Dyspnoea: Comprehensive Literature Review and Education Plan
VerifiedAdded on 2022/10/19
|17
|5638
|13
Report
AI Summary
This report provides a comprehensive literature review on dyspnoea, a condition characterized by shortness of breath. It delves into the causes, including heart, lung, and airway issues, and examines the various symptoms associated with the condition. The report explores both pharmacological and non-pharmacological interventions, detailing the effectiveness of each approach and the importance of considering individual patient needs. It also reviews the educational needs of patients, emphasizing the importance of understanding the disease, its symptoms, and the available treatment options. The report analyzes psychological, physiological, and sociocultural factors that influence dyspnoea and provides guidance on patient education, including breathing exercises, emotional control techniques, and the importance of a supportive environment. The report also explains the causes and symptoms of dyspnoea, and discusses the role of healthcare providers and the importance of early intervention and effective management to improve patient outcomes. The literature review offers a thorough analysis of the existing research, providing valuable insights into the diagnosis, treatment, and management of dyspnoea.
Dysponea
Literature Review
System04104
7/23/2019
Literature Review
System04104
7/23/2019
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction
Dyspnoea is a sign of serious disease related to heart, lungs, or airway in which
patient faces problems related to breathing. Dyspnoea generally causes problems for the
patient when it is ignored by the patient. Dyspnoea required to seek medical attention and
proper care from doctors. Shortness of breath or laboured breathing is the major symptoms of
Dyspnoea and it might be a temporary or permanent health problem for a patient. Sometimes
people who suffocated due to heavy pollution may face issues related to Dyspnoea
(Laviolette & Laveneziana, 2014). Dyspnoea can happen as a result of overexertion, spending
time on high altitude, due to heart-related issues, or dis-functioning of lungs. Sometimes it is
really difficult to identify the causes of Dyspnoea because there are many causes of such type
of different diseases. However, if the causes of the problem could not be identified by the
doctors then it is really difficult to treat the disease. However, it is one of the common forms
of health issues that can be easily found in 1 in every 4 people who visit the doctor. This
report has been prepared to identify the symptoms and causes of Dyspnoea and educates the
patient how they can fight with this disease. Apart from this, this report also includes a
literature review that analyses the different work of researchers on Dyspnoea.
Literature Review
Dyspnoea or breathlessness is a common problem in adults and old age people. It is a
type of discomfort that people face during breathing. Dyspnoea is generally observed in adult
Dyspnoea is a sign of serious disease related to heart, lungs, or airway in which
patient faces problems related to breathing. Dyspnoea generally causes problems for the
patient when it is ignored by the patient. Dyspnoea required to seek medical attention and
proper care from doctors. Shortness of breath or laboured breathing is the major symptoms of
Dyspnoea and it might be a temporary or permanent health problem for a patient. Sometimes
people who suffocated due to heavy pollution may face issues related to Dyspnoea
(Laviolette & Laveneziana, 2014). Dyspnoea can happen as a result of overexertion, spending
time on high altitude, due to heart-related issues, or dis-functioning of lungs. Sometimes it is
really difficult to identify the causes of Dyspnoea because there are many causes of such type
of different diseases. However, if the causes of the problem could not be identified by the
doctors then it is really difficult to treat the disease. However, it is one of the common forms
of health issues that can be easily found in 1 in every 4 people who visit the doctor. This
report has been prepared to identify the symptoms and causes of Dyspnoea and educates the
patient how they can fight with this disease. Apart from this, this report also includes a
literature review that analyses the different work of researchers on Dyspnoea.
Literature Review
Dyspnoea or breathlessness is a common problem in adults and old age people. It is a
type of discomfort that people face during breathing. Dyspnoea is generally observed in adult
and old age people. However, there are several factors or underlying conditions under which
Dyspnoea arises such as problem-related to heart, lungs, or breathing. However, the advance
stage of this disease requires both pharmacological and non-pharmacological interventions.
There are various researches and meta-analysis researches were presented by the researchers
and health specialists on this serious health issue (Abernethy, McDonald, Frith, Clark,
Herndon II, Marcello & Wheeler, 2010). Many researchers found that the effects of
pharmacological interventions such as benzodiazepines, opioids, and oxygen are the major
factors that play a key role in breathlessness in adult patients. However, the use of drugs in
dyspnoea is sometimes ineffective in the patients and sometimes it may have negative effects
on the health of patients. Therefore, the situation of patients, who are suffering from
breathlessness, is so essential before deciding which type of interventions patient required.
The negative effect of medicines is the major problem in breathlessness, thus non-
pharmacological treatment is an important part of intervening a dyspnoea patient (Kiely,
Elliot, Sabroe & Condliffe, 2013).
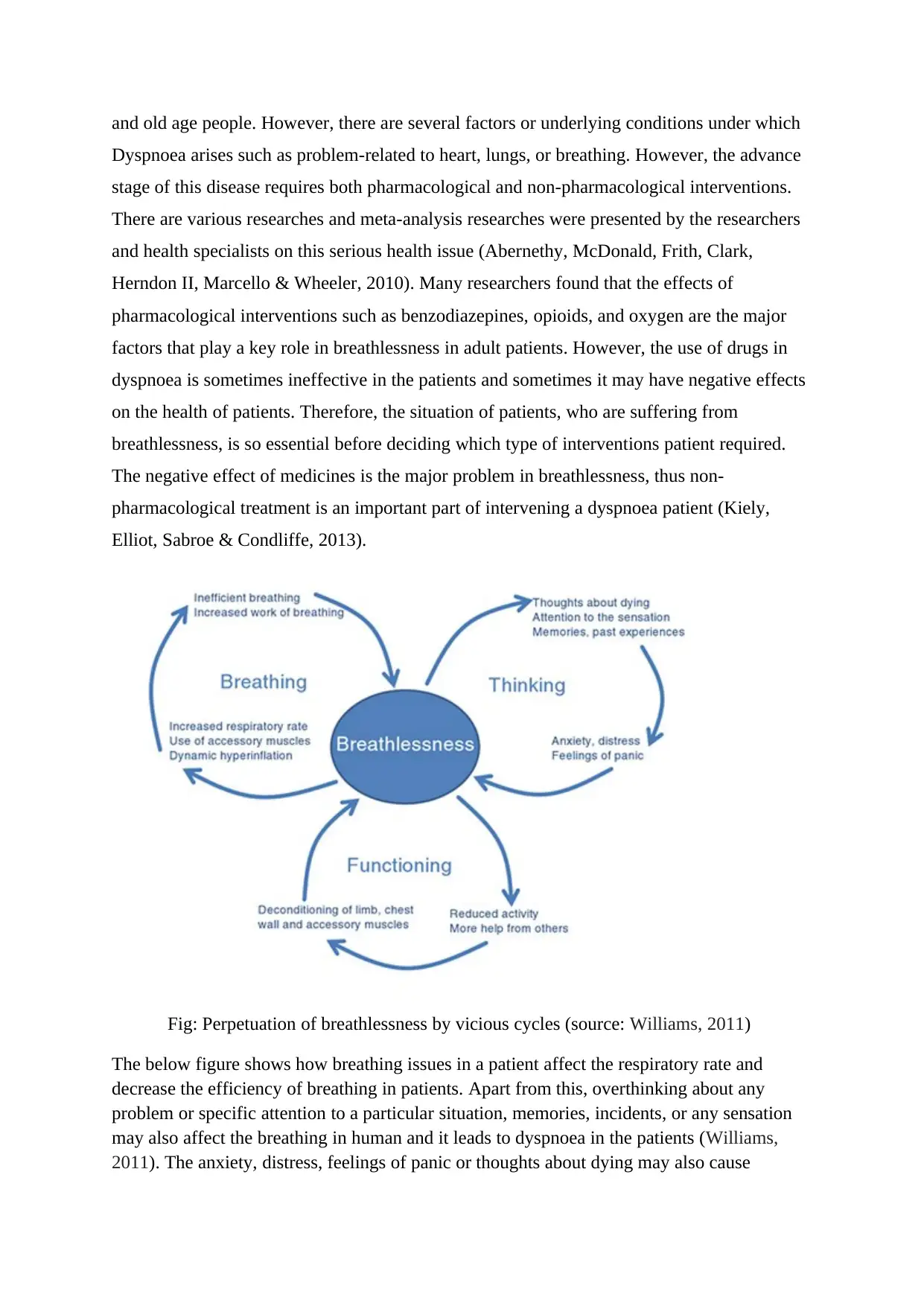
Fig: Perpetuation of breathlessness by vicious cycles (source: Williams, 2011)
The below figure shows how breathing issues in a patient affect the respiratory rate and
decrease the efficiency of breathing in patients. Apart from this, overthinking about any
problem or specific attention to a particular situation, memories, incidents, or any sensation
may also affect the breathing in human and it leads to dyspnoea in the patients (Williams,
2011). The anxiety, distress, feelings of panic or thoughts about dying may also cause
Dyspnoea arises such as problem-related to heart, lungs, or breathing. However, the advance
stage of this disease requires both pharmacological and non-pharmacological interventions.
There are various researches and meta-analysis researches were presented by the researchers
and health specialists on this serious health issue (Abernethy, McDonald, Frith, Clark,
Herndon II, Marcello & Wheeler, 2010). Many researchers found that the effects of
pharmacological interventions such as benzodiazepines, opioids, and oxygen are the major
factors that play a key role in breathlessness in adult patients. However, the use of drugs in
dyspnoea is sometimes ineffective in the patients and sometimes it may have negative effects
on the health of patients. Therefore, the situation of patients, who are suffering from
breathlessness, is so essential before deciding which type of interventions patient required.
The negative effect of medicines is the major problem in breathlessness, thus non-
pharmacological treatment is an important part of intervening a dyspnoea patient (Kiely,
Elliot, Sabroe & Condliffe, 2013).
Fig: Perpetuation of breathlessness by vicious cycles (source: Williams, 2011)
The below figure shows how breathing issues in a patient affect the respiratory rate and
decrease the efficiency of breathing in patients. Apart from this, overthinking about any
problem or specific attention to a particular situation, memories, incidents, or any sensation
may also affect the breathing in human and it leads to dyspnoea in the patients (Williams,
2011). The anxiety, distress, feelings of panic or thoughts about dying may also cause
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

dyspnoea in people. However, there are many kinds of research and interventions are
suitable to the different stage of dyspnoea and it can be divided into two interventions styles:
Pharmacological interventions and non- pharmacological interventions (Hunt, Williams, Frith
& Schembri, 2010).
Pharmacological interventions
There are huge numbers of pharmacological intervention available for patients who
are suffering from breathlessness. Numbers of studies and interventions for dyspnoea aims to
relieve breathlessness by trying available pharmacological treatment (Russell, Ehrman,
Cosby, Ansari, Tseeng, Christain & Bailitz, 2015). However, it has been seen that non-
pharmacological interventions are also required to intervene in the breathlessness issue in
patients. Breathlessness is a multidimensional symptom that shows dis-functionality of heart
or lung of even it shows several other issues in the body that causes breathing problem in the
patient. However, a serious case of dyspnoea needs pharmacological intervention rather than
non-pharmacological intervention. A patient who is suffering from dyspnoea must in touch
with the specialist doctors and should take the medicines on time (Abernethy, Wheeler, &
Currow, 2010).
Dyspnoea is a situation where the patient gets little oxygen through breathing or the
body cannot get enough air. It is sometimes the symptom of the heart attack or lungs failure.
It is also a sign of asthma in-patient. Dyspnoea is sometimes a serious problem for the patient
suitable to the different stage of dyspnoea and it can be divided into two interventions styles:
Pharmacological interventions and non- pharmacological interventions (Hunt, Williams, Frith
& Schembri, 2010).
Pharmacological interventions
There are huge numbers of pharmacological intervention available for patients who
are suffering from breathlessness. Numbers of studies and interventions for dyspnoea aims to
relieve breathlessness by trying available pharmacological treatment (Russell, Ehrman,
Cosby, Ansari, Tseeng, Christain & Bailitz, 2015). However, it has been seen that non-
pharmacological interventions are also required to intervene in the breathlessness issue in
patients. Breathlessness is a multidimensional symptom that shows dis-functionality of heart
or lung of even it shows several other issues in the body that causes breathing problem in the
patient. However, a serious case of dyspnoea needs pharmacological intervention rather than
non-pharmacological intervention. A patient who is suffering from dyspnoea must in touch
with the specialist doctors and should take the medicines on time (Abernethy, Wheeler, &
Currow, 2010).
Dyspnoea is a situation where the patient gets little oxygen through breathing or the
body cannot get enough air. It is sometimes the symptom of the heart attack or lungs failure.
It is also a sign of asthma in-patient. Dyspnoea is sometimes a serious problem for the patient
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
when the patient ignores the problem in the initial phase and fail to take the proper
intervention from specialist doctors. The patient should take the immediate treatment or
persuasion from the doctor if the patient feels a short of breath very suddenly (Wiseman,
Rowett, Allcroft, Abernethy & Currow, 2013). There are several types of dyspnoea happen
when the body of a person in certain position like orthopnoea, which is a situation where
people experience shortness of breath when the patient lie down. The lung failure or an issue
related to the lung is also a major problem in dyspnoea disease. However, if a person sitting
state or standing usually will be helpful in problem-related to orthopnoea.
Non-pharmacological interventions
Dyspnoea is not related to the health of people rather sometimes it occurs in patients
because of heavy exercise or work as well. However, this type of issue of dyspnoea is not
required pharmacological interventions rather it required non-pharmacological interventions.
According to Dr. Steven Wahls, the major causes of dyspnoea are asthma, lung failures,
chronic obstructive pulmonary disease (COPD), heart failure, and psychological issues such
as anxiety, fear, and anger. These are the some of the common causes, which can easily find
in people (Nazerian, Vanni, Zanobetti, Polidori, Pepe, Federico & Grifoni, 2010).
Respiration is the first non-pharmacological process or interventions that are helpful in
dyspnoea and it is more effective when people facing the early stage of breathing problem. It
can be said that while breathing is a physical process, respiration is a chemical process that
enables the patient to take oxygen in deep to the heart and then leave the carbon dioxide
(CO2).
intervention from specialist doctors. The patient should take the immediate treatment or
persuasion from the doctor if the patient feels a short of breath very suddenly (Wiseman,
Rowett, Allcroft, Abernethy & Currow, 2013). There are several types of dyspnoea happen
when the body of a person in certain position like orthopnoea, which is a situation where
people experience shortness of breath when the patient lie down. The lung failure or an issue
related to the lung is also a major problem in dyspnoea disease. However, if a person sitting
state or standing usually will be helpful in problem-related to orthopnoea.
Non-pharmacological interventions
Dyspnoea is not related to the health of people rather sometimes it occurs in patients
because of heavy exercise or work as well. However, this type of issue of dyspnoea is not
required pharmacological interventions rather it required non-pharmacological interventions.
According to Dr. Steven Wahls, the major causes of dyspnoea are asthma, lung failures,
chronic obstructive pulmonary disease (COPD), heart failure, and psychological issues such
as anxiety, fear, and anger. These are the some of the common causes, which can easily find
in people (Nazerian, Vanni, Zanobetti, Polidori, Pepe, Federico & Grifoni, 2010).
Respiration is the first non-pharmacological process or interventions that are helpful in
dyspnoea and it is more effective when people facing the early stage of breathing problem. It
can be said that while breathing is a physical process, respiration is a chemical process that
enables the patient to take oxygen in deep to the heart and then leave the carbon dioxide
(CO2).
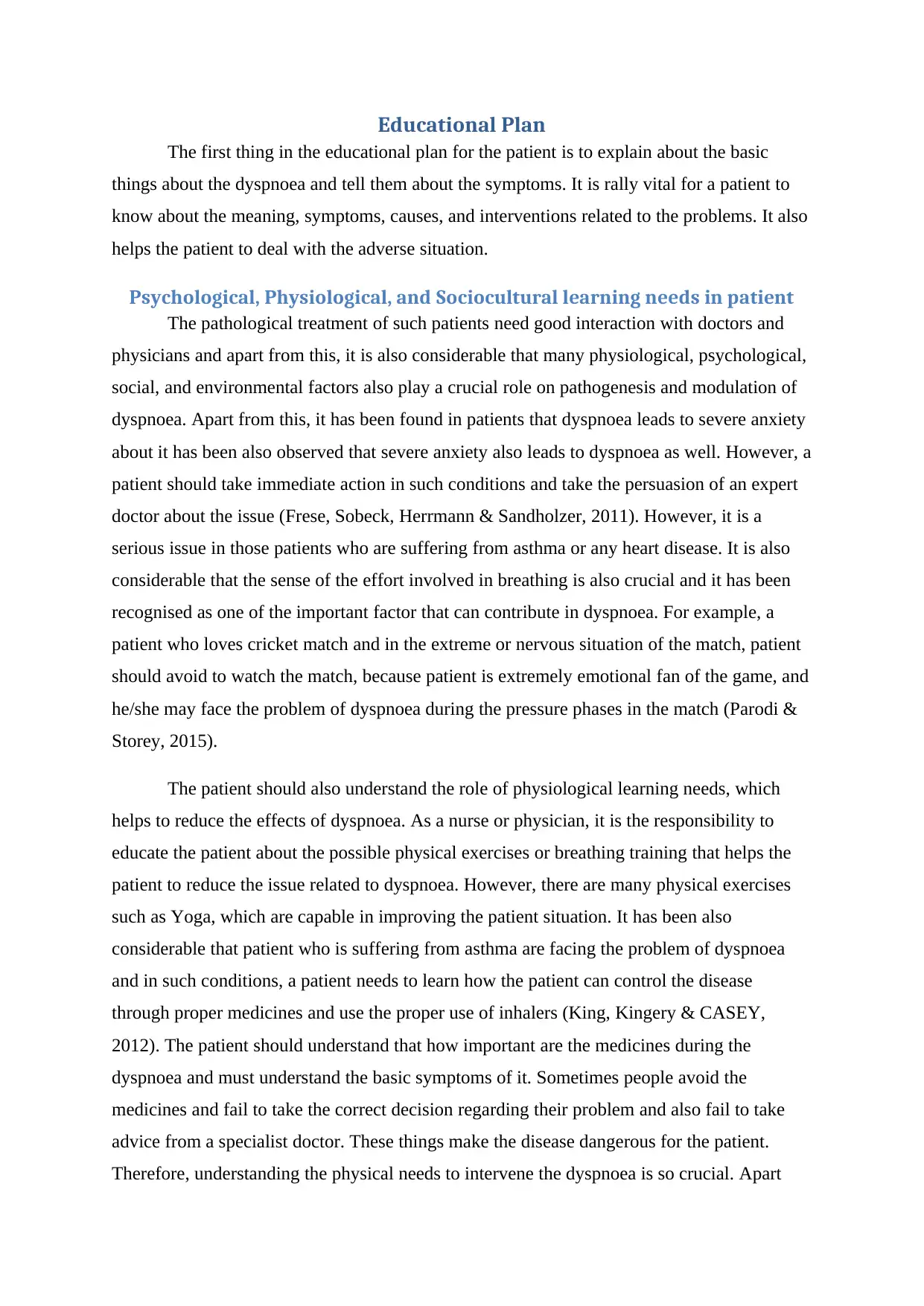
Respiration helps in continuing the breathing in natural ways and reduces the
obstruction that occurs during breathing in the patients. The increased respiratory rate can
also be controlled and here patient needs to use the accessory muscles. However, another
aspect of non-pharmacological interventions is related to control to cognition of emotions of
the patient. In this type of intervention system, the patient needs to control the emotions and
feelings of their self, which affect the breathing process. It is one of the toughest intervention
techniques, which is not developed in the patients instantly rather patient will have to work
hard to control their emotions and feelings that cause breathlessness (Wiseman et. al., 2013).
Apart from this, the non-pharmacological interventions also include physical exercise and
functioning like yoga and meditation that helps in improving the breathing issue in adults
especially. However, the major aim behind these non-pharmacological treatment procedures
is to improve the breathing in patents and train them how they can improve the breathing.
Breathing control exercises are also part of an intervention that includes taking cool and fresh
air, taking full oxygen trough breath, and do all the exercise that can be helpful in dyspnoea.
The patient should also focus on chest vibration and other techniques that can be used to
improve the dyspnoea issue in the patient. Breathing training interventions is one of the main
physiological techniques that can be used for respiration and also helpful in prolonged
exhalation in the breathing process.
obstruction that occurs during breathing in the patients. The increased respiratory rate can
also be controlled and here patient needs to use the accessory muscles. However, another
aspect of non-pharmacological interventions is related to control to cognition of emotions of
the patient. In this type of intervention system, the patient needs to control the emotions and
feelings of their self, which affect the breathing process. It is one of the toughest intervention
techniques, which is not developed in the patients instantly rather patient will have to work
hard to control their emotions and feelings that cause breathlessness (Wiseman et. al., 2013).
Apart from this, the non-pharmacological interventions also include physical exercise and
functioning like yoga and meditation that helps in improving the breathing issue in adults
especially. However, the major aim behind these non-pharmacological treatment procedures
is to improve the breathing in patents and train them how they can improve the breathing.
Breathing control exercises are also part of an intervention that includes taking cool and fresh
air, taking full oxygen trough breath, and do all the exercise that can be helpful in dyspnoea.
The patient should also focus on chest vibration and other techniques that can be used to
improve the dyspnoea issue in the patient. Breathing training interventions is one of the main
physiological techniques that can be used for respiration and also helpful in prolonged
exhalation in the breathing process.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Educational Plan
The first thing in the educational plan for the patient is to explain about the basic
things about the dyspnoea and tell them about the symptoms. It is rally vital for a patient to
know about the meaning, symptoms, causes, and interventions related to the problems. It also
helps the patient to deal with the adverse situation.
Psychological, Physiological, and Sociocultural learning needs in patient
The pathological treatment of such patients need good interaction with doctors and
physicians and apart from this, it is also considerable that many physiological, psychological,
social, and environmental factors also play a crucial role on pathogenesis and modulation of
dyspnoea. Apart from this, it has been found in patients that dyspnoea leads to severe anxiety
about it has been also observed that severe anxiety also leads to dyspnoea as well. However, a
patient should take immediate action in such conditions and take the persuasion of an expert
doctor about the issue (Frese, Sobeck, Herrmann & Sandholzer, 2011). However, it is a
serious issue in those patients who are suffering from asthma or any heart disease. It is also
considerable that the sense of the effort involved in breathing is also crucial and it has been
recognised as one of the important factor that can contribute in dyspnoea. For example, a
patient who loves cricket match and in the extreme or nervous situation of the match, patient
should avoid to watch the match, because patient is extremely emotional fan of the game, and
he/she may face the problem of dyspnoea during the pressure phases in the match (Parodi &
Storey, 2015).
The patient should also understand the role of physiological learning needs, which
helps to reduce the effects of dyspnoea. As a nurse or physician, it is the responsibility to
educate the patient about the possible physical exercises or breathing training that helps the
patient to reduce the issue related to dyspnoea. However, there are many physical exercises
such as Yoga, which are capable in improving the patient situation. It has been also
considerable that patient who is suffering from asthma are facing the problem of dyspnoea
and in such conditions, a patient needs to learn how the patient can control the disease
through proper medicines and use the proper use of inhalers (King, Kingery & CASEY,
2012). The patient should understand that how important are the medicines during the
dyspnoea and must understand the basic symptoms of it. Sometimes people avoid the
medicines and fail to take the correct decision regarding their problem and also fail to take
advice from a specialist doctor. These things make the disease dangerous for the patient.
Therefore, understanding the physical needs to intervene the dyspnoea is so crucial. Apart
The first thing in the educational plan for the patient is to explain about the basic
things about the dyspnoea and tell them about the symptoms. It is rally vital for a patient to
know about the meaning, symptoms, causes, and interventions related to the problems. It also
helps the patient to deal with the adverse situation.
Psychological, Physiological, and Sociocultural learning needs in patient
The pathological treatment of such patients need good interaction with doctors and
physicians and apart from this, it is also considerable that many physiological, psychological,
social, and environmental factors also play a crucial role on pathogenesis and modulation of
dyspnoea. Apart from this, it has been found in patients that dyspnoea leads to severe anxiety
about it has been also observed that severe anxiety also leads to dyspnoea as well. However, a
patient should take immediate action in such conditions and take the persuasion of an expert
doctor about the issue (Frese, Sobeck, Herrmann & Sandholzer, 2011). However, it is a
serious issue in those patients who are suffering from asthma or any heart disease. It is also
considerable that the sense of the effort involved in breathing is also crucial and it has been
recognised as one of the important factor that can contribute in dyspnoea. For example, a
patient who loves cricket match and in the extreme or nervous situation of the match, patient
should avoid to watch the match, because patient is extremely emotional fan of the game, and
he/she may face the problem of dyspnoea during the pressure phases in the match (Parodi &
Storey, 2015).
The patient should also understand the role of physiological learning needs, which
helps to reduce the effects of dyspnoea. As a nurse or physician, it is the responsibility to
educate the patient about the possible physical exercises or breathing training that helps the
patient to reduce the issue related to dyspnoea. However, there are many physical exercises
such as Yoga, which are capable in improving the patient situation. It has been also
considerable that patient who is suffering from asthma are facing the problem of dyspnoea
and in such conditions, a patient needs to learn how the patient can control the disease
through proper medicines and use the proper use of inhalers (King, Kingery & CASEY,
2012). The patient should understand that how important are the medicines during the
dyspnoea and must understand the basic symptoms of it. Sometimes people avoid the
medicines and fail to take the correct decision regarding their problem and also fail to take
advice from a specialist doctor. These things make the disease dangerous for the patient.
Therefore, understanding the physical needs to intervene the dyspnoea is so crucial. Apart
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
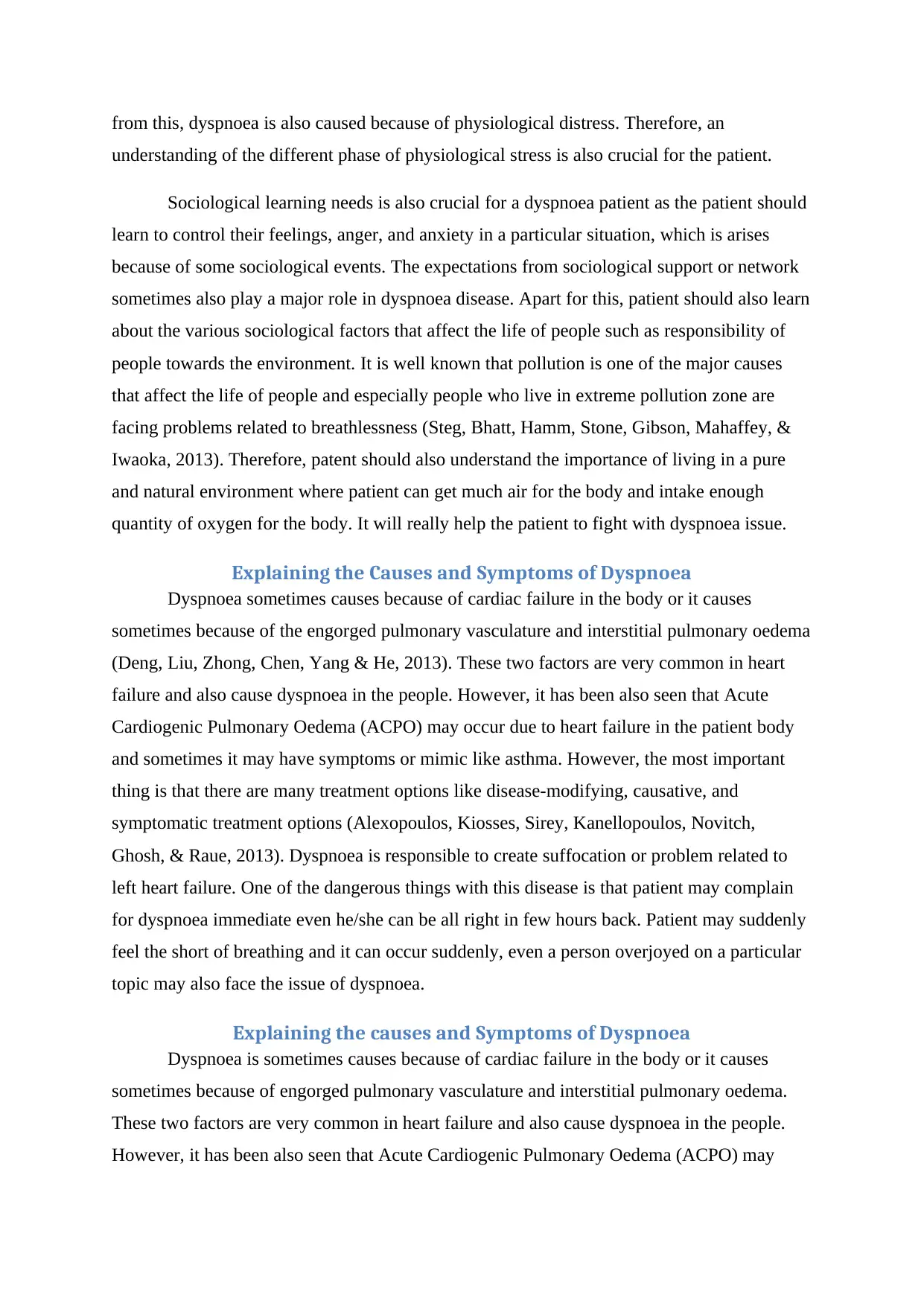
from this, dyspnoea is also caused because of physiological distress. Therefore, an
understanding of the different phase of physiological stress is also crucial for the patient.
Sociological learning needs is also crucial for a dyspnoea patient as the patient should
learn to control their feelings, anger, and anxiety in a particular situation, which is arises
because of some sociological events. The expectations from sociological support or network
sometimes also play a major role in dyspnoea disease. Apart for this, patient should also learn
about the various sociological factors that affect the life of people such as responsibility of
people towards the environment. It is well known that pollution is one of the major causes
that affect the life of people and especially people who live in extreme pollution zone are
facing problems related to breathlessness (Steg, Bhatt, Hamm, Stone, Gibson, Mahaffey, &
Iwaoka, 2013). Therefore, patent should also understand the importance of living in a pure
and natural environment where patient can get much air for the body and intake enough
quantity of oxygen for the body. It will really help the patient to fight with dyspnoea issue.
Explaining the Causes and Symptoms of Dyspnoea
Dyspnoea sometimes causes because of cardiac failure in the body or it causes
sometimes because of the engorged pulmonary vasculature and interstitial pulmonary oedema
(Deng, Liu, Zhong, Chen, Yang & He, 2013). These two factors are very common in heart
failure and also cause dyspnoea in the people. However, it has been also seen that Acute
Cardiogenic Pulmonary Oedema (ACPO) may occur due to heart failure in the patient body
and sometimes it may have symptoms or mimic like asthma. However, the most important
thing is that there are many treatment options like disease-modifying, causative, and
symptomatic treatment options (Alexopoulos, Kiosses, Sirey, Kanellopoulos, Novitch,
Ghosh, & Raue, 2013). Dyspnoea is responsible to create suffocation or problem related to
left heart failure. One of the dangerous things with this disease is that patient may complain
for dyspnoea immediate even he/she can be all right in few hours back. Patient may suddenly
feel the short of breathing and it can occur suddenly, even a person overjoyed on a particular
topic may also face the issue of dyspnoea.
Explaining the causes and Symptoms of Dyspnoea
Dyspnoea is sometimes causes because of cardiac failure in the body or it causes
sometimes because of engorged pulmonary vasculature and interstitial pulmonary oedema.
These two factors are very common in heart failure and also cause dyspnoea in the people.
However, it has been also seen that Acute Cardiogenic Pulmonary Oedema (ACPO) may
understanding of the different phase of physiological stress is also crucial for the patient.
Sociological learning needs is also crucial for a dyspnoea patient as the patient should
learn to control their feelings, anger, and anxiety in a particular situation, which is arises
because of some sociological events. The expectations from sociological support or network
sometimes also play a major role in dyspnoea disease. Apart for this, patient should also learn
about the various sociological factors that affect the life of people such as responsibility of
people towards the environment. It is well known that pollution is one of the major causes
that affect the life of people and especially people who live in extreme pollution zone are
facing problems related to breathlessness (Steg, Bhatt, Hamm, Stone, Gibson, Mahaffey, &
Iwaoka, 2013). Therefore, patent should also understand the importance of living in a pure
and natural environment where patient can get much air for the body and intake enough
quantity of oxygen for the body. It will really help the patient to fight with dyspnoea issue.
Explaining the Causes and Symptoms of Dyspnoea
Dyspnoea sometimes causes because of cardiac failure in the body or it causes
sometimes because of the engorged pulmonary vasculature and interstitial pulmonary oedema
(Deng, Liu, Zhong, Chen, Yang & He, 2013). These two factors are very common in heart
failure and also cause dyspnoea in the people. However, it has been also seen that Acute
Cardiogenic Pulmonary Oedema (ACPO) may occur due to heart failure in the patient body
and sometimes it may have symptoms or mimic like asthma. However, the most important
thing is that there are many treatment options like disease-modifying, causative, and
symptomatic treatment options (Alexopoulos, Kiosses, Sirey, Kanellopoulos, Novitch,
Ghosh, & Raue, 2013). Dyspnoea is responsible to create suffocation or problem related to
left heart failure. One of the dangerous things with this disease is that patient may complain
for dyspnoea immediate even he/she can be all right in few hours back. Patient may suddenly
feel the short of breathing and it can occur suddenly, even a person overjoyed on a particular
topic may also face the issue of dyspnoea.
Explaining the causes and Symptoms of Dyspnoea
Dyspnoea is sometimes causes because of cardiac failure in the body or it causes
sometimes because of engorged pulmonary vasculature and interstitial pulmonary oedema.
These two factors are very common in heart failure and also cause dyspnoea in the people.
However, it has been also seen that Acute Cardiogenic Pulmonary Oedema (ACPO) may
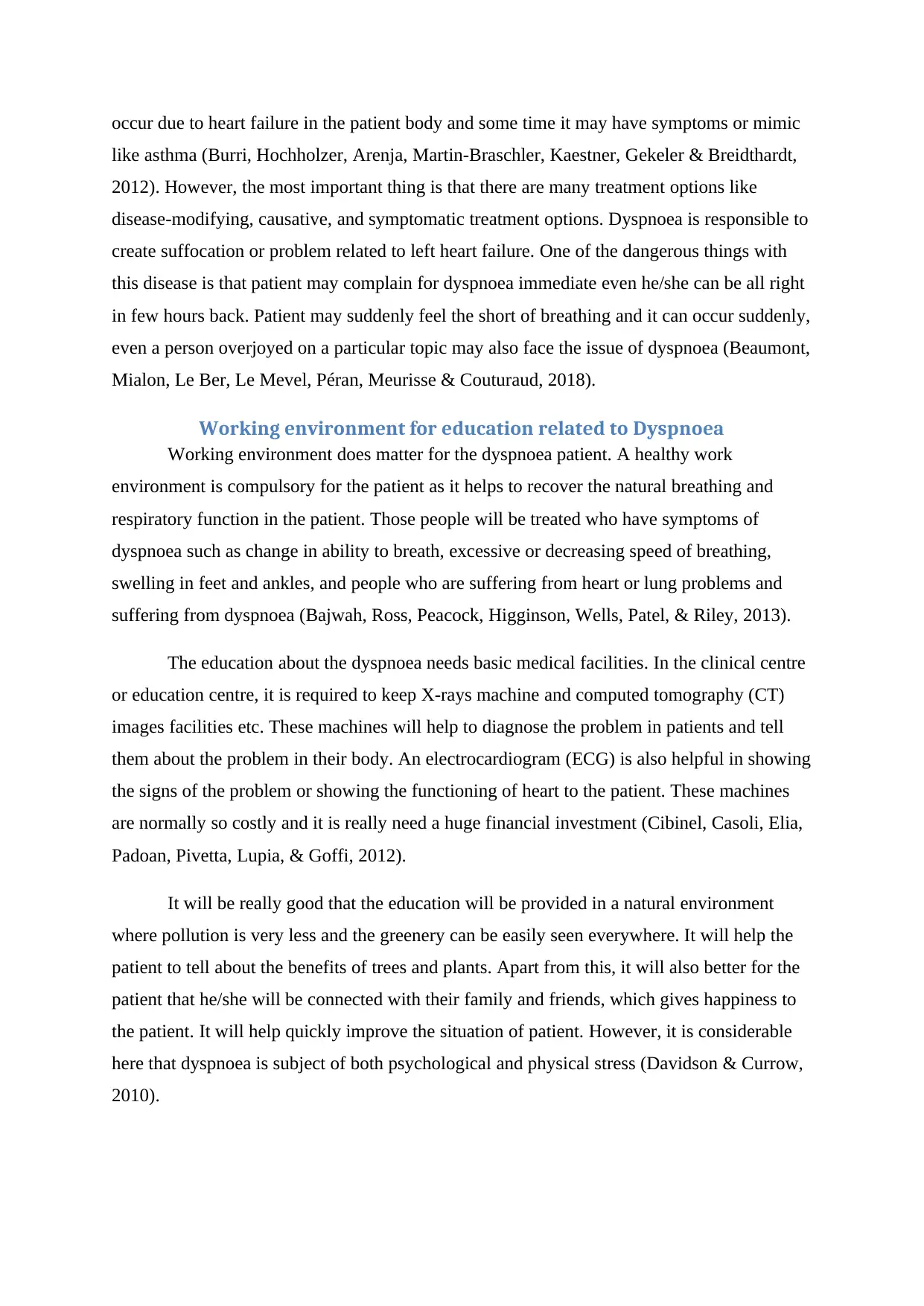
occur due to heart failure in the patient body and some time it may have symptoms or mimic
like asthma (Burri, Hochholzer, Arenja, Martin‐Braschler, Kaestner, Gekeler & Breidthardt,
2012). However, the most important thing is that there are many treatment options like
disease-modifying, causative, and symptomatic treatment options. Dyspnoea is responsible to
create suffocation or problem related to left heart failure. One of the dangerous things with
this disease is that patient may complain for dyspnoea immediate even he/she can be all right
in few hours back. Patient may suddenly feel the short of breathing and it can occur suddenly,
even a person overjoyed on a particular topic may also face the issue of dyspnoea (Beaumont,
Mialon, Le Ber, Le Mevel, Péran, Meurisse & Couturaud, 2018).
Working environment for education related to Dyspnoea
Working environment does matter for the dyspnoea patient. A healthy work
environment is compulsory for the patient as it helps to recover the natural breathing and
respiratory function in the patient. Those people will be treated who have symptoms of
dyspnoea such as change in ability to breath, excessive or decreasing speed of breathing,
swelling in feet and ankles, and people who are suffering from heart or lung problems and
suffering from dyspnoea (Bajwah, Ross, Peacock, Higginson, Wells, Patel, & Riley, 2013).
The education about the dyspnoea needs basic medical facilities. In the clinical centre
or education centre, it is required to keep X-rays machine and computed tomography (CT)
images facilities etc. These machines will help to diagnose the problem in patients and tell
them about the problem in their body. An electrocardiogram (ECG) is also helpful in showing
the signs of the problem or showing the functioning of heart to the patient. These machines
are normally so costly and it is really need a huge financial investment (Cibinel, Casoli, Elia,
Padoan, Pivetta, Lupia, & Goffi, 2012).
It will be really good that the education will be provided in a natural environment
where pollution is very less and the greenery can be easily seen everywhere. It will help the
patient to tell about the benefits of trees and plants. Apart from this, it will also better for the
patient that he/she will be connected with their family and friends, which gives happiness to
the patient. It will help quickly improve the situation of patient. However, it is considerable
here that dyspnoea is subject of both psychological and physical stress (Davidson & Currow,
2010).
like asthma (Burri, Hochholzer, Arenja, Martin‐Braschler, Kaestner, Gekeler & Breidthardt,
2012). However, the most important thing is that there are many treatment options like
disease-modifying, causative, and symptomatic treatment options. Dyspnoea is responsible to
create suffocation or problem related to left heart failure. One of the dangerous things with
this disease is that patient may complain for dyspnoea immediate even he/she can be all right
in few hours back. Patient may suddenly feel the short of breathing and it can occur suddenly,
even a person overjoyed on a particular topic may also face the issue of dyspnoea (Beaumont,
Mialon, Le Ber, Le Mevel, Péran, Meurisse & Couturaud, 2018).
Working environment for education related to Dyspnoea
Working environment does matter for the dyspnoea patient. A healthy work
environment is compulsory for the patient as it helps to recover the natural breathing and
respiratory function in the patient. Those people will be treated who have symptoms of
dyspnoea such as change in ability to breath, excessive or decreasing speed of breathing,
swelling in feet and ankles, and people who are suffering from heart or lung problems and
suffering from dyspnoea (Bajwah, Ross, Peacock, Higginson, Wells, Patel, & Riley, 2013).
The education about the dyspnoea needs basic medical facilities. In the clinical centre
or education centre, it is required to keep X-rays machine and computed tomography (CT)
images facilities etc. These machines will help to diagnose the problem in patients and tell
them about the problem in their body. An electrocardiogram (ECG) is also helpful in showing
the signs of the problem or showing the functioning of heart to the patient. These machines
are normally so costly and it is really need a huge financial investment (Cibinel, Casoli, Elia,
Padoan, Pivetta, Lupia, & Goffi, 2012).
It will be really good that the education will be provided in a natural environment
where pollution is very less and the greenery can be easily seen everywhere. It will help the
patient to tell about the benefits of trees and plants. Apart from this, it will also better for the
patient that he/she will be connected with their family and friends, which gives happiness to
the patient. It will help quickly improve the situation of patient. However, it is considerable
here that dyspnoea is subject of both psychological and physical stress (Davidson & Currow,
2010).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Short-term and long-term goals of the education session for the patient
The education session helps to understand the symptoms and better treatment for the
dyspnoea. The short-term goals of this education session for the patient are as follow:
1. Spread awareness how they can handle the issue related to breathlessness and provide
them suggestions in case of patient is suffering from any type of issues related to
dyspnoea (Sjöström, 2013).
2. The main objective and goal of this education session is to train the patient to identify
the symptoms and its nature of seriousness.
3. This education session also help the patient to improve their breathing process by
yoga and other physical exercises.
Apart from this, the log-term goals of the session helps the patient to avoid those
things in life which causes dyspnoea and provide them a healthy and safe life, where a
dyspnoea patient can enjoy their life like other people. The educations session helps both
youth and old generation people and train them to fight with dyspnoea with better life
schedules. Apart from this, the education plan also helps the patient to follow the
comprehensive treatment plan to remove the disease (Kloke & Cherny, 2015).
Identified interventions and role of specific self-management behaviours
The education session with the patient helps to understand various intervention
techniques to deal with dyspnoea. The education session explains various pathological and
non-pathological treatment and about the self-management behaviour. Self-management
behaviour is the crucial thing in that helps the patient to remain calm and compose even in
the tough situation. It also helps the patient in their daily routine and asks them to maintain a
balance between different works in the daily life schedule (Gallard, Redonnet, Bourcier,
Deshaies, Largeteau, Amalric & Geeraerts, 2015). This education session also helps to
understand the various causes of dyspnoea and explain the treatment and diagnosis ways to
face the issue related to dyspnoea. The aim of the education session to educate and improve
the health awareness of patient and tell them about the possible steps that are helpful in
dyspnoea. However, before all these things appropriate assessment of the dyspnoea is
compulsory and the patient should care about this. It is also considerable that dyspnoea is a
subjective symptom of physiological distress and there are numbers of facilities available in
the healthcare centres to measure the dyspnoea and its causes in patients (Kropski, Pritchett,
Mason, Sivarajan, Gleaves, Johnson & Loyd, 2013). However, assessment of dyspnoea is
The education session helps to understand the symptoms and better treatment for the
dyspnoea. The short-term goals of this education session for the patient are as follow:
1. Spread awareness how they can handle the issue related to breathlessness and provide
them suggestions in case of patient is suffering from any type of issues related to
dyspnoea (Sjöström, 2013).
2. The main objective and goal of this education session is to train the patient to identify
the symptoms and its nature of seriousness.
3. This education session also help the patient to improve their breathing process by
yoga and other physical exercises.
Apart from this, the log-term goals of the session helps the patient to avoid those
things in life which causes dyspnoea and provide them a healthy and safe life, where a
dyspnoea patient can enjoy their life like other people. The educations session helps both
youth and old generation people and train them to fight with dyspnoea with better life
schedules. Apart from this, the education plan also helps the patient to follow the
comprehensive treatment plan to remove the disease (Kloke & Cherny, 2015).
Identified interventions and role of specific self-management behaviours
The education session with the patient helps to understand various intervention
techniques to deal with dyspnoea. The education session explains various pathological and
non-pathological treatment and about the self-management behaviour. Self-management
behaviour is the crucial thing in that helps the patient to remain calm and compose even in
the tough situation. It also helps the patient in their daily routine and asks them to maintain a
balance between different works in the daily life schedule (Gallard, Redonnet, Bourcier,
Deshaies, Largeteau, Amalric & Geeraerts, 2015). This education session also helps to
understand the various causes of dyspnoea and explain the treatment and diagnosis ways to
face the issue related to dyspnoea. The aim of the education session to educate and improve
the health awareness of patient and tell them about the possible steps that are helpful in
dyspnoea. However, before all these things appropriate assessment of the dyspnoea is
compulsory and the patient should care about this. It is also considerable that dyspnoea is a
subjective symptom of physiological distress and there are numbers of facilities available in
the healthcare centres to measure the dyspnoea and its causes in patients (Kropski, Pritchett,
Mason, Sivarajan, Gleaves, Johnson & Loyd, 2013). However, assessment of dyspnoea is
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
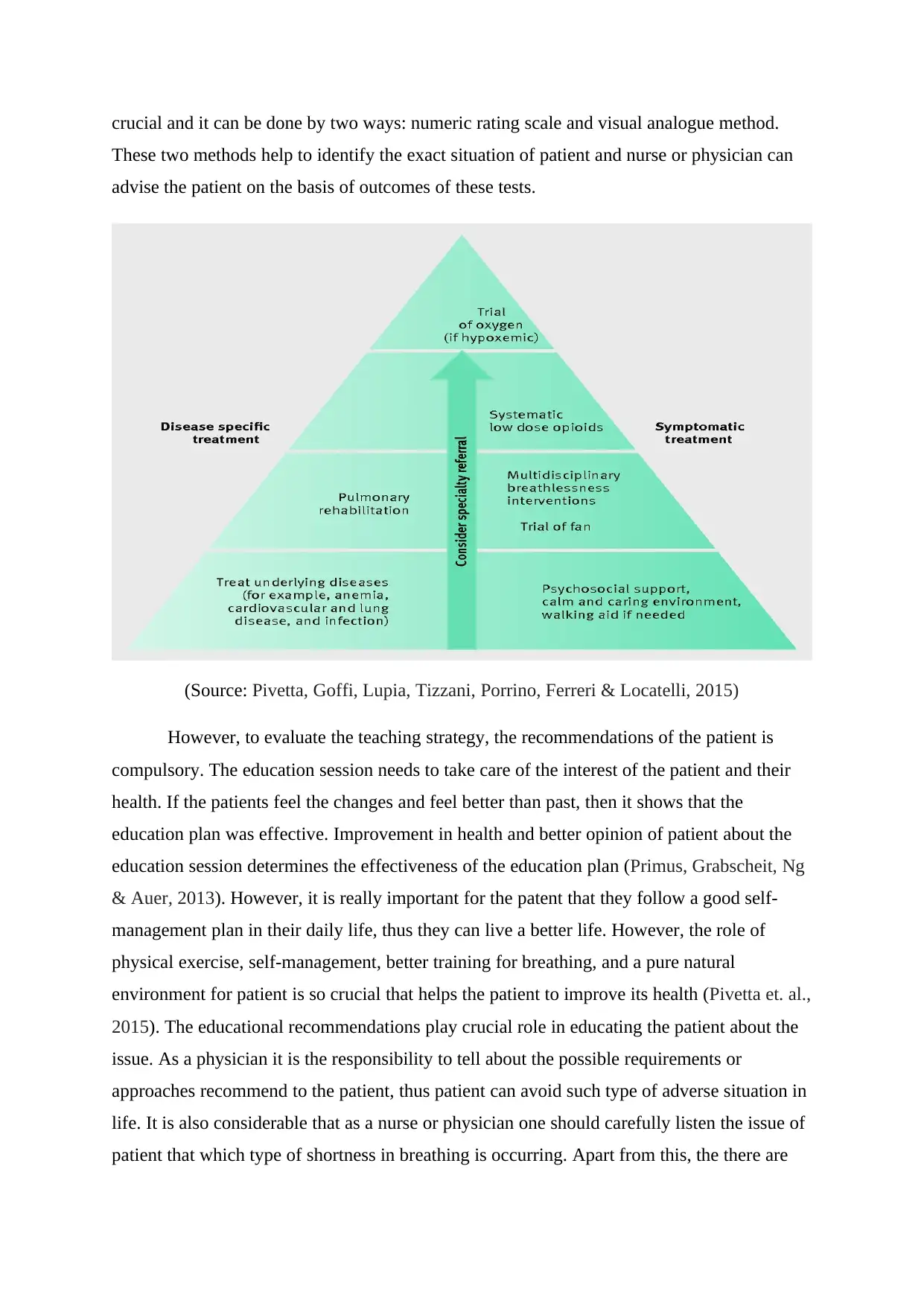
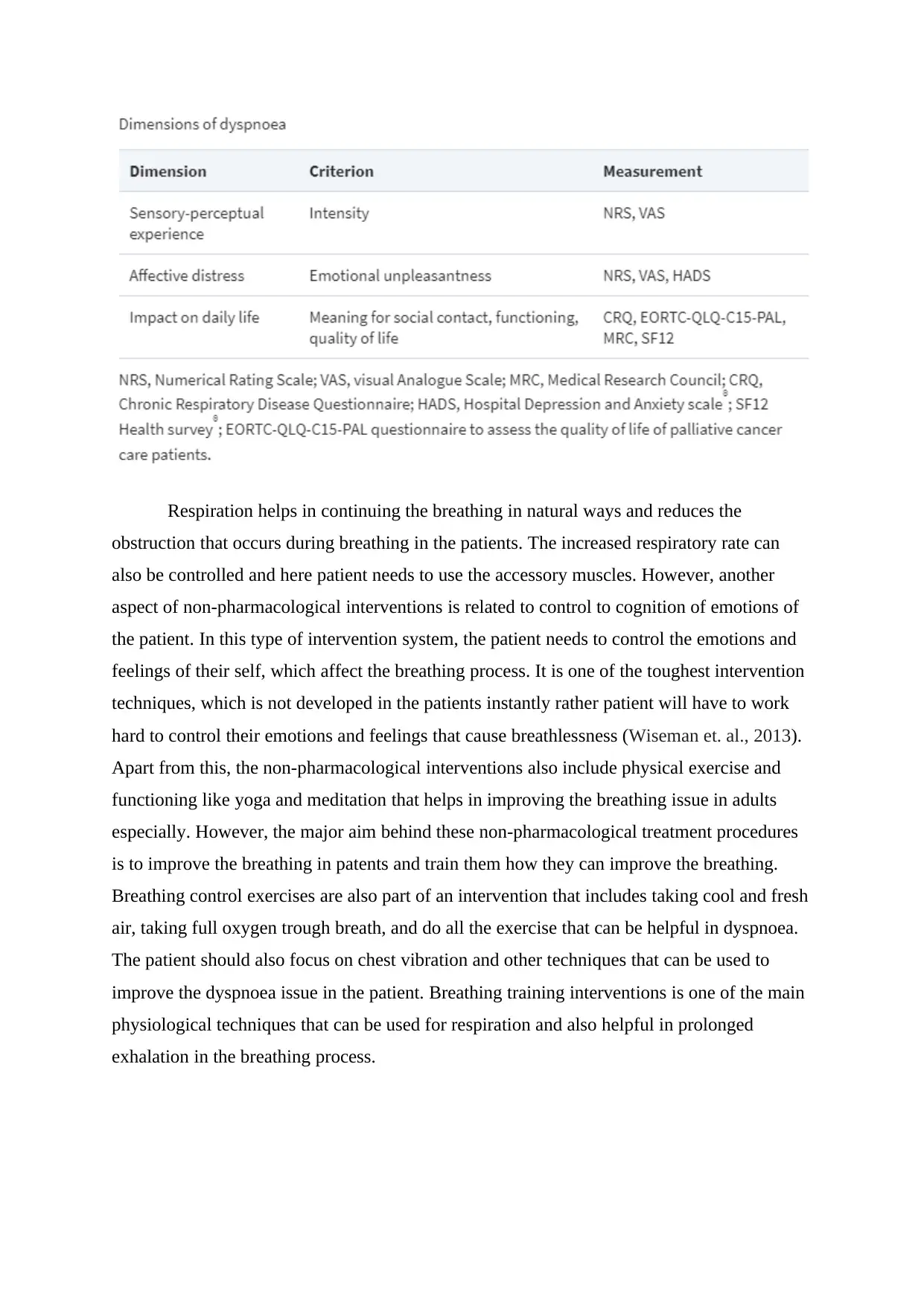
crucial and it can be done by two ways: numeric rating scale and visual analogue method.
These two methods help to identify the exact situation of patient and nurse or physician can
advise the patient on the basis of outcomes of these tests.
(Source: Pivetta, Goffi, Lupia, Tizzani, Porrino, Ferreri & Locatelli, 2015)
However, to evaluate the teaching strategy, the recommendations of the patient is
compulsory. The education session needs to take care of the interest of the patient and their
health. If the patients feel the changes and feel better than past, then it shows that the
education plan was effective. Improvement in health and better opinion of patient about the
education session determines the effectiveness of the education plan (Primus, Grabscheit, Ng
& Auer, 2013). However, it is really important for the patent that they follow a good self-
management plan in their daily life, thus they can live a better life. However, the role of
physical exercise, self-management, better training for breathing, and a pure natural
environment for patient is so crucial that helps the patient to improve its health (Pivetta et. al.,
2015). The educational recommendations play crucial role in educating the patient about the
issue. As a physician it is the responsibility to tell about the possible requirements or
approaches recommend to the patient, thus patient can avoid such type of adverse situation in
life. It is also considerable that as a nurse or physician one should carefully listen the issue of
patient that which type of shortness in breathing is occurring. Apart from this, the there are
These two methods help to identify the exact situation of patient and nurse or physician can
advise the patient on the basis of outcomes of these tests.
(Source: Pivetta, Goffi, Lupia, Tizzani, Porrino, Ferreri & Locatelli, 2015)
However, to evaluate the teaching strategy, the recommendations of the patient is
compulsory. The education session needs to take care of the interest of the patient and their
health. If the patients feel the changes and feel better than past, then it shows that the
education plan was effective. Improvement in health and better opinion of patient about the
education session determines the effectiveness of the education plan (Primus, Grabscheit, Ng
& Auer, 2013). However, it is really important for the patent that they follow a good self-
management plan in their daily life, thus they can live a better life. However, the role of
physical exercise, self-management, better training for breathing, and a pure natural
environment for patient is so crucial that helps the patient to improve its health (Pivetta et. al.,
2015). The educational recommendations play crucial role in educating the patient about the
issue. As a physician it is the responsibility to tell about the possible requirements or
approaches recommend to the patient, thus patient can avoid such type of adverse situation in
life. It is also considerable that as a nurse or physician one should carefully listen the issue of
patient that which type of shortness in breathing is occurring. Apart from this, the there are
several relaxation techniques which should be offered by the physician and nurses to the
patient, thus patient can avoid the critical stage of dyspnoea (Pratter, Abouzgheib, Akers,
Kass & Bartter, 2011).
The teaching methodology is also crucial in the education. To educate dyspnoea
patient, it is necessary to apply both theoretical and practical approach that will help the
patient to understand the scenario. The practical approach like involvement in exercise yoga
helps the patient to feel the improvement and reduction in problems related to dyspnoea.
However, it is better to evaluate the outcome of teaching through measuring the impact of
training and education on the health of patients (Storey, Becker, Harrington, Husted, James,
Cools & Cairns, 2011). If the breathing of the patient will be improved after a certain time
period, it definitely shows the effectiveness of education program on the patients. However,
through evaluation of patient’s health, the nurse or physician can determine that whether the
patient needs additional time to improve the health conditions or not. There are so many
therapies or exercise that can reduce the danger of dyspnoea such as oxygen therapy, proper
exercise, yoga, and training of breathing exercise, etc. Medications and vaccinations are the
other techniques through can this type of issue can be resolved in the body (Usmani, Carson,
Cheng, Esterman & Smith, 2011).
Conclusion
In conclusion, breathing is an important function in all function in the human body,
which is regulated by many other body functions like functioning of heart, functioning of
lungs etc. However, issues related to dyspnoea affect the natural breathing of patient.
However, if the patient focuses on self-management and physical exercise such as yoga and
training related to breathing, it definitely helps to reduce effect of the dyspnoea. However,
non-pharmacological interventions are as important as pharmacological interventions in
dyspnoea. While the pharmacological interventions help to provide treatment of a serious
case of dyspnoea, the non-pharmacological treatment helps to improve the patient health and
provide them a healthy future. The impact of dyspnoea can also be minimised through
physical exercise and better life management. it is also considerable that dyspnoea is a
subject of psychological and physical distress, therefore a happy life can also reduce the
chances of such type of disease. The physical environment also plays an important role in
dyspnoea as it provide better environment and fresh air quality to patient in which patient can
patient, thus patient can avoid the critical stage of dyspnoea (Pratter, Abouzgheib, Akers,
Kass & Bartter, 2011).
The teaching methodology is also crucial in the education. To educate dyspnoea
patient, it is necessary to apply both theoretical and practical approach that will help the
patient to understand the scenario. The practical approach like involvement in exercise yoga
helps the patient to feel the improvement and reduction in problems related to dyspnoea.
However, it is better to evaluate the outcome of teaching through measuring the impact of
training and education on the health of patients (Storey, Becker, Harrington, Husted, James,
Cools & Cairns, 2011). If the breathing of the patient will be improved after a certain time
period, it definitely shows the effectiveness of education program on the patients. However,
through evaluation of patient’s health, the nurse or physician can determine that whether the
patient needs additional time to improve the health conditions or not. There are so many
therapies or exercise that can reduce the danger of dyspnoea such as oxygen therapy, proper
exercise, yoga, and training of breathing exercise, etc. Medications and vaccinations are the
other techniques through can this type of issue can be resolved in the body (Usmani, Carson,
Cheng, Esterman & Smith, 2011).
Conclusion
In conclusion, breathing is an important function in all function in the human body,
which is regulated by many other body functions like functioning of heart, functioning of
lungs etc. However, issues related to dyspnoea affect the natural breathing of patient.
However, if the patient focuses on self-management and physical exercise such as yoga and
training related to breathing, it definitely helps to reduce effect of the dyspnoea. However,
non-pharmacological interventions are as important as pharmacological interventions in
dyspnoea. While the pharmacological interventions help to provide treatment of a serious
case of dyspnoea, the non-pharmacological treatment helps to improve the patient health and
provide them a healthy future. The impact of dyspnoea can also be minimised through
physical exercise and better life management. it is also considerable that dyspnoea is a
subject of psychological and physical distress, therefore a happy life can also reduce the
chances of such type of disease. The physical environment also plays an important role in
dyspnoea as it provide better environment and fresh air quality to patient in which patient can
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





