Systematic Review: Impact of Topical Treatments on Arterial Leg Ulcers
VerifiedAdded on 2022/04/18
|36
|10428
|52
Report
AI Summary
This report presents a systematic review investigating the impact of topical treatments and wound dressings on the healing of arterial leg ulcers. The study employed a methodology involving a comprehensive search of databases like Science Direct, Cochrane Library, Google Scholar, and PubMed to identify relevant scholarly articles published between 2000 and 2021, with an exception for a 1991 clinical trial. The review aimed to assess the effects of various topical agents (ointments and creams) and wound dressings on healing rates and patient outcomes. The findings highlight a scarcity of conclusive data on the effectiveness of specific topical medications or dressings in influencing the overall recovery of arterial ulcerations, thereby emphasizing the need for further research to establish evidence-based treatment strategies. The review also includes an overview of the etiology, pathophysiology, and current clinical practices for managing arterial ulcers, discussing assessment methods, and providing a literature review of the topic. The study underlines the significance of arterial ulcer management, which includes improving blood flow and managing the wound, in order to prevent complications like infection and amputation.

PUBLIC
Abstract
Background
According to estimates, up to 1% of persons in high-income economies will get a leg ulceration
at a certain point in life. A preponderance of ulcerations is caused by circulatory abnormalities;
venous ulceration (which account for about 70% of lesions) and arterial ulcers (which account
for the remaining 30% of ulcers) are caused by insufficient blood flow to the legs (around 22
percent of ulcers). Therapies for arterial leg ulcers focuses on improving arterial blood flow, such
as by removing arterial obstructions (either pharmaceutically or surgically). Such arterial
ulceration may recover if the vascular circulation is reinstated and wound management
procedures are followed. Dressings and topical treatments are an important aspect of wound
management for arterial ulcers, however there are a lot of them, and it's unknown how they affect
ulcer treatment.
Objectives
To investigate as to if topical treatments and wound dressings have an effect on the recovery of
artery ulceration. And assess the rates of healing and the consequences. A comparative of wound
dressings and topical treatments accessible.
Research Objectives
Is there an impact of using Topical agents (ointments and creams) and wound dressings used to
treat arterial leg ulcers healing?
Methodology
Science Direct, Cochrane Library, Google Scholar and PubMed were used to conduct a
systematic review on pertinent scholarly resources on descriptive study. Six (6) investigation
articles involving cross-sectional and descriptive methodologies was methodically chosen and
assessed through diverse resources. Thereby, publications on arterial leg ulcers topical agent and
dressing wound management were retrieved from 2000 to 2021 were included, whilst also
resources older than 2009 were excluded.
Abstract
Background
According to estimates, up to 1% of persons in high-income economies will get a leg ulceration
at a certain point in life. A preponderance of ulcerations is caused by circulatory abnormalities;
venous ulceration (which account for about 70% of lesions) and arterial ulcers (which account
for the remaining 30% of ulcers) are caused by insufficient blood flow to the legs (around 22
percent of ulcers). Therapies for arterial leg ulcers focuses on improving arterial blood flow, such
as by removing arterial obstructions (either pharmaceutically or surgically). Such arterial
ulceration may recover if the vascular circulation is reinstated and wound management
procedures are followed. Dressings and topical treatments are an important aspect of wound
management for arterial ulcers, however there are a lot of them, and it's unknown how they affect
ulcer treatment.
Objectives
To investigate as to if topical treatments and wound dressings have an effect on the recovery of
artery ulceration. And assess the rates of healing and the consequences. A comparative of wound
dressings and topical treatments accessible.
Research Objectives
Is there an impact of using Topical agents (ointments and creams) and wound dressings used to
treat arterial leg ulcers healing?
Methodology
Science Direct, Cochrane Library, Google Scholar and PubMed were used to conduct a
systematic review on pertinent scholarly resources on descriptive study. Six (6) investigation
articles involving cross-sectional and descriptive methodologies was methodically chosen and
assessed through diverse resources. Thereby, publications on arterial leg ulcers topical agent and
dressing wound management were retrieved from 2000 to 2021 were included, whilst also
resources older than 2009 were excluded.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PUBLIC
Nevertheless, a clinical trial from 1991 was chosen as it was in line with the inclusive criteria,
and some other publications which did not rely upon that research problem were excluded. Size
of sample was not limited hence individuals represented with arterial leg ulcer off all ages and
sex were included in the study.
Results
When the ketanserin subgroup was contrasted to the control cohort, lesion recovery was shown
to be faster in the ketanserin cluster. Another experiment stated that no participants encountered
adverse effects (complications) during follow-up (six weeks, poor confidence information). Yet
another study examined topical administration of blood derived concentrated growth factor
(CGF) versus conventional dressings (polyurethane films or foaming), which were either
administered weekly over 6 weeks by 61 people having non-healing ulceration.
Conclusion
The fraction of information available to assess whether the topical medication or dressing used
influences overall recovery of arterial ulcerations is inadequate.
Key words: Arterial leg ulcer, Wound healing, topical agents, dressings, creams, ointments
Nevertheless, a clinical trial from 1991 was chosen as it was in line with the inclusive criteria,
and some other publications which did not rely upon that research problem were excluded. Size
of sample was not limited hence individuals represented with arterial leg ulcer off all ages and
sex were included in the study.
Results
When the ketanserin subgroup was contrasted to the control cohort, lesion recovery was shown
to be faster in the ketanserin cluster. Another experiment stated that no participants encountered
adverse effects (complications) during follow-up (six weeks, poor confidence information). Yet
another study examined topical administration of blood derived concentrated growth factor
(CGF) versus conventional dressings (polyurethane films or foaming), which were either
administered weekly over 6 weeks by 61 people having non-healing ulceration.
Conclusion
The fraction of information available to assess whether the topical medication or dressing used
influences overall recovery of arterial ulcerations is inadequate.
Key words: Arterial leg ulcer, Wound healing, topical agents, dressings, creams, ointments
PUBLIC
Chapter One
1.0 Introduction
Nursing centers upon promoting the healthcare initiatives which every patient life or pursues.
Within such perspective, management strives to avoid illnesses & encourage disease readaptation
processes across the life cycle, as well as to fulfill the minimum human demands and achieve
maximum autonomy in everyday tasks. As a result, nursing care assists individuals in managing
community health resources while also emphasizing the need of playing a central function
throughout the unit (Fonseca et al., 2012; As a consequence of the growth of human longevity
and also the associated frequency of chronic conditions including such leg ulcers, healthcare
patients' demands are becoming more exacting and complicated (Van, Grypdonck and Defloor,
2009). The management of chronic wounds represent a serious societal concern due to its scope,
intricacy, & expense. Most leg ulcers are believed to affect 8–10 million people globally,
whereas pressure sores affect 7–8 million (Fonseca et al., 2015; Singh et al., 2003).
Limb ulcers are a frequent chronic ailment which can irritating and has a detrimental effect on
individual 's wellbeing. According to a comprehensive study, 1.1 percent to 0.12 percent of
overall adult populace is affected by lower-leg ulceration (Graham 2003). Venous insufficiency
(impaired blood circulation in the venous), vascular illness, and diabetes are the most common
causes of ulceration. Despite venous illness causes overall preponderance of leg ulcers, a
considerable proportion of persons with ulcerations (approximately 22 percent) have artery
insuFiciency. Heterogeneous aetiologies account for over 15% of leg ulcers, such as those
caused by arterial and venous illness or diabetic combined arterial pathology (Fonseca et al.,
2015; Broderick, Pagnamenta, and Forster, 2020). A restriction of blood flow to the skin causes
arterial leg ulcers. A constriction of the arteries in the legs could perhaps represent the reason
(atherosclerosis). It's critical to distinguish amongst arterial and venous leg ulcers because
compression treatments, which is the basis of management for venous leg ulcers, might cause
skin necrosis (or possibly amputation) when used on arterial leg ulceration (O'Meara 2012 ;
Fonseca et al., 2015)
Chapter One
1.0 Introduction
Nursing centers upon promoting the healthcare initiatives which every patient life or pursues.
Within such perspective, management strives to avoid illnesses & encourage disease readaptation
processes across the life cycle, as well as to fulfill the minimum human demands and achieve
maximum autonomy in everyday tasks. As a result, nursing care assists individuals in managing
community health resources while also emphasizing the need of playing a central function
throughout the unit (Fonseca et al., 2012; As a consequence of the growth of human longevity
and also the associated frequency of chronic conditions including such leg ulcers, healthcare
patients' demands are becoming more exacting and complicated (Van, Grypdonck and Defloor,
2009). The management of chronic wounds represent a serious societal concern due to its scope,
intricacy, & expense. Most leg ulcers are believed to affect 8–10 million people globally,
whereas pressure sores affect 7–8 million (Fonseca et al., 2015; Singh et al., 2003).
Limb ulcers are a frequent chronic ailment which can irritating and has a detrimental effect on
individual 's wellbeing. According to a comprehensive study, 1.1 percent to 0.12 percent of
overall adult populace is affected by lower-leg ulceration (Graham 2003). Venous insufficiency
(impaired blood circulation in the venous), vascular illness, and diabetes are the most common
causes of ulceration. Despite venous illness causes overall preponderance of leg ulcers, a
considerable proportion of persons with ulcerations (approximately 22 percent) have artery
insuFiciency. Heterogeneous aetiologies account for over 15% of leg ulcers, such as those
caused by arterial and venous illness or diabetic combined arterial pathology (Fonseca et al.,
2015; Broderick, Pagnamenta, and Forster, 2020). A restriction of blood flow to the skin causes
arterial leg ulcers. A constriction of the arteries in the legs could perhaps represent the reason
(atherosclerosis). It's critical to distinguish amongst arterial and venous leg ulcers because
compression treatments, which is the basis of management for venous leg ulcers, might cause
skin necrosis (or possibly amputation) when used on arterial leg ulceration (O'Meara 2012 ;
Fonseca et al., 2015)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PUBLIC
A medical history is used to diagnose arterial insufficiency, also known as peripheral arterial
disease (PAD). The more frequent complication is discomfort, that might emerge while moving
and exercising. Periodic claudication develops when cramping discomfort with in leg comes
following activity but disappears once the limb is rested. Such complaints may worsen to the
point where the individual is in discomfort particularly while they are at repose (Fonseca et al.,
2015; Broderick, Pagnamenta, and Forster, 2020).
Diagnostics are frequently performed to determine the existence or lack of vascular disease in
order to measure what significant blood circulation is present in the leg. The ankle brachial index
is usually the initial test (ABPI, ABI). If the ABI ratio is less than 0.7, compression intervention
is not recommended, and the patient would be directed to a vascular expert that would request
supplementary testing, including either duplex ultrasonography and arteriography (Grey 2006).
The ABI criterion is normally around 0.6 and 0.7, while there is significant heterogeneity in the
literary works. Diagnosing PAD in persons having diabetes is difficult since neuropathic
conditions may hide symptoms and non-compressible arteries could provide fallacious ABI
results (Brownrigg 2016).
The cornerstone of treating arterial insufficiency would be to enhance overall blood flow, hence
surgical to circumvent or eliminate the obstruction is sometimes necessary. Owing to individual
desire, age, or overall health, and according to diffused distal arterial disease, in which the
arteries to be repaired are extremely tiny, that might not be achievable for certain individuals
(Grey, Harding and Enoch, 2006; Hedayati et al., 2015). Wound healing, exercising to enhance
blood circulation to the leg, pharmacological treatments, and physical therapy including such
hyperbaric oxygen are all non-surgical possibilities (Grey, Harding and Enoch, 2006; Hedayati et
al., 2015).
There are indications suggesting managing chronic wounds like leg ulcers puts a significant
psychological strain upon health professionals, particularly whenever the lesions do not recover
(Morgan and Moffatt, 2008; Posnett et al, 2009). Regrettably, such cost has rarely been
adequately investigated, with the exception of a universal acknowledgement of leg ulcer
treatment have an effect on individual patients, health care systems, and society as a whole.
There was also conclusive evidence indicating leg ulcer therapy has shifted from patient-centered
A medical history is used to diagnose arterial insufficiency, also known as peripheral arterial
disease (PAD). The more frequent complication is discomfort, that might emerge while moving
and exercising. Periodic claudication develops when cramping discomfort with in leg comes
following activity but disappears once the limb is rested. Such complaints may worsen to the
point where the individual is in discomfort particularly while they are at repose (Fonseca et al.,
2015; Broderick, Pagnamenta, and Forster, 2020).
Diagnostics are frequently performed to determine the existence or lack of vascular disease in
order to measure what significant blood circulation is present in the leg. The ankle brachial index
is usually the initial test (ABPI, ABI). If the ABI ratio is less than 0.7, compression intervention
is not recommended, and the patient would be directed to a vascular expert that would request
supplementary testing, including either duplex ultrasonography and arteriography (Grey 2006).
The ABI criterion is normally around 0.6 and 0.7, while there is significant heterogeneity in the
literary works. Diagnosing PAD in persons having diabetes is difficult since neuropathic
conditions may hide symptoms and non-compressible arteries could provide fallacious ABI
results (Brownrigg 2016).
The cornerstone of treating arterial insufficiency would be to enhance overall blood flow, hence
surgical to circumvent or eliminate the obstruction is sometimes necessary. Owing to individual
desire, age, or overall health, and according to diffused distal arterial disease, in which the
arteries to be repaired are extremely tiny, that might not be achievable for certain individuals
(Grey, Harding and Enoch, 2006; Hedayati et al., 2015). Wound healing, exercising to enhance
blood circulation to the leg, pharmacological treatments, and physical therapy including such
hyperbaric oxygen are all non-surgical possibilities (Grey, Harding and Enoch, 2006; Hedayati et
al., 2015).
There are indications suggesting managing chronic wounds like leg ulcers puts a significant
psychological strain upon health professionals, particularly whenever the lesions do not recover
(Morgan and Moffatt, 2008; Posnett et al, 2009). Regrettably, such cost has rarely been
adequately investigated, with the exception of a universal acknowledgement of leg ulcer
treatment have an effect on individual patients, health care systems, and society as a whole.
There was also conclusive evidence indicating leg ulcer therapy has shifted from patient-centered
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PUBLIC
to task-oriented (Persoon et al, 2004; Parkinson, 2006; Morgan and Moffatt, 2008).
Notwithstanding, wound management throughout general and leg ulcer treatment in particular
remain among of the highest prevalent referrals to community nursing (Rubi et al, 2003;
Eleftheriadou et al, 2019).
1.1 Study Justification
With the increasing burden of Leg ulcer management among healthcare individuals worldwide,
contemporary treatment methods are available in wound management, there is little to poor
literature available in the scientific community, despite the fact that a variety of dressings and
topical treatments are available, there is presently no evidence supporting their impact on the
pace of recovery in arterial ulcers.
1.2 Aim
The main objective of this research is to systematically review on comparison of dressing and
topic agents in the wound healing of arterial leg ulcer.
1.3 Research Objectives
1. Critical evaluation of existing literature on the available dressing and topical agents used in
wound healing
2. To evaluate topical treatments and wound healing in terms of recovery speeds and patient-
centered consequences.
3. Appraisal of the effective dressing and topical agents used in wound healing of arterial leg
ulcer
1.4 Research question
Is there an impact of using Topical agents (ointments and creams) and wound dressings used to
treat arterial leg ulcers healing?
to task-oriented (Persoon et al, 2004; Parkinson, 2006; Morgan and Moffatt, 2008).
Notwithstanding, wound management throughout general and leg ulcer treatment in particular
remain among of the highest prevalent referrals to community nursing (Rubi et al, 2003;
Eleftheriadou et al, 2019).
1.1 Study Justification
With the increasing burden of Leg ulcer management among healthcare individuals worldwide,
contemporary treatment methods are available in wound management, there is little to poor
literature available in the scientific community, despite the fact that a variety of dressings and
topical treatments are available, there is presently no evidence supporting their impact on the
pace of recovery in arterial ulcers.
1.2 Aim
The main objective of this research is to systematically review on comparison of dressing and
topic agents in the wound healing of arterial leg ulcer.
1.3 Research Objectives
1. Critical evaluation of existing literature on the available dressing and topical agents used in
wound healing
2. To evaluate topical treatments and wound healing in terms of recovery speeds and patient-
centered consequences.
3. Appraisal of the effective dressing and topical agents used in wound healing of arterial leg
ulcer
1.4 Research question
Is there an impact of using Topical agents (ointments and creams) and wound dressings used to
treat arterial leg ulcers healing?

PUBLIC
1.5 Significance of the study
Atherosclerotic ulceration with in lower limbs may lead to major consequences such as
infections, gangrene, resection, and fatality. It is critical to minimize arterial ulcers as well as
thus address its fundamental circulation flow deficit as soon as possible. Improved circulation,
cautious wound debridement, and pain management are all nursing aims. To prevent an ulcer
from infection, manage exudate, improve autolytic debridement, minimize pain, and promote a
supportive therapeutic milieu, employ occlusive treatments. Dressings and topical treatments are
an important aspect of wound management for arterial ulcers, however there are a lot of them,
and it's unknown how they affect healing process. With the paucity of literature emphasizing the
best therapeutic management of atrial leg ulcers, this systematic review would analyze existing
dressing and topical agents utilized in managing wounds. On the contrary novel clinical trials
accessing efficacy and usage of topical agents and dressing would also be evaluated which could
provide key insights in drawing conclusive suggestions on the effective management strategies
that could be employed in the clinical setting.
1.5 Significance of the study
Atherosclerotic ulceration with in lower limbs may lead to major consequences such as
infections, gangrene, resection, and fatality. It is critical to minimize arterial ulcers as well as
thus address its fundamental circulation flow deficit as soon as possible. Improved circulation,
cautious wound debridement, and pain management are all nursing aims. To prevent an ulcer
from infection, manage exudate, improve autolytic debridement, minimize pain, and promote a
supportive therapeutic milieu, employ occlusive treatments. Dressings and topical treatments are
an important aspect of wound management for arterial ulcers, however there are a lot of them,
and it's unknown how they affect healing process. With the paucity of literature emphasizing the
best therapeutic management of atrial leg ulcers, this systematic review would analyze existing
dressing and topical agents utilized in managing wounds. On the contrary novel clinical trials
accessing efficacy and usage of topical agents and dressing would also be evaluated which could
provide key insights in drawing conclusive suggestions on the effective management strategies
that could be employed in the clinical setting.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
PUBLIC
Chapter Two
Literature Review
1.0 Introduction
This section will offer a comprehensive overview of the aetiology, pathophysiology, and current
dressings and topical medicines used in clinical practice for arterial ulcers. There will also be a
glimpse at the prevalence of the disease, the influence of promoting health in terms of
prevention, and the consequences of poor ulcer care on prognosis. Additional evidence would be
gathered through a study of existing medical literature that takes into account current nursing
procedures. Ultimately, the existing literature on the effectiveness of currently used treatment
approaches will be thoroughly examined.
1.1 Arterial leg ulcers and pathophysiology
A decreased arterial blood flow to the lower leg causes arterial ulceration. Atheromatous diseases
of both the large and medium arteries is the most prevalent cause. Diabetes, vasculitis,
thromboangiitis, pyoderma gangrenosum, sickle cell disease and thalassaemia are some of the
other conditions that may lead to atheroma development. Concurrent hypertension causes further
harm to the vascular system by damaging overall intimal layers of the artery. Tissue hypoxic and
tissue injury come from a decline in arterial blood flow. Tissue damage and ulcer development
may be exacerbated by thrombotic and atheroembolic events (Grey, Harding, and Enoch, 2006).
Ischemia of the dermis and underlying tissues may develop from arteriolar or arterial blockage,
which could progress to ulceration. Diabetes with macrovascular or microvascular diseases,
Atherosclerosisand/or vasculitis may all cause an ischemic leg, which can contribute to ulcers
(Sarkar and Ballantyne,2001).
The pathogenesis of an ischemic leg ulcer encompasses three pathways:
Extra - mural strangling (1) Mural hypertrophy or accumulation (2) Intramural blood flow
restriction
Extramural strangulation is caused by scar and radiodermatitis, which cause fibrotic bands
surrounding the arterioles, resulting in tiny but chronic ischemic ulcers. Mural thickening or
Chapter Two
Literature Review
1.0 Introduction
This section will offer a comprehensive overview of the aetiology, pathophysiology, and current
dressings and topical medicines used in clinical practice for arterial ulcers. There will also be a
glimpse at the prevalence of the disease, the influence of promoting health in terms of
prevention, and the consequences of poor ulcer care on prognosis. Additional evidence would be
gathered through a study of existing medical literature that takes into account current nursing
procedures. Ultimately, the existing literature on the effectiveness of currently used treatment
approaches will be thoroughly examined.
1.1 Arterial leg ulcers and pathophysiology
A decreased arterial blood flow to the lower leg causes arterial ulceration. Atheromatous diseases
of both the large and medium arteries is the most prevalent cause. Diabetes, vasculitis,
thromboangiitis, pyoderma gangrenosum, sickle cell disease and thalassaemia are some of the
other conditions that may lead to atheroma development. Concurrent hypertension causes further
harm to the vascular system by damaging overall intimal layers of the artery. Tissue hypoxic and
tissue injury come from a decline in arterial blood flow. Tissue damage and ulcer development
may be exacerbated by thrombotic and atheroembolic events (Grey, Harding, and Enoch, 2006).
Ischemia of the dermis and underlying tissues may develop from arteriolar or arterial blockage,
which could progress to ulceration. Diabetes with macrovascular or microvascular diseases,
Atherosclerosisand/or vasculitis may all cause an ischemic leg, which can contribute to ulcers
(Sarkar and Ballantyne,2001).
The pathogenesis of an ischemic leg ulcer encompasses three pathways:
Extra - mural strangling (1) Mural hypertrophy or accumulation (2) Intramural blood flow
restriction
Extramural strangulation is caused by scar and radiodermatitis, which cause fibrotic bands
surrounding the arterioles, resulting in tiny but chronic ischemic ulcers. Mural thickening or
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PUBLIC
intimal plaque accretion, as in atherosclerosis, could cause a reduction in blood circulation till
atherothrombosis, embolism, or a superimposed infection can cause full blockage, culminating in
ulceration. Changes throughout blood viscosity, platelet adhesiveness, and/or fibrinogenesis, as
in vasculitis, could obstruct the small vessels, actually results in leg ulceration.
There is frequently a significant comorbidity, and the precise etiology cannot always be
pinpointed. Owing to tissues ischemia and efflux of fibrin-like components, many acute types of
vasculitis, as well as certain subacute and chronic variants, are prone to induce leg ulcers (Sarkar
and Ballantyne,2001).
1.2 Assessment methods
There is presently insufficient significant literature which indicates on validated techniques built
particularly to acquire measurements on arterial ulcers (Beaumier et Al., 2021). Originally, the
vascular circulation to the legs were assessed manually examining the patient the palpitations on
the feet. Nevertheless, because of the mediocre predictive accuracy of such an assessment
(Moffatt 1995), objective evaluations particularly ones listed hereunder are now suggested. A
health history is taken and the blood flow to the limb is assessed to provide a prognosis (Taylor
1993). Pain is the most prevalent associated grievance. This discomfort might arise during
physical activity like walking. Intermittent claudication occurs when cramping discomfort in the
leg comes after activity and disappears when the limb is rested. This may proceed to the point
where the distance necessary to cause discomfort decreases, and the patient finally reports of
discomfort even while at rest. This is known as'rest ache.' This discomfort may not be felt by
those with neuropathy, such as diabetics. To establish the existence or absence of vascular
disease, laboratory testing are often performed. Ankle brachial pressure index (ABPI) and
doppler arterial waveform analysis are two examples.
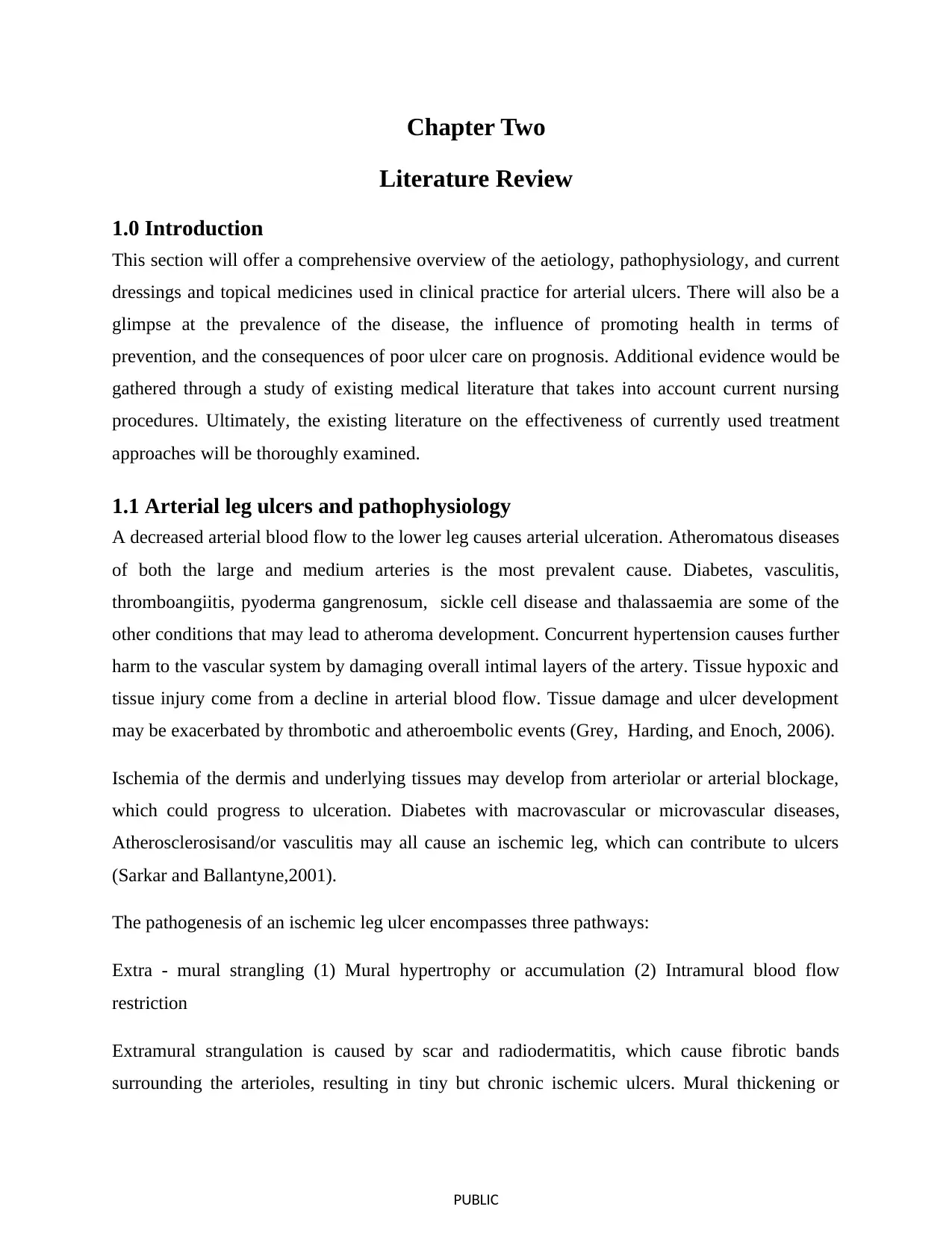
1.3 Management of Arterial leg ulcers
Limb salvage and Wound healing remain the predominant goals of therapeutic interventions.
The goals of treatment are to address the root etiology of the ulcer and promote wound healing
utilizing the most up-to-date recommendations and wound management modalities (Suman
intimal plaque accretion, as in atherosclerosis, could cause a reduction in blood circulation till
atherothrombosis, embolism, or a superimposed infection can cause full blockage, culminating in
ulceration. Changes throughout blood viscosity, platelet adhesiveness, and/or fibrinogenesis, as
in vasculitis, could obstruct the small vessels, actually results in leg ulceration.
There is frequently a significant comorbidity, and the precise etiology cannot always be
pinpointed. Owing to tissues ischemia and efflux of fibrin-like components, many acute types of
vasculitis, as well as certain subacute and chronic variants, are prone to induce leg ulcers (Sarkar
and Ballantyne,2001).
1.2 Assessment methods
There is presently insufficient significant literature which indicates on validated techniques built
particularly to acquire measurements on arterial ulcers (Beaumier et Al., 2021). Originally, the
vascular circulation to the legs were assessed manually examining the patient the palpitations on
the feet. Nevertheless, because of the mediocre predictive accuracy of such an assessment
(Moffatt 1995), objective evaluations particularly ones listed hereunder are now suggested. A
health history is taken and the blood flow to the limb is assessed to provide a prognosis (Taylor
1993). Pain is the most prevalent associated grievance. This discomfort might arise during
physical activity like walking. Intermittent claudication occurs when cramping discomfort in the
leg comes after activity and disappears when the limb is rested. This may proceed to the point
where the distance necessary to cause discomfort decreases, and the patient finally reports of
discomfort even while at rest. This is known as'rest ache.' This discomfort may not be felt by
those with neuropathy, such as diabetics. To establish the existence or absence of vascular
disease, laboratory testing are often performed. Ankle brachial pressure index (ABPI) and
doppler arterial waveform analysis are two examples.
1.3 Management of Arterial leg ulcers
Limb salvage and Wound healing remain the predominant goals of therapeutic interventions.
The goals of treatment are to address the root etiology of the ulcer and promote wound healing
utilizing the most up-to-date recommendations and wound management modalities (Suman
PUBLIC
2014). The initial stage in patient therapy is to take a complete clinical history, concentrating on
the length and extent of the ulcer as well as any concomitant lower extremity complaints.
Individuals with arterial diseases are more likely to be older and have major cardiovascular
comorbidities, thus a thorough assessment of their comorbidities and general health is critical
(Hedayati et Al., 2015).
Treatment algorithm (adapted from Valesci, 2012)
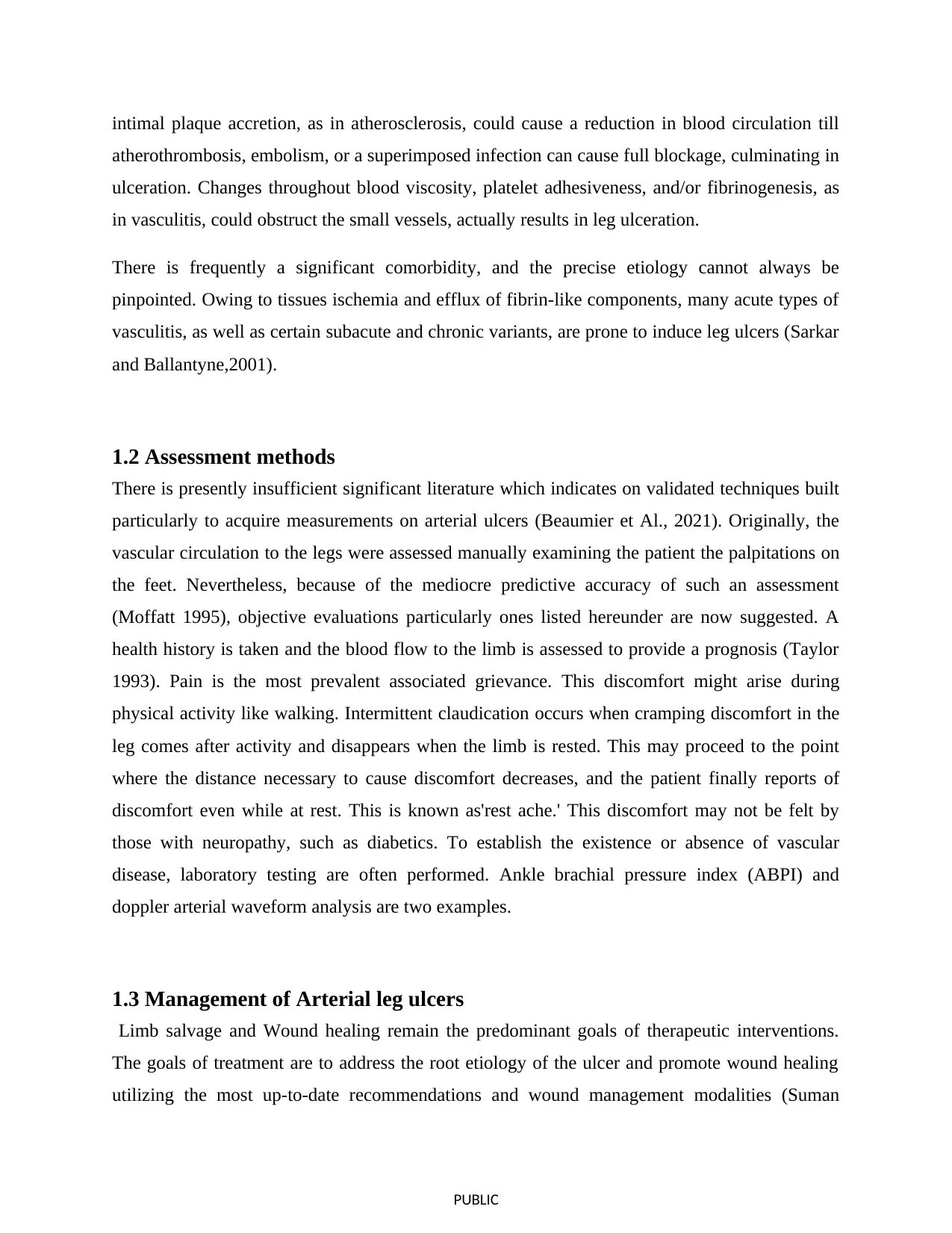
Management and treatment of arterial and venous extremities ulcers of the lower limbs requires
an integrated and multi-level strategy to ensure a satisfactory result. Ulcers should be
vascularized, devoid of necrosis and devitalized tissues, emancipate of infection, and maintained
moist to enable recovery. Optimal wound dressings drain fluid buildup while keeping the wound
moist, prevent bacterial invasion and/or propagation, remove dead zone, debride tissue
destruction, eliminate exposure of surrounding healthy tissue, and reduce discomfort during
treatment (Hedayati et Al., 2015). Various nations could utilize several methods for categorizing
dressings and topical treatments. There are also a range of topical treatments, such as cadexomer
iodine, honey, phenytoin, silver, and ketanserin, that try to modify the wound environment.
Topical antimicrobial and antibacterial treatments are often used in conjunction with dressings to
create an antimicrobial and antibacterial microenvironment (SIGN 2010). Hyperbaric oxygen,
vacuum therapy, and skin grafting are some of the other treatments for arterial ulcers (Broderick,
Pagnamenta and Forster, 2020; Forster and Pagnamenta, 2015).
2014). The initial stage in patient therapy is to take a complete clinical history, concentrating on
the length and extent of the ulcer as well as any concomitant lower extremity complaints.
Individuals with arterial diseases are more likely to be older and have major cardiovascular
comorbidities, thus a thorough assessment of their comorbidities and general health is critical
(Hedayati et Al., 2015).
Treatment algorithm (adapted from Valesci, 2012)
Management and treatment of arterial and venous extremities ulcers of the lower limbs requires
an integrated and multi-level strategy to ensure a satisfactory result. Ulcers should be
vascularized, devoid of necrosis and devitalized tissues, emancipate of infection, and maintained
moist to enable recovery. Optimal wound dressings drain fluid buildup while keeping the wound
moist, prevent bacterial invasion and/or propagation, remove dead zone, debride tissue
destruction, eliminate exposure of surrounding healthy tissue, and reduce discomfort during
treatment (Hedayati et Al., 2015). Various nations could utilize several methods for categorizing
dressings and topical treatments. There are also a range of topical treatments, such as cadexomer
iodine, honey, phenytoin, silver, and ketanserin, that try to modify the wound environment.
Topical antimicrobial and antibacterial treatments are often used in conjunction with dressings to
create an antimicrobial and antibacterial microenvironment (SIGN 2010). Hyperbaric oxygen,
vacuum therapy, and skin grafting are some of the other treatments for arterial ulcers (Broderick,
Pagnamenta and Forster, 2020; Forster and Pagnamenta, 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

PUBLIC
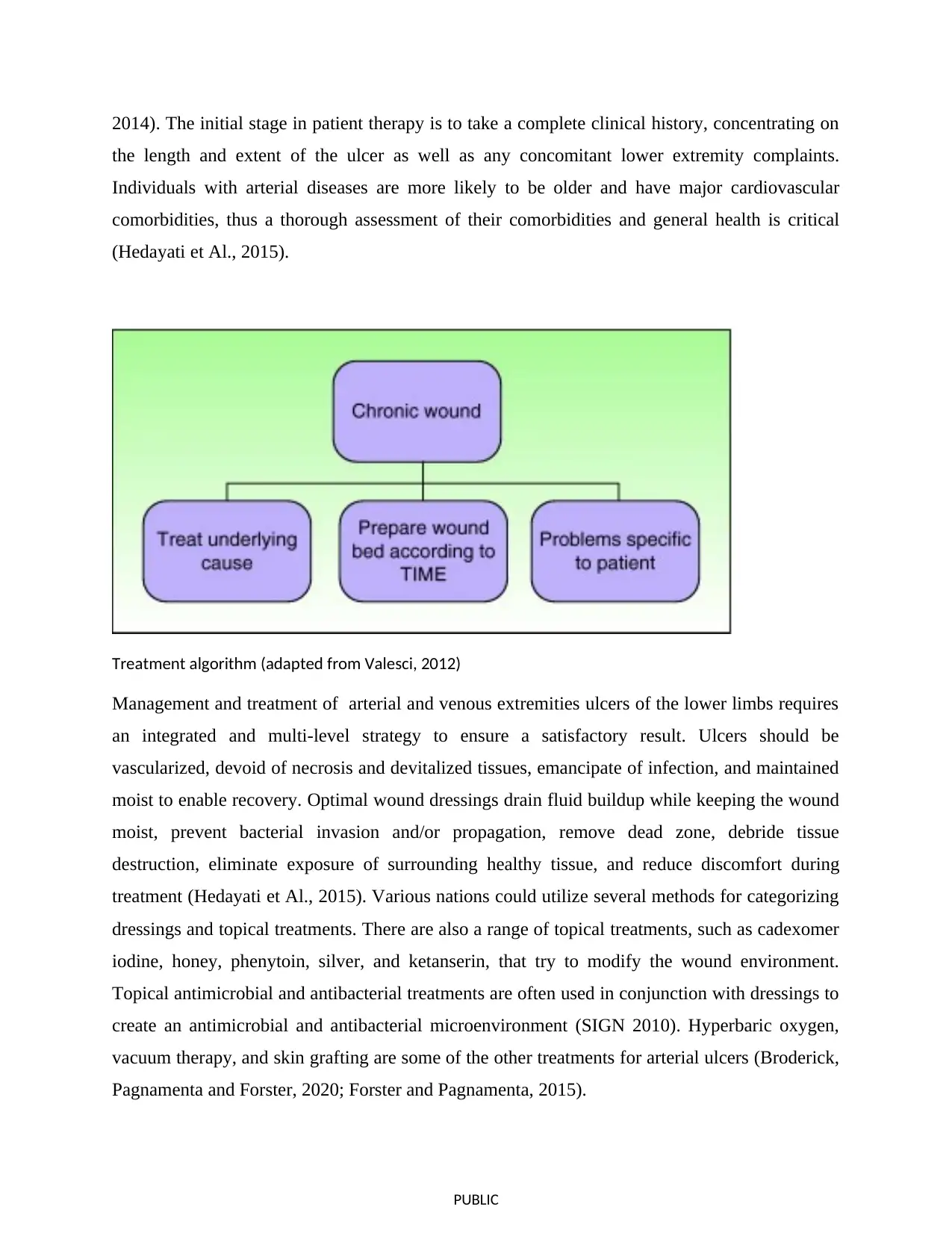
1.3.1 Dressings
The evolution of wounds dressings has progressed significantly in tandem with the increased acceptance
of wound healing philosophies. Wound coverings are now intended to encapsulate the wound and
promote wound healing (Vowden and Vowden, 2014). Because of their cheap cost and straightforward
production procedure, conventional dressings, also known as inert treatments (elastic bandage, cotton
pads, and gauze), are by far the largest extensively employed clinical dressings (Broughton et al., 2006).
Nevertheless, various drawbacks restrict their use, such as the difficulty of keeping the wound bed wet
and their proclivity for adherence with granulation tissues (Moore and Webster, 2013).
Due to its qualities that provide a humid microenvironment for healing process, advanced dressing could
be particularly viable choices (Moura et al., 2013; Heyer et al., 2013). Modern dressings have superior
biocompatibility, degradability, as well as moisture absorption as opposed to older dressings. Newer
dressings provide analgesic alleviation and ameliorate the hypoxic or anaerobic environments (Thu et
al., 2012; Hopper et al., 2012; Okuma et al., 2015). Hydrogels, hydrocolloids, foams, alginates and films
are the main often employed contemporary dressings in clinical settings.
1.3.1 Dressings
The evolution of wounds dressings has progressed significantly in tandem with the increased acceptance
of wound healing philosophies. Wound coverings are now intended to encapsulate the wound and
promote wound healing (Vowden and Vowden, 2014). Because of their cheap cost and straightforward
production procedure, conventional dressings, also known as inert treatments (elastic bandage, cotton
pads, and gauze), are by far the largest extensively employed clinical dressings (Broughton et al., 2006).
Nevertheless, various drawbacks restrict their use, such as the difficulty of keeping the wound bed wet
and their proclivity for adherence with granulation tissues (Moore and Webster, 2013).
Due to its qualities that provide a humid microenvironment for healing process, advanced dressing could
be particularly viable choices (Moura et al., 2013; Heyer et al., 2013). Modern dressings have superior
biocompatibility, degradability, as well as moisture absorption as opposed to older dressings. Newer
dressings provide analgesic alleviation and ameliorate the hypoxic or anaerobic environments (Thu et
al., 2012; Hopper et al., 2012; Okuma et al., 2015). Hydrogels, hydrocolloids, foams, alginates and films
are the main often employed contemporary dressings in clinical settings.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
PUBLIC
1.3.1.1 Hydrocolloids
A mixture of three hydrocolloids, such as sodium carboxymethylcellulose, pectin, and gelatin, is
used to coat such treatments. These are not suggested for use on infected ulcers due to their
occlusive nature. Because these generally only modestly absorbent, these may be employed in
weakly exudative ulceration or when autolytic debridement is desired. The creation of a thick,
pseudopurulent, and foul-smelling hydrogel, which might create the appearance of infections if
the physician is unaware of this potential, is one of the features of this kind of medicine that can
1.3.1.1 Hydrocolloids
A mixture of three hydrocolloids, such as sodium carboxymethylcellulose, pectin, and gelatin, is
used to coat such treatments. These are not suggested for use on infected ulcers due to their
occlusive nature. Because these generally only modestly absorbent, these may be employed in
weakly exudative ulceration or when autolytic debridement is desired. The creation of a thick,
pseudopurulent, and foul-smelling hydrogel, which might create the appearance of infections if
the physician is unaware of this potential, is one of the features of this kind of medicine that can
PUBLIC
restrict its usage. Foam products have now largely supplanted these treatments. (Dumville et al.
2015b; Sarkar and Ballantyne,2001)
1.3.1.2 cell based dressing
A live-cell composition including at minimum single stratum of living allogenic progenitors is
used to make cell-based dressing. Extracellular matix materials, independent (decellular) or in
conjunction with diverse cellular forms including such fibroblasts or keratinocytes, are used to
resemble natural skin. Skin replacements work as sterile tissue grafts that merge with native
tissue to promote cell migration, angiogenesis, and epithelialization in wounds (Jones et al.,
2013; Greaves et al., 2013).
1.3.1.3 Biological dressings
Whenever standard dressings perform poorly or are considered unsuitable, biologic dressings
may be utilized. Sheehan et al., (2006) found that using biological dressings in chronic lesions
which have ceased to recover at a suitable frequency of closures may result in a 55 percent
decrease in wound area in only four weeks. Such treatments could contain epidermal or dermal
components (Hedayati et al., 2015).
1.3.1.4 Polyurethane foams
Foam dressing generally composed of two layers: a hydrophobic exterior coating and a
hydrophilic and absorbent inner layer, which are formed up of a mix of polyurethanes, acrylates,
and other materials. Preparations are offered in both sticky & nonadhesive varieties. These are
semiocclusive and may be used on ulceration that are infected (Velasco, 2012).Foam treatments
insulate the lesion and keep it wet, as well as preventing injury to the wound when it is removed.
Such dressings might potentially be administered as a supplementary dressing for infected
wounds in combination using alginate or hydrogel dressing and a topical antibacterial treatment
(Davies et al., 2017) Furthermore, the presence of the anti-biofilm lichen metabolite usnic acids
in the polyaniline/polyurethane foam dressing suggested that the conducting polymer's
antibiofilm action had enhanced (dos Santos et al., 2018).
restrict its usage. Foam products have now largely supplanted these treatments. (Dumville et al.
2015b; Sarkar and Ballantyne,2001)
1.3.1.2 cell based dressing
A live-cell composition including at minimum single stratum of living allogenic progenitors is
used to make cell-based dressing. Extracellular matix materials, independent (decellular) or in
conjunction with diverse cellular forms including such fibroblasts or keratinocytes, are used to
resemble natural skin. Skin replacements work as sterile tissue grafts that merge with native
tissue to promote cell migration, angiogenesis, and epithelialization in wounds (Jones et al.,
2013; Greaves et al., 2013).
1.3.1.3 Biological dressings
Whenever standard dressings perform poorly or are considered unsuitable, biologic dressings
may be utilized. Sheehan et al., (2006) found that using biological dressings in chronic lesions
which have ceased to recover at a suitable frequency of closures may result in a 55 percent
decrease in wound area in only four weeks. Such treatments could contain epidermal or dermal
components (Hedayati et al., 2015).
1.3.1.4 Polyurethane foams
Foam dressing generally composed of two layers: a hydrophobic exterior coating and a
hydrophilic and absorbent inner layer, which are formed up of a mix of polyurethanes, acrylates,
and other materials. Preparations are offered in both sticky & nonadhesive varieties. These are
semiocclusive and may be used on ulceration that are infected (Velasco, 2012).Foam treatments
insulate the lesion and keep it wet, as well as preventing injury to the wound when it is removed.
Such dressings might potentially be administered as a supplementary dressing for infected
wounds in combination using alginate or hydrogel dressing and a topical antibacterial treatment
(Davies et al., 2017) Furthermore, the presence of the anti-biofilm lichen metabolite usnic acids
in the polyaniline/polyurethane foam dressing suggested that the conducting polymer's
antibiofilm action had enhanced (dos Santos et al., 2018).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 36
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





