Comprehensive Analysis of Evidence-Based Medicine Policy and Practices
VerifiedAdded on 2020/12/30
|10
|1745
|482
Report
AI Summary
This report provides a comprehensive analysis of Evidence-Based Medicine (EBM) policy, examining its core processes, major players, and the constraints imposed by the Affordable Care Act (ACA). The report begins by defining EBM and its significance in healthcare, emphasizing the integration of patient values, clinical expertise, and research evidence. It details the step-by-step process of evidence-based analysis, including assessing the patient, formulating clinical questions, acquiring and appraising evidence, applying findings, and self-evaluation. The report then identifies key players in EBM policy, such as the government, care providers, and patients, outlining their respective roles in promoting and implementing evidence-based practices. Furthermore, the report presents the levels of evidence in EBM, categorizing them based on study design and quality. Finally, the report analyzes the constraints of the ACA on EBM, highlighting how specific research types contribute to selecting best practices for quality patient care. The conclusion summarizes the key findings, reinforcing the importance of EBM in making informed healthcare decisions.
Policy Analysis
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
INTRODUCTION...........................................................................................................................1
MAIN BODY...................................................................................................................................1
Process of evidence based analysis.............................................................................................1
Major players and their roles in EBM policy..............................................................................3
EBM with levels of evidence......................................................................................................4
Analysis of the case “Constraints of the ACA on Evidence-Based Medicine”..........................5
CONCLUSION................................................................................................................................6
REFERENCES................................................................................................................................7
INTRODUCTION...........................................................................................................................1
MAIN BODY...................................................................................................................................1
Process of evidence based analysis.............................................................................................1
Major players and their roles in EBM policy..............................................................................3
EBM with levels of evidence......................................................................................................4
Analysis of the case “Constraints of the ACA on Evidence-Based Medicine”..........................5
CONCLUSION................................................................................................................................6
REFERENCES................................................................................................................................7

⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
INTRODUCTION
Evidence based medicine (EBM) refers to judicious, explicit, conscientious and
reasonable utilisation of modern & best evidence for decision making regarding care of sick
people. It integrates values of patients and clinical experience with best available research which
facilitate to increase quality of medical services (Greenhalgh, 2014). The present report will
focus on process of evidence based analysis and major players with their roles in EBM policy. It
will also include levels of evidence and constraints of ACA on evidence based medicine.
MAIN BODY
Process of evidence based analysis
Evidence based practice can be described as the integration of patient values, clinical
expertise and best research evidence in respect of making appropriate decision regarding care of
sick individual. The clinical expertise consist the knowledge level, experience and skills of
medical professionals in order to conduct medication procedures appropriately. The patient
valuers include actual requirements of sick people as per their health problems and present
situation. Moreover, the best evidence include utilisation more effective methods or tools in
order to provide correct treatment of unhealthy individual for their well-being.
Assess the patient – Initially, it is necessary to start with patient in order to ask certain
questions regarding their health problems to analyse symptoms properly (Hoffmann, Montori
and Del Mar, 2014). However, it basically consist to evaluate a clinical problem or question
which arises from the care of sick individual in respect of making them healthy.
Ask the question – Secondly, it consists to built a set of clinical question which are
related to particular case of patient including their health problem and visible symptoms
1
Evidence based medicine (EBM) refers to judicious, explicit, conscientious and
reasonable utilisation of modern & best evidence for decision making regarding care of sick
people. It integrates values of patients and clinical experience with best available research which
facilitate to increase quality of medical services (Greenhalgh, 2014). The present report will
focus on process of evidence based analysis and major players with their roles in EBM policy. It
will also include levels of evidence and constraints of ACA on evidence based medicine.
MAIN BODY
Process of evidence based analysis
Evidence based practice can be described as the integration of patient values, clinical
expertise and best research evidence in respect of making appropriate decision regarding care of
sick individual. The clinical expertise consist the knowledge level, experience and skills of
medical professionals in order to conduct medication procedures appropriately. The patient
valuers include actual requirements of sick people as per their health problems and present
situation. Moreover, the best evidence include utilisation more effective methods or tools in
order to provide correct treatment of unhealthy individual for their well-being.
Assess the patient – Initially, it is necessary to start with patient in order to ask certain
questions regarding their health problems to analyse symptoms properly (Hoffmann, Montori
and Del Mar, 2014). However, it basically consist to evaluate a clinical problem or question
which arises from the care of sick individual in respect of making them healthy.
Ask the question – Secondly, it consists to built a set of clinical question which are
related to particular case of patient including their health problem and visible symptoms
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
accordingly. Along with this, it is necessary build questions through focussing on patient care
regarding their health issue accordingly.
Acquire the evidence – Thirdly, this include to carrying out an investigation by selecting
appropriate resources in order to analyse actual information which helps to conduct correct
treatment process regarding care of sick individual (Sadeghi‐Bazargani, Tabrizi and Azami‐
Aghdash, 2014). It is significant to conduct proper investigation before providing accurate
medication to patient for their well being. Moreover, few of resources such as case reports,
observational studies, randomised controlled trials, systematic reviews etc. can be used for the
research.
Appraise the evidence – Moreover, the appraising of evidence by analysing strengths
and weaknesses of different study reports in respect of several key questions. However, these
questions involve the validity of research, results of specific study and impact of that study to
provide care & looking after the patients.
Apply on patient – Additionally, after evaluating and examining overall evidences
which are relevant, it is essential to implement desired medication procedure in respect of
making them disease free properly. It is very important to carefully take actions for providing
accurate treatment to improve experience of sick individual in terms of making them healthy (Ilic
and Maloney, 2014).
Self evaluation – Finally, it is beneficial to conduct a self evaluation in context analysing
own performance of providing proper medication to patient which facilitate to determine
mistakes or gain assurance about care. It is helpful to gain assurance for better outcomes and
make perfection in clinical practices for attaining benefits in future.
2
regarding their health issue accordingly.
Acquire the evidence – Thirdly, this include to carrying out an investigation by selecting
appropriate resources in order to analyse actual information which helps to conduct correct
treatment process regarding care of sick individual (Sadeghi‐Bazargani, Tabrizi and Azami‐
Aghdash, 2014). It is significant to conduct proper investigation before providing accurate
medication to patient for their well being. Moreover, few of resources such as case reports,
observational studies, randomised controlled trials, systematic reviews etc. can be used for the
research.
Appraise the evidence – Moreover, the appraising of evidence by analysing strengths
and weaknesses of different study reports in respect of several key questions. However, these
questions involve the validity of research, results of specific study and impact of that study to
provide care & looking after the patients.
Apply on patient – Additionally, after evaluating and examining overall evidences
which are relevant, it is essential to implement desired medication procedure in respect of
making them disease free properly. It is very important to carefully take actions for providing
accurate treatment to improve experience of sick individual in terms of making them healthy (Ilic
and Maloney, 2014).
Self evaluation – Finally, it is beneficial to conduct a self evaluation in context analysing
own performance of providing proper medication to patient which facilitate to determine
mistakes or gain assurance about care. It is helpful to gain assurance for better outcomes and
make perfection in clinical practices for attaining benefits in future.
2
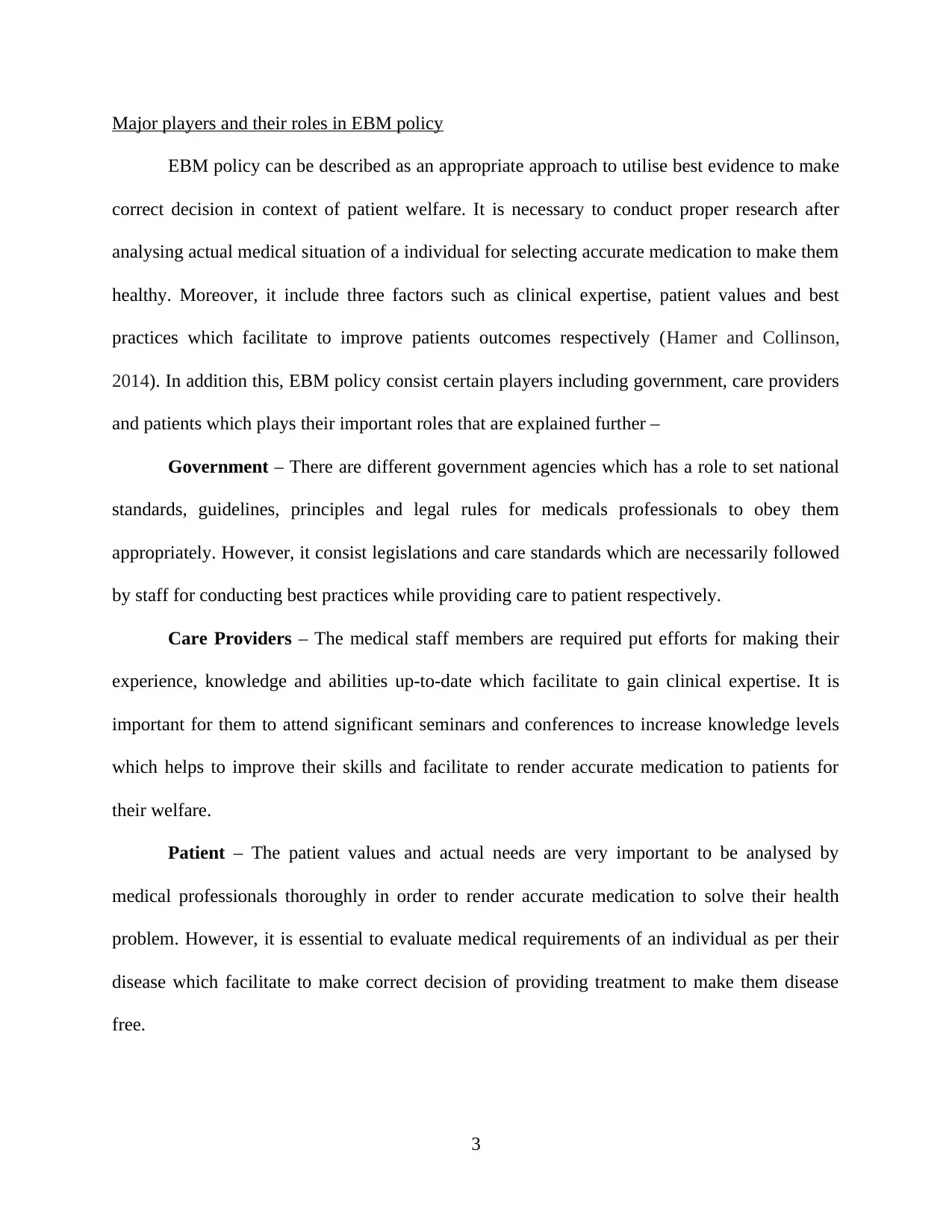
Major players and their roles in EBM policy
EBM policy can be described as an appropriate approach to utilise best evidence to make
correct decision in context of patient welfare. It is necessary to conduct proper research after
analysing actual medical situation of a individual for selecting accurate medication to make them
healthy. Moreover, it include three factors such as clinical expertise, patient values and best
practices which facilitate to improve patients outcomes respectively (Hamer and Collinson,
2014). In addition this, EBM policy consist certain players including government, care providers
and patients which plays their important roles that are explained further –
Government – There are different government agencies which has a role to set national
standards, guidelines, principles and legal rules for medicals professionals to obey them
appropriately. However, it consist legislations and care standards which are necessarily followed
by staff for conducting best practices while providing care to patient respectively.
Care Providers – The medical staff members are required put efforts for making their
experience, knowledge and abilities up-to-date which facilitate to gain clinical expertise. It is
important for them to attend significant seminars and conferences to increase knowledge levels
which helps to improve their skills and facilitate to render accurate medication to patients for
their welfare.
Patient – The patient values and actual needs are very important to be analysed by
medical professionals thoroughly in order to render accurate medication to solve their health
problem. However, it is essential to evaluate medical requirements of an individual as per their
disease which facilitate to make correct decision of providing treatment to make them disease
free.
3
EBM policy can be described as an appropriate approach to utilise best evidence to make
correct decision in context of patient welfare. It is necessary to conduct proper research after
analysing actual medical situation of a individual for selecting accurate medication to make them
healthy. Moreover, it include three factors such as clinical expertise, patient values and best
practices which facilitate to improve patients outcomes respectively (Hamer and Collinson,
2014). In addition this, EBM policy consist certain players including government, care providers
and patients which plays their important roles that are explained further –
Government – There are different government agencies which has a role to set national
standards, guidelines, principles and legal rules for medicals professionals to obey them
appropriately. However, it consist legislations and care standards which are necessarily followed
by staff for conducting best practices while providing care to patient respectively.
Care Providers – The medical staff members are required put efforts for making their
experience, knowledge and abilities up-to-date which facilitate to gain clinical expertise. It is
important for them to attend significant seminars and conferences to increase knowledge levels
which helps to improve their skills and facilitate to render accurate medication to patients for
their welfare.
Patient – The patient values and actual needs are very important to be analysed by
medical professionals thoroughly in order to render accurate medication to solve their health
problem. However, it is essential to evaluate medical requirements of an individual as per their
disease which facilitate to make correct decision of providing treatment to make them disease
free.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
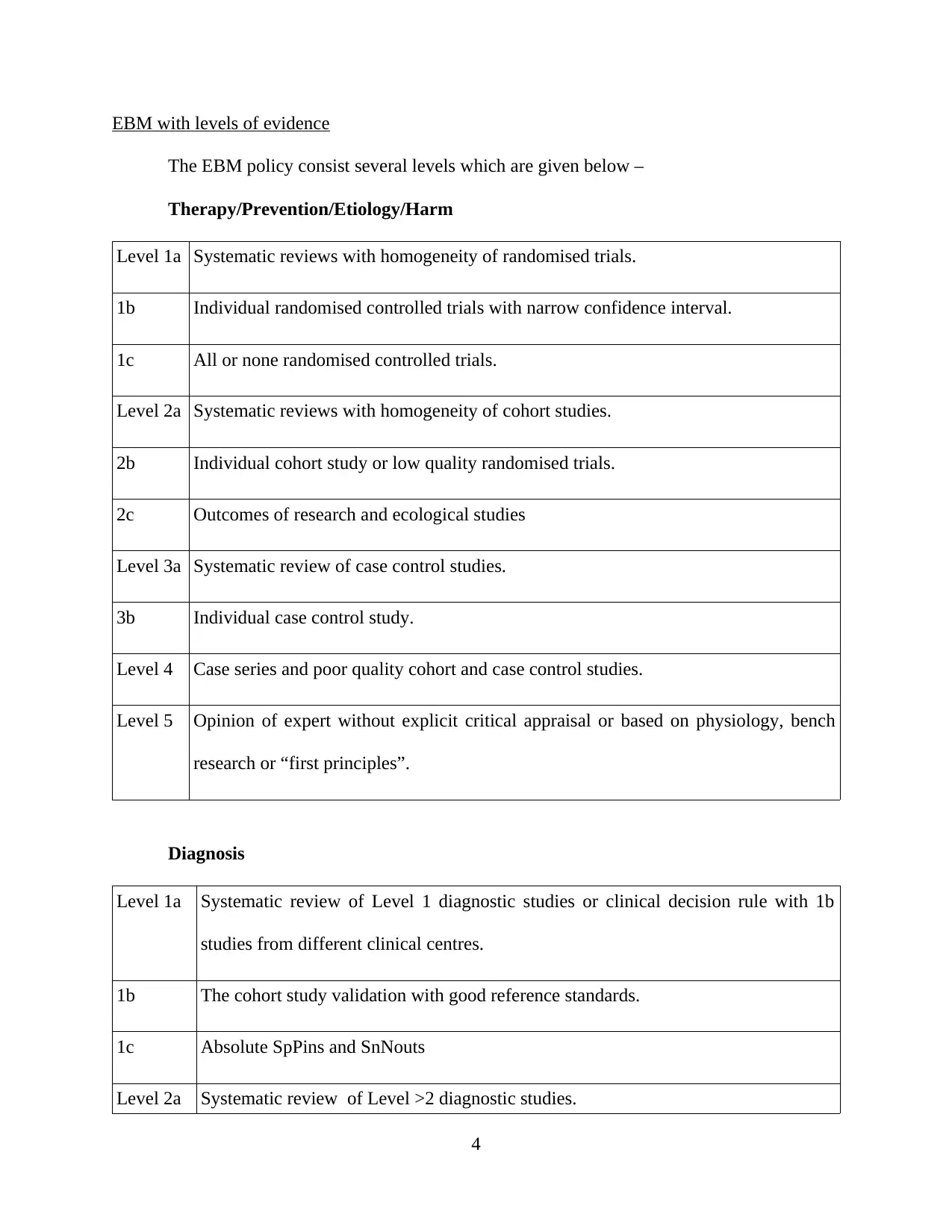
EBM with levels of evidence
The EBM policy consist several levels which are given below –
Therapy/Prevention/Etiology/Harm
Level 1a Systematic reviews with homogeneity of randomised trials.
1b Individual randomised controlled trials with narrow confidence interval.
1c All or none randomised controlled trials.
Level 2a Systematic reviews with homogeneity of cohort studies.
2b Individual cohort study or low quality randomised trials.
2c Outcomes of research and ecological studies
Level 3a Systematic review of case control studies.
3b Individual case control study.
Level 4 Case series and poor quality cohort and case control studies.
Level 5 Opinion of expert without explicit critical appraisal or based on physiology, bench
research or “first principles”.
Diagnosis
Level 1a Systematic review of Level 1 diagnostic studies or clinical decision rule with 1b
studies from different clinical centres.
1b The cohort study validation with good reference standards.
1c Absolute SpPins and SnNouts
Level 2a Systematic review of Level >2 diagnostic studies.
4
The EBM policy consist several levels which are given below –
Therapy/Prevention/Etiology/Harm
Level 1a Systematic reviews with homogeneity of randomised trials.
1b Individual randomised controlled trials with narrow confidence interval.
1c All or none randomised controlled trials.
Level 2a Systematic reviews with homogeneity of cohort studies.
2b Individual cohort study or low quality randomised trials.
2c Outcomes of research and ecological studies
Level 3a Systematic review of case control studies.
3b Individual case control study.
Level 4 Case series and poor quality cohort and case control studies.
Level 5 Opinion of expert without explicit critical appraisal or based on physiology, bench
research or “first principles”.
Diagnosis
Level 1a Systematic review of Level 1 diagnostic studies or clinical decision rule with 1b
studies from different clinical centres.
1b The cohort study validation with good reference standards.
1c Absolute SpPins and SnNouts
Level 2a Systematic review of Level >2 diagnostic studies.
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
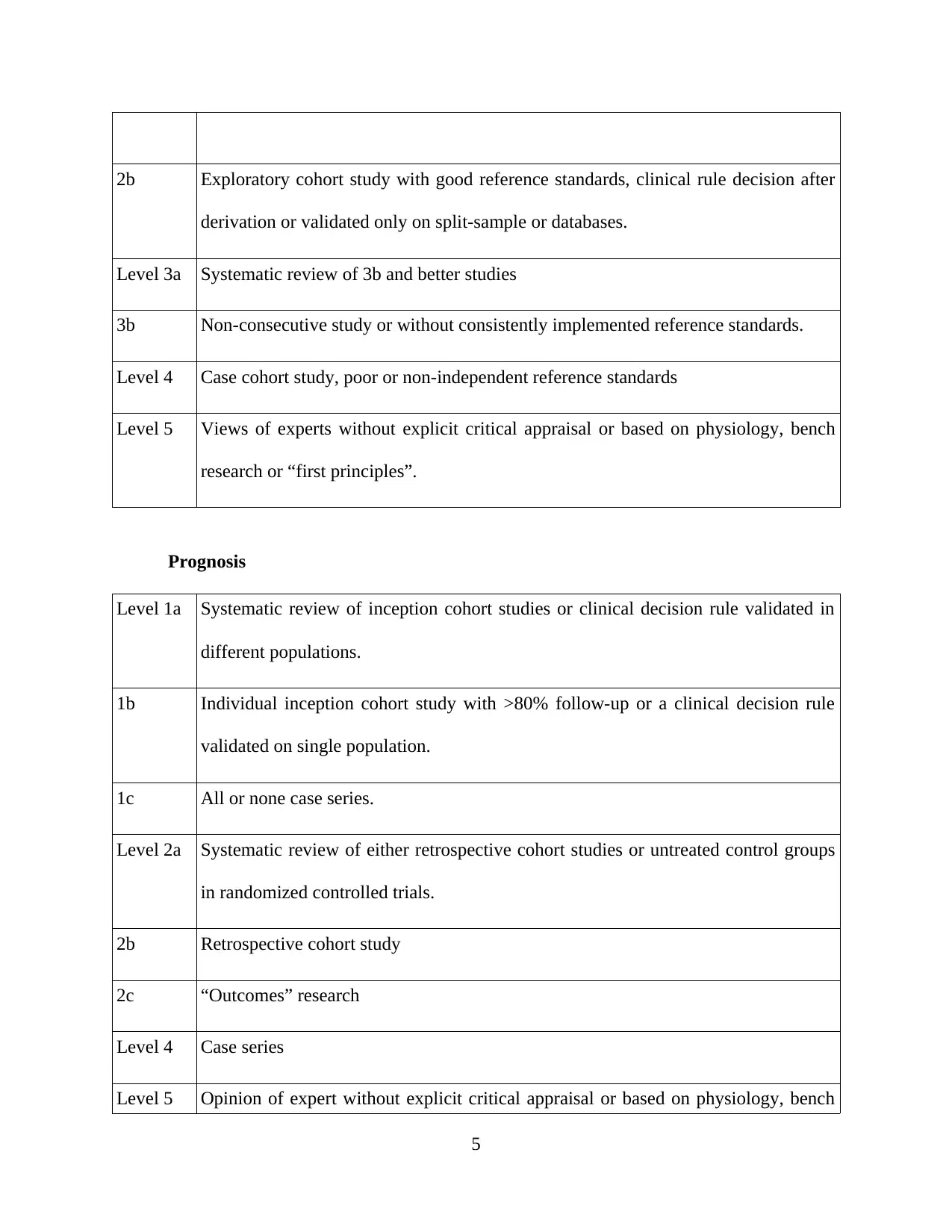
2b Exploratory cohort study with good reference standards, clinical rule decision after
derivation or validated only on split-sample or databases.
Level 3a Systematic review of 3b and better studies
3b Non-consecutive study or without consistently implemented reference standards.
Level 4 Case cohort study, poor or non-independent reference standards
Level 5 Views of experts without explicit critical appraisal or based on physiology, bench
research or “first principles”.
Prognosis
Level 1a Systematic review of inception cohort studies or clinical decision rule validated in
different populations.
1b Individual inception cohort study with >80% follow-up or a clinical decision rule
validated on single population.
1c All or none case series.
Level 2a Systematic review of either retrospective cohort studies or untreated control groups
in randomized controlled trials.
2b Retrospective cohort study
2c “Outcomes” research
Level 4 Case series
Level 5 Opinion of expert without explicit critical appraisal or based on physiology, bench
5
derivation or validated only on split-sample or databases.
Level 3a Systematic review of 3b and better studies
3b Non-consecutive study or without consistently implemented reference standards.
Level 4 Case cohort study, poor or non-independent reference standards
Level 5 Views of experts without explicit critical appraisal or based on physiology, bench
research or “first principles”.
Prognosis
Level 1a Systematic review of inception cohort studies or clinical decision rule validated in
different populations.
1b Individual inception cohort study with >80% follow-up or a clinical decision rule
validated on single population.
1c All or none case series.
Level 2a Systematic review of either retrospective cohort studies or untreated control groups
in randomized controlled trials.
2b Retrospective cohort study
2c “Outcomes” research
Level 4 Case series
Level 5 Opinion of expert without explicit critical appraisal or based on physiology, bench
5
research or “first principles”.
Analysis of the case “Constraints of the ACA on Evidence-Based Medicine”
The constraints of ACA on evidence base medicines add specific information about types
of research which helps to investigate properly to select best practices in context of providing
care an individual with better quality of services. It is beneficial to consider the levels of EBM
policy related to therapy/prevention/harm, diagnosis and prognosis in order to render accurate
medical services to make patient well-being (Malanga and Mautner, 2016). Moreover, according
to grades of recommendations, the quality of evidence factors like high, moderate, low and very
low. High quality consists several high levelled studies with consistent results and moderate
include several studies with limitations. Additionally, low quality involve one or more
investigation with severe limitations and very low refers to an estimate of effect is very uncertain
that requires experts opinion.
CONCLUSION
From the above report, it is conclude that Policy of EBM can be explained as an effective
approach which is conscientious, explicit, judicious and reasonable use of best evidence for
making accurate decision making regarding care of patients. It include three main factors which
are required to be considered such as clinical expertise, best practice and patient values.
Moreover, three players has an important role in EBP policy including government, care
providers and patients.
6
Analysis of the case “Constraints of the ACA on Evidence-Based Medicine”
The constraints of ACA on evidence base medicines add specific information about types
of research which helps to investigate properly to select best practices in context of providing
care an individual with better quality of services. It is beneficial to consider the levels of EBM
policy related to therapy/prevention/harm, diagnosis and prognosis in order to render accurate
medical services to make patient well-being (Malanga and Mautner, 2016). Moreover, according
to grades of recommendations, the quality of evidence factors like high, moderate, low and very
low. High quality consists several high levelled studies with consistent results and moderate
include several studies with limitations. Additionally, low quality involve one or more
investigation with severe limitations and very low refers to an estimate of effect is very uncertain
that requires experts opinion.
CONCLUSION
From the above report, it is conclude that Policy of EBM can be explained as an effective
approach which is conscientious, explicit, judicious and reasonable use of best evidence for
making accurate decision making regarding care of patients. It include three main factors which
are required to be considered such as clinical expertise, best practice and patient values.
Moreover, three players has an important role in EBP policy including government, care
providers and patients.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
REFERENCES
Books and journals
Greenhalgh, T. (2014). How to read a paper: The basics of evidence-based medicine. John
Wiley & Sons.
Hoffmann, T. C., Montori, V. M., & Del Mar, C. (2014). The connection between evidence-
based medicine and shared decision making. Jama. 312(13). 1295-1296.
Sadeghi‐Bazargani, H., Tabrizi, J. S., & Azami‐Aghdash, S. (2014). Barriers to evidence‐based
medicine: a systematic review. Journal of evaluation in clinical practice. 20(6). 793-
802.
Ilic, D., & Maloney, S. (2014). Methods of teaching medical trainees evidence‐based medicine: a
systematic review. Medical Education. 48(2). 124-135.
Hamer, S., & Collinson, G. (2014). Achieving Evidence-Based Practice E-Book: A Handbook for
Practitioners. Elsevier Health Sciences.
7
Books and journals
Greenhalgh, T. (2014). How to read a paper: The basics of evidence-based medicine. John
Wiley & Sons.
Hoffmann, T. C., Montori, V. M., & Del Mar, C. (2014). The connection between evidence-
based medicine and shared decision making. Jama. 312(13). 1295-1296.
Sadeghi‐Bazargani, H., Tabrizi, J. S., & Azami‐Aghdash, S. (2014). Barriers to evidence‐based
medicine: a systematic review. Journal of evaluation in clinical practice. 20(6). 793-
802.
Ilic, D., & Maloney, S. (2014). Methods of teaching medical trainees evidence‐based medicine: a
systematic review. Medical Education. 48(2). 124-135.
Hamer, S., & Collinson, G. (2014). Achieving Evidence-Based Practice E-Book: A Handbook for
Practitioners. Elsevier Health Sciences.
7
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




