ERP Implementation and Healthcare Service Quality Analysis
VerifiedAdded on 2022/08/18
|12
|9446
|10
Report
AI Summary
This research article investigates the impact of Enterprise Resource Planning (ERP) systems on the quality of healthcare services, focusing on the perspectives of healthcare professionals in Lahore, Pakistan. The study utilizes a mixed-methods approach, collecting data from 279 medical professionals across five healthcare organizations to evaluate the influence of ERP on individual attributes, organizational impressions, information quality, and system quality. The findings indicate a positive correlation between ERP implementation and improved healthcare service quality, emphasizing the benefits of integrated planning systems. The research highlights the potential of ERP systems to enhance system output, enabling healthcare professionals to deliver superior services. The article also reviews existing literature on ERP systems, discussing their evolution, benefits, and challenges, particularly in the context of developing economies and the healthcare sector. It concludes by suggesting the need for further research and emphasizing the significance of ERP adoption for improving healthcare efficiency and patient care.
administrative
sciences
Article
Enterprise Resource Planning Systems: Digitization
of Healthcare Service Quality
Muhammad Fiaz1, Amir Ikram2,3,* and Asad Ilyas1
1 Institute of Business & Management, University of Engineering & Technology, Punjab 54890, Pakistan;
muhammadfiaz@mail.xjtu.edu.cn (M.F.); asad.ilyas@live.com (A.I.)
2 School of Management, Xi’an Jiaotong University, Xi’an 710049, China
3 Department of Business Management, National College of Business Administration & Economics,
Lahore 54660, Pakistan
* Correspondence: amirikram@stu.xjtu.edu.cn
Received: 9 May 2018; Accepted: 28 June 2018; Published: 27 July 2018
Abstract:The purpose of this study is to evaluate the perception of healthcare professionals in
improving the quality of services in healthcare centers by deploying the platform of Enterprise
Resource Planning (ERP). Individual attributes,organizational impression,information,and the
system quality of ERP have been used to evaluate the overall influence of integrated planning
systems on health care service quality.A mixed methods approach is used to collect and examine
data through triangulation. Data for the empirical study was collected from 279 medical professionals
of five healthcare organizations operating in the city of Lahore, Pakistan, through a self-administered
questionnaire. Descriptive statistics squared multiple correlations and reliability coefficients were
used as data analysis tools. Moreover, the goodness of fit test of the structural model was conducted
through AMOS 20. All given dimensions of ERP are postulated to have a positive effect on healthcare
service quality.The results reveal that the use of an enterprise planning system has a positive
impact on individuals, organizational information quality, and system quality in healthcare services.
The study further concludes that a well implemented ‘Enterprise Resource Planning System’ results in
better system output and enables healthcare professionals to provide better healthcare service quality.
Keywords: enterprise resource planning; information systems; healthcare; service quality
1. Introduction
Database management systems and information analytics ensued widespread improvements of
quality and efficiency in almost every sphere of life. Moreover, the healthcare sector is no exception,
where technological advancements and information systems are transforming the sector with the
orientation of integrated systems. Most of the transformations about healthcare systems are primarily
focused on health care quality and the minimization of cost. Healthcare professionals and institutions
lack the adequate systems required to deliver strategic change. Thus, there is a sense of urgency on
their part to make use of information technology (Cucciniello et al. 2016).However, the adoption
rate of the IT-based integrated system in the healthcare sector is quite slow as compared to other
sectors, such as commerce and finance, especially in the case of emerging economies. This calls for an
empirical investigation of the healthcare sector concerning problems being faced in the implementation
of the Enterprise Resource Planning (ERP) system.ERP software can integrate all the departments
of an organization and functions into a unified system (Somers and Nelson 2001).ERP primarily
offers two welfares to the organization that are usually not prevalent in an organization with a
non-integrated system;i.e.,(a) Unified database for ERP systems where all the transactions of an
organization are entered, stored, handled, and reported.(b) A single enterprise business view that
Adm. Sci. 2018, 8, 38; doi:10.3390/admsci8030038 www.mdpi.com/journal/admsci
sciences
Article
Enterprise Resource Planning Systems: Digitization
of Healthcare Service Quality
Muhammad Fiaz1, Amir Ikram2,3,* and Asad Ilyas1
1 Institute of Business & Management, University of Engineering & Technology, Punjab 54890, Pakistan;
muhammadfiaz@mail.xjtu.edu.cn (M.F.); asad.ilyas@live.com (A.I.)
2 School of Management, Xi’an Jiaotong University, Xi’an 710049, China
3 Department of Business Management, National College of Business Administration & Economics,
Lahore 54660, Pakistan
* Correspondence: amirikram@stu.xjtu.edu.cn
Received: 9 May 2018; Accepted: 28 June 2018; Published: 27 July 2018
Abstract:The purpose of this study is to evaluate the perception of healthcare professionals in
improving the quality of services in healthcare centers by deploying the platform of Enterprise
Resource Planning (ERP). Individual attributes,organizational impression,information,and the
system quality of ERP have been used to evaluate the overall influence of integrated planning
systems on health care service quality.A mixed methods approach is used to collect and examine
data through triangulation. Data for the empirical study was collected from 279 medical professionals
of five healthcare organizations operating in the city of Lahore, Pakistan, through a self-administered
questionnaire. Descriptive statistics squared multiple correlations and reliability coefficients were
used as data analysis tools. Moreover, the goodness of fit test of the structural model was conducted
through AMOS 20. All given dimensions of ERP are postulated to have a positive effect on healthcare
service quality.The results reveal that the use of an enterprise planning system has a positive
impact on individuals, organizational information quality, and system quality in healthcare services.
The study further concludes that a well implemented ‘Enterprise Resource Planning System’ results in
better system output and enables healthcare professionals to provide better healthcare service quality.
Keywords: enterprise resource planning; information systems; healthcare; service quality
1. Introduction
Database management systems and information analytics ensued widespread improvements of
quality and efficiency in almost every sphere of life. Moreover, the healthcare sector is no exception,
where technological advancements and information systems are transforming the sector with the
orientation of integrated systems. Most of the transformations about healthcare systems are primarily
focused on health care quality and the minimization of cost. Healthcare professionals and institutions
lack the adequate systems required to deliver strategic change. Thus, there is a sense of urgency on
their part to make use of information technology (Cucciniello et al. 2016).However, the adoption
rate of the IT-based integrated system in the healthcare sector is quite slow as compared to other
sectors, such as commerce and finance, especially in the case of emerging economies. This calls for an
empirical investigation of the healthcare sector concerning problems being faced in the implementation
of the Enterprise Resource Planning (ERP) system.ERP software can integrate all the departments
of an organization and functions into a unified system (Somers and Nelson 2001).ERP primarily
offers two welfares to the organization that are usually not prevalent in an organization with a
non-integrated system;i.e.,(a) Unified database for ERP systems where all the transactions of an
organization are entered, stored, handled, and reported.(b) A single enterprise business view that
Adm. Sci. 2018, 8, 38; doi:10.3390/admsci8030038 www.mdpi.com/journal/admsci
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Adm. Sci. 2018, 8, 38 2 of 12
covers all departments of an organization and its functions. Achieving a competitive edge is considered
another reason for implementing ERP systems in healthcare organizations (Al-Mashari et al. 2003).
The design of ERP systems is based on the advancement of the ability of an organization to
generate accurate and timely information, thereby enhancing the competitiveness of an organization
(Singla 2008). These systems are complex and incur the high cost of implementation in an organization.
Therefore, organizations need to reconsider their ERP system purchasing and implementation plan
(Razi and Tarn 2015).The ERP system has substantial benefits,but it can also be responsible for
causing troublesome changes to an organization and the rate of failure of the ERP system varies.
Healthcare is a very complex sector comprising a large number of departments and patient care
systems (Acharyulu 2012). Studies have advocated that there exist a positive relation of investment in
an information system with health care service productivity (Menon et al. 1996). The reliability of the
healthcare system is increasing due to the implementation of an information system for the help in
the diagnosis of disease, improved management, and better services (Adler-Milstein and Bates 2010).
Information system (IS) in healthcare is explained as an enormous system of integration that has the
capability to support the colossal information need of the healthcare system covering the financial,
clinical, auxiliary, and patient management (Roussel et al. 2006). Implementation of IS in healthcare
has resulted in enhanced patient care quality, improving the management of health services, and access
to knowledge for decision making in administration and clinical processes (Parr and Shanks 2000).
Integral systems are requirements of healthcare for the procedure development and application of
patients at the same time considering the requirement of capacity. In the healthcare system, the ERP
system use has improved the material management process.
There is hesitation on the part of practitioners in accepting new technologies, especially in the
public sector of developing economies such as Pakistan. Many rely on persisting with the traditional
way of doing things, and that is truer for the public healthcare sector.However, the private sector
in developing countries is relatively technology privy because of their commercialized nature. ERP
is widely implemented in private sector, and there are few queries of its implementation in public
healthcare, particularly in emerging economies. Hence, this paper aims to enrich the debate concerning
public healthcare by investigating one of the first applications of it in the emerging economy of
Pakistan.The rest of the article is structured as follows:the next section reviews the literature on
enterprise resource planning and its implementation in the public healthcare sector with specific
reference to developing economies. Following that, the theoretical model and hypotheses development
are discussed.In the next section, the research methodology and framework is elaborated upon in
the research design section. Conclusions, research implications, and provocative questions for future
study bring the discussion to a close.
2. Literature Review
Healthcare service quality is the result of a collaboration between the healthcare agent and the
patient. Thus, personal characteristics of the provider and the patient and organizational factors affect
the overall service quality (Mosadeghrad 2014). Jawaid (2016) analysed recent studies about violent
incidents against doctors in South Asian countries and suggested that such incidents are triggered
by a lack of communication between healthcare professionals and the patient,reduced image of
the medical profession, and below par quality of care.A proper ERP system can take care of these
problems.In the medical and healthcare profession,there often occurs a scenario where a doctor
lacks knowledge regarding a particular disease, and this is especially common among young doctors.
For instance, Al-Arifi et al. (2016) observed that healthcare professionals lack knowledge regarding
warfarin interactions with drug and herbal medicines. Another advantage of the ERP system is that it
can accommodate for the lack of information regarding a specific disease or medicine on the part of
doctors. Bharati and Ganguly (2013) noted that the South East Asian region has the highest number of
malaria cases. They suggested that increased monitoring, surveillance, and cross-border collaboration
can alleviate this problem. Balkrishnan et al. (2013) proposed that active Comparative Effectiveness
covers all departments of an organization and its functions. Achieving a competitive edge is considered
another reason for implementing ERP systems in healthcare organizations (Al-Mashari et al. 2003).
The design of ERP systems is based on the advancement of the ability of an organization to
generate accurate and timely information, thereby enhancing the competitiveness of an organization
(Singla 2008). These systems are complex and incur the high cost of implementation in an organization.
Therefore, organizations need to reconsider their ERP system purchasing and implementation plan
(Razi and Tarn 2015).The ERP system has substantial benefits,but it can also be responsible for
causing troublesome changes to an organization and the rate of failure of the ERP system varies.
Healthcare is a very complex sector comprising a large number of departments and patient care
systems (Acharyulu 2012). Studies have advocated that there exist a positive relation of investment in
an information system with health care service productivity (Menon et al. 1996). The reliability of the
healthcare system is increasing due to the implementation of an information system for the help in
the diagnosis of disease, improved management, and better services (Adler-Milstein and Bates 2010).
Information system (IS) in healthcare is explained as an enormous system of integration that has the
capability to support the colossal information need of the healthcare system covering the financial,
clinical, auxiliary, and patient management (Roussel et al. 2006). Implementation of IS in healthcare
has resulted in enhanced patient care quality, improving the management of health services, and access
to knowledge for decision making in administration and clinical processes (Parr and Shanks 2000).
Integral systems are requirements of healthcare for the procedure development and application of
patients at the same time considering the requirement of capacity. In the healthcare system, the ERP
system use has improved the material management process.
There is hesitation on the part of practitioners in accepting new technologies, especially in the
public sector of developing economies such as Pakistan. Many rely on persisting with the traditional
way of doing things, and that is truer for the public healthcare sector.However, the private sector
in developing countries is relatively technology privy because of their commercialized nature. ERP
is widely implemented in private sector, and there are few queries of its implementation in public
healthcare, particularly in emerging economies. Hence, this paper aims to enrich the debate concerning
public healthcare by investigating one of the first applications of it in the emerging economy of
Pakistan.The rest of the article is structured as follows:the next section reviews the literature on
enterprise resource planning and its implementation in the public healthcare sector with specific
reference to developing economies. Following that, the theoretical model and hypotheses development
are discussed.In the next section, the research methodology and framework is elaborated upon in
the research design section. Conclusions, research implications, and provocative questions for future
study bring the discussion to a close.
2. Literature Review
Healthcare service quality is the result of a collaboration between the healthcare agent and the
patient. Thus, personal characteristics of the provider and the patient and organizational factors affect
the overall service quality (Mosadeghrad 2014). Jawaid (2016) analysed recent studies about violent
incidents against doctors in South Asian countries and suggested that such incidents are triggered
by a lack of communication between healthcare professionals and the patient,reduced image of
the medical profession, and below par quality of care.A proper ERP system can take care of these
problems.In the medical and healthcare profession,there often occurs a scenario where a doctor
lacks knowledge regarding a particular disease, and this is especially common among young doctors.
For instance, Al-Arifi et al. (2016) observed that healthcare professionals lack knowledge regarding
warfarin interactions with drug and herbal medicines. Another advantage of the ERP system is that it
can accommodate for the lack of information regarding a specific disease or medicine on the part of
doctors. Bharati and Ganguly (2013) noted that the South East Asian region has the highest number of
malaria cases. They suggested that increased monitoring, surveillance, and cross-border collaboration
can alleviate this problem. Balkrishnan et al. (2013) proposed that active Comparative Effectiveness
Adm. Sci. 2018, 8, 38 3 of 12
Research (CER) systems nurture the sharing of resources, skills, and capabilities. ERPs can be helpful
in this regard as they can enable regional networking and data-sharing among all stakeholders in
real time.
Rouhani and Mehri (2018) investigated ERP benefits through a survey by defining 31 empowering
benefits for this enterprise system based on reviewing the literature and classifying it into four groups
of empowering benefits including informative,communicative,growth and learning,and strategic
benefits. The results indicated that the communicative, strategic and informative empowering benefits
are significant advantages.Tasevska et al.(2014) conducted a survey on 30 SMEs in the Republic of
Macedonia. The findings revealed that SMEs implemented common project planning practices, although
they did not consider the planning process as a distinct phase of the ERP implementation. Considering
the success of the ERP implementations, this study established that most of the representatives perceive
the undertaking as useful regarding client satisfaction and perceived quality measures.By using a
multi-method approach, Cucciniello et al. (2016) conducted comparative case studies of two differen
hospitals to examine the adoption and implementation of identical medical record systems and found that
healthcare organizations benefited from deploying the integrated medical system regarding information
quality, data sharing, and cost efficiency. The ERP system has the capability of integrating information
that is used by human resources, manufacturing, distribution, and accounting departments into a single
computer system (Umble et al. 2003). ERPs provide a holistic view to organizations about every business
process ongoing in the organization. It provides one software application, a unified database, and a single
interface to the organization. The ERP system can provide enhancement in service quality, productivity
service cost decrease, and efficiency (Shaul and Tauber 2013). The earlier target of the ERP system wa
not the services sector, but instead, the ERP system vendors focused on the manufacturing companie
(Botta-Genoulaz and Millet 2006).
The Enterprise Resource Planning system emerged in 1960, beginning with material requirement
planning (MRP). After that there was an advancement in the system and it was transformed into MRP
II (Basoglu et al. 2007). From 1960 to 1970, there was a paradigm shift from inventory control to MR
improvement, and this was accepted by a lot of manufacturing companies for the efficient calculation
of the materials they required for the manufacturing process.Then the MRP system further evolved
into a system that was more sophisticated and included detailed capacity planning, master scheduling,
long-range planning, capacity planning, and resource planning (Xue et al. 2005). MRP II systems further
included planning related to operations and sales, as well as a financial interface. The MRP II system
was a useful tool for planning for all types of resources present in an organization. It was logical for the
planning of materials and production processes, but organizations realized the need for the incorporation
of customer satisfaction and profitability (Wallace and Kremzar 2002). The latest form of the ERP system
present today is capable of handling with various business units covering management of customer
relationship, human resource, purchasing, finance and accounting, manufacturing, processing of the
order, management of materials and planning of operation and sales (Botta-Genoulaz and Millet 2006).
As a result, a large number of organizations have already adopted ERPs, and its implementation is
fast increasing in the services sector (Acharyulu 2012). The services sector has dominated its share
the Growth Domestic Product (GDP) of developed countries.Therefore, the progress of technology,
globalization trends, and communication technologies have exerted pressure on the service sector fo
their new competition offerings (Costa 2015). The organizations are interested in information system
acquiring for the adoption of modern technology and making it accessible for the users. The adoption
of information technology in the healthcare system is complicated as the Enterprise Resource Planning
system in healthcare is concerned with the lives of humans (Bazhair and Sandhu 2015). The acquiring of
this system is further influenced by various actors that have multiple interests and backgrounds. There
are chances that stakeholders in health care will resist in the adoption of information system and there is
need that it should be managed carefully, as these actors will be involved in information system adoption
and implementation (MacLennan and Van Belle 2014). Various success factors make implementation of
Research (CER) systems nurture the sharing of resources, skills, and capabilities. ERPs can be helpful
in this regard as they can enable regional networking and data-sharing among all stakeholders in
real time.
Rouhani and Mehri (2018) investigated ERP benefits through a survey by defining 31 empowering
benefits for this enterprise system based on reviewing the literature and classifying it into four groups
of empowering benefits including informative,communicative,growth and learning,and strategic
benefits. The results indicated that the communicative, strategic and informative empowering benefits
are significant advantages.Tasevska et al.(2014) conducted a survey on 30 SMEs in the Republic of
Macedonia. The findings revealed that SMEs implemented common project planning practices, although
they did not consider the planning process as a distinct phase of the ERP implementation. Considering
the success of the ERP implementations, this study established that most of the representatives perceive
the undertaking as useful regarding client satisfaction and perceived quality measures.By using a
multi-method approach, Cucciniello et al. (2016) conducted comparative case studies of two differen
hospitals to examine the adoption and implementation of identical medical record systems and found that
healthcare organizations benefited from deploying the integrated medical system regarding information
quality, data sharing, and cost efficiency. The ERP system has the capability of integrating information
that is used by human resources, manufacturing, distribution, and accounting departments into a single
computer system (Umble et al. 2003). ERPs provide a holistic view to organizations about every business
process ongoing in the organization. It provides one software application, a unified database, and a single
interface to the organization. The ERP system can provide enhancement in service quality, productivity
service cost decrease, and efficiency (Shaul and Tauber 2013). The earlier target of the ERP system wa
not the services sector, but instead, the ERP system vendors focused on the manufacturing companie
(Botta-Genoulaz and Millet 2006).
The Enterprise Resource Planning system emerged in 1960, beginning with material requirement
planning (MRP). After that there was an advancement in the system and it was transformed into MRP
II (Basoglu et al. 2007). From 1960 to 1970, there was a paradigm shift from inventory control to MR
improvement, and this was accepted by a lot of manufacturing companies for the efficient calculation
of the materials they required for the manufacturing process.Then the MRP system further evolved
into a system that was more sophisticated and included detailed capacity planning, master scheduling,
long-range planning, capacity planning, and resource planning (Xue et al. 2005). MRP II systems further
included planning related to operations and sales, as well as a financial interface. The MRP II system
was a useful tool for planning for all types of resources present in an organization. It was logical for the
planning of materials and production processes, but organizations realized the need for the incorporation
of customer satisfaction and profitability (Wallace and Kremzar 2002). The latest form of the ERP system
present today is capable of handling with various business units covering management of customer
relationship, human resource, purchasing, finance and accounting, manufacturing, processing of the
order, management of materials and planning of operation and sales (Botta-Genoulaz and Millet 2006).
As a result, a large number of organizations have already adopted ERPs, and its implementation is
fast increasing in the services sector (Acharyulu 2012). The services sector has dominated its share
the Growth Domestic Product (GDP) of developed countries.Therefore, the progress of technology,
globalization trends, and communication technologies have exerted pressure on the service sector fo
their new competition offerings (Costa 2015). The organizations are interested in information system
acquiring for the adoption of modern technology and making it accessible for the users. The adoption
of information technology in the healthcare system is complicated as the Enterprise Resource Planning
system in healthcare is concerned with the lives of humans (Bazhair and Sandhu 2015). The acquiring of
this system is further influenced by various actors that have multiple interests and backgrounds. There
are chances that stakeholders in health care will resist in the adoption of information system and there is
need that it should be managed carefully, as these actors will be involved in information system adoption
and implementation (MacLennan and Van Belle 2014). Various success factors make implementation of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Adm. Sci. 2018, 8, 38 4 of 12
ERP system successful. The perspective includes setting up of an ERP system, implementation phase
evaluation step, success of ERP system and its profit (Botta-Genoulaz and Millet 2006).
Twenty-two critical success factors for ERP system implementation at various implementation
phases have been presented by Somers and Nelson (2001).Successful implementations of the ERP
system have also been linked with the management of the project,support of top management,
teamwork, program of change management, and composition of ERP system team.The culture of
an organization, economic environment, and regulation of the government also offer challenges for
the implementation of Enterprise Resource Planning system (Ward and Peppard 2016). The practical
implementations of an ERP system offers many benefits. The benefits may be intangible or tangible;
e.g.,improvement in cash flow,order management,system integration,reduction of inventory,
logistics management, and information quality enhancement (Botta-Genoulaz and Millet 2006). Some
organizations have improved their position by ERP system implementation in their business processes;
for example, a company known as Earthgains implemented an ERP system and, as a result, there was an
enhancement in their operating margin from 2.4–3.3%. Similarly, on-time delivery was also heightened
to 99% (Hong et al. 2012). The ERP system implementation is a very complex process, and organizations
encounter different types of problems while adopting ERP system phases (Kumar et al. 2003). In many
cases,the implementation of an ERP system has failed because of the enormous implementation
costs. The failure rate of implementation of an ERP system has resulted in better ERP system process
understanding (Hung et al. 2014). ERP systems have a problem, the very high cost of implementation
sometimes provides inadequate results because the individuals using the ERP system are not aware
of proper ERP system functioning and working (Altamony et al. 2016). The failure rate of Enterprise
Resource Planning system has been greatly publicized, however, it has not detracted organizations
from investing money into ERP system implementation (Scotti et al. 2007). The cost of integrating an
ERP into the business process system is 3 to 10 times higher than the original cost of the ERP software.
This increase is due to the high costs charged by system consultants and the persons involved in
system integration (Karimi et al. 2007). As well, there is cost related to the replacement of the existing
information system in the organization into the system required for ERP.
There are quite a few studies that analysed the digitization of healthcare service quality with
the help of ERP. Almajali et al.(2016) conducted an empirical analysis of 175 Jordanian healthcare
organizations and examined the data using structural equation modeling. They found a significant
relationship between antecedents of ERP and its implementation success and further suggested that
user satisfaction plays a significant mediating role between ease of use and ERP implementation success
Chiarini et al. (2018) investigated ERP implementation in public healthcare and suggested that benefits
can be classified into four theoretical categories:patients’satisfaction,stakeholders’satisfaction,
operations efficiency, and strategic and performance management.While issues surrounding ERP
implementation include the complexity of the project, process re-engineering, and staff involvement.
As per Du (2017), the performance of the healthcare service includes quality and efficiency, so there
is inevitably an association between them. In general, it is believed that there is a trade-off between
quality and efficiency; however, Du (2017) suggested that it can not be completely accurate.
One of the methods ofcurtailing costand capitalizing on competitive advantage is the
implementation of an ERP system. With respect to developing economies, there is hesitation on the
part of practitioners in accepting new technologies and there is a tendency to persist with traditional
ways of doing things.Discourse on ERP systems acceptance is prevalent among policymakers and
researchers as they intend to understand the underlying psychological and social aspects inducing user
adoption behavior. Researchers also seek to answer why the application of ERP among organizational
stakeholders remains at a perfunctory level (Lim et al. 2005).Amoako-Gyampah and Salam (2004)
proposed an extension to the technology acceptance model and empirically investigated it in an ERP
implementation setting. It was shown that both project management and training influence the shared
views that users form about the assistances of the technology and how shared philosophies affect
the perceived expediency, ease of use, and know-how.There are numerous aspects that affect the
ERP system successful. The perspective includes setting up of an ERP system, implementation phase
evaluation step, success of ERP system and its profit (Botta-Genoulaz and Millet 2006).
Twenty-two critical success factors for ERP system implementation at various implementation
phases have been presented by Somers and Nelson (2001).Successful implementations of the ERP
system have also been linked with the management of the project,support of top management,
teamwork, program of change management, and composition of ERP system team.The culture of
an organization, economic environment, and regulation of the government also offer challenges for
the implementation of Enterprise Resource Planning system (Ward and Peppard 2016). The practical
implementations of an ERP system offers many benefits. The benefits may be intangible or tangible;
e.g.,improvement in cash flow,order management,system integration,reduction of inventory,
logistics management, and information quality enhancement (Botta-Genoulaz and Millet 2006). Some
organizations have improved their position by ERP system implementation in their business processes;
for example, a company known as Earthgains implemented an ERP system and, as a result, there was an
enhancement in their operating margin from 2.4–3.3%. Similarly, on-time delivery was also heightened
to 99% (Hong et al. 2012). The ERP system implementation is a very complex process, and organizations
encounter different types of problems while adopting ERP system phases (Kumar et al. 2003). In many
cases,the implementation of an ERP system has failed because of the enormous implementation
costs. The failure rate of implementation of an ERP system has resulted in better ERP system process
understanding (Hung et al. 2014). ERP systems have a problem, the very high cost of implementation
sometimes provides inadequate results because the individuals using the ERP system are not aware
of proper ERP system functioning and working (Altamony et al. 2016). The failure rate of Enterprise
Resource Planning system has been greatly publicized, however, it has not detracted organizations
from investing money into ERP system implementation (Scotti et al. 2007). The cost of integrating an
ERP into the business process system is 3 to 10 times higher than the original cost of the ERP software.
This increase is due to the high costs charged by system consultants and the persons involved in
system integration (Karimi et al. 2007). As well, there is cost related to the replacement of the existing
information system in the organization into the system required for ERP.
There are quite a few studies that analysed the digitization of healthcare service quality with
the help of ERP. Almajali et al.(2016) conducted an empirical analysis of 175 Jordanian healthcare
organizations and examined the data using structural equation modeling. They found a significant
relationship between antecedents of ERP and its implementation success and further suggested that
user satisfaction plays a significant mediating role between ease of use and ERP implementation success
Chiarini et al. (2018) investigated ERP implementation in public healthcare and suggested that benefits
can be classified into four theoretical categories:patients’satisfaction,stakeholders’satisfaction,
operations efficiency, and strategic and performance management.While issues surrounding ERP
implementation include the complexity of the project, process re-engineering, and staff involvement.
As per Du (2017), the performance of the healthcare service includes quality and efficiency, so there
is inevitably an association between them. In general, it is believed that there is a trade-off between
quality and efficiency; however, Du (2017) suggested that it can not be completely accurate.
One of the methods ofcurtailing costand capitalizing on competitive advantage is the
implementation of an ERP system. With respect to developing economies, there is hesitation on the
part of practitioners in accepting new technologies and there is a tendency to persist with traditional
ways of doing things.Discourse on ERP systems acceptance is prevalent among policymakers and
researchers as they intend to understand the underlying psychological and social aspects inducing user
adoption behavior. Researchers also seek to answer why the application of ERP among organizational
stakeholders remains at a perfunctory level (Lim et al. 2005).Amoako-Gyampah and Salam (2004)
proposed an extension to the technology acceptance model and empirically investigated it in an ERP
implementation setting. It was shown that both project management and training influence the shared
views that users form about the assistances of the technology and how shared philosophies affect
the perceived expediency, ease of use, and know-how.There are numerous aspects that affect the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Adm. Sci. 2018, 8, 38 5 of 12
implementation of ERP, including user resistance. Shih and Huang (2009) examined the behavioral
intention and actual usage of ERP implementation, grounded in the technology acceptance model.
They used the Lisrel package of structural equation modelling to validate the causal associations
between variables. Analytical outcomes determine that top leadership support positively affects the
perceived efficacy and perceived ease of use.It was also found that behavioral intention positively
affects genuine usage.
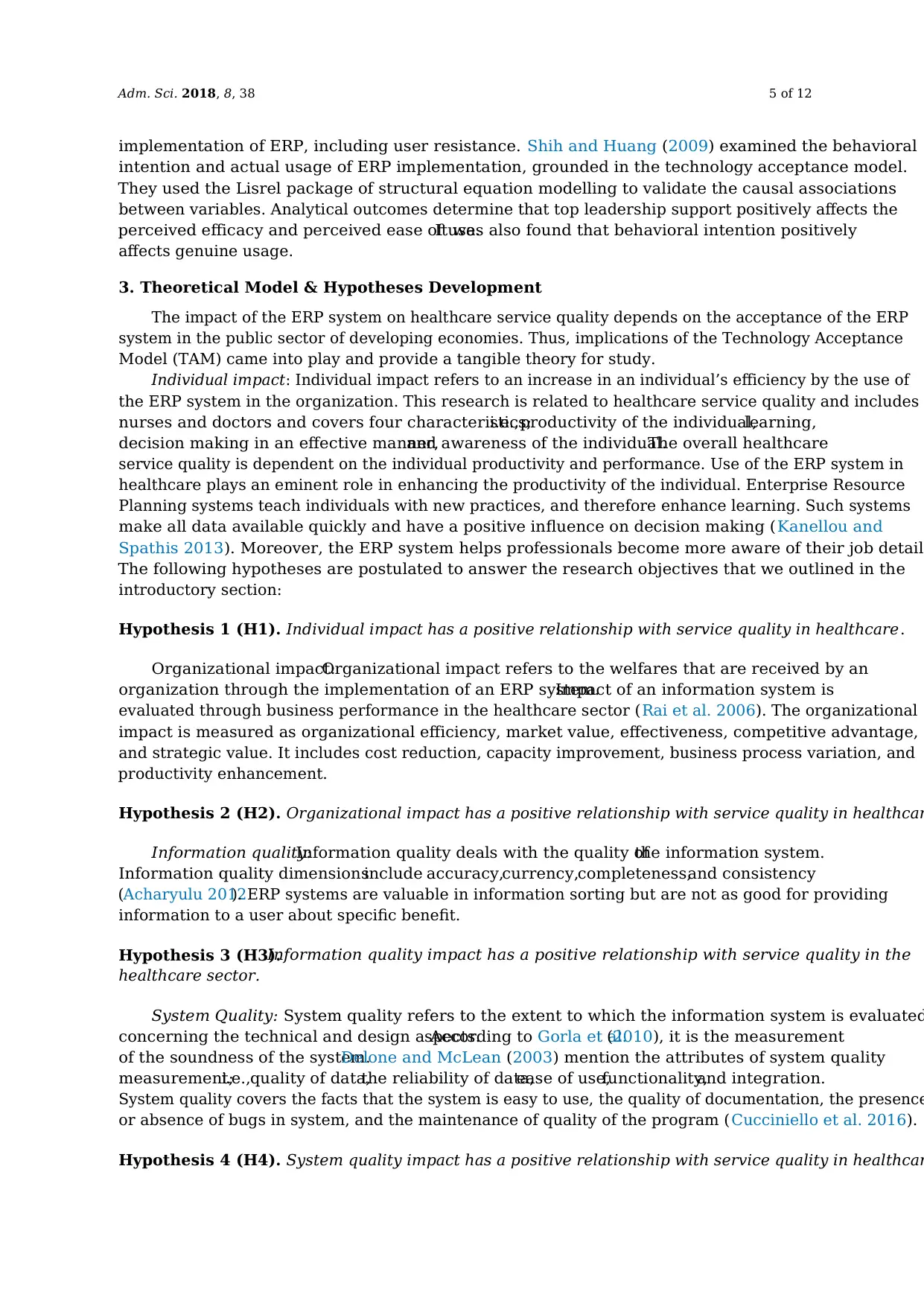
3. Theoretical Model & Hypotheses Development
The impact of the ERP system on healthcare service quality depends on the acceptance of the ERP
system in the public sector of developing economies. Thus, implications of the Technology Acceptance
Model (TAM) came into play and provide a tangible theory for study.
Individual impact: Individual impact refers to an increase in an individual’s efficiency by the use of
the ERP system in the organization. This research is related to healthcare service quality and includes
nurses and doctors and covers four characteristics;i.e.,productivity of the individual,learning,
decision making in an effective manner,and awareness of the individual.The overall healthcare
service quality is dependent on the individual productivity and performance. Use of the ERP system in
healthcare plays an eminent role in enhancing the productivity of the individual. Enterprise Resource
Planning systems teach individuals with new practices, and therefore enhance learning. Such systems
make all data available quickly and have a positive influence on decision making (Kanellou and
Spathis 2013). Moreover, the ERP system helps professionals become more aware of their job detail
The following hypotheses are postulated to answer the research objectives that we outlined in the
introductory section:
Hypothesis 1 (H1). Individual impact has a positive relationship with service quality in healthcare.
Organizational impact:Organizational impact refers to the welfares that are received by an
organization through the implementation of an ERP system.Impact of an information system is
evaluated through business performance in the healthcare sector (Rai et al. 2006). The organizational
impact is measured as organizational efficiency, market value, effectiveness, competitive advantage,
and strategic value. It includes cost reduction, capacity improvement, business process variation, and
productivity enhancement.
Hypothesis 2 (H2). Organizational impact has a positive relationship with service quality in healthcar
Information quality:Information quality deals with the quality ofthe information system.
Information quality dimensionsinclude accuracy,currency,completeness,and consistency
(Acharyulu 2012). ERP systems are valuable in information sorting but are not as good for providing
information to a user about specific benefit.
Hypothesis 3 (H3).Information quality impact has a positive relationship with service quality in the
healthcare sector.
System Quality: System quality refers to the extent to which the information system is evaluated
concerning the technical and design aspects.According to Gorla et al.(2010), it is the measurement
of the soundness of the system.Delone and McLean (2003) mention the attributes of system quality
measurement;i.e.,quality of data,the reliability of data,ease of use,functionality,and integration.
System quality covers the facts that the system is easy to use, the quality of documentation, the presence
or absence of bugs in system, and the maintenance of quality of the program (Cucciniello et al. 2016).
Hypothesis 4 (H4). System quality impact has a positive relationship with service quality in healthcar
implementation of ERP, including user resistance. Shih and Huang (2009) examined the behavioral
intention and actual usage of ERP implementation, grounded in the technology acceptance model.
They used the Lisrel package of structural equation modelling to validate the causal associations
between variables. Analytical outcomes determine that top leadership support positively affects the
perceived efficacy and perceived ease of use.It was also found that behavioral intention positively
affects genuine usage.
3. Theoretical Model & Hypotheses Development
The impact of the ERP system on healthcare service quality depends on the acceptance of the ERP
system in the public sector of developing economies. Thus, implications of the Technology Acceptance
Model (TAM) came into play and provide a tangible theory for study.
Individual impact: Individual impact refers to an increase in an individual’s efficiency by the use of
the ERP system in the organization. This research is related to healthcare service quality and includes
nurses and doctors and covers four characteristics;i.e.,productivity of the individual,learning,
decision making in an effective manner,and awareness of the individual.The overall healthcare
service quality is dependent on the individual productivity and performance. Use of the ERP system in
healthcare plays an eminent role in enhancing the productivity of the individual. Enterprise Resource
Planning systems teach individuals with new practices, and therefore enhance learning. Such systems
make all data available quickly and have a positive influence on decision making (Kanellou and
Spathis 2013). Moreover, the ERP system helps professionals become more aware of their job detail
The following hypotheses are postulated to answer the research objectives that we outlined in the
introductory section:
Hypothesis 1 (H1). Individual impact has a positive relationship with service quality in healthcare.
Organizational impact:Organizational impact refers to the welfares that are received by an
organization through the implementation of an ERP system.Impact of an information system is
evaluated through business performance in the healthcare sector (Rai et al. 2006). The organizational
impact is measured as organizational efficiency, market value, effectiveness, competitive advantage,
and strategic value. It includes cost reduction, capacity improvement, business process variation, and
productivity enhancement.
Hypothesis 2 (H2). Organizational impact has a positive relationship with service quality in healthcar
Information quality:Information quality deals with the quality ofthe information system.
Information quality dimensionsinclude accuracy,currency,completeness,and consistency
(Acharyulu 2012). ERP systems are valuable in information sorting but are not as good for providing
information to a user about specific benefit.
Hypothesis 3 (H3).Information quality impact has a positive relationship with service quality in the
healthcare sector.
System Quality: System quality refers to the extent to which the information system is evaluated
concerning the technical and design aspects.According to Gorla et al.(2010), it is the measurement
of the soundness of the system.Delone and McLean (2003) mention the attributes of system quality
measurement;i.e.,quality of data,the reliability of data,ease of use,functionality,and integration.
System quality covers the facts that the system is easy to use, the quality of documentation, the presence
or absence of bugs in system, and the maintenance of quality of the program (Cucciniello et al. 2016).
Hypothesis 4 (H4). System quality impact has a positive relationship with service quality in healthcar
Adm. Sci. 2018, 8, 38 6 of 12
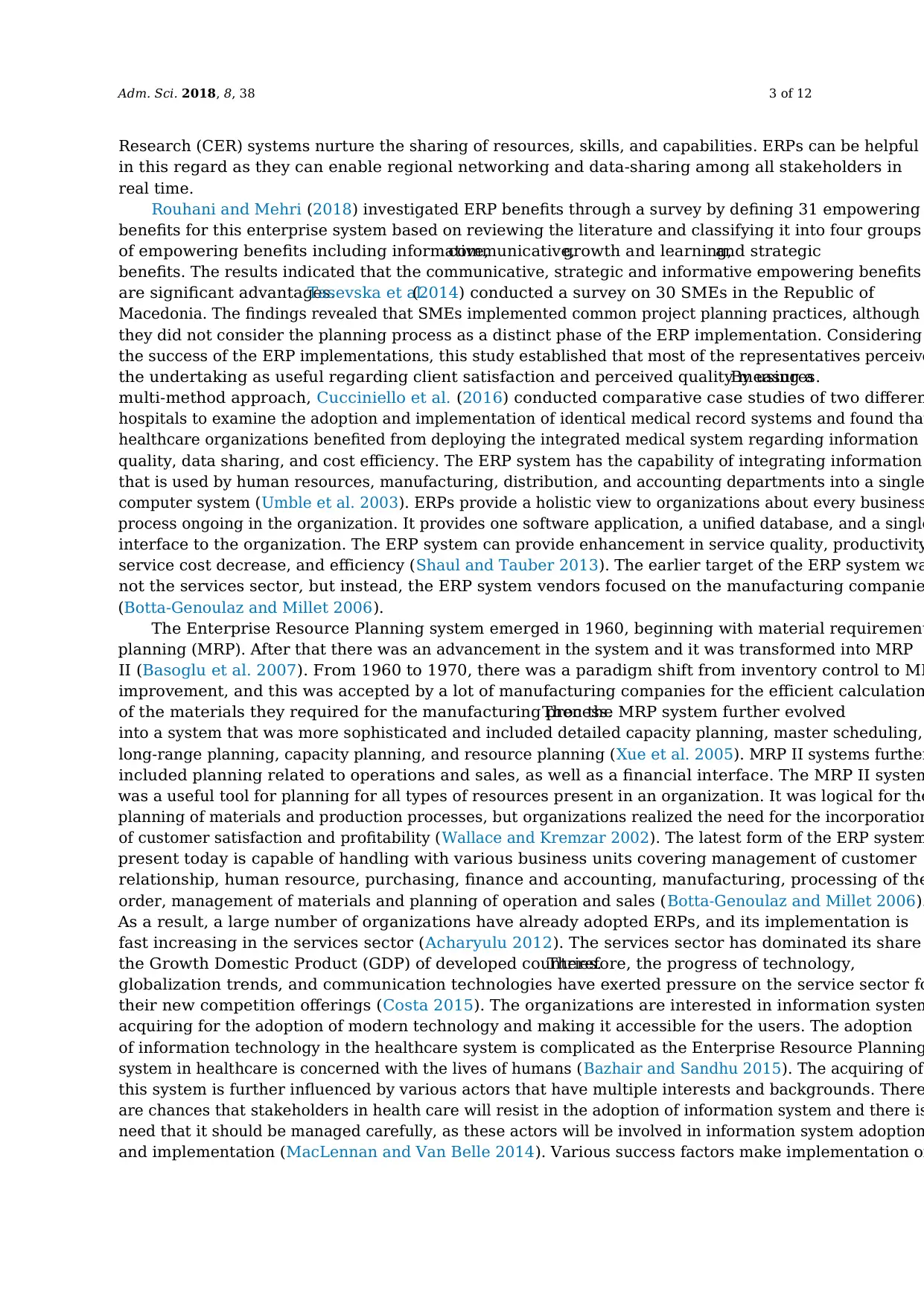
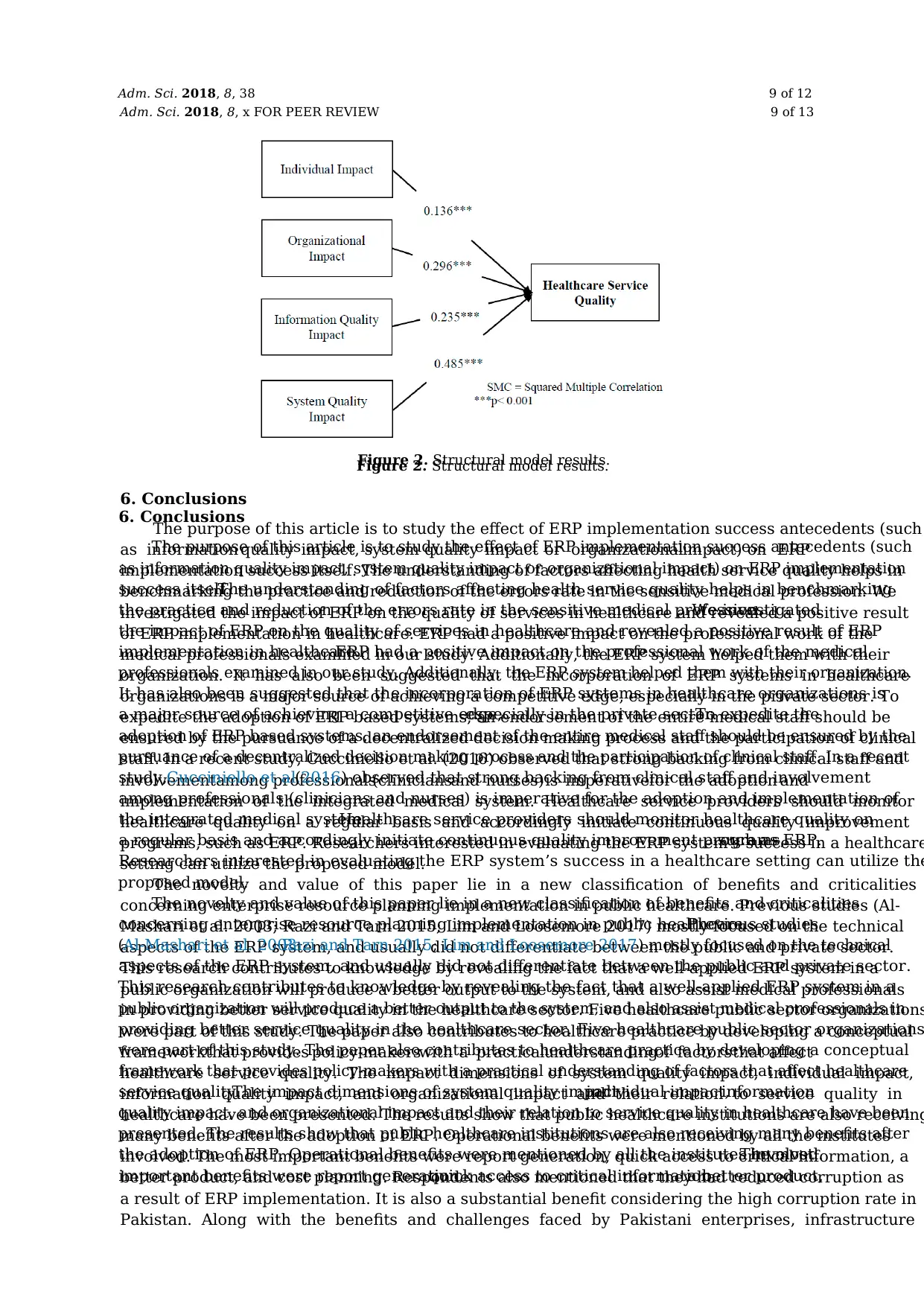
By the abovementioned formulated hypotheses, a research model is proposed to evaluate the
impact of individual, organizational, information, and the system quality of an ERP on healthcare
service quality (Figure 1).
Adm. Sci. 2018, 8, x FOR PEER REVIEW 6 of 13
By the abovementioned formulated hypotheses, a research model is proposed to evaluate the
impact of individual, organizational, information, and the system quality of an ERP on healthcare
service quality (Figure 1).
Figure 1. The proposed research model.
4. Research Design
Design of Questionnaire: The survey instrument of Questionnaire is utilized for data collection.
The questionnaire has been reproduced from the service quality of healthcare and information system
dimensions. The research instrument is based on three parts. The first part covers the use and impact
of ERP Systems; the second part deals with the service quality of healthcare, and the third part is
comprised of the demographic variables.
The first part of the questionnaire is based on five impact variables, namely, individual impact,
system quality impact, organizational impact, information quality impact, and overall impact by the
use of ERP in a healthcare setting, which was analysed through questions as put forward by Gable et
al. (2008).
System quality impact describes the performance grade of the ERP from a technical perspective.
It covers system accuracy, customization and integration, ease of use, efficiency, system features, ease
of learning, the sophistication of system, access, reliability, and flexibility and user requirements
Information quality impact deals with the quality of the information created by the ERP system to be
used in a healthcare setting. This variable is measured with the help of ten questions, which includes
content accuracy of the medical field, the usability of information for medical staff, conciseness
availability of information, timeliness and uniqueness,importance,relevance,format, and
comprehensibility. Organizational impact is measured by using eight questions that deal with
improved outcomes, organizational cost, e-government, cost reduction, business process change,
staff requirement, increased capacity, and overall productivity. The individual impact is analysed
with the help of four questions that cover individual productivity, awareness, and knowledge of
doctors about their field, individual learning, and decision effectiveness. Overall, the variable
‘impact’ covers questions about overall ERP system including impacts on the individual and impact
on the organization.
The second section of questionnaire deals with the performance of service quality in healthcare.
The measurement of this variable can be made by measuring Responsiveness, Reliability, Assurance,
and Empathy. The respondents had to answer seventeen questions, and these were reproduced using
the SERVQUAL scale, following the dimensions of healthcare setting as reported by Lee et al. (2000).
These questions were close-ended with multiple choices on the five-point Likert scale. Closed
Figure 1. The proposed research model.
4. Research Design
Design of Questionnaire:The survey instrument of Questionnaire is utilized for data collection.
The questionnaire has been reproduced from the service quality of healthcare and information system
dimensions. The research instrument is based on three parts. The first part covers the use and impact
of ERP Systems;the second part deals with the service quality of healthcare, and the third part is
comprised of the demographic variables.
The first part of the questionnaire is based on five impact variables, namely, individual impact,
system quality impact,organizational impact,information quality impact,and overall impact by
the use of ERP in a healthcare setting,which was analysed through questions as put forward by
Gable et al. (2008).
System quality impact describes the performance grade of the ERP from a technical perspective.
It covers system accuracy, customization and integration, ease of use, efficiency, system features, ease
of learning,the sophistication of system,access,reliability,and flexibility and user requirements.
Information quality impact deals with the quality of the information created by the ERP system
to be used in a healthcare setting.This variable is measured with the help often questions,
which includes content accuracy of the medical field, the usability of information for medical staff,
conciseness, availability of information, timeliness and uniqueness, importance, relevance, format,
and comprehensibility.Organizational impact is measured by using eight questions that deal with
improved outcomes,organizational cost,e-government,cost reduction,business process change,
staff requirement, increased capacity, and overall productivity.The individual impact is analysed
with the help of four questions that cover individual productivity,awareness,and knowledge of
doctors about their field, individual learning, and decision effectiveness. Overall, the variable ‘impact’
covers questions about overallERP system including impacts on the individualand impact on
the organization.
The second section of questionnaire deals with the performance of service quality in healthcare.
The measurement of this variable can be made by measuring Responsiveness, Reliability, Assurance,
and Empathy. The respondents had to answer seventeen questions, and these were reproduced using
the SERVQUAL scale, following the dimensions of healthcare setting as reported byLee et al. (2000).
By the abovementioned formulated hypotheses, a research model is proposed to evaluate the
impact of individual, organizational, information, and the system quality of an ERP on healthcare
service quality (Figure 1).
Adm. Sci. 2018, 8, x FOR PEER REVIEW 6 of 13
By the abovementioned formulated hypotheses, a research model is proposed to evaluate the
impact of individual, organizational, information, and the system quality of an ERP on healthcare
service quality (Figure 1).
Figure 1. The proposed research model.
4. Research Design
Design of Questionnaire: The survey instrument of Questionnaire is utilized for data collection.
The questionnaire has been reproduced from the service quality of healthcare and information system
dimensions. The research instrument is based on three parts. The first part covers the use and impact
of ERP Systems; the second part deals with the service quality of healthcare, and the third part is
comprised of the demographic variables.
The first part of the questionnaire is based on five impact variables, namely, individual impact,
system quality impact, organizational impact, information quality impact, and overall impact by the
use of ERP in a healthcare setting, which was analysed through questions as put forward by Gable et
al. (2008).
System quality impact describes the performance grade of the ERP from a technical perspective.
It covers system accuracy, customization and integration, ease of use, efficiency, system features, ease
of learning, the sophistication of system, access, reliability, and flexibility and user requirements
Information quality impact deals with the quality of the information created by the ERP system to be
used in a healthcare setting. This variable is measured with the help of ten questions, which includes
content accuracy of the medical field, the usability of information for medical staff, conciseness
availability of information, timeliness and uniqueness,importance,relevance,format, and
comprehensibility. Organizational impact is measured by using eight questions that deal with
improved outcomes, organizational cost, e-government, cost reduction, business process change,
staff requirement, increased capacity, and overall productivity. The individual impact is analysed
with the help of four questions that cover individual productivity, awareness, and knowledge of
doctors about their field, individual learning, and decision effectiveness. Overall, the variable
‘impact’ covers questions about overall ERP system including impacts on the individual and impact
on the organization.
The second section of questionnaire deals with the performance of service quality in healthcare.
The measurement of this variable can be made by measuring Responsiveness, Reliability, Assurance,
and Empathy. The respondents had to answer seventeen questions, and these were reproduced using
the SERVQUAL scale, following the dimensions of healthcare setting as reported by Lee et al. (2000).
These questions were close-ended with multiple choices on the five-point Likert scale. Closed
Figure 1. The proposed research model.
4. Research Design
Design of Questionnaire:The survey instrument of Questionnaire is utilized for data collection.
The questionnaire has been reproduced from the service quality of healthcare and information system
dimensions. The research instrument is based on three parts. The first part covers the use and impact
of ERP Systems;the second part deals with the service quality of healthcare, and the third part is
comprised of the demographic variables.
The first part of the questionnaire is based on five impact variables, namely, individual impact,
system quality impact,organizational impact,information quality impact,and overall impact by
the use of ERP in a healthcare setting,which was analysed through questions as put forward by
Gable et al. (2008).
System quality impact describes the performance grade of the ERP from a technical perspective.
It covers system accuracy, customization and integration, ease of use, efficiency, system features, ease
of learning,the sophistication of system,access,reliability,and flexibility and user requirements.
Information quality impact deals with the quality of the information created by the ERP system
to be used in a healthcare setting.This variable is measured with the help often questions,
which includes content accuracy of the medical field, the usability of information for medical staff,
conciseness, availability of information, timeliness and uniqueness, importance, relevance, format,
and comprehensibility.Organizational impact is measured by using eight questions that deal with
improved outcomes,organizational cost,e-government,cost reduction,business process change,
staff requirement, increased capacity, and overall productivity.The individual impact is analysed
with the help of four questions that cover individual productivity,awareness,and knowledge of
doctors about their field, individual learning, and decision effectiveness. Overall, the variable ‘impact’
covers questions about overallERP system including impacts on the individualand impact on
the organization.
The second section of questionnaire deals with the performance of service quality in healthcare.
The measurement of this variable can be made by measuring Responsiveness, Reliability, Assurance,
and Empathy. The respondents had to answer seventeen questions, and these were reproduced using
the SERVQUAL scale, following the dimensions of healthcare setting as reported byLee et al. (2000).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Adm. Sci. 2018, 8, 38 7 of 12
These questions were close-ended with multiple choices on the five-point Likert scale.Closed
questionnaires are easy to fill out by respondents and also suitable for analysis.The Likert scale
in the present study ranged from 1 to 5. 1 = strongly disagree, 2 = disagree, 3 = neither disagree no
agree, 4 = agree, and 5 = strongly disagree. The last part deals with the demographic information of the
respondent (medical staff) and includes name, position in the organization, and relevant experience.
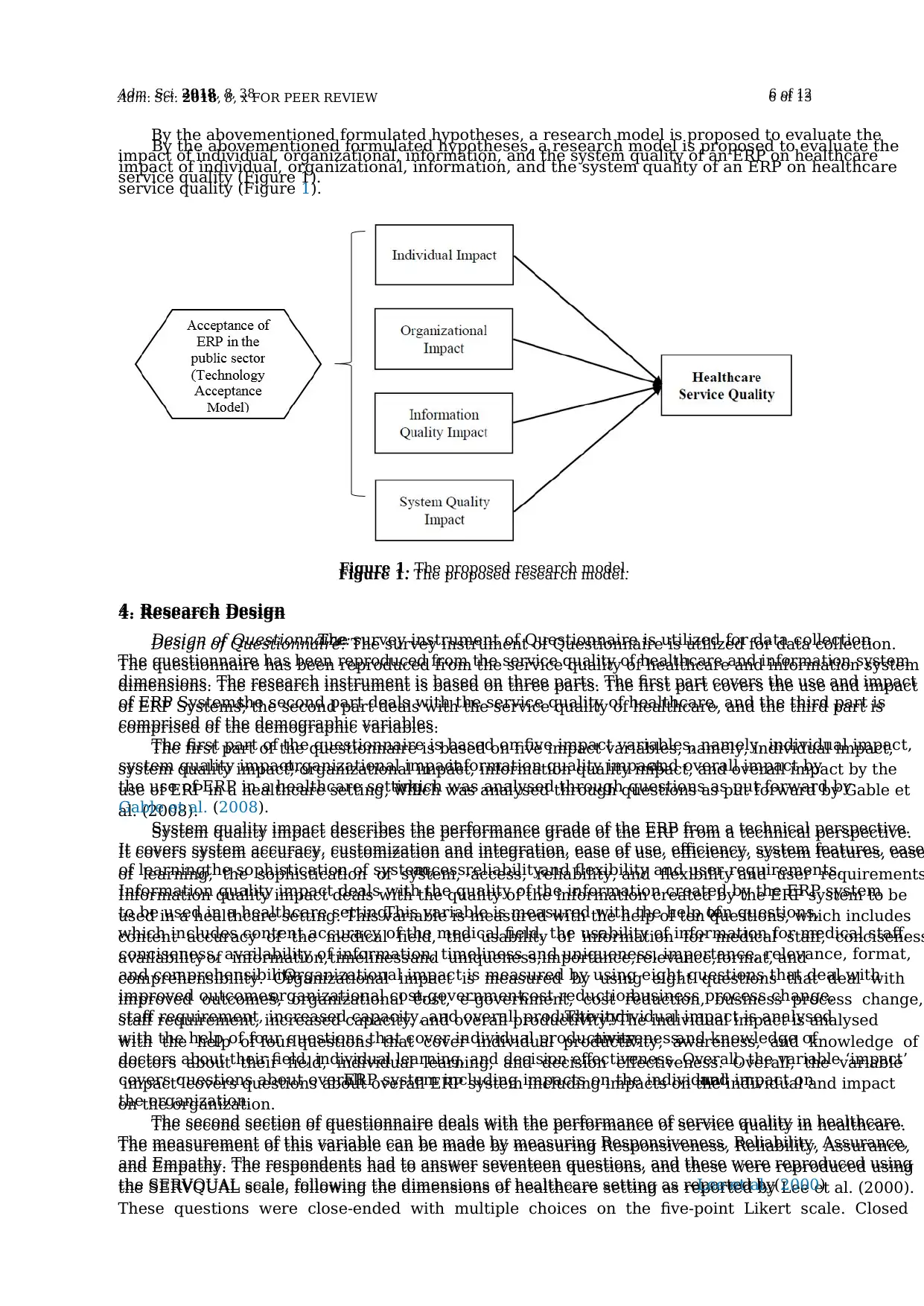
Collection of data: The study uses a mixed methods approach, wherein both primary and secondary
sources are utilized for the collection of data.For the empirical investigation, questionnaires were
used for the collection of primary data, whereas archival data is used to collect secondary data for
model construction.In total, 500 self-administered questionnaires were disbursed to respondents
of five healthcare organizations in the city of Lahore, Pakistan1. We selected both the private and
public healthcare organizations, as the primary consideration was the implementation of ERP system.
Out of which, we got feedback from 279 respondents, and this depicts that the response rate is 56%.
The respondent’s demographic characteristics are presented in Table 1.
Table 1. Demographic characteristics of the respondents.
Measure Value Frequency Percentage
Gender Male 156 55.9%
Female 123 44.1%
Age <25 104 37.3%
26–30 95 34.1%
31–35 57 20.4%
36–40 13 4.7%
>40 10 3.6%
Degree of Experience <3 92 33.0%
3–5 114 40.9%
>5 73 26.2%
Job Title Doctor 60 21.5%
Medical Staff 149 53.4%
Administration Staff 70 25.1%
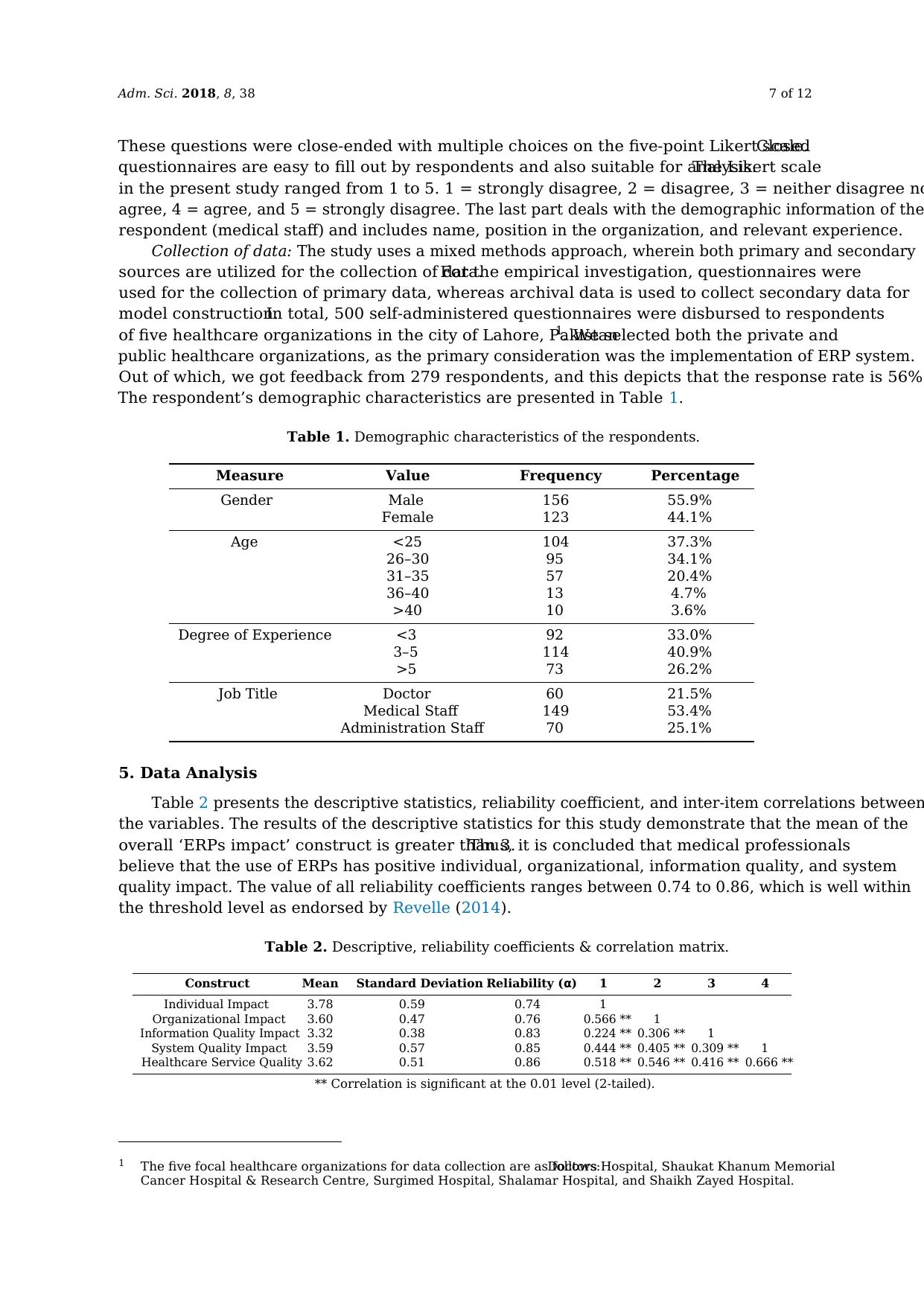
5. Data Analysis
Table 2 presents the descriptive statistics, reliability coefficient, and inter-item correlations between
the variables. The results of the descriptive statistics for this study demonstrate that the mean of the
overall ‘ERPs impact’ construct is greater than 3.Thus, it is concluded that medical professionals
believe that the use of ERPs has positive individual, organizational, information quality, and system
quality impact. The value of all reliability coefficients ranges between 0.74 to 0.86, which is well within
the threshold level as endorsed by Revelle (2014).
Table 2. Descriptive, reliability coefficients & correlation matrix.
Construct Mean Standard Deviation Reliability (α) 1 2 3 4
Individual Impact 3.78 0.59 0.74 1
Organizational Impact 3.60 0.47 0.76 0.566 ** 1
Information Quality Impact 3.32 0.38 0.83 0.224 ** 0.306 ** 1
System Quality Impact 3.59 0.57 0.85 0.444 ** 0.405 ** 0.309 ** 1
Healthcare Service Quality 3.62 0.51 0.86 0.518 ** 0.546 ** 0.416 ** 0.666 **
** Correlation is significant at the 0.01 level (2-tailed).
1 The five focal healthcare organizations for data collection are as follows:Doctors Hospital, Shaukat Khanum Memorial
Cancer Hospital & Research Centre, Surgimed Hospital, Shalamar Hospital, and Shaikh Zayed Hospital.
These questions were close-ended with multiple choices on the five-point Likert scale.Closed
questionnaires are easy to fill out by respondents and also suitable for analysis.The Likert scale
in the present study ranged from 1 to 5. 1 = strongly disagree, 2 = disagree, 3 = neither disagree no
agree, 4 = agree, and 5 = strongly disagree. The last part deals with the demographic information of the
respondent (medical staff) and includes name, position in the organization, and relevant experience.
Collection of data: The study uses a mixed methods approach, wherein both primary and secondary
sources are utilized for the collection of data.For the empirical investigation, questionnaires were
used for the collection of primary data, whereas archival data is used to collect secondary data for
model construction.In total, 500 self-administered questionnaires were disbursed to respondents
of five healthcare organizations in the city of Lahore, Pakistan1. We selected both the private and
public healthcare organizations, as the primary consideration was the implementation of ERP system.
Out of which, we got feedback from 279 respondents, and this depicts that the response rate is 56%.
The respondent’s demographic characteristics are presented in Table 1.
Table 1. Demographic characteristics of the respondents.
Measure Value Frequency Percentage
Gender Male 156 55.9%
Female 123 44.1%
Age <25 104 37.3%
26–30 95 34.1%
31–35 57 20.4%
36–40 13 4.7%
>40 10 3.6%
Degree of Experience <3 92 33.0%
3–5 114 40.9%
>5 73 26.2%
Job Title Doctor 60 21.5%
Medical Staff 149 53.4%
Administration Staff 70 25.1%
5. Data Analysis
Table 2 presents the descriptive statistics, reliability coefficient, and inter-item correlations between
the variables. The results of the descriptive statistics for this study demonstrate that the mean of the
overall ‘ERPs impact’ construct is greater than 3.Thus, it is concluded that medical professionals
believe that the use of ERPs has positive individual, organizational, information quality, and system
quality impact. The value of all reliability coefficients ranges between 0.74 to 0.86, which is well within
the threshold level as endorsed by Revelle (2014).
Table 2. Descriptive, reliability coefficients & correlation matrix.
Construct Mean Standard Deviation Reliability (α) 1 2 3 4
Individual Impact 3.78 0.59 0.74 1
Organizational Impact 3.60 0.47 0.76 0.566 ** 1
Information Quality Impact 3.32 0.38 0.83 0.224 ** 0.306 ** 1
System Quality Impact 3.59 0.57 0.85 0.444 ** 0.405 ** 0.309 ** 1
Healthcare Service Quality 3.62 0.51 0.86 0.518 ** 0.546 ** 0.416 ** 0.666 **
** Correlation is significant at the 0.01 level (2-tailed).
1 The five focal healthcare organizations for data collection are as follows:Doctors Hospital, Shaukat Khanum Memorial
Cancer Hospital & Research Centre, Surgimed Hospital, Shalamar Hospital, and Shaikh Zayed Hospital.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Adm. Sci. 2018, 8, 38 8 of 12
Correlation matrix for dependent and independent variables reveals that individual impact
(independent variable) is significantly correlated (r = 0.518, p < 0.01) with service quality in healthcare
(dependent variable). Likewise, the organizational impact is positively correlated (r = 0.546,p < 0.01)
with service quality in healthcare. Information quality impact also has a positive correlation (r = 0.416,
p < 0.01) with service quality in healthcare. “System quality impact” is found to be positively correlated
(r = 0.666, p < 0.01) with service quality in healthcare. Therefore, correlation of independent variables
including individual, organizational, and system quality impact is strong in nature and the correlation
of “Information Quality Impact” with “Healthcare Service Quality” is a moderator in nature as
described by Field (2013).
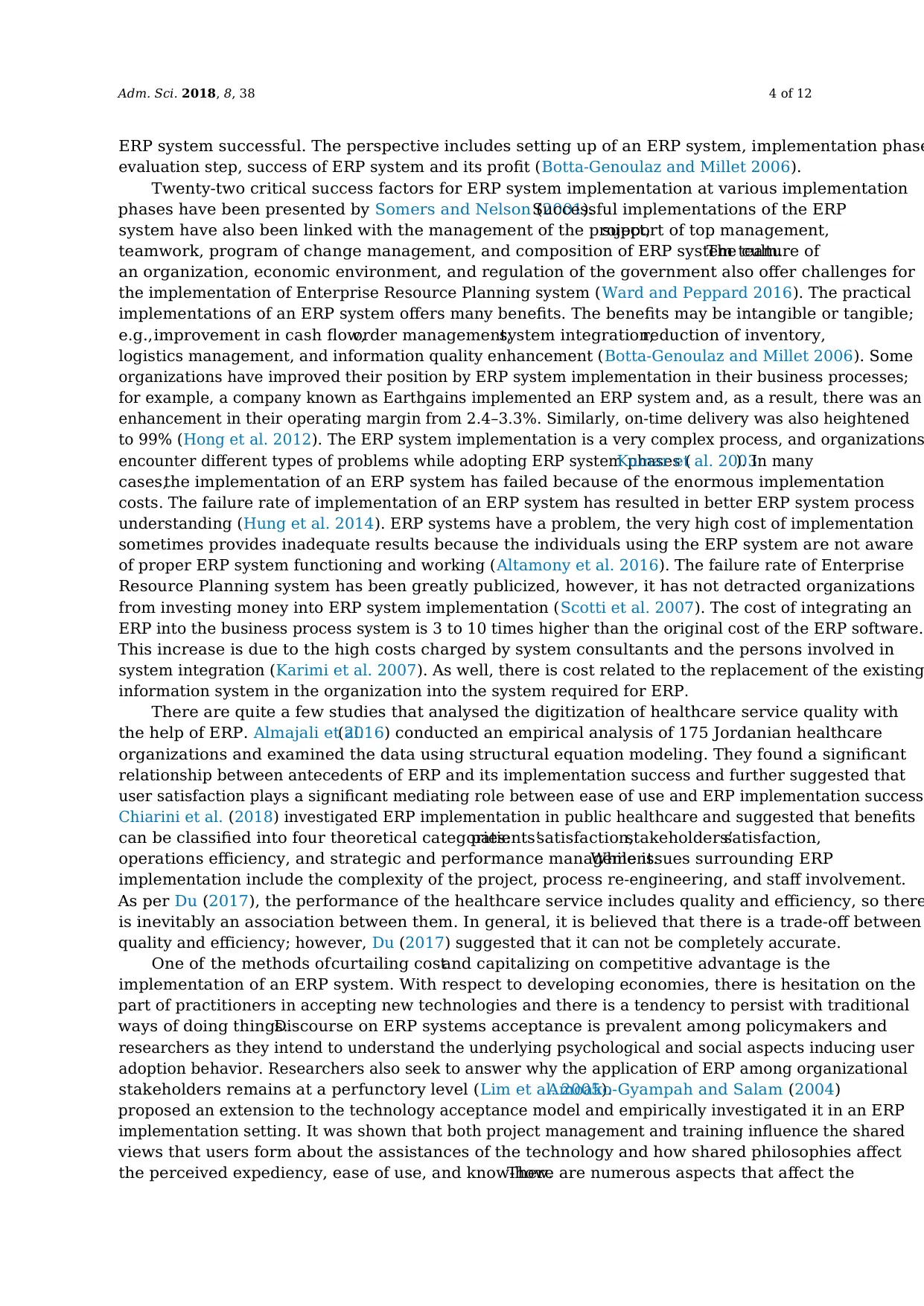
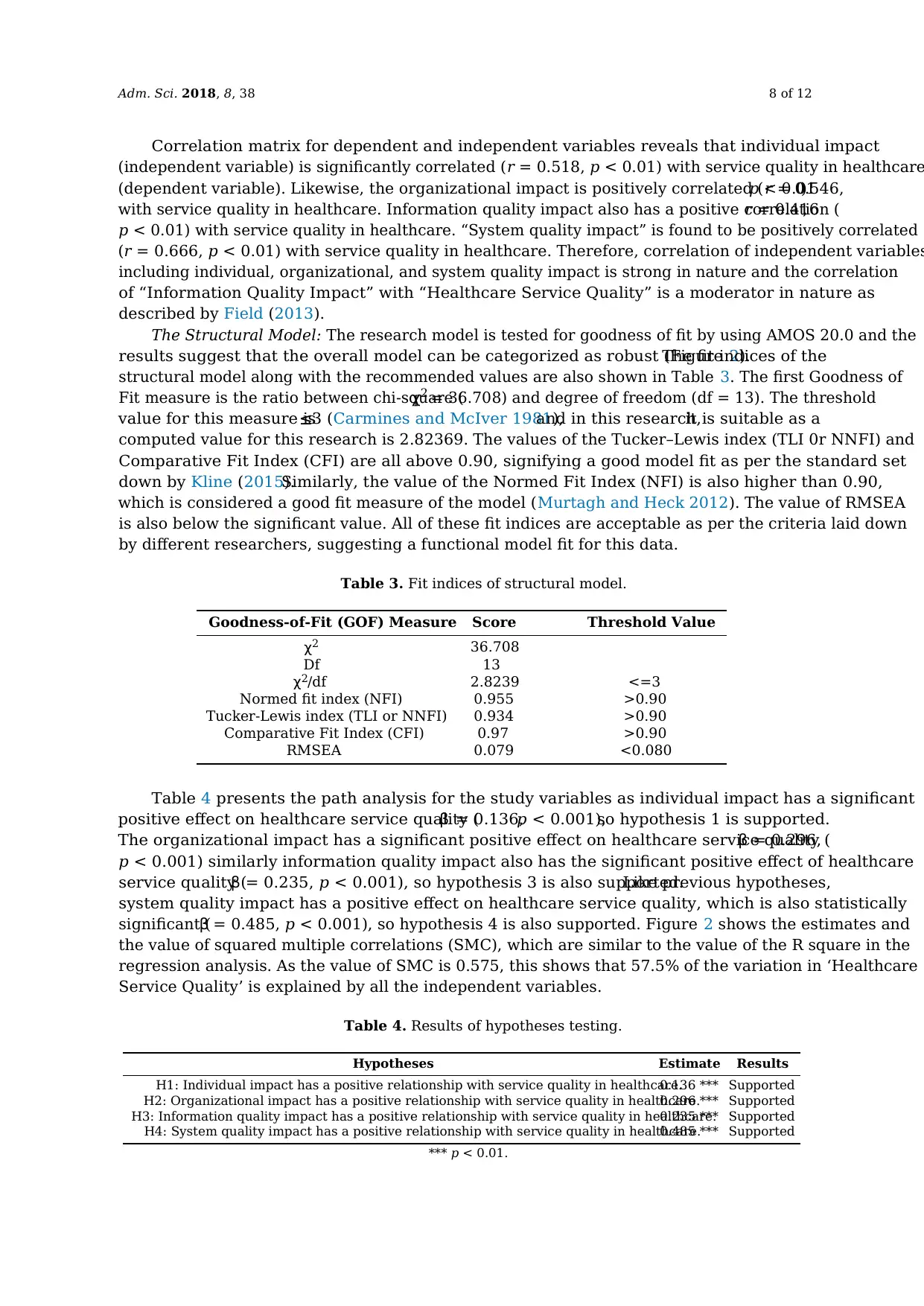
The Structural Model: The research model is tested for goodness of fit by using AMOS 20.0 and the
results suggest that the overall model can be categorized as robust (Figure 2).The fit indices of the
structural model along with the recommended values are also shown in Table 3. The first Goodness of
Fit measure is the ratio between chi-square (χ2 = 36.708) and degree of freedom (df = 13). The threshold
value for this measure is≤3 (Carmines and McIver 1981),and in this research,it is suitable as a
computed value for this research is 2.82369. The values of the Tucker–Lewis index (TLI 0r NNFI) and
Comparative Fit Index (CFI) are all above 0.90, signifying a good model fit as per the standard set
down by Kline (2015).Similarly, the value of the Normed Fit Index (NFI) is also higher than 0.90,
which is considered a good fit measure of the model (Murtagh and Heck 2012). The value of RMSEA
is also below the significant value. All of these fit indices are acceptable as per the criteria laid down
by different researchers, suggesting a functional model fit for this data.
Table 3. Fit indices of structural model.
Goodness-of-Fit (GOF) Measure Score Threshold Value
χ2 36.708
Df 13
χ2/df 2.8239 <=3
Normed fit index (NFI) 0.955 >0.90
Tucker-Lewis index (TLI or NNFI) 0.934 >0.90
Comparative Fit Index (CFI) 0.97 >0.90
RMSEA 0.079 <0.080
Table 4 presents the path analysis for the study variables as individual impact has a significant
positive effect on healthcare service quality (β = 0.136,p < 0.001),so hypothesis 1 is supported.
The organizational impact has a significant positive effect on healthcare service quality (β = 0.296,
p < 0.001) similarly information quality impact also has the significant positive effect of healthcare
service quality (β = 0.235, p < 0.001), so hypothesis 3 is also supported.Like previous hypotheses,
system quality impact has a positive effect on healthcare service quality, which is also statistically
significant (β = 0.485, p < 0.001), so hypothesis 4 is also supported. Figure 2 shows the estimates and
the value of squared multiple correlations (SMC), which are similar to the value of the R square in the
regression analysis. As the value of SMC is 0.575, this shows that 57.5% of the variation in ‘Healthcare
Service Quality’ is explained by all the independent variables.
Table 4. Results of hypotheses testing.
Hypotheses Estimate Results
H1: Individual impact has a positive relationship with service quality in healthcare.0.136 *** Supported
H2: Organizational impact has a positive relationship with service quality in healthcare.0.296 *** Supported
H3: Information quality impact has a positive relationship with service quality in healthcare.0.235 *** Supported
H4: System quality impact has a positive relationship with service quality in healthcare.0.485 *** Supported
*** p < 0.01.
Correlation matrix for dependent and independent variables reveals that individual impact
(independent variable) is significantly correlated (r = 0.518, p < 0.01) with service quality in healthcare
(dependent variable). Likewise, the organizational impact is positively correlated (r = 0.546,p < 0.01)
with service quality in healthcare. Information quality impact also has a positive correlation (r = 0.416,
p < 0.01) with service quality in healthcare. “System quality impact” is found to be positively correlated
(r = 0.666, p < 0.01) with service quality in healthcare. Therefore, correlation of independent variables
including individual, organizational, and system quality impact is strong in nature and the correlation
of “Information Quality Impact” with “Healthcare Service Quality” is a moderator in nature as
described by Field (2013).
The Structural Model: The research model is tested for goodness of fit by using AMOS 20.0 and the
results suggest that the overall model can be categorized as robust (Figure 2).The fit indices of the
structural model along with the recommended values are also shown in Table 3. The first Goodness of
Fit measure is the ratio between chi-square (χ2 = 36.708) and degree of freedom (df = 13). The threshold
value for this measure is≤3 (Carmines and McIver 1981),and in this research,it is suitable as a
computed value for this research is 2.82369. The values of the Tucker–Lewis index (TLI 0r NNFI) and
Comparative Fit Index (CFI) are all above 0.90, signifying a good model fit as per the standard set
down by Kline (2015).Similarly, the value of the Normed Fit Index (NFI) is also higher than 0.90,
which is considered a good fit measure of the model (Murtagh and Heck 2012). The value of RMSEA
is also below the significant value. All of these fit indices are acceptable as per the criteria laid down
by different researchers, suggesting a functional model fit for this data.
Table 3. Fit indices of structural model.
Goodness-of-Fit (GOF) Measure Score Threshold Value
χ2 36.708
Df 13
χ2/df 2.8239 <=3
Normed fit index (NFI) 0.955 >0.90
Tucker-Lewis index (TLI or NNFI) 0.934 >0.90
Comparative Fit Index (CFI) 0.97 >0.90
RMSEA 0.079 <0.080
Table 4 presents the path analysis for the study variables as individual impact has a significant
positive effect on healthcare service quality (β = 0.136,p < 0.001),so hypothesis 1 is supported.
The organizational impact has a significant positive effect on healthcare service quality (β = 0.296,
p < 0.001) similarly information quality impact also has the significant positive effect of healthcare
service quality (β = 0.235, p < 0.001), so hypothesis 3 is also supported.Like previous hypotheses,
system quality impact has a positive effect on healthcare service quality, which is also statistically
significant (β = 0.485, p < 0.001), so hypothesis 4 is also supported. Figure 2 shows the estimates and
the value of squared multiple correlations (SMC), which are similar to the value of the R square in the
regression analysis. As the value of SMC is 0.575, this shows that 57.5% of the variation in ‘Healthcare
Service Quality’ is explained by all the independent variables.
Table 4. Results of hypotheses testing.
Hypotheses Estimate Results
H1: Individual impact has a positive relationship with service quality in healthcare.0.136 *** Supported
H2: Organizational impact has a positive relationship with service quality in healthcare.0.296 *** Supported
H3: Information quality impact has a positive relationship with service quality in healthcare.0.235 *** Supported
H4: System quality impact has a positive relationship with service quality in healthcare.0.485 *** Supported
*** p < 0.01.
Adm. Sci. 2018, 8, 38 9 of 12
Adm. Sci. 2018, 8, x FOR PEER REVIEW 9 of 13
Figure 2. Structural model results.
6. Conclusions
The purpose of this article is to study the effect of ERP implementation success antecedents (such
as information quality impact, system quality impact or organizationalimpact) on ERP
implementation success itself. The understanding of factors affecting health service quality helps in
benchmarking the practice and reduction of the errors rate in the sensitive medical profession. We
investigated the impact of ERP on the quality of services in healthcare and revealed a positive result
of ERP implementation in healthcare. ERP had a positive impact on the professional work of the
medical professionals examined in our study. Additionally, the ERP system helped them with their
organization. It has also been suggested that the incorporation of ERP systems in healthcare
organizations is a major source of achieving a competitive edge, especially in the private sector. To
expedite the adoption of ERP based systems, an endorsement of the entire medical staff should be
ensured by the pursuance of a decentralized decision making process and the participation of clinical
staff. In a recent study, Cucciniello et al. (2016) observed that strong backing from clinical staff and
involvementamong professionals(cliniciansand nurses) is imperativefor the adoption and
implementation of the integrated medical system. Healthcare service providers should monitor
healthcare quality on a regular basis and accordingly initiate continuous quality improvement
programs, such as ERP. Researchers interested in evaluating the ERP system’s success in a healthcare
setting can utilize the proposed model.
The novelty and value of this paper lie in a new classification of benefits and criticalities
concerning enterprise resource planning implementation in public healthcare. Previous studies (Al-
Mashari et al. 2003; Razi and Tarn 2015; Lim and Loosemore 2017) mostly focused on the technical
aspects of the ERP system, and usually did not differentiate between the public and private sector.
This research contributes to knowledge by revealing the fact that a well-applied ERP system in a
public organization will produce a better output to the system, and also assist medical professionals
in providing better service quality in the healthcare sector. Five healthcare public sector organizations
were part of this study. The paper also contributes to healthcare practice by developing a conceptual
frameworkthat provides policy-makerswith a practicalunderstandingof factors that affect
healthcare service quality. The impact dimensions of system quality impact, individual impact,
information quality impact, and organizational impact and their relation to service quality in
healthcare have been presented. The results show that public healthcare institutions are also receiving
many benefits after the adoption of ERP. Operational benefits were mentioned by all the institutes
involved. The most important benefits were report generation, quick access to critical information, a
better product, and cost planning. Respondents also mentioned that they had reduced corruption as
a result of ERP implementation. It is also a substantial benefit considering the high corruption rate in
Pakistan. Along with the benefits and challenges faced by Pakistani enterprises, infrastructure
Figure 2. Structural model results.
6. Conclusions
The purpose of this article is to study the effect of ERP implementation success antecedents (such
as information quality impact, system quality impact or organizational impact) on ERP implementation
success itself.The understanding of factors affecting health service quality helps in benchmarking
the practice and reduction of the errors rate in the sensitive medical profession.We investigated
the impact of ERP on the quality of services in healthcare and revealed a positive result of ERP
implementation in healthcare.ERP had a positive impact on the professional work of the medical
professionals examined in our study. Additionally, the ERP system helped them with their organization.
It has also been suggested that the incorporation of ERP systems in healthcare organizations is
a major source of achieving a competitive edge,especially in the private sector.To expedite the
adoption of ERP based systems, an endorsement of the entire medical staff should be ensured by the
pursuance of a decentralized decision making process and the participation of clinical staff. In a recent
study,Cucciniello et al.(2016) observed that strong backing from clinical staff and involvement
among professionals (clinicians and nurses) is imperative for the adoption and implementation of
the integrated medical system.Healthcare service providers should monitor healthcare quality on
a regular basis and accordingly initiate continuous quality improvement programs,such as ERP.
Researchers interested in evaluating the ERP system’s success in a healthcare setting can utilize the
proposed model.
The novelty and value of this paper lie in a new classification of benefits and criticalities
concerning enterprise resource planning implementation in public healthcare.Previous studies
(Al-Mashari et al. 2003; Razi and Tarn 2015; Lim and Loosemore 2017) mostly focused on the technical
aspects of the ERP system, and usually did not differentiate between the public and private sector.
This research contributes to knowledge by revealing the fact that a well-applied ERP system in a
public organization will produce a better output to the system, and also assist medical professionals in
providing better service quality in the healthcare sector. Five healthcare public sector organizations
were part of this study. The paper also contributes to healthcare practice by developing a conceptual
framework that provides policy-makers with a practical understanding of factors that affect healthcare
service quality.The impact dimensions of system quality impact,individual impact,information
quality impact, and organizational impact and their relation to service quality in healthcare have been
presented. The results show that public healthcare institutions are also receiving many benefits after
the adoption of ERP. Operational benefits were mentioned by all the institutes involved.The most
important benefits were report generation,quick access to critical information,a better product,
Adm. Sci. 2018, 8, x FOR PEER REVIEW 9 of 13
Figure 2. Structural model results.
6. Conclusions
The purpose of this article is to study the effect of ERP implementation success antecedents (such
as information quality impact, system quality impact or organizationalimpact) on ERP
implementation success itself. The understanding of factors affecting health service quality helps in
benchmarking the practice and reduction of the errors rate in the sensitive medical profession. We
investigated the impact of ERP on the quality of services in healthcare and revealed a positive result
of ERP implementation in healthcare. ERP had a positive impact on the professional work of the
medical professionals examined in our study. Additionally, the ERP system helped them with their
organization. It has also been suggested that the incorporation of ERP systems in healthcare
organizations is a major source of achieving a competitive edge, especially in the private sector. To
expedite the adoption of ERP based systems, an endorsement of the entire medical staff should be
ensured by the pursuance of a decentralized decision making process and the participation of clinical
staff. In a recent study, Cucciniello et al. (2016) observed that strong backing from clinical staff and
involvementamong professionals(cliniciansand nurses) is imperativefor the adoption and
implementation of the integrated medical system. Healthcare service providers should monitor
healthcare quality on a regular basis and accordingly initiate continuous quality improvement
programs, such as ERP. Researchers interested in evaluating the ERP system’s success in a healthcare
setting can utilize the proposed model.
The novelty and value of this paper lie in a new classification of benefits and criticalities
concerning enterprise resource planning implementation in public healthcare. Previous studies (Al-
Mashari et al. 2003; Razi and Tarn 2015; Lim and Loosemore 2017) mostly focused on the technical
aspects of the ERP system, and usually did not differentiate between the public and private sector.
This research contributes to knowledge by revealing the fact that a well-applied ERP system in a
public organization will produce a better output to the system, and also assist medical professionals
in providing better service quality in the healthcare sector. Five healthcare public sector organizations
were part of this study. The paper also contributes to healthcare practice by developing a conceptual
frameworkthat provides policy-makerswith a practicalunderstandingof factors that affect
healthcare service quality. The impact dimensions of system quality impact, individual impact,
information quality impact, and organizational impact and their relation to service quality in
healthcare have been presented. The results show that public healthcare institutions are also receiving
many benefits after the adoption of ERP. Operational benefits were mentioned by all the institutes
involved. The most important benefits were report generation, quick access to critical information, a
better product, and cost planning. Respondents also mentioned that they had reduced corruption as
a result of ERP implementation. It is also a substantial benefit considering the high corruption rate in
Pakistan. Along with the benefits and challenges faced by Pakistani enterprises, infrastructure
Figure 2. Structural model results.
6. Conclusions
The purpose of this article is to study the effect of ERP implementation success antecedents (such
as information quality impact, system quality impact or organizational impact) on ERP implementation
success itself.The understanding of factors affecting health service quality helps in benchmarking
the practice and reduction of the errors rate in the sensitive medical profession.We investigated
the impact of ERP on the quality of services in healthcare and revealed a positive result of ERP
implementation in healthcare.ERP had a positive impact on the professional work of the medical
professionals examined in our study. Additionally, the ERP system helped them with their organization.
It has also been suggested that the incorporation of ERP systems in healthcare organizations is
a major source of achieving a competitive edge,especially in the private sector.To expedite the
adoption of ERP based systems, an endorsement of the entire medical staff should be ensured by the
pursuance of a decentralized decision making process and the participation of clinical staff. In a recent
study,Cucciniello et al.(2016) observed that strong backing from clinical staff and involvement
among professionals (clinicians and nurses) is imperative for the adoption and implementation of
the integrated medical system.Healthcare service providers should monitor healthcare quality on
a regular basis and accordingly initiate continuous quality improvement programs,such as ERP.
Researchers interested in evaluating the ERP system’s success in a healthcare setting can utilize the
proposed model.
The novelty and value of this paper lie in a new classification of benefits and criticalities
concerning enterprise resource planning implementation in public healthcare.Previous studies
(Al-Mashari et al. 2003; Razi and Tarn 2015; Lim and Loosemore 2017) mostly focused on the technical
aspects of the ERP system, and usually did not differentiate between the public and private sector.
This research contributes to knowledge by revealing the fact that a well-applied ERP system in a
public organization will produce a better output to the system, and also assist medical professionals in
providing better service quality in the healthcare sector. Five healthcare public sector organizations
were part of this study. The paper also contributes to healthcare practice by developing a conceptual
framework that provides policy-makers with a practical understanding of factors that affect healthcare
service quality.The impact dimensions of system quality impact,individual impact,information
quality impact, and organizational impact and their relation to service quality in healthcare have been
presented. The results show that public healthcare institutions are also receiving many benefits after
the adoption of ERP. Operational benefits were mentioned by all the institutes involved.The most
important benefits were report generation,quick access to critical information,a better product,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
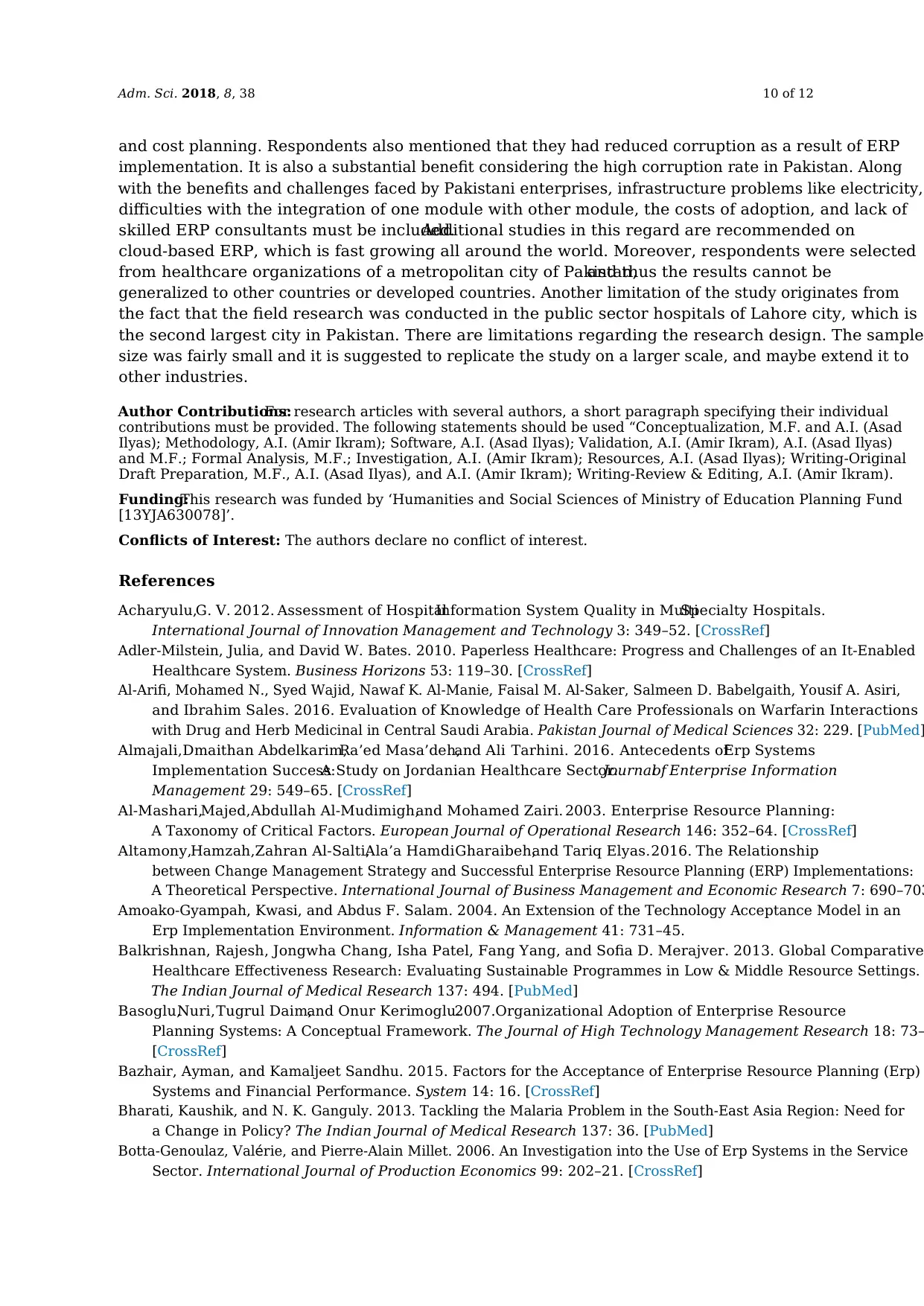
Adm. Sci. 2018, 8, 38 10 of 12
and cost planning. Respondents also mentioned that they had reduced corruption as a result of ERP
implementation. It is also a substantial benefit considering the high corruption rate in Pakistan. Along
with the benefits and challenges faced by Pakistani enterprises, infrastructure problems like electricity,
difficulties with the integration of one module with other module, the costs of adoption, and lack of
skilled ERP consultants must be included.Additional studies in this regard are recommended on
cloud-based ERP, which is fast growing all around the world. Moreover, respondents were selected
from healthcare organizations of a metropolitan city of Pakistan,and thus the results cannot be
generalized to other countries or developed countries. Another limitation of the study originates from
the fact that the field research was conducted in the public sector hospitals of Lahore city, which is
the second largest city in Pakistan. There are limitations regarding the research design. The sample
size was fairly small and it is suggested to replicate the study on a larger scale, and maybe extend it to
other industries.
Author Contributions:For research articles with several authors, a short paragraph specifying their individual
contributions must be provided. The following statements should be used “Conceptualization, M.F. and A.I. (Asad
Ilyas); Methodology, A.I. (Amir Ikram); Software, A.I. (Asad Ilyas); Validation, A.I. (Amir Ikram), A.I. (Asad Ilyas)
and M.F.; Formal Analysis, M.F.; Investigation, A.I. (Amir Ikram); Resources, A.I. (Asad Ilyas); Writing-Original
Draft Preparation, M.F., A.I. (Asad Ilyas), and A.I. (Amir Ikram); Writing-Review & Editing, A.I. (Amir Ikram).
Funding:This research was funded by ‘Humanities and Social Sciences of Ministry of Education Planning Fund
[13YJA630078]’.
Conflicts of Interest: The authors declare no conflict of interest.
References
Acharyulu,G. V. 2012. Assessment of HospitalInformation System Quality in MultiSpecialty Hospitals.
International Journal of Innovation Management and Technology 3: 349–52. [CrossRef]
Adler-Milstein, Julia, and David W. Bates. 2010. Paperless Healthcare: Progress and Challenges of an It-Enabled
Healthcare System. Business Horizons 53: 119–30. [CrossRef]
Al-Arifi, Mohamed N., Syed Wajid, Nawaf K. Al-Manie, Faisal M. Al-Saker, Salmeen D. Babelgaith, Yousif A. Asiri,
and Ibrahim Sales. 2016. Evaluation of Knowledge of Health Care Professionals on Warfarin Interactions
with Drug and Herb Medicinal in Central Saudi Arabia. Pakistan Journal of Medical Sciences 32: 229. [PubMed]
Almajali,Dmaithan Abdelkarim,Ra’ed Masa’deh,and Ali Tarhini. 2016. Antecedents ofErp Systems
Implementation Success:A Study on Jordanian Healthcare Sector.Journalof Enterprise Information
Management 29: 549–65. [CrossRef]
Al-Mashari,Majed,Abdullah Al-Mudimigh,and Mohamed Zairi. 2003. Enterprise Resource Planning:
A Taxonomy of Critical Factors. European Journal of Operational Research 146: 352–64. [CrossRef]
Altamony,Hamzah,Zahran Al-Salti,Ala’a HamdiGharaibeh,and Tariq Elyas.2016. The Relationship
between Change Management Strategy and Successful Enterprise Resource Planning (ERP) Implementations:
A Theoretical Perspective. International Journal of Business Management and Economic Research 7: 690–703
Amoako-Gyampah, Kwasi, and Abdus F. Salam. 2004. An Extension of the Technology Acceptance Model in an
Erp Implementation Environment. Information & Management 41: 731–45.
Balkrishnan, Rajesh, Jongwha Chang, Isha Patel, Fang Yang, and Sofia D. Merajver. 2013. Global Comparative
Healthcare Effectiveness Research: Evaluating Sustainable Programmes in Low & Middle Resource Settings.
The Indian Journal of Medical Research 137: 494. [PubMed]
Basoglu,Nuri,Tugrul Daim,and Onur Kerimoglu.2007.Organizational Adoption of Enterprise Resource
Planning Systems: A Conceptual Framework. The Journal of High Technology Management Research 18: 73–
[CrossRef]
Bazhair, Ayman, and Kamaljeet Sandhu. 2015. Factors for the Acceptance of Enterprise Resource Planning (Erp)
Systems and Financial Performance. System 14: 16. [CrossRef]
Bharati, Kaushik, and N. K. Ganguly. 2013. Tackling the Malaria Problem in the South-East Asia Region: Need for
a Change in Policy? The Indian Journal of Medical Research 137: 36. [PubMed]
Botta-Genoulaz, Valérie, and Pierre-Alain Millet. 2006. An Investigation into the Use of Erp Systems in the Service
Sector. International Journal of Production Economics 99: 202–21. [CrossRef]
and cost planning. Respondents also mentioned that they had reduced corruption as a result of ERP
implementation. It is also a substantial benefit considering the high corruption rate in Pakistan. Along
with the benefits and challenges faced by Pakistani enterprises, infrastructure problems like electricity,
difficulties with the integration of one module with other module, the costs of adoption, and lack of
skilled ERP consultants must be included.Additional studies in this regard are recommended on
cloud-based ERP, which is fast growing all around the world. Moreover, respondents were selected
from healthcare organizations of a metropolitan city of Pakistan,and thus the results cannot be
generalized to other countries or developed countries. Another limitation of the study originates from
the fact that the field research was conducted in the public sector hospitals of Lahore city, which is
the second largest city in Pakistan. There are limitations regarding the research design. The sample
size was fairly small and it is suggested to replicate the study on a larger scale, and maybe extend it to
other industries.
Author Contributions:For research articles with several authors, a short paragraph specifying their individual
contributions must be provided. The following statements should be used “Conceptualization, M.F. and A.I. (Asad
Ilyas); Methodology, A.I. (Amir Ikram); Software, A.I. (Asad Ilyas); Validation, A.I. (Amir Ikram), A.I. (Asad Ilyas)
and M.F.; Formal Analysis, M.F.; Investigation, A.I. (Amir Ikram); Resources, A.I. (Asad Ilyas); Writing-Original
Draft Preparation, M.F., A.I. (Asad Ilyas), and A.I. (Amir Ikram); Writing-Review & Editing, A.I. (Amir Ikram).
Funding:This research was funded by ‘Humanities and Social Sciences of Ministry of Education Planning Fund
[13YJA630078]’.
Conflicts of Interest: The authors declare no conflict of interest.
References
Acharyulu,G. V. 2012. Assessment of HospitalInformation System Quality in MultiSpecialty Hospitals.
International Journal of Innovation Management and Technology 3: 349–52. [CrossRef]
Adler-Milstein, Julia, and David W. Bates. 2010. Paperless Healthcare: Progress and Challenges of an It-Enabled
Healthcare System. Business Horizons 53: 119–30. [CrossRef]
Al-Arifi, Mohamed N., Syed Wajid, Nawaf K. Al-Manie, Faisal M. Al-Saker, Salmeen D. Babelgaith, Yousif A. Asiri,
and Ibrahim Sales. 2016. Evaluation of Knowledge of Health Care Professionals on Warfarin Interactions
with Drug and Herb Medicinal in Central Saudi Arabia. Pakistan Journal of Medical Sciences 32: 229. [PubMed]
Almajali,Dmaithan Abdelkarim,Ra’ed Masa’deh,and Ali Tarhini. 2016. Antecedents ofErp Systems
Implementation Success:A Study on Jordanian Healthcare Sector.Journalof Enterprise Information
Management 29: 549–65. [CrossRef]
Al-Mashari,Majed,Abdullah Al-Mudimigh,and Mohamed Zairi. 2003. Enterprise Resource Planning:
A Taxonomy of Critical Factors. European Journal of Operational Research 146: 352–64. [CrossRef]
Altamony,Hamzah,Zahran Al-Salti,Ala’a HamdiGharaibeh,and Tariq Elyas.2016. The Relationship
between Change Management Strategy and Successful Enterprise Resource Planning (ERP) Implementations:
A Theoretical Perspective. International Journal of Business Management and Economic Research 7: 690–703
Amoako-Gyampah, Kwasi, and Abdus F. Salam. 2004. An Extension of the Technology Acceptance Model in an
Erp Implementation Environment. Information & Management 41: 731–45.
Balkrishnan, Rajesh, Jongwha Chang, Isha Patel, Fang Yang, and Sofia D. Merajver. 2013. Global Comparative
Healthcare Effectiveness Research: Evaluating Sustainable Programmes in Low & Middle Resource Settings.
The Indian Journal of Medical Research 137: 494. [PubMed]
Basoglu,Nuri,Tugrul Daim,and Onur Kerimoglu.2007.Organizational Adoption of Enterprise Resource
Planning Systems: A Conceptual Framework. The Journal of High Technology Management Research 18: 73–
[CrossRef]
Bazhair, Ayman, and Kamaljeet Sandhu. 2015. Factors for the Acceptance of Enterprise Resource Planning (Erp)
Systems and Financial Performance. System 14: 16. [CrossRef]
Bharati, Kaushik, and N. K. Ganguly. 2013. Tackling the Malaria Problem in the South-East Asia Region: Need for
a Change in Policy? The Indian Journal of Medical Research 137: 36. [PubMed]
Botta-Genoulaz, Valérie, and Pierre-Alain Millet. 2006. An Investigation into the Use of Erp Systems in the Service
Sector. International Journal of Production Economics 99: 202–21. [CrossRef]
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Adm. Sci. 2018, 8, 38 11 of 12
Carmines, E. G., and J. P. McIver.1981.Analyzing Models with Unobserved Variables.In Social Measurement:
Current Issues. Edited by G. W. Bohrnstedt and E. F. Borgatta. Beverly Hills: Sage Publications.
Chiarini, Andrea, Emidia Vagnoni, and Luca Chiarini. 2018. Erp Implementation in Public Healthcare, Achievable
Benefits and Encountered Criticalities-an Investigation from Italy.InternationalJournalof Services and
Operations Management 29: 1–17. [CrossRef]
Costa,RaquelMouta Faria da. 2015. New Service Developmentat the MultinationalLevel. Doctoral
dissertation.Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=
1&ved=0ahUKEwiR7JbwkYXcAhXSOSwKHeURBg0QFggxMAA&url=https%3A%2F%2Frepositorio.ucp.
pt%2Fbitstream%2F10400.14%2F19295%2F1%2FRaquel%2520Costa%2520-%2520Gest%25C3%25A3o%
2520Servi%25C3%25A7os%2520-%2520TFM.pdf&usg=AOvVaw3gKEyUXghbUVG8XFUv9iR3 (accessed
on 4 July 2018).
Cucciniello,Maria,Irvine Lapsley,and Greta Nasi. 2016. Managing Health Care in the DigitalWorld:
A Comparative Analysis. Health Services Management Research 29: 132–42. [CrossRef]
Delone, William H, and Ephraim R. McLean. 2003. The Delone and Mclean Model of Information Systems Success:
A Ten-Year Update. Journal of Management Information Systems 19: 9–30.
Du, Tao. 2017. Performance Measurement of Healthcare Service and Association Discussion between Quality and
Efficiency: Evidence from 31 Provinces of Mainland China. Sustainability 10: 74. [CrossRef]
Field, Andy. 2013. Discovering Statistics Using Ibm Spss Statistics. Newcastle-upon-Tyne: Sage.
Gable,Guy G, Darshana Sedera,and Taizan Chan.2008.Re-Conceptualizing Information System Success:
The Is-Impact Measurement Model. Journal of the Association for Information Systems 9: 377. [CrossRef]
Gorla, Narasimhaiah, Toni M Somers, and Betty Wong. 2010. Organizational Impact of System Quality, Information
Quality, and Service Quality. The Journal of Strategic Information Systems 19: 207–28. [CrossRef]
Hong,Paul,David Dobrzykowski,Young Won Park,Hassan R HassabElnaby,Woosang Hwang,and Mark
A Vonderembse.2012. The Impact of Erp Implementation on OrganizationalCapabilities and Firm
Performance. Benchmarking: An International Journal 19: 618–33.
Hung, Shin-Yuan, Charlie Chen, and Kuan-Hsiuang Wang. 2014. Critical Success Factors for the Implementation
of Integrated Healthcare Information Systems Projects: An Organizational Fit Perspective. Communications of
the Association for Information Systems 34: 39.
Jawaid, Shaukat Ali. 2016. Prevention and Intervention Strategies to Check Increasing Violence against Healthcare
Facilities and Healthcare Professionals. Pakistan Journal of Medical Sciences 32: 1. [CrossRef] [PubMed]
Kanellou, Alexandra, and Charalambos Spathis. 2013. Accounting Benefits and Satisfaction in an Erp Environment.
International Journal of Accounting Information Systems 14: 209–34. [CrossRef]
Karimi, Jahangir, Toni M. Somers, and Anol Bhattacherjee.2007.The Role of Information Systems Resources
in Erp Capability Building and Business Process Outcomes. Journal of Management Information Systems 2
221–60. [CrossRef]
Kline, Rex B. 2015. Principles and Practice of Structural Equation Modeling. New York: Guilford Publications.
Kumar, Vinod, Bharat Maheshwari, and Uma Kumar. 2003. An Investigation of Critical Management Issues in Erp
Implementation: Emperical Evidence from Canadian Organizations. Technovation 23: 793–807. [CrossRef]
Lee, Hanjoon, Linda M. Delene, Mary Anne Bunda, and Chankon Kim. 2000. Methods of Measuring Health-Care
Service Quality. Journal of Business Research 48: 233–46. [CrossRef]
Lim, Benson T.H., and Martin Loosemore.2017.The effect of inter-organizationaljustice perceptions on
organizational citizenship behaviors in construction projects. International Journal of Project Management 35
95–106. [CrossRef]
Lim, Eric T. K., Shan Ling Pan, and Chee Wee Tan. 2005. Managing User Acceptance Towards Enterprise Resource
Planning (Erp) Systems–Understanding the Dissonance between User Expectations and Managerial Policies.
European Journal of Information Systems 14: 135–49. [CrossRef]
MacLennan,Elzavita,and Jean-PaulVan Belle. 2014. Factors Affecting the OrganizationalAdoption of
Service-Oriented Architecture (SOA). Information Systems and e-Business Management 12: 71–100. [CrossRe
Menon, Nirup, Byungtae Lee, and Leslie Eldenberg.1996.Information Technology Productivity in the Health
Care Industry. In ICIS 1996 Proceedings. vol. 56. Available online: https://www.google.com/url?sa=t&rct=
j&q=&esrc=s&source=web&cd=1&ved=0ahUKEwjutNe1koXcAhUKFSwKHRsRA8sQFggoMAA&url=
https%3A%2F%2Fpdfs.semanticscholar.org%2F4d97%2Fc684cf2d337d60416b6304e1ece2dcd5c917.pdf&
usg=AOvVaw3qZP0jnLu9mV83tXXHlvsN (accessed on 4 July 2018).
Carmines, E. G., and J. P. McIver.1981.Analyzing Models with Unobserved Variables.In Social Measurement:
Current Issues. Edited by G. W. Bohrnstedt and E. F. Borgatta. Beverly Hills: Sage Publications.
Chiarini, Andrea, Emidia Vagnoni, and Luca Chiarini. 2018. Erp Implementation in Public Healthcare, Achievable
Benefits and Encountered Criticalities-an Investigation from Italy.InternationalJournalof Services and
Operations Management 29: 1–17. [CrossRef]
Costa,RaquelMouta Faria da. 2015. New Service Developmentat the MultinationalLevel. Doctoral
dissertation.Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=
1&ved=0ahUKEwiR7JbwkYXcAhXSOSwKHeURBg0QFggxMAA&url=https%3A%2F%2Frepositorio.ucp.
pt%2Fbitstream%2F10400.14%2F19295%2F1%2FRaquel%2520Costa%2520-%2520Gest%25C3%25A3o%
2520Servi%25C3%25A7os%2520-%2520TFM.pdf&usg=AOvVaw3gKEyUXghbUVG8XFUv9iR3 (accessed
on 4 July 2018).
Cucciniello,Maria,Irvine Lapsley,and Greta Nasi. 2016. Managing Health Care in the DigitalWorld:
A Comparative Analysis. Health Services Management Research 29: 132–42. [CrossRef]
Delone, William H, and Ephraim R. McLean. 2003. The Delone and Mclean Model of Information Systems Success:
A Ten-Year Update. Journal of Management Information Systems 19: 9–30.
Du, Tao. 2017. Performance Measurement of Healthcare Service and Association Discussion between Quality and
Efficiency: Evidence from 31 Provinces of Mainland China. Sustainability 10: 74. [CrossRef]
Field, Andy. 2013. Discovering Statistics Using Ibm Spss Statistics. Newcastle-upon-Tyne: Sage.
Gable,Guy G, Darshana Sedera,and Taizan Chan.2008.Re-Conceptualizing Information System Success:
The Is-Impact Measurement Model. Journal of the Association for Information Systems 9: 377. [CrossRef]
Gorla, Narasimhaiah, Toni M Somers, and Betty Wong. 2010. Organizational Impact of System Quality, Information
Quality, and Service Quality. The Journal of Strategic Information Systems 19: 207–28. [CrossRef]
Hong,Paul,David Dobrzykowski,Young Won Park,Hassan R HassabElnaby,Woosang Hwang,and Mark
A Vonderembse.2012. The Impact of Erp Implementation on OrganizationalCapabilities and Firm
Performance. Benchmarking: An International Journal 19: 618–33.
Hung, Shin-Yuan, Charlie Chen, and Kuan-Hsiuang Wang. 2014. Critical Success Factors for the Implementation
of Integrated Healthcare Information Systems Projects: An Organizational Fit Perspective. Communications of
the Association for Information Systems 34: 39.
Jawaid, Shaukat Ali. 2016. Prevention and Intervention Strategies to Check Increasing Violence against Healthcare
Facilities and Healthcare Professionals. Pakistan Journal of Medical Sciences 32: 1. [CrossRef] [PubMed]
Kanellou, Alexandra, and Charalambos Spathis. 2013. Accounting Benefits and Satisfaction in an Erp Environment.
International Journal of Accounting Information Systems 14: 209–34. [CrossRef]
Karimi, Jahangir, Toni M. Somers, and Anol Bhattacherjee.2007.The Role of Information Systems Resources
in Erp Capability Building and Business Process Outcomes. Journal of Management Information Systems 2
221–60. [CrossRef]
Kline, Rex B. 2015. Principles and Practice of Structural Equation Modeling. New York: Guilford Publications.
Kumar, Vinod, Bharat Maheshwari, and Uma Kumar. 2003. An Investigation of Critical Management Issues in Erp
Implementation: Emperical Evidence from Canadian Organizations. Technovation 23: 793–807. [CrossRef]
Lee, Hanjoon, Linda M. Delene, Mary Anne Bunda, and Chankon Kim. 2000. Methods of Measuring Health-Care
Service Quality. Journal of Business Research 48: 233–46. [CrossRef]
Lim, Benson T.H., and Martin Loosemore.2017.The effect of inter-organizationaljustice perceptions on
organizational citizenship behaviors in construction projects. International Journal of Project Management 35
95–106. [CrossRef]
Lim, Eric T. K., Shan Ling Pan, and Chee Wee Tan. 2005. Managing User Acceptance Towards Enterprise Resource
Planning (Erp) Systems–Understanding the Dissonance between User Expectations and Managerial Policies.
European Journal of Information Systems 14: 135–49. [CrossRef]
MacLennan,Elzavita,and Jean-PaulVan Belle. 2014. Factors Affecting the OrganizationalAdoption of
Service-Oriented Architecture (SOA). Information Systems and e-Business Management 12: 71–100. [CrossRe
Menon, Nirup, Byungtae Lee, and Leslie Eldenberg.1996.Information Technology Productivity in the Health
Care Industry. In ICIS 1996 Proceedings. vol. 56. Available online: https://www.google.com/url?sa=t&rct=
j&q=&esrc=s&source=web&cd=1&ved=0ahUKEwjutNe1koXcAhUKFSwKHRsRA8sQFggoMAA&url=
https%3A%2F%2Fpdfs.semanticscholar.org%2F4d97%2Fc684cf2d337d60416b6304e1ece2dcd5c917.pdf&
usg=AOvVaw3qZP0jnLu9mV83tXXHlvsN (accessed on 4 July 2018).
Adm. Sci. 2018, 8, 38 12 of 12
Mosadeghrad, Ali Mohammad. 2014. Factors Influencing Healthcare Service Quality. International Journal of Health
Policy and Management 3: 77. [CrossRef] [PubMed]
Murtagh, Fionn, and André Heck. 2012. Multivariate Data Analysis. Cham: Springer Science & Business Media
vol. 131.
Parr, Anne, and Graeme Shanks. 2000. A Model of Erp Project Implementation. Journal of information Technology
15: 289–303. [CrossRef]
Rai, Arun, Ravi Patnayakuni, and Nainika Seth.2006.Firm Performance Impacts of Digitally Enabled Supply
Chain Integration Capabilities. MIS Quarterly, 225–46. [CrossRef]
Razi,Muhammad A.,and J.Michael Tarn.2015.ERP System Solutions for Small Companies:Readiness &
Selection. Journal of Small Business Strategy 14: 71–85.
Revelle, William. 2014. Psychology 371: Personality Research PsychometricTheory. Available
online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=3&ved=
0ahUKEwiUkq76koXcAhWJhiwKHcwXALsQFgg4MAI&url=http%3A%2F%2Fciteseerx.ist.psu.
edu%2Fviewdoc%2Fdownload%3Fdoi%3D10.1.1.587.963%26rep%3Drep1%26type%3Dpdf&usg=
AOvVaw0cuoheaQH3qdHeSEWW4xeT (accessed on 4 July 2018).
Rouhani, Saeed, and Mobin Mehri. 2018. Empowering Benefits of Erp Systems Implementation: Empirical Study
of Industrial Firms. Journal of Systems and Information Technology 12: 54–72. [CrossRef]
Roussel, Linda A., Russell C. Swansburg, and Richard J. Swansburg. 2006. Management and Leadership for Nur
Administrators. Burlington: Jones & Bartlett Learning.
Scotti, Dennis J., Joel Harmon, Scott J. Behson, and Daniel J. Messina. 2007. Links among High-Performance Work
Environment, Service Quality, and Customer Satisfaction: An Extension to the Healthcare Sector/Practitioner
Application. Journal of Healthcare Management 52: 109. [CrossRef] [PubMed]
Shaul, Levi, and Doron Tauber. 2013. Critical Success Factors in Enterprise Resource Planning Systems: Review of
the Last Decade. ACM Computing Surveys (CSUR) 45: 55. [CrossRef]
Shih, Ya-Yueh, and Siao-Sian Huang. 2009. The Actual Usage of Erp Systems: An Extended Technology Acceptance
Perspective. Journal of Research and Practice in Information Technology 41: 263.
Singla, Ashim Raj.2008.Impact of ERP Systems on Small and Mid Sized Public Sector Enterprises.Journal of
Theoretical and Applied Information Technology 4: 119–31.
Somers, Toni M., and Klara Nelson. 2001. The Impact of Critical Success Factors across the Stages of Enterprise
Resource Planning Implementations. Paper presented at the 34th Annual Hawaii International Conference
on System Sciences, Maui, HI, USA, January 6.
Tasevska, Frosina, Talib Damij, and Nadja Damij. 2014. Project Planning Practices Based on Enterprise Resource
Planning Systems in Small and Medium Enterprises—A Case Study from the Republic of Macedonia.
International Journal of Project Management 32: 529–39. [CrossRef]
Umble, Elisabeth J., Ronald R. Haft, and M. Michael Umble. 2003. Enterprise Resource Planning: Implementation
Procedures and Critical Success Factors. European Journal of Operational Research 146: 241–57. [CrossRef]
Wallace, Thomas F., and Michael H. Kremzar. 2002. Erp: Making It Happen: The Implementers’ Guide to Success
Enterprise Resource Planning. Hoboken: John Wiley & Sons, vol. 14.
Ward, John, and Joe Peppard.2016.The Strategic Management of Information Systems:Building a Digital Strategy.
Hoboken: John Wiley & Sons.
Xue, Yajiong, Huigang Liang, William R. Boulton, and Charles A. Snyder.2005.Erp Implementation Failures
in China: Case Studies with Implications for Erp Vendors. International Journal of Production Economics 9
279–95. [CrossRef]
©2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access
article distributed under the terms and conditions of the Creative Commons Attribution
(CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Mosadeghrad, Ali Mohammad. 2014. Factors Influencing Healthcare Service Quality. International Journal of Health
Policy and Management 3: 77. [CrossRef] [PubMed]
Murtagh, Fionn, and André Heck. 2012. Multivariate Data Analysis. Cham: Springer Science & Business Media
vol. 131.
Parr, Anne, and Graeme Shanks. 2000. A Model of Erp Project Implementation. Journal of information Technology
15: 289–303. [CrossRef]
Rai, Arun, Ravi Patnayakuni, and Nainika Seth.2006.Firm Performance Impacts of Digitally Enabled Supply
Chain Integration Capabilities. MIS Quarterly, 225–46. [CrossRef]
Razi,Muhammad A.,and J.Michael Tarn.2015.ERP System Solutions for Small Companies:Readiness &
Selection. Journal of Small Business Strategy 14: 71–85.
Revelle, William. 2014. Psychology 371: Personality Research PsychometricTheory. Available
online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=3&ved=
0ahUKEwiUkq76koXcAhWJhiwKHcwXALsQFgg4MAI&url=http%3A%2F%2Fciteseerx.ist.psu.
edu%2Fviewdoc%2Fdownload%3Fdoi%3D10.1.1.587.963%26rep%3Drep1%26type%3Dpdf&usg=
AOvVaw0cuoheaQH3qdHeSEWW4xeT (accessed on 4 July 2018).
Rouhani, Saeed, and Mobin Mehri. 2018. Empowering Benefits of Erp Systems Implementation: Empirical Study
of Industrial Firms. Journal of Systems and Information Technology 12: 54–72. [CrossRef]
Roussel, Linda A., Russell C. Swansburg, and Richard J. Swansburg. 2006. Management and Leadership for Nur
Administrators. Burlington: Jones & Bartlett Learning.
Scotti, Dennis J., Joel Harmon, Scott J. Behson, and Daniel J. Messina. 2007. Links among High-Performance Work
Environment, Service Quality, and Customer Satisfaction: An Extension to the Healthcare Sector/Practitioner
Application. Journal of Healthcare Management 52: 109. [CrossRef] [PubMed]
Shaul, Levi, and Doron Tauber. 2013. Critical Success Factors in Enterprise Resource Planning Systems: Review of
the Last Decade. ACM Computing Surveys (CSUR) 45: 55. [CrossRef]
Shih, Ya-Yueh, and Siao-Sian Huang. 2009. The Actual Usage of Erp Systems: An Extended Technology Acceptance
Perspective. Journal of Research and Practice in Information Technology 41: 263.
Singla, Ashim Raj.2008.Impact of ERP Systems on Small and Mid Sized Public Sector Enterprises.Journal of
Theoretical and Applied Information Technology 4: 119–31.
Somers, Toni M., and Klara Nelson. 2001. The Impact of Critical Success Factors across the Stages of Enterprise
Resource Planning Implementations. Paper presented at the 34th Annual Hawaii International Conference
on System Sciences, Maui, HI, USA, January 6.
Tasevska, Frosina, Talib Damij, and Nadja Damij. 2014. Project Planning Practices Based on Enterprise Resource
Planning Systems in Small and Medium Enterprises—A Case Study from the Republic of Macedonia.
International Journal of Project Management 32: 529–39. [CrossRef]
Umble, Elisabeth J., Ronald R. Haft, and M. Michael Umble. 2003. Enterprise Resource Planning: Implementation
Procedures and Critical Success Factors. European Journal of Operational Research 146: 241–57. [CrossRef]
Wallace, Thomas F., and Michael H. Kremzar. 2002. Erp: Making It Happen: The Implementers’ Guide to Success
Enterprise Resource Planning. Hoboken: John Wiley & Sons, vol. 14.
Ward, John, and Joe Peppard.2016.The Strategic Management of Information Systems:Building a Digital Strategy.
Hoboken: John Wiley & Sons.
Xue, Yajiong, Huigang Liang, William R. Boulton, and Charles A. Snyder.2005.Erp Implementation Failures
in China: Case Studies with Implications for Erp Vendors. International Journal of Production Economics 9
279–95. [CrossRef]
©2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access
article distributed under the terms and conditions of the Creative Commons Attribution
(CC BY) license (http://creativecommons.org/licenses/by/4.0/).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





