NUR2300 Evidence-Based Practice Report: Clinical Issue and Analysis
VerifiedAdded on 2022/11/11
|18
|4514
|79
Report
AI Summary
This report, prepared for a nursing course, focuses on evidence-based practice (EBP) in healthcare, specifically addressing the establishment of positive therapeutic relationships with culturally diverse patients. The report begins by identifying the clinical issue of poor access to healthcare for indigenous and diverse communities. It then provides background information, emphasizing the importance of effective communication and cultural competence in fostering positive patient outcomes. A research question is formulated using the PICO format, and a comprehensive search strategy is outlined, including inclusion and exclusion criteria. The report synthesizes findings from several research articles, highlighting the significance of communication skills, language barriers, person-centered care, and cultural humility. It also includes critical appraisal of the research articles and justifies the selection of a high-level evidence study. The report concludes by emphasizing the importance of adapting cultural humility by healthcare professionals and patients to improve ethical and racial diversity.

Running head: NURSING
NURSING
Name of the Student:
Name of the University:
Author Note:
NURSING
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1NURSING
Identification of the clinical issue:
The first quality standard of the NSQHS standard focuses on the establishment of a
positive therapeutic relationship with the client. Positive therapeutic relationship typically
refers to the creation of a positive rapport with the patients on the elements of mutual trust,
dignity and respect. Research studies mention in this regard that the establishment of positive
rapport with patients is directly dependent on acquiring positive patient outcome and
increased level of patient satisfaction (Betancourt et al., 2016).
Summary of the evidence base:
A large number of research studies suggest that the primary requisite for the creation
of a positive therapeutic relationship is based on the aspect of effective communication.
Effective communication refers to the use of both verbal and non-verbal gestures and
reinforcement of a comfortable therapeutic environment (Hermann et al., 2019). Poor quality
of communication has been studied to diminish access to care services and at the same time
contribute to poor care outcome for a significant percentage of the patient that includes
patients belonging to diverse cultures (Purnell et al., 2016). On the contrary fostering a
positive therapeutic environment can help to acquire positive healthcare outcome.
Justification for the choice of research topic:
The justification for the choice of the research topic can be explained as the
increased prevalence of poor access to health care facilities by the indigenous community
members and individuals of diverse community members. Despite a large number of
initiatives taken by the Australian government such as Close the gap policy, access to health
care services has remained poor for the indigenous community members that primarily
include Aboriginal and Torres Islander community members. Investigating best evidence best
Identification of the clinical issue:
The first quality standard of the NSQHS standard focuses on the establishment of a
positive therapeutic relationship with the client. Positive therapeutic relationship typically
refers to the creation of a positive rapport with the patients on the elements of mutual trust,
dignity and respect. Research studies mention in this regard that the establishment of positive
rapport with patients is directly dependent on acquiring positive patient outcome and
increased level of patient satisfaction (Betancourt et al., 2016).
Summary of the evidence base:
A large number of research studies suggest that the primary requisite for the creation
of a positive therapeutic relationship is based on the aspect of effective communication.
Effective communication refers to the use of both verbal and non-verbal gestures and
reinforcement of a comfortable therapeutic environment (Hermann et al., 2019). Poor quality
of communication has been studied to diminish access to care services and at the same time
contribute to poor care outcome for a significant percentage of the patient that includes
patients belonging to diverse cultures (Purnell et al., 2016). On the contrary fostering a
positive therapeutic environment can help to acquire positive healthcare outcome.
Justification for the choice of research topic:
The justification for the choice of the research topic can be explained as the
increased prevalence of poor access to health care facilities by the indigenous community
members and individuals of diverse community members. Despite a large number of
initiatives taken by the Australian government such as Close the gap policy, access to health
care services has remained poor for the indigenous community members that primarily
include Aboriginal and Torres Islander community members. Investigating best evidence best
2NURSING
practice to overcome cultural barriers can help improve access to care facilities and improve
associated healthcare outcome (Vermeir et al., 2015).
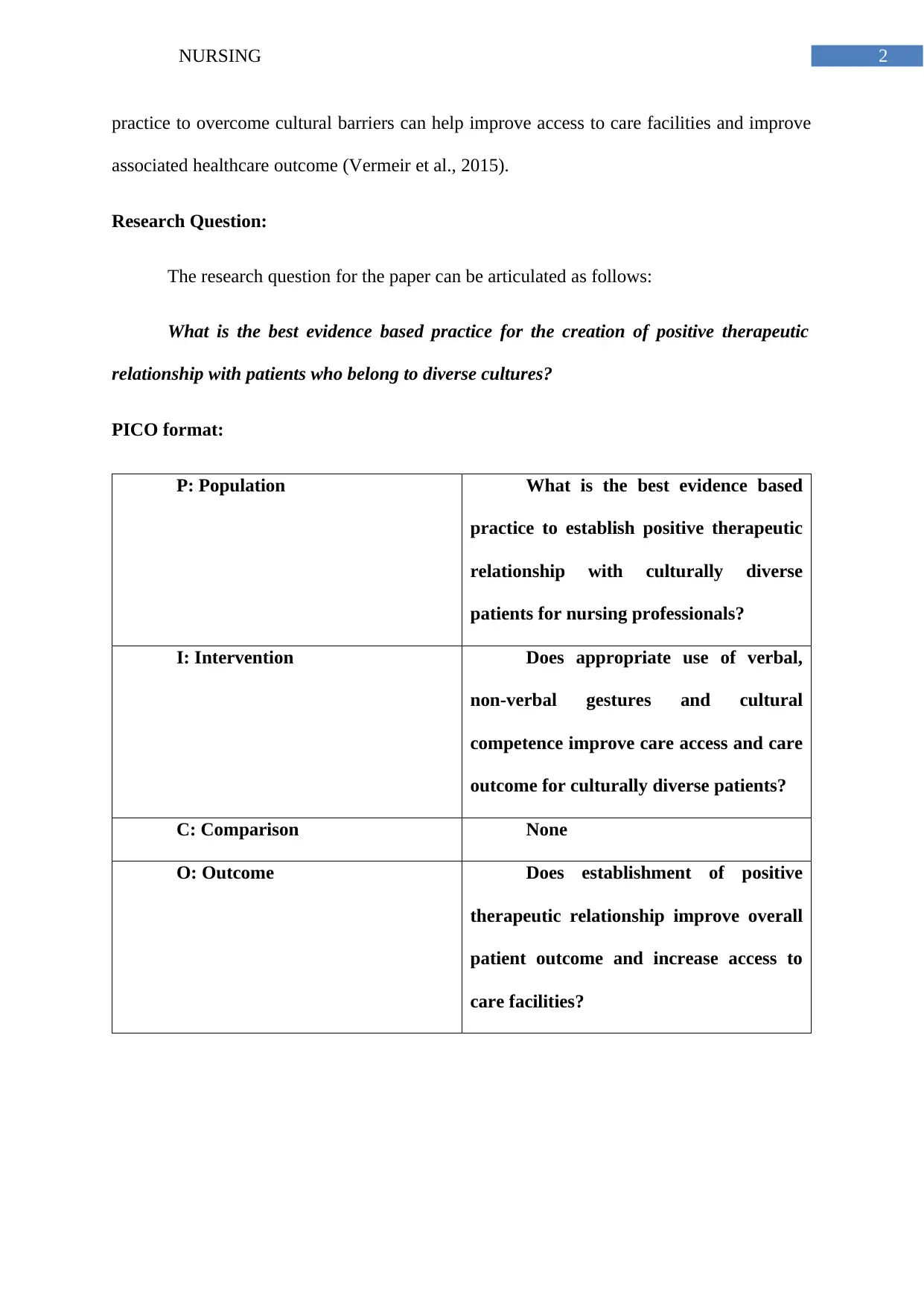
Research Question:
The research question for the paper can be articulated as follows:
What is the best evidence based practice for the creation of positive therapeutic
relationship with patients who belong to diverse cultures?
PICO format:
P: Population What is the best evidence based
practice to establish positive therapeutic
relationship with culturally diverse
patients for nursing professionals?
I: Intervention Does appropriate use of verbal,
non-verbal gestures and cultural
competence improve care access and care
outcome for culturally diverse patients?
C: Comparison None
O: Outcome Does establishment of positive
therapeutic relationship improve overall
patient outcome and increase access to
care facilities?
practice to overcome cultural barriers can help improve access to care facilities and improve
associated healthcare outcome (Vermeir et al., 2015).
Research Question:
The research question for the paper can be articulated as follows:
What is the best evidence based practice for the creation of positive therapeutic
relationship with patients who belong to diverse cultures?
PICO format:
P: Population What is the best evidence based
practice to establish positive therapeutic
relationship with culturally diverse
patients for nursing professionals?
I: Intervention Does appropriate use of verbal,
non-verbal gestures and cultural
competence improve care access and care
outcome for culturally diverse patients?
C: Comparison None
O: Outcome Does establishment of positive
therapeutic relationship improve overall
patient outcome and increase access to
care facilities?
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3NURSING
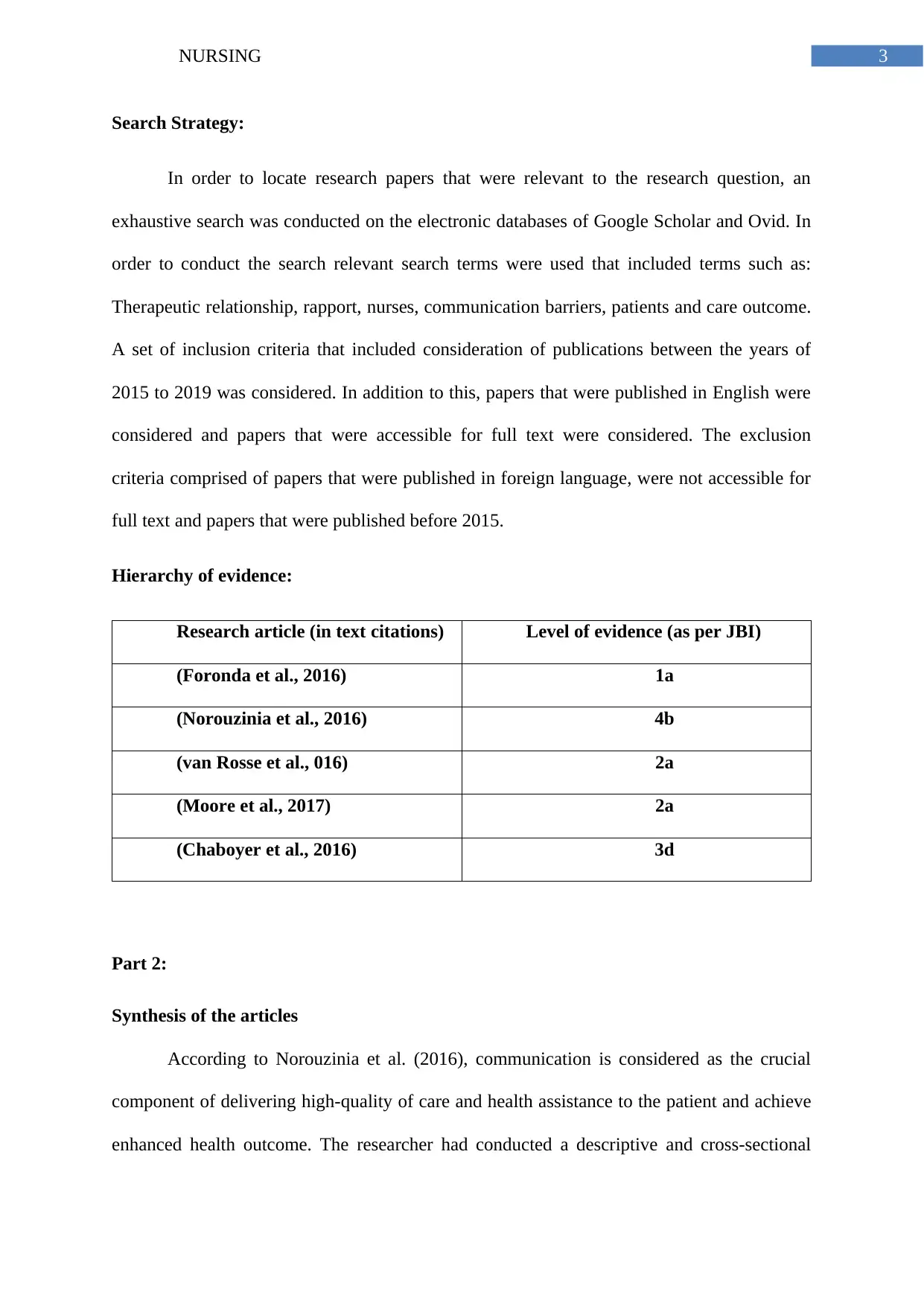
Search Strategy:
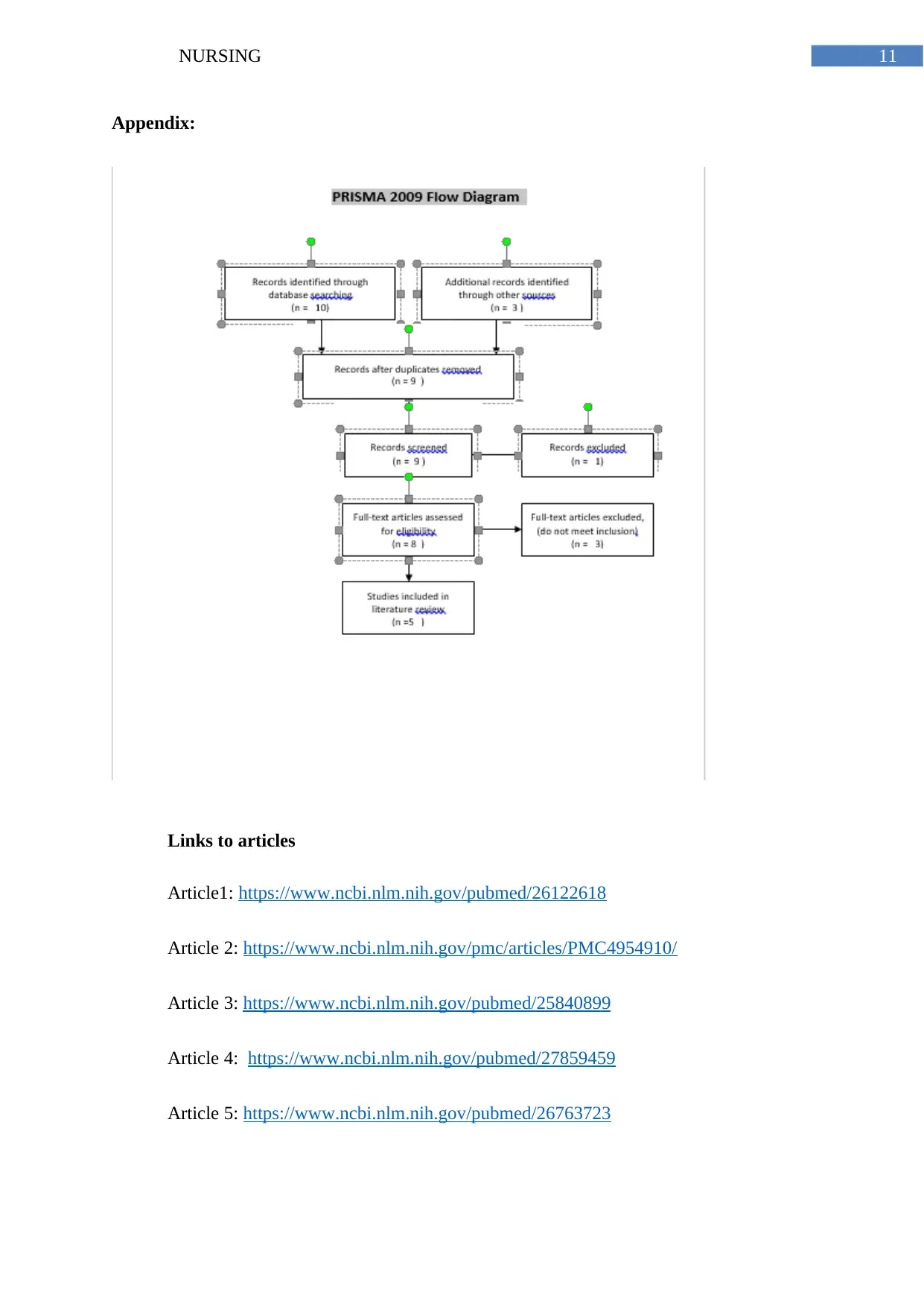
In order to locate research papers that were relevant to the research question, an
exhaustive search was conducted on the electronic databases of Google Scholar and Ovid. In
order to conduct the search relevant search terms were used that included terms such as:
Therapeutic relationship, rapport, nurses, communication barriers, patients and care outcome.
A set of inclusion criteria that included consideration of publications between the years of
2015 to 2019 was considered. In addition to this, papers that were published in English were
considered and papers that were accessible for full text were considered. The exclusion
criteria comprised of papers that were published in foreign language, were not accessible for
full text and papers that were published before 2015.
Hierarchy of evidence:
Research article (in text citations) Level of evidence (as per JBI)
(Foronda et al., 2016) 1a
(Norouzinia et al., 2016) 4b
(van Rosse et al., 016) 2a
(Moore et al., 2017) 2a
(Chaboyer et al., 2016) 3d
Part 2:
Synthesis of the articles
According to Norouzinia et al. (2016), communication is considered as the crucial
component of delivering high-quality of care and health assistance to the patient and achieve
enhanced health outcome. The researcher had conducted a descriptive and cross-sectional
Search Strategy:
In order to locate research papers that were relevant to the research question, an
exhaustive search was conducted on the electronic databases of Google Scholar and Ovid. In
order to conduct the search relevant search terms were used that included terms such as:
Therapeutic relationship, rapport, nurses, communication barriers, patients and care outcome.
A set of inclusion criteria that included consideration of publications between the years of
2015 to 2019 was considered. In addition to this, papers that were published in English were
considered and papers that were accessible for full text were considered. The exclusion
criteria comprised of papers that were published in foreign language, were not accessible for
full text and papers that were published before 2015.
Hierarchy of evidence:
Research article (in text citations) Level of evidence (as per JBI)
(Foronda et al., 2016) 1a
(Norouzinia et al., 2016) 4b
(van Rosse et al., 016) 2a
(Moore et al., 2017) 2a
(Chaboyer et al., 2016) 3d
Part 2:
Synthesis of the articles
According to Norouzinia et al. (2016), communication is considered as the crucial
component of delivering high-quality of care and health assistance to the patient and achieve
enhanced health outcome. The researcher had conducted a descriptive and cross-sectional
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4NURSING
analysis study using 50 patients and 70 nurses in two different hospitals. Two different
questionnaire set was prepared for both the nurses and the barriers were classified into four
different categories namely environmental, nurse-associated, patient-associated and common
barriers. The nurse and patients were invited to participate based on the inclusion criteria
which stated that that nurse must hold bachelor’s degree, willingness to participate and they
must have minimum 6 months of working experience. The patient must be more than 15
years of age, willingness to participate, they should have the capability to develop
communication and literacy. The inferential and descriptive method of data analysis was
considered. Based on the analysis, the major barrier was nurse-associated barriers that was
hindering the communication between the nurse and the patient and the least important
barrier were common barrier. The researcher had recommended that the nurse must be trained
with appropriate communication skills and should be encouraged to develop a healthy
communication surrounding with the patient. On the other hand, Rosse et al. (2016), had
highlighted that language barrier is the major threat for deteriorating the quality of care
within the hospital setting. The researcher had focused on identifying the patient safety threat
that arises due to language barrier while hospitalization and also exhibited the method in
which the language barrier is identified, reported and connected within the hospital setting.
The researcher had combined the qualitative and quantitative method for collecting the
sample of 576 patients and later the patients were screened and analysed for identifying any
language barrier risk. The language barrier was evaluated on the grounds of ethnic
inequalities and the major areas were identified while performing the routine nursing task and
while the physician-patient communication related to their acute situation, diagnosis and risk
communication. Hence, the researcher recommended that the language barrier can be reduced
if the bridging, identification and reporting of language barrier is conducted adequately and
new solutions are such as routine safety is performed by the healthcare professionals.
analysis study using 50 patients and 70 nurses in two different hospitals. Two different
questionnaire set was prepared for both the nurses and the barriers were classified into four
different categories namely environmental, nurse-associated, patient-associated and common
barriers. The nurse and patients were invited to participate based on the inclusion criteria
which stated that that nurse must hold bachelor’s degree, willingness to participate and they
must have minimum 6 months of working experience. The patient must be more than 15
years of age, willingness to participate, they should have the capability to develop
communication and literacy. The inferential and descriptive method of data analysis was
considered. Based on the analysis, the major barrier was nurse-associated barriers that was
hindering the communication between the nurse and the patient and the least important
barrier were common barrier. The researcher had recommended that the nurse must be trained
with appropriate communication skills and should be encouraged to develop a healthy
communication surrounding with the patient. On the other hand, Rosse et al. (2016), had
highlighted that language barrier is the major threat for deteriorating the quality of care
within the hospital setting. The researcher had focused on identifying the patient safety threat
that arises due to language barrier while hospitalization and also exhibited the method in
which the language barrier is identified, reported and connected within the hospital setting.
The researcher had combined the qualitative and quantitative method for collecting the
sample of 576 patients and later the patients were screened and analysed for identifying any
language barrier risk. The language barrier was evaluated on the grounds of ethnic
inequalities and the major areas were identified while performing the routine nursing task and
while the physician-patient communication related to their acute situation, diagnosis and risk
communication. Hence, the researcher recommended that the language barrier can be reduced
if the bridging, identification and reporting of language barrier is conducted adequately and
new solutions are such as routine safety is performed by the healthcare professionals.
5NURSING
According to Moore et al. (2017), person-centred care is defined as the significant
method of performing or thinking any activity that includes social and health services and
will also aim in evolving the quality fi care and support to the patient. The researcher had
focused on exploring the facilitator and barriers towards delivering effective person-centred
care intervention to the patient. Qualitative interviews were conducted for GPCC researchers
who were involved in executing the GPCC model. The interview was not conducted in
English and was performed in the year 2013-2014. The result were analysed using thematic
analysis process and based on the research findings the barriers were identified, which were
classified under the different themes namely traditional structures and practices, attitude and
establishment of PCC intervention. The above mentioned barriers were inhibiting the
effective implementation of person-centred intervention and care. The facilitator were also
identified in the study which were responsible for effective implementation of person-centred
intervention care namely organisational factors, training and leadership associated with an
empowering approach and attitude by professionals. According to Chaboyer et al. (2016), the
researcher had focused on exploring how the healthcare professionals will effectively
communicate with the patient related to care transitions. The researcher had followed
collective and instrumental case study method to make empirical data regarding the patient
transition care. Group and individual semi-structured interview was conducted to explain the
engagement of patient within their transition planning and from the research findings five
different themes were identified namely organisational assurance towards patient
engagement, effect of professional norms and hierarchical culture on the patient engagement,
condoning specific healthcare experts’ actions and orientations, understanding and discussing
the preferences of patient and enacting communication strategy evidence sharing. Based on
the research findings, the themes were identified that extensively illustrated the enabling
factors for patient engagement. Professional and organisational commitment is the enabling
According to Moore et al. (2017), person-centred care is defined as the significant
method of performing or thinking any activity that includes social and health services and
will also aim in evolving the quality fi care and support to the patient. The researcher had
focused on exploring the facilitator and barriers towards delivering effective person-centred
care intervention to the patient. Qualitative interviews were conducted for GPCC researchers
who were involved in executing the GPCC model. The interview was not conducted in
English and was performed in the year 2013-2014. The result were analysed using thematic
analysis process and based on the research findings the barriers were identified, which were
classified under the different themes namely traditional structures and practices, attitude and
establishment of PCC intervention. The above mentioned barriers were inhibiting the
effective implementation of person-centred intervention and care. The facilitator were also
identified in the study which were responsible for effective implementation of person-centred
intervention care namely organisational factors, training and leadership associated with an
empowering approach and attitude by professionals. According to Chaboyer et al. (2016), the
researcher had focused on exploring how the healthcare professionals will effectively
communicate with the patient related to care transitions. The researcher had followed
collective and instrumental case study method to make empirical data regarding the patient
transition care. Group and individual semi-structured interview was conducted to explain the
engagement of patient within their transition planning and from the research findings five
different themes were identified namely organisational assurance towards patient
engagement, effect of professional norms and hierarchical culture on the patient engagement,
condoning specific healthcare experts’ actions and orientations, understanding and discussing
the preferences of patient and enacting communication strategy evidence sharing. Based on
the research findings, the themes were identified that extensively illustrated the enabling
factors for patient engagement. Professional and organisational commitment is the enabling
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6NURSING
factor that will enhance the patient-centred care and also assist the patient in developing their
communication.
According to Foronda et al. (2016), diversity is considered as the crucial and
recognized area within the healthcare setting, where the concept of cultural humility is most
frequently used. The researcher had focused to provide a concept analysis and the appropriate
definition of cultural humanity within the healthcare setting. Cultural humility is widely used
in various areas of practice and individual with racial or ethnic difference, sexual preference
difference, relationship between the patient and the healthcare providers, social status and
inter-professional role. The articles were screened in different database such as PubMed or
CINAHL Plus and based on the screening of articles, the most relevant or appropriate articles
were included in the study. 154 articles were selected out of which the article published
before 2009 were removed and the researcher also excluded the articles which were
published in English and which did not discuss or include cultural humility. From the
research findings, it was established that many article have explained the concept of cultural
humility and few novel attributes were also discovered that included openness, egoless, self-
awareness, self-reflection and critique and supportive interactions. Hence, cultural humility is
defined as the life-long process, where the consequences are based on partnership, mutual
empowerment, optimal care, lifelong learning and respect.
Identification and selection of critical appraisal tool
The critical appraisal tools are used for critically evaluating the research article based
on the research method and examine the way the study is conducted. Using critical appraisal
tool, the clinicians can identify the efficiency and reliability of the research article and help
the healthcare professionals to enhance their clinical skills and accordingly determine if the
research evidence is biased or not-biased and can be used for delivering enhanced patient care
(). In this study, Critical appraising skills programme (CASP) tool is used that consist of
factor that will enhance the patient-centred care and also assist the patient in developing their
communication.
According to Foronda et al. (2016), diversity is considered as the crucial and
recognized area within the healthcare setting, where the concept of cultural humility is most
frequently used. The researcher had focused to provide a concept analysis and the appropriate
definition of cultural humanity within the healthcare setting. Cultural humility is widely used
in various areas of practice and individual with racial or ethnic difference, sexual preference
difference, relationship between the patient and the healthcare providers, social status and
inter-professional role. The articles were screened in different database such as PubMed or
CINAHL Plus and based on the screening of articles, the most relevant or appropriate articles
were included in the study. 154 articles were selected out of which the article published
before 2009 were removed and the researcher also excluded the articles which were
published in English and which did not discuss or include cultural humility. From the
research findings, it was established that many article have explained the concept of cultural
humility and few novel attributes were also discovered that included openness, egoless, self-
awareness, self-reflection and critique and supportive interactions. Hence, cultural humility is
defined as the life-long process, where the consequences are based on partnership, mutual
empowerment, optimal care, lifelong learning and respect.
Identification and selection of critical appraisal tool
The critical appraisal tools are used for critically evaluating the research article based
on the research method and examine the way the study is conducted. Using critical appraisal
tool, the clinicians can identify the efficiency and reliability of the research article and help
the healthcare professionals to enhance their clinical skills and accordingly determine if the
research evidence is biased or not-biased and can be used for delivering enhanced patient care
(). In this study, Critical appraising skills programme (CASP) tool is used that consist of
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7NURSING
different checklist question, which aim to determine the reliability and efficiency of the high-
evidence research article (Kim, Sefcik & Bradway, 2017). CASP tool was used to identify
what novel strategy can be used from the evidence to enhance the communication between
the patient and the nurse.
Critically appraising the research article
Yes, the result of the review was valid because the researcher have clearly explained
the outcome and highlighted that there are various attributes present within the cultural
humility to enhance the quality of care and competence in the healthcare setting. Yes, the
authors have considered the correct papers based on the inclusion and exclusion criteria. Yes,
the researcher have included the relevant and important studies and the participants were
belonging to different cultural background associated with non-English language study. No,
the researcher have not reviewed the quality of the included articles adequately, as they have
just highlighted which articles were explaining the cultural humility and have considered
those articles on a general basis. Yes, the result of the review was combined to identify the
best explanation and definition of cultural humility. The overall result of the review stated
that cultural humility must be adapted by both the healthcare professional and the patient
within the healthcare setting to understand the racial and ethical diversity. The result is
precise enough to explain the effectiveness and attributes of cultural humility within the
healthcare setting. Yes, the result can be applied to the local population as it is important for
the general population and the healthcare professional to be aware of the concept and adapt it
in their daily life. Yes, the crucial outcomes were considered for explaining the definition of
cultural humility. Yes, the benefits are essential to understand the general point-of-view
related do ethical and racial diversity.
different checklist question, which aim to determine the reliability and efficiency of the high-
evidence research article (Kim, Sefcik & Bradway, 2017). CASP tool was used to identify
what novel strategy can be used from the evidence to enhance the communication between
the patient and the nurse.
Critically appraising the research article
Yes, the result of the review was valid because the researcher have clearly explained
the outcome and highlighted that there are various attributes present within the cultural
humility to enhance the quality of care and competence in the healthcare setting. Yes, the
authors have considered the correct papers based on the inclusion and exclusion criteria. Yes,
the researcher have included the relevant and important studies and the participants were
belonging to different cultural background associated with non-English language study. No,
the researcher have not reviewed the quality of the included articles adequately, as they have
just highlighted which articles were explaining the cultural humility and have considered
those articles on a general basis. Yes, the result of the review was combined to identify the
best explanation and definition of cultural humility. The overall result of the review stated
that cultural humility must be adapted by both the healthcare professional and the patient
within the healthcare setting to understand the racial and ethical diversity. The result is
precise enough to explain the effectiveness and attributes of cultural humility within the
healthcare setting. Yes, the result can be applied to the local population as it is important for
the general population and the healthcare professional to be aware of the concept and adapt it
in their daily life. Yes, the crucial outcomes were considered for explaining the definition of
cultural humility. Yes, the benefits are essential to understand the general point-of-view
related do ethical and racial diversity.
8NURSING
Choice of high level of evidence and rationale:
The highest level of evidence was considered as the research paper authored by
Foronda et al. (2016). As per the Joanna-Briggs level of evidence mentioned in the research
articles, systematic reviews has been considered as the higher level of study. One of the
primary reason of this is the multiple randomised control trails which is used in the analysis
process, and these articles include participants that are blinded to the process. Therefore, the
risk of personal bias of lowered. Further, these papers help the researchers to understand the
importance of the intervention and analyse the positives and negatives associated with it. The
rationale for the selection of the paper can be explained as the systematic review study design
that evaluated all the randomised control aspect of cultural competency and cultural
sensitivity between the patients and nurses. In addition to this, the paper considered the power
balance and cultural humility as the primary pillars of cultural competency of the paper so
that the research findings could help to develop a holistic approach of care involved in the
care process. Hence, this paper by Foronda et al. (2016), was chosen for the analysis and
critical appraisal through the JBI hierarchy of level of evidence and then the findings and
analysis were used for the development of effective environment for cultural competency in
the care process.
Choice of high level of evidence and rationale:
The highest level of evidence was considered as the research paper authored by
Foronda et al. (2016). As per the Joanna-Briggs level of evidence mentioned in the research
articles, systematic reviews has been considered as the higher level of study. One of the
primary reason of this is the multiple randomised control trails which is used in the analysis
process, and these articles include participants that are blinded to the process. Therefore, the
risk of personal bias of lowered. Further, these papers help the researchers to understand the
importance of the intervention and analyse the positives and negatives associated with it. The
rationale for the selection of the paper can be explained as the systematic review study design
that evaluated all the randomised control aspect of cultural competency and cultural
sensitivity between the patients and nurses. In addition to this, the paper considered the power
balance and cultural humility as the primary pillars of cultural competency of the paper so
that the research findings could help to develop a holistic approach of care involved in the
care process. Hence, this paper by Foronda et al. (2016), was chosen for the analysis and
critical appraisal through the JBI hierarchy of level of evidence and then the findings and
analysis were used for the development of effective environment for cultural competency in
the care process.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9NURSING
References:
Betancourt, J. R., Green, A. R., Carrillo, J. E., & Owusu Ananeh-Firempong, I. I. (2016).
Defining cultural competence: a practical framework for addressing racial/ethnic
disparities in health and health care. Public health reports.
Chaboyer, W., McMurray, A., Marshall, A., Gillespie, B., Roberts, S., Hutchinson, A. M., ...
& Bucknall, T. (2016). Patient engagement in clinical communication: an exploratory
study. Scandinavian journal of caring sciences, 30(3), 565-573. doi:
10.1111/scs.12279.
Foronda, C., Baptiste, D. L., Reinholdt, M. M., & Ousman, K. (2016). Cultural humility: A
concept analysis. Journal of Transcultural Nursing, 27(3), 210-217. DOI;
10.1177/1043659615592677
Hermann, R. M., Long, E., & Trotta, R. L. (2019). Improving Patients' Experiences
Communicating With Nurses and Providers in the Emergency Department. Journal of
Emergency Nursing.
Moore, L., Britten, N., Lydahl, D., Naldemirci, Ö., Elam, M., & Wolf, A. (2017). Barriers
and facilitators to the implementation of person‐centred care in different healthcare
contexts. Scandinavian journal of caring sciences, 31(4), 662-673. doi:
10.1111/scs.12376.
Norouzinia, R., Aghabarari, M., Shiri, M., Karimi, M., & Samami, E. (2016).
Communication barriers perceived by nurses and patients. Global journal of health
science, 8(6), 65. DOI: https://dx.doi.org/10.5539%2Fgjhs.v8n6p65
References:
Betancourt, J. R., Green, A. R., Carrillo, J. E., & Owusu Ananeh-Firempong, I. I. (2016).
Defining cultural competence: a practical framework for addressing racial/ethnic
disparities in health and health care. Public health reports.
Chaboyer, W., McMurray, A., Marshall, A., Gillespie, B., Roberts, S., Hutchinson, A. M., ...
& Bucknall, T. (2016). Patient engagement in clinical communication: an exploratory
study. Scandinavian journal of caring sciences, 30(3), 565-573. doi:
10.1111/scs.12279.
Foronda, C., Baptiste, D. L., Reinholdt, M. M., & Ousman, K. (2016). Cultural humility: A
concept analysis. Journal of Transcultural Nursing, 27(3), 210-217. DOI;
10.1177/1043659615592677
Hermann, R. M., Long, E., & Trotta, R. L. (2019). Improving Patients' Experiences
Communicating With Nurses and Providers in the Emergency Department. Journal of
Emergency Nursing.
Moore, L., Britten, N., Lydahl, D., Naldemirci, Ö., Elam, M., & Wolf, A. (2017). Barriers
and facilitators to the implementation of person‐centred care in different healthcare
contexts. Scandinavian journal of caring sciences, 31(4), 662-673. doi:
10.1111/scs.12376.
Norouzinia, R., Aghabarari, M., Shiri, M., Karimi, M., & Samami, E. (2016).
Communication barriers perceived by nurses and patients. Global journal of health
science, 8(6), 65. DOI: https://dx.doi.org/10.5539%2Fgjhs.v8n6p65
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10NURSING
Purnell, T. S., Calhoun, E. A., Golden, S. H., Halladay, J. R., Krok-Schoen, J. L., Appelhans,
B. M., & Cooper, L. A. (2016). Achieving health equity: closing the gaps in health
care disparities, interventions, and research. Health Affairs, 35(8), 1410-1415.
van Rosse, F., de Bruijne, M., Suurmond, J., Essink-Bot, M. L., & Wagner, C. (2016).
Language barriers and patient safety risks in hospital care. A mixed methods study.
International journal of nursing studies, 54, 45-53. doi:
10.1016/j.ijnurstu.2015.03.012
Vermeir, P., Vandijck, D., Degroote, S., Peleman, R., Verhaeghe, R., Mortier, E., ... &
Vogelaers, D. (2015). Communication in healthcare: a narrative review of the
literature and practical recommendations. International journal of clinical
practice, 69(11), 1257-1267.
Purnell, T. S., Calhoun, E. A., Golden, S. H., Halladay, J. R., Krok-Schoen, J. L., Appelhans,
B. M., & Cooper, L. A. (2016). Achieving health equity: closing the gaps in health
care disparities, interventions, and research. Health Affairs, 35(8), 1410-1415.
van Rosse, F., de Bruijne, M., Suurmond, J., Essink-Bot, M. L., & Wagner, C. (2016).
Language barriers and patient safety risks in hospital care. A mixed methods study.
International journal of nursing studies, 54, 45-53. doi:
10.1016/j.ijnurstu.2015.03.012
Vermeir, P., Vandijck, D., Degroote, S., Peleman, R., Verhaeghe, R., Mortier, E., ... &
Vogelaers, D. (2015). Communication in healthcare: a narrative review of the
literature and practical recommendations. International journal of clinical
practice, 69(11), 1257-1267.
11NURSING
Appendix:
Links to articles
Article1: https://www.ncbi.nlm.nih.gov/pubmed/26122618
Article 2: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4954910/
Article 3: https://www.ncbi.nlm.nih.gov/pubmed/25840899
Article 4: https://www.ncbi.nlm.nih.gov/pubmed/27859459
Article 5: https://www.ncbi.nlm.nih.gov/pubmed/26763723
Appendix:
Links to articles
Article1: https://www.ncbi.nlm.nih.gov/pubmed/26122618
Article 2: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4954910/
Article 3: https://www.ncbi.nlm.nih.gov/pubmed/25840899
Article 4: https://www.ncbi.nlm.nih.gov/pubmed/27859459
Article 5: https://www.ncbi.nlm.nih.gov/pubmed/26763723
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





