Project Management: EHR Implementation Plan at Apollo Hospital
VerifiedAdded on 2023/06/04
|9
|2232
|63
Project
AI Summary
This project outlines the plan for implementing Electronic Health Records (EHR) at Apollo Hospital, aiming to transition from manual data keeping to a digital system for increased efficiency and data privacy. It highlights the rationale for change, objectives, and principles, emphasizing improved employee efficiency, patient outcomes, and financial gains. The project addresses the challenges associated with transitioning to EHRs, such as resistance to change, costs, and the need for staff training. It details the change elements, including structural changes, responsibilities, resources, processes, and performance measures, stressing the importance of support structures and a staged introduction process. The change plan involves balancing time, cost, and scope, with stages including decision-making, selection, and pre- and post-implementation phases. The evaluation process begins in the initial infrastructure stage and continues throughout the implementation, with surveys to ensure the project's effectiveness, and it insists on the importance of individual staff members and relationship management.
Project Management 1
PROJECT MANAGEMENT
BY
Course
Tutor
Institution
Location
Date
PROJECT MANAGEMENT
BY
Course
Tutor
Institution
Location
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Project Management 2
Company Overview
Apollo hospital has been ranked among the top best Asian hospitals and among some
of the few hospitals that have embraced and leveraged different technological trends with a
view to facilitative effective and seamless healthcare delivery. However, there are a number
of technologies that the hospital needs to adopt with a view to increase efficiency, improve
patient-staff communication and also to improve patient data recording and privacy within
the organization. The organization still relies on paper documentation as their main record-
keeping method. However, given the nature of technology today, there are several methods of
keeping patient data some of which are digital (Madden et al., 2016).
Rationale for the Change
Therefore, to increase efficiency and privacy of the patient’s data, there is a need for the
hospital to change into the electronic and digital method of data keep known as the EHR
system.
Change Objectives and Principals
The technology makes sharing of information easy and safe as it is instant and secured
(Ben-Assuli, 2015). Consequently, building on these capabilities of the technology, it is clear
that it will be of much importance to Apollo Hospital upon its implementation. The benefits
of the implementation of EHR include improved employee efficiency, improved patient
outcomes, and financial gain (Palvia et al., 2015).
Project Summary
Over the past few years, most health organizations have been transitioning from
manual data recording and keeping systems to electronic health records (EHRs) (Charles et
al., 2013). The initiative of EHRs was also established a few years ago and at the moment
most of the health institutions have been trying to leverage the use of these computerized
records (Fragidis & Chatzoglou, 2018). The transitioning from the manual systems has led to
Company Overview
Apollo hospital has been ranked among the top best Asian hospitals and among some
of the few hospitals that have embraced and leveraged different technological trends with a
view to facilitative effective and seamless healthcare delivery. However, there are a number
of technologies that the hospital needs to adopt with a view to increase efficiency, improve
patient-staff communication and also to improve patient data recording and privacy within
the organization. The organization still relies on paper documentation as their main record-
keeping method. However, given the nature of technology today, there are several methods of
keeping patient data some of which are digital (Madden et al., 2016).
Rationale for the Change
Therefore, to increase efficiency and privacy of the patient’s data, there is a need for the
hospital to change into the electronic and digital method of data keep known as the EHR
system.
Change Objectives and Principals
The technology makes sharing of information easy and safe as it is instant and secured
(Ben-Assuli, 2015). Consequently, building on these capabilities of the technology, it is clear
that it will be of much importance to Apollo Hospital upon its implementation. The benefits
of the implementation of EHR include improved employee efficiency, improved patient
outcomes, and financial gain (Palvia et al., 2015).
Project Summary
Over the past few years, most health organizations have been transitioning from
manual data recording and keeping systems to electronic health records (EHRs) (Charles et
al., 2013). The initiative of EHRs was also established a few years ago and at the moment
most of the health institutions have been trying to leverage the use of these computerized
records (Fragidis & Chatzoglou, 2018). The transitioning from the manual systems has led to
Project Management 3
a lot of changes in the documentation and data keeping processes in hospitals (Nguyen et al.,
2014). Moreover, it has brought about changes to the staff in the hospitals. This is because it
is a real-time patient centred record digital version that allows medical staff to access
information instantly when need be (Patterson et al., 2017). It contains treatment and medical
history of the patients which makes it possible for healthcare providers to make easy follow-
ups on a patient’s condition (Friend et al., 2017).
Transitioning from the conventional data keeping method to this digital version will
come along with a number of challenges and losses for the key stakeholders in the change
process (Liao et al., 2017). Adapting to change is quite difficult and this applies to almost all
industries. Creating a vision and urgency for the proposed change is necessary as this will
help stakeholders understand the essence of the change. It is worth to note that if the entire
working staff understands the necessity of change, it will be easy to instil the change since
they can resonate with the fact that change is beneficial and this makes it easy for the
employees to embrace the change and become more motivated to the change hence
facilitating the process of change smoothly (Van et al., 2015). Therefore it is essential for
stakeholders to understand how change affects the employee efficiency and performance and
patient outcomes.
Possible losses associated with EHRs include lack of standardized EHR products,
costs and resistance to change by the members of staff (Heisey-Grove et al., 2014). This is
brought by the difficulty from the use especially during the initial stages of implementation
which leads to the reduction of productivity and finally lack of perceived benefits to the
providers since the benefits accrued are those of society and the payers (Gabriel et al., 2014).
The transition requires a change in software and also training among the employees with a
view to equip them with the necessary skills required in the operation of the technology
(Adler-Milstein et al., 2014). Due to the day in day out technological advancements,
a lot of changes in the documentation and data keeping processes in hospitals (Nguyen et al.,
2014). Moreover, it has brought about changes to the staff in the hospitals. This is because it
is a real-time patient centred record digital version that allows medical staff to access
information instantly when need be (Patterson et al., 2017). It contains treatment and medical
history of the patients which makes it possible for healthcare providers to make easy follow-
ups on a patient’s condition (Friend et al., 2017).
Transitioning from the conventional data keeping method to this digital version will
come along with a number of challenges and losses for the key stakeholders in the change
process (Liao et al., 2017). Adapting to change is quite difficult and this applies to almost all
industries. Creating a vision and urgency for the proposed change is necessary as this will
help stakeholders understand the essence of the change. It is worth to note that if the entire
working staff understands the necessity of change, it will be easy to instil the change since
they can resonate with the fact that change is beneficial and this makes it easy for the
employees to embrace the change and become more motivated to the change hence
facilitating the process of change smoothly (Van et al., 2015). Therefore it is essential for
stakeholders to understand how change affects the employee efficiency and performance and
patient outcomes.
Possible losses associated with EHRs include lack of standardized EHR products,
costs and resistance to change by the members of staff (Heisey-Grove et al., 2014). This is
brought by the difficulty from the use especially during the initial stages of implementation
which leads to the reduction of productivity and finally lack of perceived benefits to the
providers since the benefits accrued are those of society and the payers (Gabriel et al., 2014).
The transition requires a change in software and also training among the employees with a
view to equip them with the necessary skills required in the operation of the technology
(Adler-Milstein et al., 2014). Due to the day in day out technological advancements,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Project Management 4
organizations will be faced by the challenge of the ever-changing electronic health systems
due to software implementations (Chan et al., 2016). Consequently, the advantages from the
adaption of change clearly outweigh the challenges faced by employees during the change
transition (Vahdat et al., 2018).
Change Elements
Structural, responsibilities, resources, processes, and performance measures
For the technology to be effectively implemented in the institution, there are a number
of structures that will require change. For instance, the responsibilities of the staff members,
processes, structures of data keeping, timeframes and resources will change. The support
structure will change since most of the staff members responsible for data keeping will be
replaced with trained personnel who have the know-how of operating the system.
Need for Particular Support Structures
Selection of a champion will be significant as he will act as the technology’s advocate
through encouragement and also through providing the project such as redesigning and
assessing workflow, conducting training to the staff members, understanding the financial
issues and finally evaluating the process of implementation.
Staging the Introduction Change Process
On developing a realistic EHR change plan, there are a lot of pieces that need to be
coordinated before the execution of an EHR successful implementation. The introduction of
the change process needs to be staged since there will be a change in the software systems in
the organization.
Impact on Workloads
The technology will have an impact on the workloads hence this needs to be
managed. The technology will reduce the workload of the staffs since work around the
processes will be eliminated. Health care providers such as the nurses, clinicians, and
organizations will be faced by the challenge of the ever-changing electronic health systems
due to software implementations (Chan et al., 2016). Consequently, the advantages from the
adaption of change clearly outweigh the challenges faced by employees during the change
transition (Vahdat et al., 2018).
Change Elements
Structural, responsibilities, resources, processes, and performance measures
For the technology to be effectively implemented in the institution, there are a number
of structures that will require change. For instance, the responsibilities of the staff members,
processes, structures of data keeping, timeframes and resources will change. The support
structure will change since most of the staff members responsible for data keeping will be
replaced with trained personnel who have the know-how of operating the system.
Need for Particular Support Structures
Selection of a champion will be significant as he will act as the technology’s advocate
through encouragement and also through providing the project such as redesigning and
assessing workflow, conducting training to the staff members, understanding the financial
issues and finally evaluating the process of implementation.
Staging the Introduction Change Process
On developing a realistic EHR change plan, there are a lot of pieces that need to be
coordinated before the execution of an EHR successful implementation. The introduction of
the change process needs to be staged since there will be a change in the software systems in
the organization.
Impact on Workloads
The technology will have an impact on the workloads hence this needs to be
managed. The technology will reduce the workload of the staffs since work around the
processes will be eliminated. Health care providers such as the nurses, clinicians, and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Project Management 5
physicians should be informed frequently about the progress of the on-going change so as to
less painfully experience the benefits. Keeping in mind that the patient care comes first and
the main reasons for implementing change are ultimately for patient safety and care.
Therefore it is crucial to keep the staff members continuously at the forefront of their minds
throughout the implementation process. Communications to the staffs should begin as early
as possible regardless of the scale or the scope of a project so as to prepare the members of
staff of what is clearly to come.
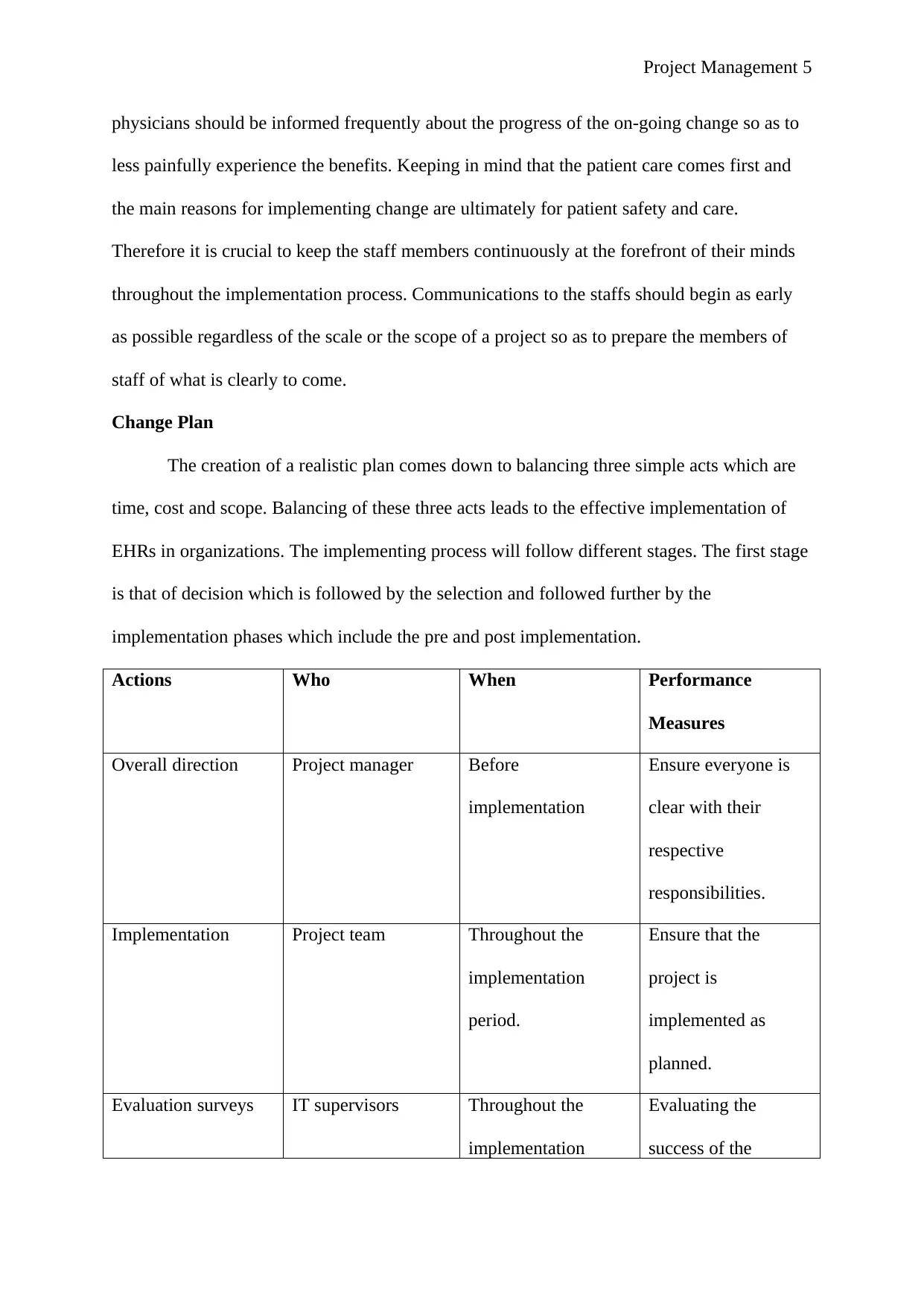
Change Plan
The creation of a realistic plan comes down to balancing three simple acts which are
time, cost and scope. Balancing of these three acts leads to the effective implementation of
EHRs in organizations. The implementing process will follow different stages. The first stage
is that of decision which is followed by the selection and followed further by the
implementation phases which include the pre and post implementation.
Actions Who When Performance
Measures
Overall direction Project manager Before
implementation
Ensure everyone is
clear with their
respective
responsibilities.
Implementation Project team Throughout the
implementation
period.
Ensure that the
project is
implemented as
planned.
Evaluation surveys IT supervisors Throughout the
implementation
Evaluating the
success of the
physicians should be informed frequently about the progress of the on-going change so as to
less painfully experience the benefits. Keeping in mind that the patient care comes first and
the main reasons for implementing change are ultimately for patient safety and care.
Therefore it is crucial to keep the staff members continuously at the forefront of their minds
throughout the implementation process. Communications to the staffs should begin as early
as possible regardless of the scale or the scope of a project so as to prepare the members of
staff of what is clearly to come.
Change Plan
The creation of a realistic plan comes down to balancing three simple acts which are
time, cost and scope. Balancing of these three acts leads to the effective implementation of
EHRs in organizations. The implementing process will follow different stages. The first stage
is that of decision which is followed by the selection and followed further by the
implementation phases which include the pre and post implementation.
Actions Who When Performance
Measures
Overall direction Project manager Before
implementation
Ensure everyone is
clear with their
respective
responsibilities.
Implementation Project team Throughout the
implementation
period.
Ensure that the
project is
implemented as
planned.
Evaluation surveys IT supervisors Throughout the
implementation
Evaluating the
success of the
Project Management 6
period. change.
Consolidation
Clearly, there is a need to adopt a flexible strategy in the change management while
implementing the use of EHRs in the Apollo organization. The strategy should clearly insist
on the importance on the role of individual staff members and relationship management so as
to help the entire staff to manage change. The practice staff must have set goals and visions
for the implementation of EHRs and the staff members must buy into the project.
Evaluation
The evaluation of the implementation process will begin in the infrastructure initial
stage. At this stage, the coordinator will ensure that the technology is implemented as
required. The constant survey will also be made throughout the implementation process to
ensure that everything is done as scheduled and planned. Upon completion, the final survey
will be conducted to ensure that every step has been done as planned. The effectiveness of the
change plan will be evaluated based on the outcomes of the technology.
period. change.
Consolidation
Clearly, there is a need to adopt a flexible strategy in the change management while
implementing the use of EHRs in the Apollo organization. The strategy should clearly insist
on the importance on the role of individual staff members and relationship management so as
to help the entire staff to manage change. The practice staff must have set goals and visions
for the implementation of EHRs and the staff members must buy into the project.
Evaluation
The evaluation of the implementation process will begin in the infrastructure initial
stage. At this stage, the coordinator will ensure that the technology is implemented as
required. The constant survey will also be made throughout the implementation process to
ensure that everything is done as scheduled and planned. Upon completion, the final survey
will be conducted to ensure that every step has been done as planned. The effectiveness of the
change plan will be evaluated based on the outcomes of the technology.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Project Management 7
References
Adler-Milstein, J., DesRoches, C.M., Furukawa, M.F., Worzala, C., Charles, D., Kralovec,
P., Stalley, S. and Jha, A.K., 2014. More than half of US hospitals have at least a basic EHR,
but stage 2 criteria remain challenging for most. Health Affairs, 33(9), pp.1664-1671.
Bajwa, N.K., Singh, H. and De, K.K., 2017. Critical Success Factors in Electronic Health
Records (EHR) Implementation: An Exploratory Study in North India. International Journal
of Healthcare Information Systems and Informatics (IJHISI), 12(2), pp.1-17.
Ben-Assuli, O., 2015. Electronic health records, adoption, quality of care, legal and privacy
issues and their implementation in emergency departments. Health Policy, 119(3), pp.287-
297.
Chan, K.S., Kharrazi, H., Parikh, M.A. and Ford, E.W., 2016. Assessing electronic health
record implementation challenges using item response theory. Am J Manag Care, 22(12),
pp.e409-e415.
Charles, D., Gabriel, M. and Furukawa, M.F., 2013. Adoption of electronic health record
systems among US non-federal acute care hospitals: 2008-2012. ONC data brief, 9, pp.1-9.
Fragidis, L.L. and Chatzoglou, P.D., 2018. Implementation of a nationwide electronic health
record (EHR) The international experience in 13 countries. International journal of health
care quality assurance, 31(2), pp.116-130.
Friend, T.H., Jennings, S.J. and Levine, W.C., 2017. Communication patterns in the
perioperative environment during epic electronic health record system
implementation. Journal of medical systems, 41(2), p.22.
Gabriel, M.H., Jones, E.B., Samy, L. and King, J., 2014. Progress and challenges:
implementation and use of health information technology among critical-access
hospitals. Health Affairs, 33(7), pp.1262-1270.
References
Adler-Milstein, J., DesRoches, C.M., Furukawa, M.F., Worzala, C., Charles, D., Kralovec,
P., Stalley, S. and Jha, A.K., 2014. More than half of US hospitals have at least a basic EHR,
but stage 2 criteria remain challenging for most. Health Affairs, 33(9), pp.1664-1671.
Bajwa, N.K., Singh, H. and De, K.K., 2017. Critical Success Factors in Electronic Health
Records (EHR) Implementation: An Exploratory Study in North India. International Journal
of Healthcare Information Systems and Informatics (IJHISI), 12(2), pp.1-17.
Ben-Assuli, O., 2015. Electronic health records, adoption, quality of care, legal and privacy
issues and their implementation in emergency departments. Health Policy, 119(3), pp.287-
297.
Chan, K.S., Kharrazi, H., Parikh, M.A. and Ford, E.W., 2016. Assessing electronic health
record implementation challenges using item response theory. Am J Manag Care, 22(12),
pp.e409-e415.
Charles, D., Gabriel, M. and Furukawa, M.F., 2013. Adoption of electronic health record
systems among US non-federal acute care hospitals: 2008-2012. ONC data brief, 9, pp.1-9.
Fragidis, L.L. and Chatzoglou, P.D., 2018. Implementation of a nationwide electronic health
record (EHR) The international experience in 13 countries. International journal of health
care quality assurance, 31(2), pp.116-130.
Friend, T.H., Jennings, S.J. and Levine, W.C., 2017. Communication patterns in the
perioperative environment during epic electronic health record system
implementation. Journal of medical systems, 41(2), p.22.
Gabriel, M.H., Jones, E.B., Samy, L. and King, J., 2014. Progress and challenges:
implementation and use of health information technology among critical-access
hospitals. Health Affairs, 33(7), pp.1262-1270.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Project Management 8
Heisey-Grove, D., Danehy, L.N., Consolazio, M., Lynch, K. and Mostashari, F., 2014. A
national study of challenges to electronic health record adoption and meaningful use. Medical
care, 52(2), pp.144-148.
Liao, T.V., Rabinovich, M., Abraham, P., Perez, S., DiPlotti, C., Han, J.E., Martin, G.S. and
Honig, E., 2017. Evaluation of medication errors with implementation of electronic health
record technology in the medical intensive care unit. Open Access Journal of Clinical
Trials, 9, pp.31-40.
Madden, J.M., Lakoma, M.D., Rusinak, D., Lu, C.Y. and Soumerai, S.B., 2016. Missing
clinical and behavioral health data in a large electronic health record (EHR) system. Journal
of the American Medical Informatics Association, 23(6), pp.1143-1149.
Nguyen, L., Bellucci, E. and Nguyen, L.T., 2014. Electronic health records implementation:
an evaluation of information system impact and contingency factors. International journal of
medical informatics, 83(11), pp.779-796.
Palvia, P., Jacks, T. and Brown, W.S., 2015. Critical Issues in EHR Implementation: Provider
and Vendor Perspectives. CAIS, 36, p.36.
Patterson, E.S., Anders, S. and Moffatt-Bruce, S., 2017, June. Clustering and Prioritizing
Patient Safety Issues during EHR Implementation and Upgrades in Hospital Settings.
In Proceedings of the International Symposium on Human Factors and Ergonomics in Health
Care (Vol. 6, No. 1, pp. 125-131). Sage India: New Delhi, India: SAGE Publications.
Vahdat, V., Griffin, J.A., Stahl, J.E. and Yang, F.C., 2018. Analysis of the effects of EHR
implementation on timeliness of care in a dermatology clinic: a simulation study. Journal of
the American Medical Informatics Association.
Van den Heuvel, S., Schalk, R. and van Assen, M.A., 2015. Does a well-informed employee
have a more positive attitude toward change? The mediating role of psychological contract
Heisey-Grove, D., Danehy, L.N., Consolazio, M., Lynch, K. and Mostashari, F., 2014. A
national study of challenges to electronic health record adoption and meaningful use. Medical
care, 52(2), pp.144-148.
Liao, T.V., Rabinovich, M., Abraham, P., Perez, S., DiPlotti, C., Han, J.E., Martin, G.S. and
Honig, E., 2017. Evaluation of medication errors with implementation of electronic health
record technology in the medical intensive care unit. Open Access Journal of Clinical
Trials, 9, pp.31-40.
Madden, J.M., Lakoma, M.D., Rusinak, D., Lu, C.Y. and Soumerai, S.B., 2016. Missing
clinical and behavioral health data in a large electronic health record (EHR) system. Journal
of the American Medical Informatics Association, 23(6), pp.1143-1149.
Nguyen, L., Bellucci, E. and Nguyen, L.T., 2014. Electronic health records implementation:
an evaluation of information system impact and contingency factors. International journal of
medical informatics, 83(11), pp.779-796.
Palvia, P., Jacks, T. and Brown, W.S., 2015. Critical Issues in EHR Implementation: Provider
and Vendor Perspectives. CAIS, 36, p.36.
Patterson, E.S., Anders, S. and Moffatt-Bruce, S., 2017, June. Clustering and Prioritizing
Patient Safety Issues during EHR Implementation and Upgrades in Hospital Settings.
In Proceedings of the International Symposium on Human Factors and Ergonomics in Health
Care (Vol. 6, No. 1, pp. 125-131). Sage India: New Delhi, India: SAGE Publications.
Vahdat, V., Griffin, J.A., Stahl, J.E. and Yang, F.C., 2018. Analysis of the effects of EHR
implementation on timeliness of care in a dermatology clinic: a simulation study. Journal of
the American Medical Informatics Association.
Van den Heuvel, S., Schalk, R. and van Assen, M.A., 2015. Does a well-informed employee
have a more positive attitude toward change? The mediating role of psychological contract

Project Management 9
fulfillment, trust, and perceived need for change. The Journal of Applied Behavioral
Science, 51(3), pp.401-422.
fulfillment, trust, and perceived need for change. The Journal of Applied Behavioral
Science, 51(3), pp.401-422.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





