Evidence-Based Practice Report: Hypertension Management in Australia
VerifiedAdded on 2022/11/01
|18
|3569
|82
Report
AI Summary
This report delves into the evidence-based practice of hypertension management, a prevalent chronic clinical issue in Australia. The assignment, based on the PICO framework, investigates guidelines and recommendations for managing hypertension, addressing the rising rates of mortality and morbidity associated with the condition. It synthesizes findings from various research articles, including studies on home blood pressure monitoring, guidelines for adult hypertension management, and nursing practices in Australia. The report identifies key interventions such as blood pressure measurement techniques (clinical, ambulatory, and home monitoring) and drug therapies. It provides recommendations and guidelines for healthcare professionals and individuals, emphasizing the importance of regular blood pressure monitoring, lifestyle modifications, and appropriate medication. The report also highlights the need for updated guidelines and the significance of considering the patient's state of mind during blood pressure readings, advocating for the use of home monitoring for accurate assessments. The report concludes by emphasizing the evolving nature of hypertension treatment and the importance of continued research and updated practices to improve patient outcomes.

Running head: EVIDENCE BASED PRACTICE IN NURSING 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EVIDENCE BASED PRACTICE IN NURSING 2
PART-1: Evidence Search
Identification and Discussion
The chronic clinical issue prevalent in Australians is Hypertension which is a clinical term for
high blood pressure over a prolonged time. It is said that every one in ten Australians have
been reported to have hypertension which was stable over a decade.
The frequency of hypertensive people has amplified in Australian due to their habits and
lifestyle. The continuous increase in hypertensive people are elevating the rate of mortality
and morbidity in Australia. This is because prolonged high in blood pressure can lead to
serious health issues like heart attack, stroke, heart failure and kidney disease.
Researchable questions based on PICO
The PICO format suggests; Problem of the patient is dealing with hypertension; Intervention
or therapeutic measures taken by the health care for recording the blood pressure at a regular
basis.; Comparison or Controlled drug usage to prevent the elevated blood pressure;
Outcomes not being favourable as people needs to find the correct medication suitable for its
disease.
Thus, based upon the PICO format the research question which has been framed is that, what
are the guidelines to manage hypertension and some recommendations to improve the
managing techniques.
PART-1: Evidence Search
Identification and Discussion
The chronic clinical issue prevalent in Australians is Hypertension which is a clinical term for
high blood pressure over a prolonged time. It is said that every one in ten Australians have
been reported to have hypertension which was stable over a decade.
The frequency of hypertensive people has amplified in Australian due to their habits and
lifestyle. The continuous increase in hypertensive people are elevating the rate of mortality
and morbidity in Australia. This is because prolonged high in blood pressure can lead to
serious health issues like heart attack, stroke, heart failure and kidney disease.
Researchable questions based on PICO
The PICO format suggests; Problem of the patient is dealing with hypertension; Intervention
or therapeutic measures taken by the health care for recording the blood pressure at a regular
basis.; Comparison or Controlled drug usage to prevent the elevated blood pressure;
Outcomes not being favourable as people needs to find the correct medication suitable for its
disease.
Thus, based upon the PICO format the research question which has been framed is that, what
are the guidelines to manage hypertension and some recommendations to improve the
managing techniques.

EVIDENCE BASED PRACTICE IN NURSING 3
Researched articles and justifications
Researched articles and justifications
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EVIDENCE BASED PRACTICE IN NURSING 4
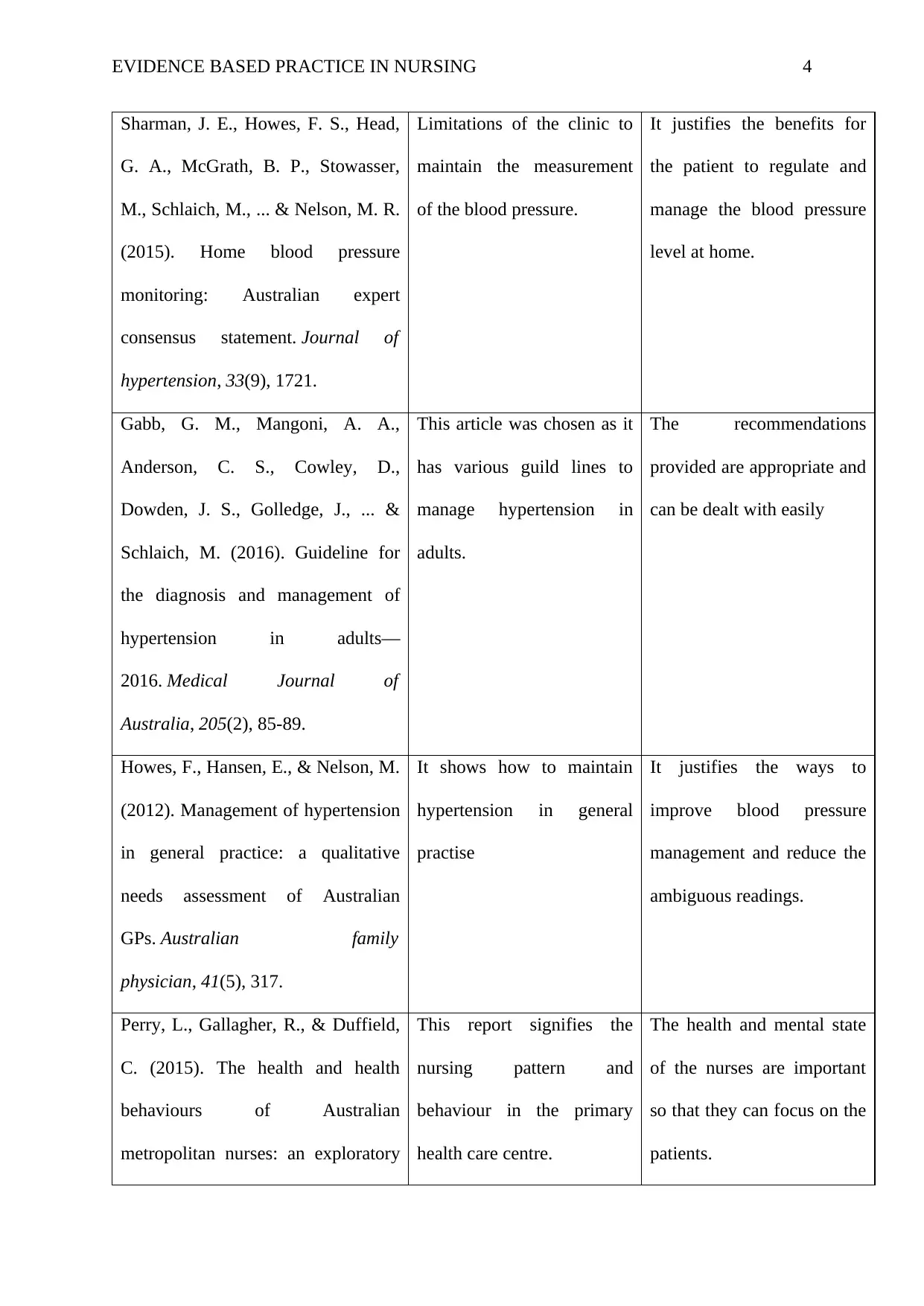
Sharman, J. E., Howes, F. S., Head,
G. A., McGrath, B. P., Stowasser,
M., Schlaich, M., ... & Nelson, M. R.
(2015). Home blood pressure
monitoring: Australian expert
consensus statement. Journal of
hypertension, 33(9), 1721.
Limitations of the clinic to
maintain the measurement
of the blood pressure.
It justifies the benefits for
the patient to regulate and
manage the blood pressure
level at home.
Gabb, G. M., Mangoni, A. A.,
Anderson, C. S., Cowley, D.,
Dowden, J. S., Golledge, J., ... &
Schlaich, M. (2016). Guideline for
the diagnosis and management of
hypertension in adults—
2016. Medical Journal of
Australia, 205(2), 85-89.
This article was chosen as it
has various guild lines to
manage hypertension in
adults.
The recommendations
provided are appropriate and
can be dealt with easily
Howes, F., Hansen, E., & Nelson, M.
(2012). Management of hypertension
in general practice: a qualitative
needs assessment of Australian
GPs. Australian family
physician, 41(5), 317.
It shows how to maintain
hypertension in general
practise
It justifies the ways to
improve blood pressure
management and reduce the
ambiguous readings.
Perry, L., Gallagher, R., & Duffield,
C. (2015). The health and health
behaviours of Australian
metropolitan nurses: an exploratory
This report signifies the
nursing pattern and
behaviour in the primary
health care centre.
The health and mental state
of the nurses are important
so that they can focus on the
patients.
Sharman, J. E., Howes, F. S., Head,
G. A., McGrath, B. P., Stowasser,
M., Schlaich, M., ... & Nelson, M. R.
(2015). Home blood pressure
monitoring: Australian expert
consensus statement. Journal of
hypertension, 33(9), 1721.
Limitations of the clinic to
maintain the measurement
of the blood pressure.
It justifies the benefits for
the patient to regulate and
manage the blood pressure
level at home.
Gabb, G. M., Mangoni, A. A.,
Anderson, C. S., Cowley, D.,
Dowden, J. S., Golledge, J., ... &
Schlaich, M. (2016). Guideline for
the diagnosis and management of
hypertension in adults—
2016. Medical Journal of
Australia, 205(2), 85-89.
This article was chosen as it
has various guild lines to
manage hypertension in
adults.
The recommendations
provided are appropriate and
can be dealt with easily
Howes, F., Hansen, E., & Nelson, M.
(2012). Management of hypertension
in general practice: a qualitative
needs assessment of Australian
GPs. Australian family
physician, 41(5), 317.
It shows how to maintain
hypertension in general
practise
It justifies the ways to
improve blood pressure
management and reduce the
ambiguous readings.
Perry, L., Gallagher, R., & Duffield,
C. (2015). The health and health
behaviours of Australian
metropolitan nurses: an exploratory
This report signifies the
nursing pattern and
behaviour in the primary
health care centre.
The health and mental state
of the nurses are important
so that they can focus on the
patients.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EVIDENCE BASED PRACTICE IN NURSING 5
study. BMC nursing, 14(1), 45.
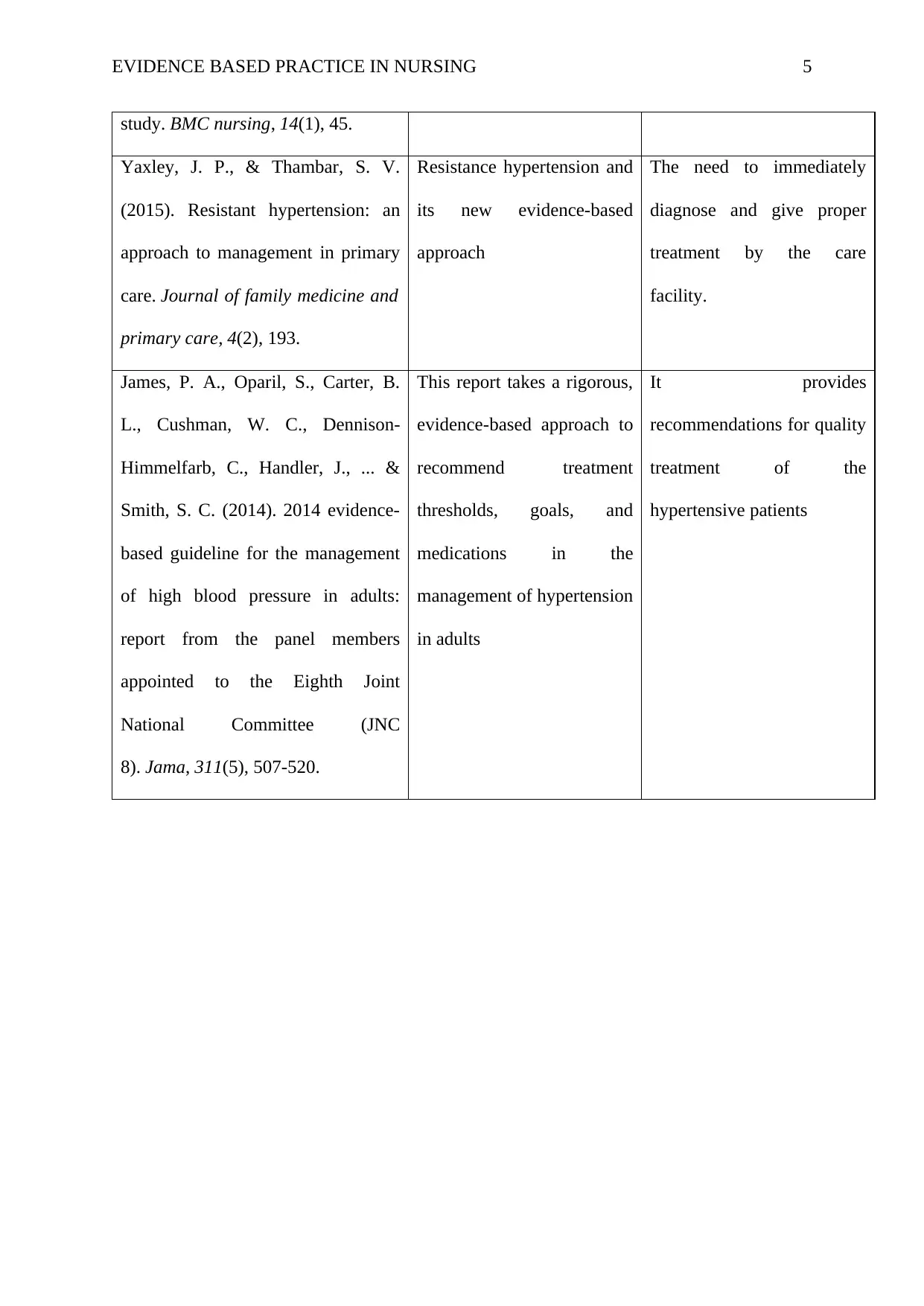
Yaxley, J. P., & Thambar, S. V.
(2015). Resistant hypertension: an
approach to management in primary
care. Journal of family medicine and
primary care, 4(2), 193.
Resistance hypertension and
its new evidence-based
approach
The need to immediately
diagnose and give proper
treatment by the care
facility.
James, P. A., Oparil, S., Carter, B.
L., Cushman, W. C., Dennison-
Himmelfarb, C., Handler, J., ... &
Smith, S. C. (2014). 2014 evidence-
based guideline for the management
of high blood pressure in adults:
report from the panel members
appointed to the Eighth Joint
National Committee (JNC
8). Jama, 311(5), 507-520.
This report takes a rigorous,
evidence-based approach to
recommend treatment
thresholds, goals, and
medications in the
management of hypertension
in adults
It provides
recommendations for quality
treatment of the
hypertensive patients
study. BMC nursing, 14(1), 45.
Yaxley, J. P., & Thambar, S. V.
(2015). Resistant hypertension: an
approach to management in primary
care. Journal of family medicine and
primary care, 4(2), 193.
Resistance hypertension and
its new evidence-based
approach
The need to immediately
diagnose and give proper
treatment by the care
facility.
James, P. A., Oparil, S., Carter, B.
L., Cushman, W. C., Dennison-
Himmelfarb, C., Handler, J., ... &
Smith, S. C. (2014). 2014 evidence-
based guideline for the management
of high blood pressure in adults:
report from the panel members
appointed to the Eighth Joint
National Committee (JNC
8). Jama, 311(5), 507-520.
This report takes a rigorous,
evidence-based approach to
recommend treatment
thresholds, goals, and
medications in the
management of hypertension
in adults
It provides
recommendations for quality
treatment of the
hypertensive patients
EVIDENCE BASED PRACTICE IN NURSING 6
PART-11
Evidence Report and Recommendations
Introduction
Hypertension or high blood pressure is the most common disease in Australia that affects the
heart and the blood vessels. The warning signs are rare in high blood pressure; thus, the
people should regularly measure their blood pressure in order to be vigilant (Howes et.al
2012). Family history, genetics, old age are common unavoidable factors for high blood
pressure. But lifestyle of the Australians such as increase in smoking and alcohol
consumption, lack of physical exercise, obesity, salty diet, and stress resulting in sleep
apnoea have strong influence on the blood pressure on an individual. If not treated or
managed in the correct time, hypertension can lead to hardening of arterial walls known as
atherosclerosis or heart stroke, kidney failure or failure of heart.
Synthesis
In spite a solid evidence from various journals and research that there are numerous benefits
of monitoring hypertension and many available guidelines provided to achieve this goal. But
it is still a national challenge to control the raised blood pressure at a population level.
According to Sharman et al (2015) a protocol should be conducted by the doctors or nursing
staff for the patient or carer on how to assess blood pressure at home. In his article Gabb,
Mangoni, Anderson et.al (2016) discusses about various techniques and guidelines to manage
blood pressure. It suggests tremendous recommendations for the patients on taking
appropriate medication to lower the pressure. Four main themes were introduced in Howes,
Hansen, & Nelson (2012) research about the uncertain measurement of BP, achieving
harmony in the practise, cooperating with the patient’s alteration and addressing the barriers
in the system.
PART-11
Evidence Report and Recommendations
Introduction
Hypertension or high blood pressure is the most common disease in Australia that affects the
heart and the blood vessels. The warning signs are rare in high blood pressure; thus, the
people should regularly measure their blood pressure in order to be vigilant (Howes et.al
2012). Family history, genetics, old age are common unavoidable factors for high blood
pressure. But lifestyle of the Australians such as increase in smoking and alcohol
consumption, lack of physical exercise, obesity, salty diet, and stress resulting in sleep
apnoea have strong influence on the blood pressure on an individual. If not treated or
managed in the correct time, hypertension can lead to hardening of arterial walls known as
atherosclerosis or heart stroke, kidney failure or failure of heart.
Synthesis
In spite a solid evidence from various journals and research that there are numerous benefits
of monitoring hypertension and many available guidelines provided to achieve this goal. But
it is still a national challenge to control the raised blood pressure at a population level.
According to Sharman et al (2015) a protocol should be conducted by the doctors or nursing
staff for the patient or carer on how to assess blood pressure at home. In his article Gabb,
Mangoni, Anderson et.al (2016) discusses about various techniques and guidelines to manage
blood pressure. It suggests tremendous recommendations for the patients on taking
appropriate medication to lower the pressure. Four main themes were introduced in Howes,
Hansen, & Nelson (2012) research about the uncertain measurement of BP, achieving
harmony in the practise, cooperating with the patient’s alteration and addressing the barriers
in the system.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EVIDENCE BASED PRACTICE IN NURSING 7
Identification
The PICO question which was framed was, what are the guidelines to manage hypertension
and some recommendations to improve the managing techniques.
Thus, the question is being answered by giving some appropriate guidelines and managing
techniques used by the healthcare facility in dealing with hypertensive patients. The first
intervention or managing techniques used to manage hypertension is blood pressure
measurement (James, Oparil, Carter, Cushman et.al 2014). A complete assessment of blood
pressure based on multiple measurements on a regular basis is necessary. There is various
method available to measure the BP each providing dissimilar but useful information. The
methods used are clinical BP, ambulatory of twenty-four hour and monitoring of BP at home.
Most medical studies demonstrate that the use of clinical BP is very efficient and has various
benefits for treating hypertension. All the above-mentioned ways to measure BP predict risk
of heart events.
Automated office BP measurement comprises of taking constant measurements by means of
a mechanical device without the clinician present in the room. This procedure usually results
in lower analyses than conventional clinical BP device. The British Hypertension Society
delivers a list of authenticated BP monitoring devices. Use of legalized and frequently
sustained non-mercury devices or mercury sphygmomanometers are phased out for
professional health and protection for environmental reasons (Howes et.al 2012).
There has been drug therapy initiation by the health-care centres. A person diagnosed with
mild hypertension if given a drug treatment can reduce cardiovascular effects and decrease
the chances of stroke. It will also lead to lowering of cardiovascular death and reduction in
mortality rate. But the decision to state the drug treatment at an initial level of hypertension is
a very risky move as it can lead to damaging of various organs concluding to death.
Identification
The PICO question which was framed was, what are the guidelines to manage hypertension
and some recommendations to improve the managing techniques.
Thus, the question is being answered by giving some appropriate guidelines and managing
techniques used by the healthcare facility in dealing with hypertensive patients. The first
intervention or managing techniques used to manage hypertension is blood pressure
measurement (James, Oparil, Carter, Cushman et.al 2014). A complete assessment of blood
pressure based on multiple measurements on a regular basis is necessary. There is various
method available to measure the BP each providing dissimilar but useful information. The
methods used are clinical BP, ambulatory of twenty-four hour and monitoring of BP at home.
Most medical studies demonstrate that the use of clinical BP is very efficient and has various
benefits for treating hypertension. All the above-mentioned ways to measure BP predict risk
of heart events.
Automated office BP measurement comprises of taking constant measurements by means of
a mechanical device without the clinician present in the room. This procedure usually results
in lower analyses than conventional clinical BP device. The British Hypertension Society
delivers a list of authenticated BP monitoring devices. Use of legalized and frequently
sustained non-mercury devices or mercury sphygmomanometers are phased out for
professional health and protection for environmental reasons (Howes et.al 2012).
There has been drug therapy initiation by the health-care centres. A person diagnosed with
mild hypertension if given a drug treatment can reduce cardiovascular effects and decrease
the chances of stroke. It will also lead to lowering of cardiovascular death and reduction in
mortality rate. But the decision to state the drug treatment at an initial level of hypertension is
a very risky move as it can lead to damaging of various organs concluding to death.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EVIDENCE BASED PRACTICE IN NURSING 8
optimal blood pressure treatment was extensively debatable and it has shown to be beneficial
amongst the patients with high cardiovascular risk. The age is also a common cause for
hypertension as it is shown to be a common disease amongst the elderly’s in Australia. The
Systolic Blood Pressure Intervention Trial inspected that most of the people over 50 years of
age is said to have cardiovascular disease initially. Many of them had mild or low
cardiovascular events or mild renal impairment or were on blood pressure lowering therapy
(James, Oparil, Carter, Cushman et.al 2014).
Recommendation and guidelines
New recommendations and guidelines are provided to insure the improvement of treatment
for hypertension among the people. The healthcare professionals and the individual needs to
follow the guidelines in order to reduce the risk of death caused by high blood pressure. The
hospital should manage the patient diagnosed with hypertension with a strategized
management plan (Gabb, et.al. 2016). The treatment strategies should be different for
different individual at extreme risk of heart events to those at minimum risk of cardiovascular
disease. If the individual is detected with mild hypertension they should be provided with
blood-pressure lowering therapy or antihypertensive therapy instead of hard medication. A
healthy lifestyle should be encouraged by the doctors including quitting smoking and
drinking, a balanced and nutritious diet and proper body movement and regular exercise for
all Australians. If the patient is diagnosed with hypertension he should be treated until he
reached the required blood pressure rate. An intense treatment should be considered and
offered to the high cardiovascular risk population to regulate their blood pressure. But if the
treatment it started, the patient has to watched and monitored every hour. This close-follow-
up is required so that the nursing staff can analyse if there are any problems caused by the
optimal blood pressure treatment was extensively debatable and it has shown to be beneficial
amongst the patients with high cardiovascular risk. The age is also a common cause for
hypertension as it is shown to be a common disease amongst the elderly’s in Australia. The
Systolic Blood Pressure Intervention Trial inspected that most of the people over 50 years of
age is said to have cardiovascular disease initially. Many of them had mild or low
cardiovascular events or mild renal impairment or were on blood pressure lowering therapy
(James, Oparil, Carter, Cushman et.al 2014).
Recommendation and guidelines
New recommendations and guidelines are provided to insure the improvement of treatment
for hypertension among the people. The healthcare professionals and the individual needs to
follow the guidelines in order to reduce the risk of death caused by high blood pressure. The
hospital should manage the patient diagnosed with hypertension with a strategized
management plan (Gabb, et.al. 2016). The treatment strategies should be different for
different individual at extreme risk of heart events to those at minimum risk of cardiovascular
disease. If the individual is detected with mild hypertension they should be provided with
blood-pressure lowering therapy or antihypertensive therapy instead of hard medication. A
healthy lifestyle should be encouraged by the doctors including quitting smoking and
drinking, a balanced and nutritious diet and proper body movement and regular exercise for
all Australians. If the patient is diagnosed with hypertension he should be treated until he
reached the required blood pressure rate. An intense treatment should be considered and
offered to the high cardiovascular risk population to regulate their blood pressure. But if the
treatment it started, the patient has to watched and monitored every hour. This close-follow-
up is required so that the nursing staff can analyse if there are any problems caused by the
EVIDENCE BASED PRACTICE IN NURSING 9
treatment like hypotension, syncope, electrolyte abnormalities and acute kidney injury (Perry,
Gallagher, & Duffield, 2015).
Unless contradicted, patients diagnosed with simple hypertension ACE inhibitors or ARBs,
calcium channel blockers, and thiazide diuretics are all suitable first-line antihypertensive
drugs, either as monotherapy or in some mixtures. Beta-blockers should be discarded as a
first-line drug therapy as stability between efficacy and care is less favourable for beta-
blockers than any other first-line antihypertensive drugs. Due to increased risk of negative
effects ACE inhibitors and ARBs are not suggested in combination (Gabb, et.al. 2016) .
Recommendations to monitor the blood pressure in patients dealing with hypertension or
moderate hypertension is also been provided. If in the clinical BP hypertension is suspected,
an immediate accessibility of home monitoring should be available to confirm the level of BP
(James, Oparil, Carter, Cushman et.al 2014). Clinical BP should be used in absolute heart
risk. If in absolute cardiovascular risk home blood pressure is used, it can generate
inappropriate readings. The technique of measure BP should be followed rigorously if not an
overestimation or underestimation of result is guaranteed. Fingers or wrist BP monitoring
devices is not appropriate and hence not recommended (Sharman et.al 2015).
Thus, the article by Gabb, Mangoni, Anderson, et.al (2016). “Guideline for the diagnosis and
management of hypertension in adults — 2016” expresses the best evidence and hence
identifies the formulated PICO question. It gives appropriate managing techniques used by
the clinical institution. Its also researches about the outcome that techniques have on the
present conditions. The recommendations provided by this article is appropriate and easy to
follow. It gives a detail recommendation on how to deal with the people having high
hypertension and also low hypertensive people. the recommendations are not only for the
treatment like hypotension, syncope, electrolyte abnormalities and acute kidney injury (Perry,
Gallagher, & Duffield, 2015).
Unless contradicted, patients diagnosed with simple hypertension ACE inhibitors or ARBs,
calcium channel blockers, and thiazide diuretics are all suitable first-line antihypertensive
drugs, either as monotherapy or in some mixtures. Beta-blockers should be discarded as a
first-line drug therapy as stability between efficacy and care is less favourable for beta-
blockers than any other first-line antihypertensive drugs. Due to increased risk of negative
effects ACE inhibitors and ARBs are not suggested in combination (Gabb, et.al. 2016) .
Recommendations to monitor the blood pressure in patients dealing with hypertension or
moderate hypertension is also been provided. If in the clinical BP hypertension is suspected,
an immediate accessibility of home monitoring should be available to confirm the level of BP
(James, Oparil, Carter, Cushman et.al 2014). Clinical BP should be used in absolute heart
risk. If in absolute cardiovascular risk home blood pressure is used, it can generate
inappropriate readings. The technique of measure BP should be followed rigorously if not an
overestimation or underestimation of result is guaranteed. Fingers or wrist BP monitoring
devices is not appropriate and hence not recommended (Sharman et.al 2015).
Thus, the article by Gabb, Mangoni, Anderson, et.al (2016). “Guideline for the diagnosis and
management of hypertension in adults — 2016” expresses the best evidence and hence
identifies the formulated PICO question. It gives appropriate managing techniques used by
the clinical institution. Its also researches about the outcome that techniques have on the
present conditions. The recommendations provided by this article is appropriate and easy to
follow. It gives a detail recommendation on how to deal with the people having high
hypertension and also low hypertensive people. the recommendations are not only for the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
EVIDENCE BASED PRACTICE IN NURSING 10
health-care centre but also for the people of Australia on how to lead a life without
hypertension.
Justification and Significance
As very well known that hypertension which is the basic cause for cardiovascular disease,
thus constant researches are going on to understand this issue and come up with a valuable
and effective treatment (Gabb, et.al. 2016). Since last five years it has been seen that the
blood pressure of an individual keeps changing during the day and in specific situations such
as while eating, sleeping, exercising and crying or angry. Thus, now it is known that before
taking a reading of an individual his state of mind or situation must be taken into
consideration. So, it is recommended by Sharman et.al (2015).to offer home monitoring to
ensure that the level of BP is accurate subsequently a correct treatment will be originated.
The treatment is evolving but it still needs to evolve faster as the rate of hypertension is also
increasing leading to premature death. The National Heart Foundation of Australia is taking
initiative to up to date the clinics with the changing practices. The guidelines that will be
introduced in the future will have special addendums and will be updated from time to time
as required. It is also stated that the treating the low hypertensive individuals with the drugs
has not been established to be beneficial. It has said that people should maintain and relate
their diet as these lifestyle treatments has a potential to reduce hypertension.
health-care centre but also for the people of Australia on how to lead a life without
hypertension.
Justification and Significance
As very well known that hypertension which is the basic cause for cardiovascular disease,
thus constant researches are going on to understand this issue and come up with a valuable
and effective treatment (Gabb, et.al. 2016). Since last five years it has been seen that the
blood pressure of an individual keeps changing during the day and in specific situations such
as while eating, sleeping, exercising and crying or angry. Thus, now it is known that before
taking a reading of an individual his state of mind or situation must be taken into
consideration. So, it is recommended by Sharman et.al (2015).to offer home monitoring to
ensure that the level of BP is accurate subsequently a correct treatment will be originated.
The treatment is evolving but it still needs to evolve faster as the rate of hypertension is also
increasing leading to premature death. The National Heart Foundation of Australia is taking
initiative to up to date the clinics with the changing practices. The guidelines that will be
introduced in the future will have special addendums and will be updated from time to time
as required. It is also stated that the treating the low hypertensive individuals with the drugs
has not been established to be beneficial. It has said that people should maintain and relate
their diet as these lifestyle treatments has a potential to reduce hypertension.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
EVIDENCE BASED PRACTICE IN NURSING 11
Reference List
Sharman, J. E., Howes, F. S., Head, G. A., McGrath, B. P., Stowasser, M., Schlaich, M., ... &
Nelson, M. R. (2015). Home blood pressure monitoring: Australian expert consensus
statement. Journal of hypertension, 33(9), 1721.
Gabb, G. M., Mangoni, A. A., Anderson, C. S., Cowley, D., Dowden, J. S., Golledge, J., ... &
Schlaich, M. (2016). Guideline for the diagnosis and management of hypertension in
adults—2016. Medical Journal of Australia, 205(2), 85-89.
Howes, F., Hansen, E., & Nelson, M. (2012). Management of hypertension in general
practice: a qualitative needs assessment of Australian GPs. Australian family
physician, 41(5), 317.
Perry, L., Gallagher, R., & Duffield, C. (2015). The health and health behaviours of
Australian metropolitan nurses: an exploratory study. BMC nursing, 14(1), 45.
Yaxley, J. P., & Thambar, S. V. (2015). Resistant hypertension: an approach to management
in primary care. Journal of family medicine and primary care, 4(2), 193.
James, P. A., Oparil, S., Carter, B. L., Cushman, W. C., Dennison-Himmelfarb, C., Handler,
J., ... & Smith, S. C. (2014). 2014 evidence-based guideline for the management of
high blood pressure in adults: report from the panel members appointed to the Eighth
Joint National Committee (JNC 8). Jama, 311(5), 507-520.
Reference List
Sharman, J. E., Howes, F. S., Head, G. A., McGrath, B. P., Stowasser, M., Schlaich, M., ... &
Nelson, M. R. (2015). Home blood pressure monitoring: Australian expert consensus
statement. Journal of hypertension, 33(9), 1721.
Gabb, G. M., Mangoni, A. A., Anderson, C. S., Cowley, D., Dowden, J. S., Golledge, J., ... &
Schlaich, M. (2016). Guideline for the diagnosis and management of hypertension in
adults—2016. Medical Journal of Australia, 205(2), 85-89.
Howes, F., Hansen, E., & Nelson, M. (2012). Management of hypertension in general
practice: a qualitative needs assessment of Australian GPs. Australian family
physician, 41(5), 317.
Perry, L., Gallagher, R., & Duffield, C. (2015). The health and health behaviours of
Australian metropolitan nurses: an exploratory study. BMC nursing, 14(1), 45.
Yaxley, J. P., & Thambar, S. V. (2015). Resistant hypertension: an approach to management
in primary care. Journal of family medicine and primary care, 4(2), 193.
James, P. A., Oparil, S., Carter, B. L., Cushman, W. C., Dennison-Himmelfarb, C., Handler,
J., ... & Smith, S. C. (2014). 2014 evidence-based guideline for the management of
high blood pressure in adults: report from the panel members appointed to the Eighth
Joint National Committee (JNC 8). Jama, 311(5), 507-520.
EVIDENCE BASED PRACTICE IN NURSING 12
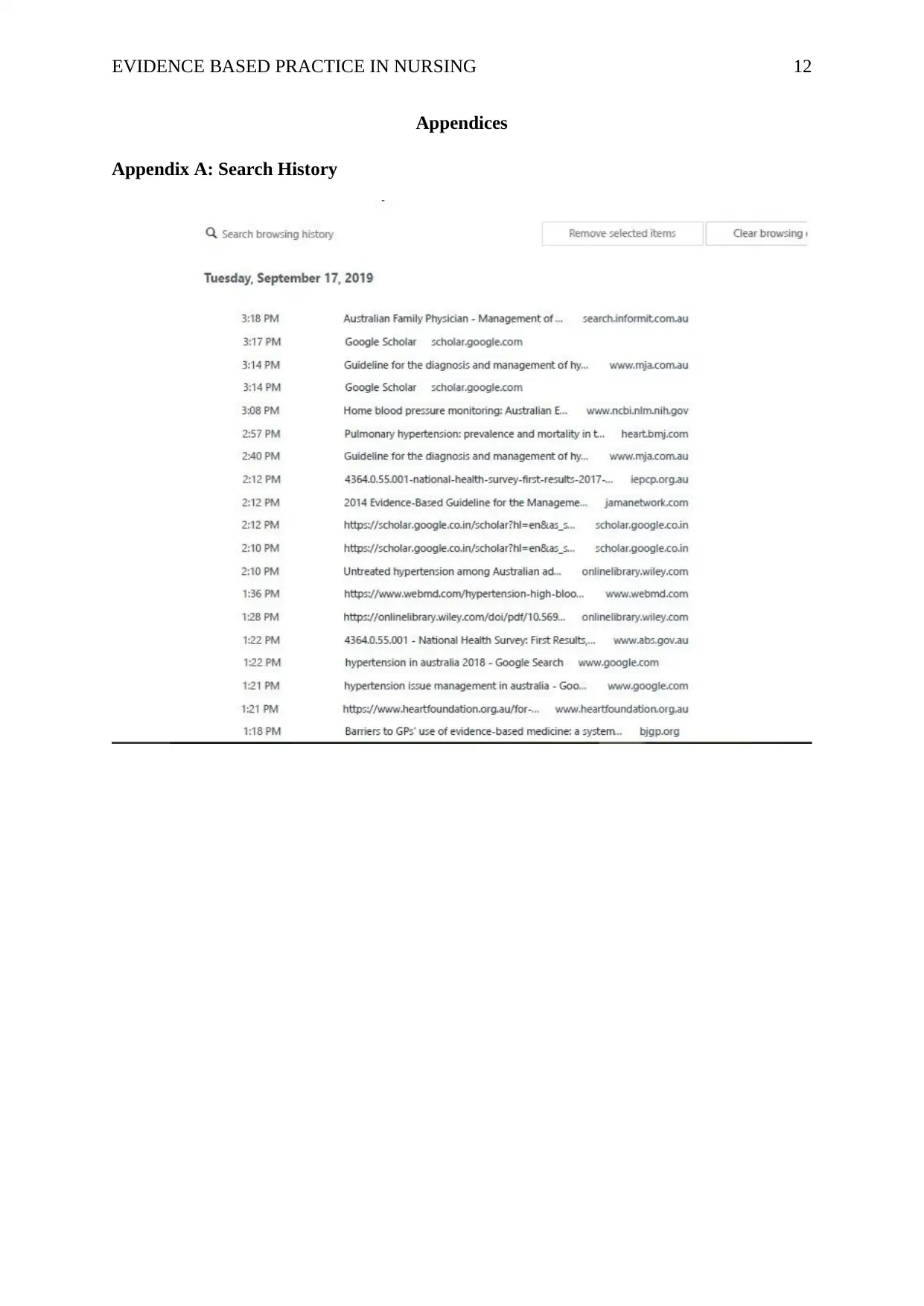
Appendices
Appendix A: Search History
Appendices
Appendix A: Search History
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





