associated with CHD (RR: 0.86; 95% CI: 0.78 to 0.94)
(232). However, that study and another meta-
analysis of 8 prospective cohort studies found no
association between legumes and diabetes (207) or
stroke (232,233). A large prospective study of 2
cohorts of U.S. health professionals found a 45%
increased risk of ischemic stroke per daily serving of
legumes (RR: 1.45; 95% CI: 1.06 to 2.00) (234). This
suggests that although legumes are valuable to
reduce CHD risk, more research is required to
understand their impact on total stroke risk.
LMIC. In a cohort of Chinese men and women, soy
(the primary legume consumed in China) was
protein were less likely to develop CHD (RR:
0.25; 95% CI: 0.10 to 0.63) than were those
consuming #4.5 g/day (238).
S u m m a r y o f m a j o r p r o t e i n s o u r c e s .Reducing red
meats, especially processed meats, and increasing
fish, nuts, legumes, and possibly fermented dairy
products are likely beneficial. Sustainability issues
discussed in this paper must also be addressed spe-
cifically in relation to meat, fish, and dairy foods
(12,34,239–241).
FRUITS AND VEGETABLES. C V D r i s k f a c t o r s .In the
DASH RCT, higher intake of fruits and vegetables,
either as part of a typical Western diet or the DASH
eating plan, reduced blood pressure, TC, LDL-C, and
HDL-C without affecting triglycerides (242). A meta-
analysis of 3 prospective cohorts (3,415 cases) found
high adherence to the DASH eating reduced T2DM
risk by 27% (243). A strong evidence base from
observational studies indicates that high consump-
tion of vegetables and fruits reduces CHD and
stroke (196).
C V D i n H I C a n d L M I C .Large global studies and
systematic reviews of prospective cohorts generally
support a protective role of fruits and vegetables
against CVD (244–246). In the global INTERSTROKE
study (3,000 stroke cases and 3,000 control cases),
compared with fewer than 1 serving per day, 1
serving of fruit was protective against stroke (OR:
0.61; 95% CI: 0.50 to 0.73), but the benefits were
not clear with higher consumption of up to 3 serv-
ings/day of vegetables was not (OR: 0.91; 95% CI:
0.75 to 1.10) (244). A meta-analysis of 20 prospec-
tive cohort studies (16,981 stroke events) found that
fruit and vegetable consumption was associated
with decreased stroke risk (RR: 0.79; 95% CI: 0.75 to
0.84 for highest vs. lowest categories), as were
fruits (RR: 0.77; 95% CI: 0.71 to 0.84) and vegeta-
bles (RR: 0.86; 95% CI: 0.79 to 0.93) separately
(245). In unpublished INTERHEART study data a
Anand et al. J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5
Diet, Cardiovascular Disease, and the Food System O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4
1600
Overall summary. Increased refined grains, starches,
and added sugar (i.e., carbohydrates of lower quality)
have paralleled the rise in obesity and T2DM. Collec-
tively, the data support emphasizing low-GI whole
grains, legumes, and nuts, fruits, and vegetables and
minimizing high-GI refined grains and foods with
added sugars, including SSBs (Table 1).
DIETARY SODIUM. Sodium is an essential nutrient
required for normal physiological function (249–251).
Increasing sodium intake well beyond physiological
requirements increases blood pressure (241–243) and
CVD mortality (95–97). In LMIC sodium sources
include table salt and salt additives and spices;
whereas processed foods are the primary source in
HIC. Sodium consumption has declined slightly in
LMIC as refrigeration has replaced salted-preserved
foods. Short-term RCTs have reported reductions
in blood pressure with reduced sodium intake
to <1.5 g/day. Population recommendations for low
sodium intake (252–254) (<2.0 g/day) have been ach-
ieved in short-term feeding clinical trials (254), but not
sustained in longer-term clinical trials (>6 months)
(255–257). No RCTs have determined whether low so-
dium intake reduces CVD events or deaths compared
with moderate intake (249). Meta-analyses of CVD
event trials did not report a significant reduction in
CVD with lower sodium intake, but the included trials
were underpowered to detect moderate risk re-
ductions (258). Prospective cohort studies suggest a
J-shaped association between sodium intake and CVD
events, consistent across methods of sodium estima-
tion (259–265). In a recent Cochrane Review (266) of 23
epidemiological studies (n ¼ 274,683), the lowest
risk of CVD events and deaths occurs at an intake be-
tween 2.7 and 5.0 g/day. PURE study findings (263)
are consistent with this evidence, with sodium
excretion both >6 g/day and <3 g/day being associated
with higher mortality and CVD events compared to
4.00 to 5.99 g/day, despite an overall positive associ-
ation between sodium excretion and blood pressure
the use of homemade or unsafe alcohol products
(e.g., industrial or medical) (271). In the PURE study,
31% of participants identified as current drinkers,
with considerable variation across income regions
(13% to 80%). In all regions, men were more likely to
be current drinkers than were women (272).
C V D r i s k f a c t o r s .In a meta-analysis of randomized
controlled intervention studies of 2 to 8 weeks’
duration (273), moderate alcohol consumption (up to
1 drink or 15 g/day in women; or up to 2 drinks or
30 g/day in men) compared with no alcohol: raised
HDL-C, Apo-A1, and adiponectin, and reduced LDL-C
and fibrinogen. Total cholesterol, triglycerides, and
lipoprotein (a) were not significantly affected. Results
stratified by beverage type (wine/beer/spirits) were
similar to the pooled analyses. The changes in lipid
and hemostatic risk factors align with lower cardio-
vascular risk.
C V D .The EPIC (European Prospective Investigation
on Cancer and Nutrition) study monitored 380,395
participants for 13 years (4,187 CVD deaths) (274).
Female never-drinkers were at increased risk of CVD
death (RR: 1.31;95% CI: 1.13 to 1.53)compared with
moderate drinkers (0.1 to 4.9 g/day); but the associ-
ation was not significant for male never-drinkers (RR:
1.20; 95% CI: 0.89 to 1.62). In a dose-response meta-
analysis of 24 prospective cohort studies (275), the
association of drinking with CHD was J-shaped:
nondrinkers were at slightly increased risk; in men
the greatest protection was at 31 g/day with a trend
for increased risk beginning at 63 g/day; for women,
the greatest protection was at 11 g/day with a trend
for increased risk beginning at 14 g/day. In a meta-
analysis of 27 prospective studies of alcohol and
stroke, no association was found between light or
moderate alcohol use and stroke, but heavy alcohol
use (>45 g/day) was shown to increase total stroke
risk (RR: 1.20; 95% CI: 1.01 to 1.43), particularly
hemorrhagic stroke (RR: 1.29 ; 95% CI: 0.98 to 1.71)
(275). Patterns of alcohol consumption may be a
J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5 Anand et al.
O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4 Diet, Cardiovascular Disease, and the Food System
1601
and added sugar (i.e., carbohydrates of lower quality)
have paralleled the rise in obesity and T2DM. Collec-
tively, the data support emphasizing low-GI whole
grains, legumes, and nuts, fruits, and vegetables and
minimizing high-GI refined grains and foods with
added sugars, including SSBs (Table 1).
DIETARY SODIUM. Sodium is an essential nutrient
required for normal physiological function (249–251).
Increasing sodium intake well beyond physiological
requirements increases blood pressure (241–243) and
CVD mortality (95–97). In LMIC sodium sources
include table salt and salt additives and spices;
whereas processed foods are the primary source in
HIC. Sodium consumption has declined slightly in
LMIC as refrigeration has replaced salted-preserved
foods. Short-term RCTs have reported reductions
in blood pressure with reduced sodium intake
to <1.5 g/day. Population recommendations for low
sodium intake (252–254) (<2.0 g/day) have been ach-
ieved in short-term feeding clinical trials (254), but not
sustained in longer-term clinical trials (>6 months)
(255–257). No RCTs have determined whether low so-
dium intake reduces CVD events or deaths compared
with moderate intake (249). Meta-analyses of CVD
event trials did not report a significant reduction in
CVD with lower sodium intake, but the included trials
were underpowered to detect moderate risk re-
ductions (258). Prospective cohort studies suggest a
J-shaped association between sodium intake and CVD
events, consistent across methods of sodium estima-
tion (259–265). In a recent Cochrane Review (266) of 23
epidemiological studies (n ¼ 274,683), the lowest
risk of CVD events and deaths occurs at an intake be-
tween 2.7 and 5.0 g/day. PURE study findings (263)
are consistent with this evidence, with sodium
excretion both >6 g/day and <3 g/day being associated
with higher mortality and CVD events compared to
4.00 to 5.99 g/day, despite an overall positive associ-
ation between sodium excretion and blood pressure
the use of homemade or unsafe alcohol products
(e.g., industrial or medical) (271). In the PURE study,
31% of participants identified as current drinkers,
with considerable variation across income regions
(13% to 80%). In all regions, men were more likely to
be current drinkers than were women (272).
C V D r i s k f a c t o r s .In a meta-analysis of randomized
controlled intervention studies of 2 to 8 weeks’
duration (273), moderate alcohol consumption (up to
1 drink or 15 g/day in women; or up to 2 drinks or
30 g/day in men) compared with no alcohol: raised
HDL-C, Apo-A1, and adiponectin, and reduced LDL-C
and fibrinogen. Total cholesterol, triglycerides, and
lipoprotein (a) were not significantly affected. Results
stratified by beverage type (wine/beer/spirits) were
similar to the pooled analyses. The changes in lipid
and hemostatic risk factors align with lower cardio-
vascular risk.
C V D .The EPIC (European Prospective Investigation
on Cancer and Nutrition) study monitored 380,395
participants for 13 years (4,187 CVD deaths) (274).
Female never-drinkers were at increased risk of CVD
death (RR: 1.31;95% CI: 1.13 to 1.53)compared with
moderate drinkers (0.1 to 4.9 g/day); but the associ-
ation was not significant for male never-drinkers (RR:
1.20; 95% CI: 0.89 to 1.62). In a dose-response meta-
analysis of 24 prospective cohort studies (275), the
association of drinking with CHD was J-shaped:
nondrinkers were at slightly increased risk; in men
the greatest protection was at 31 g/day with a trend
for increased risk beginning at 63 g/day; for women,
the greatest protection was at 11 g/day with a trend
for increased risk beginning at 14 g/day. In a meta-
analysis of 27 prospective studies of alcohol and
stroke, no association was found between light or
moderate alcohol use and stroke, but heavy alcohol
use (>45 g/day) was shown to increase total stroke
risk (RR: 1.20; 95% CI: 1.01 to 1.43), particularly
hemorrhagic stroke (RR: 1.29 ; 95% CI: 0.98 to 1.71)
(275). Patterns of alcohol consumption may be a
J A C C V O L . 6 6 , N O . 1 4 ,2 0 1 5 Anand et al.
O C T O B E R 6 ,2 0 1 5 : 1 5 9 0 – 6 1 4 Diet, Cardiovascular Disease, and the Food System
1601
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 25
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.