Six Key Components for Effective Public Health Program Implementation
VerifiedAdded on 2023/06/11
|6
|6505
|74
Essay
AI Summary
This essay delves into the critical components necessary for effective public health program implementation, highlighting six key areas: innovation, a rigorously established technical package, management, partnerships, communication, and political commitment. Innovation is central, driving the development and refinement of technical elements through new diagnostic techniques, information systems, and communication strategies. The technical package focuses on a select group of evidence-based interventions that achieve substantial improvements in specific risk factors or disease outcomes, exemplified by initiatives like DOTS for tuberculosis control and WHO’s MPOWER for tobacco control. Effective performance management requires accurate, timely information systems for surveillance and program implementation, with rigorous monitoring and evaluation to facilitate continuous refinement. Partnerships and coalitions with public and private sector organizations are essential, along with clear communication to engage the health care community, decision-makers, and the public. Finally, sustained political commitment ensures the necessary resources and support for effective action. The essay underscores that by addressing these six areas, public health programs can significantly improve health outcomes and achieve long-term success.
Six Components Necessary for Effective Public
Program Implementation
Public health programs
succeed and survive if or-
ganizations and coalitions
address 6 key areas.
(1) Innovation to develop
the evidence base for action;
(2) a technical package of
a limited number of high-
priority, evidence-based in-
terventions that together
will have a major impact;
(3) effective performance
management, especially
through rigorous, real-time
monitoring, evaluation, and
program improvement; (4)
partnerships and coalitions
with public- and private-
sector organizations; (5)
communication of accurate
and timely information to
the health care community,
decision makers, and the
public to effect behavior
change and engage civil
society; and (6) political
commitment to obtain re-
sources and support for
effective action.
Programs including small-
pox eradication, tuberculo-
sis control, tobacco control,
polio eradication, and others
have made progress by
addressing these 6 areas.
(Am J Public Health. 2014;
104:17–22. doi:10.2105/AJPH.
2013.301608)
Thomas R. Frieden, MD, MPH
WHEREAS MANY PUBLIC
health programs do not achieve
their potential impact,other pro-
grams succeed in improving
health outcomes drastically.Lim-
ited and unstable funding,lack of
automatic means to track and im-
prove performance,workforce
limitations,and insufficient politi-
cal commitment can all cause
public health programs to fail.
Implementation can succeed and
be sustained if organizations and
coalitions effectively address 6 key
areas: innovation,a rigorously
established technical package,
management,partnerships,com-
munication,and political commit-
ment.
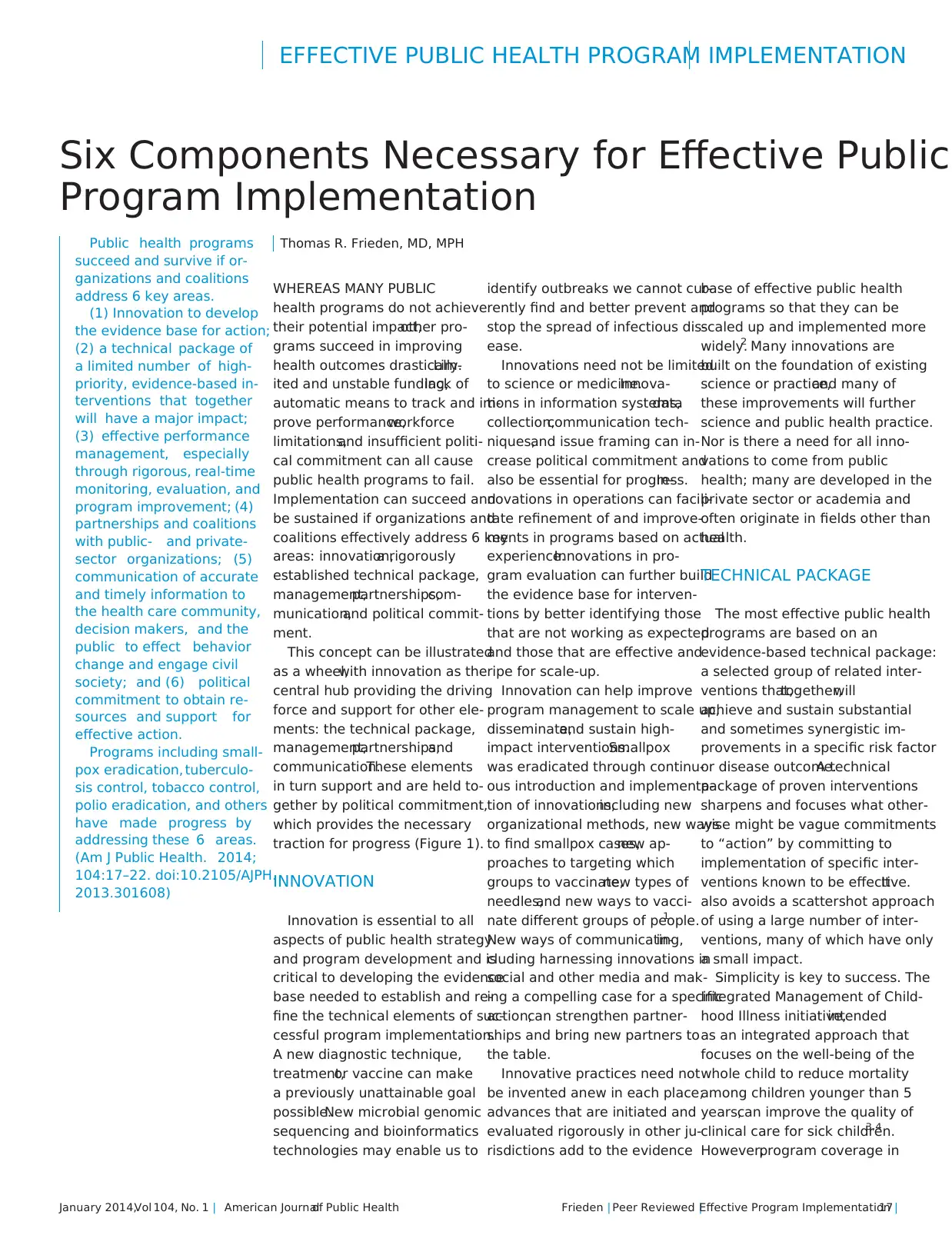
This concept can be illustrated
as a wheel,with innovation as the
central hub providing the driving
force and support for other ele-
ments: the technical package,
management,partnerships,and
communication.These elements
in turn support and are held to-
gether by political commitment,
which provides the necessary
traction for progress (Figure 1).
INNOVATION
Innovation is essential to all
aspects of public health strategy
and program development and is
critical to developing the evidence
base needed to establish and re-
fine the technical elements of suc-
cessful program implementation.
A new diagnostic technique,
treatment,or vaccine can make
a previously unattainable goal
possible.New microbial genomic
sequencing and bioinformatics
technologies may enable us to
identify outbreaks we cannot cur-
rently find and better prevent and
stop the spread of infectious dis-
ease.
Innovations need not be limited
to science or medicine.Innova-
tions in information systems,data
collection,communication tech-
niques,and issue framing can in-
crease political commitment and
also be essential for progress.In-
novations in operations can facili-
tate refinement of and improve-
ments in programs based on actual
experience.Innovations in pro-
gram evaluation can further build
the evidence base for interven-
tions by better identifying those
that are not working as expected
and those that are effective and
ripe for scale-up.
Innovation can help improve
program management to scale up,
disseminate,and sustain high-
impact interventions.Smallpox
was eradicated through continu-
ous introduction and implementa-
tion of innovations,including new
organizational methods, new ways
to find smallpox cases,new ap-
proaches to targeting which
groups to vaccinate,new types of
needles,and new ways to vacci-
nate different groups of people.1
New ways of communicating,in-
cluding harnessing innovations in
social and other media and mak-
ing a compelling case for a specific
action,can strengthen partner-
ships and bring new partners to
the table.
Innovative practices need not
be invented anew in each place;
advances that are initiated and
evaluated rigorously in other ju-
risdictions add to the evidence
base of effective public health
programs so that they can be
scaled up and implemented more
widely.2 Many innovations are
built on the foundation of existing
science or practice,and many of
these improvements will further
science and public health practice.
Nor is there a need for all inno-
vations to come from public
health; many are developed in the
private sector or academia and
often originate in fields other than
health.
TECHNICAL PACKAGE
The most effective public health
programs are based on an
evidence-based technical package:
a selected group of related inter-
ventions that,together,will
achieve and sustain substantial
and sometimes synergistic im-
provements in a specific risk factor
or disease outcome.A technical
package of proven interventions
sharpens and focuses what other-
wise might be vague commitments
to “action” by committing to
implementation of specific inter-
ventions known to be effective.It
also avoids a scattershot approach
of using a large number of inter-
ventions, many of which have only
a small impact.
Simplicity is key to success. The
Integrated Management of Child-
hood Illness initiative,intended
as an integrated approach that
focuses on the well-being of the
whole child to reduce mortality
among children younger than 5
years,can improve the quality of
clinical care for sick children.3,4
However,program coverage in
EFFECTIVE PUBLIC HEALTH PROGRAM IMPLEMENTATION
January 2014,Vol 104, No. 1 | American Journalof Public Health Frieden | Peer Reviewed |Effective Program Implementation |17
Program Implementation
Public health programs
succeed and survive if or-
ganizations and coalitions
address 6 key areas.
(1) Innovation to develop
the evidence base for action;
(2) a technical package of
a limited number of high-
priority, evidence-based in-
terventions that together
will have a major impact;
(3) effective performance
management, especially
through rigorous, real-time
monitoring, evaluation, and
program improvement; (4)
partnerships and coalitions
with public- and private-
sector organizations; (5)
communication of accurate
and timely information to
the health care community,
decision makers, and the
public to effect behavior
change and engage civil
society; and (6) political
commitment to obtain re-
sources and support for
effective action.
Programs including small-
pox eradication, tuberculo-
sis control, tobacco control,
polio eradication, and others
have made progress by
addressing these 6 areas.
(Am J Public Health. 2014;
104:17–22. doi:10.2105/AJPH.
2013.301608)
Thomas R. Frieden, MD, MPH
WHEREAS MANY PUBLIC
health programs do not achieve
their potential impact,other pro-
grams succeed in improving
health outcomes drastically.Lim-
ited and unstable funding,lack of
automatic means to track and im-
prove performance,workforce
limitations,and insufficient politi-
cal commitment can all cause
public health programs to fail.
Implementation can succeed and
be sustained if organizations and
coalitions effectively address 6 key
areas: innovation,a rigorously
established technical package,
management,partnerships,com-
munication,and political commit-
ment.
This concept can be illustrated
as a wheel,with innovation as the
central hub providing the driving
force and support for other ele-
ments: the technical package,
management,partnerships,and
communication.These elements
in turn support and are held to-
gether by political commitment,
which provides the necessary
traction for progress (Figure 1).
INNOVATION
Innovation is essential to all
aspects of public health strategy
and program development and is
critical to developing the evidence
base needed to establish and re-
fine the technical elements of suc-
cessful program implementation.
A new diagnostic technique,
treatment,or vaccine can make
a previously unattainable goal
possible.New microbial genomic
sequencing and bioinformatics
technologies may enable us to
identify outbreaks we cannot cur-
rently find and better prevent and
stop the spread of infectious dis-
ease.
Innovations need not be limited
to science or medicine.Innova-
tions in information systems,data
collection,communication tech-
niques,and issue framing can in-
crease political commitment and
also be essential for progress.In-
novations in operations can facili-
tate refinement of and improve-
ments in programs based on actual
experience.Innovations in pro-
gram evaluation can further build
the evidence base for interven-
tions by better identifying those
that are not working as expected
and those that are effective and
ripe for scale-up.
Innovation can help improve
program management to scale up,
disseminate,and sustain high-
impact interventions.Smallpox
was eradicated through continu-
ous introduction and implementa-
tion of innovations,including new
organizational methods, new ways
to find smallpox cases,new ap-
proaches to targeting which
groups to vaccinate,new types of
needles,and new ways to vacci-
nate different groups of people.1
New ways of communicating,in-
cluding harnessing innovations in
social and other media and mak-
ing a compelling case for a specific
action,can strengthen partner-
ships and bring new partners to
the table.
Innovative practices need not
be invented anew in each place;
advances that are initiated and
evaluated rigorously in other ju-
risdictions add to the evidence
base of effective public health
programs so that they can be
scaled up and implemented more
widely.2 Many innovations are
built on the foundation of existing
science or practice,and many of
these improvements will further
science and public health practice.
Nor is there a need for all inno-
vations to come from public
health; many are developed in the
private sector or academia and
often originate in fields other than
health.
TECHNICAL PACKAGE
The most effective public health
programs are based on an
evidence-based technical package:
a selected group of related inter-
ventions that,together,will
achieve and sustain substantial
and sometimes synergistic im-
provements in a specific risk factor
or disease outcome.A technical
package of proven interventions
sharpens and focuses what other-
wise might be vague commitments
to “action” by committing to
implementation of specific inter-
ventions known to be effective.It
also avoids a scattershot approach
of using a large number of inter-
ventions, many of which have only
a small impact.
Simplicity is key to success. The
Integrated Management of Child-
hood Illness initiative,intended
as an integrated approach that
focuses on the well-being of the
whole child to reduce mortality
among children younger than 5
years,can improve the quality of
clinical care for sick children.3,4
However,program coverage in
EFFECTIVE PUBLIC HEALTH PROGRAM IMPLEMENTATION
January 2014,Vol 104, No. 1 | American Journalof Public Health Frieden | Peer Reviewed |Effective Program Implementation |17
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

most countries has rarely reached
levels high enough to achieve
expected reductions in mortality,
in part because of the complexity
of this approach.
The DOTS (directly observed
treatment,short-course)strategy
for tuberculosis controlhas only
5 components:sustained political
and financialcommitment,good
laboratory diagnosis,standard-
ized treatmentprovided under
directobservation,a steady sup-
ply of high-quality anti-tubercu-
losis drugs,and rigorous moni-
toring and evaluation ofand
accountability for each patient’s
outcome.In the nearly 2 decades
since widespread adoption of
the DOTS strategy,more than
56 million people have been
successfully treated and 22 mil-
lion lives have been saved.5 In
the absence ofHIV, DOTS can
reduce the incidence ofactive
tuberculosis by abouthalfin
10 years.6
WHO’s MPOWER package
for tobacco control consists of 6
key policy measures: monitoring
tobacco use and prevention poli-
cies; protecting people from to-
bacco smoke; offering help to
quit tobacco use; warning about
the dangers of tobacco; enforcing
bans on tobacco advertising,
promotion,and sponsorship;
and raising tobacco prices.7 The
state of California and the city of
New York each invested in sus-
tained implementation of compre-
hensive tobacco control technical
packages that helped establish
the MPOWER strategy and have
recorded steady,long-term de-
clines in smoking prevalence.8,9
In Uruguay,which imple-
mented most elements of the
MPOWER strategy sooner than
any other country,smoking prev-
alence fell by a quarter in just
3 years, perhaps the fastest decline
ever recorded.10,11
Turkey, the first
country to attain the highest level
of achievement in all 6 MPOWER
measures,saw a 13.4% decline in
smoking prevalence in the 3.5
years after it enacted a compre-
hensive tobacco control law that
specifically addressed require-
ments of the WHO Framework
Convention on Tobacco Control
and incorporated the MPOWER
technical package.12 Progress in all
of these places was achieved be-
cause of sustained political sup-
port for difficult and sometimes
controversial decisions,as well as
adherence to the established evi-
dence base of a limited set of
proven interventions that are af-
fordable and scalable and have the
largest impact on health.
A technical package of surveil-
lance and vaccination has brought
the world to the brink of polio
eradication.13 Surveillance of
acute flaccid paralysis in children
through collection and laboratory
examination of stool specimens
enables public health programs to
know whether children with
symptomatic polio are being di-
agnosed and reported.14 In appro-
priate conditions,environmental
samples can help identify unrec-
ognized viral circulation and also
monitor virus persistence and dis-
appearance.15 National immuniza-
tion days,supported by both
strengthened routine immuniza-
tion programs and supplemental
campaigns,had stopped the
spread of polio by 2012 in all but
3 countries (Afghanistan,Nigeria,
and Pakistan).16
Infections associated with
health care affect about 1 in 20
hospitalized patients,cause nearly
100 000 deaths,and cost an esti-
mated $30 billion per year in the
United States.To reverse this,the
Centers for Disease Control and
Prevention developed and dis-
seminated a technical package
consisting of hand and respiratory
hygiene practices; use of masks,
gloves,and other protective
equipment; appropriate injection
and insertion practices; disinfec-
tion of equipment and environ-
mental surfaces; and surveil-
lance.17 Adherence to these
guidelines has substantially re-
duced the incidence of some
health care---associated infec-
tions,18,19
with central line---associ-
ated bloodstream infections low-
ered by more than 40% and
surgical site infections reduced by
17% between 2008 and 2011.20
A technical package ensures
focus on the most effective,feasi-
ble,and sustainable interventions
and can sometimes achieve syn-
ergy among intervention ele-
ments.Pressure to include all
approaches can make the estab-
lishment of a technical package
difficult; a technical package
established with inclusiveness of
approaches as a goal is likely to
fail. The key is to identify elements
that are both highly effective and
scalable to reach populations of
varying size,demographic com-
position,or geographic location,
and that can be sustained over
a long period.This may mean
that some interventions with
proven evidence of effectiveness
will not be included because their
effect is small,is not sustainable,
or—for fiscal,managerial,or other
reasons—cannot be scaled for
population impact.
Scalability is a key and poten-
tially controversial concept.Al-
though justifiable moral outrage
may suggest that “everything” be
done for everyone,and although
leadership and advocacy (e.g.,for
the US President’s Emergency
Plan for AIDS Relief [PEPFAR],
which has enabled treatment of
millions of people who would
have otherwise died) can make
possible programs previously
considered to be impossible,there
is almost always a delicate
FIGURE 1—Six key areas for effective public health program
implementation.
EFFECTIVE PUBLIC HEALTH PROGRAM IMPLEMENTATION
18 | Effective Program Implementation |Peer Reviewed |Frieden American Journalof Public Health |January 2014,Vol 104, No. 1
levels high enough to achieve
expected reductions in mortality,
in part because of the complexity
of this approach.
The DOTS (directly observed
treatment,short-course)strategy
for tuberculosis controlhas only
5 components:sustained political
and financialcommitment,good
laboratory diagnosis,standard-
ized treatmentprovided under
directobservation,a steady sup-
ply of high-quality anti-tubercu-
losis drugs,and rigorous moni-
toring and evaluation ofand
accountability for each patient’s
outcome.In the nearly 2 decades
since widespread adoption of
the DOTS strategy,more than
56 million people have been
successfully treated and 22 mil-
lion lives have been saved.5 In
the absence ofHIV, DOTS can
reduce the incidence ofactive
tuberculosis by abouthalfin
10 years.6
WHO’s MPOWER package
for tobacco control consists of 6
key policy measures: monitoring
tobacco use and prevention poli-
cies; protecting people from to-
bacco smoke; offering help to
quit tobacco use; warning about
the dangers of tobacco; enforcing
bans on tobacco advertising,
promotion,and sponsorship;
and raising tobacco prices.7 The
state of California and the city of
New York each invested in sus-
tained implementation of compre-
hensive tobacco control technical
packages that helped establish
the MPOWER strategy and have
recorded steady,long-term de-
clines in smoking prevalence.8,9
In Uruguay,which imple-
mented most elements of the
MPOWER strategy sooner than
any other country,smoking prev-
alence fell by a quarter in just
3 years, perhaps the fastest decline
ever recorded.10,11
Turkey, the first
country to attain the highest level
of achievement in all 6 MPOWER
measures,saw a 13.4% decline in
smoking prevalence in the 3.5
years after it enacted a compre-
hensive tobacco control law that
specifically addressed require-
ments of the WHO Framework
Convention on Tobacco Control
and incorporated the MPOWER
technical package.12 Progress in all
of these places was achieved be-
cause of sustained political sup-
port for difficult and sometimes
controversial decisions,as well as
adherence to the established evi-
dence base of a limited set of
proven interventions that are af-
fordable and scalable and have the
largest impact on health.
A technical package of surveil-
lance and vaccination has brought
the world to the brink of polio
eradication.13 Surveillance of
acute flaccid paralysis in children
through collection and laboratory
examination of stool specimens
enables public health programs to
know whether children with
symptomatic polio are being di-
agnosed and reported.14 In appro-
priate conditions,environmental
samples can help identify unrec-
ognized viral circulation and also
monitor virus persistence and dis-
appearance.15 National immuniza-
tion days,supported by both
strengthened routine immuniza-
tion programs and supplemental
campaigns,had stopped the
spread of polio by 2012 in all but
3 countries (Afghanistan,Nigeria,
and Pakistan).16
Infections associated with
health care affect about 1 in 20
hospitalized patients,cause nearly
100 000 deaths,and cost an esti-
mated $30 billion per year in the
United States.To reverse this,the
Centers for Disease Control and
Prevention developed and dis-
seminated a technical package
consisting of hand and respiratory
hygiene practices; use of masks,
gloves,and other protective
equipment; appropriate injection
and insertion practices; disinfec-
tion of equipment and environ-
mental surfaces; and surveil-
lance.17 Adherence to these
guidelines has substantially re-
duced the incidence of some
health care---associated infec-
tions,18,19
with central line---associ-
ated bloodstream infections low-
ered by more than 40% and
surgical site infections reduced by
17% between 2008 and 2011.20
A technical package ensures
focus on the most effective,feasi-
ble,and sustainable interventions
and can sometimes achieve syn-
ergy among intervention ele-
ments.Pressure to include all
approaches can make the estab-
lishment of a technical package
difficult; a technical package
established with inclusiveness of
approaches as a goal is likely to
fail. The key is to identify elements
that are both highly effective and
scalable to reach populations of
varying size,demographic com-
position,or geographic location,
and that can be sustained over
a long period.This may mean
that some interventions with
proven evidence of effectiveness
will not be included because their
effect is small,is not sustainable,
or—for fiscal,managerial,or other
reasons—cannot be scaled for
population impact.
Scalability is a key and poten-
tially controversial concept.Al-
though justifiable moral outrage
may suggest that “everything” be
done for everyone,and although
leadership and advocacy (e.g.,for
the US President’s Emergency
Plan for AIDS Relief [PEPFAR],
which has enabled treatment of
millions of people who would
have otherwise died) can make
possible programs previously
considered to be impossible,there
is almost always a delicate
FIGURE 1—Six key areas for effective public health program
implementation.
EFFECTIVE PUBLIC HEALTH PROGRAM IMPLEMENTATION
18 | Effective Program Implementation |Peer Reviewed |Frieden American Journalof Public Health |January 2014,Vol 104, No. 1

interplay between the ideal and
the realistic.There are practical
limitations to how rapidly and
broadly public health programs
can increase their reach,with sep-
arate although related limitations
in financial and human resources,
institutional capacity,health care
system quality, behavioral change,
and politics.
To establish an effective inter-
vention package,it is critical to
understand the full range of
available evidence-based strate-
gies,the size and characteristics of
the population to be reached,the
projected impact of each inter-
vention,and the estimated cost.
The more expensive or complex
each intervention is,the less likely
it will have broad population im-
pact. More strategies in a technical
package result in more costly and
unwieldy programs with a lower
likelihood of success.An analysis
that determines the burden caused
by each risk factor can help iden-
tify which risk factors have the
greatest impact on population
health and thus can lead to the
greatest health improvements if
addressed effectively.
In some cases,organizations,
physicians, or advocates may insist
on individualized approaches.Al-
though customization of treatment
and care can in theory benefit
individual patients,this may make
it difficult or impossible to estab-
lish a scalable technical package
that leads to widespread adoption
of at least a minimum standard of
care.Standardization of immuni-
zation schedules and of treatment
of HIV,drug-susceptible tubercu-
losis,and malaria has led to lower
medication prices,greater ease of
program implementation and su-
pervision,and improved ability of
nurses and other trained health
workers to initiate and monitor
treatment; all of these factors are
essential for successful scale-up.
MANAGING
PERFORMANCE
For many public health pro-
grams,implementation is essen-
tially a management problem.
Even if political commitment,re-
sources,and a technical package
are in place, effective management
may not be. Management of public
health activities is particularly dif-
ficult because, unlike in the private
sector where metrics such as
product sales provide prompt
feedback on performance,there is
often no automatic,accurate,and
affordable way to track public
health program performance in
real time. In addition, the impact of
public health programs may not
be evident for months or years,
further complicating measurement
of performance.
Effective public health pro-
grams require accurate,timely
information systems for disease
or risk factor surveillance and
program implementation.For this
reason,every effective technical
package includes surveillance and
information systems that can be
sustained and that provide accu-
rate,simple,timely,and critical
information on program imple-
mentation and impact over the
long term.21
Rigorous monitoring and eval-
uation,with mechanisms to avoid
bias in the data or misplaced con-
fidence in program effectiveness,
are essential for both progress and
sustainability.Honest and trans-
parent assessment of progress or
the lack thereof—even or espe-
cially if temporarily inconvenient
or embarrassing because of lack of
progress—is critical to allow con-
tinuous refinement of and im-
provements in program strategy
and implementation.It is particu-
larly important for programs that
have made some progress to avoid
complacency.Only by having and
acting on accurate information can
a program that has made progress
prevent itself from stalling.
New York City made reducing
smoking a top priority,increasing
the tobacco tax in 2002 and
making virtually all workplaces
smoke free in 2003.22 Tobacco
use declined rapidly in 2003 and
2004, but the decline then stalled,
a development that would not
have been known if New York
City had not begun conducting
large community surveys on an
annual basis beginning in 2002.
As a result, in 2005 New York City
initiated another tobacco control
intervention—hard-hitting anti-
tobacco advertising—which led to
a resumption of the decline the
following and subsequent years.23
Ongoing analysis to improve
virtually every aspect of program
operations and management is
critical to innovation and progress.
Information technology to im-
prove management can facilitate
the establishment of feedback
loops that enable real-time pro-
gram assessment and improve-
ment,but the costs of information
technology are often underesti-
mated and its benefits often over-
estimated.Simple systems driven
by a clear understanding of the
requirements and limitations of
essential data elements are most
likely to be useful. One example of
such a system is the tuberculosis
patient registry maintained in
public health tuberculosis control
units in nearly every country.
These registries track the outcome
of every patient started on treat-
ment and do not require large
investments in information tech-
nology.24
Public health human resource
management is challenging.It is
often difficult to recruit,train,and
retain the qualified work force
needed to implement effective
public health programs.Budget
shortfalls,salaries generally lower
than in the private sector,and
vocal opposition to public health
initiatives can demoralize staff.
Effective human resource man-
agement can be achieved,at least
in part,through career develop-
ment measures that focus on or-
ganizational mission and include
ongoing training and education,
clear paths for career advance-
ment,and financial and other re-
wards for outstanding perfor-
mance.Globally,effective public
health programs have addressed
human resource limitations
through task sharing,with nurses
and lay health workers initiating
or titrating medications,perform-
ing some surgeries,and supervis-
ing programs.25,26Information
technology,use of community
health workers,and broader part-
nerships can help address man-
agement challenges.
PARTNERSHIPS
Public health is increasingly
complex,with key roles played
by public- and private-sector
partners that are critical to sus-
taining and improving the popu-
lation’s health.27 Coalitions are
often essential to progress.Getting
many organizations to collaborate
can be slow and frustrating but is
often crucial to create the advo-
cacy needed to support budgetary,
legislative,or regulatory change
and to implement new or im-
proved programs.Government
programs are more likely to suc-
ceed—and to be sustained—when
organizations outside of govern-
ment advocate for them.28
Partners can supplement avail-
able human or financial resources
and can support and undertake
critical activities.Helping disparate
groups agree on and take action
to achieve a common agenda can
build effective long-term coalitions
EFFECTIVE PUBLIC HEALTH PROGRAM IMPLEMENTATION
January 2014,Vol 104, No. 1 | American Journalof Public Health Frieden | Peer Reviewed |Effective Program Implementation |19
the realistic.There are practical
limitations to how rapidly and
broadly public health programs
can increase their reach,with sep-
arate although related limitations
in financial and human resources,
institutional capacity,health care
system quality, behavioral change,
and politics.
To establish an effective inter-
vention package,it is critical to
understand the full range of
available evidence-based strate-
gies,the size and characteristics of
the population to be reached,the
projected impact of each inter-
vention,and the estimated cost.
The more expensive or complex
each intervention is,the less likely
it will have broad population im-
pact. More strategies in a technical
package result in more costly and
unwieldy programs with a lower
likelihood of success.An analysis
that determines the burden caused
by each risk factor can help iden-
tify which risk factors have the
greatest impact on population
health and thus can lead to the
greatest health improvements if
addressed effectively.
In some cases,organizations,
physicians, or advocates may insist
on individualized approaches.Al-
though customization of treatment
and care can in theory benefit
individual patients,this may make
it difficult or impossible to estab-
lish a scalable technical package
that leads to widespread adoption
of at least a minimum standard of
care.Standardization of immuni-
zation schedules and of treatment
of HIV,drug-susceptible tubercu-
losis,and malaria has led to lower
medication prices,greater ease of
program implementation and su-
pervision,and improved ability of
nurses and other trained health
workers to initiate and monitor
treatment; all of these factors are
essential for successful scale-up.
MANAGING
PERFORMANCE
For many public health pro-
grams,implementation is essen-
tially a management problem.
Even if political commitment,re-
sources,and a technical package
are in place, effective management
may not be. Management of public
health activities is particularly dif-
ficult because, unlike in the private
sector where metrics such as
product sales provide prompt
feedback on performance,there is
often no automatic,accurate,and
affordable way to track public
health program performance in
real time. In addition, the impact of
public health programs may not
be evident for months or years,
further complicating measurement
of performance.
Effective public health pro-
grams require accurate,timely
information systems for disease
or risk factor surveillance and
program implementation.For this
reason,every effective technical
package includes surveillance and
information systems that can be
sustained and that provide accu-
rate,simple,timely,and critical
information on program imple-
mentation and impact over the
long term.21
Rigorous monitoring and eval-
uation,with mechanisms to avoid
bias in the data or misplaced con-
fidence in program effectiveness,
are essential for both progress and
sustainability.Honest and trans-
parent assessment of progress or
the lack thereof—even or espe-
cially if temporarily inconvenient
or embarrassing because of lack of
progress—is critical to allow con-
tinuous refinement of and im-
provements in program strategy
and implementation.It is particu-
larly important for programs that
have made some progress to avoid
complacency.Only by having and
acting on accurate information can
a program that has made progress
prevent itself from stalling.
New York City made reducing
smoking a top priority,increasing
the tobacco tax in 2002 and
making virtually all workplaces
smoke free in 2003.22 Tobacco
use declined rapidly in 2003 and
2004, but the decline then stalled,
a development that would not
have been known if New York
City had not begun conducting
large community surveys on an
annual basis beginning in 2002.
As a result, in 2005 New York City
initiated another tobacco control
intervention—hard-hitting anti-
tobacco advertising—which led to
a resumption of the decline the
following and subsequent years.23
Ongoing analysis to improve
virtually every aspect of program
operations and management is
critical to innovation and progress.
Information technology to im-
prove management can facilitate
the establishment of feedback
loops that enable real-time pro-
gram assessment and improve-
ment,but the costs of information
technology are often underesti-
mated and its benefits often over-
estimated.Simple systems driven
by a clear understanding of the
requirements and limitations of
essential data elements are most
likely to be useful. One example of
such a system is the tuberculosis
patient registry maintained in
public health tuberculosis control
units in nearly every country.
These registries track the outcome
of every patient started on treat-
ment and do not require large
investments in information tech-
nology.24
Public health human resource
management is challenging.It is
often difficult to recruit,train,and
retain the qualified work force
needed to implement effective
public health programs.Budget
shortfalls,salaries generally lower
than in the private sector,and
vocal opposition to public health
initiatives can demoralize staff.
Effective human resource man-
agement can be achieved,at least
in part,through career develop-
ment measures that focus on or-
ganizational mission and include
ongoing training and education,
clear paths for career advance-
ment,and financial and other re-
wards for outstanding perfor-
mance.Globally,effective public
health programs have addressed
human resource limitations
through task sharing,with nurses
and lay health workers initiating
or titrating medications,perform-
ing some surgeries,and supervis-
ing programs.25,26Information
technology,use of community
health workers,and broader part-
nerships can help address man-
agement challenges.
PARTNERSHIPS
Public health is increasingly
complex,with key roles played
by public- and private-sector
partners that are critical to sus-
taining and improving the popu-
lation’s health.27 Coalitions are
often essential to progress.Getting
many organizations to collaborate
can be slow and frustrating but is
often crucial to create the advo-
cacy needed to support budgetary,
legislative,or regulatory change
and to implement new or im-
proved programs.Government
programs are more likely to suc-
ceed—and to be sustained—when
organizations outside of govern-
ment advocate for them.28
Partners can supplement avail-
able human or financial resources
and can support and undertake
critical activities.Helping disparate
groups agree on and take action
to achieve a common agenda can
build effective long-term coalitions
EFFECTIVE PUBLIC HEALTH PROGRAM IMPLEMENTATION
January 2014,Vol 104, No. 1 | American Journalof Public Health Frieden | Peer Reviewed |Effective Program Implementation |19
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

that extend beyond a specific issue.
Schools,businesses,law enforce-
ment,transportation,agriculture,
labor,and many other sectors in
society can contribute greatly to,
and benefit greatly from,public
health programs,policies,and
priorities.
Effective partnerships between
agencies at different levels of gov-
ernment can be difficult to estab-
lish and maintain.Sharing re-
sources and responsibilities
between state and local health
departments,for example,can be
politically charged and complex.
Research on the sustainability of
community health coalitions sug-
gests that accepting collective re-
sponsibility and mutual account-
ability,articulating a shared
mission and vision to achieve
common goals,and maintaining
focus can keep governmental and
nongovernmental partners coor-
dinated and avoid turf wars and
resource competition among part-
ners.29
There can be ethical issues in
developing public---private part-
nerships in public health.Partner-
ships between government and
the food,beverage,and other in-
dustries that address health issues
are expanding; these partnerships
have the potential to either further
or undermine effective change
and should be systematically and
transparently monitored and
evaluated.30 The tobacco industry
attempts to position itself as a le-
gitimate partner and stakeholder
in tobacco control,a situation
addressed by provisions in the
WHO Framework Convention on
Tobacco Control that proscribe
industry involvement.31
Examples of effective multisec-
toral partnerships include immu-
nization coalitions at the national
and state levels that involve part-
ners such as government agencies,
community organizations,
corporations,foundations,indi-
vidual philanthropists,patients,
and volunteers.These partner-
ships build comprehensive,sus-
tained community programs that
advocate for policies that will re-
sult in the immunization of people
against vaccine-preventable dis-
eases. Partnerships are particularly
important to sustain programs
during difficult budgetary times.
COMMUNICATION
Effective communication can
lead to behavior change, but, more
importantly,it can lead to in-
creased political commitment and
program effectiveness by engaging
a wide range of civil society sec-
tors and by contributing to
a change in the public perception
of an issue. With the advent of the
Internet,social media,and other
communication technologies,
more information is available from
more sources than ever,although
some is incorrect or potentially
harmful.New communication
tools and technologies facilitate
interactive conversations,giving
public health practitioners the
ability to have dialogues with
people from affected communities
and other stakeholders.With the
increase in communication chan-
nels and voices,public health
communications can be drowned
out unless communication strate-
gies are timely,well defined,well
executed,and sustained to meet
specific objectives.
Effective communication can
convey critical information,con-
vince key individuals to support or
lead an initiative,and,perhaps
most importantly,change the con-
text for public health action.
Mothers Against Drunk Driving
and Remove Intoxicated Drivers
changed the context for road safety
by transforming societal percep-
tions of drunk driving,helping
people recognize it as an unaccept-
able endangerment of others.32
Social change and changes in
the law and public health pro-
grams both influence and are
influenced by each other.Over
time, the prevailing social mores of
“one for the road” and “Would
you like a cigarette?” changed to
“friends don’t let friends drink and
drive” and “Do you mind if I
smoke?” These changes in social
norms both emanated from and
facilitated the enactment and
implementation of legal and policy
changes. Effective communication,
such as hard-hitting anti-tobacco
campaigns, can lead to widespread
behavioral change and can also
help change social norms.33,34
With better information,indi-
viduals and communities can
make better decisions about their
own health and about public
health programs.Different audi-
ences need to be presented with
different types of data in different
ways to have the intended impact.
Health care providers need up-to-
date information,which can be
provided through traditional
means such as publications and
medical association guidance,as
well as through electronic out-
reach,messaging systems,and
other newer communication
channels that can facilitate navi-
gation of an often rapidly changing
clinical and health care delivery
environment.Decision makers
need accurate,timely,and concise
information about the health and
fiscal effects of different policy
options.
An effective program needs to
effectively communicate its suc-
cess and benefits,as well as the
threats to health and health equity
being addressed,with anecdotes
and case studies to illustrate these
points. Presenting a human face to
demonstrate the impact of abstract
data can show decision makers
that health and lives are at stake.
The business community needs
information that shows the busi-
ness case. Media framing and news
coverage are often essential to in-
troduce,explain,generate support
for,and facilitate implementation
of public health policies and pro-
grams.By providing accurate,
timely,and convincing informa-
tion that includes data on out-
comes,public health entities can
increase their credibility with po-
tential stakeholders such as deci-
sion makers, health care providers,
the public,and public and private
program funders.
Communication is also crucial
to save lives during emergencies.
Communication with first re-
sponders,the public,and other
groups may need to be instanta-
neous and clear and must occur in
real time during a rapidly evolving
event.Even when a public health
emergency evolves more slowly,
such as during the 2009 global
outbreak of H1N1 influenza,new
information may need to be com-
municated on an ongoing basis as
the event unfolds,both to imple-
ment specific activities and to
minimize confusion and distrust.
POLITICAL COMMITMENT
Political commitment is built on
and supported by the components
described thus far, all of which are
critical to provide government
with a strong foundation for ac-
tion.Effectively engaged political
commitment leads to the re-
sources and support needed to
coordinate,implement,and sus-
tain public health interventions,
including policy change where
needed.Change is often controver-
sial, and the entities that implement
public health programs—usually
led by public health departments
or other government agencies—
may have less ability to influence
EFFECTIVE PUBLIC HEALTH PROGRAM IMPLEMENTATION
20 | Effective Program Implementation |Peer Reviewed |Frieden American Journalof Public Health |January 2014,Vol 104, No. 1
Schools,businesses,law enforce-
ment,transportation,agriculture,
labor,and many other sectors in
society can contribute greatly to,
and benefit greatly from,public
health programs,policies,and
priorities.
Effective partnerships between
agencies at different levels of gov-
ernment can be difficult to estab-
lish and maintain.Sharing re-
sources and responsibilities
between state and local health
departments,for example,can be
politically charged and complex.
Research on the sustainability of
community health coalitions sug-
gests that accepting collective re-
sponsibility and mutual account-
ability,articulating a shared
mission and vision to achieve
common goals,and maintaining
focus can keep governmental and
nongovernmental partners coor-
dinated and avoid turf wars and
resource competition among part-
ners.29
There can be ethical issues in
developing public---private part-
nerships in public health.Partner-
ships between government and
the food,beverage,and other in-
dustries that address health issues
are expanding; these partnerships
have the potential to either further
or undermine effective change
and should be systematically and
transparently monitored and
evaluated.30 The tobacco industry
attempts to position itself as a le-
gitimate partner and stakeholder
in tobacco control,a situation
addressed by provisions in the
WHO Framework Convention on
Tobacco Control that proscribe
industry involvement.31
Examples of effective multisec-
toral partnerships include immu-
nization coalitions at the national
and state levels that involve part-
ners such as government agencies,
community organizations,
corporations,foundations,indi-
vidual philanthropists,patients,
and volunteers.These partner-
ships build comprehensive,sus-
tained community programs that
advocate for policies that will re-
sult in the immunization of people
against vaccine-preventable dis-
eases. Partnerships are particularly
important to sustain programs
during difficult budgetary times.
COMMUNICATION
Effective communication can
lead to behavior change, but, more
importantly,it can lead to in-
creased political commitment and
program effectiveness by engaging
a wide range of civil society sec-
tors and by contributing to
a change in the public perception
of an issue. With the advent of the
Internet,social media,and other
communication technologies,
more information is available from
more sources than ever,although
some is incorrect or potentially
harmful.New communication
tools and technologies facilitate
interactive conversations,giving
public health practitioners the
ability to have dialogues with
people from affected communities
and other stakeholders.With the
increase in communication chan-
nels and voices,public health
communications can be drowned
out unless communication strate-
gies are timely,well defined,well
executed,and sustained to meet
specific objectives.
Effective communication can
convey critical information,con-
vince key individuals to support or
lead an initiative,and,perhaps
most importantly,change the con-
text for public health action.
Mothers Against Drunk Driving
and Remove Intoxicated Drivers
changed the context for road safety
by transforming societal percep-
tions of drunk driving,helping
people recognize it as an unaccept-
able endangerment of others.32
Social change and changes in
the law and public health pro-
grams both influence and are
influenced by each other.Over
time, the prevailing social mores of
“one for the road” and “Would
you like a cigarette?” changed to
“friends don’t let friends drink and
drive” and “Do you mind if I
smoke?” These changes in social
norms both emanated from and
facilitated the enactment and
implementation of legal and policy
changes. Effective communication,
such as hard-hitting anti-tobacco
campaigns, can lead to widespread
behavioral change and can also
help change social norms.33,34
With better information,indi-
viduals and communities can
make better decisions about their
own health and about public
health programs.Different audi-
ences need to be presented with
different types of data in different
ways to have the intended impact.
Health care providers need up-to-
date information,which can be
provided through traditional
means such as publications and
medical association guidance,as
well as through electronic out-
reach,messaging systems,and
other newer communication
channels that can facilitate navi-
gation of an often rapidly changing
clinical and health care delivery
environment.Decision makers
need accurate,timely,and concise
information about the health and
fiscal effects of different policy
options.
An effective program needs to
effectively communicate its suc-
cess and benefits,as well as the
threats to health and health equity
being addressed,with anecdotes
and case studies to illustrate these
points. Presenting a human face to
demonstrate the impact of abstract
data can show decision makers
that health and lives are at stake.
The business community needs
information that shows the busi-
ness case. Media framing and news
coverage are often essential to in-
troduce,explain,generate support
for,and facilitate implementation
of public health policies and pro-
grams.By providing accurate,
timely,and convincing informa-
tion that includes data on out-
comes,public health entities can
increase their credibility with po-
tential stakeholders such as deci-
sion makers, health care providers,
the public,and public and private
program funders.
Communication is also crucial
to save lives during emergencies.
Communication with first re-
sponders,the public,and other
groups may need to be instanta-
neous and clear and must occur in
real time during a rapidly evolving
event.Even when a public health
emergency evolves more slowly,
such as during the 2009 global
outbreak of H1N1 influenza,new
information may need to be com-
municated on an ongoing basis as
the event unfolds,both to imple-
ment specific activities and to
minimize confusion and distrust.
POLITICAL COMMITMENT
Political commitment is built on
and supported by the components
described thus far, all of which are
critical to provide government
with a strong foundation for ac-
tion.Effectively engaged political
commitment leads to the re-
sources and support needed to
coordinate,implement,and sus-
tain public health interventions,
including policy change where
needed.Change is often controver-
sial, and the entities that implement
public health programs—usually
led by public health departments
or other government agencies—
may have less ability to influence
EFFECTIVE PUBLIC HEALTH PROGRAM IMPLEMENTATION
20 | Effective Program Implementation |Peer Reviewed |Frieden American Journalof Public Health |January 2014,Vol 104, No. 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

budget and policy decisions than
other groups within government
and civil society.
Interventions touch many sec-
tors of society, some of which may
oppose public health proposals
vigorously.Opponents of specific
public health programs may be
highly vocal, well funded, and well
organized,and opposition from
a specific interest group can be
potent,even when the overall
societal benefits of a public health
program are large.Many public
health initiatives, such as measures
to reduce tobacco use,greatly
improve the public’s health by
benefiting tens of millions of peo-
ple (smokers and those exposed to
secondhand smoke,in this case)
but are contrary to the interests of
a small but powerful group: in this
case,tobacco companies.Political
commitment can be critical to
overcome opposition to public
health programs by special inter-
est groups such as the tobacco
industry,and it requires under-
standing industry tactics,effective
communications with all stake-
holders,and involvement of the
public and civil society in public
health efforts.35
The beneficiaries of specific
public health programs may be
unaware of the health and other
benefits received or unaware that
specific programs are under the
purview of public health; they may
be only moderately vocal in ad-
vocating for programs and ser-
vices,and in some cases they
may be politically disenfranchised.
Increased public awareness of
the benefits of public health pro-
grams can increase advocacy and
generate higher levels of political
commitment.
Public health is often under-
funded,and ongoing fiscal con-
straints have further reduced
spending.In the United States,
state and local budget cuts have
led to the loss of more than
46 000 state and local public
health jobs since 2008.36 Polit-
ical commitment is a prerequi-
site for sufficient funding.As
Hermann Biggs stated a century
ago: “Public health is purchas-
able.Within natural limitations
a community can determine its
own death rate.”37
Public health programs that
have generated opposition in the
past include water fluoridation,38
vaccination mandates,39 smoke-
free workplace laws,40 disease
reporting,41environmental pro-
tection,42 and motor vehicle
safety.43 In each of these cases, the
intervention produced substantial
net benefits to the public’s health
that outweighed the costs of
implementation.However,most
individuals do not experience im-
mediate benefits, and often a small
but vocal group opposes the
program vigorously.
Public health programs are
sometimes not adopted because of
the “prevention paradox,” accord-
ing to which “a preventive mea-
sure that brings large benefits to
the community offers little to each
participating individual.”44(p47)
Large gains in population health
often come from small changes for
many people rather than from
large changes for fewer people.
For this reason,leadership,com-
munication,and partnerships are
essential to progress.
Political commitment by broad
coalitions led to successful imple-
mentation of the Vaccines for
Children program and PEPFAR.
Vaccines for Children,a federally
funded program that provides
vaccines at no cost to children who
might not otherwise be vaccinated
because of inability to pay,has
helped ensure vaccination for
millions of US children since 1994
and virtually eliminated racial and
ethnic disparities in childhood
immunization rates.45 Since being
established in 2003,PEPFAR
programs have helped millions of
people worldwide: life-saving
antiretroviral treatment has been
provided directly to more than 5
million people,HIV counseling
and testing have been provided to
more than 46 million people,and
more than 1 million infants have
been prevented from becoming
infected.46
CONCLUSIONS
Those who work in and support
public health improve the health
of individuals and communities.
The greatest strength of public
health is its singular focus on
maximizing health so that society
can achieve its most cherished
values: that children are born
healthy and grow up healthy,that
students are healthy and able to
learn,that workers are healthy
and productive,that parents are
empowered to help their children
reach their full potential,that
health disparities are reduced, and
that people are able to age with
independence and dignity.
Compelling data and evidence
for action,broad coalitions,and
effective communication generate
and sustain the political commit-
ment necessary for successful
public health action.To improve
public health programs,it is often
essential to highlight unacceptable
existing disease burdens,health
outcomes,disparities,and threats
to health.It is also useful to pro-
vide real-life examples of individ-
uals harmed by failure to act or
benefited by specific programs.
Effective coalitions with key sup-
port and leadership from individ-
uals and groups outside of gov-
ernment are often essential for
progress.An effective and coordi-
nated alliance of political,techni-
cal, and managerial leadership can
increase the likelihood of imple-
mentation of programs that protect
and improve the public’s health.j
About the Author
Thomas R.Frieden is director of the
Centers for Disease Control and Prevention,
Atlanta,GA.
Correspondence should be sent to Thomas
R. Frieden, MD, MPH, Centers for Disease
Control and Prevention, 1600 Clifton Rd NE,
MS D-14, Atlanta, GA 30333 (e-mail:
tfrieden@cdc.gov). Reprints can be ordered
at http://www.ajph.org by clicking on the
“Reprints” link.
This article was accepted July 26,
2013.
Acknowledgments
I thank Thomas A.Farley,Kelly J.Hen-
ning,Janet Collins,and Linda Degutis for
critical reviews of the article and Drew
Blakeman for assistance with article
preparation.
Human Participant Protection
No protocol approval was needed be-
cause no human participants were in-
volved.
References
1. Foege WH.House on Fire: The Fight
to Eliminate Smallpox.Berkeley,CA: Uni-
versity of California Press; 2011.
2. Centers for Disease Control and
Prevention.Guide to community preven-
tive services.Available at: http://www.
thecommunityguide.org.Accessed Sep-
tember 12,2013.
3. Rakha MA,Abdelmoneim AN,
Farhoud S,et al.Does implementation of
the IMCI strategy have an impact on child
mortality? A retrospective analysis of
routine data from Egypt.BMJ Open.
2013;3(1):e001852.
4. Chopra M,Binkin NJ,Mason E,et al.
Integrated management of childhood ill-
ness: what have we learned and how can
it be improved? Arch Dis Child.2012;97
(4):350---354.
5. Global Tuberculosis Report 2013.
Geneva,Switzerland: World Health
Organization; 2013.
6. Dye C,Garnett GP,Sleeman K,et al.
Prospects for worldwide tuberculosis
control under the WHO DOTS strategy.
Lancet.1998;352(9144):1886---1891.
7. MPOWER: A Policy Package to
Reverse the Tobacco Epidemic.Geneva,
Switzerland: World Health Organization;
2008.
8. California Tobacco Control Program.
California Tobacco Control Update 2009:
EFFECTIVE PUBLIC HEALTH PROGRAM IMPLEMENTATION
January 2014,Vol 104, No. 1 | American Journalof Public Health Frieden | Peer Reviewed |Effective Program Implementation |21
other groups within government
and civil society.
Interventions touch many sec-
tors of society, some of which may
oppose public health proposals
vigorously.Opponents of specific
public health programs may be
highly vocal, well funded, and well
organized,and opposition from
a specific interest group can be
potent,even when the overall
societal benefits of a public health
program are large.Many public
health initiatives, such as measures
to reduce tobacco use,greatly
improve the public’s health by
benefiting tens of millions of peo-
ple (smokers and those exposed to
secondhand smoke,in this case)
but are contrary to the interests of
a small but powerful group: in this
case,tobacco companies.Political
commitment can be critical to
overcome opposition to public
health programs by special inter-
est groups such as the tobacco
industry,and it requires under-
standing industry tactics,effective
communications with all stake-
holders,and involvement of the
public and civil society in public
health efforts.35
The beneficiaries of specific
public health programs may be
unaware of the health and other
benefits received or unaware that
specific programs are under the
purview of public health; they may
be only moderately vocal in ad-
vocating for programs and ser-
vices,and in some cases they
may be politically disenfranchised.
Increased public awareness of
the benefits of public health pro-
grams can increase advocacy and
generate higher levels of political
commitment.
Public health is often under-
funded,and ongoing fiscal con-
straints have further reduced
spending.In the United States,
state and local budget cuts have
led to the loss of more than
46 000 state and local public
health jobs since 2008.36 Polit-
ical commitment is a prerequi-
site for sufficient funding.As
Hermann Biggs stated a century
ago: “Public health is purchas-
able.Within natural limitations
a community can determine its
own death rate.”37
Public health programs that
have generated opposition in the
past include water fluoridation,38
vaccination mandates,39 smoke-
free workplace laws,40 disease
reporting,41environmental pro-
tection,42 and motor vehicle
safety.43 In each of these cases, the
intervention produced substantial
net benefits to the public’s health
that outweighed the costs of
implementation.However,most
individuals do not experience im-
mediate benefits, and often a small
but vocal group opposes the
program vigorously.
Public health programs are
sometimes not adopted because of
the “prevention paradox,” accord-
ing to which “a preventive mea-
sure that brings large benefits to
the community offers little to each
participating individual.”44(p47)
Large gains in population health
often come from small changes for
many people rather than from
large changes for fewer people.
For this reason,leadership,com-
munication,and partnerships are
essential to progress.
Political commitment by broad
coalitions led to successful imple-
mentation of the Vaccines for
Children program and PEPFAR.
Vaccines for Children,a federally
funded program that provides
vaccines at no cost to children who
might not otherwise be vaccinated
because of inability to pay,has
helped ensure vaccination for
millions of US children since 1994
and virtually eliminated racial and
ethnic disparities in childhood
immunization rates.45 Since being
established in 2003,PEPFAR
programs have helped millions of
people worldwide: life-saving
antiretroviral treatment has been
provided directly to more than 5
million people,HIV counseling
and testing have been provided to
more than 46 million people,and
more than 1 million infants have
been prevented from becoming
infected.46
CONCLUSIONS
Those who work in and support
public health improve the health
of individuals and communities.
The greatest strength of public
health is its singular focus on
maximizing health so that society
can achieve its most cherished
values: that children are born
healthy and grow up healthy,that
students are healthy and able to
learn,that workers are healthy
and productive,that parents are
empowered to help their children
reach their full potential,that
health disparities are reduced, and
that people are able to age with
independence and dignity.
Compelling data and evidence
for action,broad coalitions,and
effective communication generate
and sustain the political commit-
ment necessary for successful
public health action.To improve
public health programs,it is often
essential to highlight unacceptable
existing disease burdens,health
outcomes,disparities,and threats
to health.It is also useful to pro-
vide real-life examples of individ-
uals harmed by failure to act or
benefited by specific programs.
Effective coalitions with key sup-
port and leadership from individ-
uals and groups outside of gov-
ernment are often essential for
progress.An effective and coordi-
nated alliance of political,techni-
cal, and managerial leadership can
increase the likelihood of imple-
mentation of programs that protect
and improve the public’s health.j
About the Author
Thomas R.Frieden is director of the
Centers for Disease Control and Prevention,
Atlanta,GA.
Correspondence should be sent to Thomas
R. Frieden, MD, MPH, Centers for Disease
Control and Prevention, 1600 Clifton Rd NE,
MS D-14, Atlanta, GA 30333 (e-mail:
tfrieden@cdc.gov). Reprints can be ordered
at http://www.ajph.org by clicking on the
“Reprints” link.
This article was accepted July 26,
2013.
Acknowledgments
I thank Thomas A.Farley,Kelly J.Hen-
ning,Janet Collins,and Linda Degutis for
critical reviews of the article and Drew
Blakeman for assistance with article
preparation.
Human Participant Protection
No protocol approval was needed be-
cause no human participants were in-
volved.
References
1. Foege WH.House on Fire: The Fight
to Eliminate Smallpox.Berkeley,CA: Uni-
versity of California Press; 2011.
2. Centers for Disease Control and
Prevention.Guide to community preven-
tive services.Available at: http://www.
thecommunityguide.org.Accessed Sep-
tember 12,2013.
3. Rakha MA,Abdelmoneim AN,
Farhoud S,et al.Does implementation of
the IMCI strategy have an impact on child
mortality? A retrospective analysis of
routine data from Egypt.BMJ Open.
2013;3(1):e001852.
4. Chopra M,Binkin NJ,Mason E,et al.
Integrated management of childhood ill-
ness: what have we learned and how can
it be improved? Arch Dis Child.2012;97
(4):350---354.
5. Global Tuberculosis Report 2013.
Geneva,Switzerland: World Health
Organization; 2013.
6. Dye C,Garnett GP,Sleeman K,et al.
Prospects for worldwide tuberculosis
control under the WHO DOTS strategy.
Lancet.1998;352(9144):1886---1891.
7. MPOWER: A Policy Package to
Reverse the Tobacco Epidemic.Geneva,
Switzerland: World Health Organization;
2008.
8. California Tobacco Control Program.
California Tobacco Control Update 2009:
EFFECTIVE PUBLIC HEALTH PROGRAM IMPLEMENTATION
January 2014,Vol 104, No. 1 | American Journalof Public Health Frieden | Peer Reviewed |Effective Program Implementation |21

20 Years of Tobacco Control in California.
Sacramento,CA: California Department
of Public Health; 2009.
9. Coady MH,Jasek J,Davis K,et al.
Changes in smoking prevalence and
number of cigarettes smoked per day
following the implementation of a com-
prehensive tobacco control plan in New
York City.J Urban Health.2012;89
(5):802---808.
10. International Tobacco Control
Policy Evaluation Project.ITC Uruguay
National Report: Findings From the Wave
1 to 3 Surveys (2006---2011).Waterloo,
Ontario: University of Waterloo; 2012.
11. Mackay JM,Bettcher DW,Minhas R,
Schotte K.Successes and new emerging
challenges in tobacco control: addressing
the vector. Tob Control. 2012;21(2):77---79.
12. TurkStat.Global Adult Tobacco
Survey,2012.Available at: http://www.
turkstat.gov.tr/PreHaberBultenleri.do?
id=13142.Accessed September 12,
2013.
13. Centers for Disease Control and
Prevention.Progress toward eradication
of polio—worldwide,January 2011---
March 2013.MMWR Morb Mortal Wkly
Rep.2013;62(17):335---338.
14. Deshpande J,Ram M,Durranio S,
Wenger J.Detecting polio through sur-
veillance for acute flaccid paralysis (AFP).
J Indian Med Assoc.2005;103(12):671---
675.
15. Hovi T.Surveillance for poliovi-
ruses.Biologicals.2006;34(2):123---126.
16. Mohammadi D.The final push for
polio eradication? Lancet.2012;380
(9840):460---462.
17. Centers for Disease Control and
Prevention.Guide to infection prevention
in outpatient settings: minimum expecta-
tions for safe care.Available at: http://
www.cdc.gov/HAI/pdfs/guidelines/
standatds-of-ambulatory-care-7-2011.
pdf.Accessed September 12,2013.
18. Pronovost P,Needham D,
Berenholtz S,et al.An intervention to
decrease catheter-related bloodstream
infections in the ICU.N Engl J Med.
2006;355(26):2725---2732.
19. Burton DC,Edwards JR,Horan TC,
et al.Methicillin-resistant Staphylococcus
aureus central line-associated blood-
stream infections in US intensive care
units,1997---2007.JAMA. 2009;301
(7):727---736.
20. Malpiedi PJ,Peterson KD,Soe MM,
et al.2011 National and State
Healthcare-Associated Infections Stan-
dardized Infection Ratio Report.Avail-
able at: http://www.cdc.gov/hai/pdfs/
SIR/SIR-Report_02_07_2013.pdf.
Accessed September 12,2013.
21. German RR, Lee LM, Horan JM, et al.
Updated guidelines for evaluating public
health surveillance systems: recommen-
dations from the Guidelines Working
Group.MMWR Recomm Rep.2001;50
(RR-13):1---35.
22. Frieden TR,Mostashari F,Kerker
BD,et al.Adult tobacco use levels after
intensive tobacco control measures: New
York City,2002---2003.Am J Public
Health.2005;95(6):1016---1023.
23. Centers for Disease Control and
Prevention.Decline in smoking preva-
lence—New York City,2002---2006.
MMWR Morb Mortal Wkly Rep. 2007;56
(24):604---608.
24. Maher D,Raviglione T.Why is
a recording and reporting system needed,
and what system is recommended? In:
Frieden T, ed.Toman’s Tuberculosis: Case
Detection,Treatment,and Monitoring—
Questions and Answers.2nd ed.Geneva,
Switzerland: World Health Organization;
2004:270---273.
25. McCord C,Mbaruku G,Pereira C,
et al. The quality of emergency obstetrical
surgery by assistant medical officers in
Tanzanian district hospitals.Health Aff
(Millwood).2009;28(5):w876---w885.
26. Mafigiri DK,McGrath JW,Whalen
CC.Task shifting for tuberculosis control:
a qualitative study of community-based
directly observed therapy in urban
Uganda.Glob Public Health.2012;7
(3):270---284.
27. National Prevention Council.
National Prevention Strategy: America’s
Plan for Better Health and Wellness.
Washington,DC: US Department of
Health and Human Services,Office of
the Surgeon General; 2011.
28. Wilson JQ.Bureaucracy: What Gov-
ernment Agencies Do and Why They Do It.
New York,NY: Basic Books; 1991.
29. Centers for Disease Control and
Prevention.A sustainable planning
guide for healthy communities.Avail-
able at: http://www.cdc.gov/
healthycommunitiesprogram/pdf/
sustainability_guide.pdf.Accessed Sep-
tember 12,2013.
30. Marks JH.What’s the big deal? The
ethics of public-private partnerships re-
lated to food and health.Available at:
http://papers.ssrn.com/sol3/papers.cfm?
abstract_id=2268079.Accessed Sep-
tember 12,2013.
31. World Health Organization.
WHO Framework Convention on
Tobacco Control.Available at: http://
whqlibdoc.who.int/publications/2003/
9241591013.pdf.Accessed September
12, 2013.
32. Lerner BH.One for the Road: Drunk
Driving Since 1900. Baltimore, MD: Johns
Hopkins University Press; 2011.
33. Centers for Disease Control and
Prevention.Increases in quitline calls and
smoking cessation website visitors during
a national tobacco education campaign—
March 19---June 10,2012.MMWR Morb
Mortal Wkly Rep.2012;61(34):667---
670.
34. Terry-McElrath YM,Emery S,
Wakefield MA,et al.Effects of tobacco-
related media campaigns on smoking
among 20-30-year-old adults: longitudi-
nal data from the USA.Tob Control.
2013;22(1):38---45.
35. Tobacco Industry Interference With
Tobacco Control.Geneva,Switzerland:
World Health Organization; 2008.
36. Association of State and Territorial
Health Officials.Budget cuts continue to
affect the health of Americans: update
December 2012.Available at: http://
www.astho.org/budget-cuts-dec-2012.
Accessed September 12,2013.
37. Winslow CEA.The Life of Hermann
Biggs.Philadelphia,PA: Lea & Febiger;
1929.
38. Rubini ME.Fluoridation: the un-
popular controversy.Am J Clin Nutr.
1969;22(10):1343---1345.
39. Lantos JD,Jackson MA,Opel DJ,
et al.Controversies in vaccine mandates.
Curr Probl Pediatr Adolesc Health Care.
2010;40(3):38---58.
40. Chang C,Leighton J,Mostashari F,
et al.The New York City Smoke-Free Air
Act: second-hand smoke as a worker
health and safety issue.Am J Ind Med.
2004;46(2):188---195.
41. Frieden TR,Lerner BH,Rutherford
BR. Lessons from the 1800s: tuberculosis
control in the new millennium.Lancet.
2000;355(9209):1088---1092.
42. Cox LA Jr.Reassessing the human
health benefits from cleaner air.Risk
Anal.2012;32(5):816---829.
43. Homer J,French M.Motorcycle
helmet laws in the United States from
1990 to 2005: politics and public health.
Am J Public Health.2009;99(3):415---
423.
44. Rose G.Rose’s Strategy of Preventive
Medicine.New York,NY: Oxford Univer-
sity Press; 2008.
45. Zhao Z,Smith PJ.Trends in vacci-
nation coverage disparities among chil-
dren,United States,2001---2010.Vac-
cine.2013;31(19):2324---2327.
46. US President’s Emergency Plan for
AIDS Relief.PEPFAR 9th annual report
to Congress.Available at: http://www.
pepfar.gov/documents/organization/
207759.pdf.Accessed September 12,
2013.
EFFECTIVE PUBLIC HEALTH PROGRAM IMPLEMENTATION
22 | Effective Program Implementation |Peer Reviewed |Frieden American Journalof Public Health |January 2014,Vol 104, No. 1
Sacramento,CA: California Department
of Public Health; 2009.
9. Coady MH,Jasek J,Davis K,et al.
Changes in smoking prevalence and
number of cigarettes smoked per day
following the implementation of a com-
prehensive tobacco control plan in New
York City.J Urban Health.2012;89
(5):802---808.
10. International Tobacco Control
Policy Evaluation Project.ITC Uruguay
National Report: Findings From the Wave
1 to 3 Surveys (2006---2011).Waterloo,
Ontario: University of Waterloo; 2012.
11. Mackay JM,Bettcher DW,Minhas R,
Schotte K.Successes and new emerging
challenges in tobacco control: addressing
the vector. Tob Control. 2012;21(2):77---79.
12. TurkStat.Global Adult Tobacco
Survey,2012.Available at: http://www.
turkstat.gov.tr/PreHaberBultenleri.do?
id=13142.Accessed September 12,
2013.
13. Centers for Disease Control and
Prevention.Progress toward eradication
of polio—worldwide,January 2011---
March 2013.MMWR Morb Mortal Wkly
Rep.2013;62(17):335---338.
14. Deshpande J,Ram M,Durranio S,
Wenger J.Detecting polio through sur-
veillance for acute flaccid paralysis (AFP).
J Indian Med Assoc.2005;103(12):671---
675.
15. Hovi T.Surveillance for poliovi-
ruses.Biologicals.2006;34(2):123---126.
16. Mohammadi D.The final push for
polio eradication? Lancet.2012;380
(9840):460---462.
17. Centers for Disease Control and
Prevention.Guide to infection prevention
in outpatient settings: minimum expecta-
tions for safe care.Available at: http://
www.cdc.gov/HAI/pdfs/guidelines/
standatds-of-ambulatory-care-7-2011.
pdf.Accessed September 12,2013.
18. Pronovost P,Needham D,
Berenholtz S,et al.An intervention to
decrease catheter-related bloodstream
infections in the ICU.N Engl J Med.
2006;355(26):2725---2732.
19. Burton DC,Edwards JR,Horan TC,
et al.Methicillin-resistant Staphylococcus
aureus central line-associated blood-
stream infections in US intensive care
units,1997---2007.JAMA. 2009;301
(7):727---736.
20. Malpiedi PJ,Peterson KD,Soe MM,
et al.2011 National and State
Healthcare-Associated Infections Stan-
dardized Infection Ratio Report.Avail-
able at: http://www.cdc.gov/hai/pdfs/
SIR/SIR-Report_02_07_2013.pdf.
Accessed September 12,2013.
21. German RR, Lee LM, Horan JM, et al.
Updated guidelines for evaluating public
health surveillance systems: recommen-
dations from the Guidelines Working
Group.MMWR Recomm Rep.2001;50
(RR-13):1---35.
22. Frieden TR,Mostashari F,Kerker
BD,et al.Adult tobacco use levels after
intensive tobacco control measures: New
York City,2002---2003.Am J Public
Health.2005;95(6):1016---1023.
23. Centers for Disease Control and
Prevention.Decline in smoking preva-
lence—New York City,2002---2006.
MMWR Morb Mortal Wkly Rep. 2007;56
(24):604---608.
24. Maher D,Raviglione T.Why is
a recording and reporting system needed,
and what system is recommended? In:
Frieden T, ed.Toman’s Tuberculosis: Case
Detection,Treatment,and Monitoring—
Questions and Answers.2nd ed.Geneva,
Switzerland: World Health Organization;
2004:270---273.
25. McCord C,Mbaruku G,Pereira C,
et al. The quality of emergency obstetrical
surgery by assistant medical officers in
Tanzanian district hospitals.Health Aff
(Millwood).2009;28(5):w876---w885.
26. Mafigiri DK,McGrath JW,Whalen
CC.Task shifting for tuberculosis control:
a qualitative study of community-based
directly observed therapy in urban
Uganda.Glob Public Health.2012;7
(3):270---284.
27. National Prevention Council.
National Prevention Strategy: America’s
Plan for Better Health and Wellness.
Washington,DC: US Department of
Health and Human Services,Office of
the Surgeon General; 2011.
28. Wilson JQ.Bureaucracy: What Gov-
ernment Agencies Do and Why They Do It.
New York,NY: Basic Books; 1991.
29. Centers for Disease Control and
Prevention.A sustainable planning
guide for healthy communities.Avail-
able at: http://www.cdc.gov/
healthycommunitiesprogram/pdf/
sustainability_guide.pdf.Accessed Sep-
tember 12,2013.
30. Marks JH.What’s the big deal? The
ethics of public-private partnerships re-
lated to food and health.Available at:
http://papers.ssrn.com/sol3/papers.cfm?
abstract_id=2268079.Accessed Sep-
tember 12,2013.
31. World Health Organization.
WHO Framework Convention on
Tobacco Control.Available at: http://
whqlibdoc.who.int/publications/2003/
9241591013.pdf.Accessed September
12, 2013.
32. Lerner BH.One for the Road: Drunk
Driving Since 1900. Baltimore, MD: Johns
Hopkins University Press; 2011.
33. Centers for Disease Control and
Prevention.Increases in quitline calls and
smoking cessation website visitors during
a national tobacco education campaign—
March 19---June 10,2012.MMWR Morb
Mortal Wkly Rep.2012;61(34):667---
670.
34. Terry-McElrath YM,Emery S,
Wakefield MA,et al.Effects of tobacco-
related media campaigns on smoking
among 20-30-year-old adults: longitudi-
nal data from the USA.Tob Control.
2013;22(1):38---45.
35. Tobacco Industry Interference With
Tobacco Control.Geneva,Switzerland:
World Health Organization; 2008.
36. Association of State and Territorial
Health Officials.Budget cuts continue to
affect the health of Americans: update
December 2012.Available at: http://
www.astho.org/budget-cuts-dec-2012.
Accessed September 12,2013.
37. Winslow CEA.The Life of Hermann
Biggs.Philadelphia,PA: Lea & Febiger;
1929.
38. Rubini ME.Fluoridation: the un-
popular controversy.Am J Clin Nutr.
1969;22(10):1343---1345.
39. Lantos JD,Jackson MA,Opel DJ,
et al.Controversies in vaccine mandates.
Curr Probl Pediatr Adolesc Health Care.
2010;40(3):38---58.
40. Chang C,Leighton J,Mostashari F,
et al.The New York City Smoke-Free Air
Act: second-hand smoke as a worker
health and safety issue.Am J Ind Med.
2004;46(2):188---195.
41. Frieden TR,Lerner BH,Rutherford
BR. Lessons from the 1800s: tuberculosis
control in the new millennium.Lancet.
2000;355(9209):1088---1092.
42. Cox LA Jr.Reassessing the human
health benefits from cleaner air.Risk
Anal.2012;32(5):816---829.
43. Homer J,French M.Motorcycle
helmet laws in the United States from
1990 to 2005: politics and public health.
Am J Public Health.2009;99(3):415---
423.
44. Rose G.Rose’s Strategy of Preventive
Medicine.New York,NY: Oxford Univer-
sity Press; 2008.
45. Zhao Z,Smith PJ.Trends in vacci-
nation coverage disparities among chil-
dren,United States,2001---2010.Vac-
cine.2013;31(19):2324---2327.
46. US President’s Emergency Plan for
AIDS Relief.PEPFAR 9th annual report
to Congress.Available at: http://www.
pepfar.gov/documents/organization/
207759.pdf.Accessed September 12,
2013.
EFFECTIVE PUBLIC HEALTH PROGRAM IMPLEMENTATION
22 | Effective Program Implementation |Peer Reviewed |Frieden American Journalof Public Health |January 2014,Vol 104, No. 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.