Evaluating the Between The Flags (BTF) Program: A NSW Initiative
VerifiedAdded on 2023/06/13
|1
|969
|314
AI Summary
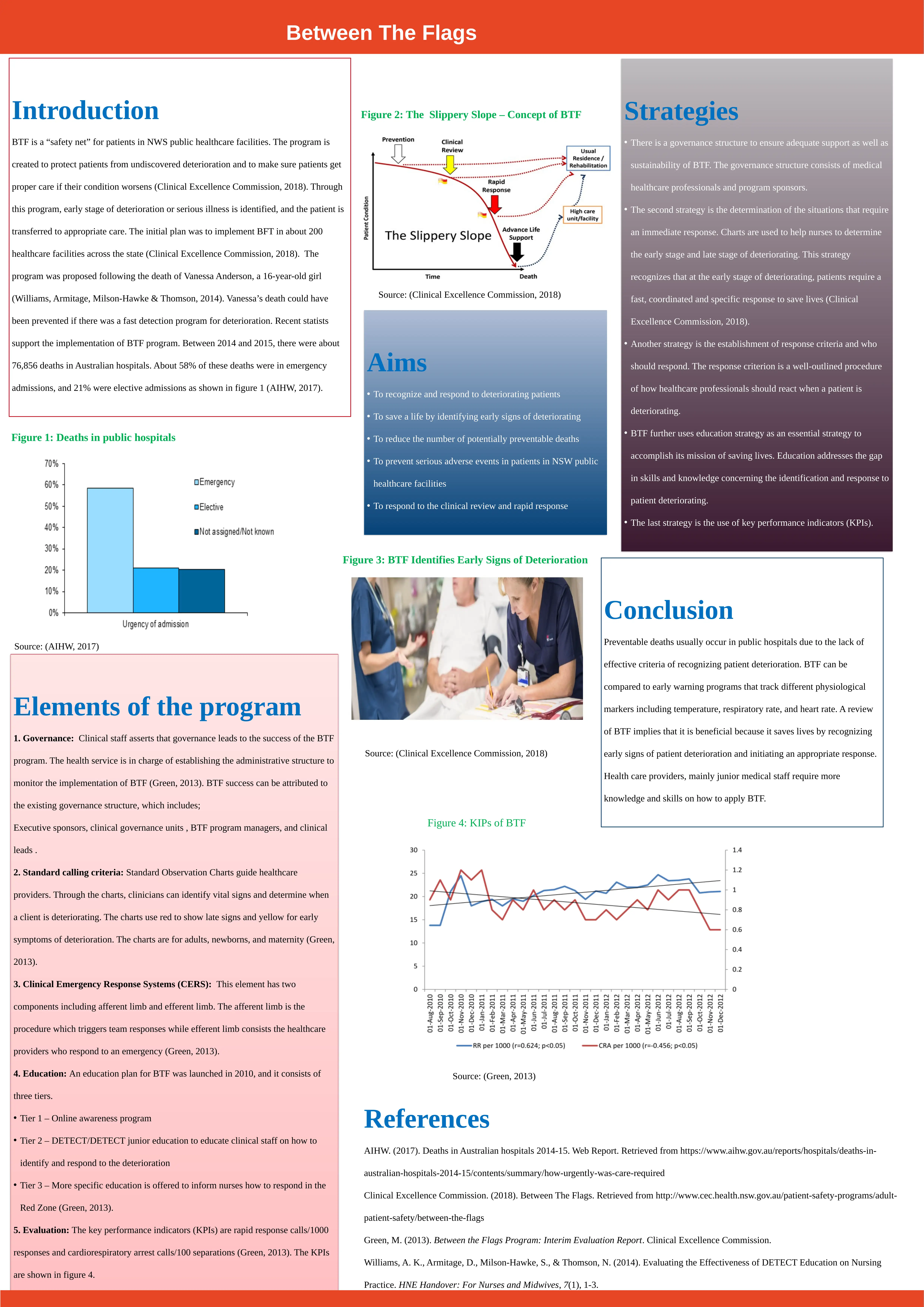
The Between The Flags (BTF) program is a safety net initiative implemented in New South Wales (NSW) public healthcare facilities to protect patients from undetected deterioration and ensure timely and appropriate care. Originating from the preventable death of a young patient, Vanessa Anderson, BTF aims to recognize and respond to deteriorating patients, save lives, reduce preventable deaths, and prevent serious adverse events. The program's elements include governance structures, standard calling criteria, Clinical Emergency Response Systems (CERS), education tiers, and key performance indicators (KPIs). Governance ensures support and sustainability, while standard observation charts help clinicians identify vital signs indicating deterioration. CERS involves afferent and efferent limbs for triggering and responding to emergencies. Education addresses skill gaps in identifying and responding to deterioration. KPIs, such as rapid response calls, are used for evaluation. The program's success relies on early detection and coordinated responses, highlighting the need for continuous education and skill development among healthcare providers, especially junior medical staff. The BTF program serves as a crucial early warning system, tracking physiological markers to improve patient outcomes and reduce preventable deaths in NSW hospitals.






![[object Object]](/_next/static/media/star-bottom.7253800d.svg)