Western Sydney University 401168: Evidence-Based Treatment Report
VerifiedAdded on 2022/09/16
|10
|2435
|22
Report
AI Summary
This report provides a detailed overview of evidence-based treatment (EBT) in healthcare, examining its evolution, principles, and processes. It highlights the importance of integrating research evidence with clinical expertise and patient preferences. The report discusses the principles governing EBT, including the order of evidence, best practices, and the role of clinical practice instructions. The processes for EBT, such as formulating clinical questions, retrieving evidence, critically appraising the evidence, applying the evidence, evaluating performance, and disseminating outcomes are explained. The report also explores the advantages of EBT, such as improved patient care and reduced costs. The document then addresses barriers to EBT implementation, including time constraints, staff shortages, and a lack of understanding, while also suggesting facilitators like research institution associations, improved staffing, and robust organizational structures. A case study on the use of combined antipsychotic treatments is presented, and the report concludes by emphasizing the importance of using EBT in the treatment of psychotic disorders, focusing on the patient's values and preferences while using one antipsychotic treatment plan. The report also includes clinical questions, keywords, and references to support the discussion.

1
RUNNING HEAD: EVIDENCE-BASED TREATMENT
Evidence-Based Treatment
Name
Institution
RUNNING HEAD: EVIDENCE-BASED TREATMENT
Evidence-Based Treatment
Name
Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
EVIDENCE-BASED TREATMENT
Evidence-Based Treatment
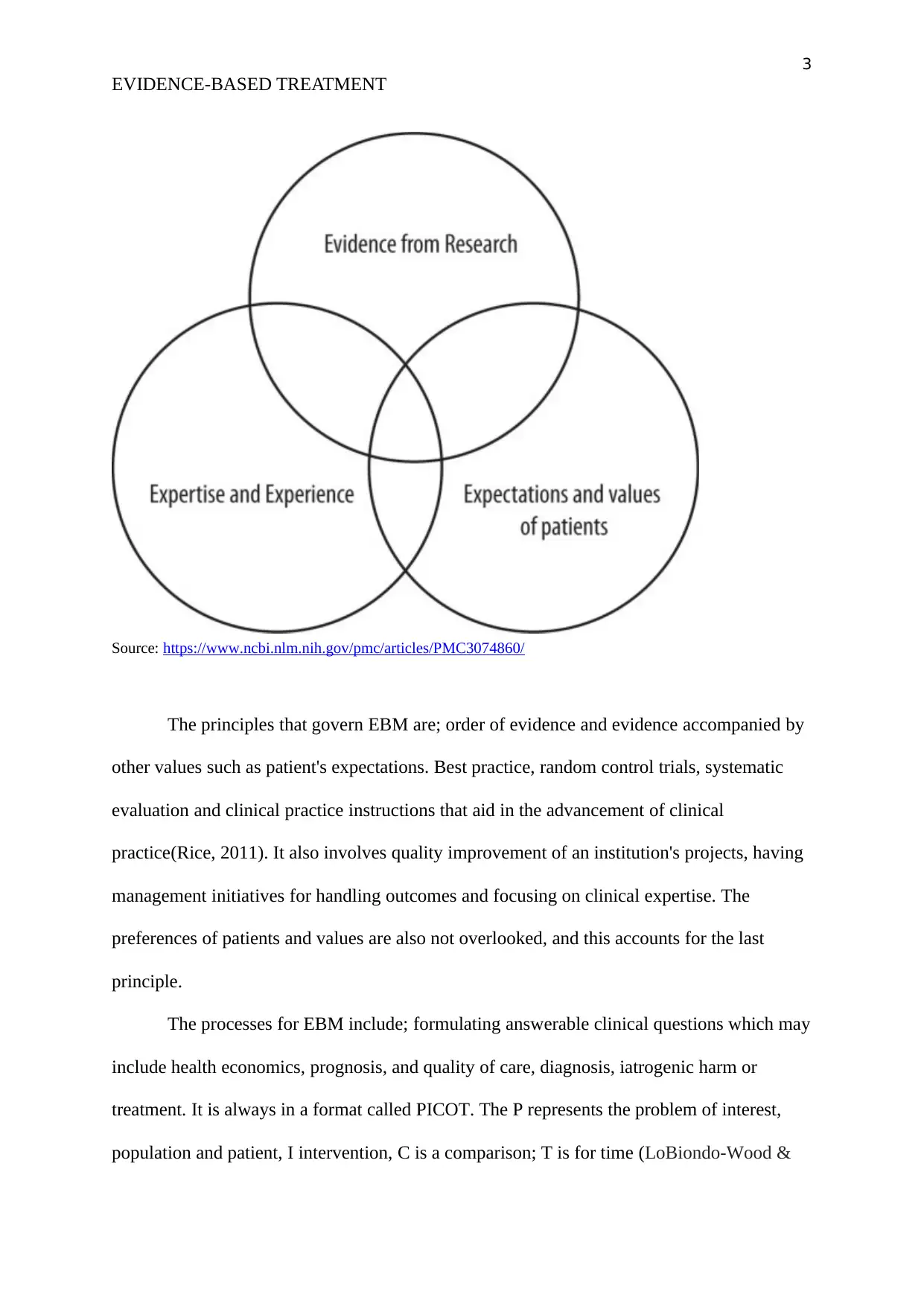
Long before World War II, health care systems were not as diverse. This was mainly
attributed to a low internet connection and research materials available. Health care systems
started evolving after the Second World War. Different methods were used in the treatment
of diseases. A lot of research was done on drugs, application of those drugs and their effects.
Due to good internet connection and a lot of information available in the medical world,
health care resolutions have hadlots of changes since then. The health care decisions took
different angles of standing from those with little or no attention to evidence to those that
heavily relied on evidence (Greenhalgh, Howick & Maskrey, 2014). These differences
brought about distinct health care systems like the Evidence-based Medicine, which was first
identified in a journal called American College of Physicians in 1991. EBM cannot only do
with research evidence but also the incorporation of clinical skill, the distinct values and set
of situations of the particular patient (Greenhalgh, Howick & Maskrey, 2014). A lot of
advances has been made ever since. EBM has been on the rise because of the profusion of
information, ever-rising patient presumption, a populace that is ageing and new technologies
being developed. Some of its advantages are patented care of the victim, the cost of patient
care reduces, and the prowess of the professional caregiver is enhanced. The following is a
diagram explaining EBM:
Figure one
EVIDENCE-BASED TREATMENT
Evidence-Based Treatment
Long before World War II, health care systems were not as diverse. This was mainly
attributed to a low internet connection and research materials available. Health care systems
started evolving after the Second World War. Different methods were used in the treatment
of diseases. A lot of research was done on drugs, application of those drugs and their effects.
Due to good internet connection and a lot of information available in the medical world,
health care resolutions have hadlots of changes since then. The health care decisions took
different angles of standing from those with little or no attention to evidence to those that
heavily relied on evidence (Greenhalgh, Howick & Maskrey, 2014). These differences
brought about distinct health care systems like the Evidence-based Medicine, which was first
identified in a journal called American College of Physicians in 1991. EBM cannot only do
with research evidence but also the incorporation of clinical skill, the distinct values and set
of situations of the particular patient (Greenhalgh, Howick & Maskrey, 2014). A lot of
advances has been made ever since. EBM has been on the rise because of the profusion of
information, ever-rising patient presumption, a populace that is ageing and new technologies
being developed. Some of its advantages are patented care of the victim, the cost of patient
care reduces, and the prowess of the professional caregiver is enhanced. The following is a
diagram explaining EBM:
Figure one
3
EVIDENCE-BASED TREATMENT
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3074860/
The principles that govern EBM are; order of evidence and evidence accompanied by
other values such as patient's expectations. Best practice, random control trials, systematic
evaluation and clinical practice instructions that aid in the advancement of clinical
practice(Rice, 2011). It also involves quality improvement of an institution's projects, having
management initiatives for handling outcomes and focusing on clinical expertise. The
preferences of patients and values are also not overlooked, and this accounts for the last
principle.
The processes for EBM include; formulating answerable clinical questions which may
include health economics, prognosis, and quality of care, diagnosis, iatrogenic harm or
treatment. It is always in a format called PICOT. The P represents the problem of interest,
population and patient, I intervention, C is a comparison; T is for time (LoBiondo-Wood &
EVIDENCE-BASED TREATMENT
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3074860/
The principles that govern EBM are; order of evidence and evidence accompanied by
other values such as patient's expectations. Best practice, random control trials, systematic
evaluation and clinical practice instructions that aid in the advancement of clinical
practice(Rice, 2011). It also involves quality improvement of an institution's projects, having
management initiatives for handling outcomes and focusing on clinical expertise. The
preferences of patients and values are also not overlooked, and this accounts for the last
principle.
The processes for EBM include; formulating answerable clinical questions which may
include health economics, prognosis, and quality of care, diagnosis, iatrogenic harm or
treatment. It is always in a format called PICOT. The P represents the problem of interest,
population and patient, I intervention, C is a comparison; T is for time (LoBiondo-Wood &
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
EVIDENCE-BASED TREATMENT
Haber, 2017). The next step is systematic retrieval of the best evidence available. A selection
of relevant information and relationships should be distinctly researched for the particular
disease. The results found should be sufficient to answer the questions asked. Concepts,
keywords, Boolean connectors and multiple search terms should be used. Searching for the
right evidence is always critical to improving the work already done. Critically appraising the
Evidence is also vital. In this step, each study done should be applicable, reliable and valid to
the patient in question. The evidence found should also be analyzed in terms of weaknesses
and strengths. This will ensure that a clear and decisive decision is arrived at. Another step is
to apply the Evidence found (LoBiondo-Wood & Haber, 2017) . One should find out whether
the evidence applies to a patient in matters to do with their biological structure,
socioeconomic strength and epidemiology. The evidence can be integrated with the best
clinical skill and the preferences of the patient before it is used in the case victim. Evaluating
performance is another crucial step. In this step, the performance has to be evaluated so that
its relevance and authenticity can be known. If the outcome was not achieved, then reasons
for what went wrong should be identified and corrected. Disseminate the outcome is the last
step. When the evidence has already been verified as authentic and applicable, then it can be
released to the organization, one is employed to and given to the rest of the world. This can
either be done through posters, online media, conferences, journal clubs, Intra and
interdepartmental in-services, manuscripts and lectures.
EBM cannot be applicable if it only relies on evidence, it becomes efficient if it is
accompanies with the skill of the clinician and being considerate to the patient’s preference
and values. Sometimes evidence is not available and therefore having the patient's
preferences, and values are very vital (Greenhalgh, Howick & Maskrey, 2014) . Moreover,
having the patient's choices will determine how the evidence will be applied. It makes the
individual patient more comfortable with the treatment, and it also avoids
EVIDENCE-BASED TREATMENT
Haber, 2017). The next step is systematic retrieval of the best evidence available. A selection
of relevant information and relationships should be distinctly researched for the particular
disease. The results found should be sufficient to answer the questions asked. Concepts,
keywords, Boolean connectors and multiple search terms should be used. Searching for the
right evidence is always critical to improving the work already done. Critically appraising the
Evidence is also vital. In this step, each study done should be applicable, reliable and valid to
the patient in question. The evidence found should also be analyzed in terms of weaknesses
and strengths. This will ensure that a clear and decisive decision is arrived at. Another step is
to apply the Evidence found (LoBiondo-Wood & Haber, 2017) . One should find out whether
the evidence applies to a patient in matters to do with their biological structure,
socioeconomic strength and epidemiology. The evidence can be integrated with the best
clinical skill and the preferences of the patient before it is used in the case victim. Evaluating
performance is another crucial step. In this step, the performance has to be evaluated so that
its relevance and authenticity can be known. If the outcome was not achieved, then reasons
for what went wrong should be identified and corrected. Disseminate the outcome is the last
step. When the evidence has already been verified as authentic and applicable, then it can be
released to the organization, one is employed to and given to the rest of the world. This can
either be done through posters, online media, conferences, journal clubs, Intra and
interdepartmental in-services, manuscripts and lectures.
EBM cannot be applicable if it only relies on evidence, it becomes efficient if it is
accompanies with the skill of the clinician and being considerate to the patient’s preference
and values. Sometimes evidence is not available and therefore having the patient's
preferences, and values are very vital (Greenhalgh, Howick & Maskrey, 2014) . Moreover,
having the patient's choices will determine how the evidence will be applied. It makes the
individual patient more comfortable with the treatment, and it also avoids
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
EVIDENCE-BASED TREATMENT
paternalism.Another advantage of having the patient's preferences and values is that the
patient gets to participate actively in their treatment. The patient is more experienced in his
illness; thus, the clinician can focus on the psychosocial aspects of the disease. Since the
preferences and values of the patient will be known, the best treatment decision is made for
the patient. Choices of the patient and costs are essential and have been cited to bring out the
best outcomes in the treatment of any disease.
Evidence-based practices in health systems have improved lots of lives and thus are
expected to grow even more in the coming years. Nevertheless, some factors act as a barrier
for its full usage. One of the obstacles is the lack of time. It takes time to have the expertise
and research on one particular disease (Majid, Foo, Luyt, Zhang, Theng, Chang & Mokhtar,
2011). It takes even more time to learn the preferences of a patient and look for a way to best
ingest the medicine into the patient. Another barrier cited by Solomons & Spross (2011) is
shortage of staff. Very few people have ventured into Evidence-Based practices, and thus, the
number of staff continues to be a problem. If the patients are many, and the professionals are
few, the treatment offered will not cater for many. Another barrier cited is little understanding
of evidence-based health. Some who know it have a negative perspective on it (Solomons &
Spross, 2011). This means that a lot of awareness needs to be done so that a lot of people can
know its advantages and be able to use it. Academic skills are another barrier. A lot of nurses
trained twenty years ago were nottrained in evidence-based health practice, and thus, there is
a real gap. Some of them do not want to change or teach because they believe what they have
been doing for the past twenty years is working just fine.
Facilitators that simplify the implementation of evidence-based health practice
include; association with research institutions so that more research can be done (Mathieson,
Grande & Luker, 2018). Another facilitator is improving the number of employed staff.
Increasing the number of working team will cater for the high number of patients. More
EVIDENCE-BASED TREATMENT
paternalism.Another advantage of having the patient's preferences and values is that the
patient gets to participate actively in their treatment. The patient is more experienced in his
illness; thus, the clinician can focus on the psychosocial aspects of the disease. Since the
preferences and values of the patient will be known, the best treatment decision is made for
the patient. Choices of the patient and costs are essential and have been cited to bring out the
best outcomes in the treatment of any disease.
Evidence-based practices in health systems have improved lots of lives and thus are
expected to grow even more in the coming years. Nevertheless, some factors act as a barrier
for its full usage. One of the obstacles is the lack of time. It takes time to have the expertise
and research on one particular disease (Majid, Foo, Luyt, Zhang, Theng, Chang & Mokhtar,
2011). It takes even more time to learn the preferences of a patient and look for a way to best
ingest the medicine into the patient. Another barrier cited by Solomons & Spross (2011) is
shortage of staff. Very few people have ventured into Evidence-Based practices, and thus, the
number of staff continues to be a problem. If the patients are many, and the professionals are
few, the treatment offered will not cater for many. Another barrier cited is little understanding
of evidence-based health. Some who know it have a negative perspective on it (Solomons &
Spross, 2011). This means that a lot of awareness needs to be done so that a lot of people can
know its advantages and be able to use it. Academic skills are another barrier. A lot of nurses
trained twenty years ago were nottrained in evidence-based health practice, and thus, there is
a real gap. Some of them do not want to change or teach because they believe what they have
been doing for the past twenty years is working just fine.
Facilitators that simplify the implementation of evidence-based health practice
include; association with research institutions so that more research can be done (Mathieson,
Grande & Luker, 2018). Another facilitator is improving the number of employed staff.
Increasing the number of working team will cater for the high number of patients. More
6
EVIDENCE-BASED TREATMENT
strategies that can be used include establishing a robust organizational structure that is going
to act as an accountability point. The practitioners should be educated early beforehand so
that they can be prepared for change. Another strategy that can be used can be encouraging
and facilitating the improvement of skills in the area of expertise (Rycroft-Malone, &
Bucknall, (Eds.), 2011). Encouraging staff to improve one's ability will increase the chances
of getting accurate results, and there will be more qualified EBP professionals. The financial
investment can also go a long way to sustain the research involved and the academic learning
required to be a piece of evidence-based health practitioners.
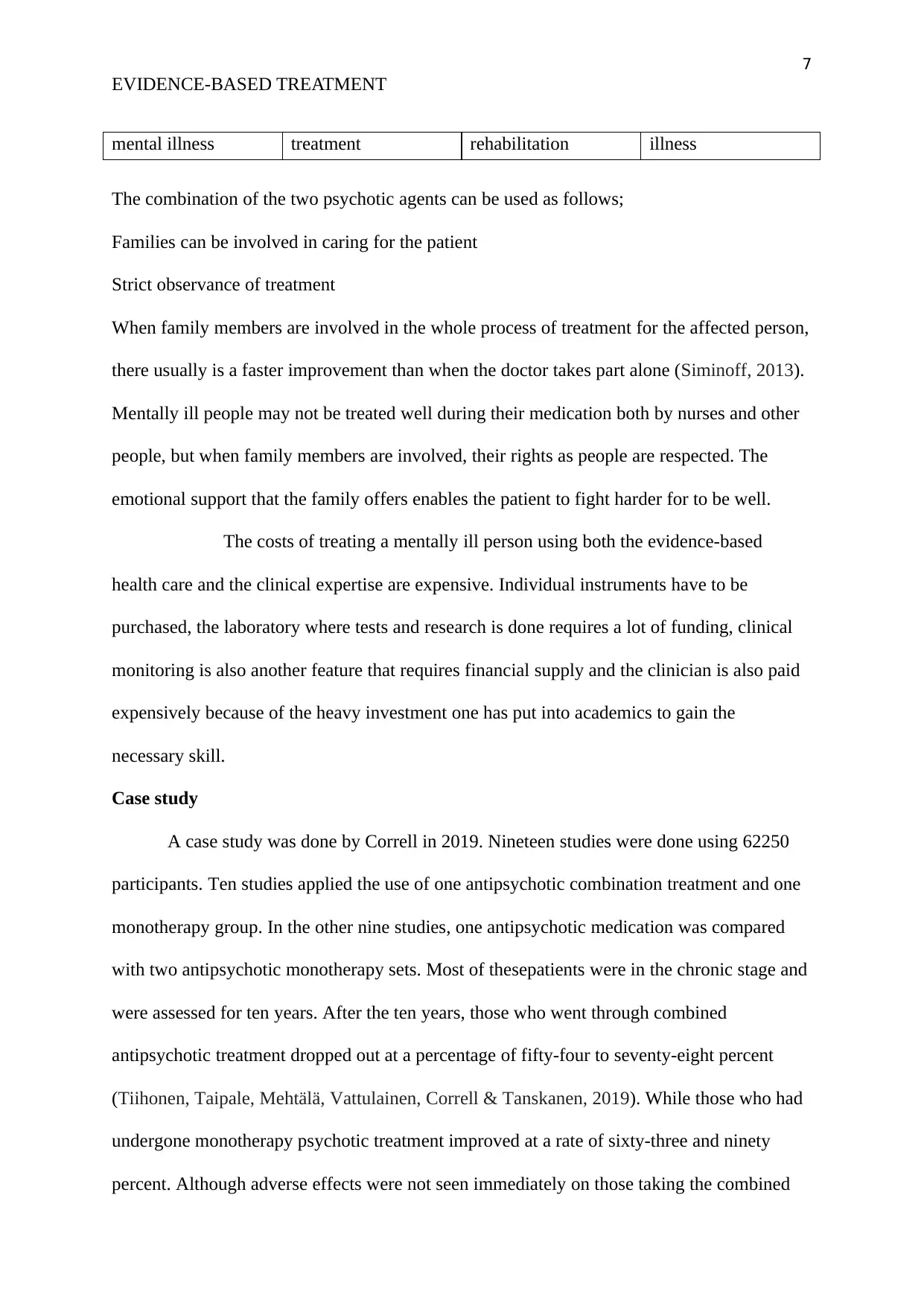
Clinical questions and keywords
In the treatment of patients with psychotic disorders, is it more safe and effective to
use only one mode of psychotic disorder treatment, or is it useful and reliable to use two
psychotic disorders treatments concurrently?The treatment of psychotic disorders with more
than one antipsychotic disorder treatment is dangerous and weak. Most of the evidence to
support it as an excellent method of treatment is unsupportive. It is not safe and therefore,
there has been a need to define which psychotic disorder agents can be combined and used
for treatment.
Question
Type of patient or
problem
Intervention Comparison
intervention
Outcome
Patients with
psychotic disorders
Antipsychotic
blending therapy
Antipsychotic
monotherapy
Avoidance of
relapses
hostile effects of
treatment
incapacity and
functioning
all-cause mortality
signs severity
quality of life
Keywords: drugs, Keywords: mind Keywords: Keywords: mental
EVIDENCE-BASED TREATMENT
strategies that can be used include establishing a robust organizational structure that is going
to act as an accountability point. The practitioners should be educated early beforehand so
that they can be prepared for change. Another strategy that can be used can be encouraging
and facilitating the improvement of skills in the area of expertise (Rycroft-Malone, &
Bucknall, (Eds.), 2011). Encouraging staff to improve one's ability will increase the chances
of getting accurate results, and there will be more qualified EBP professionals. The financial
investment can also go a long way to sustain the research involved and the academic learning
required to be a piece of evidence-based health practitioners.
Clinical questions and keywords
In the treatment of patients with psychotic disorders, is it more safe and effective to
use only one mode of psychotic disorder treatment, or is it useful and reliable to use two
psychotic disorders treatments concurrently?The treatment of psychotic disorders with more
than one antipsychotic disorder treatment is dangerous and weak. Most of the evidence to
support it as an excellent method of treatment is unsupportive. It is not safe and therefore,
there has been a need to define which psychotic disorder agents can be combined and used
for treatment.
Question
Type of patient or
problem
Intervention Comparison
intervention
Outcome
Patients with
psychotic disorders
Antipsychotic
blending therapy
Antipsychotic
monotherapy
Avoidance of
relapses
hostile effects of
treatment
incapacity and
functioning
all-cause mortality
signs severity
quality of life
Keywords: drugs, Keywords: mind Keywords: Keywords: mental
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
EVIDENCE-BASED TREATMENT
mental illness treatment rehabilitation illness
The combination of the two psychotic agents can be used as follows;
Families can be involved in caring for the patient
Strict observance of treatment
When family members are involved in the whole process of treatment for the affected person,
there usually is a faster improvement than when the doctor takes part alone (Siminoff, 2013).
Mentally ill people may not be treated well during their medication both by nurses and other
people, but when family members are involved, their rights as people are respected. The
emotional support that the family offers enables the patient to fight harder for to be well.
The costs of treating a mentally ill person using both the evidence-based
health care and the clinical expertise are expensive. Individual instruments have to be
purchased, the laboratory where tests and research is done requires a lot of funding, clinical
monitoring is also another feature that requires financial supply and the clinician is also paid
expensively because of the heavy investment one has put into academics to gain the
necessary skill.
Case study
A case study was done by Correll in 2019. Nineteen studies were done using 62250
participants. Ten studies applied the use of one antipsychotic combination treatment and one
monotherapy group. In the other nine studies, one antipsychotic medication was compared
with two antipsychotic monotherapy sets. Most of thesepatients were in the chronic stage and
were assessed for ten years. After the ten years, those who went through combined
antipsychotic treatment dropped out at a percentage of fifty-four to seventy-eight percent
(Tiihonen, Taipale, Mehtälä, Vattulainen, Correll & Tanskanen, 2019). While those who had
undergone monotherapy psychotic treatment improved at a rate of sixty-three and ninety
percent. Although adverse effects were not seen immediately on those taking the combined
EVIDENCE-BASED TREATMENT
mental illness treatment rehabilitation illness
The combination of the two psychotic agents can be used as follows;
Families can be involved in caring for the patient
Strict observance of treatment
When family members are involved in the whole process of treatment for the affected person,
there usually is a faster improvement than when the doctor takes part alone (Siminoff, 2013).
Mentally ill people may not be treated well during their medication both by nurses and other
people, but when family members are involved, their rights as people are respected. The
emotional support that the family offers enables the patient to fight harder for to be well.
The costs of treating a mentally ill person using both the evidence-based
health care and the clinical expertise are expensive. Individual instruments have to be
purchased, the laboratory where tests and research is done requires a lot of funding, clinical
monitoring is also another feature that requires financial supply and the clinician is also paid
expensively because of the heavy investment one has put into academics to gain the
necessary skill.
Case study
A case study was done by Correll in 2019. Nineteen studies were done using 62250
participants. Ten studies applied the use of one antipsychotic combination treatment and one
monotherapy group. In the other nine studies, one antipsychotic medication was compared
with two antipsychotic monotherapy sets. Most of thesepatients were in the chronic stage and
were assessed for ten years. After the ten years, those who went through combined
antipsychotic treatment dropped out at a percentage of fifty-four to seventy-eight percent
(Tiihonen, Taipale, Mehtälä, Vattulainen, Correll & Tanskanen, 2019). While those who had
undergone monotherapy psychotic treatment improved at a rate of sixty-three and ninety
percent. Although adverse effects were not seen immediately on those taking the combined
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
EVIDENCE-BASED TREATMENT
antipsychotic medication, the results were seen later on and thus was considered not to be
safe.
In conclusion, using two different antipsychotic agent treatments for those who have a
mental illness should not be used. It can only be used if three various monopsychotic
treatment attempts have been tried and all have failed (Bergendal, Schiöler, Wettermark, &
Björkstén, 2015). Using two different antipsychotic treatment plans can only be used as a last
resort. On the other hand, evidence-based health care should be used with one antipsychotic
treatment plan. This way, patients values' and preferences will be considered while the
professional applies the best expertise he has acquired.
EVIDENCE-BASED TREATMENT
antipsychotic medication, the results were seen later on and thus was considered not to be
safe.
In conclusion, using two different antipsychotic agent treatments for those who have a
mental illness should not be used. It can only be used if three various monopsychotic
treatment attempts have been tried and all have failed (Bergendal, Schiöler, Wettermark, &
Björkstén, 2015). Using two different antipsychotic treatment plans can only be used as a last
resort. On the other hand, evidence-based health care should be used with one antipsychotic
treatment plan. This way, patients values' and preferences will be considered while the
professional applies the best expertise he has acquired.
9
EVIDENCE-BASED TREATMENT
References
Bergendal, A., Schiöler, H., Wettermark, B., & Björkstén, K. S. (2015). Concomitant use of
two or more antipsychotic drugs is every day in Sweden. Therapeutic advances in
psychopharmacology, 5(4), 224-231.
Greenhalgh, T., Howick, J., & Maskrey, N. (2014). Evidence based medicine: a movement in
crisis?. Bmj, 348, g3725.
LoBiondo-Wood, G., & Haber, J. (2017). Nursing research-E-book: methods and critical
appraisal for evidence-based practice. Elsevier Health Sciences.
Mathieson, A., Grande, G., & Luker, K. (2018). Strategies, facilitators and barriers to
implementation of evidence-based practice in community nursing: a systematic
mixed-studies review and qualitative synthesis. Primary health care research &
development, 20.
Majid, S., Foo, S., Luyt, B., Zhang, X., Theng, Y. L., Chang, Y. K., & Mokhtar, I. A. (2011).
Adopting evidence-based practice in clinical decision making: nurses' perceptions,
knowledge, and barriers. Journal of the Medical Library Association: JMLA, 99(3),
229.
Rice, M. (2011). Evidence-Based Practice Principles: Using the Highest Level When
Evidence Is Limited. Retrieved 28 August 2019, from
https://journals.sagepub.com/doi/abs/10.1177/1078390311426289?journalCode=japa
Rycroft-Malone, J., & Bucknall, T. (Eds.). (2011). Models and frameworks for implementing
evidence-based practice: linking evidence to action (Vol. 2). John Wiley & Sons.
EVIDENCE-BASED TREATMENT
References
Bergendal, A., Schiöler, H., Wettermark, B., & Björkstén, K. S. (2015). Concomitant use of
two or more antipsychotic drugs is every day in Sweden. Therapeutic advances in
psychopharmacology, 5(4), 224-231.
Greenhalgh, T., Howick, J., & Maskrey, N. (2014). Evidence based medicine: a movement in
crisis?. Bmj, 348, g3725.
LoBiondo-Wood, G., & Haber, J. (2017). Nursing research-E-book: methods and critical
appraisal for evidence-based practice. Elsevier Health Sciences.
Mathieson, A., Grande, G., & Luker, K. (2018). Strategies, facilitators and barriers to
implementation of evidence-based practice in community nursing: a systematic
mixed-studies review and qualitative synthesis. Primary health care research &
development, 20.
Majid, S., Foo, S., Luyt, B., Zhang, X., Theng, Y. L., Chang, Y. K., & Mokhtar, I. A. (2011).
Adopting evidence-based practice in clinical decision making: nurses' perceptions,
knowledge, and barriers. Journal of the Medical Library Association: JMLA, 99(3),
229.
Rice, M. (2011). Evidence-Based Practice Principles: Using the Highest Level When
Evidence Is Limited. Retrieved 28 August 2019, from
https://journals.sagepub.com/doi/abs/10.1177/1078390311426289?journalCode=japa
Rycroft-Malone, J., & Bucknall, T. (Eds.). (2011). Models and frameworks for implementing
evidence-based practice: linking evidence to action (Vol. 2). John Wiley & Sons.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
EVIDENCE-BASED TREATMENT
Siminoff, L. A. (2013, December). Incorporating patient and family preferences into
evidence-based medicine. In BMC medical informatics and decision making (Vol. 13,
No. 3, p. S6). BioMed Central.
Solomons, N. M., & Spross, J. A. (2011). Evidence‐based practice barriers and facilitators
from a continuous quality improvement perspective: an integrative review. Journal of
nursing management, 19(1), 109-120.
Tiihonen, J., Taipale, H., Mehtälä, J., Vattulainen, P., Correll, C. U., & Tanskanen, A. (2019).
Association of Antipsychotic Polypharmacy vs Monotherapy With Psychiatric
Rehospitalization Among Adults With Schizophrenia. JAMA psychiatry, 76(5), 499-
507.
EVIDENCE-BASED TREATMENT
Siminoff, L. A. (2013, December). Incorporating patient and family preferences into
evidence-based medicine. In BMC medical informatics and decision making (Vol. 13,
No. 3, p. S6). BioMed Central.
Solomons, N. M., & Spross, J. A. (2011). Evidence‐based practice barriers and facilitators
from a continuous quality improvement perspective: an integrative review. Journal of
nursing management, 19(1), 109-120.
Tiihonen, J., Taipale, H., Mehtälä, J., Vattulainen, P., Correll, C. U., & Tanskanen, A. (2019).
Association of Antipsychotic Polypharmacy vs Monotherapy With Psychiatric
Rehospitalization Among Adults With Schizophrenia. JAMA psychiatry, 76(5), 499-
507.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





