Disease Pathophysiology and Ultrasound: Case Studies and Analysis
VerifiedAdded on 2020/03/23
|20
|4909
|80
Report
AI Summary
This report provides a comprehensive overview of the use of ultrasonography in the diagnosis of various medical conditions. It focuses on three specific cases: pancreatitis, endometriomas, and epididymitis. For each condition, the report is divided into two parts: Part A details the pathophysiology of the disease, including the underlying mechanisms and risk factors, while Part B describes the sonographic features observed using ultrasound imaging. The report explains the benefits of ultrasound as a cost-effective, non-invasive, and efficient method for early diagnosis. It covers both acute and chronic pancreatitis, outlining the changes in pancreatic structure and the appearance of fluid collections. For endometriomas, the report discusses the pathophysiology of endometrial lesion development and the associated sonographic appearances. Lastly, it examines epididymitis, detailing its pathophysiology and sonographic features. The report concludes by highlighting the importance of ultrasound in modern medical imaging for effective diagnosis.

Running head: DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
Name of the Student
Name of the University
Author Note
DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
Executive Summary
In the modern world medical imaging techniques play a very important role in the early
diagnosis of diseases. These are non-invasive techniques which do not cause any harm to the
human body. Ultrasonography is one such technique which involves the use of high
frequency sound waves in order to visualize the presence of abnormalities in tissues and
organs associated with a particular medical condition. This report describes the benefits of
Ultrasonography in the diagnosis of pancreatitis, endometriomas and epididymitis. The Part
A of each medical condition describes the pathophysiology of the disease and Part B
describes the sonographic features associated with each of these diseases. Thus it can be
concluded that Ultrasonography is a cost effective, efficient and non-invasive method for
diagnosis of critical medical conditions.
Executive Summary
In the modern world medical imaging techniques play a very important role in the early
diagnosis of diseases. These are non-invasive techniques which do not cause any harm to the
human body. Ultrasonography is one such technique which involves the use of high
frequency sound waves in order to visualize the presence of abnormalities in tissues and
organs associated with a particular medical condition. This report describes the benefits of
Ultrasonography in the diagnosis of pancreatitis, endometriomas and epididymitis. The Part
A of each medical condition describes the pathophysiology of the disease and Part B
describes the sonographic features associated with each of these diseases. Thus it can be
concluded that Ultrasonography is a cost effective, efficient and non-invasive method for
diagnosis of critical medical conditions.
2DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
Table of Contents
1. Introduction......................................................................................................................3
2. Case 1.................................................................................................................................4
2.1. Pancreatitis..................................................................................................................4
2.1.a. Part A........................................................................................................................4
2.1.b. Part B........................................................................................................................6
3. Case 2.................................................................................................................................8
3.1. Endometriomas............................................................................................................8
3.1.a. Part A........................................................................................................................8
3.1.b. Part B......................................................................................................................10
4. Case 3...............................................................................................................................12
4.1. Epididymitis..............................................................................................................12
4.1.a. Part A......................................................................................................................12
4.1.b. Part B......................................................................................................................13
5. Conclusion.......................................................................................................................15
6. Reference List.................................................................................................................17
Table of Contents
1. Introduction......................................................................................................................3
2. Case 1.................................................................................................................................4
2.1. Pancreatitis..................................................................................................................4
2.1.a. Part A........................................................................................................................4
2.1.b. Part B........................................................................................................................6
3. Case 2.................................................................................................................................8
3.1. Endometriomas............................................................................................................8
3.1.a. Part A........................................................................................................................8
3.1.b. Part B......................................................................................................................10
4. Case 3...............................................................................................................................12
4.1. Epididymitis..............................................................................................................12
4.1.a. Part A......................................................................................................................12
4.1.b. Part B......................................................................................................................13
5. Conclusion.......................................................................................................................15
6. Reference List.................................................................................................................17
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
1. Introduction
Medical imaging involves the use of various technologies for monitoring, diagnosis
and treatment of medical conditions. There are different types of medical imaging techniques
like the computed tomography (CT), medical resonance imaging, ultrasound, X-ray, positron
emission tomography (PET), PET-CT, among others. The features of a medical condition like
a tumor mass or cyst can be visualized using these techniques. X-ray imaging was the first
diagnostic tool to be discovered followed by the invention of ultrasound imaging (Haidekker
2013).
This report focuses on the use of ultrasound technology for the detection of various
medical conditions like pancreatitis, endometriomas and epididymitis. Ultrasound imaging
makes use of the properties of high frequency sound waves to image abnormalities in organs
during a diseased condition. Ultrasound has frequency ranging between 20 Hz to 20 kHz.
This technology involves the use of sound waves which travel through the body and are
reflected at the tissue interfaces. The time taken for the waves to return determines the depth
of the surface. The ultrasound waves travel from the transducer to the different tissues or
organs and then gets reflected back to the transducer as echoes. The transducer converts these
echoes to electrical impulses which are finally transformed into a computerized ultrasound
image. It has a low instrumentation cost and it is easy to use which essentially adds to its
popularity in diagnosis of critical medical conditions (Wilhjelm et al. 2013).
This report focuses on 3 different cases of medical conditions, their pathophysiology
and their surface appearances in ultrasound imaging. The 3 different medical conditions
described in this study are Pancreatitis, Endometriomas/Endometriosis and Epididymitis.
These diseases are caused by various environmental factors as well as bacterial infections.
1. Introduction
Medical imaging involves the use of various technologies for monitoring, diagnosis
and treatment of medical conditions. There are different types of medical imaging techniques
like the computed tomography (CT), medical resonance imaging, ultrasound, X-ray, positron
emission tomography (PET), PET-CT, among others. The features of a medical condition like
a tumor mass or cyst can be visualized using these techniques. X-ray imaging was the first
diagnostic tool to be discovered followed by the invention of ultrasound imaging (Haidekker
2013).
This report focuses on the use of ultrasound technology for the detection of various
medical conditions like pancreatitis, endometriomas and epididymitis. Ultrasound imaging
makes use of the properties of high frequency sound waves to image abnormalities in organs
during a diseased condition. Ultrasound has frequency ranging between 20 Hz to 20 kHz.
This technology involves the use of sound waves which travel through the body and are
reflected at the tissue interfaces. The time taken for the waves to return determines the depth
of the surface. The ultrasound waves travel from the transducer to the different tissues or
organs and then gets reflected back to the transducer as echoes. The transducer converts these
echoes to electrical impulses which are finally transformed into a computerized ultrasound
image. It has a low instrumentation cost and it is easy to use which essentially adds to its
popularity in diagnosis of critical medical conditions (Wilhjelm et al. 2013).
This report focuses on 3 different cases of medical conditions, their pathophysiology
and their surface appearances in ultrasound imaging. The 3 different medical conditions
described in this study are Pancreatitis, Endometriomas/Endometriosis and Epididymitis.
These diseases are caused by various environmental factors as well as bacterial infections.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
Part A of each medical condition describes its pathophysiology while part B describes the
sonographic appearances associated with the disease.
2. Case 1
2.1. Pancreatitis
2.1.a. Part A
Pancreatitis can be divided into acute and chronic Pancreatitis. Acute Pancreatitis
(AP) is characterized by the presence of necrotic areas, interstitial edema, pancreatic tissue
hemorrhage and fluid collections. Chronic Pancreatitis (CP) is characterized by the presence
of ductal calcifications, dilations, obstructions, pseudocysts and lesions (Sankaran et al.
2015).
AP involves the loss of compartmentalization both at the intracellular and
extracellular levels. Obstruction of the outflow of bile salts and their subsequent toxic effects
leads to destruction of the pancreatic ducts. Alcohol consumption causes disruption of the
plasma membrane functions, balance between protease inhibitors and proteolytic enzymes,
resulting in cell destruction, enzyme activation and autodigestion (Sah, Garg and Saluja
2012). Interstitial edema and inflammation are the major features of pancreatitis. Further
progression of the disease is characterized by the polymorphonuclear granulocyte
accumulation in pancreatic areas and release of enzymes from leukocytes. Various risk
factors lead to the development of CP. These include various environmental factors like
nicotine and alcohol consumption, nutritional factors, among others (Yadav and Lowenfels
2013). Other factors include hereditary mutations, autoimmune factors and obstruction of
ducts. CP involves fibrosis of the glandular tissue. The secretory parenchymal cells undergo
various processes like apoptosis or necrosis, duct obstruction and inflammation. Pancreatic
Part A of each medical condition describes its pathophysiology while part B describes the
sonographic appearances associated with the disease.
2. Case 1
2.1. Pancreatitis
2.1.a. Part A
Pancreatitis can be divided into acute and chronic Pancreatitis. Acute Pancreatitis
(AP) is characterized by the presence of necrotic areas, interstitial edema, pancreatic tissue
hemorrhage and fluid collections. Chronic Pancreatitis (CP) is characterized by the presence
of ductal calcifications, dilations, obstructions, pseudocysts and lesions (Sankaran et al.
2015).
AP involves the loss of compartmentalization both at the intracellular and
extracellular levels. Obstruction of the outflow of bile salts and their subsequent toxic effects
leads to destruction of the pancreatic ducts. Alcohol consumption causes disruption of the
plasma membrane functions, balance between protease inhibitors and proteolytic enzymes,
resulting in cell destruction, enzyme activation and autodigestion (Sah, Garg and Saluja
2012). Interstitial edema and inflammation are the major features of pancreatitis. Further
progression of the disease is characterized by the polymorphonuclear granulocyte
accumulation in pancreatic areas and release of enzymes from leukocytes. Various risk
factors lead to the development of CP. These include various environmental factors like
nicotine and alcohol consumption, nutritional factors, among others (Yadav and Lowenfels
2013). Other factors include hereditary mutations, autoimmune factors and obstruction of
ducts. CP involves fibrosis of the glandular tissue. The secretory parenchymal cells undergo
various processes like apoptosis or necrosis, duct obstruction and inflammation. Pancreatic
5DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
stellate cells (PSCs) are responsible for fibrosis, which results in extracellular matrix (ECM)
formation in the various interstitial spaces (Apte et al. 2013). ECM formation also occurs in
the spaces that lack acinar cells or consist of injured duct cells. The various morphological
changes associated with CP involve loss of lobular morphology and structure of pancreas. It
also involves malformation of large ducts, abnormalities in the composition and arrangement
of the islets. These are irreversible processes and the abnormal morphological changes leads
to impairment of the endocrine and exocrine functions. This ultimately results in malnutrition
and even diabetes.
Pancreatitis arises due to injury to the duct or acinar cells and cells of the interstitial
mesenchyma. Following injury, the activation step involves expression of α smooth muscle
actins, proliferation and secretion of fibrillar collagens by the PSCs. Injury to various tissues
or cells of the pancreas lead to cellular apotosis or necrosis and cytokine release from
macrophages or already existing mesenchymal cells. The damaged pancreatic cells undergo
phagocytosis by the macrophages resulting in cytokine release, subsequently resulting in
activation and eventual proliferation of PCSs surrounding the injury site. This results in
transformation of PCSs to myofibroblasts.
However, another alternative hypothesis describes a direct role of the etiological
factor in Pancreatitis development. The factors like alcohol, nicotine directly activates the
existing fibroblast cells. Subsequently myofibroblasts are produced and the ECM replaces the
alcohol or nicotine infiltrates. This results in architectural and functional damage to the
pancreatic cells. It involves enhanced production of matrix metalloproteinases (MMP) 3 and
9 by the myofibroblasts. These metalloproteinases are regulated by the tumor growth factor
cytokines resulting in increased pancreatic fibrogenesis. Apart from alcohol and nicotine
consumption, hereditary factors also play an important role in the development of
stellate cells (PSCs) are responsible for fibrosis, which results in extracellular matrix (ECM)
formation in the various interstitial spaces (Apte et al. 2013). ECM formation also occurs in
the spaces that lack acinar cells or consist of injured duct cells. The various morphological
changes associated with CP involve loss of lobular morphology and structure of pancreas. It
also involves malformation of large ducts, abnormalities in the composition and arrangement
of the islets. These are irreversible processes and the abnormal morphological changes leads
to impairment of the endocrine and exocrine functions. This ultimately results in malnutrition
and even diabetes.
Pancreatitis arises due to injury to the duct or acinar cells and cells of the interstitial
mesenchyma. Following injury, the activation step involves expression of α smooth muscle
actins, proliferation and secretion of fibrillar collagens by the PSCs. Injury to various tissues
or cells of the pancreas lead to cellular apotosis or necrosis and cytokine release from
macrophages or already existing mesenchymal cells. The damaged pancreatic cells undergo
phagocytosis by the macrophages resulting in cytokine release, subsequently resulting in
activation and eventual proliferation of PCSs surrounding the injury site. This results in
transformation of PCSs to myofibroblasts.
However, another alternative hypothesis describes a direct role of the etiological
factor in Pancreatitis development. The factors like alcohol, nicotine directly activates the
existing fibroblast cells. Subsequently myofibroblasts are produced and the ECM replaces the
alcohol or nicotine infiltrates. This results in architectural and functional damage to the
pancreatic cells. It involves enhanced production of matrix metalloproteinases (MMP) 3 and
9 by the myofibroblasts. These metalloproteinases are regulated by the tumor growth factor
cytokines resulting in increased pancreatic fibrogenesis. Apart from alcohol and nicotine
consumption, hereditary factors also play an important role in the development of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
Pancreatitis. Mutation in the SPINK1 gene, which encodes the pancreatic secretory trypsin
inhibitor also results in the development of hereditary CP (Brock et al. 2013).
2.1.b. Part B
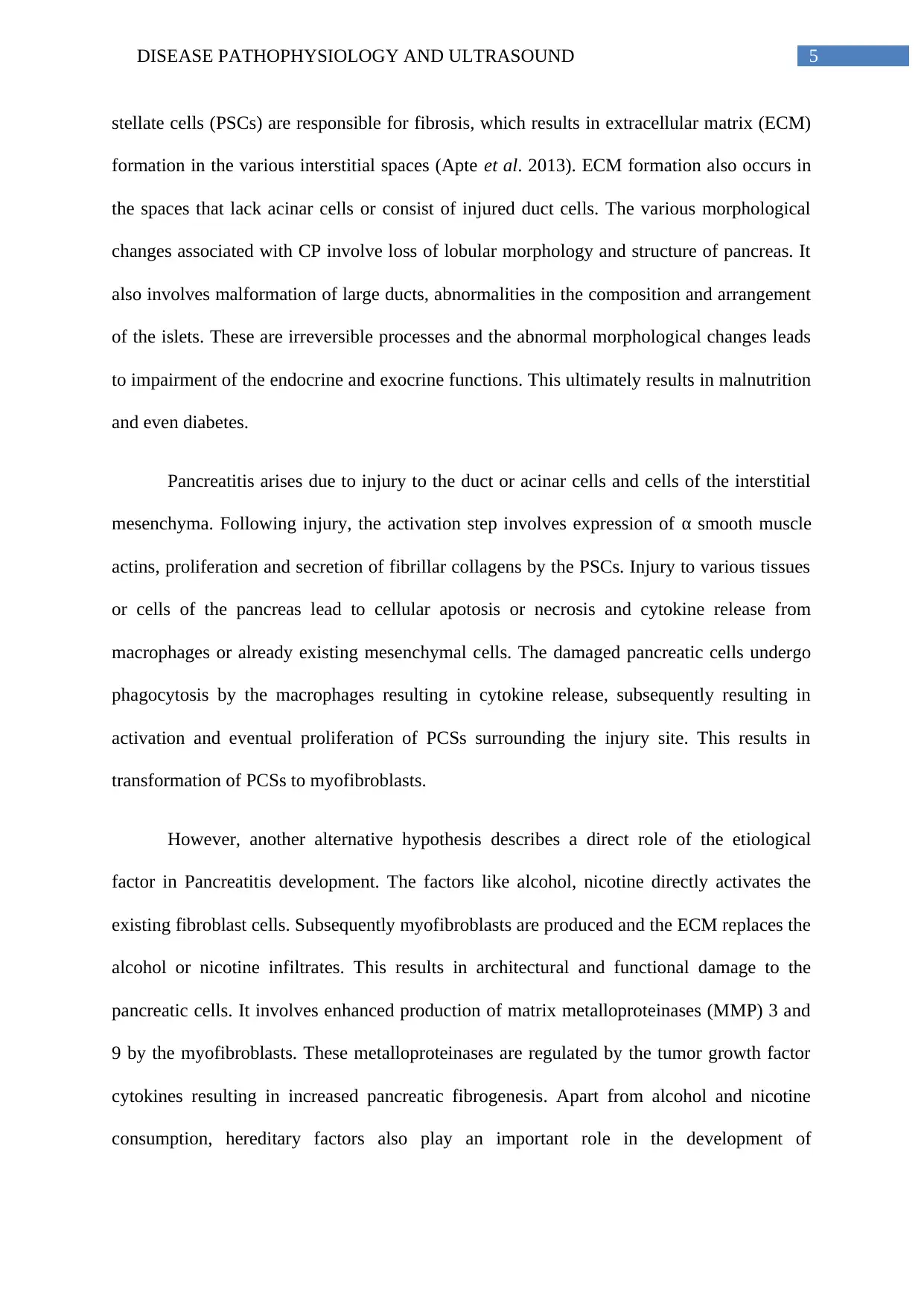
The various diagnostic techniques provided by ultrasonography include the grayscale
B mode, Doppler imaging and tissue harmonic imaging. Grayscale B mode helps to
determine the pancreatic structure, size, volume, border, echogenicity, surrounding regions
and ducts. Doppler imaging helps to determine the outline of the pancreas, and the structure
of the surrounding vessels. Small calcifications present in the pancreas, which are
characteristics of CP, is visualized as twinkling artifacts using Doppler imaging technique. It
can also help to distinguish between necrosis (without blood supply) and inflammation (with
blood supply) associated with Pancreatitis. Tissue harmonic imaging helps to distinguish
between solid and liquid necrotic masses (Dimcevski et al. 2013).
Figure 1: Sonographic appearance in
pancreatitis
(Source: Dimcevski et al. 2013, p. 7247)
Ultrasound generally determines the severe changes in pancreatic structure and size in
AP. A typical horseshoe shape, homogenous and echogenic structure constitutes the
Pancreatitis. Mutation in the SPINK1 gene, which encodes the pancreatic secretory trypsin
inhibitor also results in the development of hereditary CP (Brock et al. 2013).
2.1.b. Part B
The various diagnostic techniques provided by ultrasonography include the grayscale
B mode, Doppler imaging and tissue harmonic imaging. Grayscale B mode helps to
determine the pancreatic structure, size, volume, border, echogenicity, surrounding regions
and ducts. Doppler imaging helps to determine the outline of the pancreas, and the structure
of the surrounding vessels. Small calcifications present in the pancreas, which are
characteristics of CP, is visualized as twinkling artifacts using Doppler imaging technique. It
can also help to distinguish between necrosis (without blood supply) and inflammation (with
blood supply) associated with Pancreatitis. Tissue harmonic imaging helps to distinguish
between solid and liquid necrotic masses (Dimcevski et al. 2013).
Figure 1: Sonographic appearance in
pancreatitis
(Source: Dimcevski et al. 2013, p. 7247)
Ultrasound generally determines the severe changes in pancreatic structure and size in
AP. A typical horseshoe shape, homogenous and echogenic structure constitutes the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

7DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
sonographic appearances of a normal pancreas. The diameter of a normal pancreas does not
exceed 20-22mm. A normal pancreas is also characterized by the absence of fluid structures,
fluid collections and lymph node like structures. AP is associated by the volume increase,
changes in the structure of the parenchyma and loss or significant decrease of echogenicity.
Increased size of the pancreas results in significant displacement of the organs in the
abdomen like the stomach and the colon, among others. A diameter of greater than 24mm is
generally a sign of Pancreatitis. Other sonographic appearances involve the appearance of a
bulge in the anterior position of the abdominal wall, necrotic or oedemic areas (due to non-
homogenicity of the pancreas). There are 2 types of oedema: incipient and massive. In
incipient oedema, echogenicity is normal while the pancreas is hypoechogenic in massive
oedema.
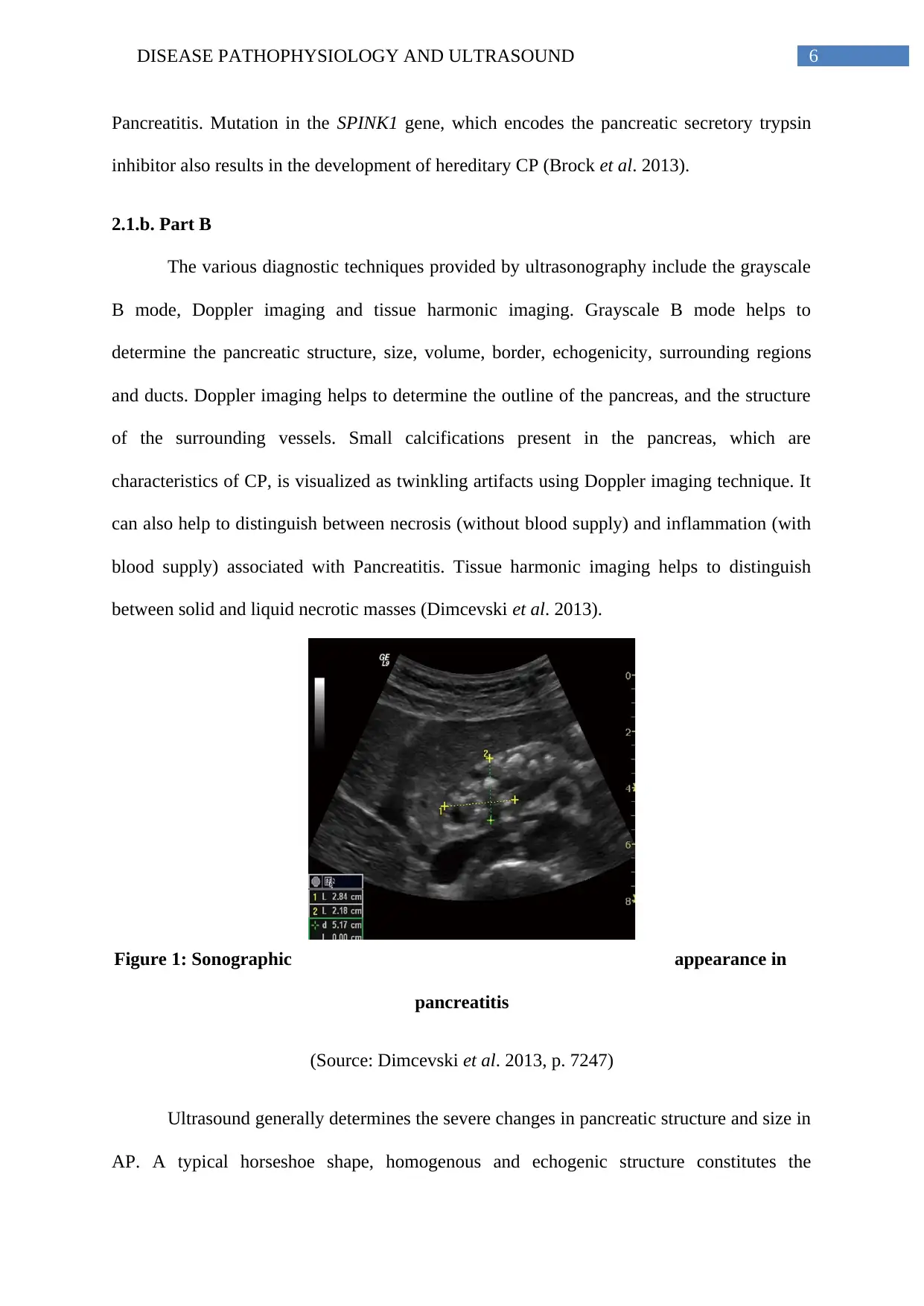
Figure 2: Acute interstitial pancreatitis with presence of oedema
(Source: Banks et al. 2013, pp 102-111)
Accumulation of fluid in acute necrotic Pancreatitis is visualized by endoscopic
ultrasound. The fluid accumulations occurring during AP can be classified into Walled off
pancreatic necrosis (WOPN) and acute pseudocysts. WOPN occurs four weeks after the
development of AP and consists of masses of encapsulated necrotic materials with fluid
accumulations. Acute pseudocysts arise during interstitial pancreatitis characterized by the
sonographic appearances of a normal pancreas. The diameter of a normal pancreas does not
exceed 20-22mm. A normal pancreas is also characterized by the absence of fluid structures,
fluid collections and lymph node like structures. AP is associated by the volume increase,
changes in the structure of the parenchyma and loss or significant decrease of echogenicity.
Increased size of the pancreas results in significant displacement of the organs in the
abdomen like the stomach and the colon, among others. A diameter of greater than 24mm is
generally a sign of Pancreatitis. Other sonographic appearances involve the appearance of a
bulge in the anterior position of the abdominal wall, necrotic or oedemic areas (due to non-
homogenicity of the pancreas). There are 2 types of oedema: incipient and massive. In
incipient oedema, echogenicity is normal while the pancreas is hypoechogenic in massive
oedema.
Figure 2: Acute interstitial pancreatitis with presence of oedema
(Source: Banks et al. 2013, pp 102-111)
Accumulation of fluid in acute necrotic Pancreatitis is visualized by endoscopic
ultrasound. The fluid accumulations occurring during AP can be classified into Walled off
pancreatic necrosis (WOPN) and acute pseudocysts. WOPN occurs four weeks after the
development of AP and consists of masses of encapsulated necrotic materials with fluid
accumulations. Acute pseudocysts arise during interstitial pancreatitis characterized by the
8DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
presence of oedema. Acute pseudocysts contain negligible amounts of solid necrotic
materials and consist primarily of fluid contents (Ramia et al. 2012).
3. Case 2
3.1. Endometriomas
3.1.a. Part A
Endometriosis is a proinflammatory disease, chronic and dependant on the estrogen
hormone. It affects women who have reached their reproductive age. It is a gynecological
condition involved in aberrant growth of endometrium like tissues outside of the uterus. It is
generally asymptomatic but symptoms can also arise like dysmennorhea, severe pelvic pain,
irregular and severe bleeding, pain during urination and defecation, nausea, vomiting,
dyspareunia, fertility reduction, among others (Vercellini et al. 2014). Endometriosis is
generally found in the pelvic regions like the ovaries, fallopian tubes, uterus and its
associated ligaments, cul-de-sac, as well as in the ureters, rectovaginal septum, bowels,
urinary bladders, appendix, among others. The pathophysiology of endometriosis involves
endometrial lesion development, increase in estradiol production and progesterone resistance,
vasculogenesis, angiogenesis and immune dysfunction (Rocha, Reis and Taylor 2013).
The endometrial lesion development is described by 3 different hypotheses. The
Sampson theory proposes the dissemination of endometrial tissue into the peritoneal cavity
during menstruation and subsequently is implanted on either the pelvic organs or the
peritoneal tissue. The theory of coelomic metaplasia describes that various environmental,
hormonal or infectious stimuli induces metaplasia of visceral and abdominal peritoneal cells
leading to endometriosis. The theory of embryonic rest describes that estrogen stimulus
enables migration of the Mullerian duct during embryonic development. The cells remaining
presence of oedema. Acute pseudocysts contain negligible amounts of solid necrotic
materials and consist primarily of fluid contents (Ramia et al. 2012).
3. Case 2
3.1. Endometriomas
3.1.a. Part A
Endometriosis is a proinflammatory disease, chronic and dependant on the estrogen
hormone. It affects women who have reached their reproductive age. It is a gynecological
condition involved in aberrant growth of endometrium like tissues outside of the uterus. It is
generally asymptomatic but symptoms can also arise like dysmennorhea, severe pelvic pain,
irregular and severe bleeding, pain during urination and defecation, nausea, vomiting,
dyspareunia, fertility reduction, among others (Vercellini et al. 2014). Endometriosis is
generally found in the pelvic regions like the ovaries, fallopian tubes, uterus and its
associated ligaments, cul-de-sac, as well as in the ureters, rectovaginal septum, bowels,
urinary bladders, appendix, among others. The pathophysiology of endometriosis involves
endometrial lesion development, increase in estradiol production and progesterone resistance,
vasculogenesis, angiogenesis and immune dysfunction (Rocha, Reis and Taylor 2013).
The endometrial lesion development is described by 3 different hypotheses. The
Sampson theory proposes the dissemination of endometrial tissue into the peritoneal cavity
during menstruation and subsequently is implanted on either the pelvic organs or the
peritoneal tissue. The theory of coelomic metaplasia describes that various environmental,
hormonal or infectious stimuli induces metaplasia of visceral and abdominal peritoneal cells
leading to endometriosis. The theory of embryonic rest describes that estrogen stimulus
enables migration of the Mullerian duct during embryonic development. The cells remaining
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
after the migration gives rise to endometrial lesions. The recent stem cell theory is supported
by several experimental data. It proposes the participation of endometrial and bone-marrow
stem cells in the development of endometriosis (Gargett et al. 2014).
The attachment of the lesion depends on the stromal cells of the endometrium; while
the glandular cells are involved in the growth and subsequent spread of the lesion. Women
showing overexpression of collagen, fibronectin, laminin of the peritoneal cavity have an
increased risk of developing endometriosis. After attachment, the extracellular matrix (ECM)
is degraded, enabling invasion of the endometrial cells, development of endometriotic foci
leading to lesion progress. Endometriosis is characterized by increased expression of MMPs
like MMP-2, 3, 7 and 9 (Shan et al. 2013). Moreover, the expression of the urokinase-type
plasminogen activator (uPA) is also found to be increased in endometriosis. After
menstruation, endometrium reconstruction is brought about by Estradiol (active form of
estrogen). The endometriotic lesions produce estradiol in high amounts, thereby helping in
implantation in peritoneal cavity.
Angiogenesis involves the development of new blood vessels from pre-existing ones,
while vascularization involves the de novo production of blood vessels during
embryogenesis. Lesion development in endometriosis depends on the development of new
blood vessels for supply of oxygen and nutrients. Increased expression of vascular
endothelial growth factor is responsible for angiogenesis during endometriosis.
Endometriosis also involves the process of vascularization for establishment of vascular
network.
Functional loss or alterations of immune mediators produced by cells of both innate
and adaptive immunity are also involved in endometriosis. These cells include macrophages,
neutrophils, dendritic cells, natural killer cells, T and B lymphocytes. Cytokines and
after the migration gives rise to endometrial lesions. The recent stem cell theory is supported
by several experimental data. It proposes the participation of endometrial and bone-marrow
stem cells in the development of endometriosis (Gargett et al. 2014).
The attachment of the lesion depends on the stromal cells of the endometrium; while
the glandular cells are involved in the growth and subsequent spread of the lesion. Women
showing overexpression of collagen, fibronectin, laminin of the peritoneal cavity have an
increased risk of developing endometriosis. After attachment, the extracellular matrix (ECM)
is degraded, enabling invasion of the endometrial cells, development of endometriotic foci
leading to lesion progress. Endometriosis is characterized by increased expression of MMPs
like MMP-2, 3, 7 and 9 (Shan et al. 2013). Moreover, the expression of the urokinase-type
plasminogen activator (uPA) is also found to be increased in endometriosis. After
menstruation, endometrium reconstruction is brought about by Estradiol (active form of
estrogen). The endometriotic lesions produce estradiol in high amounts, thereby helping in
implantation in peritoneal cavity.
Angiogenesis involves the development of new blood vessels from pre-existing ones,
while vascularization involves the de novo production of blood vessels during
embryogenesis. Lesion development in endometriosis depends on the development of new
blood vessels for supply of oxygen and nutrients. Increased expression of vascular
endothelial growth factor is responsible for angiogenesis during endometriosis.
Endometriosis also involves the process of vascularization for establishment of vascular
network.
Functional loss or alterations of immune mediators produced by cells of both innate
and adaptive immunity are also involved in endometriosis. These cells include macrophages,
neutrophils, dendritic cells, natural killer cells, T and B lymphocytes. Cytokines and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
chemokines like tumor necrosis factor α, Interleukin 6, 8, 10 and monocyte chemoattractant
protein 1 are involved in the establishment and subsequent survival of lesions in
endometriosis (Ahn et al. 2015).
3.1.b. Part B
The endometrium undergoes changes during the menstrual cycle. During the
menstrual phase, it appears as thin, bright and echogenic. A trilaminar appearance, outer
echogenic layer, middle hypoechoic layer, and inner echogenic layer characterize the
proliferative phase. A thick and uniform echogenic layer characterizes the secretory phase.
The functional layer appears oedematous, while the basal layer remains isoechoic. In
premenopausal women, the endometrium varies in thickness. During menstruation it is 2-
4mm, during early proliferative phase it is 5-7mm, in late proliferative phase it is 11mm in
thickness while in the secretory phase it is 7-16mm. In post menopausal women the
endometrial thickness is generally less than 5mm.
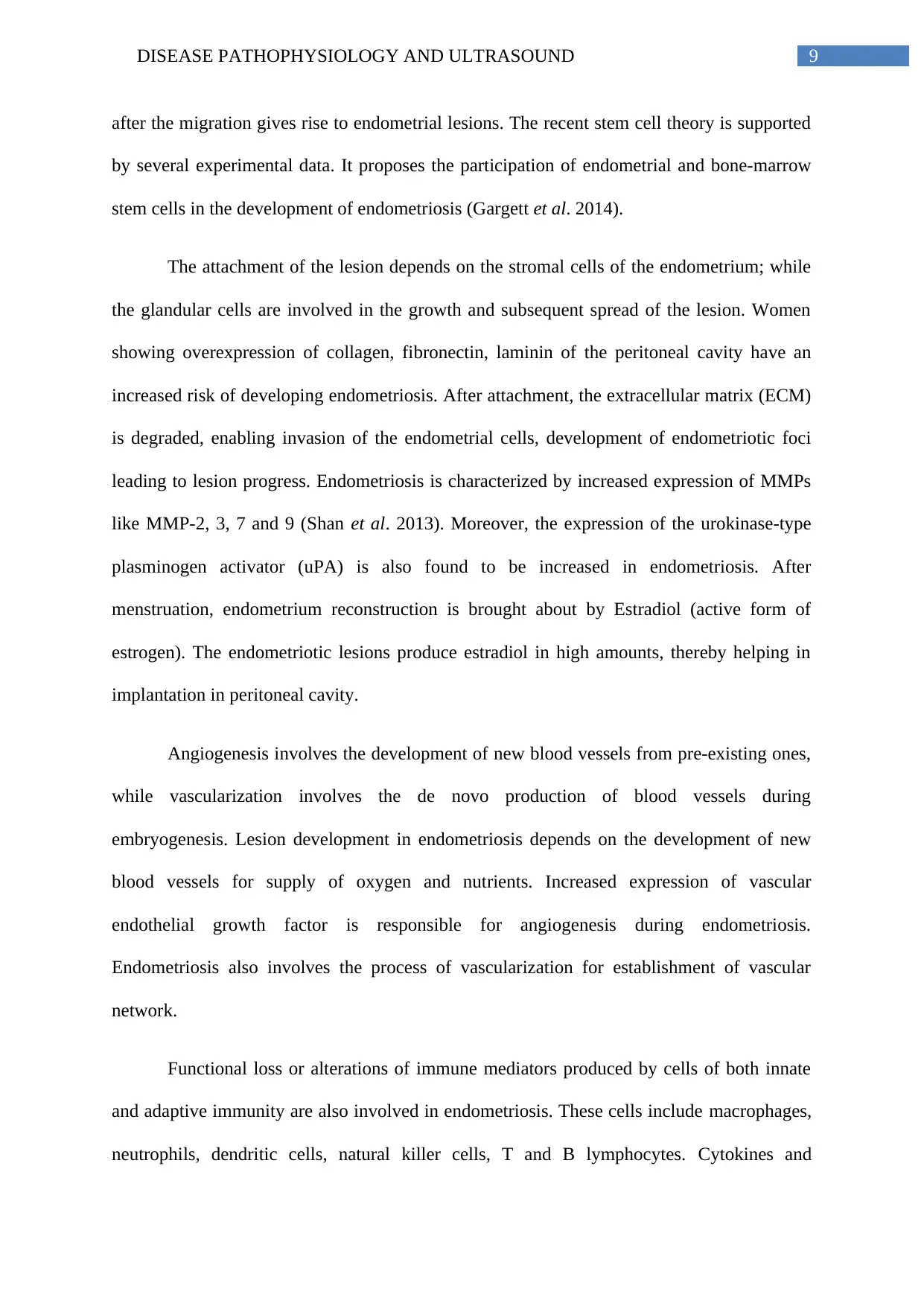
Transvaginal sonography is the standard in diagnosing endometriosis, which involves
imaging the ovaries and uterus. However, patients suffering from severe pelvic pain are
subjected to sonography of additional regions like the bowel wall, cul-de-sac and the
rectovaginal septum. This helps in the detection of rectosigmoid endometriosis (Said and
Azzam 2014).
chemokines like tumor necrosis factor α, Interleukin 6, 8, 10 and monocyte chemoattractant
protein 1 are involved in the establishment and subsequent survival of lesions in
endometriosis (Ahn et al. 2015).
3.1.b. Part B
The endometrium undergoes changes during the menstrual cycle. During the
menstrual phase, it appears as thin, bright and echogenic. A trilaminar appearance, outer
echogenic layer, middle hypoechoic layer, and inner echogenic layer characterize the
proliferative phase. A thick and uniform echogenic layer characterizes the secretory phase.
The functional layer appears oedematous, while the basal layer remains isoechoic. In
premenopausal women, the endometrium varies in thickness. During menstruation it is 2-
4mm, during early proliferative phase it is 5-7mm, in late proliferative phase it is 11mm in
thickness while in the secretory phase it is 7-16mm. In post menopausal women the
endometrial thickness is generally less than 5mm.
Transvaginal sonography is the standard in diagnosing endometriosis, which involves
imaging the ovaries and uterus. However, patients suffering from severe pelvic pain are
subjected to sonography of additional regions like the bowel wall, cul-de-sac and the
rectovaginal septum. This helps in the detection of rectosigmoid endometriosis (Said and
Azzam 2014).
11DISEASE PATHOPHYSIOLOGY AND ULTRASOUND
Figure 3: Transvaginal sonography to detect endometriomas
(Source: Said and Azzam 2014, pp.197-207)
Endometriosis is characterized by the presence of implants, which can be either
superficial or deep. Ultrasound is poor in detecting peritoneal implants but can better detect
endometriomas. Endometriomas appear as homogenous and focal lesions. They appear
unilocular but in some cases may be multilocular with presence of septa. Multiple
endometriomas may appear with presence of mural nodules, which are hyperechoic. Color
Doppler imaging shows absence of blood flow.
Early diagnosis of endometriosis is a major challenge but women showing possible
symptoms should be subjected to imaging techniques. Endometriomas also called chocolate
cysts appear on the ovary and constitute the most common feature associated with
sonography of patients suffering from endometriosis. Sonographic appearances of
endometriosis involve the appearance of solid nodules with poorly defined and blurred
borders. Ultrasonographic scan in Endometriosis reveals the presence of a cystic mass with
diffused and low echo levels. However, Endometriomas may sometimes appear as a solid or
cystic mass (either simple or complex). Endometriomas are visualized as vascularized,
rounded, papillary projections having smooth contours with the presence of cyst locules and
cyst fluid showing low echogenicity levels.
Figure 3: Transvaginal sonography to detect endometriomas
(Source: Said and Azzam 2014, pp.197-207)
Endometriosis is characterized by the presence of implants, which can be either
superficial or deep. Ultrasound is poor in detecting peritoneal implants but can better detect
endometriomas. Endometriomas appear as homogenous and focal lesions. They appear
unilocular but in some cases may be multilocular with presence of septa. Multiple
endometriomas may appear with presence of mural nodules, which are hyperechoic. Color
Doppler imaging shows absence of blood flow.
Early diagnosis of endometriosis is a major challenge but women showing possible
symptoms should be subjected to imaging techniques. Endometriomas also called chocolate
cysts appear on the ovary and constitute the most common feature associated with
sonography of patients suffering from endometriosis. Sonographic appearances of
endometriosis involve the appearance of solid nodules with poorly defined and blurred
borders. Ultrasonographic scan in Endometriosis reveals the presence of a cystic mass with
diffused and low echo levels. However, Endometriomas may sometimes appear as a solid or
cystic mass (either simple or complex). Endometriomas are visualized as vascularized,
rounded, papillary projections having smooth contours with the presence of cyst locules and
cyst fluid showing low echogenicity levels.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 20
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
