Establishing Primary Healthcare for Mentally Ill Individuals: A Study
VerifiedAdded on 2022/12/30
|14
|3345
|1
Essay
AI Summary
This essay critically examines the establishment of effective primary health care for mentally ill individuals. It begins with an introduction highlighting the importance of primary health care and the specific challenges faced by the mentally ill in accessing it. The essay poses a research question, outlines the search strategy used to gather relevant literature from databases such as PubMed and Medline, and summarizes key findings from selected studies. The analysis focuses on the integration of mental health into primary care, the importance of addressing health conditions of the mentally ill, and the impact of stigma. The essay also includes a critical review of the methodologies employed in the studies, discussing their strengths, limitations, and recommendations for improved healthcare practices. The findings emphasize the need to address the unique vulnerabilities of mentally ill individuals and advocate for their equal access to primary health care. Appraisal tools are provided to assess the quality of the articles reviewed. The conclusion highlights the importance of primary health care access for mentally ill individuals.

Running head: ESSAY AND A CRITICAL APPRAISAL 1
Establishment of the effective primary health care among the mentally ill individuals
Student’s Name
Institutional Affiliation
Establishment of the effective primary health care among the mentally ill individuals
Student’s Name
Institutional Affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ESSAY AND A CRITICAL APPRAISAL 2
Title: Establishment of the effective primary health care among the mentally ill individuals
Introduction
Primary health care is a basic component that averagely should be the baseline of every
individual that has an encounter with the physical environment every day. A significant number
of individuals who are mentally ill most often lack the capability of recognizing what is
appropriate and what is inappropriate to do, therefore when it comes to their basic primary
health, there are a lot of issues that if not addressed by a normal person they might find
themselves into serious health problems and risks. Overtime there has been assumption by
various people concerning the state of health of the mentally ill or those with mental disorders.
Mentally ill individuals hardly find an experience in achieving basic hygiene. It is important
therefore to recognize that the mentally ill individuals are also people just like the normal people
who deserve basic right to proper health care. There is a great need to establish proper and
appropriate mechanisms that will enhance achievement of the primary health care services
among the individuals who are mentally ill.
Search question
How can primary health be achieved among the mentally ill individuals?
Search Summary
A search through online was carried out in PubMed, Medline, mental hospital database of
metanalysis reviews. The strategy for the search involved the resulting vital notions based on the
question under the research: primary health care, mental illness and wellbeing of the mentally ill.
Search terms and key words were identified by the help of search fields of abstract and by
inserting the key word into google scholar ad explored on the subject heading. Truncating,
Title: Establishment of the effective primary health care among the mentally ill individuals
Introduction
Primary health care is a basic component that averagely should be the baseline of every
individual that has an encounter with the physical environment every day. A significant number
of individuals who are mentally ill most often lack the capability of recognizing what is
appropriate and what is inappropriate to do, therefore when it comes to their basic primary
health, there are a lot of issues that if not addressed by a normal person they might find
themselves into serious health problems and risks. Overtime there has been assumption by
various people concerning the state of health of the mentally ill or those with mental disorders.
Mentally ill individuals hardly find an experience in achieving basic hygiene. It is important
therefore to recognize that the mentally ill individuals are also people just like the normal people
who deserve basic right to proper health care. There is a great need to establish proper and
appropriate mechanisms that will enhance achievement of the primary health care services
among the individuals who are mentally ill.
Search question
How can primary health be achieved among the mentally ill individuals?
Search Summary
A search through online was carried out in PubMed, Medline, mental hospital database of
metanalysis reviews. The strategy for the search involved the resulting vital notions based on the
question under the research: primary health care, mental illness and wellbeing of the mentally ill.
Search terms and key words were identified by the help of search fields of abstract and by
inserting the key word into google scholar ad explored on the subject heading. Truncating,
ESSAY AND A CRITICAL APPRAISAL 3
paraphrasing and repetitive search were used to in accordance to each database. Studies were
from across the world as there are those that compare the countries state of technological and
health advancement regardless of whether it is a developed or a developing nation. The studies
were also limited to those in English and published since 2015 with the focus on human, nursing,
social and medicinal sciences and applied randomized controlled trail method. A total over
approximately 200 probable related online materials were found. After sieving and removing the
unwanted papers that had no information that was required, were eliminated remaining with only
15 randomized measured trials that were gone through and analyzed critically.
Summary of the evidence
The studies were analyzed based on two components: one, primary healthcare and two
mental illness. The two components were very essential in determining different healthcare
activities among the mentally ill individuals. The two key terms called for critical analysis using
the same key terms. The interventional studies that only focused on primary health care among
the mentally ill individuals include: Lund, Tomlinson and Patel (2016); Crowley and Kirschner
(2015) and lastly Thornicroft Deb and Henderson (2016). The two studies were effective in
increasing knowledge on the general state of the mentally ill locally and globally to gain an
understanding that there are substantial number of groups of people along all the tribal lines ad
transactional orientation in describing that the mentally ill are a people that that deserves to enjoy
life on earth and they are meant to also live the life that other normal people are supposed to live.
In the randomized controlled trial of Thornicroft Deb and Henderson (2016), they provide a total
number of 90 countries worldwide that have had experiences with primary health care among the
mentally ill. Most individuals in the world who have mental illnesses receive no treatments.
Lund, Tomlinson and Patel (2016) outlines the development of the health care plans by the
paraphrasing and repetitive search were used to in accordance to each database. Studies were
from across the world as there are those that compare the countries state of technological and
health advancement regardless of whether it is a developed or a developing nation. The studies
were also limited to those in English and published since 2015 with the focus on human, nursing,
social and medicinal sciences and applied randomized controlled trail method. A total over
approximately 200 probable related online materials were found. After sieving and removing the
unwanted papers that had no information that was required, were eliminated remaining with only
15 randomized measured trials that were gone through and analyzed critically.
Summary of the evidence
The studies were analyzed based on two components: one, primary healthcare and two
mental illness. The two components were very essential in determining different healthcare
activities among the mentally ill individuals. The two key terms called for critical analysis using
the same key terms. The interventional studies that only focused on primary health care among
the mentally ill individuals include: Lund, Tomlinson and Patel (2016); Crowley and Kirschner
(2015) and lastly Thornicroft Deb and Henderson (2016). The two studies were effective in
increasing knowledge on the general state of the mentally ill locally and globally to gain an
understanding that there are substantial number of groups of people along all the tribal lines ad
transactional orientation in describing that the mentally ill are a people that that deserves to enjoy
life on earth and they are meant to also live the life that other normal people are supposed to live.
In the randomized controlled trial of Thornicroft Deb and Henderson (2016), they provide a total
number of 90 countries worldwide that have had experiences with primary health care among the
mentally ill. Most individuals in the world who have mental illnesses receive no treatments.
Lund, Tomlinson and Patel (2016) outlines the development of the health care plans by the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ESSAY AND A CRITICAL APPRAISAL 4
district in ensuring mental health care plans among the five low and middle-income countries
together with the design methods, coating and evaluation. Crowley and Kirschner (2015)
considers the importance of the health care system in succinctly addressing health condition of
the mentally ill. They also state that factors and concerns of health among the mentally ill
including the awareness of the prospects individuals is essential even if they are mentally ill and
are unable to recognize their rights. There is agreat need to stand with them and for them, they
have sometimes no voice. Nevertheless, the results did not get to the statistical significance
(p=0.12) showing lack of effectiveness of the health intervention.
Key Terms
Mentally ill: refers to an individual who has developed abnormality in the way they think
such that they are less developed and less in thinking properly to come to a concise judgment.
Primary health care: it refers to the basic health that an average person can afford to get access to
through the aid of the concerned parties or stakeholders in the community.
Critical review
The general quality of the methodology of the three were generally good. All the studies
included contained actual random distribution to the groups of individuals mentally ill, they all
had analogous groups at the entry and performed equivalent assessment of the similar group in
the same way hence making them the amazing studies for determining the trends in mental
health across the world and the nation (Zeanah, 2018). Both sides utilize and makes use of the
available studies, reports and the surveys on the integration of the health behavioral in primary
health care from PubMed, google scholar, web sites and policy documents. Recommendations
were vastly based on the different board of governance and the assisted health care professional’s
district in ensuring mental health care plans among the five low and middle-income countries
together with the design methods, coating and evaluation. Crowley and Kirschner (2015)
considers the importance of the health care system in succinctly addressing health condition of
the mentally ill. They also state that factors and concerns of health among the mentally ill
including the awareness of the prospects individuals is essential even if they are mentally ill and
are unable to recognize their rights. There is agreat need to stand with them and for them, they
have sometimes no voice. Nevertheless, the results did not get to the statistical significance
(p=0.12) showing lack of effectiveness of the health intervention.
Key Terms
Mentally ill: refers to an individual who has developed abnormality in the way they think
such that they are less developed and less in thinking properly to come to a concise judgment.
Primary health care: it refers to the basic health that an average person can afford to get access to
through the aid of the concerned parties or stakeholders in the community.
Critical review
The general quality of the methodology of the three were generally good. All the studies
included contained actual random distribution to the groups of individuals mentally ill, they all
had analogous groups at the entry and performed equivalent assessment of the similar group in
the same way hence making them the amazing studies for determining the trends in mental
health across the world and the nation (Zeanah, 2018). Both sides utilize and makes use of the
available studies, reports and the surveys on the integration of the health behavioral in primary
health care from PubMed, google scholar, web sites and policy documents. Recommendations
were vastly based on the different board of governance and the assisted health care professional’s
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ESSAY AND A CRITICAL APPRAISAL 5
stakeholders (Thompson, Anisimowicz, Miedema, Hogg, Wodchis & Aubrey-Bassler, 2016).
The policy papers and the policy committee on studies had financial funding aspect of the
development of the different projects.
Strengths and limitations of the evidence
Assumption by different kind of people and individual that mentally ill individuals do not
need much attention to primary health care is evident throughout all studies. The studies have it
that there is no consideration of mentally ill individuals regarding primary health care. (Liu,
Daumit, Dua, Aquila, Charlson, Cuijpers... & Gaebel, 2017). The mentally ill people ae not
considered to be normal therefore no social attention is given to what they eat and intercept the
family members but even them, they have limited access to making their loved ones feel the
sense of belonging in their sate of mental illness.
Despite the extended literature however, the systematic review is aiming at giving a
report on the effectiveness of interventions to increase more care and promotion of primary
health care among the mentally ill to increase the use of the available resources for handling and
keeping them safe regardless of where they are. It could be that they are in a prison, it is also
necessary to follow the systematic review and promote primary health care services among the
mentally disordered individuals (Demarzo, Montero-Marin, Cuijpers, Zabaleta-del-Olmo,
Mahtani, Vellinga... & García-Campayo, 2015).
Considering the appropriateness of the intervention, they are all likely to promote and
bring about changes and the desired outcome of the question at the beginning of the paper. There
is one review however by Crowley and Kirschner (2015) that cases a whole new thing in terms
of reproduction and the general wellbeing of the individual with mental illness. Well known
stakeholders (Thompson, Anisimowicz, Miedema, Hogg, Wodchis & Aubrey-Bassler, 2016).
The policy papers and the policy committee on studies had financial funding aspect of the
development of the different projects.
Strengths and limitations of the evidence
Assumption by different kind of people and individual that mentally ill individuals do not
need much attention to primary health care is evident throughout all studies. The studies have it
that there is no consideration of mentally ill individuals regarding primary health care. (Liu,
Daumit, Dua, Aquila, Charlson, Cuijpers... & Gaebel, 2017). The mentally ill people ae not
considered to be normal therefore no social attention is given to what they eat and intercept the
family members but even them, they have limited access to making their loved ones feel the
sense of belonging in their sate of mental illness.
Despite the extended literature however, the systematic review is aiming at giving a
report on the effectiveness of interventions to increase more care and promotion of primary
health care among the mentally ill to increase the use of the available resources for handling and
keeping them safe regardless of where they are. It could be that they are in a prison, it is also
necessary to follow the systematic review and promote primary health care services among the
mentally disordered individuals (Demarzo, Montero-Marin, Cuijpers, Zabaleta-del-Olmo,
Mahtani, Vellinga... & García-Campayo, 2015).
Considering the appropriateness of the intervention, they are all likely to promote and
bring about changes and the desired outcome of the question at the beginning of the paper. There
is one review however by Crowley and Kirschner (2015) that cases a whole new thing in terms
of reproduction and the general wellbeing of the individual with mental illness. Well known
ESSAY AND A CRITICAL APPRAISAL 6
leading factors to interventions are all calling and advocating for the first-time involvement of
the people in matters concerning the wellbeing of the mentally ill. There should also be outer
concern by individuals keeping it in mind that the mentally impaired have a slow personal role to
play in these societies, therefore they all require equal treatment like other people; in this case
the equal treatment is the equal access to primary health care. The educators and the trainers of
the public great should stand out and advocate for the rights of the mentally impaired.
Nevertheless, the system review had a few limitations. One of the limitation is that the
publications themselves are recent however there is a lot of quoting and referring to old
traditional examples that might have contained biasness because the way mentally ill were
regarded and treated in the past is not how they are treated today. Another limitation is that there
was a small number of trials of inclusion and random estimation. Not every RCT reported every
outcome of concern.
Impact
This review provides evidence that can be used as the benchmark for the establishment of
the provisions for medical performance. In one accord with the national and the international
agencies concerning the treatment and provision of the basic primary health care to then that
have a disorder of the mind. There are also some evidences that concentrating and dwelling so
much on providing primary health care to the mentally ill will be a waste of time and resources
(Happell, Ewart, Platania‐Phung & Stanton, 2016). There is also another evidence that societies
are making the efforts to address various complexities of providing the health care to individuals
might be involving and at the end it all there will be nothing to celebrate (Demarzo et al., 2015).
Synthesis
leading factors to interventions are all calling and advocating for the first-time involvement of
the people in matters concerning the wellbeing of the mentally ill. There should also be outer
concern by individuals keeping it in mind that the mentally impaired have a slow personal role to
play in these societies, therefore they all require equal treatment like other people; in this case
the equal treatment is the equal access to primary health care. The educators and the trainers of
the public great should stand out and advocate for the rights of the mentally impaired.
Nevertheless, the system review had a few limitations. One of the limitation is that the
publications themselves are recent however there is a lot of quoting and referring to old
traditional examples that might have contained biasness because the way mentally ill were
regarded and treated in the past is not how they are treated today. Another limitation is that there
was a small number of trials of inclusion and random estimation. Not every RCT reported every
outcome of concern.
Impact
This review provides evidence that can be used as the benchmark for the establishment of
the provisions for medical performance. In one accord with the national and the international
agencies concerning the treatment and provision of the basic primary health care to then that
have a disorder of the mind. There are also some evidences that concentrating and dwelling so
much on providing primary health care to the mentally ill will be a waste of time and resources
(Happell, Ewart, Platania‐Phung & Stanton, 2016). There is also another evidence that societies
are making the efforts to address various complexities of providing the health care to individuals
might be involving and at the end it all there will be nothing to celebrate (Demarzo et al., 2015).
Synthesis
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ESSAY AND A CRITICAL APPRAISAL 7
The findings show that stigma and discrimination regarding mental illnesses have been
described as comprising of so many consequences than the conditions themselves (Stenius-
Ayoade, Haaramo, Erkkilä, Marola, Nousiainen, Wahlbeck, & Eriksson, 2017). Most of the
related, medical researches concerning mental illness have been concentrating more on the
attitude that the people have towards the people with mental disorders than what people can do to
ease or rather promote the wellbeing of the mentally ill (Scott, Lim, Al-Hamzawi, Alonso,
Bruffaerts, Caldas-de-Almeida... & Kawakami, 2016). It is also coming out clearly that
transgender youth represents a population that is vulnerable to the risk for negative mental health
results including ‘depression, self-harm and suicidality’ (Sheehan, Hassiotis, Walters, Osborn,
Strydom, & Horsfall, 2015. The amount of data concerning this group of individuals is limited in
this group of individuals from the setting of the community including the comparative data that
determines differences in the outcomes of the mental illness (Crowley & Kirschner, 2015);
(Pedrelli, Nyer, Yeung, Zulauf, & Wilens, 2015); (Patel, Weobong, Weiss, Anand, Bhat, Katti...
& Vijayakumar, 2017). Different mentally ill patient has negative differences compared to other
group of people having equally high burden for the young (Moore, Shiers, Daly, Mitchell &
Gaughran, 2015). In concluding, it is also coming out evidently that clinicals that serve the trans
gender youth should perform content screening of the mental health outcomes but as they do
they must also have the consideration that there is need to address the primary health care among
the mentally ill individuals. These individuals are also vulnerable to illnesses and diseases
associated with ignorance on primary health care (Coventry, Lovell, Dickens, Bower, Chew-
Graham, C., McElvenny... & Baguley, 2015).
The findings show that stigma and discrimination regarding mental illnesses have been
described as comprising of so many consequences than the conditions themselves (Stenius-
Ayoade, Haaramo, Erkkilä, Marola, Nousiainen, Wahlbeck, & Eriksson, 2017). Most of the
related, medical researches concerning mental illness have been concentrating more on the
attitude that the people have towards the people with mental disorders than what people can do to
ease or rather promote the wellbeing of the mentally ill (Scott, Lim, Al-Hamzawi, Alonso,
Bruffaerts, Caldas-de-Almeida... & Kawakami, 2016). It is also coming out clearly that
transgender youth represents a population that is vulnerable to the risk for negative mental health
results including ‘depression, self-harm and suicidality’ (Sheehan, Hassiotis, Walters, Osborn,
Strydom, & Horsfall, 2015. The amount of data concerning this group of individuals is limited in
this group of individuals from the setting of the community including the comparative data that
determines differences in the outcomes of the mental illness (Crowley & Kirschner, 2015);
(Pedrelli, Nyer, Yeung, Zulauf, & Wilens, 2015); (Patel, Weobong, Weiss, Anand, Bhat, Katti...
& Vijayakumar, 2017). Different mentally ill patient has negative differences compared to other
group of people having equally high burden for the young (Moore, Shiers, Daly, Mitchell &
Gaughran, 2015). In concluding, it is also coming out evidently that clinicals that serve the trans
gender youth should perform content screening of the mental health outcomes but as they do
they must also have the consideration that there is need to address the primary health care among
the mentally ill individuals. These individuals are also vulnerable to illnesses and diseases
associated with ignorance on primary health care (Coventry, Lovell, Dickens, Bower, Chew-
Graham, C., McElvenny... & Baguley, 2015).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ESSAY AND A CRITICAL APPRAISAL 8
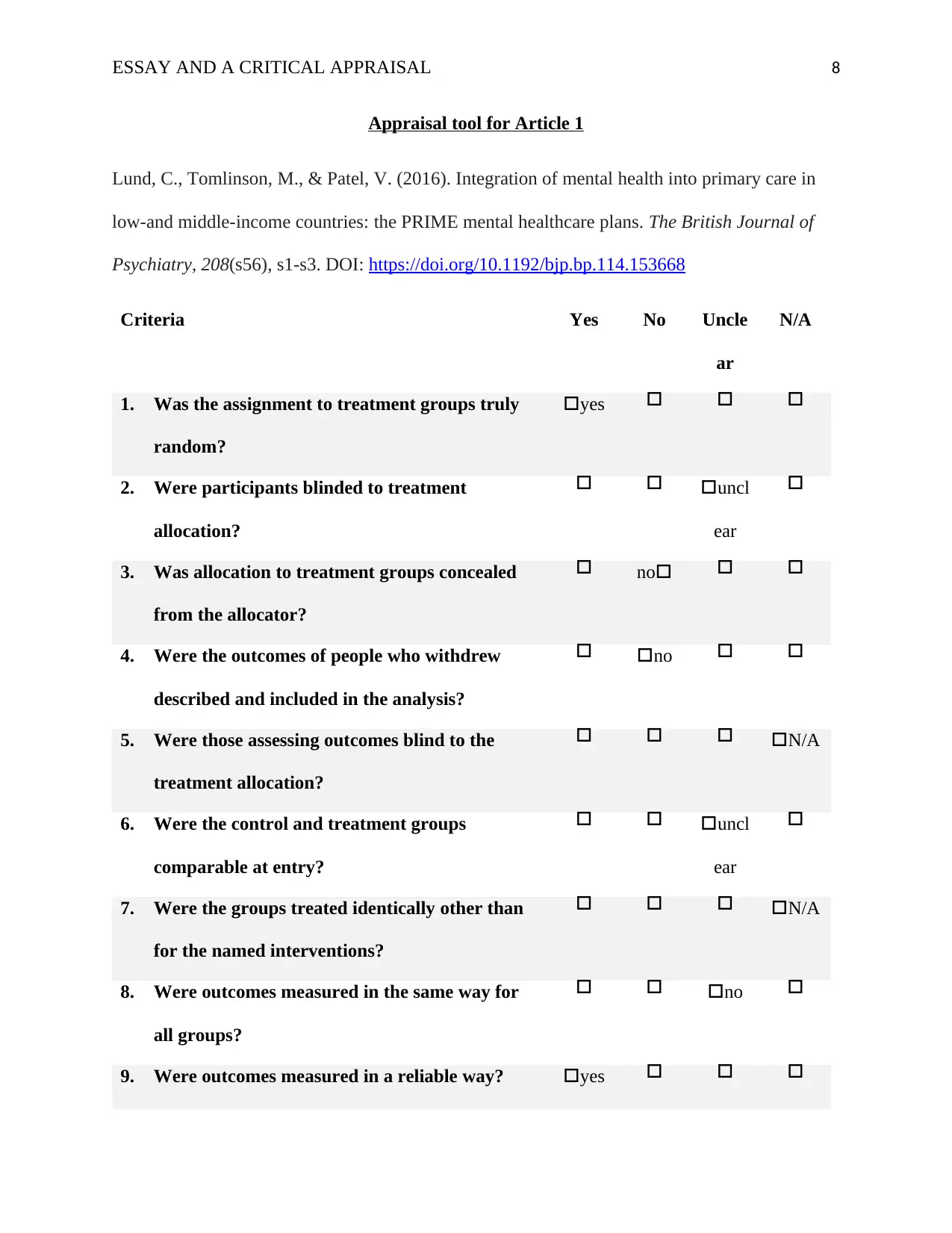
Appraisal tool for Article 1
Lund, C., Tomlinson, M., & Patel, V. (2016). Integration of mental health into primary care in
low-and middle-income countries: the PRIME mental healthcare plans. The British Journal of
Psychiatry, 208(s56), s1-s3. DOI: https://doi.org/10.1192/bjp.bp.114.153668
Criteria Yes No Uncle
ar
N/A
1. Was the assignment to treatment groups truly
random?
yes
2. Were participants blinded to treatment
allocation?
uncl
ear
3. Was allocation to treatment groups concealed
from the allocator?
no
4. Were the outcomes of people who withdrew
described and included in the analysis?
no
5. Were those assessing outcomes blind to the
treatment allocation?
N/A
6. Were the control and treatment groups
comparable at entry?
uncl
ear
7. Were the groups treated identically other than
for the named interventions?
N/A
8. Were outcomes measured in the same way for
all groups?
no
9. Were outcomes measured in a reliable way? yes
Appraisal tool for Article 1
Lund, C., Tomlinson, M., & Patel, V. (2016). Integration of mental health into primary care in
low-and middle-income countries: the PRIME mental healthcare plans. The British Journal of
Psychiatry, 208(s56), s1-s3. DOI: https://doi.org/10.1192/bjp.bp.114.153668
Criteria Yes No Uncle
ar
N/A
1. Was the assignment to treatment groups truly
random?
yes
2. Were participants blinded to treatment
allocation?
uncl
ear
3. Was allocation to treatment groups concealed
from the allocator?
no
4. Were the outcomes of people who withdrew
described and included in the analysis?
no
5. Were those assessing outcomes blind to the
treatment allocation?
N/A
6. Were the control and treatment groups
comparable at entry?
uncl
ear
7. Were the groups treated identically other than
for the named interventions?
N/A
8. Were outcomes measured in the same way for
all groups?
no
9. Were outcomes measured in a reliable way? yes
ESSAY AND A CRITICAL APPRAISAL 9
10. Was appropriate statistical analysis used? yes
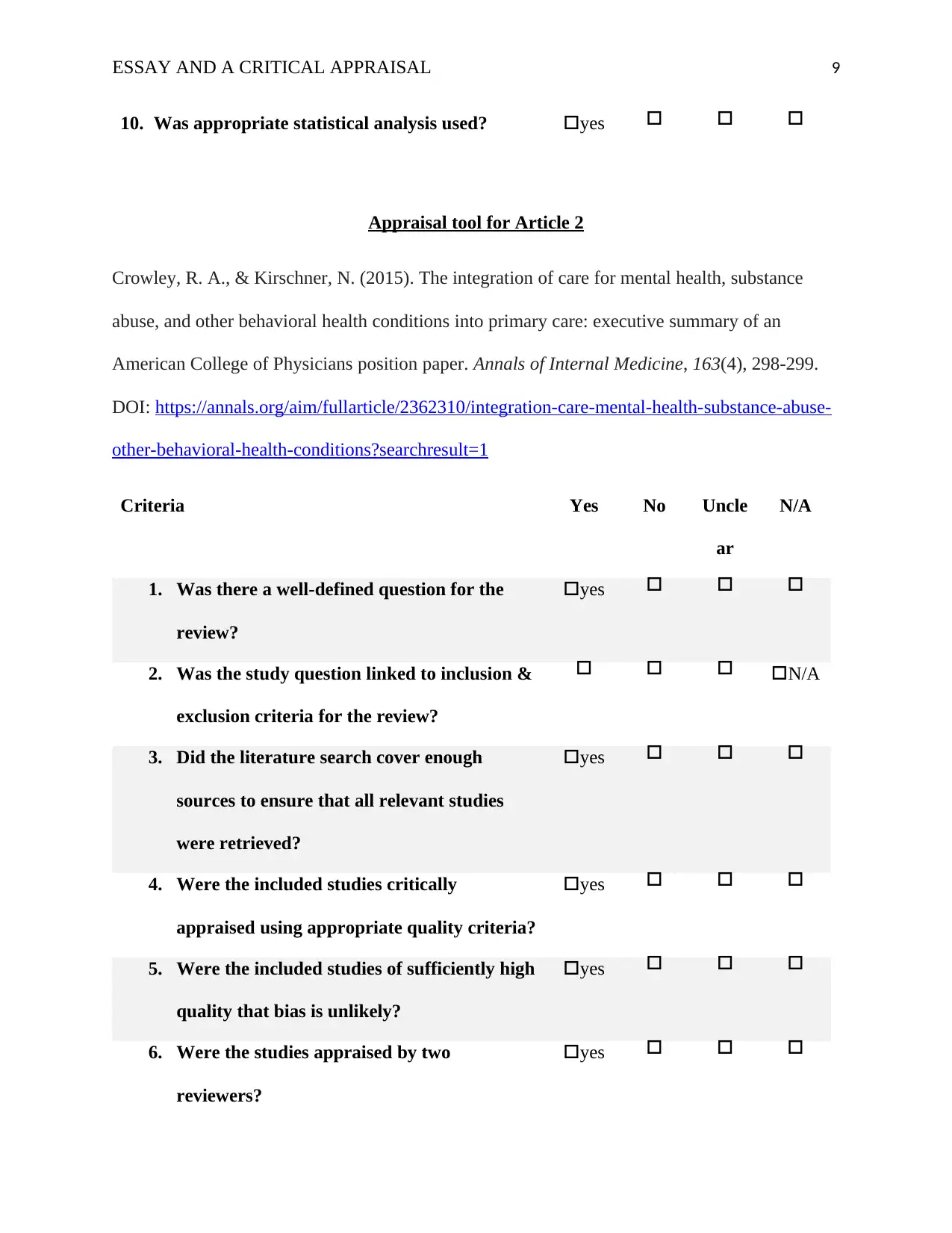
Appraisal tool for Article 2
Crowley, R. A., & Kirschner, N. (2015). The integration of care for mental health, substance
abuse, and other behavioral health conditions into primary care: executive summary of an
American College of Physicians position paper. Annals of Internal Medicine, 163(4), 298-299.
DOI: https://annals.org/aim/fullarticle/2362310/integration-care-mental-health-substance-abuse-
other-behavioral-health-conditions?searchresult=1
Criteria Yes No Uncle
ar
N/A
1. Was there a well-defined question for the
review?
yes
2. Was the study question linked to inclusion &
exclusion criteria for the review?
N/A
3. Did the literature search cover enough
sources to ensure that all relevant studies
were retrieved?
yes
4. Were the included studies critically
appraised using appropriate quality criteria?
yes
5. Were the included studies of sufficiently high
quality that bias is unlikely?
yes
6. Were the studies appraised by two
reviewers?
yes
10. Was appropriate statistical analysis used? yes
Appraisal tool for Article 2
Crowley, R. A., & Kirschner, N. (2015). The integration of care for mental health, substance
abuse, and other behavioral health conditions into primary care: executive summary of an
American College of Physicians position paper. Annals of Internal Medicine, 163(4), 298-299.
DOI: https://annals.org/aim/fullarticle/2362310/integration-care-mental-health-substance-abuse-
other-behavioral-health-conditions?searchresult=1
Criteria Yes No Uncle
ar
N/A
1. Was there a well-defined question for the
review?
yes
2. Was the study question linked to inclusion &
exclusion criteria for the review?
N/A
3. Did the literature search cover enough
sources to ensure that all relevant studies
were retrieved?
yes
4. Were the included studies critically
appraised using appropriate quality criteria?
yes
5. Were the included studies of sufficiently high
quality that bias is unlikely?
yes
6. Were the studies appraised by two
reviewers?
yes
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
ESSAY AND A CRITICAL APPRAISAL 10
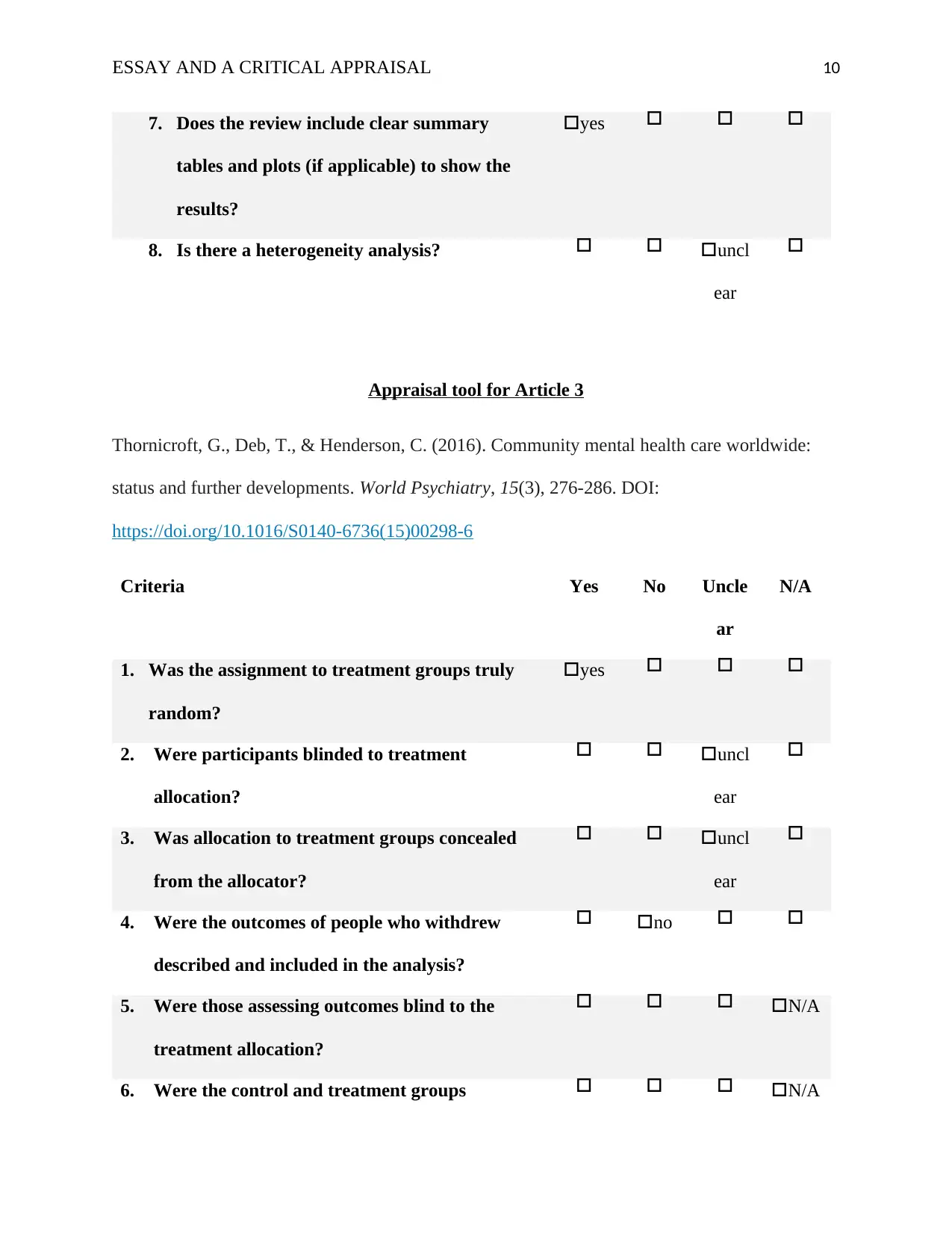
7. Does the review include clear summary
tables and plots (if applicable) to show the
results?
yes
8. Is there a heterogeneity analysis? uncl
ear
Appraisal tool for Article 3
Thornicroft, G., Deb, T., & Henderson, C. (2016). Community mental health care worldwide:
status and further developments. World Psychiatry, 15(3), 276-286. DOI:
https://doi.org/10.1016/S0140-6736(15)00298-6
Criteria Yes No Uncle
ar
N/A
1. Was the assignment to treatment groups truly
random?
yes
2. Were participants blinded to treatment
allocation?
uncl
ear
3. Was allocation to treatment groups concealed
from the allocator?
uncl
ear
4. Were the outcomes of people who withdrew
described and included in the analysis?
no
5. Were those assessing outcomes blind to the
treatment allocation?
N/A
6. Were the control and treatment groups N/A
7. Does the review include clear summary
tables and plots (if applicable) to show the
results?
yes
8. Is there a heterogeneity analysis? uncl
ear
Appraisal tool for Article 3
Thornicroft, G., Deb, T., & Henderson, C. (2016). Community mental health care worldwide:
status and further developments. World Psychiatry, 15(3), 276-286. DOI:
https://doi.org/10.1016/S0140-6736(15)00298-6
Criteria Yes No Uncle
ar
N/A
1. Was the assignment to treatment groups truly
random?
yes
2. Were participants blinded to treatment
allocation?
uncl
ear
3. Was allocation to treatment groups concealed
from the allocator?
uncl
ear
4. Were the outcomes of people who withdrew
described and included in the analysis?
no
5. Were those assessing outcomes blind to the
treatment allocation?
N/A
6. Were the control and treatment groups N/A
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
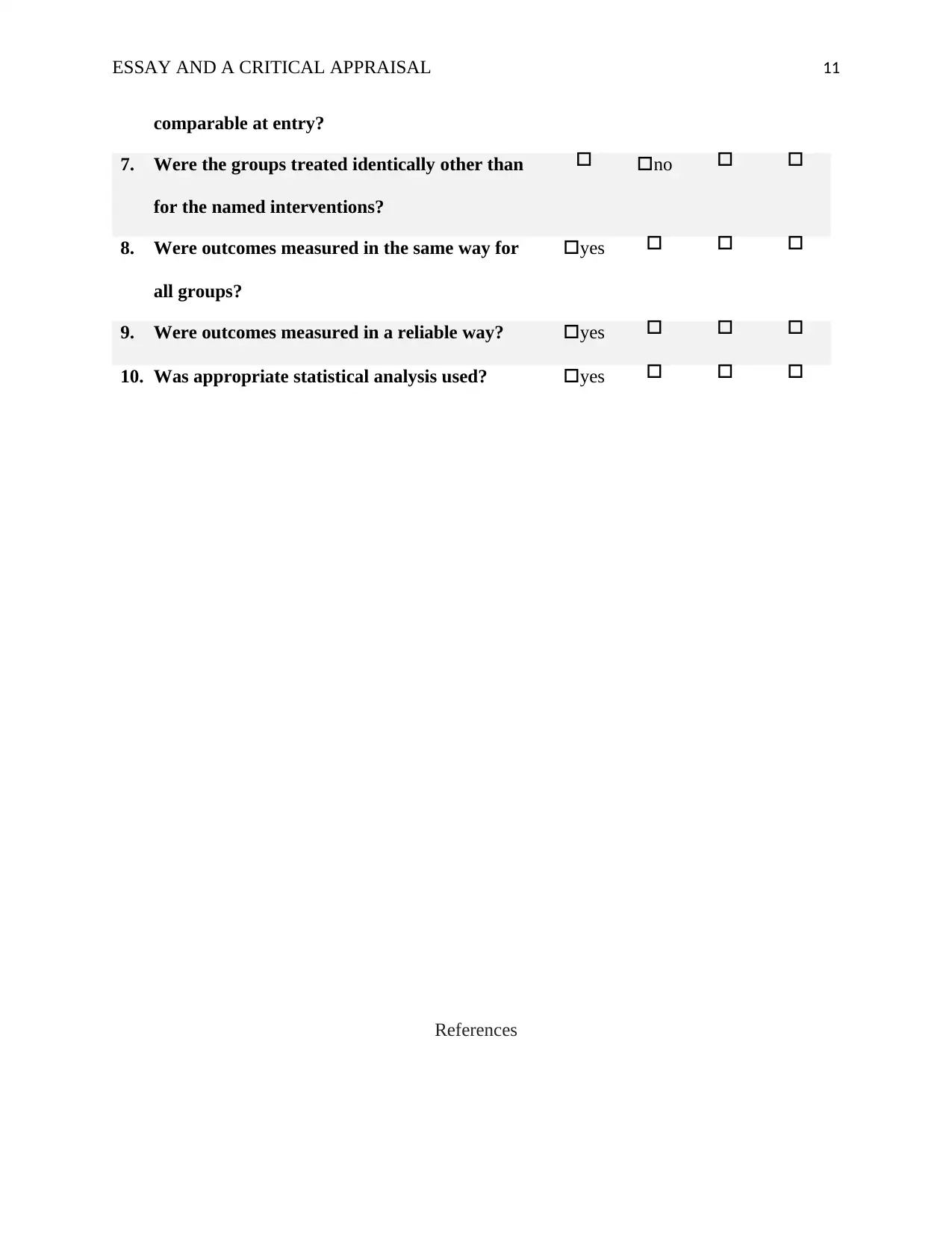
ESSAY AND A CRITICAL APPRAISAL 11
comparable at entry?
7. Were the groups treated identically other than
for the named interventions?
no
8. Were outcomes measured in the same way for
all groups?
yes
9. Were outcomes measured in a reliable way? yes
10. Was appropriate statistical analysis used? yes
References
comparable at entry?
7. Were the groups treated identically other than
for the named interventions?
no
8. Were outcomes measured in the same way for
all groups?
yes
9. Were outcomes measured in a reliable way? yes
10. Was appropriate statistical analysis used? yes
References
ESSAY AND A CRITICAL APPRAISAL 12
Coventry, P., Lovell, K., Dickens, C., Bower, P., Chew-Graham, C., McElvenny, D., ... &
Baguley, C. (2015). Integrated primary care for patients with mental and physical
multimorbidity: cluster randomised controlled trial of collaborative care for patients
with depression comorbid with diabetes or cardiovascular disease. bmj, 350, h638.
Crowley, R. A., & Kirschner, N. (2015). The integration of care for mental health, substance
abuse, and other behavioral health conditions into primary care: executive summary of
an American College of Physicians position paper. Annals of Internal
Medicine, 163(4), 298-299.
Demarzo, M. M., Montero-Marin, J., Cuijpers, P., Zabaleta-del-Olmo, E., Mahtani, K. R.,
Vellinga, A., ... & García-Campayo, J. (2015). The efficacy of mindfulness-based
interventions in primary care: a meta-analytic review. The Annals of Family
Medicine, 13(6), 573-582.
Happell, B., Ewart, S. B., Platania‐Phung, C., & Stanton, R. (2016). Participative mental health
consumer research for improving physical health care: An integrative
review. International journal of mental health nursing, 25(5), 399-408.
Liu, N. H., Daumit, G. L., Dua, T., Aquila, R., Charlson, F., Cuijpers, P., ... & Gaebel, W.
(2017). Excess mortality in persons with severe mental disorders: a multilevel
intervention framework and priorities for clinical practice, policy and research
agendas. World psychiatry, 16(1), 30-40.
Lund, C., Tomlinson, M., & Patel, V. (2016). Integration of mental health into primary care in
low-and middle-income countries: the PRIME mental healthcare plans. The British
Journal of Psychiatry, 208(s56), s1-s3.
Coventry, P., Lovell, K., Dickens, C., Bower, P., Chew-Graham, C., McElvenny, D., ... &
Baguley, C. (2015). Integrated primary care for patients with mental and physical
multimorbidity: cluster randomised controlled trial of collaborative care for patients
with depression comorbid with diabetes or cardiovascular disease. bmj, 350, h638.
Crowley, R. A., & Kirschner, N. (2015). The integration of care for mental health, substance
abuse, and other behavioral health conditions into primary care: executive summary of
an American College of Physicians position paper. Annals of Internal
Medicine, 163(4), 298-299.
Demarzo, M. M., Montero-Marin, J., Cuijpers, P., Zabaleta-del-Olmo, E., Mahtani, K. R.,
Vellinga, A., ... & García-Campayo, J. (2015). The efficacy of mindfulness-based
interventions in primary care: a meta-analytic review. The Annals of Family
Medicine, 13(6), 573-582.
Happell, B., Ewart, S. B., Platania‐Phung, C., & Stanton, R. (2016). Participative mental health
consumer research for improving physical health care: An integrative
review. International journal of mental health nursing, 25(5), 399-408.
Liu, N. H., Daumit, G. L., Dua, T., Aquila, R., Charlson, F., Cuijpers, P., ... & Gaebel, W.
(2017). Excess mortality in persons with severe mental disorders: a multilevel
intervention framework and priorities for clinical practice, policy and research
agendas. World psychiatry, 16(1), 30-40.
Lund, C., Tomlinson, M., & Patel, V. (2016). Integration of mental health into primary care in
low-and middle-income countries: the PRIME mental healthcare plans. The British
Journal of Psychiatry, 208(s56), s1-s3.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




