Comparative Analysis: Iowa and Kotter Models for EBP Implementation
VerifiedAdded on 2023/03/29
|11
|1180
|141
Presentation
AI Summary
This presentation delves into the application of the Iowa and Kotter models for implementing evidence-based practice (EBP) in healthcare, using a case study focused on reducing catheter-associated urinary tract infections (CAUTIs). The Iowa model is presented as a problem-solving framework, outlining key decision points and steps from topic selection to change evaluation. The Kotter and Cohen's change model, with its eight stages, is also described, emphasizing creating a sense of urgency, forming a team, and fostering a new culture. The presentation integrates these models by illustrating how they can be used to address a specific clinical problem: high rates of UTIs linked to catheter use. It details the formation of a multidisciplinary team, the retrieval and synthesis of evidence (including the use of PICO questions), and the pilot implementation of a practice change (switching to silicone catheters). Furthermore, the presentation outlines the process of instituting change, including communicating a vision, removing hindrances, and monitoring outcomes. The presentation concludes with a discussion of disseminating findings and making the new practice a standard of care.

INTRODUCTION
• Evidence-based practice (EBP) is a
problem solving strategy to clinical
decision-making in healthcare
institutions
• It integrates high quality scientific
evidence with experiential evidence
• There are various EBP models that have
been developed to help to conceptualize
transferring evidence into practice
• One EBP model and change model is
Iowa EBP model
• The aim of the current presentation is
– To describe the Iowa EBP and Kotter and
Cohen’s models
– To describe how these two models can be
used to implement an EBP change in
clinical practice
• Evidence-based practice (EBP) is a
problem solving strategy to clinical
decision-making in healthcare
institutions
• It integrates high quality scientific
evidence with experiential evidence
• There are various EBP models that have
been developed to help to conceptualize
transferring evidence into practice
• One EBP model and change model is
Iowa EBP model
• The aim of the current presentation is
– To describe the Iowa EBP and Kotter and
Cohen’s models
– To describe how these two models can be
used to implement an EBP change in
clinical practice
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
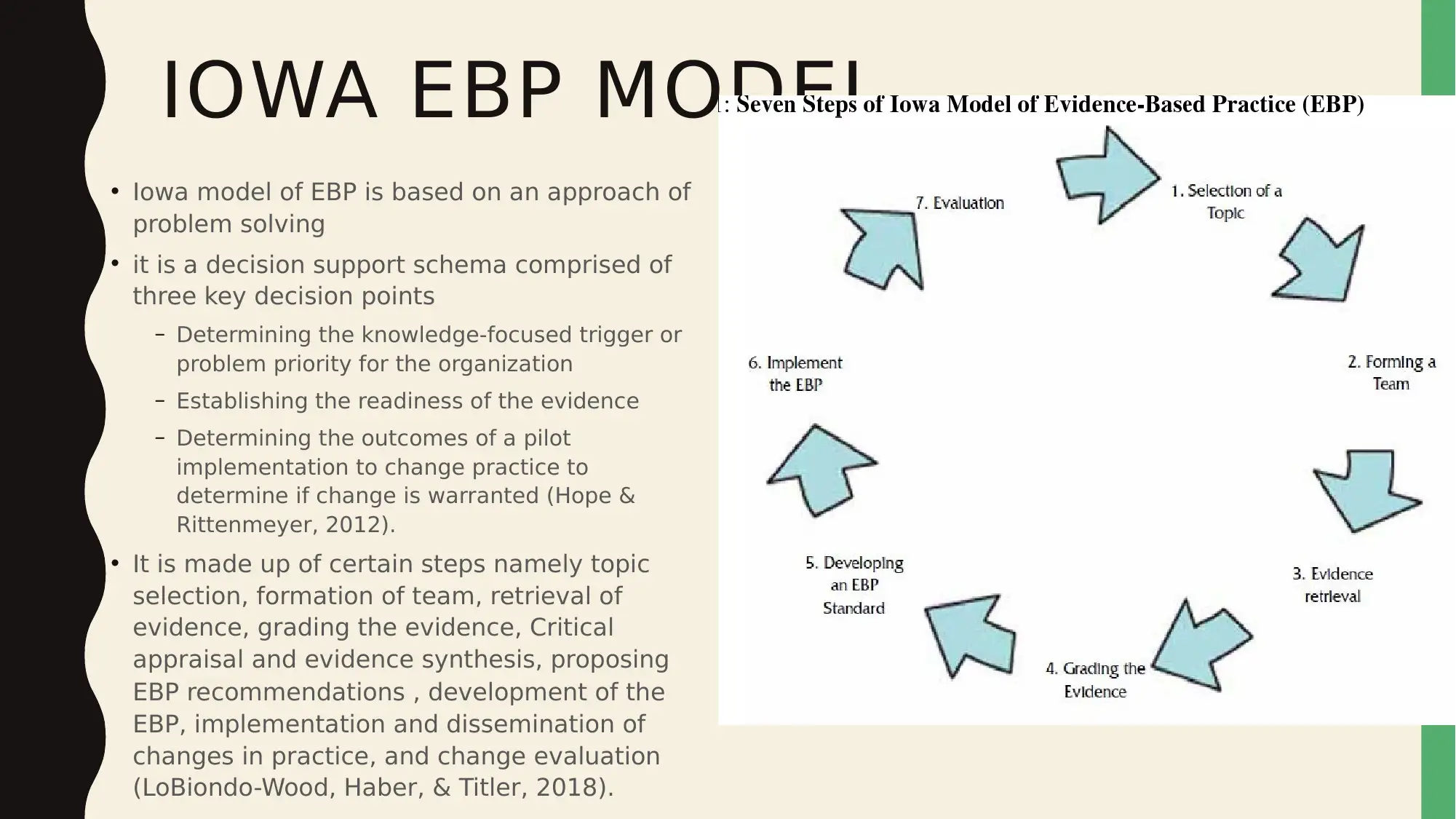
IOWA EBP MODEL
• Iowa model of EBP is based on an approach of
problem solving
• it is a decision support schema comprised of
three key decision points
– Determining the knowledge-focused trigger or
problem priority for the organization
– Establishing the readiness of the evidence
– Determining the outcomes of a pilot
implementation to change practice to
determine if change is warranted (Hope &
Rittenmeyer, 2012).
• It is made up of certain steps namely topic
selection, formation of team, retrieval of
evidence, grading the evidence, Critical
appraisal and evidence synthesis, proposing
EBP recommendations , development of the
EBP, implementation and dissemination of
changes in practice, and change evaluation
(LoBiondo-Wood, Haber, & Titler, 2018).
• Iowa model of EBP is based on an approach of
problem solving
• it is a decision support schema comprised of
three key decision points
– Determining the knowledge-focused trigger or
problem priority for the organization
– Establishing the readiness of the evidence
– Determining the outcomes of a pilot
implementation to change practice to
determine if change is warranted (Hope &
Rittenmeyer, 2012).
• It is made up of certain steps namely topic
selection, formation of team, retrieval of
evidence, grading the evidence, Critical
appraisal and evidence synthesis, proposing
EBP recommendations , development of the
EBP, implementation and dissemination of
changes in practice, and change evaluation
(LoBiondo-Wood, Haber, & Titler, 2018).

KOTTER AND COHEN’S
CHANGE MODEL
• Kotter and Cohen’s change model has the
following stages.
• Creating a sense of urgency
• Forming a team
• Creating a vision and strategy
• Sharing the vision
• Removing hindrances to successful change
• Discovering interim successes
• Forging persistence
• Encouraging the new culture (Melnyk &
Fineout-Overholt, 2015)
CHANGE MODEL
• Kotter and Cohen’s change model has the
following stages.
• Creating a sense of urgency
• Forming a team
• Creating a vision and strategy
• Sharing the vision
• Removing hindrances to successful change
• Discovering interim successes
• Forging persistence
• Encouraging the new culture (Melnyk &
Fineout-Overholt, 2015)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

IMPLEMENTATION OF IOWA
MODEL
• Problem focused triggers
– Process improvement data
– risk management data
– External or internal benchmarking data
– Financial data
– Clinical problem identification
• Knowledge-focused triggers
– Current, new research
– Organizational standards and guidelines
– Care philosophies
– Questions from institutional standards
committee
PICO Question
Problem: high rates of urinary tract infections associated with use of catheters
Intervention: use of new silicone catheters
Comparison: Common latex catheters
Outcome: Reduced rates of urinary tract infections linked to catheter use
Does use of silicone catheters in comparison to common latex catheters within one
month reduce the rate of occurrence of urinary tract infections associated with
catheter use?
MODEL
• Problem focused triggers
– Process improvement data
– risk management data
– External or internal benchmarking data
– Financial data
– Clinical problem identification
• Knowledge-focused triggers
– Current, new research
– Organizational standards and guidelines
– Care philosophies
– Questions from institutional standards
committee
PICO Question
Problem: high rates of urinary tract infections associated with use of catheters
Intervention: use of new silicone catheters
Comparison: Common latex catheters
Outcome: Reduced rates of urinary tract infections linked to catheter use
Does use of silicone catheters in comparison to common latex catheters within one
month reduce the rate of occurrence of urinary tract infections associated with
catheter use?
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

FORMATION OF A TEAM
Decision Point 1
Ye
s
Is this
topic a
priority
for the
organiza
tion?
No
Consider
other
triggers
Form a
team
The formed team will be
comprised of nurses,
physicians, doctors, and
management staff. Most of
the members will be
Decision Point 1
Ye
s
Is this
topic a
priority
for the
organiza
tion?
No
Consider
other
triggers
Form a
team
The formed team will be
comprised of nurses,
physicians, doctors, and
management staff. Most of
the members will be

ASSEMBLE RELEVANT RESEARCH
& RELATED LITERATURE
S OU R C E S O F IN F O R M AT I ON
– Electronic databases to be used
• Cinahl
• Cochrane
• Medlin
– National Institute of Health and
Clinical Excellence guidelines
KE Y WO R D S T O BE US E D
• Urinary tract infections
• Catheter associated infections
• Silicone catheters
• Latex catheters
• Rate of infections
The team will target to retrieve strongest evidence and that of highest quality to
answer the PICO question
Randomized controlled trials will be targeted as they are more rigorously designed
& RELATED LITERATURE
S OU R C E S O F IN F O R M AT I ON
– Electronic databases to be used
• Cinahl
• Cochrane
• Medlin
– National Institute of Health and
Clinical Excellence guidelines
KE Y WO R D S T O BE US E D
• Urinary tract infections
• Catheter associated infections
• Silicone catheters
• Latex catheters
• Rate of infections
The team will target to retrieve strongest evidence and that of highest quality to
answer the PICO question
Randomized controlled trials will be targeted as they are more rigorously designed
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

CRITIQUE & SYNTHESIZE RESEARCH
FOR UTILIZATION IN PRACTICE
• After gathering the evidence the next step would
involve critically appraising the evidence
• the team will review every evidence piece
individually to determine its quality
• An appropriate appraisal tool will be chosen as a
guide for the process
• For instance, if all retrieved researches will be
randomized controlled trials then the appropriate
instrument for this design will be used
• The team will then make recommendations for
practice through synthesis of findings across the
reviewed evidence
• The team will decide whether the found evidence
is strong enough
Pilot the change
In practice
Is there
a
sufficie
nt
researc
h base?
Ye
s
No
Base practice on other
evidence types such
as case reports,
scientific principles,
expert opinions, and
Conduct
research
FOR UTILIZATION IN PRACTICE
• After gathering the evidence the next step would
involve critically appraising the evidence
• the team will review every evidence piece
individually to determine its quality
• An appropriate appraisal tool will be chosen as a
guide for the process
• For instance, if all retrieved researches will be
randomized controlled trials then the appropriate
instrument for this design will be used
• The team will then make recommendations for
practice through synthesis of findings across the
reviewed evidence
• The team will decide whether the found evidence
is strong enough
Pilot the change
In practice
Is there
a
sufficie
nt
researc
h base?
Ye
s
No
Base practice on other
evidence types such
as case reports,
scientific principles,
expert opinions, and
Conduct
research
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

PILOT CHANGE IN PRACTICE
• Selecting outcomes to be achieved
– To reduce catheter associated urinary tract infection
• Collecting baseline data
– Number of diagnosed urinary tract infections in past 2 weeks
– Types of catheters used in past 2 weeks
• Designing EBP guidelines
– Consistent communication
– Teaching of staff and patients
• Implementing EBP on pilot units
– 1 July 2019-starting implementation
– Silicone catheters availed and replaces latex catheters
– Only silicone catheters are used for the next two weeks in the words that are pilot tested
• Evaluating process and outcomes
– 15 July 2019 data is reviewed to determine the rate of occurrence of urinary tract infections
• Modifying practice guidelines
– Silicone catheters to be provided to hospital as replacement to latex catheters
• Selecting outcomes to be achieved
– To reduce catheter associated urinary tract infection
• Collecting baseline data
– Number of diagnosed urinary tract infections in past 2 weeks
– Types of catheters used in past 2 weeks
• Designing EBP guidelines
– Consistent communication
– Teaching of staff and patients
• Implementing EBP on pilot units
– 1 July 2019-starting implementation
– Silicone catheters availed and replaces latex catheters
– Only silicone catheters are used for the next two weeks in the words that are pilot tested
• Evaluating process and outcomes
– 15 July 2019 data is reviewed to determine the rate of occurrence of urinary tract infections
• Modifying practice guidelines
– Silicone catheters to be provided to hospital as replacement to latex catheters
INSTITUTING CHANGE AND MONITORING
AND ANALYZING STRUCTURE, PROCESS,
AND OUTCOME DATA
• To institute change evidence-based guidelines will be used and kotter’s change model will be used
to cultivate change
• A sense of urgency will be created by sensitizing staff on the high rate of urinary tract infections
reported after catheter use and the associated social and economic outcomes.
• The same team developed to implement Iowa model will be used. More leaders will be added
• Vision
– To ensure reduction of occurrence of catheter associated urinary tract infections by 50% within one
month of change enactment
• The vision will be communicated by engaging in constant dialogue with stakeholders. Here, direct
interactions between care providers, leaders, and organization at large will be considered to
support change enactment
• The benefits of the change will be communicated to all stakeholders
AND ANALYZING STRUCTURE, PROCESS,
AND OUTCOME DATA
• To institute change evidence-based guidelines will be used and kotter’s change model will be used
to cultivate change
• A sense of urgency will be created by sensitizing staff on the high rate of urinary tract infections
reported after catheter use and the associated social and economic outcomes.
• The same team developed to implement Iowa model will be used. More leaders will be added
• Vision
– To ensure reduction of occurrence of catheter associated urinary tract infections by 50% within one
month of change enactment
• The vision will be communicated by engaging in constant dialogue with stakeholders. Here, direct
interactions between care providers, leaders, and organization at large will be considered to
support change enactment
• The benefits of the change will be communicated to all stakeholders
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

CONT..
• Action will be empowered by providing the engaged parties with feedback
regarding progress and showing them the areas of improvement
• The short-term wins will be made clear. For instance, weekly reduction in
rate of occurrence of urinary tract infections will be communicated and staff
congratulated for their roles in making it happen
• These changes will then be made a standard of practice
• The environment, staff, cost, and patient and family will then be monitored
• Dissemination of findings will then be done
• Action will be empowered by providing the engaged parties with feedback
regarding progress and showing them the areas of improvement
• The short-term wins will be made clear. For instance, weekly reduction in
rate of occurrence of urinary tract infections will be communicated and staff
congratulated for their roles in making it happen
• These changes will then be made a standard of practice
• The environment, staff, cost, and patient and family will then be monitored
• Dissemination of findings will then be done
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

REFERENCES
• Hopp, L., & Rittenmeyer, L. (2012). Introduction to evidence-based practice:
A practical guide for nursing. Philadelphia: F.A. Davis Company.
• LoBiondo-Wood, G., Haber, J., & Titler, M. G. (2018). Evidence-Based
Practice for Nursing and Healthcare Quality Improvement - E-Book. Mosby
• Melnyk, B. M. & Fineout-Overholt, E. (2015). Evidence-based practice in
nursing & healthcare: A guide to best practice (3rd ed.) Philadelphia, PA:
Wolters Kluwer Health
• Hopp, L., & Rittenmeyer, L. (2012). Introduction to evidence-based practice:
A practical guide for nursing. Philadelphia: F.A. Davis Company.
• LoBiondo-Wood, G., Haber, J., & Titler, M. G. (2018). Evidence-Based
Practice for Nursing and Healthcare Quality Improvement - E-Book. Mosby
• Melnyk, B. M. & Fineout-Overholt, E. (2015). Evidence-based practice in
nursing & healthcare: A guide to best practice (3rd ed.) Philadelphia, PA:
Wolters Kluwer Health
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





