In-service: Acute Management of Drowning in Paediatric Patients
VerifiedAdded on 2023/01/19
|10
|975
|80
Presentation
AI Summary
This presentation provides an overview of the acute management of drowning in paediatric patients, focusing on evidence-based practice. It begins by defining drowning and its impact, including the physiological effects of submersion and the associated health risks. The presentation then details the assessment process, emphasizing the importance of evaluating the child's level of consciousness, respiratory rate, and signs of pulmonary edema. Following assessment, the presentation outlines crucial nursing interventions, such as providing supplemental oxygen, maintaining the airway, and assisting with ventilation if necessary. The rationale behind each intervention is explained, highlighting the importance of maintaining optimal gas exchange and preventing complications. The presentation concludes with a review of relevant research and evidence supporting the proposed management strategies.
ACUTE MANAGEMENT OF
DROWNING IN PAEDIATRIC
PATIENTS
NAME:
INSTITUTION:
TUTOR:
DATE:
DROWNING IN PAEDIATRIC
PATIENTS
NAME:
INSTITUTION:
TUTOR:
DATE:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Overview
Drowning is respiratory impairment after being in or under a liquid.
The assessment of this condition in children involve assessing the
respiratory rate, depth and rhythm of the heart.
Assessing the level of consciousness and any signs of worsening
pulmonary edema.
The nursing interventions involve providing oxygen as ordered and
maintaining the airway while protecting the cervical spine.
Drowning is respiratory impairment after being in or under a liquid.
The assessment of this condition in children involve assessing the
respiratory rate, depth and rhythm of the heart.
Assessing the level of consciousness and any signs of worsening
pulmonary edema.
The nursing interventions involve providing oxygen as ordered and
maintaining the airway while protecting the cervical spine.
The goal of the intervention is to maintain optimal gas exchange
which can be seen through normal arterial blood gases results.
which can be seen through normal arterial blood gases results.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
BACKGROUND
According to the World Health Organization, Drowning is defined as
impaired gaseous exchange after being in or under a liquid(Conover
& Romero, 2018).
Plasma is pulled into the lungs due to aspiration of the liquid leading
to hypoxemia, acidosis and hypovolemia in pediatrics.
Drowning is a serious health problem in Australia.
According to statistics,148 children between 0 and 4 years drowned
between 2002 and 2017(Numa, Hammer, & Newth, 2012).
According to the World Health Organization, Drowning is defined as
impaired gaseous exchange after being in or under a liquid(Conover
& Romero, 2018).
Plasma is pulled into the lungs due to aspiration of the liquid leading
to hypoxemia, acidosis and hypovolemia in pediatrics.
Drowning is a serious health problem in Australia.
According to statistics,148 children between 0 and 4 years drowned
between 2002 and 2017(Numa, Hammer, & Newth, 2012).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
62.6% of the drowning children were male with majority born in
Australia. Furthermore, 40.7% occurred in the summer(Macintosh &
Austin, 2017).
Home swimming pools were the leading locations for the fatalities.
Strategies for preventing drowning among children include adult
supervision, restricting children's access to water and resuscitation.
There are different nursing interventions proposed after drowning in
children such as resuscitation with over 30 years of research and
evidence. The rationale of resuscitation is to ensure that the child is
able to breath normally again(Moler et al., 2016).
Australia. Furthermore, 40.7% occurred in the summer(Macintosh &
Austin, 2017).
Home swimming pools were the leading locations for the fatalities.
Strategies for preventing drowning among children include adult
supervision, restricting children's access to water and resuscitation.
There are different nursing interventions proposed after drowning in
children such as resuscitation with over 30 years of research and
evidence. The rationale of resuscitation is to ensure that the child is
able to breath normally again(Moler et al., 2016).
ASSESSMENT
The nurse is supposed to assess the level of consciousness in the
drowned child. The rationale of this assessment is to find out if the
patient is at risk of cerebral edema which occurs within three minutes
of submersion(Chotai et al., 2017).
The nurse should assess the respiratory rate, depth and rhythm. The
rationale of this assessment is to find out if the patient is
experiencing breathing difficulties. This can be seen through rapid,
shallow breathing patterns and hypoventilation(Numa, Hammer, &
Newth, 2012).
The nurse is supposed to assess the level of consciousness in the
drowned child. The rationale of this assessment is to find out if the
patient is at risk of cerebral edema which occurs within three minutes
of submersion(Chotai et al., 2017).
The nurse should assess the respiratory rate, depth and rhythm. The
rationale of this assessment is to find out if the patient is
experiencing breathing difficulties. This can be seen through rapid,
shallow breathing patterns and hypoventilation(Numa, Hammer, &
Newth, 2012).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Assess for any sings of worsening pulmonary edema. The rationale
for this assessment is to find out if the child is experiencing
pulmonary edema.
This can be visible through pink, frothy sputum. Incase of such, then
the nurse should initiate mechanical ventilation(Macintosh & Austin,
2017).
for this assessment is to find out if the child is experiencing
pulmonary edema.
This can be visible through pink, frothy sputum. Incase of such, then
the nurse should initiate mechanical ventilation(Macintosh & Austin,
2017).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
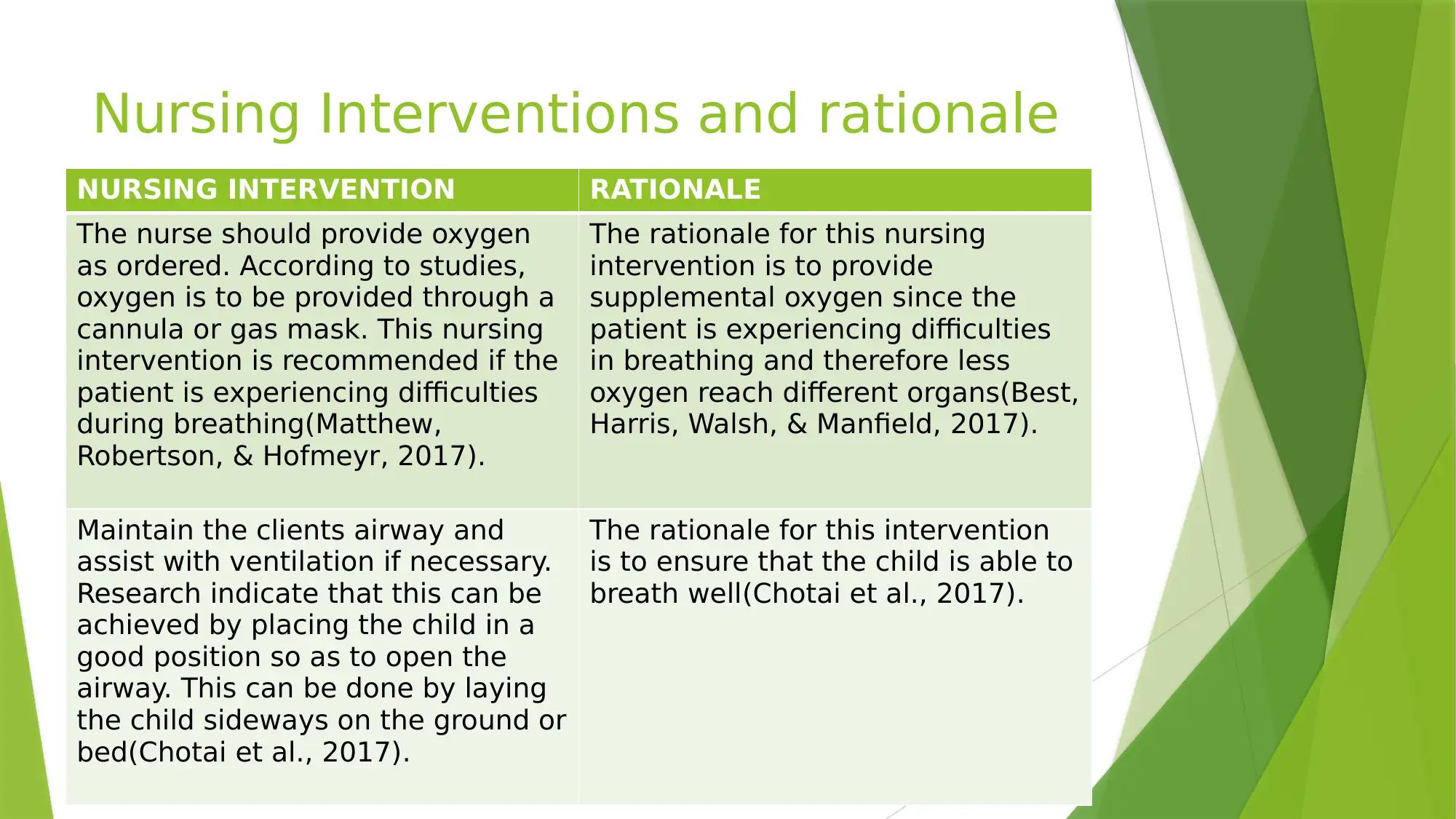
Nursing Interventions and rationale
NURSING INTERVENTION RATIONALE
The nurse should provide oxygen
as ordered. According to studies,
oxygen is to be provided through a
cannula or gas mask. This nursing
intervention is recommended if the
patient is experiencing difficulties
during breathing(Matthew,
Robertson, & Hofmeyr, 2017).
The rationale for this nursing
intervention is to provide
supplemental oxygen since the
patient is experiencing difficulties
in breathing and therefore less
oxygen reach different organs(Best,
Harris, Walsh, & Manfield, 2017).
Maintain the clients airway and
assist with ventilation if necessary.
Research indicate that this can be
achieved by placing the child in a
good position so as to open the
airway. This can be done by laying
the child sideways on the ground or
bed(Chotai et al., 2017).
The rationale for this intervention
is to ensure that the child is able to
breath well(Chotai et al., 2017).
NURSING INTERVENTION RATIONALE
The nurse should provide oxygen
as ordered. According to studies,
oxygen is to be provided through a
cannula or gas mask. This nursing
intervention is recommended if the
patient is experiencing difficulties
during breathing(Matthew,
Robertson, & Hofmeyr, 2017).
The rationale for this nursing
intervention is to provide
supplemental oxygen since the
patient is experiencing difficulties
in breathing and therefore less
oxygen reach different organs(Best,
Harris, Walsh, & Manfield, 2017).
Maintain the clients airway and
assist with ventilation if necessary.
Research indicate that this can be
achieved by placing the child in a
good position so as to open the
airway. This can be done by laying
the child sideways on the ground or
bed(Chotai et al., 2017).
The rationale for this intervention
is to ensure that the child is able to
breath well(Chotai et al., 2017).
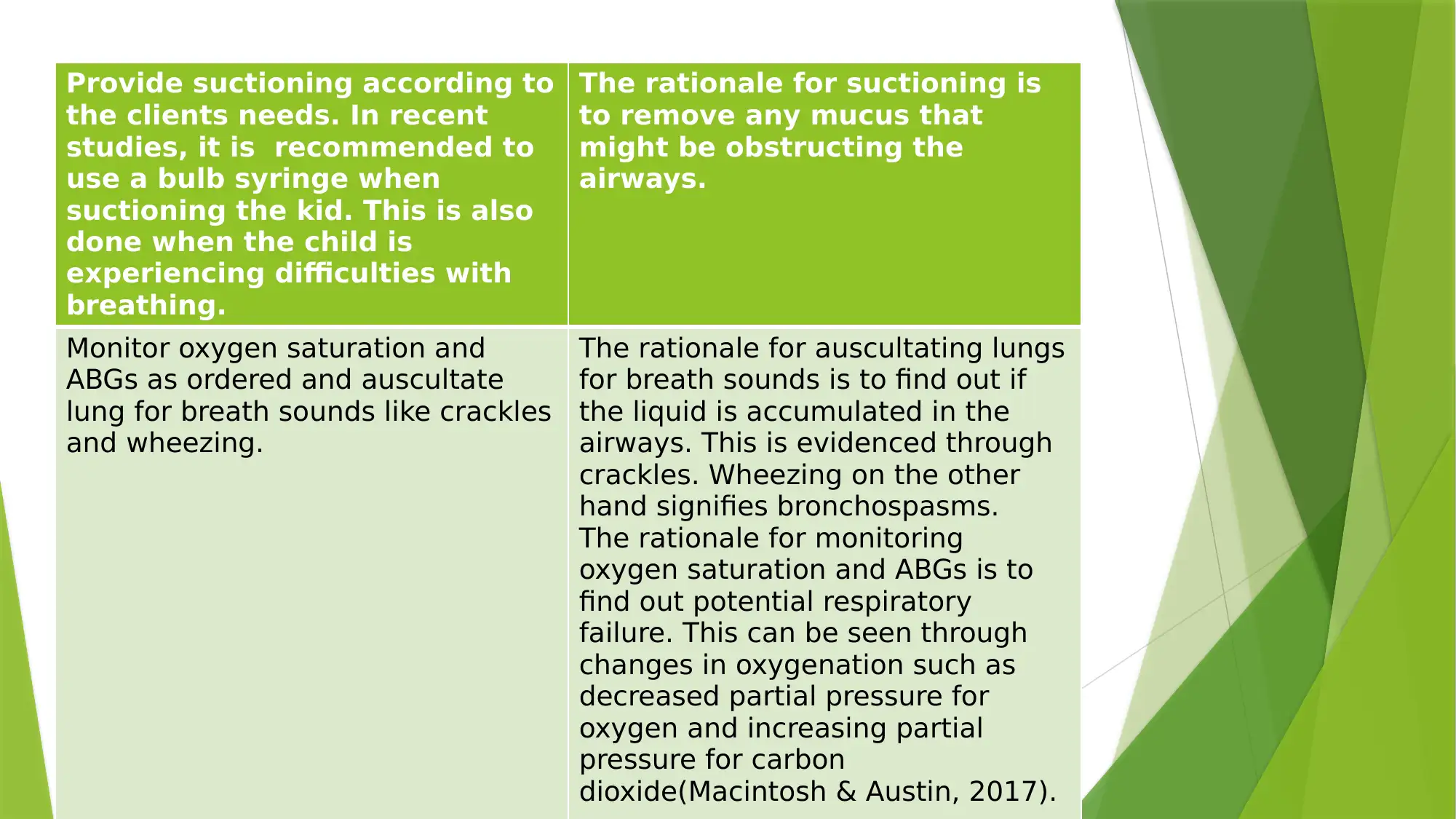
Provide suctioning according to
the clients needs. In recent
studies, it is recommended to
use a bulb syringe when
suctioning the kid. This is also
done when the child is
experiencing difficulties with
breathing.
The rationale for suctioning is
to remove any mucus that
might be obstructing the
airways.
Monitor oxygen saturation and
ABGs as ordered and auscultate
lung for breath sounds like crackles
and wheezing.
The rationale for auscultating lungs
for breath sounds is to find out if
the liquid is accumulated in the
airways. This is evidenced through
crackles. Wheezing on the other
hand signifies bronchospasms.
The rationale for monitoring
oxygen saturation and ABGs is to
find out potential respiratory
failure. This can be seen through
changes in oxygenation such as
decreased partial pressure for
oxygen and increasing partial
pressure for carbon
dioxide(Macintosh & Austin, 2017).
the clients needs. In recent
studies, it is recommended to
use a bulb syringe when
suctioning the kid. This is also
done when the child is
experiencing difficulties with
breathing.
The rationale for suctioning is
to remove any mucus that
might be obstructing the
airways.
Monitor oxygen saturation and
ABGs as ordered and auscultate
lung for breath sounds like crackles
and wheezing.
The rationale for auscultating lungs
for breath sounds is to find out if
the liquid is accumulated in the
airways. This is evidenced through
crackles. Wheezing on the other
hand signifies bronchospasms.
The rationale for monitoring
oxygen saturation and ABGs is to
find out potential respiratory
failure. This can be seen through
changes in oxygenation such as
decreased partial pressure for
oxygen and increasing partial
pressure for carbon
dioxide(Macintosh & Austin, 2017).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References
Best, R. R., Harris, B. H., Walsh, J. L., & Manfield, T. (2017). Pediatric Drowning.
Pediatric Emergency Care, 1. doi:10.1097/pec.0000000000001169
Chotai, P. N., Manning, L., Eithun, B., Ross, J. C., Eubanks, J. W., Hamner, C., &
Gosain, A. (2017). Pediatric near-drowning events: do they warrant trauma team
activation? Journal of Surgical Research, 212, 108-113.
doi:10.1016/j.jss.2017.01.024
Macintosh, I., & Austin, S. (2017). Management of drowning in children. Paediatrics
and Child Health, 27(9), 415-419. doi:10.1016/j.paed.2017.05.008
Matthew, J., Robertson, C., & Hofmeyr, R. (2017). Update on drowning. South African
Medical Journal, 107(7), 562. doi:10.7196/samj.2017.v107i7.12609
Numa, A., Hammer, J., & Newth, C. (2012). Drowning. Kendig & Chernickâs Disorders
of the Respiratory Tract in Children, 600-604. doi:10.1016/b978-1-4377-1984-
0.00041-3
Best, R. R., Harris, B. H., Walsh, J. L., & Manfield, T. (2017). Pediatric Drowning.
Pediatric Emergency Care, 1. doi:10.1097/pec.0000000000001169
Chotai, P. N., Manning, L., Eithun, B., Ross, J. C., Eubanks, J. W., Hamner, C., &
Gosain, A. (2017). Pediatric near-drowning events: do they warrant trauma team
activation? Journal of Surgical Research, 212, 108-113.
doi:10.1016/j.jss.2017.01.024
Macintosh, I., & Austin, S. (2017). Management of drowning in children. Paediatrics
and Child Health, 27(9), 415-419. doi:10.1016/j.paed.2017.05.008
Matthew, J., Robertson, C., & Hofmeyr, R. (2017). Update on drowning. South African
Medical Journal, 107(7), 562. doi:10.7196/samj.2017.v107i7.12609
Numa, A., Hammer, J., & Newth, C. (2012). Drowning. Kendig & Chernickâs Disorders
of the Respiratory Tract in Children, 600-604. doi:10.1016/b978-1-4377-1984-
0.00041-3
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.



