Analysis of EIA Frameworks for E-Health Record Implementation
VerifiedAdded on 2023/06/12
|11
|3393
|81
Report
AI Summary
This report evaluates and discusses various Enterprise Information Architecture (EIA) frameworks for implementing electronic health records (EHR), aiming to improve healthcare service delivery through e-governance. It analyzes models like the Federal Enterprise Architecture Model, TOGAF, Department of Defense Architecture Framework, and Zachman Architecture Model, highlighting the importance of interoperability and data integration. The proposed framework seeks to eliminate the disadvantages of existing models, emphasizing data accessibility, cost-effectiveness, and interoperability. Functional elements such as resource management, billing, departmental support, and clinical care delivery are discussed, along with challenges like security and system availability. The report concludes with recommendations for further system improvements, underscoring the benefits of EHRs for both healthcare providers and patients. Desklib provides access to this report, along with numerous other solved assignments and study resources.

EIA IMPLEMENTATION
Name of the Student:
Name of the University:
Author Note:
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

EIA IMPLEMENTATION
Executive Summery
The electronic health record is the way of keeping the health record regarding the patients. This
is an advanced way of e-governance. The main aim of the electronic health record is to keep
the record of the health record by the health care providers. The health records can be shared
among the doctors and other medical practicing people. E-health record can be implemented
using EIA framework. The main purpose of this paper is to evaluate and discuss different health
EIA framework for the implementation of the e-health record. Certain framework has been
proposed after the analysis of different frameworks and it can be assumed that the proposed
framework will eliminate all the disadvantages of the previous frameworks. The paper
concludes that e-health record will be beneficial for the users. Some recommendations have
been made for the further improvement of the system.
<Student Name> Page | i
Executive Summery
The electronic health record is the way of keeping the health record regarding the patients. This
is an advanced way of e-governance. The main aim of the electronic health record is to keep
the record of the health record by the health care providers. The health records can be shared
among the doctors and other medical practicing people. E-health record can be implemented
using EIA framework. The main purpose of this paper is to evaluate and discuss different health
EIA framework for the implementation of the e-health record. Certain framework has been
proposed after the analysis of different frameworks and it can be assumed that the proposed
framework will eliminate all the disadvantages of the previous frameworks. The paper
concludes that e-health record will be beneficial for the users. Some recommendations have
been made for the further improvement of the system.
<Student Name> Page | i
EIA IMPLEMENTATION
Table of Contents
1.0 Introduction...............................................................................................................................1
2.0 Architecture regarding Enterprise Information.........................................................................1
2.1Model regarding Enterprise Information...............................................................................1
2.2 Conceptual level:...................................................................................................................2
3.0 Information Integration and management...............................................................................4
3.1 Functional elements :............................................................................................................4
3.2 Challenges:.............................................................................................................................5
3.2 Methods of managing the challenges:..................................................................................6
4.0 Conclusion..................................................................................................................................6
5.0 Recommendation......................................................................................................................6
Table of Figures
Figure 1: Block Diagram at Conceptual Level for the proposed E-Health Record...........................6
(Source: Created by author)............................................................................................................6
Figure 2: Architecture of Health Care Information System.............................................................7
(Source: Vogel, JAlonso Coello and Rada 2017 )‐ .............................................................................7
<Student Name> Page | ii
Table of Contents
1.0 Introduction...............................................................................................................................1
2.0 Architecture regarding Enterprise Information.........................................................................1
2.1Model regarding Enterprise Information...............................................................................1
2.2 Conceptual level:...................................................................................................................2
3.0 Information Integration and management...............................................................................4
3.1 Functional elements :............................................................................................................4
3.2 Challenges:.............................................................................................................................5
3.2 Methods of managing the challenges:..................................................................................6
4.0 Conclusion..................................................................................................................................6
5.0 Recommendation......................................................................................................................6
Table of Figures
Figure 1: Block Diagram at Conceptual Level for the proposed E-Health Record...........................6
(Source: Created by author)............................................................................................................6
Figure 2: Architecture of Health Care Information System.............................................................7
(Source: Vogel, JAlonso Coello and Rada 2017 )‐ .............................................................................7
<Student Name> Page | ii
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EIA IMPLEMENTATION
1.0 Introduction
The advancement of technology has opened up a way to get all the relevant information
from the media regarding a service or the organizations. The use of internet ids becoming
important and the governments have realized its importance for providing the service to
the people. Providing service through the internet by the government is known as e-
governance. Government is using internet for controlling and monitoring the system and
the services provided by them. This bill has made the health providers to keep the
electronic record of the patients. The data integration is achieved by the health record as it
allows to share the patient details among the care providers. The patients and the
healthcare providers.
Enterprise information architecture has been used to develop th ehelath care record
keeping model. This framework provides the logical way of designing the way for
implementation of the healthcare record. The development of the health care record will be
done according to the methods and the pattern provided by EIA framework. The risk
assessment of the developed system will also be done by this framework.
2.0 Architecture regarding Enterprise Information
2.1Model regarding Enterprise Information
In order to develop the health record various EIA model can be used. These are-
Federal Enterprise Architecture Model
The open Group Model
Department of Defense Architecture Model
Zachman Architecture Model
Problem regarding interoperability can be solved by Zachmn Model. The ideas in this
model are combined and expressed into the combination of five columns and six rows. In order
to implement the health record with proper functioning the interoperability is needed.
Requirements for describing the enterprise business are described in this model. However, this
model does not indicate any sequential steps for the development of the architecture.The use
of Federal Enterprise Architecture can be useful in elimination this problem. This model clearly
states the exact mission and vision of the organization.
Advantages
There are certain advantages of electronic health record. The data in the record can be
accessed from the any parts of the place at any time. The availability of data is helpful for
boththe health care providers and the patients in argent basis. Some of the features of the
electronic health records which attribute to its advantage-
Integration of data: One of the main advantage of this system is data integration. All the
data associated to the health conditions and treatments of the patients are recorded in
the health record. This enables the options to use the past medical records as a
<Student Name> Page | 1
1.0 Introduction
The advancement of technology has opened up a way to get all the relevant information
from the media regarding a service or the organizations. The use of internet ids becoming
important and the governments have realized its importance for providing the service to
the people. Providing service through the internet by the government is known as e-
governance. Government is using internet for controlling and monitoring the system and
the services provided by them. This bill has made the health providers to keep the
electronic record of the patients. The data integration is achieved by the health record as it
allows to share the patient details among the care providers. The patients and the
healthcare providers.
Enterprise information architecture has been used to develop th ehelath care record
keeping model. This framework provides the logical way of designing the way for
implementation of the healthcare record. The development of the health care record will be
done according to the methods and the pattern provided by EIA framework. The risk
assessment of the developed system will also be done by this framework.
2.0 Architecture regarding Enterprise Information
2.1Model regarding Enterprise Information
In order to develop the health record various EIA model can be used. These are-
Federal Enterprise Architecture Model
The open Group Model
Department of Defense Architecture Model
Zachman Architecture Model
Problem regarding interoperability can be solved by Zachmn Model. The ideas in this
model are combined and expressed into the combination of five columns and six rows. In order
to implement the health record with proper functioning the interoperability is needed.
Requirements for describing the enterprise business are described in this model. However, this
model does not indicate any sequential steps for the development of the architecture.The use
of Federal Enterprise Architecture can be useful in elimination this problem. This model clearly
states the exact mission and vision of the organization.
Advantages
There are certain advantages of electronic health record. The data in the record can be
accessed from the any parts of the place at any time. The availability of data is helpful for
boththe health care providers and the patients in argent basis. Some of the features of the
electronic health records which attribute to its advantage-
Integration of data: One of the main advantage of this system is data integration. All the
data associated to the health conditions and treatments of the patients are recorded in
the health record. This enables the options to use the past medical records as a
<Student Name> Page | 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EIA IMPLEMENTATION
reference for evaluation of the current health status of the patient. The data can be
accessed from the health record in case if the patient can not provide relevant
information about his or health . The records are electronically stored, so there are a
few chances for the record misplacement.
Cost effectiveness: Another major advantage of using the electronic health record
system is that, it reduces the cost in an effective measure (Andersen et al.2017). The
initial implementation of the framework and the system may cost some amount of
resources; however, the system will be cost effective in long run.
Interoperability elimination: Interoperability refers the interconnection between the two
working system, when one system works for another system (Farooq et al. 2015). It can
happen in three levels-data service and process. The main attribute of the electronic
health record is to eliminate the inoperability property. Using the EIA framework, this
property can be removed.
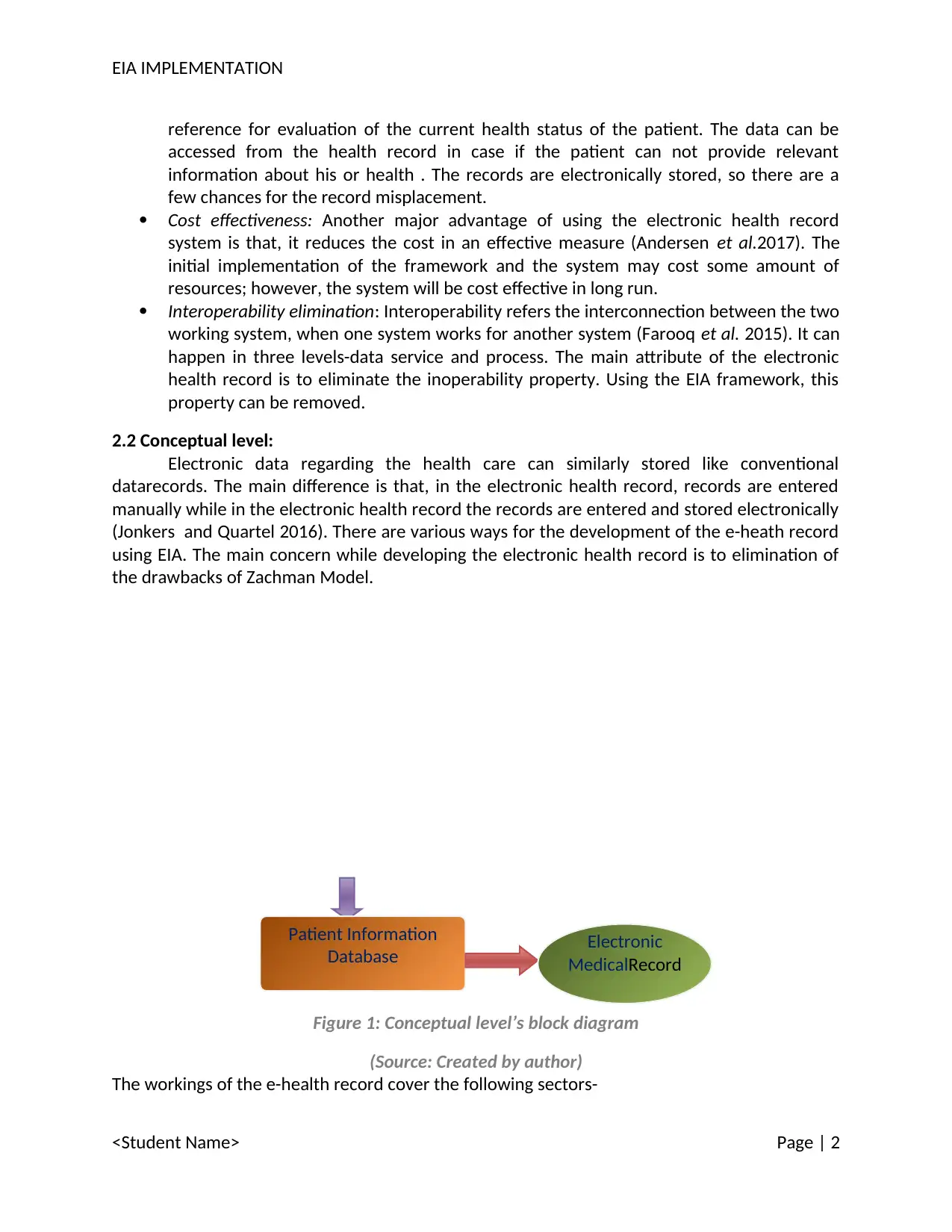
2.2 Conceptual level:
Electronic data regarding the health care can similarly stored like conventional
datarecords. The main difference is that, in the electronic health record, records are entered
manually while in the electronic health record the records are entered and stored electronically
(Jonkers and Quartel 2016). There are various ways for the development of the e-heath record
using EIA. The main concern while developing the electronic health record is to elimination of
the drawbacks of Zachman Model.
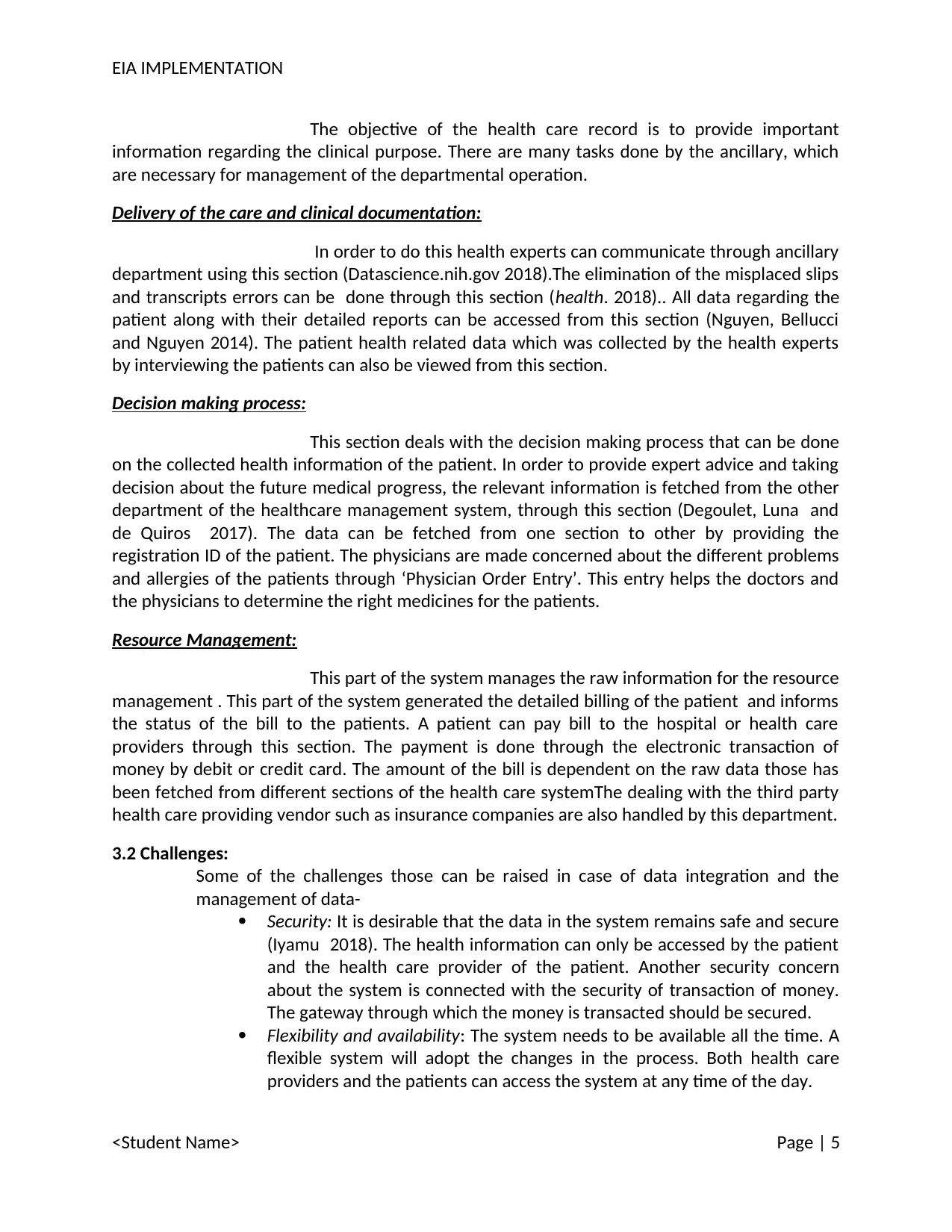
Figure 1: Conceptual level’s block diagram
(Source: Created by author)
The workings of the e-health record cover the following sectors-
<Student Name> Page | 2
Patient Information
Database Electronic
MedicalRecord
reference for evaluation of the current health status of the patient. The data can be
accessed from the health record in case if the patient can not provide relevant
information about his or health . The records are electronically stored, so there are a
few chances for the record misplacement.
Cost effectiveness: Another major advantage of using the electronic health record
system is that, it reduces the cost in an effective measure (Andersen et al.2017). The
initial implementation of the framework and the system may cost some amount of
resources; however, the system will be cost effective in long run.
Interoperability elimination: Interoperability refers the interconnection between the two
working system, when one system works for another system (Farooq et al. 2015). It can
happen in three levels-data service and process. The main attribute of the electronic
health record is to eliminate the inoperability property. Using the EIA framework, this
property can be removed.
2.2 Conceptual level:
Electronic data regarding the health care can similarly stored like conventional
datarecords. The main difference is that, in the electronic health record, records are entered
manually while in the electronic health record the records are entered and stored electronically
(Jonkers and Quartel 2016). There are various ways for the development of the e-heath record
using EIA. The main concern while developing the electronic health record is to elimination of
the drawbacks of Zachman Model.
Figure 1: Conceptual level’s block diagram
(Source: Created by author)
The workings of the e-health record cover the following sectors-
<Student Name> Page | 2
Patient Information
Database Electronic
MedicalRecord
EIA IMPLEMENTATION
Providing relevant information regarding the patient: This section will
include all the relevant information regarding the health of the patients. The relevant
information covers the details about the prescribed medicine and health checkup information.
The sub section of this part is ‘patient management’, which keeps the personal information of
the patient such as name and identification details of the patient (Romero and Vernadat
2016).This information helps to keep the details of the patient in an organized way and the set
of information can be shared among the other health care providers if it is necessary. The
clinical data is stored in the clinical information system. The clinical information is connected to
the system database.
Managing the information system: This section holds the
information regarding the patient’s health policies and other medical facilities. This is the
section, which can be accessed by the patients and health officials only.
Data Domain: It is the master data storage which is centralized in
manner.
Aim of the proposed framework:
The system aims to provide the information storage and the
information sharing among the health experts and the patients. The data integration related to
the service is used in this system.
<Student Name> Page | 3
Providing relevant information regarding the patient: This section will
include all the relevant information regarding the health of the patients. The relevant
information covers the details about the prescribed medicine and health checkup information.
The sub section of this part is ‘patient management’, which keeps the personal information of
the patient such as name and identification details of the patient (Romero and Vernadat
2016).This information helps to keep the details of the patient in an organized way and the set
of information can be shared among the other health care providers if it is necessary. The
clinical data is stored in the clinical information system. The clinical information is connected to
the system database.
Managing the information system: This section holds the
information regarding the patient’s health policies and other medical facilities. This is the
section, which can be accessed by the patients and health officials only.
Data Domain: It is the master data storage which is centralized in
manner.
Aim of the proposed framework:
The system aims to provide the information storage and the
information sharing among the health experts and the patients. The data integration related to
the service is used in this system.
<Student Name> Page | 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EIA IMPLEMENTATION
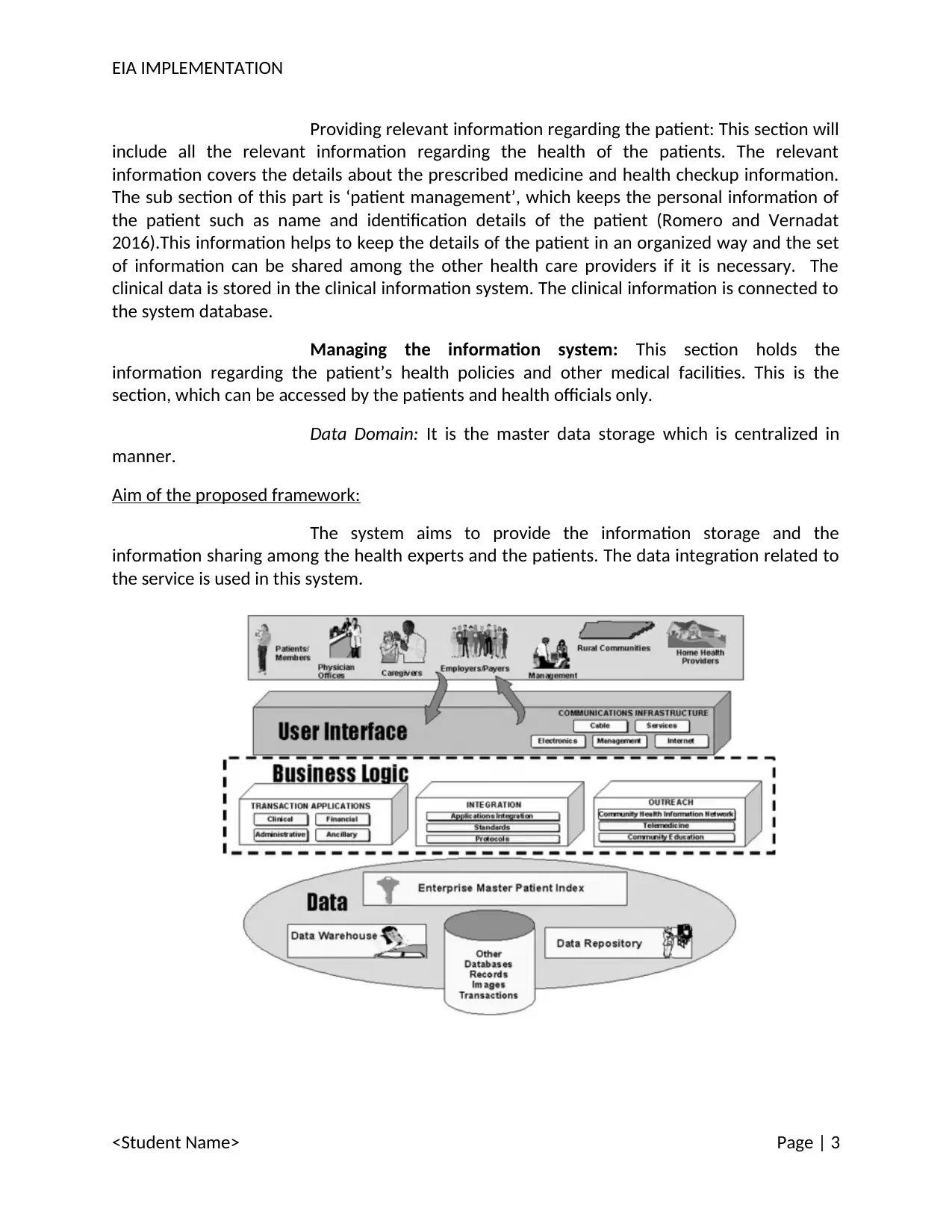
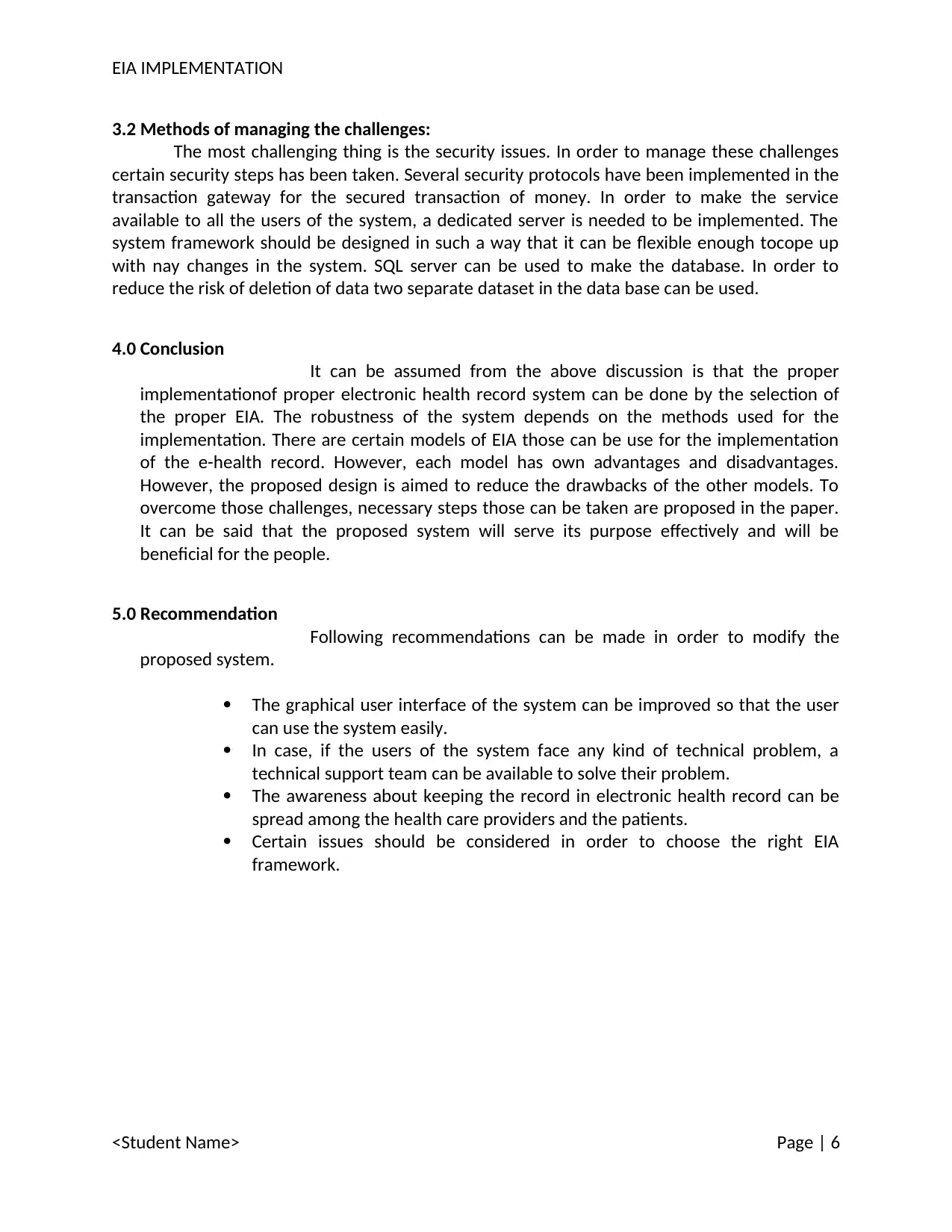
Figure 2: Architecture of Health Care Information System
(Source:Vogel, JAlonso Coello and Rada 2017 )‐
3.0 Information Integration and management
3.1 Functional elements :
The functional components in health care information system have different
important purpose. Some of the functional elements are –
Management of resource.
Billing
Managing finance
Supporting the department
Providing the care and delivery
Billing and management of patient:
This section of the system deals with detailed information of the
patients. Theses information is helpful for the identification of the patients and making the bill.
The billing task is proposed to be automated in the system (Julia, Kurt and Ulf 2017). The use of
‘master patient index’ has been proposed by the hospital, through which they can keep track of
the patents (Singh 2018). This master index helps to integrate the data between hospitals,
health care providers and patients.
Registration details stored in the system serves as the reference
during the billing process. In the other case such as the billing and report generation process for
the laboratory and medicine, the patient is referenced and identified by the name and the
registration number (Fernandes and Fragoso 2017). The data is stored in the centralized data
base (Jones et al. 2014). The access of the data base is permitted only to the authorized user
(Yuehong et al. 2016). The fetching of the information can be triggered other activities such as
retrieval of the prescription and past medical records. Duplicate of the entire database is made
for the use of the hospitals and healthcare providers.
This part of the system also maintains scheduling issues. In health
care function, scheduling is a complex process. It requires the synchronization of the availability
of health care service. The availability of the service at hospitals and the health care clinics are
not same for each day (Wang et al. 2016). The scheduling helps to inform the patients about
the time of availability of the requested service. Another challenging activity managed by this
section is the resource management (Weaver et al. 2016).Resources, in this case, indicate the
type and kind of service a patient can avail.
Handling the Department:
<Student Name> Page | 4
Figure 2: Architecture of Health Care Information System
(Source:Vogel, JAlonso Coello and Rada 2017 )‐
3.0 Information Integration and management
3.1 Functional elements :
The functional components in health care information system have different
important purpose. Some of the functional elements are –
Management of resource.
Billing
Managing finance
Supporting the department
Providing the care and delivery
Billing and management of patient:
This section of the system deals with detailed information of the
patients. Theses information is helpful for the identification of the patients and making the bill.
The billing task is proposed to be automated in the system (Julia, Kurt and Ulf 2017). The use of
‘master patient index’ has been proposed by the hospital, through which they can keep track of
the patents (Singh 2018). This master index helps to integrate the data between hospitals,
health care providers and patients.
Registration details stored in the system serves as the reference
during the billing process. In the other case such as the billing and report generation process for
the laboratory and medicine, the patient is referenced and identified by the name and the
registration number (Fernandes and Fragoso 2017). The data is stored in the centralized data
base (Jones et al. 2014). The access of the data base is permitted only to the authorized user
(Yuehong et al. 2016). The fetching of the information can be triggered other activities such as
retrieval of the prescription and past medical records. Duplicate of the entire database is made
for the use of the hospitals and healthcare providers.
This part of the system also maintains scheduling issues. In health
care function, scheduling is a complex process. It requires the synchronization of the availability
of health care service. The availability of the service at hospitals and the health care clinics are
not same for each day (Wang et al. 2016). The scheduling helps to inform the patients about
the time of availability of the requested service. Another challenging activity managed by this
section is the resource management (Weaver et al. 2016).Resources, in this case, indicate the
type and kind of service a patient can avail.
Handling the Department:
<Student Name> Page | 4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EIA IMPLEMENTATION
The objective of the health care record is to provide important
information regarding the clinical purpose. There are many tasks done by the ancillary, which
are necessary for management of the departmental operation.
Delivery of the care and clinical documentation:
In order to do this health experts can communicate through ancillary
department using this section (Datascience.nih.gov 2018).The elimination of the misplaced slips
and transcripts errors can be done through this section (health. 2018).. All data regarding the
patient along with their detailed reports can be accessed from this section (Nguyen, Bellucci
and Nguyen 2014). The patient health related data which was collected by the health experts
by interviewing the patients can also be viewed from this section.
Decision making process:
This section deals with the decision making process that can be done
on the collected health information of the patient. In order to provide expert advice and taking
decision about the future medical progress, the relevant information is fetched from the other
department of the healthcare management system, through this section (Degoulet, Luna and
de Quiros 2017). The data can be fetched from one section to other by providing the
registration ID of the patient. The physicians are made concerned about the different problems
and allergies of the patients through ‘Physician Order Entry’. This entry helps the doctors and
the physicians to determine the right medicines for the patients.
Resource Management:
This part of the system manages the raw information for the resource
management . This part of the system generated the detailed billing of the patient and informs
the status of the bill to the patients. A patient can pay bill to the hospital or health care
providers through this section. The payment is done through the electronic transaction of
money by debit or credit card. The amount of the bill is dependent on the raw data those has
been fetched from different sections of the health care systemThe dealing with the third party
health care providing vendor such as insurance companies are also handled by this department.
3.2 Challenges:
Some of the challenges those can be raised in case of data integration and the
management of data-
Security: It is desirable that the data in the system remains safe and secure
(Iyamu 2018). The health information can only be accessed by the patient
and the health care provider of the patient. Another security concern
about the system is connected with the security of transaction of money.
The gateway through which the money is transacted should be secured.
Flexibility and availability: The system needs to be available all the time. A
flexible system will adopt the changes in the process. Both health care
providers and the patients can access the system at any time of the day.
<Student Name> Page | 5
The objective of the health care record is to provide important
information regarding the clinical purpose. There are many tasks done by the ancillary, which
are necessary for management of the departmental operation.
Delivery of the care and clinical documentation:
In order to do this health experts can communicate through ancillary
department using this section (Datascience.nih.gov 2018).The elimination of the misplaced slips
and transcripts errors can be done through this section (health. 2018).. All data regarding the
patient along with their detailed reports can be accessed from this section (Nguyen, Bellucci
and Nguyen 2014). The patient health related data which was collected by the health experts
by interviewing the patients can also be viewed from this section.
Decision making process:
This section deals with the decision making process that can be done
on the collected health information of the patient. In order to provide expert advice and taking
decision about the future medical progress, the relevant information is fetched from the other
department of the healthcare management system, through this section (Degoulet, Luna and
de Quiros 2017). The data can be fetched from one section to other by providing the
registration ID of the patient. The physicians are made concerned about the different problems
and allergies of the patients through ‘Physician Order Entry’. This entry helps the doctors and
the physicians to determine the right medicines for the patients.
Resource Management:
This part of the system manages the raw information for the resource
management . This part of the system generated the detailed billing of the patient and informs
the status of the bill to the patients. A patient can pay bill to the hospital or health care
providers through this section. The payment is done through the electronic transaction of
money by debit or credit card. The amount of the bill is dependent on the raw data those has
been fetched from different sections of the health care systemThe dealing with the third party
health care providing vendor such as insurance companies are also handled by this department.
3.2 Challenges:
Some of the challenges those can be raised in case of data integration and the
management of data-
Security: It is desirable that the data in the system remains safe and secure
(Iyamu 2018). The health information can only be accessed by the patient
and the health care provider of the patient. Another security concern
about the system is connected with the security of transaction of money.
The gateway through which the money is transacted should be secured.
Flexibility and availability: The system needs to be available all the time. A
flexible system will adopt the changes in the process. Both health care
providers and the patients can access the system at any time of the day.
<Student Name> Page | 5
EIA IMPLEMENTATION
3.2 Methods of managing the challenges:
The most challenging thing is the security issues. In order to manage these challenges
certain security steps has been taken. Several security protocols have been implemented in the
transaction gateway for the secured transaction of money. In order to make the service
available to all the users of the system, a dedicated server is needed to be implemented. The
system framework should be designed in such a way that it can be flexible enough tocope up
with nay changes in the system. SQL server can be used to make the database. In order to
reduce the risk of deletion of data two separate dataset in the data base can be used.
4.0 Conclusion
It can be assumed from the above discussion is that the proper
implementationof proper electronic health record system can be done by the selection of
the proper EIA. The robustness of the system depends on the methods used for the
implementation. There are certain models of EIA those can be use for the implementation
of the e-health record. However, each model has own advantages and disadvantages.
However, the proposed design is aimed to reduce the drawbacks of the other models. To
overcome those challenges, necessary steps those can be taken are proposed in the paper.
It can be said that the proposed system will serve its purpose effectively and will be
beneficial for the people.
5.0 Recommendation
Following recommendations can be made in order to modify the
proposed system.
The graphical user interface of the system can be improved so that the user
can use the system easily.
In case, if the users of the system face any kind of technical problem, a
technical support team can be available to solve their problem.
The awareness about keeping the record in electronic health record can be
spread among the health care providers and the patients.
Certain issues should be considered in order to choose the right EIA
framework.
<Student Name> Page | 6
3.2 Methods of managing the challenges:
The most challenging thing is the security issues. In order to manage these challenges
certain security steps has been taken. Several security protocols have been implemented in the
transaction gateway for the secured transaction of money. In order to make the service
available to all the users of the system, a dedicated server is needed to be implemented. The
system framework should be designed in such a way that it can be flexible enough tocope up
with nay changes in the system. SQL server can be used to make the database. In order to
reduce the risk of deletion of data two separate dataset in the data base can be used.
4.0 Conclusion
It can be assumed from the above discussion is that the proper
implementationof proper electronic health record system can be done by the selection of
the proper EIA. The robustness of the system depends on the methods used for the
implementation. There are certain models of EIA those can be use for the implementation
of the e-health record. However, each model has own advantages and disadvantages.
However, the proposed design is aimed to reduce the drawbacks of the other models. To
overcome those challenges, necessary steps those can be taken are proposed in the paper.
It can be said that the proposed system will serve its purpose effectively and will be
beneficial for the people.
5.0 Recommendation
Following recommendations can be made in order to modify the
proposed system.
The graphical user interface of the system can be improved so that the user
can use the system easily.
In case, if the users of the system face any kind of technical problem, a
technical support team can be available to solve their problem.
The awareness about keeping the record in electronic health record can be
spread among the health care providers and the patients.
Certain issues should be considered in order to choose the right EIA
framework.
<Student Name> Page | 6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EIA IMPLEMENTATION
Bibliography
Andersen, S.B., Rasmussen, C.K. and Frøkjær, E., 2017, July. Bringing content understanding into
usability testing in complex application domains—a case study in eHealth. In International
Conference of Design, User Experience, and Usability (pp. 327-341). Springer, Cham.
Datascience.nih.gov. (2018). Is the EHR the New Big Data? | Data Science at NIH. [online]
Available at: https://datascience.nih.gov/BlogIsTheEHR [Accessed 16 Apr. 2018].
Degoulet, P., Luna, D. and de Quiros, F.G.B., 2017. Clinical Information Systems. In Global
Health Informatics (pp. 129-151).
Farooq, F., Rosales, R.E., Yu, S., Krishnapuram, B. and Rao, B.R., Siemens Medical Solutions USA
Inc, 2015. Healthcare information technology system for predicting or preventing readmissions.
U.S. Patent 8,949,082.
Fernandes, S. and Fragoso, J.L., 2017. Information Systems’ Portfolio: Contributions Of
Enterprise And Process Architecture. Journal of Spatial and Organizational Dynamics, 5(3),
pp.208-221.
health. (2018). Healthit.gov. Retrieved 16 April 2018, from
https://www.healthit.gov/sites/default/files/hitech_act_excerpt_from_arra_with_index.pdf#
%5B%7
Iyamu, T., 2018. Implementation of the enterprise architecture through the Zachman
Framework. Journal of Systems and Information Technology, 20(1), pp.2-18.
Jones, S.S., Rudin, R.S., Perry, T. and Shekelle, P.G., 2014. Health information technology: an
updated systematic review with a focus on meaningful use. Annals of internal medicine, 160(1),
pp.48-54.
Jonkers, H. and Quartel, D.A., 2016, June. Enterprise Architecture-Based Risk and Security
Modelling and Analysis. In International Workshop on Graphical Models for Security(pp. 94-
101). Springer, Cham.
Julia, K., Kurt, S. and Ulf, S., 2017. Challenges in Integrating Product-IT into Enterprise
Architecture–a case study. Procedia Computer Science, 121, pp.525-533.
<Student Name> Page | 7
Bibliography
Andersen, S.B., Rasmussen, C.K. and Frøkjær, E., 2017, July. Bringing content understanding into
usability testing in complex application domains—a case study in eHealth. In International
Conference of Design, User Experience, and Usability (pp. 327-341). Springer, Cham.
Datascience.nih.gov. (2018). Is the EHR the New Big Data? | Data Science at NIH. [online]
Available at: https://datascience.nih.gov/BlogIsTheEHR [Accessed 16 Apr. 2018].
Degoulet, P., Luna, D. and de Quiros, F.G.B., 2017. Clinical Information Systems. In Global
Health Informatics (pp. 129-151).
Farooq, F., Rosales, R.E., Yu, S., Krishnapuram, B. and Rao, B.R., Siemens Medical Solutions USA
Inc, 2015. Healthcare information technology system for predicting or preventing readmissions.
U.S. Patent 8,949,082.
Fernandes, S. and Fragoso, J.L., 2017. Information Systems’ Portfolio: Contributions Of
Enterprise And Process Architecture. Journal of Spatial and Organizational Dynamics, 5(3),
pp.208-221.
health. (2018). Healthit.gov. Retrieved 16 April 2018, from
https://www.healthit.gov/sites/default/files/hitech_act_excerpt_from_arra_with_index.pdf#
%5B%7
Iyamu, T., 2018. Implementation of the enterprise architecture through the Zachman
Framework. Journal of Systems and Information Technology, 20(1), pp.2-18.
Jones, S.S., Rudin, R.S., Perry, T. and Shekelle, P.G., 2014. Health information technology: an
updated systematic review with a focus on meaningful use. Annals of internal medicine, 160(1),
pp.48-54.
Jonkers, H. and Quartel, D.A., 2016, June. Enterprise Architecture-Based Risk and Security
Modelling and Analysis. In International Workshop on Graphical Models for Security(pp. 94-
101). Springer, Cham.
Julia, K., Kurt, S. and Ulf, S., 2017. Challenges in Integrating Product-IT into Enterprise
Architecture–a case study. Procedia Computer Science, 121, pp.525-533.
<Student Name> Page | 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EIA IMPLEMENTATION
Nguyen, L., Bellucci, E. and Nguyen, L.T., 2014. Electronic health records implementation: an
evaluation of information system impact and contingency factors. International journal of
medical informatics, 83(11), pp.779-796.
Romero, D. and Vernadat, F., 2016. Enterprise information systems state of the art: Past,
present and future trends. Computers in Industry, 79, pp.3-13.
Rosenbaum, S.E., Moberg, J., Glenton, C., Schünemann, H.J., Lewin, S., Akl, E., Mustafa, R.A.,
Morelli, A., Vogel, J.P., Alonso Coello, P. and Rada, G., 2017. Developing Evidence to Decision‐
Frameworks and an Interactive Evidence to Decision Tool for Making and Using Decisions and
Recommendations in Health Care. Global Challenges
Shah, G.H., Leider, J.P., Castrucci, B.C., Williams, K.S. and Luo, H., 2016. Characteristics of local
health departments associated with implementation of electronic health records and other
informatics systems. Public Health Reports, 131(2), pp.272-282.
Singh, N., 2018. Strategic Operating Model for Enterprise Architecture.
Vargas, A., Cuenca, L., Boza, A., Sacala, I. and Moisescu, M., 2016. Towards the development of
the framework for inter sensing enterprise architecture. Journal of Intelligent
Manufacturing, 27(1), pp.55-72.
Vogel, L.H., 2014. Management of information in health care organizations. In Biomedical
Informatics (pp. 443-474). Springer, London.
Wang, J.W., Wang, H.F., Ding, J.L., Furuta, K., Kanno, T., Ip, W.H. and Zhang, W.J., 2016. On
domain modelling of the service system with its application to enterprise information
systems. Enterprise Information Systems, 10(1), pp.1-16.
Weaver, C.A., Ball, M.J., Kim, G.R. and Kiel, J.M., 2016. Healthcare information management
systems. Cham: Springer International Publishing.
Yuehong, Y.I.N., Zeng, Y., Chen, X. and Fan, Y., 2016. The internet of things in healthcare: An
overview. Journal of Industrial Information Integration, 1, pp.3-13.
<Student Name> Page | 8
Nguyen, L., Bellucci, E. and Nguyen, L.T., 2014. Electronic health records implementation: an
evaluation of information system impact and contingency factors. International journal of
medical informatics, 83(11), pp.779-796.
Romero, D. and Vernadat, F., 2016. Enterprise information systems state of the art: Past,
present and future trends. Computers in Industry, 79, pp.3-13.
Rosenbaum, S.E., Moberg, J., Glenton, C., Schünemann, H.J., Lewin, S., Akl, E., Mustafa, R.A.,
Morelli, A., Vogel, J.P., Alonso Coello, P. and Rada, G., 2017. Developing Evidence to Decision‐
Frameworks and an Interactive Evidence to Decision Tool for Making and Using Decisions and
Recommendations in Health Care. Global Challenges
Shah, G.H., Leider, J.P., Castrucci, B.C., Williams, K.S. and Luo, H., 2016. Characteristics of local
health departments associated with implementation of electronic health records and other
informatics systems. Public Health Reports, 131(2), pp.272-282.
Singh, N., 2018. Strategic Operating Model for Enterprise Architecture.
Vargas, A., Cuenca, L., Boza, A., Sacala, I. and Moisescu, M., 2016. Towards the development of
the framework for inter sensing enterprise architecture. Journal of Intelligent
Manufacturing, 27(1), pp.55-72.
Vogel, L.H., 2014. Management of information in health care organizations. In Biomedical
Informatics (pp. 443-474). Springer, London.
Wang, J.W., Wang, H.F., Ding, J.L., Furuta, K., Kanno, T., Ip, W.H. and Zhang, W.J., 2016. On
domain modelling of the service system with its application to enterprise information
systems. Enterprise Information Systems, 10(1), pp.1-16.
Weaver, C.A., Ball, M.J., Kim, G.R. and Kiel, J.M., 2016. Healthcare information management
systems. Cham: Springer International Publishing.
Yuehong, Y.I.N., Zeng, Y., Chen, X. and Fan, Y., 2016. The internet of things in healthcare: An
overview. Journal of Industrial Information Integration, 1, pp.3-13.
<Student Name> Page | 8
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




