HSN734: Report on Overweight and Obesity in Australia
VerifiedAdded on 2022/09/16
|9
|2116
|13
Report
AI Summary
This report provides a comprehensive overview of the epidemiology of overweight and obesity in Australia. It begins by establishing the prevalence of overweight and obesity among both children and adults, highlighting the concerning trends and statistics from the ABS. The report then delves into the demographics of those affected, including a specific focus on Indigenous populations, and their higher likelihood of being obese or overweight. The report examines the health consequences of obesity, including its association with chronic diseases and mortality, particularly among Indigenous Australians. It explores factors contributing to obesity, such as energy imbalance, lack of physical activity, and socio-economic determinants. The report also discusses various strategies and initiatives, including national plans, community engagement programs, and policy interventions, aimed at addressing and preventing overweight and obesity within the Australian population, with a particular focus on community-based approaches and the involvement of organizations like WHO. The report concludes by emphasizing the need for comprehensive, integrated approaches involving various sectors to effectively manage and reduce obesity levels across all population groups, with special attention given to Indigenous communities.
Surname 1
Name
Professor
Institution
Course
THE EPIDEMIOLOGY OF OVERWEIGHT AND OBESITY IN AUSTRALIA
Overweight and obesity make a significant public health problem in Australia. The latter is
caused by a sustained imbalance when there is higher energy intake from drinking than the
energy utilized in physical activity. Energy imbalance is predisposed by the organic and genetic
features of a person and also by the lifestyle factors. The discussion below will show different
information that will be used to create an image of overweight and obesity in Australia.
Research from ABS shows that in Australia, 1 out of every four children aged from 5-15
is overweight or obese. 20% of these children are either overweight or obese while for the
Name
Professor
Institution
Course
THE EPIDEMIOLOGY OF OVERWEIGHT AND OBESITY IN AUSTRALIA
Overweight and obesity make a significant public health problem in Australia. The latter is
caused by a sustained imbalance when there is higher energy intake from drinking than the
energy utilized in physical activity. Energy imbalance is predisposed by the organic and genetic
features of a person and also by the lifestyle factors. The discussion below will show different
information that will be used to create an image of overweight and obesity in Australia.
Research from ABS shows that in Australia, 1 out of every four children aged from 5-15
is overweight or obese. 20% of these children are either overweight or obese while for the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Surname 2
children aged 2-4 and 5-15, the proportions are similar. The pervasiveness of overweight and
obesity for children aged 5-15 rose from 21% in 1995 to 25% in 2008 while the statistics
remained stable as of 2014. In 2015, 63% of the total Australian population was obese and
overweight (1). The prevalence of adverse obesity amid Australian adults has increased from 5%
in 1995 to 9% in 2015. Research shows that 71% of Australian men were obese equated to 56%
of the women.42% of men's and 29% of women's population were obese but not overweight (1).
The indigenous people have a high probability of being obese as compared to non-indigenous.
The people living outside major cities and in lower socio-economic groups are more likely to be
obese or overweight.
Many aboriginal people have exclusive languages, systems of awareness, and
philosophies. They possess an ancient culture for supportable administration of the natural assets
and have a certain relation to the utilization of their land (2). Australia's native people have two
unique cultural groups comprising the Aboriginal and Torres Strait Islander persons. The
aboriginal people have distinct groups like Murri, Koori, or Nunga, and they identify themselves
with where they originate. For instance, the Gunditjatmara community is the guardian of the
western victoria, while Yawuru people are the guardians of Western Australia (2).
The Torres Islander people are approximately 800,000. The age structure of the Torres
Strait Islander is composed of young population. The median age for indigenous Australian is 22
years while that of non-Indigenous Australian (3). National statistics released in 2016 showed
that 36% of the indigenous Australians were between 0-14 years while the non-indigenous make
only 18%. The Torres Islander persons are unique in that they are of Melanesian origin and have
various identities, histories, and cultural traditions. Cases of overweight and obesity are shared
among the Torres Strait Islander aged 15 years (61%) and above when compared to the
children aged 2-4 and 5-15, the proportions are similar. The pervasiveness of overweight and
obesity for children aged 5-15 rose from 21% in 1995 to 25% in 2008 while the statistics
remained stable as of 2014. In 2015, 63% of the total Australian population was obese and
overweight (1). The prevalence of adverse obesity amid Australian adults has increased from 5%
in 1995 to 9% in 2015. Research shows that 71% of Australian men were obese equated to 56%
of the women.42% of men's and 29% of women's population were obese but not overweight (1).
The indigenous people have a high probability of being obese as compared to non-indigenous.
The people living outside major cities and in lower socio-economic groups are more likely to be
obese or overweight.
Many aboriginal people have exclusive languages, systems of awareness, and
philosophies. They possess an ancient culture for supportable administration of the natural assets
and have a certain relation to the utilization of their land (2). Australia's native people have two
unique cultural groups comprising the Aboriginal and Torres Strait Islander persons. The
aboriginal people have distinct groups like Murri, Koori, or Nunga, and they identify themselves
with where they originate. For instance, the Gunditjatmara community is the guardian of the
western victoria, while Yawuru people are the guardians of Western Australia (2).
The Torres Islander people are approximately 800,000. The age structure of the Torres
Strait Islander is composed of young population. The median age for indigenous Australian is 22
years while that of non-Indigenous Australian (3). National statistics released in 2016 showed
that 36% of the indigenous Australians were between 0-14 years while the non-indigenous make
only 18%. The Torres Islander persons are unique in that they are of Melanesian origin and have
various identities, histories, and cultural traditions. Cases of overweight and obesity are shared
among the Torres Strait Islander aged 15 years (61%) and above when compared to the
Surname 3
Aboriginal individuals. The Aboriginals make about 56% .The levels of obesity and overweight
was high among the Torres Strait Islanders living in the Torres Strait region whereby 86% of the
dwellers had a BMI of 25.0 or even higher than that.
PART 2
Being weighty and obese upsurges the risk of several health disorders. The affliction of
obesity in the aboriginal populace in Australia is approximated to explain the life anticipation
gap. Recent report released by the ABS shows that obesity contributes 16% of the health gap
amid aboriginal and Torres islanders (3). Obesity has an association with the risk features for the
primary origins of mortality among the Torres Strait Islander people. It affects widely via
diabetes and heart diseases. For both the Aboriginals and Torres Strait Islanders, the rate of
obesity and overweight cases increases with age. Obesity is strongly affiliated with chronic
disease biomarkers. Indigenous people are seven times more likely to get obese more than those
of average or underweight(3). Lack of enough physical activity is also a primary factor and
causative agent of obesity and overweight. Childhood is also a vital period whereby the
disparities in health contributing factors such as the socio-economic status emerge. The
aboriginal and Torres Strait Islander young people aged between 2-14 years have a high
probability of being underweight when compared to the non-indigenous young people. The rate
of obesity for the indigenous children is high, with the highest rate being at 10-14 years.
Generally, obesity is associated with other health factors and social factors that determine health.
Prolonged financial stress is a primary factor that leads to obesity and overweight. Low income
is linked with food security challenges and dietary conducts. Incarceration also has a direct
association with weight gain and obesity in the indigenous youth.
Aboriginal individuals. The Aboriginals make about 56% .The levels of obesity and overweight
was high among the Torres Strait Islanders living in the Torres Strait region whereby 86% of the
dwellers had a BMI of 25.0 or even higher than that.
PART 2
Being weighty and obese upsurges the risk of several health disorders. The affliction of
obesity in the aboriginal populace in Australia is approximated to explain the life anticipation
gap. Recent report released by the ABS shows that obesity contributes 16% of the health gap
amid aboriginal and Torres islanders (3). Obesity has an association with the risk features for the
primary origins of mortality among the Torres Strait Islander people. It affects widely via
diabetes and heart diseases. For both the Aboriginals and Torres Strait Islanders, the rate of
obesity and overweight cases increases with age. Obesity is strongly affiliated with chronic
disease biomarkers. Indigenous people are seven times more likely to get obese more than those
of average or underweight(3). Lack of enough physical activity is also a primary factor and
causative agent of obesity and overweight. Childhood is also a vital period whereby the
disparities in health contributing factors such as the socio-economic status emerge. The
aboriginal and Torres Strait Islander young people aged between 2-14 years have a high
probability of being underweight when compared to the non-indigenous young people. The rate
of obesity for the indigenous children is high, with the highest rate being at 10-14 years.
Generally, obesity is associated with other health factors and social factors that determine health.
Prolonged financial stress is a primary factor that leads to obesity and overweight. Low income
is linked with food security challenges and dietary conducts. Incarceration also has a direct
association with weight gain and obesity in the indigenous youth.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

Surname 4
Whereas several factors may affect a person's heath, heaviness and obesity appear
primarily as a result of an imbalance amid the inequality amid energy consumption from the diet
and the expenditure of the energy taken (4). Genetic and environmental factors also play an
essential role in influencing weight. The primary cause of overweight and obesity is the Intake of
energy and its expenditure. The amount of food taken by a person relies on their age, sex, body
mass, and the level of somatic activity. The body converts proteins, carbohydrates, and fats into
energy. The energy in the human body is utilized in basal metabolism, thermic processes, and
physical activity (5). Physical activity is the fundamental variable in the consumption of energy,
and it is the primary component that a person has the power to control.
Improvement of nourishment and the curbing of obesity are substantial in regulating the
primary causes of ill health in the indigenous people. Reducing dietetic energy can lead to weight
loss in the short term basis. However, the reduction of weight in the long term requires attention
to behavioral alteration and regular physical activity (5). A small weight loss can possess
significant health benefits, and hence, it is suitable for persons to set realistic objectives.
Emphasis made by WHO show that obesity is a challenge to the population and also at the
individual level. Effective prevention and management will need an integrated approach which
involves all sectors in the society.
Indigenous particular policies have been devised to offer an outline for the nationwide
action in the improvement of the nourishing status of the Aboriginal and Torres Strait Islander
persons. The NATSINSAP was printed together with ‘Eat Healthy Australia’ and a multiple of
the exploit areas that beleaguered the causal factors that contribute to overweight and obesity in
indigenous and Torres Islander people(6). Several strategies have been put in place for the
Whereas several factors may affect a person's heath, heaviness and obesity appear
primarily as a result of an imbalance amid the inequality amid energy consumption from the diet
and the expenditure of the energy taken (4). Genetic and environmental factors also play an
essential role in influencing weight. The primary cause of overweight and obesity is the Intake of
energy and its expenditure. The amount of food taken by a person relies on their age, sex, body
mass, and the level of somatic activity. The body converts proteins, carbohydrates, and fats into
energy. The energy in the human body is utilized in basal metabolism, thermic processes, and
physical activity (5). Physical activity is the fundamental variable in the consumption of energy,
and it is the primary component that a person has the power to control.
Improvement of nourishment and the curbing of obesity are substantial in regulating the
primary causes of ill health in the indigenous people. Reducing dietetic energy can lead to weight
loss in the short term basis. However, the reduction of weight in the long term requires attention
to behavioral alteration and regular physical activity (5). A small weight loss can possess
significant health benefits, and hence, it is suitable for persons to set realistic objectives.
Emphasis made by WHO show that obesity is a challenge to the population and also at the
individual level. Effective prevention and management will need an integrated approach which
involves all sectors in the society.
Indigenous particular policies have been devised to offer an outline for the nationwide
action in the improvement of the nourishing status of the Aboriginal and Torres Strait Islander
persons. The NATSINSAP was printed together with ‘Eat Healthy Australia’ and a multiple of
the exploit areas that beleaguered the causal factors that contribute to overweight and obesity in
indigenous and Torres Islander people(6). Several strategies have been put in place for the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Surname 5
community stores, food subsidies, and health store guidelines in the aboriginal communities. The
instructions have led to increased consumption of healthy foods.
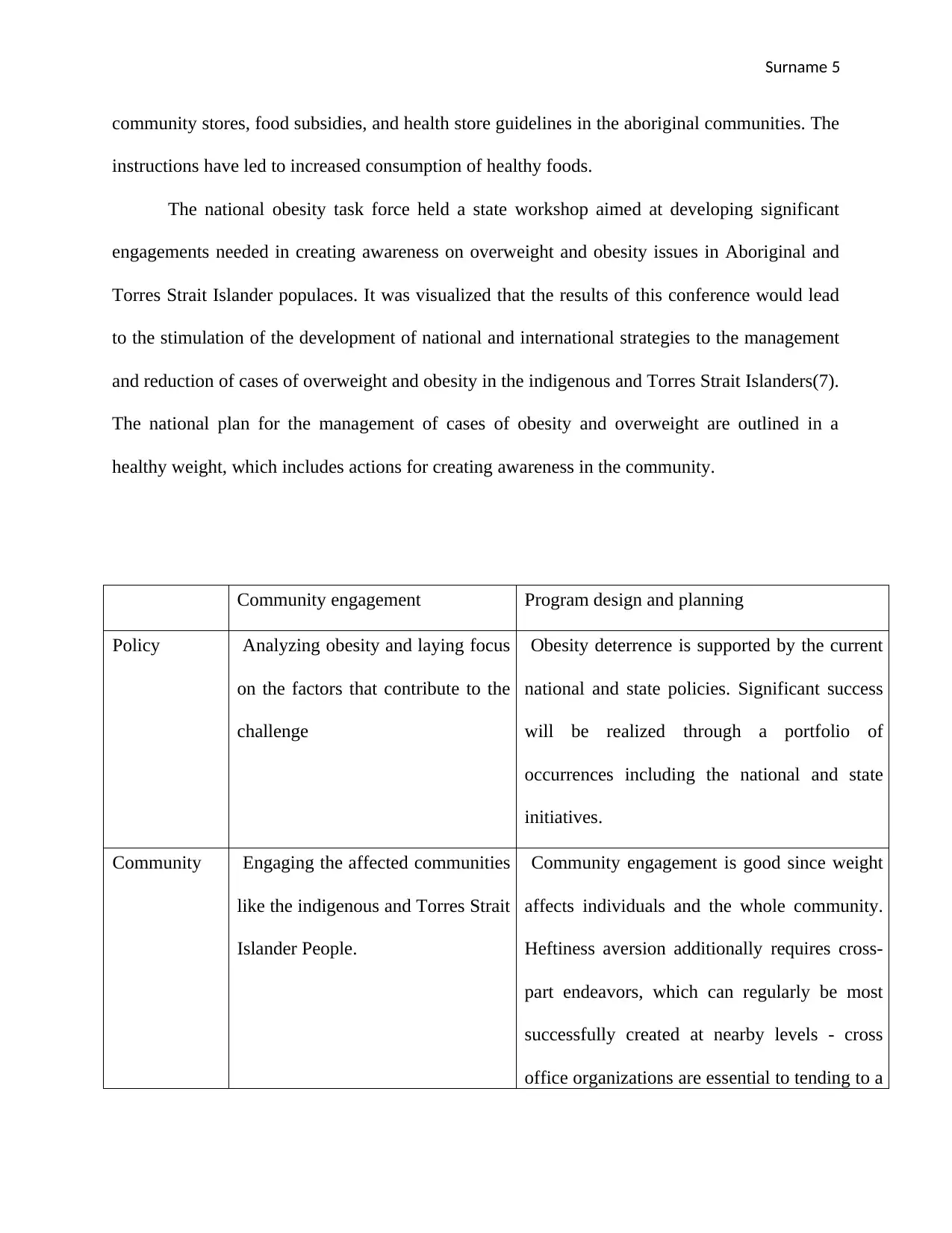
The national obesity task force held a state workshop aimed at developing significant
engagements needed in creating awareness on overweight and obesity issues in Aboriginal and
Torres Strait Islander populaces. It was visualized that the results of this conference would lead
to the stimulation of the development of national and international strategies to the management
and reduction of cases of overweight and obesity in the indigenous and Torres Strait Islanders(7).
The national plan for the management of cases of obesity and overweight are outlined in a
healthy weight, which includes actions for creating awareness in the community.
Community engagement Program design and planning
Policy Analyzing obesity and laying focus
on the factors that contribute to the
challenge
Obesity deterrence is supported by the current
national and state policies. Significant success
will be realized through a portfolio of
occurrences including the national and state
initiatives.
Community Engaging the affected communities
like the indigenous and Torres Strait
Islander People.
Community engagement is good since weight
affects individuals and the whole community.
Heftiness aversion additionally requires cross-
part endeavors, which can regularly be most
successfully created at nearby levels - cross
office organizations are essential to tending to a
community stores, food subsidies, and health store guidelines in the aboriginal communities. The
instructions have led to increased consumption of healthy foods.
The national obesity task force held a state workshop aimed at developing significant
engagements needed in creating awareness on overweight and obesity issues in Aboriginal and
Torres Strait Islander populaces. It was visualized that the results of this conference would lead
to the stimulation of the development of national and international strategies to the management
and reduction of cases of overweight and obesity in the indigenous and Torres Strait Islanders(7).
The national plan for the management of cases of obesity and overweight are outlined in a
healthy weight, which includes actions for creating awareness in the community.
Community engagement Program design and planning
Policy Analyzing obesity and laying focus
on the factors that contribute to the
challenge
Obesity deterrence is supported by the current
national and state policies. Significant success
will be realized through a portfolio of
occurrences including the national and state
initiatives.
Community Engaging the affected communities
like the indigenous and Torres Strait
Islander People.
Community engagement is good since weight
affects individuals and the whole community.
Heftiness aversion additionally requires cross-
part endeavors, which can regularly be most
successfully created at nearby levels - cross
office organizations are essential to tending to a
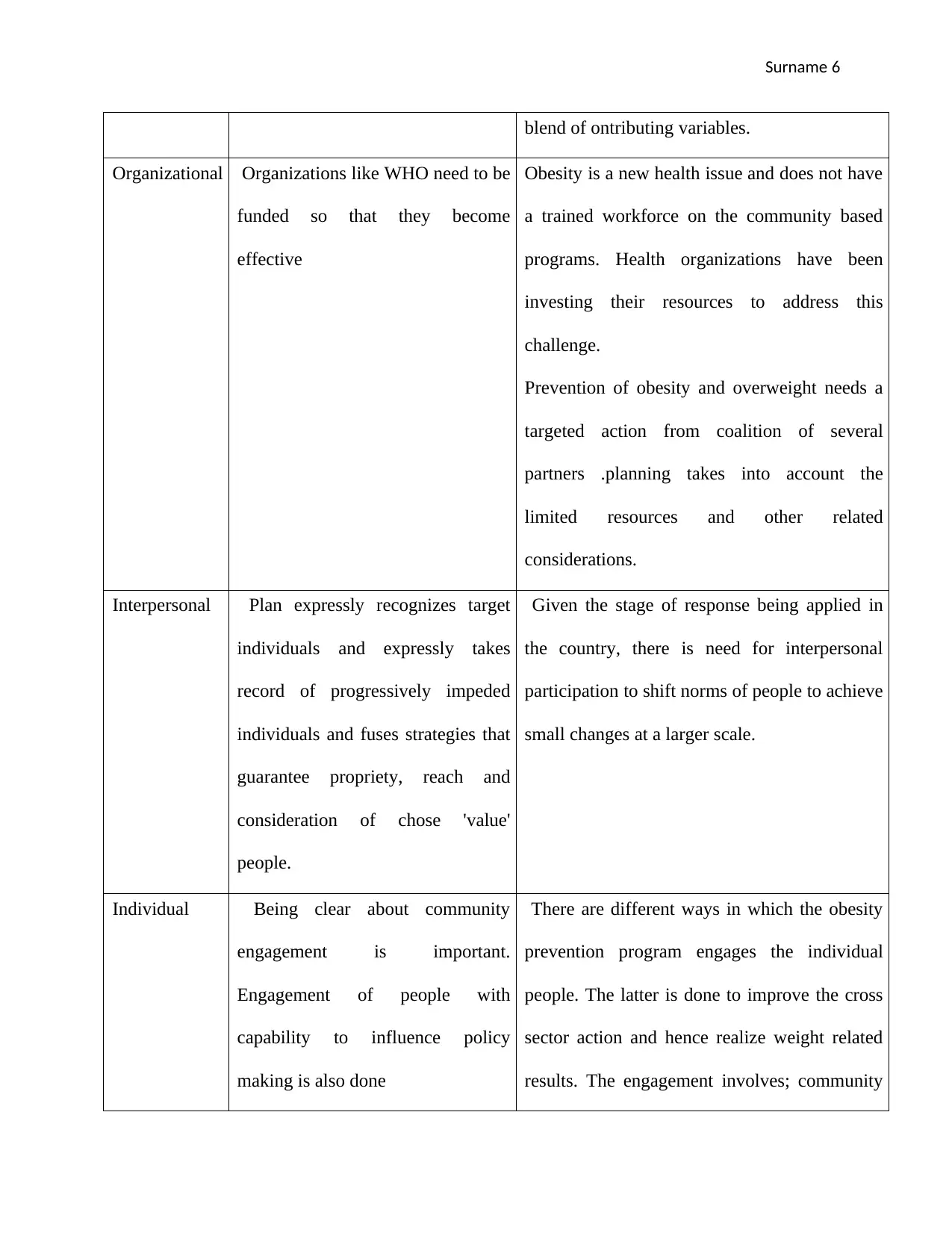
Surname 6
blend of ontributing variables.
Organizational Organizations like WHO need to be
funded so that they become
effective
Obesity is a new health issue and does not have
a trained workforce on the community based
programs. Health organizations have been
investing their resources to address this
challenge.
Prevention of obesity and overweight needs a
targeted action from coalition of several
partners .planning takes into account the
limited resources and other related
considerations.
Interpersonal Plan expressly recognizes target
individuals and expressly takes
record of progressively impeded
individuals and fuses strategies that
guarantee propriety, reach and
consideration of chose 'value'
people.
Given the stage of response being applied in
the country, there is need for interpersonal
participation to shift norms of people to achieve
small changes at a larger scale.
Individual Being clear about community
engagement is important.
Engagement of people with
capability to influence policy
making is also done
There are different ways in which the obesity
prevention program engages the individual
people. The latter is done to improve the cross
sector action and hence realize weight related
results. The engagement involves; community
blend of ontributing variables.
Organizational Organizations like WHO need to be
funded so that they become
effective
Obesity is a new health issue and does not have
a trained workforce on the community based
programs. Health organizations have been
investing their resources to address this
challenge.
Prevention of obesity and overweight needs a
targeted action from coalition of several
partners .planning takes into account the
limited resources and other related
considerations.
Interpersonal Plan expressly recognizes target
individuals and expressly takes
record of progressively impeded
individuals and fuses strategies that
guarantee propriety, reach and
consideration of chose 'value'
people.
Given the stage of response being applied in
the country, there is need for interpersonal
participation to shift norms of people to achieve
small changes at a larger scale.
Individual Being clear about community
engagement is important.
Engagement of people with
capability to influence policy
making is also done
There are different ways in which the obesity
prevention program engages the individual
people. The latter is done to improve the cross
sector action and hence realize weight related
results. The engagement involves; community
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Surname 7
participation at individual level,
implementation of the program at local level
and seeking to achieve changes in the local
communities.
Conclusion
The overall increment in obesity and overweight incorporates Australia, where all
populace gatherings are influenced, with Aboriginal and Torres Strait Islander people sets being
especially powerless. Complex components add to the elevated amounts of overweight and
stoutness among Aboriginal and Torres Strait Islander people; however, unfortunate eating
regimen and an absence of physical movement are principle givers. There is little question that
numerous constant wellbeing situations that occur amongst Aboriginal people groups are linked
to overweight and obesity. The 2014-2015 NATSIHS illustrates that significant extents of
Indigenous individuals are overweight or obese in all age groups beyond 15 years. Activities
tending to overweight and obesity incorporate appropriate training and solace of physical
movement and sound nourishment. Sound conditions and ventures to address the social
imbalances in wellbeing are essential for counteractive action methodologies. Improving
admission to nourishing sustenance is a crucial advance, especially for Indigenous individuals in
the country and remote territories. Large systems, including those for youths, are important to
foresee overweight and obesity, motivating further wellbeing among Indigenous persons.
Activities should be situated inside expansive systems tending to the proceeding with social and
monetary detriments that numerous Indigenous individuals experience.
participation at individual level,
implementation of the program at local level
and seeking to achieve changes in the local
communities.
Conclusion
The overall increment in obesity and overweight incorporates Australia, where all
populace gatherings are influenced, with Aboriginal and Torres Strait Islander people sets being
especially powerless. Complex components add to the elevated amounts of overweight and
stoutness among Aboriginal and Torres Strait Islander people; however, unfortunate eating
regimen and an absence of physical movement are principle givers. There is little question that
numerous constant wellbeing situations that occur amongst Aboriginal people groups are linked
to overweight and obesity. The 2014-2015 NATSIHS illustrates that significant extents of
Indigenous individuals are overweight or obese in all age groups beyond 15 years. Activities
tending to overweight and obesity incorporate appropriate training and solace of physical
movement and sound nourishment. Sound conditions and ventures to address the social
imbalances in wellbeing are essential for counteractive action methodologies. Improving
admission to nourishing sustenance is a crucial advance, especially for Indigenous individuals in
the country and remote territories. Large systems, including those for youths, are important to
foresee overweight and obesity, motivating further wellbeing among Indigenous persons.
Activities should be situated inside expansive systems tending to the proceeding with social and
monetary detriments that numerous Indigenous individuals experience.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Surname 8
Bibliography
Bibliography

Surname 9
1. Bogossian, F E, J Hepworth , and G M Leong. "A cross-sectional analysis of patterns of
obesity in a cohort of working nurses and midwives in Australia, New Zealand, and the
United Kingdom." International journal of nursing studies 43, no. 5 (2016): 34-56.
2. Buchmueller, T C, and M Johar. "Obesity and health expenditures: evidence from
Australia." Economics & Human Biology 14, no. 5 (2015): 134-153.
3. King , L, and T B Gill . Best Practice Principles for Community-based Obesity
Prevention. Geelong: Deakin University, 2009.
4. McIntyre , H D, K S Gibbons , and V J Flenady. "Overweight and obesity in Australian
mothers: epidemic or endemic?" Medical Journal of Australia 34, no. 4 (2014): 143-187.
5. Rahman , A, and A Harding. "Prevalence of overweight and obesity epidemic in
Australia: some causes and consequences." JP Journal of Biostatistics 23, no. 4 (2014):
56-67.
6. Schultz , R. "Prevalences of overweight and obesity among children in remote Aboriginal
communities in central Australia. Rural and remote health." Obesity and Overweight 45,
no. 2 (2015): 132-154.
7. Walls , H L, D J Magliano, and C E Stevenson. "Projected progression of the prevalence
of obesity in Australia." OBesity 56, no. 3 (2014): 65-78.
1. Bogossian, F E, J Hepworth , and G M Leong. "A cross-sectional analysis of patterns of
obesity in a cohort of working nurses and midwives in Australia, New Zealand, and the
United Kingdom." International journal of nursing studies 43, no. 5 (2016): 34-56.
2. Buchmueller, T C, and M Johar. "Obesity and health expenditures: evidence from
Australia." Economics & Human Biology 14, no. 5 (2015): 134-153.
3. King , L, and T B Gill . Best Practice Principles for Community-based Obesity
Prevention. Geelong: Deakin University, 2009.
4. McIntyre , H D, K S Gibbons , and V J Flenady. "Overweight and obesity in Australian
mothers: epidemic or endemic?" Medical Journal of Australia 34, no. 4 (2014): 143-187.
5. Rahman , A, and A Harding. "Prevalence of overweight and obesity epidemic in
Australia: some causes and consequences." JP Journal of Biostatistics 23, no. 4 (2014):
56-67.
6. Schultz , R. "Prevalences of overweight and obesity among children in remote Aboriginal
communities in central Australia. Rural and remote health." Obesity and Overweight 45,
no. 2 (2015): 132-154.
7. Walls , H L, D J Magliano, and C E Stevenson. "Projected progression of the prevalence
of obesity in Australia." OBesity 56, no. 3 (2014): 65-78.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





![Diabetes Mellitus and Health Promotion Campaign Report - [University]](/_next/image/?url=https%3A%2F%2Fdesklib.com%2Fmedia%2Fimages%2Fws%2F94896ae70d2542399b982aab97667cb3.jpg&w=256&q=75)