Non-Invasive Diagnosis of COPD Patients Using EMG and MMG Signals
VerifiedAdded on 2023/01/18
|16
|3813
|28
Report
AI Summary
This report presents a comprehensive analysis of using Electromyography (EMG) and Mechanomyography (MMG) signal analysis for the non-invasive diagnosis of Chronic Obstructive Pulmonary Disease (COPD) patients. The study focuses on the diaphragm, neck, and chest wall muscles, examining their activity through signal processing techniques. The introduction highlights COPD's global impact and the limitations of current diagnostic methods, emphasizing the potential of non-invasive approaches. The literature review explores various methods, including adaptive filter analysis and the use of adaptive noise cancellers, to improve signal quality and accurately detect respiratory onset. The report evaluates tools for better analysis of COPD patients and discusses the application of fixed sample entropy (fSE) and adaptive filtering to remove electrocardiographic (ECG) interference. The discussion section synthesizes the findings, comparing the performance of different methods and addressing the challenges in accurately detecting respiratory onset. The study concludes with the effectiveness of EMG and MMG analysis in COPD diagnosis and suggests future research directions. The study provides detailed insights into the methods, results, and implications of the study.

Diaphragm, Neck and Chest Wall Muscles Activity in COPD patients for Non-Invasive
Diagnosis using EMG and MMG
Signal Analysis
Diagnosis using EMG and MMG
Signal Analysis
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
Introduction.................................................................................................................................................3
Critical evaluation:......................................................................................................................................4
Literature Review........................................................................................................................................5
Evaluating tool to understand the better analysis of Copd patient.............................................................5
Adaptive Filter analysis:...............................................................................................................................6
Use of Adaptive Noise Canceller..................................................................................................................7
Discussion...................................................................................................................................................8
Conclusions...............................................................................................................................................11
Reference...................................................................................................................................................12
Appendix:..................................................................................................................................................14
Introduction.................................................................................................................................................3
Critical evaluation:......................................................................................................................................4
Literature Review........................................................................................................................................5
Evaluating tool to understand the better analysis of Copd patient.............................................................5
Adaptive Filter analysis:...............................................................................................................................6
Use of Adaptive Noise Canceller..................................................................................................................7
Discussion...................................................................................................................................................8
Conclusions...............................................................................................................................................11
Reference...................................................................................................................................................12
Appendix:..................................................................................................................................................14
Introduction
Chronic obstructive pulmonary disease (COPD) is fourth foremostreason of death in the world .
Due to ageing of the population and continuation of risk factors, this problem will keep
increasing in the coming decades. The disease is characterized by an airway obstruction leading
to airflow limitation and, as a consequence, persisted respiratory symptoms such as dyspnea and
production of sputum (Estrada et al. 2016). Last-stage COPD patient normally suffers chronic
hypercapnic respiratory failure, which is accompanying with the end-of-life. Long-term
application of nocturnal intermittent non-invasive ventilation (NIV) in sufferer with chronic
hypercapnic respiratory failure due to neuromuscular and thoracic restrictive disorders improves
clinical outcomes and survival. However, this therapy has long been controversial in COPD
patients [3, 4]. High-intensity NIV is well-defined as a mode of ventilation that delivers
sufficient inspiratory progressive airway pressure in arrangement with higher backup breathing
incidence to decrease arterial carbon dioxide levels. However, for some patients, adapting to
high-intensity NIV is difficult and compliance rates in clinical practice are therefore sometimes
disappointing. Furthermore, the response to NIV in context of progress in gas altercation and
patient-centered results such as improvement in healthy quality of life is variable between
patients, despite the application of high-intensity NIV. A reason for a more prolonged adaption
period, lower compliance rates and less effective ventilation might be the occurrence of patient-
ventilator asynchrony with high-intensity NIV. The surface diaphragm electromyography
(EMGdi) indicatordelivers a real-time ancillary measure of neural respiratory drive that shows
the load on respiratory muscles (Stocks and quanjer, 2015). Its non-invasive nature makes the
method extremely useful during NIV; both to visually detect patient-ventilator asynchrony, and
for repeated measurements (Quanjer et al. 2012). However, for longer recordings, such as whole
night recordings, visual inspection is burdensome and time-consuming. In addition, NIV is
normally applied during sleep. Thus, there is a clear need to develop an instinctiveprocess to
reliably detect the respiratory onset from the EMGdi signal. This is crucial since the timing of
respiratory effort versus the timing of the ventilator pressure wave determines the control of
ventilation. Nevertheless, the EMGdi signal is heavily contaminated by the electrocardiographic
(ECG) activity, compromising inspiratory onset detection.
Chronic obstructive pulmonary disease (COPD) is fourth foremostreason of death in the world .
Due to ageing of the population and continuation of risk factors, this problem will keep
increasing in the coming decades. The disease is characterized by an airway obstruction leading
to airflow limitation and, as a consequence, persisted respiratory symptoms such as dyspnea and
production of sputum (Estrada et al. 2016). Last-stage COPD patient normally suffers chronic
hypercapnic respiratory failure, which is accompanying with the end-of-life. Long-term
application of nocturnal intermittent non-invasive ventilation (NIV) in sufferer with chronic
hypercapnic respiratory failure due to neuromuscular and thoracic restrictive disorders improves
clinical outcomes and survival. However, this therapy has long been controversial in COPD
patients [3, 4]. High-intensity NIV is well-defined as a mode of ventilation that delivers
sufficient inspiratory progressive airway pressure in arrangement with higher backup breathing
incidence to decrease arterial carbon dioxide levels. However, for some patients, adapting to
high-intensity NIV is difficult and compliance rates in clinical practice are therefore sometimes
disappointing. Furthermore, the response to NIV in context of progress in gas altercation and
patient-centered results such as improvement in healthy quality of life is variable between
patients, despite the application of high-intensity NIV. A reason for a more prolonged adaption
period, lower compliance rates and less effective ventilation might be the occurrence of patient-
ventilator asynchrony with high-intensity NIV. The surface diaphragm electromyography
(EMGdi) indicatordelivers a real-time ancillary measure of neural respiratory drive that shows
the load on respiratory muscles (Stocks and quanjer, 2015). Its non-invasive nature makes the
method extremely useful during NIV; both to visually detect patient-ventilator asynchrony, and
for repeated measurements (Quanjer et al. 2012). However, for longer recordings, such as whole
night recordings, visual inspection is burdensome and time-consuming. In addition, NIV is
normally applied during sleep. Thus, there is a clear need to develop an instinctiveprocess to
reliably detect the respiratory onset from the EMGdi signal. This is crucial since the timing of
respiratory effort versus the timing of the ventilator pressure wave determines the control of
ventilation. Nevertheless, the EMGdi signal is heavily contaminated by the electrocardiographic
(ECG) activity, compromising inspiratory onset detection.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Critical evaluation:
A number of methods have been used to estimate the envelope of EMGdi and automatically
identify inspiratory onset in the journal "Inspiratory muscle activation increases with COPD
severity as confirmed by non-invasive mechanographic" - by Leonardo Sarlabous. Recently,
fixed sample entropy (fSE) has proved to be a more robust technique to estimate the amplitude
variation in respiratory EMGdisignals. In addition, fSE permits extracting the EMGdi envelope
without requiring a prior removal of QRS complexes thus it is identified as the research
relevancy. However, poor EMGdi signal quality or high ECG interference can reduce the
robustness of fSE. The use of adaptive filters has also been proposed to remove ECG
interference and then estimate EMGdi amplitude and has made the research accurate as well as
reliable. However, these methods have been evaluated separately and in different contexts and it
lacks in biasness and timeliness. Therefore, there is a clear need to explore whether reducing
ECG interference by adaptive filtering can improve EMGdi envelope estimation and
consequently respiratory onset detection.
In this study, the article" Normative measurement of inspiratory muscles performance by meams
of diaphragm muscle mechanographic signals in CoPD patients during an incremental load
respiratory test”is aimed to compare the performance of previously proposed methods estimating
EMGdi envelope and respiratory onset, to optimize the automatic detection of the onset of neural
respiratory drive in COPD patients initiated on home NIV this includes the relevance of the test.
First, to estimate EMGdi envelope, the use of fSE in combination with adaptive straining was
compared and explored to the RMS-based EMGdi envelope provided by EMG acquisition device
helps in understanding the realistic nature of the study. Formerly, dynamic threshold based on
the kernel density estimation (KDE), applied to the EMGdi envelopes, and was proposed to
detect the respiratory onset. The performance of the onset detection was validated using EMG-
based visual scores completed by two well-trained clinicians and describes the timeliness and
completeness of the research.
A number of methods have been used to estimate the envelope of EMGdi and automatically
identify inspiratory onset in the journal "Inspiratory muscle activation increases with COPD
severity as confirmed by non-invasive mechanographic" - by Leonardo Sarlabous. Recently,
fixed sample entropy (fSE) has proved to be a more robust technique to estimate the amplitude
variation in respiratory EMGdisignals. In addition, fSE permits extracting the EMGdi envelope
without requiring a prior removal of QRS complexes thus it is identified as the research
relevancy. However, poor EMGdi signal quality or high ECG interference can reduce the
robustness of fSE. The use of adaptive filters has also been proposed to remove ECG
interference and then estimate EMGdi amplitude and has made the research accurate as well as
reliable. However, these methods have been evaluated separately and in different contexts and it
lacks in biasness and timeliness. Therefore, there is a clear need to explore whether reducing
ECG interference by adaptive filtering can improve EMGdi envelope estimation and
consequently respiratory onset detection.
In this study, the article" Normative measurement of inspiratory muscles performance by meams
of diaphragm muscle mechanographic signals in CoPD patients during an incremental load
respiratory test”is aimed to compare the performance of previously proposed methods estimating
EMGdi envelope and respiratory onset, to optimize the automatic detection of the onset of neural
respiratory drive in COPD patients initiated on home NIV this includes the relevance of the test.
First, to estimate EMGdi envelope, the use of fSE in combination with adaptive straining was
compared and explored to the RMS-based EMGdi envelope provided by EMG acquisition device
helps in understanding the realistic nature of the study. Formerly, dynamic threshold based on
the kernel density estimation (KDE), applied to the EMGdi envelopes, and was proposed to
detect the respiratory onset. The performance of the onset detection was validated using EMG-
based visual scores completed by two well-trained clinicians and describes the timeliness and
completeness of the research.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Literature Review
Evaluating tool to understand the better analysis of Copd patient
According to the article on clinical study performed at the Department of Pulmonary Diseases of
the University Medical Center Groningen (Groningen, The Netherlands). Nine patients with
COPD initiated on home NIV in the hospital were included in this analysis. All patients
participated in a randomized controlled trial of which investigating respiratory EMG and patient-
ventilator asynchrony during NIV initiation was a secondary objective. Both studies, including
the EMG measurements, were approved by the Ethical Committee Groningen (ClinicalTrials.gov
NCT02652559 and NCT03053973). All patients gave written informed consent for participation
in the trial and for the EMG measurements. TheEMGdi was measured in the COPD patients once
they got used to sleeping with NIV during the night. In 7 patients nocturnal measurements were
performed during the initiation period performed in the hospital after 2–5 nights NIV
acclimatization and titration, and in 2 patients the EMG measurements were performed after a
longer period of NIV used at home (in 1 patient a nocturnal measurement was performed after 6
months NIV use and in the other patient a daytime measurement was performed after more than
2 years NIV use). The EMGdi was measured using two 24 mm surface electrodes.
In this case, EMGdi signals were filtered with a 4th-order zero-phase Butterworth band-pass
filter between 5 Hz and 400 Hz. Power line interference at 50 Hz and its harmonics were
removed using 10th-order zero-phase notch filters. For each patient, one hour of the EMGdi
recording was selected. The EMGdi signals were visually evaluated separately by two
physicians. The visual analysis included the onset annotations of every inspiration (Altintas,
2016). A graphic user interface developed in MATLAB facilitated visually determining the onset
points over the EMGdi signals (see Figure S1). The onset of diaphragm activity was selected as
the point at which the surface EMGdi amplitude exceeds the value of basal expiratory activity.
Respiratory cycles where the visual onset marks significantly differed between both experts (a
difference greater than a specific tolerance value) were considered unreliable and removed from
further analysis. The physicians, based on their clinical experience, set this tolerance value to
150 ms. when the visual onset marks were within the tolerance value, the mean of the two
annotations was considered as the gold standard. This metric provides a more objective onset
Evaluating tool to understand the better analysis of Copd patient
According to the article on clinical study performed at the Department of Pulmonary Diseases of
the University Medical Center Groningen (Groningen, The Netherlands). Nine patients with
COPD initiated on home NIV in the hospital were included in this analysis. All patients
participated in a randomized controlled trial of which investigating respiratory EMG and patient-
ventilator asynchrony during NIV initiation was a secondary objective. Both studies, including
the EMG measurements, were approved by the Ethical Committee Groningen (ClinicalTrials.gov
NCT02652559 and NCT03053973). All patients gave written informed consent for participation
in the trial and for the EMG measurements. TheEMGdi was measured in the COPD patients once
they got used to sleeping with NIV during the night. In 7 patients nocturnal measurements were
performed during the initiation period performed in the hospital after 2–5 nights NIV
acclimatization and titration, and in 2 patients the EMG measurements were performed after a
longer period of NIV used at home (in 1 patient a nocturnal measurement was performed after 6
months NIV use and in the other patient a daytime measurement was performed after more than
2 years NIV use). The EMGdi was measured using two 24 mm surface electrodes.
In this case, EMGdi signals were filtered with a 4th-order zero-phase Butterworth band-pass
filter between 5 Hz and 400 Hz. Power line interference at 50 Hz and its harmonics were
removed using 10th-order zero-phase notch filters. For each patient, one hour of the EMGdi
recording was selected. The EMGdi signals were visually evaluated separately by two
physicians. The visual analysis included the onset annotations of every inspiration (Altintas,
2016). A graphic user interface developed in MATLAB facilitated visually determining the onset
points over the EMGdi signals (see Figure S1). The onset of diaphragm activity was selected as
the point at which the surface EMGdi amplitude exceeds the value of basal expiratory activity.
Respiratory cycles where the visual onset marks significantly differed between both experts (a
difference greater than a specific tolerance value) were considered unreliable and removed from
further analysis. The physicians, based on their clinical experience, set this tolerance value to
150 ms. when the visual onset marks were within the tolerance value, the mean of the two
annotations was considered as the gold standard. This metric provides a more objective onset
value that reduces the subjective judgments of single scorers, thus minimizing the imperfect
nature of visual inspection scorers.
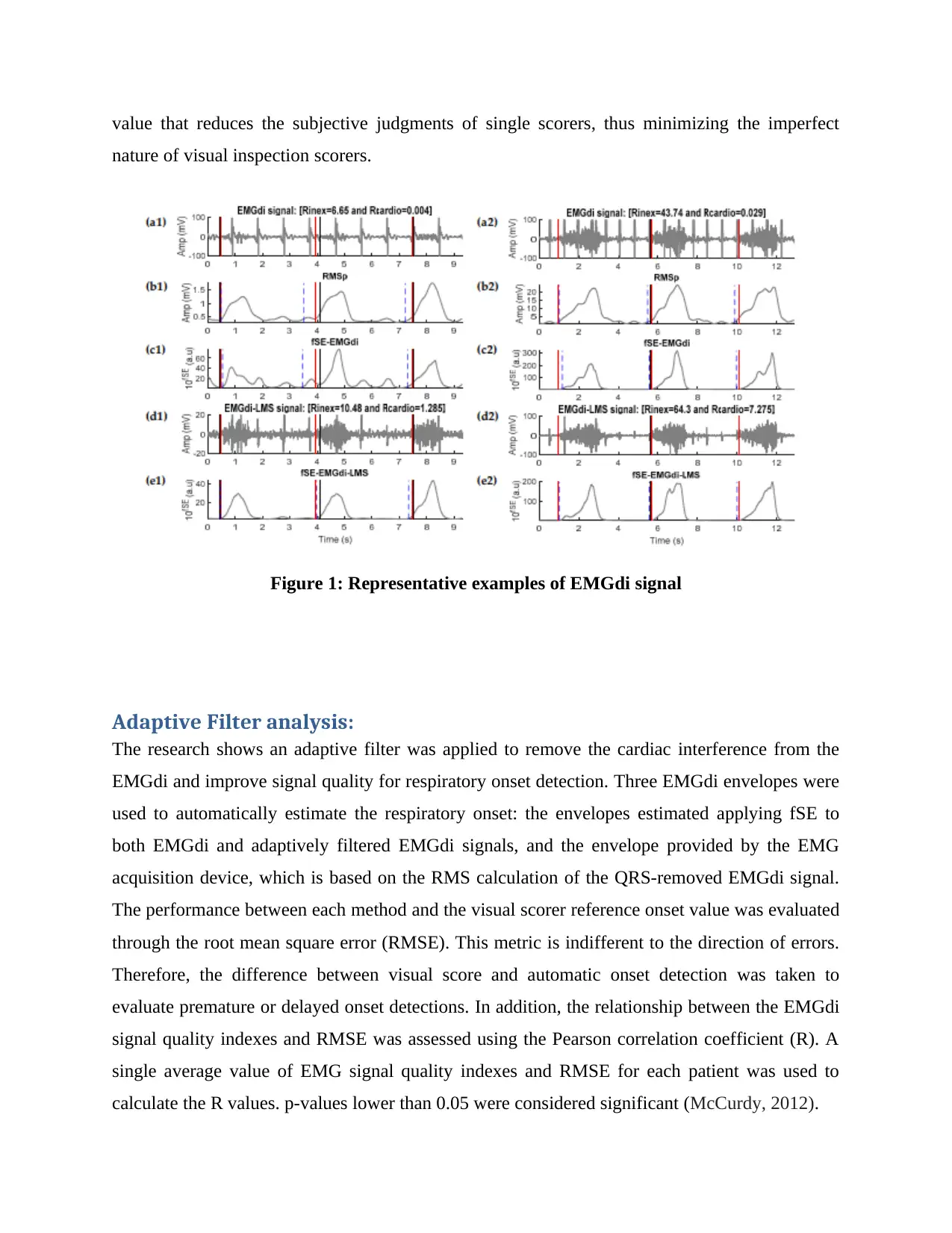
Figure 1: Representative examples of EMGdi signal
Adaptive Filter analysis:
The research shows an adaptive filter was applied to remove the cardiac interference from the
EMGdi and improve signal quality for respiratory onset detection. Three EMGdi envelopes were
used to automatically estimate the respiratory onset: the envelopes estimated applying fSE to
both EMGdi and adaptively filtered EMGdi signals, and the envelope provided by the EMG
acquisition device, which is based on the RMS calculation of the QRS-removed EMGdi signal.
The performance between each method and the visual scorer reference onset value was evaluated
through the root mean square error (RMSE). This metric is indifferent to the direction of errors.
Therefore, the difference between visual score and automatic onset detection was taken to
evaluate premature or delayed onset detections. In addition, the relationship between the EMGdi
signal quality indexes and RMSE was assessed using the Pearson correlation coefficient (R). A
single average value of EMG signal quality indexes and RMSE for each patient was used to
calculate the R values. p-values lower than 0.05 were considered significant (McCurdy, 2012).
nature of visual inspection scorers.
Figure 1: Representative examples of EMGdi signal
Adaptive Filter analysis:
The research shows an adaptive filter was applied to remove the cardiac interference from the
EMGdi and improve signal quality for respiratory onset detection. Three EMGdi envelopes were
used to automatically estimate the respiratory onset: the envelopes estimated applying fSE to
both EMGdi and adaptively filtered EMGdi signals, and the envelope provided by the EMG
acquisition device, which is based on the RMS calculation of the QRS-removed EMGdi signal.
The performance between each method and the visual scorer reference onset value was evaluated
through the root mean square error (RMSE). This metric is indifferent to the direction of errors.
Therefore, the difference between visual score and automatic onset detection was taken to
evaluate premature or delayed onset detections. In addition, the relationship between the EMGdi
signal quality indexes and RMSE was assessed using the Pearson correlation coefficient (R). A
single average value of EMG signal quality indexes and RMSE for each patient was used to
calculate the R values. p-values lower than 0.05 were considered significant (McCurdy, 2012).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
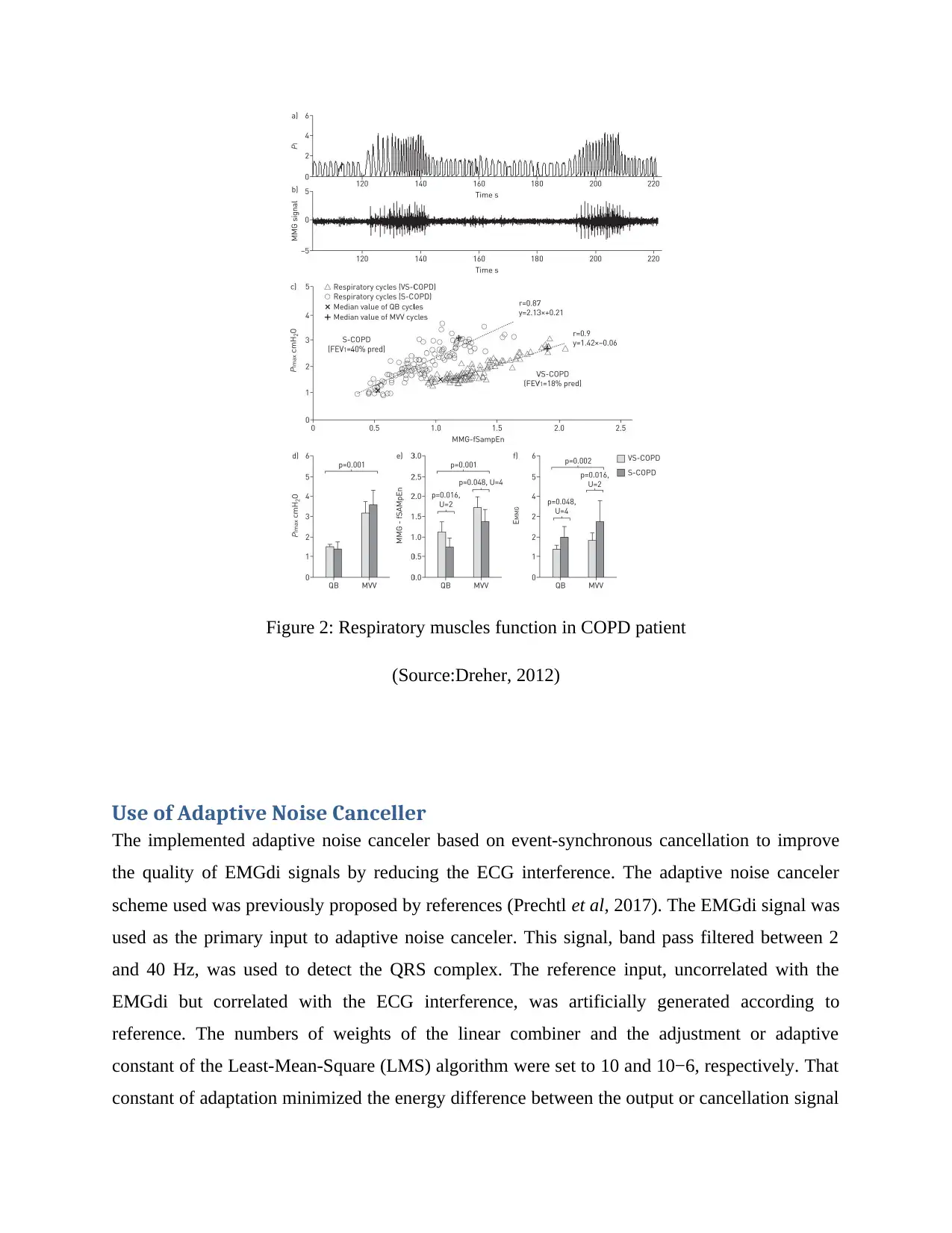
Figure 2: Respiratory muscles function in COPD patient
(Source:Dreher, 2012)
Use of Adaptive Noise Canceller
The implemented adaptive noise canceler based on event-synchronous cancellation to improve
the quality of EMGdi signals by reducing the ECG interference. The adaptive noise canceler
scheme used was previously proposed by references (Prechtl et al, 2017). The EMGdi signal was
used as the primary input to adaptive noise canceler. This signal, band pass filtered between 2
and 40 Hz, was used to detect the QRS complex. The reference input, uncorrelated with the
EMGdi but correlated with the ECG interference, was artificially generated according to
reference. The numbers of weights of the linear combiner and the adjustment or adaptive
constant of the Least-Mean-Square (LMS) algorithm were set to 10 and 10−6, respectively. That
constant of adaptation minimized the energy difference between the output or cancellation signal
(Source:Dreher, 2012)
Use of Adaptive Noise Canceller
The implemented adaptive noise canceler based on event-synchronous cancellation to improve
the quality of EMGdi signals by reducing the ECG interference. The adaptive noise canceler
scheme used was previously proposed by references (Prechtl et al, 2017). The EMGdi signal was
used as the primary input to adaptive noise canceler. This signal, band pass filtered between 2
and 40 Hz, was used to detect the QRS complex. The reference input, uncorrelated with the
EMGdi but correlated with the ECG interference, was artificially generated according to
reference. The numbers of weights of the linear combiner and the adjustment or adaptive
constant of the Least-Mean-Square (LMS) algorithm were set to 10 and 10−6, respectively. That
constant of adaptation minimized the energy difference between the output or cancellation signal
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
and the reference input signal. The EMGdi-LMS signal represents the EMGdi signal adaptively
filtered using the LMS algorithm and fSE-EMGdi-LMS represents the envelope extracted with
fSE.
Discussion
In the present study, a new approach has been developed to automatically detect respiratory
onset from EMGdi. We proposed a novel method using sample entropy to compute the envelope
of EMGdi and a Gaussian-KDE based threshold to non-invasively estimate the onset of the
inspiratory activity in COPD patients initiated on home NIV in the hospital. The envelope,
derived using fSE (mean RMSE = 298 ms), showed slightly higher values in estimating the onset
compared to the RMS-based envelope (mean RMSE = 301 ms) provided by the EMG acquisition
device; both evaluated during day and/or night, and with poor EMG signal-to-noise ratios.
In addition, this study is the first to our knowledge to introduce the combination of the fSE and
the adaptive filtering techniques to improve the estimation of EMGdi envelope when dealing
with low quality EMGdi signals, which further reduced the RMSE to 264 ms. Furthermore, we
proposed EMGdi quality indexes to assess the impact of EMGdi signal quality detecting
inspiratory onset. This showed that there is significant moderate to strong negative correlations
between the quality indices and RMSE. However, as observed for patient 7, the LMS approach
slightly reduced the Rinex index from 3.65 to 3.29, without compromising the performance of
the automatic onset detections. All automated methods detected the onset before the visual
scores; with a mean premature detection of 159 ms, 152 ms and 196 ms, for fSE-EMGdi, fSE-
EMGdi-LMS and RMSp, respectively. The mean and dispersion of onset detection errors were
higher for patients with lower EMGdi signal quality (Duiverman et al. 2015). The estimation of
inspiratory onset is the necessary key step to detect patient-ventilator asynchrony, which is
normally done by visual inspection. In an attempt to automatize patient-ventilator asynchrony
detection, we showed that it is feasible to automatically detect inspiratory onset from EMGdi.
However, compared to visual analysis, the automatic methods estimate the onset prematurely
with an error ranging from 30 ms to 309 ms, 47 ms to 233 ms, and 89 ms to 255 ms, using fSE-
EMGdi, fSE-EMGdi-LMS and RMSp, respectively.
filtered using the LMS algorithm and fSE-EMGdi-LMS represents the envelope extracted with
fSE.
Discussion
In the present study, a new approach has been developed to automatically detect respiratory
onset from EMGdi. We proposed a novel method using sample entropy to compute the envelope
of EMGdi and a Gaussian-KDE based threshold to non-invasively estimate the onset of the
inspiratory activity in COPD patients initiated on home NIV in the hospital. The envelope,
derived using fSE (mean RMSE = 298 ms), showed slightly higher values in estimating the onset
compared to the RMS-based envelope (mean RMSE = 301 ms) provided by the EMG acquisition
device; both evaluated during day and/or night, and with poor EMG signal-to-noise ratios.
In addition, this study is the first to our knowledge to introduce the combination of the fSE and
the adaptive filtering techniques to improve the estimation of EMGdi envelope when dealing
with low quality EMGdi signals, which further reduced the RMSE to 264 ms. Furthermore, we
proposed EMGdi quality indexes to assess the impact of EMGdi signal quality detecting
inspiratory onset. This showed that there is significant moderate to strong negative correlations
between the quality indices and RMSE. However, as observed for patient 7, the LMS approach
slightly reduced the Rinex index from 3.65 to 3.29, without compromising the performance of
the automatic onset detections. All automated methods detected the onset before the visual
scores; with a mean premature detection of 159 ms, 152 ms and 196 ms, for fSE-EMGdi, fSE-
EMGdi-LMS and RMSp, respectively. The mean and dispersion of onset detection errors were
higher for patients with lower EMGdi signal quality (Duiverman et al. 2015). The estimation of
inspiratory onset is the necessary key step to detect patient-ventilator asynchrony, which is
normally done by visual inspection. In an attempt to automatize patient-ventilator asynchrony
detection, we showed that it is feasible to automatically detect inspiratory onset from EMGdi.
However, compared to visual analysis, the automatic methods estimate the onset prematurely
with an error ranging from 30 ms to 309 ms, 47 ms to 233 ms, and 89 ms to 255 ms, using fSE-
EMGdi, fSE-EMGdi-LMS and RMSp, respectively.
Nevertheless, it should be considered that the variability between visual scorers was very high.
The lack of exact mathematical definition of the EMGdi onset represents a challenging problem .
This is reflected by the percentages of cycles removed, up to 45% in one patient with low
EMGdi signal quality, because the inter-scorer’s difference was very high. Only cycles where the
scorers agreed within a tolerance of 150 ms were included in the analysis. The mean between
both scores was considered the reference onset, which included some error in our analysis, as
both marks could be 150 ms apart. The main source of variability was the onsets that lay close to
QRS complexes. In addition, the visual marks were performed in the EMGdi signal, without the
adaptive filter that reduced ECG interference, which might have negatively influenced the visual
onset detection. This can be observed in Figure 2, where the automatic marks look more reliable
than the visual marks.
Several studies based on sample entropy analysis have properly estimated respiratory onset
without removal of ECG artifacts from good quality EMGdi signals (Zhan et al. 2010). The main
challenge on onset detection studies using the fSE technique is to determine the optimal
parameters. Recommendations for estimating respiratory muscle activity using fSE on EMGdi
for different levels of inspiratory effort developed by a healthy subject in seated position were
established by Estrada et al. (2012). However, such recommendations were not made considering
surface EMGdi signals from COPD patients with home mechanical ventilation. Therefore, we
investigated the effect of fSE parameters: r values of 0.1, 0.2 and 0.3 times the standard deviation
of the EMGdi signal excluding ECG interference segments, m = 1 and 2, and overlapping sliding
windows between 0.25 s to 0.5 s on estimation of neural onset. The optimal parameters were set
to m = 1, r = 0.3, and sliding moving window equal to 0.25 s, based on the lowest geometric
mean RMSE found for fSE-EMGdi (276.4 ms) and fSE-EMGdi-LMS (253.7 ms). Interestingly,
the selected parameters were in accordance with the recommendations made by Estrada et al.
[25], and were suitable to extract respiratory muscle activity in COPD patients undergoing NIV.
Other problems related to background noise presented during EMG signal recording and signal
to noise ratio notably could also affect the accuracy of onset detection [31]. In studies with
EMGdi signals, the interference and frequency overlap between ECG and EMGdi signals can
affect the analysis and interpretation of researchers and clinicians. ECG and EMGdi signals
could be viewed as being derived from two dynamic systems with different complexity
characteristics [29]. Despite fSE permits extracting the EMGdi envelope without removing ECG
The lack of exact mathematical definition of the EMGdi onset represents a challenging problem .
This is reflected by the percentages of cycles removed, up to 45% in one patient with low
EMGdi signal quality, because the inter-scorer’s difference was very high. Only cycles where the
scorers agreed within a tolerance of 150 ms were included in the analysis. The mean between
both scores was considered the reference onset, which included some error in our analysis, as
both marks could be 150 ms apart. The main source of variability was the onsets that lay close to
QRS complexes. In addition, the visual marks were performed in the EMGdi signal, without the
adaptive filter that reduced ECG interference, which might have negatively influenced the visual
onset detection. This can be observed in Figure 2, where the automatic marks look more reliable
than the visual marks.
Several studies based on sample entropy analysis have properly estimated respiratory onset
without removal of ECG artifacts from good quality EMGdi signals (Zhan et al. 2010). The main
challenge on onset detection studies using the fSE technique is to determine the optimal
parameters. Recommendations for estimating respiratory muscle activity using fSE on EMGdi
for different levels of inspiratory effort developed by a healthy subject in seated position were
established by Estrada et al. (2012). However, such recommendations were not made considering
surface EMGdi signals from COPD patients with home mechanical ventilation. Therefore, we
investigated the effect of fSE parameters: r values of 0.1, 0.2 and 0.3 times the standard deviation
of the EMGdi signal excluding ECG interference segments, m = 1 and 2, and overlapping sliding
windows between 0.25 s to 0.5 s on estimation of neural onset. The optimal parameters were set
to m = 1, r = 0.3, and sliding moving window equal to 0.25 s, based on the lowest geometric
mean RMSE found for fSE-EMGdi (276.4 ms) and fSE-EMGdi-LMS (253.7 ms). Interestingly,
the selected parameters were in accordance with the recommendations made by Estrada et al.
[25], and were suitable to extract respiratory muscle activity in COPD patients undergoing NIV.
Other problems related to background noise presented during EMG signal recording and signal
to noise ratio notably could also affect the accuracy of onset detection [31]. In studies with
EMGdi signals, the interference and frequency overlap between ECG and EMGdi signals can
affect the analysis and interpretation of researchers and clinicians. ECG and EMGdi signals
could be viewed as being derived from two dynamic systems with different complexity
characteristics [29]. Despite fSE permits extracting the EMGdi envelope without removing ECG
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
interference, the quality of EMGdi is a key factor in robust envelope estimation. Thus, in this
study, for the first time, we proposed EMG quality indices and a combined adaptive filter with
fSE to detect respiratory onset when dealing with challenging EMGdi signals. These quality
indices enabled quantifying the performance of adaptive filtering. Although the ECG
interference was not completely removed, the quality of the EMGdi signal improved, which
enhanced the fSE performance and the automatic onset detection. Nevertheless, despite being
beneficial in low quality signals, adaptive filtering is very time consuming and could be avoided
when working with high quality signals since the improvement could be minimal. Patient-
ventilator interaction is generally evaluated through indirect estimates of neural onset time based
on a drop in esophageal pressure and the onset of airflow at the mouth. However, indirect
estimates of neural onset can be affected by physiological factors such as intrinsic positive end-
expiratory pressure (PEEPi), or mechanical changes of rib cage (Kondili et al. 2007). Therefore,
more direct measures of respiratory muscle electrical activity have been proposed to alleviate
imprecisions whilst using surrogate estimates of neural onset in mechanical ventilation. Although
it is possible to detect diaphragm EMG with esophageal or even needle electrodes, these invasive
methods are impractical in patients on chronic home NIV. Therefore, we focused on using
surface EMG, being aware of its drawbacks in terms of more signal noise and crosstalk by other
muscles, to detect respiratory neural drive in patients on home mechanical ventilation. The
present study does have certain limitations. Firstly, it is a study with a relatively small sample
size that could limit the generalization of the results. A second limitation is that despite the visual
EMG onset detection approach being the gold standard and considered to provide accurate onset
detection; this method strongly depends on the experience of the expert. It is highly subjective
and with poor reproducibility, and thus could be heavily biased by personal skills (Dreher et al.
2012). A third limitation is the fact that the EMGdi signals, unlike EMG signals recorded in
other muscles, have low signal-to-noise ratio and the manual annotations are more difficult to
make. Therefore, in future works, we plan to make manual annotations over the EMGdi-LMS
signals and compare them with those made on the EMGdi signal. Another limitation of the study
is that the implemented adaptive noise canceler filter was based on a fixed ECG template. In the
future, we will investigate whether generating an adaptive noise canceler that better represents
the variability of the cardiac pattern, improves the cancelation of ECG interference. In this sense,
different templates obtained every 5 min will be used instead of single template. We will also
study, for the first time, we proposed EMG quality indices and a combined adaptive filter with
fSE to detect respiratory onset when dealing with challenging EMGdi signals. These quality
indices enabled quantifying the performance of adaptive filtering. Although the ECG
interference was not completely removed, the quality of the EMGdi signal improved, which
enhanced the fSE performance and the automatic onset detection. Nevertheless, despite being
beneficial in low quality signals, adaptive filtering is very time consuming and could be avoided
when working with high quality signals since the improvement could be minimal. Patient-
ventilator interaction is generally evaluated through indirect estimates of neural onset time based
on a drop in esophageal pressure and the onset of airflow at the mouth. However, indirect
estimates of neural onset can be affected by physiological factors such as intrinsic positive end-
expiratory pressure (PEEPi), or mechanical changes of rib cage (Kondili et al. 2007). Therefore,
more direct measures of respiratory muscle electrical activity have been proposed to alleviate
imprecisions whilst using surrogate estimates of neural onset in mechanical ventilation. Although
it is possible to detect diaphragm EMG with esophageal or even needle electrodes, these invasive
methods are impractical in patients on chronic home NIV. Therefore, we focused on using
surface EMG, being aware of its drawbacks in terms of more signal noise and crosstalk by other
muscles, to detect respiratory neural drive in patients on home mechanical ventilation. The
present study does have certain limitations. Firstly, it is a study with a relatively small sample
size that could limit the generalization of the results. A second limitation is that despite the visual
EMG onset detection approach being the gold standard and considered to provide accurate onset
detection; this method strongly depends on the experience of the expert. It is highly subjective
and with poor reproducibility, and thus could be heavily biased by personal skills (Dreher et al.
2012). A third limitation is the fact that the EMGdi signals, unlike EMG signals recorded in
other muscles, have low signal-to-noise ratio and the manual annotations are more difficult to
make. Therefore, in future works, we plan to make manual annotations over the EMGdi-LMS
signals and compare them with those made on the EMGdi signal. Another limitation of the study
is that the implemented adaptive noise canceler filter was based on a fixed ECG template. In the
future, we will investigate whether generating an adaptive noise canceler that better represents
the variability of the cardiac pattern, improves the cancelation of ECG interference. In this sense,
different templates obtained every 5 min will be used instead of single template. We will also
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

explore the use of other adaptive filtering algorithms such as the Recursive-Least-Squares
algorithm. 6.
Conclusions
In this work, a new fSE-based approach to detect neural onset from muscle respiratory signals
was proposed for COPD patients during non-invasive ventilation. The performance of fSE was
improved including an adaptive filtering step that allowed us to reduce cardiac interference when
evaluating EMGdi recordings with low signal quality. The fSE combined with the KDE resulted
in a suitable tool for onset detection where the muscle activation profile can be difficult to
evaluate. Our findings suggest that using fSE is promising to detect neural onset from muscle
respiratory signals in COPD patients during non-invasive ventilation. We recommend using fSE
alongside adaptive filtering when EMGdi recordings have low signal-to-noise ratio. More
research is required to further validate our findings in a larger cohort and to investigate whether
it can be used to detect and treat patient-ventilator asynchrony in order to improve clinical
outcomes.
algorithm. 6.
Conclusions
In this work, a new fSE-based approach to detect neural onset from muscle respiratory signals
was proposed for COPD patients during non-invasive ventilation. The performance of fSE was
improved including an adaptive filtering step that allowed us to reduce cardiac interference when
evaluating EMGdi recordings with low signal quality. The fSE combined with the KDE resulted
in a suitable tool for onset detection where the muscle activation profile can be difficult to
evaluate. Our findings suggest that using fSE is promising to detect neural onset from muscle
respiratory signals in COPD patients during non-invasive ventilation. We recommend using fSE
alongside adaptive filtering when EMGdi recordings have low signal-to-noise ratio. More
research is required to further validate our findings in a larger cohort and to investigate whether
it can be used to detect and treat patient-ventilator asynchrony in order to improve clinical
outcomes.
Reference
1. GOLD: Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the
Diagnosis,Management, and Prevention of Chronic Obstructive Pulmonary Disease (2018
Report). Availableonline: https://goldcopd.org/wp-content/uploads/2017/11/GOLD-2018-v6.0-
FINAL-revised-20-Nov_WMS.pdf (accessed on 13 April 2019).
2. Lopez, A.D., Shibuya, K., Rao, C., Mathers, C.D., Hansell, A.L., Held, L.S., Schmid, V. and
Buist, S., 2006. Chronic obstructive pulmonary disease: current burden and future projections.
European Respiratory Journal, 27(2), pp.397-412.
3. Duiverman, M.L., Huberts, A.S., van Eykern, L.A., Bladder, G. and Wijkstra, P.J., 2017.
respiratory muscle activity and patient–ventilator asynchrony during different settings of
noninvasive ventilation in stable hypercapnic COPD: does high inspiratory pressure lead to
respiratory muscle unloading?. International journal of chronic obstructive pulmonary
disease, 12, p.243.
4. McCurdy, B.R., 2012. Noninvasive positive pressure ventilation for acute respiratory failure
patients with chronic obstructive pulmonary disease (COPD): an evidence-based
analysis. Ontario health technology assessment series, 12(8), p.1.
5. Altintas, N., 2016. Update: non-invasive positive pressure ventilation in chronic respiratory
failure due to COPD. COPD: Journal of Chronic Obstructive Pulmonary Disease, 13(1), pp.110-
121.
6. Dreher, M., Storre, J.H., Schmoor, C. and Windisch, W., 2010. High-intensity versus low-
intensity non-invasive ventilation in patients with stable hypercapnic COPD: a randomised
crossover trial. Thorax, 65(4), pp.303-308.7.
9. Kondili, E., Xirouchaki, N. and Georgopoulos, D., 2007. Modulation and treatment of patient–
ventilator dyssynchrony. Current opinion in critical care, 13(1), pp.84-89.
1. GOLD: Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the
Diagnosis,Management, and Prevention of Chronic Obstructive Pulmonary Disease (2018
Report). Availableonline: https://goldcopd.org/wp-content/uploads/2017/11/GOLD-2018-v6.0-
FINAL-revised-20-Nov_WMS.pdf (accessed on 13 April 2019).
2. Lopez, A.D., Shibuya, K., Rao, C., Mathers, C.D., Hansell, A.L., Held, L.S., Schmid, V. and
Buist, S., 2006. Chronic obstructive pulmonary disease: current burden and future projections.
European Respiratory Journal, 27(2), pp.397-412.
3. Duiverman, M.L., Huberts, A.S., van Eykern, L.A., Bladder, G. and Wijkstra, P.J., 2017.
respiratory muscle activity and patient–ventilator asynchrony during different settings of
noninvasive ventilation in stable hypercapnic COPD: does high inspiratory pressure lead to
respiratory muscle unloading?. International journal of chronic obstructive pulmonary
disease, 12, p.243.
4. McCurdy, B.R., 2012. Noninvasive positive pressure ventilation for acute respiratory failure
patients with chronic obstructive pulmonary disease (COPD): an evidence-based
analysis. Ontario health technology assessment series, 12(8), p.1.
5. Altintas, N., 2016. Update: non-invasive positive pressure ventilation in chronic respiratory
failure due to COPD. COPD: Journal of Chronic Obstructive Pulmonary Disease, 13(1), pp.110-
121.
6. Dreher, M., Storre, J.H., Schmoor, C. and Windisch, W., 2010. High-intensity versus low-
intensity non-invasive ventilation in patients with stable hypercapnic COPD: a randomised
crossover trial. Thorax, 65(4), pp.303-308.7.
9. Kondili, E., Xirouchaki, N. and Georgopoulos, D., 2007. Modulation and treatment of patient–
ventilator dyssynchrony. Current opinion in critical care, 13(1), pp.84-89.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



