EBP in Nursing: PICOT Question, Poster and Implementation Plan
VerifiedAdded on 2022/08/19
|7
|1381
|8
Project
AI Summary
This assignment presents an evidence-based practice (EBP) project focusing on the effectiveness of alcohol-based hand rubbing solutions versus soap and water in reducing nosocomial infections within a nephrology unit. The project begins with a detailed PICOT question, defining the population, intervention, comparison, and outcome. It then synthesizes evidence supporting the intervention, discusses potential barriers to change (including lack of knowledge and organizational issues), and outlines the project team, which includes nurses, administrators, and physicians. A transformational leadership approach is proposed for facilitating change, along with educational and administrative interventions. The evaluation plan includes weekly debriefing sessions and outcome measurements, such as pre- and post-intervention colony counts. The implementation plan provides a timeline, details educational plans, and specifies required equipment. The references support the evidence-based approach to the project, highlighting the importance of hand hygiene in healthcare settings. This project aims to improve patient outcomes by implementing effective hand hygiene practices.

Running head: EVIDENCE PRACTICE IN NURSING: PICOT QUESTION AND POSTER
EVIDENCE BASED PRACTICE IN NURSING: PICOT QUESTION AND POSTER
Name of the Student:
Name of the University:
Author note:
EVIDENCE BASED PRACTICE IN NURSING: PICOT QUESTION AND POSTER
Name of the Student:
Name of the University:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1EVIDENCE BASED PRACTICE IN NURSING: PICOT QUESTION AND POSTER
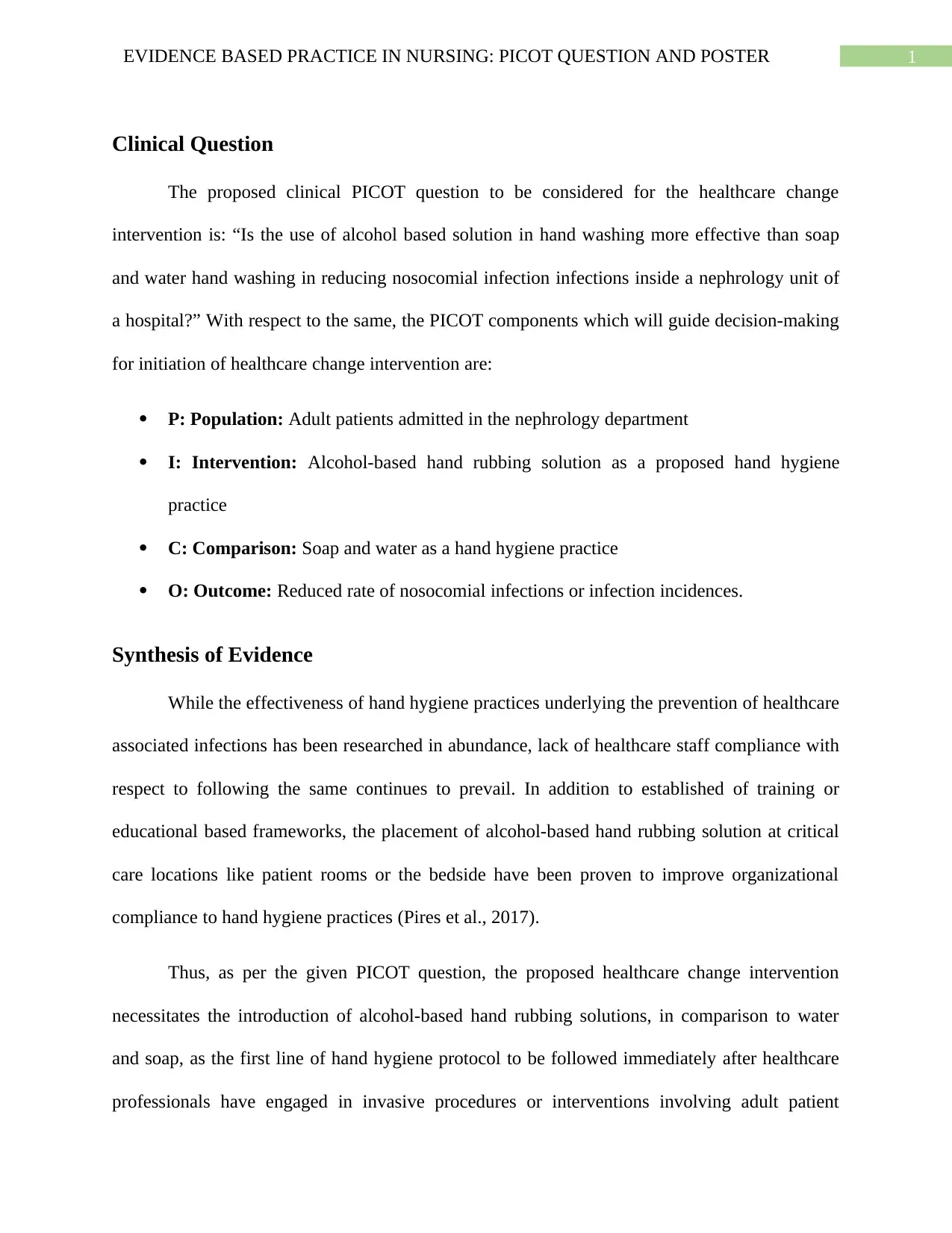
Clinical Question
The proposed clinical PICOT question to be considered for the healthcare change
intervention is: “Is the use of alcohol based solution in hand washing more effective than soap
and water hand washing in reducing nosocomial infection infections inside a nephrology unit of
a hospital?” With respect to the same, the PICOT components which will guide decision-making
for initiation of healthcare change intervention are:
P: Population: Adult patients admitted in the nephrology department
I: Intervention: Alcohol-based hand rubbing solution as a proposed hand hygiene
practice
C: Comparison: Soap and water as a hand hygiene practice
O: Outcome: Reduced rate of nosocomial infections or infection incidences.
Synthesis of Evidence
While the effectiveness of hand hygiene practices underlying the prevention of healthcare
associated infections has been researched in abundance, lack of healthcare staff compliance with
respect to following the same continues to prevail. In addition to established of training or
educational based frameworks, the placement of alcohol-based hand rubbing solution at critical
care locations like patient rooms or the bedside have been proven to improve organizational
compliance to hand hygiene practices (Pires et al., 2017).
Thus, as per the given PICOT question, the proposed healthcare change intervention
necessitates the introduction of alcohol-based hand rubbing solutions, in comparison to water
and soap, as the first line of hand hygiene protocol to be followed immediately after healthcare
professionals have engaged in invasive procedures or interventions involving adult patient
Clinical Question
The proposed clinical PICOT question to be considered for the healthcare change
intervention is: “Is the use of alcohol based solution in hand washing more effective than soap
and water hand washing in reducing nosocomial infection infections inside a nephrology unit of
a hospital?” With respect to the same, the PICOT components which will guide decision-making
for initiation of healthcare change intervention are:
P: Population: Adult patients admitted in the nephrology department
I: Intervention: Alcohol-based hand rubbing solution as a proposed hand hygiene
practice
C: Comparison: Soap and water as a hand hygiene practice
O: Outcome: Reduced rate of nosocomial infections or infection incidences.
Synthesis of Evidence
While the effectiveness of hand hygiene practices underlying the prevention of healthcare
associated infections has been researched in abundance, lack of healthcare staff compliance with
respect to following the same continues to prevail. In addition to established of training or
educational based frameworks, the placement of alcohol-based hand rubbing solution at critical
care locations like patient rooms or the bedside have been proven to improve organizational
compliance to hand hygiene practices (Pires et al., 2017).
Thus, as per the given PICOT question, the proposed healthcare change intervention
necessitates the introduction of alcohol-based hand rubbing solutions, in comparison to water
and soap, as the first line of hand hygiene protocol to be followed immediately after healthcare
professionals have engaged in invasive procedures or interventions involving adult patient
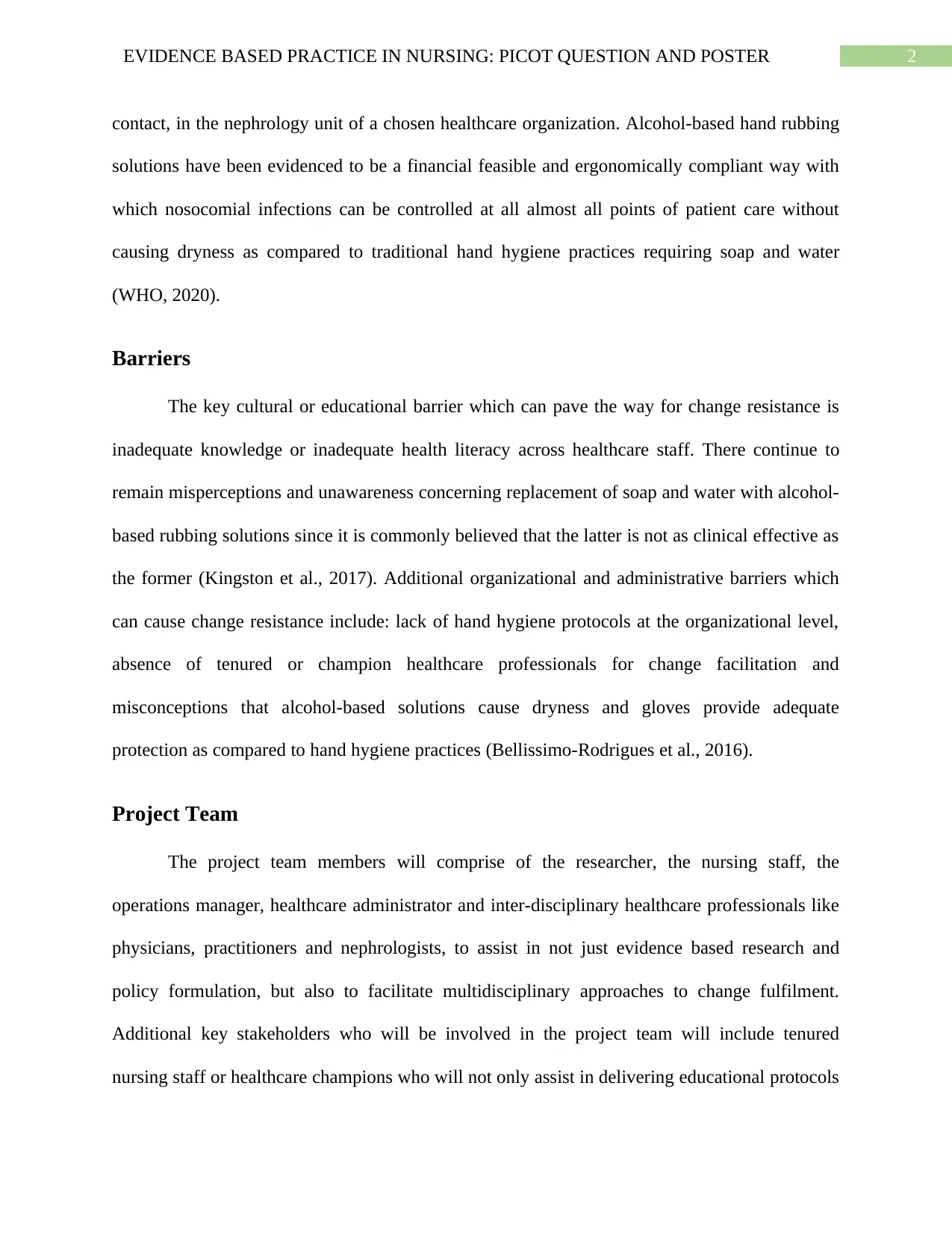
2EVIDENCE BASED PRACTICE IN NURSING: PICOT QUESTION AND POSTER
contact, in the nephrology unit of a chosen healthcare organization. Alcohol-based hand rubbing
solutions have been evidenced to be a financial feasible and ergonomically compliant way with
which nosocomial infections can be controlled at all almost all points of patient care without
causing dryness as compared to traditional hand hygiene practices requiring soap and water
(WHO, 2020).
Barriers
The key cultural or educational barrier which can pave the way for change resistance is
inadequate knowledge or inadequate health literacy across healthcare staff. There continue to
remain misperceptions and unawareness concerning replacement of soap and water with alcohol-
based rubbing solutions since it is commonly believed that the latter is not as clinical effective as
the former (Kingston et al., 2017). Additional organizational and administrative barriers which
can cause change resistance include: lack of hand hygiene protocols at the organizational level,
absence of tenured or champion healthcare professionals for change facilitation and
misconceptions that alcohol-based solutions cause dryness and gloves provide adequate
protection as compared to hand hygiene practices (Bellissimo-Rodrigues et al., 2016).
Project Team
The project team members will comprise of the researcher, the nursing staff, the
operations manager, healthcare administrator and inter-disciplinary healthcare professionals like
physicians, practitioners and nephrologists, to assist in not just evidence based research and
policy formulation, but also to facilitate multidisciplinary approaches to change fulfilment.
Additional key stakeholders who will be involved in the project team will include tenured
nursing staff or healthcare champions who will not only assist in delivering educational protocols
contact, in the nephrology unit of a chosen healthcare organization. Alcohol-based hand rubbing
solutions have been evidenced to be a financial feasible and ergonomically compliant way with
which nosocomial infections can be controlled at all almost all points of patient care without
causing dryness as compared to traditional hand hygiene practices requiring soap and water
(WHO, 2020).
Barriers
The key cultural or educational barrier which can pave the way for change resistance is
inadequate knowledge or inadequate health literacy across healthcare staff. There continue to
remain misperceptions and unawareness concerning replacement of soap and water with alcohol-
based rubbing solutions since it is commonly believed that the latter is not as clinical effective as
the former (Kingston et al., 2017). Additional organizational and administrative barriers which
can cause change resistance include: lack of hand hygiene protocols at the organizational level,
absence of tenured or champion healthcare professionals for change facilitation and
misconceptions that alcohol-based solutions cause dryness and gloves provide adequate
protection as compared to hand hygiene practices (Bellissimo-Rodrigues et al., 2016).
Project Team
The project team members will comprise of the researcher, the nursing staff, the
operations manager, healthcare administrator and inter-disciplinary healthcare professionals like
physicians, practitioners and nephrologists, to assist in not just evidence based research and
policy formulation, but also to facilitate multidisciplinary approaches to change fulfilment.
Additional key stakeholders who will be involved in the project team will include tenured
nursing staff or healthcare champions who will not only assist in delivering educational protocols
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
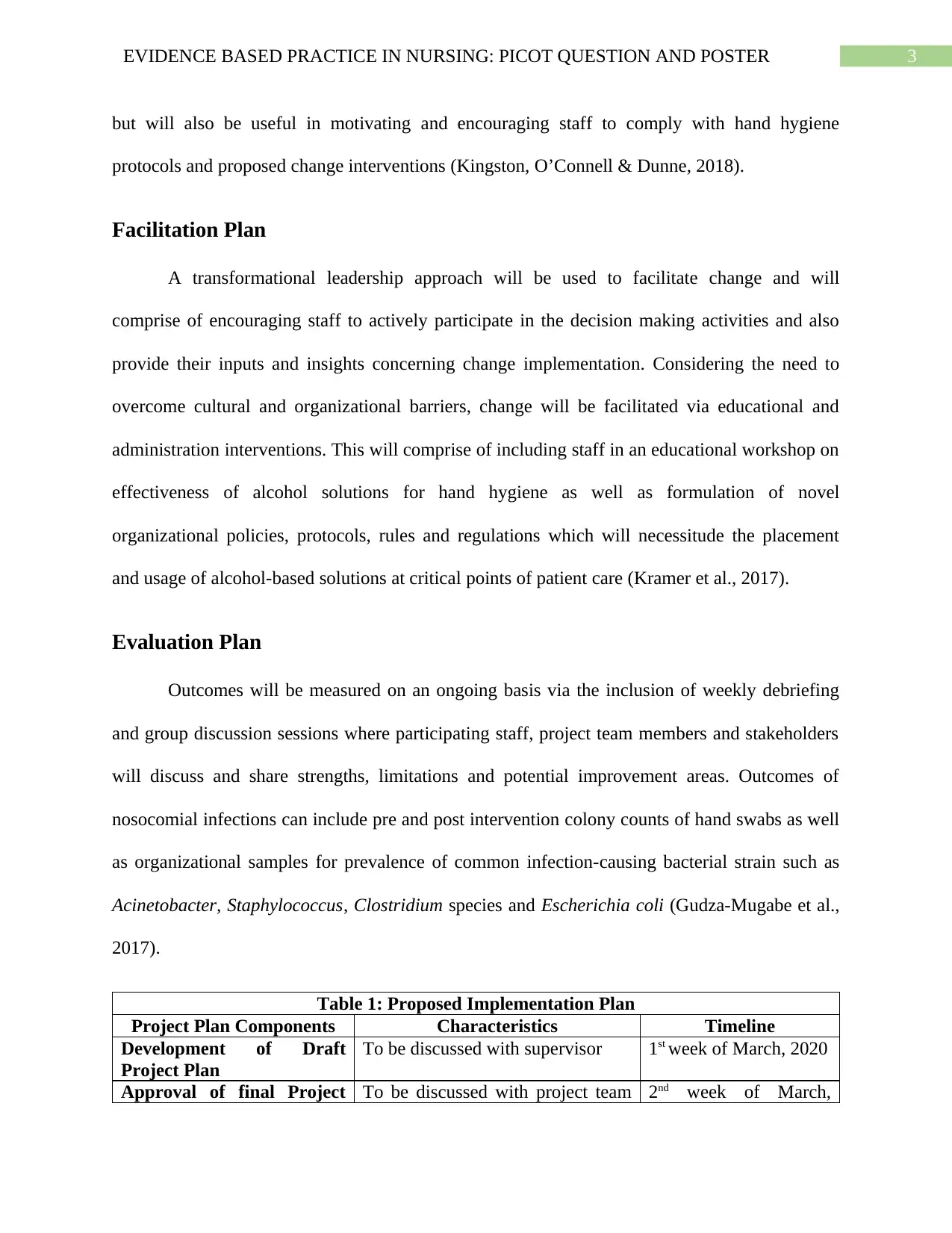
3EVIDENCE BASED PRACTICE IN NURSING: PICOT QUESTION AND POSTER
but will also be useful in motivating and encouraging staff to comply with hand hygiene
protocols and proposed change interventions (Kingston, O’Connell & Dunne, 2018).
Facilitation Plan
A transformational leadership approach will be used to facilitate change and will
comprise of encouraging staff to actively participate in the decision making activities and also
provide their inputs and insights concerning change implementation. Considering the need to
overcome cultural and organizational barriers, change will be facilitated via educational and
administration interventions. This will comprise of including staff in an educational workshop on
effectiveness of alcohol solutions for hand hygiene as well as formulation of novel
organizational policies, protocols, rules and regulations which will necessitude the placement
and usage of alcohol-based solutions at critical points of patient care (Kramer et al., 2017).
Evaluation Plan
Outcomes will be measured on an ongoing basis via the inclusion of weekly debriefing
and group discussion sessions where participating staff, project team members and stakeholders
will discuss and share strengths, limitations and potential improvement areas. Outcomes of
nosocomial infections can include pre and post intervention colony counts of hand swabs as well
as organizational samples for prevalence of common infection-causing bacterial strain such as
Acinetobacter, Staphylococcus, Clostridium species and Escherichia coli (Gudza-Mugabe et al.,
2017).
Table 1: Proposed Implementation Plan
Project Plan Components Characteristics Timeline
Development of Draft
Project Plan
To be discussed with supervisor 1st week of March, 2020
Approval of final Project To be discussed with project team 2nd week of March,
but will also be useful in motivating and encouraging staff to comply with hand hygiene
protocols and proposed change interventions (Kingston, O’Connell & Dunne, 2018).
Facilitation Plan
A transformational leadership approach will be used to facilitate change and will
comprise of encouraging staff to actively participate in the decision making activities and also
provide their inputs and insights concerning change implementation. Considering the need to
overcome cultural and organizational barriers, change will be facilitated via educational and
administration interventions. This will comprise of including staff in an educational workshop on
effectiveness of alcohol solutions for hand hygiene as well as formulation of novel
organizational policies, protocols, rules and regulations which will necessitude the placement
and usage of alcohol-based solutions at critical points of patient care (Kramer et al., 2017).
Evaluation Plan
Outcomes will be measured on an ongoing basis via the inclusion of weekly debriefing
and group discussion sessions where participating staff, project team members and stakeholders
will discuss and share strengths, limitations and potential improvement areas. Outcomes of
nosocomial infections can include pre and post intervention colony counts of hand swabs as well
as organizational samples for prevalence of common infection-causing bacterial strain such as
Acinetobacter, Staphylococcus, Clostridium species and Escherichia coli (Gudza-Mugabe et al.,
2017).
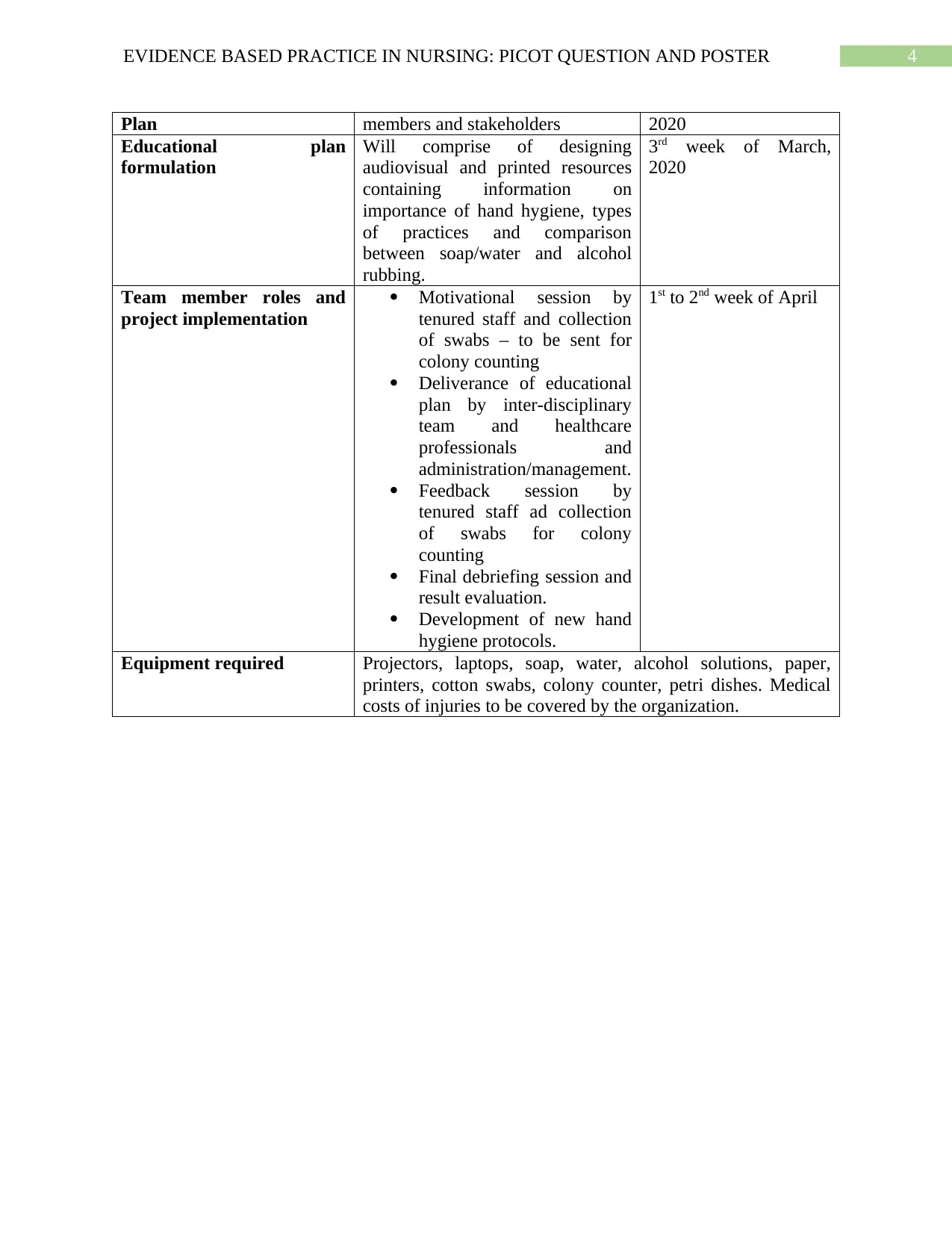
Table 1: Proposed Implementation Plan
Project Plan Components Characteristics Timeline
Development of Draft
Project Plan
To be discussed with supervisor 1st week of March, 2020
Approval of final Project To be discussed with project team 2nd week of March,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4EVIDENCE BASED PRACTICE IN NURSING: PICOT QUESTION AND POSTER
Plan members and stakeholders 2020
Educational plan
formulation
Will comprise of designing
audiovisual and printed resources
containing information on
importance of hand hygiene, types
of practices and comparison
between soap/water and alcohol
rubbing.
3rd week of March,
2020
Team member roles and
project implementation
Motivational session by
tenured staff and collection
of swabs – to be sent for
colony counting
Deliverance of educational
plan by inter-disciplinary
team and healthcare
professionals and
administration/management.
Feedback session by
tenured staff ad collection
of swabs for colony
counting
Final debriefing session and
result evaluation.
Development of new hand
hygiene protocols.
1st to 2nd week of April
Equipment required Projectors, laptops, soap, water, alcohol solutions, paper,
printers, cotton swabs, colony counter, petri dishes. Medical
costs of injuries to be covered by the organization.
Plan members and stakeholders 2020
Educational plan
formulation
Will comprise of designing
audiovisual and printed resources
containing information on
importance of hand hygiene, types
of practices and comparison
between soap/water and alcohol
rubbing.
3rd week of March,
2020
Team member roles and
project implementation
Motivational session by
tenured staff and collection
of swabs – to be sent for
colony counting
Deliverance of educational
plan by inter-disciplinary
team and healthcare
professionals and
administration/management.
Feedback session by
tenured staff ad collection
of swabs for colony
counting
Final debriefing session and
result evaluation.
Development of new hand
hygiene protocols.
1st to 2nd week of April
Equipment required Projectors, laptops, soap, water, alcohol solutions, paper,
printers, cotton swabs, colony counter, petri dishes. Medical
costs of injuries to be covered by the organization.
5EVIDENCE BASED PRACTICE IN NURSING: PICOT QUESTION AND POSTER
References
Bellissimo-Rodrigues, F., Soule, H., Gayet-Ageron, A., Martin, Y., & Pittet, D. (2016). Should
alcohol-based handrub use be customized to healthcare workers’ hand size?. infection
control & hospital epidemiology, 37(2), 219-221.
Gudza-Mugabe, M., Magwenzi, M. T., Mujuru, H. A., Bwakura-Dangarembizi, M., Robertson,
V., & Aiken, A. M. (2017). Effect of handrubbing using locally-manufactured alcohol-
based handrubs in paediatric wards in Harare, Zimbabwe. Antimicrobial Resistance &
Infection Control, 6(1), 8.
Kingston, L. M., O’Connell, N. H., & Dunne, C. P. (2018). A comparative study of hand hygiene
and alcohol-based hand rub use among Irish nursing and medical students. Nurse
education today, 63, 112-118.
Kingston, L. M., Slevin, B. L., O'Connell, N. H., & Dunne, C. P. (2017). Attitudes and practices
of Irish hospital-based physicians towards hand hygiene and hand rubbing using alcohol-
based hand rub: a comparison between 2007 and 2015. Journal of Hospital
Infection, 97(1), 17-25.
Kramer, A., Pittet, D., Klasinc, R., Krebs, S., Koburger, T., Fusch, C., & Assadian, O. (2017).
Shortening the application time of alcohol-based hand rubs to 15 seconds may improve
the frequency of hand antisepsis actions in a neonatal intensive care unit. infection
control & hospital epidemiology, 38(12), 1430-1434.
References
Bellissimo-Rodrigues, F., Soule, H., Gayet-Ageron, A., Martin, Y., & Pittet, D. (2016). Should
alcohol-based handrub use be customized to healthcare workers’ hand size?. infection
control & hospital epidemiology, 37(2), 219-221.
Gudza-Mugabe, M., Magwenzi, M. T., Mujuru, H. A., Bwakura-Dangarembizi, M., Robertson,
V., & Aiken, A. M. (2017). Effect of handrubbing using locally-manufactured alcohol-
based handrubs in paediatric wards in Harare, Zimbabwe. Antimicrobial Resistance &
Infection Control, 6(1), 8.
Kingston, L. M., O’Connell, N. H., & Dunne, C. P. (2018). A comparative study of hand hygiene
and alcohol-based hand rub use among Irish nursing and medical students. Nurse
education today, 63, 112-118.
Kingston, L. M., Slevin, B. L., O'Connell, N. H., & Dunne, C. P. (2017). Attitudes and practices
of Irish hospital-based physicians towards hand hygiene and hand rubbing using alcohol-
based hand rub: a comparison between 2007 and 2015. Journal of Hospital
Infection, 97(1), 17-25.
Kramer, A., Pittet, D., Klasinc, R., Krebs, S., Koburger, T., Fusch, C., & Assadian, O. (2017).
Shortening the application time of alcohol-based hand rubs to 15 seconds may improve
the frequency of hand antisepsis actions in a neonatal intensive care unit. infection
control & hospital epidemiology, 38(12), 1430-1434.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6EVIDENCE BASED PRACTICE IN NURSING: PICOT QUESTION AND POSTER
Pires, D., Soule, H., Bellissimo-Rodrigues, F., Gayet-Ageron, A., & Pittet, D. (2017). Hand
hygiene with alcohol-based hand rub: how long is long enough?. infection control &
hospital epidemiology, 38(5), 547-552.
WHO. (2020). WHO | System change - changing hand hygiene behaviour at the point of care.
Retrieved 11 February 2020, from https://www.who.int/gpsc/tools/faqs/system_
change/en/.
Pires, D., Soule, H., Bellissimo-Rodrigues, F., Gayet-Ageron, A., & Pittet, D. (2017). Hand
hygiene with alcohol-based hand rub: how long is long enough?. infection control &
hospital epidemiology, 38(5), 547-552.
WHO. (2020). WHO | System change - changing hand hygiene behaviour at the point of care.
Retrieved 11 February 2020, from https://www.who.int/gpsc/tools/faqs/system_
change/en/.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





