BIOH12008: Disease Awareness Pamphlet on Pseudomembranous Colitis
VerifiedAdded on 2023/06/08
|2
|868
|83
Report
AI Summary
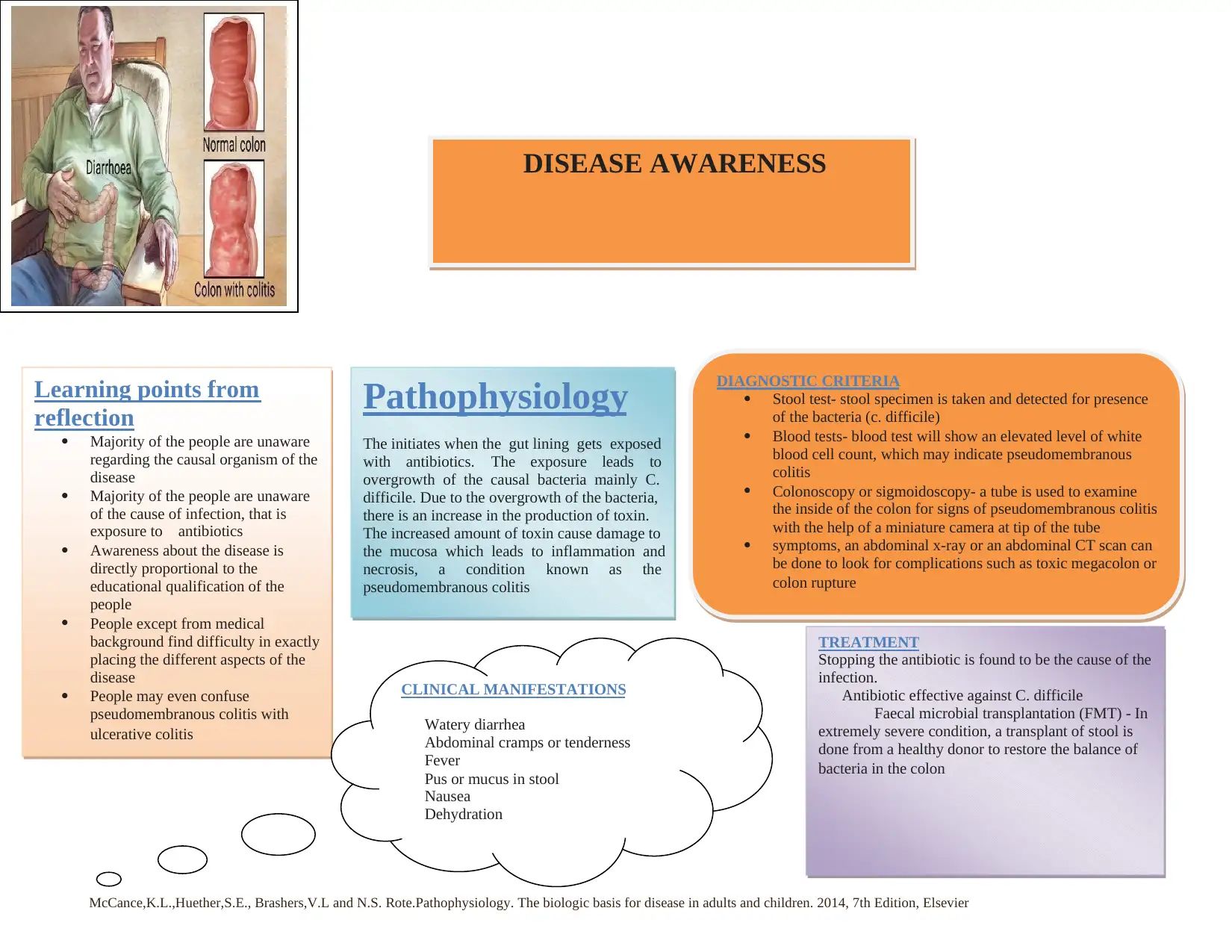
This document presents a disease awareness pamphlet focused on pseudomembranous colitis, along with a summary of interviews conducted to inform its design. The pamphlet aims to educate the public about the disease, its causes (primarily Clostridium difficile overgrowth due to antibiotic exposure), pathophysiology involving toxin production and mucosal damage, clinical manifestations such as watery diarrhea and abdominal cramps, diagnostic criteria including stool tests and colonoscopy, and treatment options like stopping the causative antibiotic and fecal microbial transplantation. The reflection highlights common misconceptions and knowledge gaps among the public regarding the disease, emphasizing the importance of targeted education and awareness initiatives. The assessment also includes interview sheets capturing public perceptions and feedback on the pamphlet's draft version, guiding improvements in clarity and design. The references used for pamphlet creation are McCance et al Pathophysiology (2014) and VanMeter, K.C., Hubert, R.J. Gould's Pathophysiology for the Health Professions (2014).
1 out of 2






![[object Object]](/_next/static/media/star-bottom.7253800d.svg)