NUR2300 Assignment: Evidence-Based Practice for Patient-Centered Care
VerifiedAdded on 2022/11/13
|21
|3841
|213
Report
AI Summary
This report provides an in-depth analysis of evidence-based nursing practice, specifically focusing on patient-centered care. It begins by defining the concept and highlighting its importance in healthcare, emphasizing the goal of placing patients at the center of their treatment and care. The report identifies and discusses the barriers to patient-centered care, such as traditional care practices, skeptical opinions, and system limitations. It explores the benefits of this approach, including increased patient empowerment and improved outcomes. The report formulates PICOT questions to guide the investigation, searches online databases for relevant research, and summarizes the evidence. The synthesis of information addresses obstacles and benefits, identifies evidence addressing PICOT questions, and appraises the evidence critically. The report concludes by emphasizing the need for further development and implementation of patient-centered care to improve patient outcomes and overall quality of care, particularly for vulnerable populations such as the elderly and children.
1
Evidence based Nursing practice
EVIDENCE BASED NURSING PRACTICE
Evidence based Nursing practice
EVIDENCE BASED NURSING PRACTICE
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Evidence based Nursing practice
Part 1 Evidence search
Identify and discuss
Person-centered care is a phenomenon of clinical treatment which aims to position the
patient at the center of the care approach and treatment. It is a way of providing care
and treatment which perceives the care seeker as a partner in the involved process of
thinking, planning, developing and monitoring (Moore et al. 2017). The aim was to
ensure that the care facilities met the needs and preferences of the patient so that they
could recover better without any obstacles.
summarize the content
There are several barriers in the system which need to be overcome for providing
patient centered care. The barriers are dynamic and arise from both the ends of the
doctor and the healthcare user. The need for a genuinely interested care person and
care seeker is required who is devoted to the patient's health. Mostly the vulnerable
groups of people are either too anxious or asymptomatic to the care which makes them
difficult to care for. With the lack of failing cognitive skills in elderly patients or among
patients who are yet to accept their condition, the providers have to deal with dangerous
and achievable goals that cannot be changed without the patient's agreement
(Thomson, Outram, Gilligan & Levett-Jones, 2015). Frail and sedated patients who are
acutely ill are unable to force upon their will and are their needs are often disregarded,
they are not viewed as a person which is the biggest barrier in the patient-centered care
system.
Justify and support the rationale
The idea behind patient-centered was to empower the patients and to remove the
mistrust that the patient and their family had towards the chosen treatment and care
approach. This mistrust often acted as a barrier between patient and doctor interactions,
the patients were hesitant to accept the care plan suggested (Tobiano et al. 2016).
Moreover, the family members involved often turned aggressive when the recovery did
not occur as planned or hoped for.
Patients often involved patient-family advisors but the care system did not have a set
place or role for them (Morera-Balaguer et al. 2018). As a result, their services
depended on the nature of the healthcare organization.
Evidence based Nursing practice
Part 1 Evidence search
Identify and discuss
Person-centered care is a phenomenon of clinical treatment which aims to position the
patient at the center of the care approach and treatment. It is a way of providing care
and treatment which perceives the care seeker as a partner in the involved process of
thinking, planning, developing and monitoring (Moore et al. 2017). The aim was to
ensure that the care facilities met the needs and preferences of the patient so that they
could recover better without any obstacles.
summarize the content
There are several barriers in the system which need to be overcome for providing
patient centered care. The barriers are dynamic and arise from both the ends of the
doctor and the healthcare user. The need for a genuinely interested care person and
care seeker is required who is devoted to the patient's health. Mostly the vulnerable
groups of people are either too anxious or asymptomatic to the care which makes them
difficult to care for. With the lack of failing cognitive skills in elderly patients or among
patients who are yet to accept their condition, the providers have to deal with dangerous
and achievable goals that cannot be changed without the patient's agreement
(Thomson, Outram, Gilligan & Levett-Jones, 2015). Frail and sedated patients who are
acutely ill are unable to force upon their will and are their needs are often disregarded,
they are not viewed as a person which is the biggest barrier in the patient-centered care
system.
Justify and support the rationale
The idea behind patient-centered was to empower the patients and to remove the
mistrust that the patient and their family had towards the chosen treatment and care
approach. This mistrust often acted as a barrier between patient and doctor interactions,
the patients were hesitant to accept the care plan suggested (Tobiano et al. 2016).
Moreover, the family members involved often turned aggressive when the recovery did
not occur as planned or hoped for.
Patients often involved patient-family advisors but the care system did not have a set
place or role for them (Morera-Balaguer et al. 2018). As a result, their services
depended on the nature of the healthcare organization.
3
Evidence based Nursing practice
Collaborating with patients and their families to be better aware of their needs was
essential for increasing patient satisfaction rates all over the country.
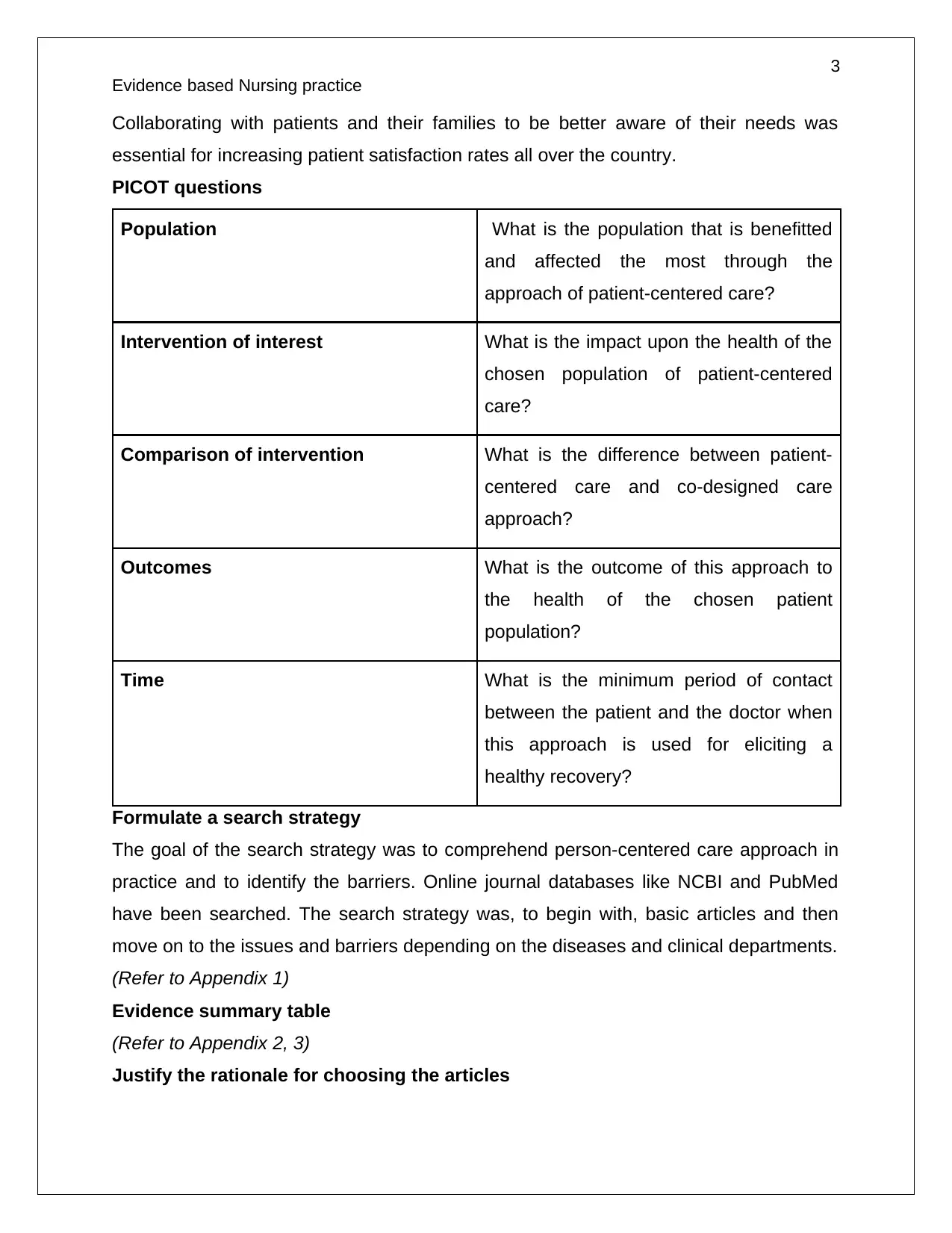
PICOT questions
Population What is the population that is benefitted
and affected the most through the
approach of patient-centered care?
Intervention of interest What is the impact upon the health of the
chosen population of patient-centered
care?
Comparison of intervention What is the difference between patient-
centered care and co-designed care
approach?
Outcomes What is the outcome of this approach to
the health of the chosen patient
population?
Time What is the minimum period of contact
between the patient and the doctor when
this approach is used for eliciting a
healthy recovery?
Formulate a search strategy
The goal of the search strategy was to comprehend person-centered care approach in
practice and to identify the barriers. Online journal databases like NCBI and PubMed
have been searched. The search strategy was, to begin with, basic articles and then
move on to the issues and barriers depending on the diseases and clinical departments.
(Refer to Appendix 1)
Evidence summary table
(Refer to Appendix 2, 3)
Justify the rationale for choosing the articles
Evidence based Nursing practice
Collaborating with patients and their families to be better aware of their needs was
essential for increasing patient satisfaction rates all over the country.
PICOT questions
Population What is the population that is benefitted
and affected the most through the
approach of patient-centered care?
Intervention of interest What is the impact upon the health of the
chosen population of patient-centered
care?
Comparison of intervention What is the difference between patient-
centered care and co-designed care
approach?
Outcomes What is the outcome of this approach to
the health of the chosen patient
population?
Time What is the minimum period of contact
between the patient and the doctor when
this approach is used for eliciting a
healthy recovery?
Formulate a search strategy
The goal of the search strategy was to comprehend person-centered care approach in
practice and to identify the barriers. Online journal databases like NCBI and PubMed
have been searched. The search strategy was, to begin with, basic articles and then
move on to the issues and barriers depending on the diseases and clinical departments.
(Refer to Appendix 1)
Evidence summary table
(Refer to Appendix 2, 3)
Justify the rationale for choosing the articles
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

4
Evidence based Nursing practice
The journals chosen for this assignment were from a dependable source and were
chosen for the relevance of the information contained in them. Most of the journals were
research articles provided with first-hand details and reports from both the patients and
their physicians.
Evidence based Nursing practice
The journals chosen for this assignment were from a dependable source and were
chosen for the relevance of the information contained in them. Most of the journals were
research articles provided with first-hand details and reports from both the patients and
their physicians.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
Evidence based Nursing practice
Part 2
Synthesis of information
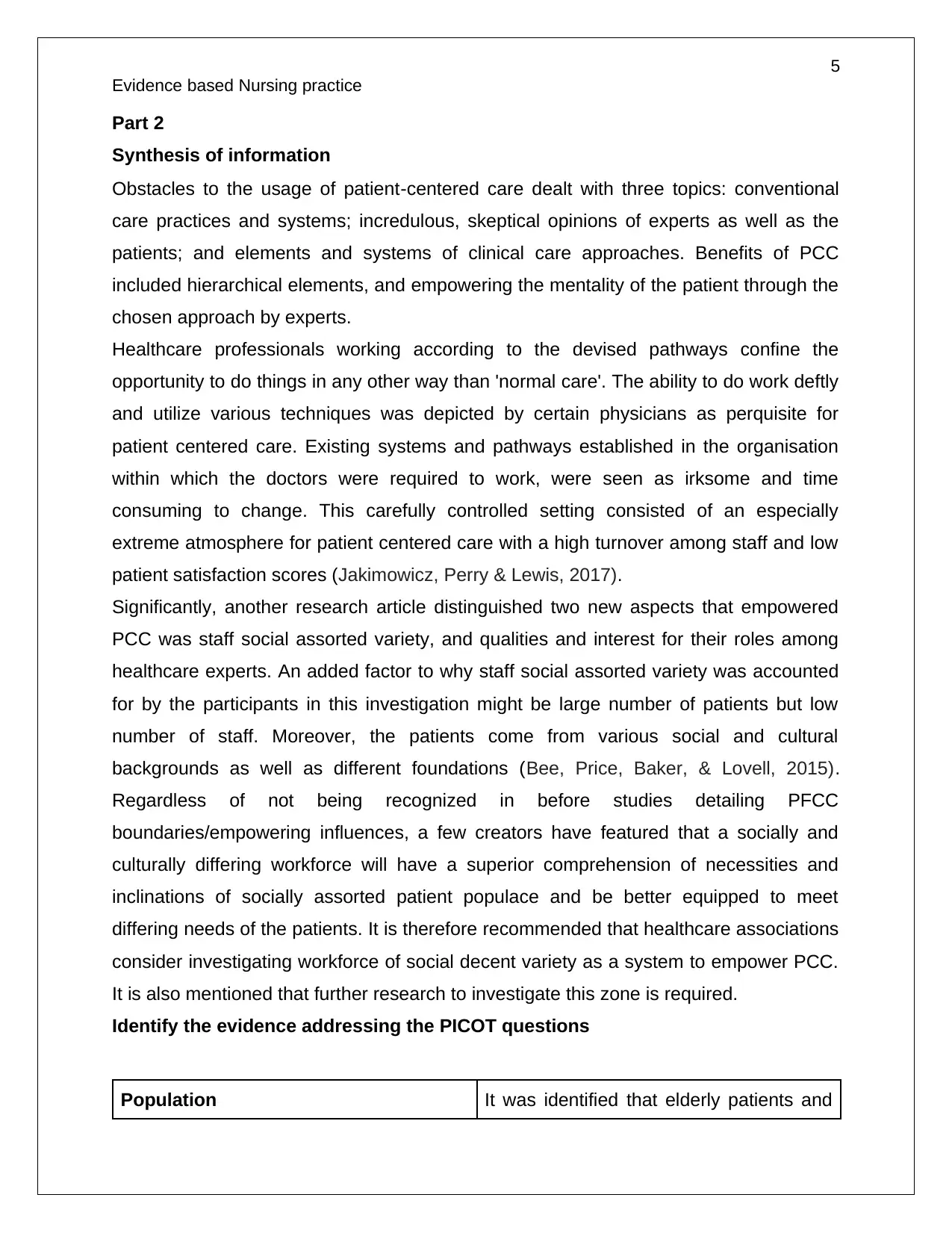
Obstacles to the usage of patient‐centered care dealt with three topics: conventional
care practices and systems; incredulous, skeptical opinions of experts as well as the
patients; and elements and systems of clinical care approaches. Benefits of PCC
included hierarchical elements, and empowering the mentality of the patient through the
chosen approach by experts.
Healthcare professionals working according to the devised pathways confine the
opportunity to do things in any other way than 'normal care'. The ability to do work deftly
and utilize various techniques was depicted by certain physicians as perquisite for
patient centered care. Existing systems and pathways established in the organisation
within which the doctors were required to work, were seen as irksome and time
consuming to change. This carefully controlled setting consisted of an especially
extreme atmosphere for patient centered care with a high turnover among staff and low
patient satisfaction scores (Jakimowicz, Perry & Lewis, 2017).
Significantly, another research article distinguished two new aspects that empowered
PCC was staff social assorted variety, and qualities and interest for their roles among
healthcare experts. An added factor to why staff social assorted variety was accounted
for by the participants in this investigation might be large number of patients but low
number of staff. Moreover, the patients come from various social and cultural
backgrounds as well as different foundations (Bee, Price, Baker, & Lovell, 2015).
Regardless of not being recognized in before studies detailing PFCC
boundaries/empowering influences, a few creators have featured that a socially and
culturally differing workforce will have a superior comprehension of necessities and
inclinations of socially assorted patient populace and be better equipped to meet
differing needs of the patients. It is therefore recommended that healthcare associations
consider investigating workforce of social decent variety as a system to empower PCC.
It is also mentioned that further research to investigate this zone is required.
Identify the evidence addressing the PICOT questions
Population It was identified that elderly patients and
Evidence based Nursing practice
Part 2
Synthesis of information
Obstacles to the usage of patient‐centered care dealt with three topics: conventional
care practices and systems; incredulous, skeptical opinions of experts as well as the
patients; and elements and systems of clinical care approaches. Benefits of PCC
included hierarchical elements, and empowering the mentality of the patient through the
chosen approach by experts.
Healthcare professionals working according to the devised pathways confine the
opportunity to do things in any other way than 'normal care'. The ability to do work deftly
and utilize various techniques was depicted by certain physicians as perquisite for
patient centered care. Existing systems and pathways established in the organisation
within which the doctors were required to work, were seen as irksome and time
consuming to change. This carefully controlled setting consisted of an especially
extreme atmosphere for patient centered care with a high turnover among staff and low
patient satisfaction scores (Jakimowicz, Perry & Lewis, 2017).
Significantly, another research article distinguished two new aspects that empowered
PCC was staff social assorted variety, and qualities and interest for their roles among
healthcare experts. An added factor to why staff social assorted variety was accounted
for by the participants in this investigation might be large number of patients but low
number of staff. Moreover, the patients come from various social and cultural
backgrounds as well as different foundations (Bee, Price, Baker, & Lovell, 2015).
Regardless of not being recognized in before studies detailing PFCC
boundaries/empowering influences, a few creators have featured that a socially and
culturally differing workforce will have a superior comprehension of necessities and
inclinations of socially assorted patient populace and be better equipped to meet
differing needs of the patients. It is therefore recommended that healthcare associations
consider investigating workforce of social decent variety as a system to empower PCC.
It is also mentioned that further research to investigate this zone is required.
Identify the evidence addressing the PICOT questions
Population It was identified that elderly patients and
6
Evidence based Nursing practice
children, patients who are very weak and
come from the neglected parts of the
society form the patient population that is
the most affected by patient-centered
care. Due to their lack of understanding,
cognitive skills and strength to control
their surroundings, their preferences and
needs are often overlooked (Greysen et
al. 2017). As a result, this population will
be the most benefitted through the
person-centered care approach as it
gives them an opportunity to be in control
of their situation and to accept a more
involvement in their health and wellbeing.
Intervention of interest They will feel increasingly great and
certain about administration, as
maintaining their poise and freedom
constructs common regard. The patient
will confide with and trust their physicians
to do what's best for them, which makes
the circumstance simpler for both the
patient and the physicians.
The physicians will meet their
enthusiastic, social, and down to earth
needs, which guarantees they keep up a
high quality of life.
The physicians can bolster the individuals
who will most likely be unable to
straightforwardly impart their needs and
needs (Wolf et al. 2017). Various
Evidence based Nursing practice
children, patients who are very weak and
come from the neglected parts of the
society form the patient population that is
the most affected by patient-centered
care. Due to their lack of understanding,
cognitive skills and strength to control
their surroundings, their preferences and
needs are often overlooked (Greysen et
al. 2017). As a result, this population will
be the most benefitted through the
person-centered care approach as it
gives them an opportunity to be in control
of their situation and to accept a more
involvement in their health and wellbeing.
Intervention of interest They will feel increasingly great and
certain about administration, as
maintaining their poise and freedom
constructs common regard. The patient
will confide with and trust their physicians
to do what's best for them, which makes
the circumstance simpler for both the
patient and the physicians.
The physicians will meet their
enthusiastic, social, and down to earth
needs, which guarantees they keep up a
high quality of life.
The physicians can bolster the individuals
who will most likely be unable to
straightforwardly impart their needs and
needs (Wolf et al. 2017). Various
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
Evidence based Nursing practice
conditions or inabilities can influence a
person's capacity to convey adequately.
For instance, dementia, learning
incapacities, or the individuals who just
don't have the certainty to do as such.
Person-focused care allows the
physicians to find appropriate approaches
to enable them to impart and augment
their nature of care.
It improves their freedom. In addition to
the fact that this is gainful on a personal
level for the patient, yet it additionally
urges them to partake in choices
( Sladdin, Chaboyer & Ball, (2018). It
raises their commitment, which
encourages physicians to arrive at better,
increasingly appropriate choices
identifying with their care. Moreover, it
gives them the certainty and capacity to
take care of themselves with less
contribution from physicians.
Comparison of intervention The patient centered care is a system to
devise the care and treatment, that
focuses on the needs of the patient. As
only the most important needs which
have an impact on the health are
sustained within the system, it is possible
to devise a care approach without the
patient actually being in the room (Aronis
et al. 2017). Whereas the co-design
Evidence based Nursing practice
conditions or inabilities can influence a
person's capacity to convey adequately.
For instance, dementia, learning
incapacities, or the individuals who just
don't have the certainty to do as such.
Person-focused care allows the
physicians to find appropriate approaches
to enable them to impart and augment
their nature of care.
It improves their freedom. In addition to
the fact that this is gainful on a personal
level for the patient, yet it additionally
urges them to partake in choices
( Sladdin, Chaboyer & Ball, (2018). It
raises their commitment, which
encourages physicians to arrive at better,
increasingly appropriate choices
identifying with their care. Moreover, it
gives them the certainty and capacity to
take care of themselves with less
contribution from physicians.
Comparison of intervention The patient centered care is a system to
devise the care and treatment, that
focuses on the needs of the patient. As
only the most important needs which
have an impact on the health are
sustained within the system, it is possible
to devise a care approach without the
patient actually being in the room (Aronis
et al. 2017). Whereas the co-design
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
Evidence based Nursing practice
model necessitates the involvement of the
patient in the care policy. Co-designed
care system is included as a tenet in the
care and promotes interaction between
the healthcare professionals and the
patient.
Outcomes Patients had fundamentally higher levels
of self-efficacy and autonomous abilities
than other patients who were had lesser
control over their health decisions. Also,
the intercession gathering came back to
work in a more noteworthy degree than
controls; their physical movement level
had expanded, which means higher
wellbeing related personal satisfaction.
These last impacts are not noteworthy but
rather are largely pointing towards the
gainful impacts of patient-focused care
(Gondek et al. 2017). Every one of the
impacts was evaluated while controlling
for significant financial and sickness
related factors.
Time Time is not a factor that has been
considered in any of the research articles.
This is because PCC comes into play at
basic level of primary care. The patients
who are admitted from chronic disorders
and for the lengthy recovery process are
likely to be more impacted by the care
Evidence based Nursing practice
model necessitates the involvement of the
patient in the care policy. Co-designed
care system is included as a tenet in the
care and promotes interaction between
the healthcare professionals and the
patient.
Outcomes Patients had fundamentally higher levels
of self-efficacy and autonomous abilities
than other patients who were had lesser
control over their health decisions. Also,
the intercession gathering came back to
work in a more noteworthy degree than
controls; their physical movement level
had expanded, which means higher
wellbeing related personal satisfaction.
These last impacts are not noteworthy but
rather are largely pointing towards the
gainful impacts of patient-focused care
(Gondek et al. 2017). Every one of the
impacts was evaluated while controlling
for significant financial and sickness
related factors.
Time Time is not a factor that has been
considered in any of the research articles.
This is because PCC comes into play at
basic level of primary care. The patients
who are admitted from chronic disorders
and for the lengthy recovery process are
likely to be more impacted by the care

9
Evidence based Nursing practice
approach (Ringdal et al. 2017).
Justify and support the evidence
The PICOT questions were framed in a way that allows the analysis of the important
aspects of Person-centered care. The evidence collected was able to answer most of
the PICOT questions. However, the question raised for the time period of the healthcare
intervention was not satisfactorily covered. The aspect of the time period required to
elicit a health outcome is not clear. Person-centered care should also be accompanied
by medication and clinical treatment to ensure complete recovery. It is required for
enhancing the quality of life of a patient.
Evidence based Nursing practice
approach (Ringdal et al. 2017).
Justify and support the evidence
The PICOT questions were framed in a way that allows the analysis of the important
aspects of Person-centered care. The evidence collected was able to answer most of
the PICOT questions. However, the question raised for the time period of the healthcare
intervention was not satisfactorily covered. The aspect of the time period required to
elicit a health outcome is not clear. Person-centered care should also be accompanied
by medication and clinical treatment to ensure complete recovery. It is required for
enhancing the quality of life of a patient.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
Evidence based Nursing practice
Tools for appraising evidence
(Refer to appendix 4)
Critical appraisal of evidence
Three themes have been identified among the barriers to PCC. The primary barrier are
the traditional ways of practice and clinical systems which keep the patient in the dark
and believe that the patient should not be provided with their health data collected. Next
is the attitude and belief among the care providers who perceive that considering patient
as a partner is tiresome and time consuming. Lastly, the interventions and
implementation systems for person centered care need to be developed further for
practical application.
The historical healthcare systems that still continue in some forms or the other, gave
importance to a positivist approach where information and health data was considered
supreme (Sladdin, Ball, Bull & Chaboyer, 2017). This caused them to disregard what
the patient was feeling or their opinions about their condition. Professionals have
agreed that this system is often restrictive and does not provide much opportunity of
interaction between the healthcare professionals and the patient. As a result, many
salient points that are key to the well being of the patient are often lost (Phillips et al.
2015). Moreover, the patient is kept in the dark and feel that they do not have enough
say in their own health matters.
However, other articles relay that time constraints also acts as an obstacle in the
delivery of patient centered care. In urgent and critical cases PCC is often disregarded
and the physicians consider the positivist mode for treatment. It is true that PCC is time
consuming as it requires extensive interaction with the patient and the formation of
cordial bond between them. On the other hand, the time constraints are made intense
by the skewed ratio of the care givers and care seekers. Essentially, experts expected
to adapt new correspondence procedures for patients with correspondence issue or
work with more seasoned transients, through interpreters (van Dongen et al. 2016). The
quick pace of social insurance exercises, in certain unique circumstances, made PCC
execution troublesome. Be that as it may, when implanted, a few scientists depicted
how patient centered care spared time when patients assumed liability for their own
Evidence based Nursing practice
Tools for appraising evidence
(Refer to appendix 4)
Critical appraisal of evidence
Three themes have been identified among the barriers to PCC. The primary barrier are
the traditional ways of practice and clinical systems which keep the patient in the dark
and believe that the patient should not be provided with their health data collected. Next
is the attitude and belief among the care providers who perceive that considering patient
as a partner is tiresome and time consuming. Lastly, the interventions and
implementation systems for person centered care need to be developed further for
practical application.
The historical healthcare systems that still continue in some forms or the other, gave
importance to a positivist approach where information and health data was considered
supreme (Sladdin, Ball, Bull & Chaboyer, 2017). This caused them to disregard what
the patient was feeling or their opinions about their condition. Professionals have
agreed that this system is often restrictive and does not provide much opportunity of
interaction between the healthcare professionals and the patient. As a result, many
salient points that are key to the well being of the patient are often lost (Phillips et al.
2015). Moreover, the patient is kept in the dark and feel that they do not have enough
say in their own health matters.
However, other articles relay that time constraints also acts as an obstacle in the
delivery of patient centered care. In urgent and critical cases PCC is often disregarded
and the physicians consider the positivist mode for treatment. It is true that PCC is time
consuming as it requires extensive interaction with the patient and the formation of
cordial bond between them. On the other hand, the time constraints are made intense
by the skewed ratio of the care givers and care seekers. Essentially, experts expected
to adapt new correspondence procedures for patients with correspondence issue or
work with more seasoned transients, through interpreters (van Dongen et al. 2016). The
quick pace of social insurance exercises, in certain unique circumstances, made PCC
execution troublesome. Be that as it may, when implanted, a few scientists depicted
how patient centered care spared time when patients assumed liability for their own
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

11
Evidence based Nursing practice
consideration or in case when an individual's objectives were successfully explained
and bolstered.
Specialists referred to the significance of intrigued staff and a submitted gathering of
experts with an inspirational frame of mind that took into consideration trust and
association building. Effective execution was reliant upon experts' skillfulness appeared
in tuning 'in an alternate way' to patients, affirming, recording and more than once
recognizing the individual's account (Herrin et al. 2016). Considering the to be as an
individual who is dynamic and a competent or equivalent accomplice was referred to as
a typical facilitator.
Evidence based Nursing practice
consideration or in case when an individual's objectives were successfully explained
and bolstered.
Specialists referred to the significance of intrigued staff and a submitted gathering of
experts with an inspirational frame of mind that took into consideration trust and
association building. Effective execution was reliant upon experts' skillfulness appeared
in tuning 'in an alternate way' to patients, affirming, recording and more than once
recognizing the individual's account (Herrin et al. 2016). Considering the to be as an
individual who is dynamic and a competent or equivalent accomplice was referred to as
a typical facilitator.
12
Evidence based Nursing practice
References
Aronis, K. N., Edgar, B., Lin, W., Martins, M. A. P., Paasche-Orlow, M. K., & Magnani, J.
W. (2017). Health literacy and atrial fibrillation: relevance and future directions for
patient-centred care. European cardiology, 12(1), 52.
Bee, P., Price, O., Baker, J., & Lovell, K. (2015). Systematic synthesis of barriers and
facilitators to service user-led care planning. The British Journal of
Psychiatry, 207(2), 104-114.
Gondek, D., Edbrooke‐Childs, J., Velikonja, T., Chapman, L., Saunders, F., Hayes, D.,
& Wolpert, M. (2017). Facilitators and barriers to person‐centred care in child and
young people mental health services: A systematic review. Clinical psychology &
psychotherapy, 24(4), 870-886.
Greysen, S. R., Harrison, J. D., Kripalani, S., Vasilevskis, E., Robinson, E., Metlay, J., ...
& Williams, M. V. (2017). Understanding patient-centred readmission factors: a
multi-site, mixed-methods study. BMJ Qual Saf, 26(1), 33-41.
Herrin, J., Harris, K. G., Kenward, K., Hines, S., Joshi, M. S., & Frosch, D. L. (2016).
Patient and family engagement: a survey of US hospital practices. BMJ Qual
Saf, 25(3), 182-189.
Jakimowicz, S., Perry, L., & Lewis, J. (2017). An integrative review of supports,
facilitators and barriers to patient‐centred nursing in the intensive care
unit. Journal of clinical nursing, 26(23-24), 4153-4171.
Moore, L., Britten, N., Lydahl, D., Naldemirci, Ö., Elam, M., & Wolf, A. (2017). Barriers
and facilitators to the implementation of person‐centred care in different
healthcare contexts. Scandinavian journal of caring sciences, 31(4), 662-673.
Morera-Balaguer, J., Botella-Rico, J. M., Martínez-González, M. C., Medina-Mirapeix,
F., & Rodríguez-Nogueira, Ó. (2018). Physical therapists’ perceptions and
experiences about barriers and facilitators of therapeutic patient-centred
relationships during outpatient rehabilitation: a qualitative study. Brazilian journal
of physical therapy, 22(6), 484-492.
Phillips, R. L., Short, A., Kenning, A., Dugdale, P., Nugus, P., McGowan, R., &
Greenfield, D. (2015). Achieving patient‐centred care: the potential and challenge
of the patient‐as‐professional role. Health Expectations, 18(6), 2616-2628.
Evidence based Nursing practice
References
Aronis, K. N., Edgar, B., Lin, W., Martins, M. A. P., Paasche-Orlow, M. K., & Magnani, J.
W. (2017). Health literacy and atrial fibrillation: relevance and future directions for
patient-centred care. European cardiology, 12(1), 52.
Bee, P., Price, O., Baker, J., & Lovell, K. (2015). Systematic synthesis of barriers and
facilitators to service user-led care planning. The British Journal of
Psychiatry, 207(2), 104-114.
Gondek, D., Edbrooke‐Childs, J., Velikonja, T., Chapman, L., Saunders, F., Hayes, D.,
& Wolpert, M. (2017). Facilitators and barriers to person‐centred care in child and
young people mental health services: A systematic review. Clinical psychology &
psychotherapy, 24(4), 870-886.
Greysen, S. R., Harrison, J. D., Kripalani, S., Vasilevskis, E., Robinson, E., Metlay, J., ...
& Williams, M. V. (2017). Understanding patient-centred readmission factors: a
multi-site, mixed-methods study. BMJ Qual Saf, 26(1), 33-41.
Herrin, J., Harris, K. G., Kenward, K., Hines, S., Joshi, M. S., & Frosch, D. L. (2016).
Patient and family engagement: a survey of US hospital practices. BMJ Qual
Saf, 25(3), 182-189.
Jakimowicz, S., Perry, L., & Lewis, J. (2017). An integrative review of supports,
facilitators and barriers to patient‐centred nursing in the intensive care
unit. Journal of clinical nursing, 26(23-24), 4153-4171.
Moore, L., Britten, N., Lydahl, D., Naldemirci, Ö., Elam, M., & Wolf, A. (2017). Barriers
and facilitators to the implementation of person‐centred care in different
healthcare contexts. Scandinavian journal of caring sciences, 31(4), 662-673.
Morera-Balaguer, J., Botella-Rico, J. M., Martínez-González, M. C., Medina-Mirapeix,
F., & Rodríguez-Nogueira, Ó. (2018). Physical therapists’ perceptions and
experiences about barriers and facilitators of therapeutic patient-centred
relationships during outpatient rehabilitation: a qualitative study. Brazilian journal
of physical therapy, 22(6), 484-492.
Phillips, R. L., Short, A., Kenning, A., Dugdale, P., Nugus, P., McGowan, R., &
Greenfield, D. (2015). Achieving patient‐centred care: the potential and challenge
of the patient‐as‐professional role. Health Expectations, 18(6), 2616-2628.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





