University Nursing Care Plan: Schizophrenia Recovery and Management
VerifiedAdded on 2022/09/26
|26
|5653
|21
Essay
AI Summary
This essay develops an evidence-based nursing care plan for a 52-year-old male patient, Tom, diagnosed with schizophrenia, focusing on addressing auditory hallucinations and self-care deficits. The care plan incorporates a person-centered approach, emphasizing therapeutic communication, psychological education, and adherence to medication. The analysis delves into the nature of hallucinations, the importance of empathy, and the application of the stress-vulnerability model to understand the patient's condition. Nursing interventions include cognitive behavioral therapy (CBT), art therapy, music therapy, and family involvement. The essay highlights the significance of promoting self-help strategies, ensuring medication adherence, and providing a supportive environment to facilitate the patient's recovery. Ethical considerations are addressed, ensuring patient confidentiality and rights. The plan aims to improve the patient's psychological and physiological state, manage symptoms, and promote long-term well-being.

Running head: MENTAL HEALTH NURSING
MENTAL HEALTH NURSING
Name of the student:
Name of the university:
Author note
MENTAL HEALTH NURSING
Name of the student:
Name of the university:
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
MENTAL HEALTH NURSING
Introduction:
Introduction:
The purpose of the essay is to develop an evidence-based nursing care plan to support the
recovery of a patient diagnosed with schizophrenia. In order to develop an effective patient-
centered care plan, this essay will consider evidence-based approaches and set goals based on the
patient needs and requirements to render high quality person-centered care (Morin and Franck
2017). It is very important that as a psychiatric intensive care unit nurse, it is very important to
facilitate communication with the subject in order to develop rapport for a better person centered
care (Martin and Higueras 2016). This paper will apply the knowledge of legal and ethical
concepts within the context of professional practice. This essay also aimed to analyses the
practice regarding drug administration and side effects of drugs, interaction and sensitivity in
order to provide patient psychoeducation and thus aims to creat awareness and insight into their
own illness (Lazzari et al. 2015).
All names mentioned are changed for maintaining confidentiality aligned with Nursing
and Midwifery Council Code of Conduct (NMC 2017) and the Data Protection Act (1998).
Discussion:
Description:
Tom is a 52 year old male, brought to the hospital by the police under section-136 to the
acute ward as he is creating tension in the traffic by trying to stop all the cars in the middle of the
traffic which may lead to the accidents. When he arrived ward, he appears restless, chaotic and
observed to have visible wounds on his feet. Tom visibly looks like he is completely neglecting
his hygienic care needs as he has got unexplained injuries, unkempt appearance and unpleasant
MENTAL HEALTH NURSING
Introduction:
Introduction:
The purpose of the essay is to develop an evidence-based nursing care plan to support the
recovery of a patient diagnosed with schizophrenia. In order to develop an effective patient-
centered care plan, this essay will consider evidence-based approaches and set goals based on the
patient needs and requirements to render high quality person-centered care (Morin and Franck
2017). It is very important that as a psychiatric intensive care unit nurse, it is very important to
facilitate communication with the subject in order to develop rapport for a better person centered
care (Martin and Higueras 2016). This paper will apply the knowledge of legal and ethical
concepts within the context of professional practice. This essay also aimed to analyses the
practice regarding drug administration and side effects of drugs, interaction and sensitivity in
order to provide patient psychoeducation and thus aims to creat awareness and insight into their
own illness (Lazzari et al. 2015).
All names mentioned are changed for maintaining confidentiality aligned with Nursing
and Midwifery Council Code of Conduct (NMC 2017) and the Data Protection Act (1998).
Discussion:
Description:
Tom is a 52 year old male, brought to the hospital by the police under section-136 to the
acute ward as he is creating tension in the traffic by trying to stop all the cars in the middle of the
traffic which may lead to the accidents. When he arrived ward, he appears restless, chaotic and
observed to have visible wounds on his feet. Tom visibly looks like he is completely neglecting
his hygienic care needs as he has got unexplained injuries, unkempt appearance and unpleasant
2
MENTAL HEALTH NURSING
body odor which can be due to hygiene issues. Tom believes that he hasn’t done nothing wTomg
and he thinks he is absolutely fine. Tom has been assessed by the Mental health team and been
decided by the team to admit him to the ward under section-2 of the mental health act 1983 for
his own safety and safety of others for his assessment and treatment purposes. Tom is refusing
his medications too as he believes that there is nothing wTomg with him. As a student nurse I
have taken the initiation to make him comfortable as he brought in police van it will be a
daunting experience so offered him drink and some food and eventually sat with him read his
initially section 136 rights and also when he got admitted to the ward as he is placed on section-
2. I have gone through the section-2 rights and ensure he understood them. Initially he was
nursed on the low-stimulus environment to keep him away from the loud noises and ward
environment.
According to the Maslow’s hierarchy of needs, I need to prioritize my goals, as the voices are
distressing to him. My main aim is to lower the distress caused due to voices and long term goal
is to terminate the voices. Other problem is self-care-deficit evidenced by poor personal hygiene
and lack of self-worth (Gage and Munafò 2015). In this essay I am going to focus on these two
problems and formulate a care plan with the patient to render effective care. My other focus will
be on psychological education which creates awareness and explain importance of taking
medication and to provide least restrictive recovery focused care.
As a psychiatric intensive care unit nurse, it is important that treat and care for Tom in a
very person centered way and take up a humanistic approach in order to heal and treat the
underpinnings of the problem from within. It is important that the behavioral modification is
done to the patient as a clinical or rather a psycho-social outcome and for that, building an
effective therapeutic communication with the patient is critical to the care process (Gage and
MENTAL HEALTH NURSING
body odor which can be due to hygiene issues. Tom believes that he hasn’t done nothing wTomg
and he thinks he is absolutely fine. Tom has been assessed by the Mental health team and been
decided by the team to admit him to the ward under section-2 of the mental health act 1983 for
his own safety and safety of others for his assessment and treatment purposes. Tom is refusing
his medications too as he believes that there is nothing wTomg with him. As a student nurse I
have taken the initiation to make him comfortable as he brought in police van it will be a
daunting experience so offered him drink and some food and eventually sat with him read his
initially section 136 rights and also when he got admitted to the ward as he is placed on section-
2. I have gone through the section-2 rights and ensure he understood them. Initially he was
nursed on the low-stimulus environment to keep him away from the loud noises and ward
environment.
According to the Maslow’s hierarchy of needs, I need to prioritize my goals, as the voices are
distressing to him. My main aim is to lower the distress caused due to voices and long term goal
is to terminate the voices. Other problem is self-care-deficit evidenced by poor personal hygiene
and lack of self-worth (Gage and Munafò 2015). In this essay I am going to focus on these two
problems and formulate a care plan with the patient to render effective care. My other focus will
be on psychological education which creates awareness and explain importance of taking
medication and to provide least restrictive recovery focused care.
As a psychiatric intensive care unit nurse, it is important that treat and care for Tom in a
very person centered way and take up a humanistic approach in order to heal and treat the
underpinnings of the problem from within. It is important that the behavioral modification is
done to the patient as a clinical or rather a psycho-social outcome and for that, building an
effective therapeutic communication with the patient is critical to the care process (Gage and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
MENTAL HEALTH NURSING
Munafò, 2015). As per the NICE guidelines, the psychotic disorders such as schizophrenia,
schizophreniform disorder, delusional disorder. Schizoaffective disorder needs a specific type of
nursing care and I will follow the same to recognize, treat and manage the affective psychoses
associated with Tom’s case.
ANALYSIS
Hallucinations come in many forms and is a common feature of schizophrenia and related
disorders. Hallucinations are false perceptions of things that are actually not present and these
hallucinations are of different types – visual, auditory, olfactory, gustatory and even tactile
(Www.nhs.uk 2019). It can even be thermo-receptive, chemoreceptive and nociceptive. Hence,
in case of Tom, as a psychiatric intensive care unit nurse, I have to take care of the psychosocial
issue that has led to denial state in which Tom believes he has not done anything (despite the fact
he has created a scene in the traffic trying to stop other cars). Auditory hallucinations are very
common in schizophrenia which is the case with Tom. The subject in a psychosocial state of
denial and the state is very strong that is defending itself from within. Therefore, before changing
the behavioral pattern of the subject which is the second part of my nursing intervention – at
first, it is important that I talk to the patient politely with demonstration of compassion and
kindness and be humanistic while assessing his psychological and psychosocial state with
empathy (Www.nice.org.uk 2019). Empathy is a very important tool that can evoke a very strong
response in this case in order to know and understand the underlying hallucination, memory,
behavioral and emotional issues associated with Tom’s present mental state ( as per the NICE
guidelines ) (Richardson, Percy and Hughes 2015).
There are injuries in Tom’s body for which he do not have any logical reasons which can
be indicative of a deep seated amnesia underpinning the case as well. In my nursing assessment
MENTAL HEALTH NURSING
Munafò, 2015). As per the NICE guidelines, the psychotic disorders such as schizophrenia,
schizophreniform disorder, delusional disorder. Schizoaffective disorder needs a specific type of
nursing care and I will follow the same to recognize, treat and manage the affective psychoses
associated with Tom’s case.
ANALYSIS
Hallucinations come in many forms and is a common feature of schizophrenia and related
disorders. Hallucinations are false perceptions of things that are actually not present and these
hallucinations are of different types – visual, auditory, olfactory, gustatory and even tactile
(Www.nhs.uk 2019). It can even be thermo-receptive, chemoreceptive and nociceptive. Hence,
in case of Tom, as a psychiatric intensive care unit nurse, I have to take care of the psychosocial
issue that has led to denial state in which Tom believes he has not done anything (despite the fact
he has created a scene in the traffic trying to stop other cars). Auditory hallucinations are very
common in schizophrenia which is the case with Tom. The subject in a psychosocial state of
denial and the state is very strong that is defending itself from within. Therefore, before changing
the behavioral pattern of the subject which is the second part of my nursing intervention – at
first, it is important that I talk to the patient politely with demonstration of compassion and
kindness and be humanistic while assessing his psychological and psychosocial state with
empathy (Www.nice.org.uk 2019). Empathy is a very important tool that can evoke a very strong
response in this case in order to know and understand the underlying hallucination, memory,
behavioral and emotional issues associated with Tom’s present mental state ( as per the NICE
guidelines ) (Richardson, Percy and Hughes 2015).
There are injuries in Tom’s body for which he do not have any logical reasons which can
be indicative of a deep seated amnesia underpinning the case as well. In my nursing assessment
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
MENTAL HEALTH NURSING
where I observed Tom’s body language and psychological state closely and found out that the
subject is very chaotic and restless which I clinically reasoned – to have occurred due to some
internal negative stimuli or rather a thought that is continuously troubling him and the
aforementioned ‘defense mechanisms’ is not allowing Tom to express the issue clearly. The
injuries are signs that something noxious might have happened to him. These can even be self-
harm behaviors that is typical of schizophrenia (Uhlmann, Pizarro and Diermeier 2015). The self
-harm behavior could have been triggered due to the auditory hallucinations. As a nurse, it is
critical I talk to him about that has been troubling him and who else are there in his family
(Oliveira, Carvalho and Esteves 2016.). If the communication with the patient works properly, I
would be able to ring over his family member to come to the PICU unit and help me with the
patient’s history and condition (Yong-Shian et al. 2016). Secondly, a very important part of my
nursing intervention with a humanistic approach will be helping Tom with self-help and personal
hygiene strategies for the self-deficit problem. The humanistic approach of nursing, will focus on
fulfilling the subject’s physiological, social, belonging, safety, esteem and self-actualization
needs in a step wise manner (Hayes et al. 2017). Reflecting on my nursing assessment and
humanistic intervention – I shall be able to understand that what level – lies the clinical or the
psycho social deficiency as any of the deficiency at any level can lead to further derangement or
extreme physical or behavioral outbursts in psychotic subjects like Tom.
I would incorporate the Stress vulnerability model, in my nursing acre plan in order to
decipher the genetic and socio psychological predispositions to the mental derangement in Tom.
Taking family history and knowing about would provide me with the information about the
genetic actor being involved in the case. Identifying the physiological intricacies is another
important or rather a vital nursing strategy to develop the care plan for Tom. There can be
MENTAL HEALTH NURSING
where I observed Tom’s body language and psychological state closely and found out that the
subject is very chaotic and restless which I clinically reasoned – to have occurred due to some
internal negative stimuli or rather a thought that is continuously troubling him and the
aforementioned ‘defense mechanisms’ is not allowing Tom to express the issue clearly. The
injuries are signs that something noxious might have happened to him. These can even be self-
harm behaviors that is typical of schizophrenia (Uhlmann, Pizarro and Diermeier 2015). The self
-harm behavior could have been triggered due to the auditory hallucinations. As a nurse, it is
critical I talk to him about that has been troubling him and who else are there in his family
(Oliveira, Carvalho and Esteves 2016.). If the communication with the patient works properly, I
would be able to ring over his family member to come to the PICU unit and help me with the
patient’s history and condition (Yong-Shian et al. 2016). Secondly, a very important part of my
nursing intervention with a humanistic approach will be helping Tom with self-help and personal
hygiene strategies for the self-deficit problem. The humanistic approach of nursing, will focus on
fulfilling the subject’s physiological, social, belonging, safety, esteem and self-actualization
needs in a step wise manner (Hayes et al. 2017). Reflecting on my nursing assessment and
humanistic intervention – I shall be able to understand that what level – lies the clinical or the
psycho social deficiency as any of the deficiency at any level can lead to further derangement or
extreme physical or behavioral outbursts in psychotic subjects like Tom.
I would incorporate the Stress vulnerability model, in my nursing acre plan in order to
decipher the genetic and socio psychological predispositions to the mental derangement in Tom.
Taking family history and knowing about would provide me with the information about the
genetic actor being involved in the case. Identifying the physiological intricacies is another
important or rather a vital nursing strategy to develop the care plan for Tom. There can be
5
MENTAL HEALTH NURSING
problems with working of the Hypothalamus – pituitary- axis and the neurodegeneration of the
hippocampus and memory consolidation areas can lead to behavioral suppression, apathy and
idiopathic anxiety in the subject leading to complex neuro psychological presentations and
related symptoms of amnesia, aggression, social detachment and social withdrawal,
hallucinations as well (Ulin et al. 2016). Hence comply with psychiatric nursing practice with the
stress – vulnerability model – I must closely follow the hematological and metabolic reports of
the patients in order to understand and diagnose the physiological underlying the case. My
nursing intervention will include making sure that the patient receives a proper diet, nutrition and
sleep that restores the distorted neuro biological rhythms leading to anxiety, chaotic and
restlessness in the patient (Bighelli et al. 2018). Promoting sleep, relaxation and adherence to
activities of daily life in Tom would help better his psychological and physiological state. My
nursing care plan should include fulfillment of the patient’s covert drives and needs – eating,
sleeping, social, socio cultural, emotional, belonging and psychosocial needs (Priebe et al. 2016).
Using he stress vulnerability model, the three important factors such as biological vulnerability
(the unfulfilled level at Maslow’s hierarchy of needs), the stress (that is disturbing the patient)
and the protective factors (the defense mechanisms such as ego, repression and outbursts) needs
to diagnosed and addressed very closely.
In order to manage the auditory hallucinations which is a chief symptom in Tom – I will
incorporating CBT and other procedures in the nursing management (Dellazizzo et al., 2018). At
first I will question the patient and show genuine interest in his auditory hallucinations (in order
to engage the patient). The second step would be to normalize the hallucination where I will ask
Tom whether he agrees with rationalized explanation acting behind the auditory hallucination
which can be sleep deprivation, AOD abuse, social isolation, stress and conflicting emotions and
MENTAL HEALTH NURSING
problems with working of the Hypothalamus – pituitary- axis and the neurodegeneration of the
hippocampus and memory consolidation areas can lead to behavioral suppression, apathy and
idiopathic anxiety in the subject leading to complex neuro psychological presentations and
related symptoms of amnesia, aggression, social detachment and social withdrawal,
hallucinations as well (Ulin et al. 2016). Hence comply with psychiatric nursing practice with the
stress – vulnerability model – I must closely follow the hematological and metabolic reports of
the patients in order to understand and diagnose the physiological underlying the case. My
nursing intervention will include making sure that the patient receives a proper diet, nutrition and
sleep that restores the distorted neuro biological rhythms leading to anxiety, chaotic and
restlessness in the patient (Bighelli et al. 2018). Promoting sleep, relaxation and adherence to
activities of daily life in Tom would help better his psychological and physiological state. My
nursing care plan should include fulfillment of the patient’s covert drives and needs – eating,
sleeping, social, socio cultural, emotional, belonging and psychosocial needs (Priebe et al. 2016).
Using he stress vulnerability model, the three important factors such as biological vulnerability
(the unfulfilled level at Maslow’s hierarchy of needs), the stress (that is disturbing the patient)
and the protective factors (the defense mechanisms such as ego, repression and outbursts) needs
to diagnosed and addressed very closely.
In order to manage the auditory hallucinations which is a chief symptom in Tom – I will
incorporating CBT and other procedures in the nursing management (Dellazizzo et al., 2018). At
first I will question the patient and show genuine interest in his auditory hallucinations (in order
to engage the patient). The second step would be to normalize the hallucination where I will ask
Tom whether he agrees with rationalized explanation acting behind the auditory hallucination
which can be sleep deprivation, AOD abuse, social isolation, stress and conflicting emotions and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
MENTAL HEALTH NURSING
this step of CBT should treat the hallucination (Jauhar, Laws & McKenna, 2019). Then, I will
teach him coping strategies such as listening to songs, talking with others, having a social group,
exercise and taking care of himself (self-hygiene) as important tools to counter and cope with the
hallucinations. Explaining briefly the neurobiology (revealed from stress vulnerability model) to
Tom, would help him realize the presenting symptom by himself as well. On a weekly basis, to
keep Tom distracted, I decided to take him to music classes and art classes as art therapy and
music therapy has been reported by many researches to synchronize the brain waves and return
sanity to the subject with development of personal skills such as stress management, emotional
intelligence, patience, endurance and calmness. Other than that, my nursing plan will also have a
morning and evening walk for Tom where he can be in touch with the healing environment of
therapeutic gardens in our hospital, under my supervision. Distracting the patient from evoking
the noxious stimuli present within and then making the negative and distressing emotions
reconcile with his positive and profound side – shall be an important part of my nursing
intervention. Acting with empathy, politeness and talk therapy as a psycho therapeutic tool – I
would be able to gain Tom’s trust and help him get better, clinically and psychosocially.
Forgetting the medications can lead to array of other aggravated problems and care has to
be taken to ensure that Tom is adhering to the prescribed medications (Shattock et al. 2018).
Providing memory support by usage of memory aids and memory tracking exercises, I will be
able to help Tom adhere to the activities of daily life like eating, sleeping and hygiene needs, in a
more effective manner for addressing the self-care deficits (Wang et al. 2015). Incorporating a
therapeutic counselling such as CBT (cognitive behavioral therapy), talk therapy will be the
other important mental health nursing tools that according to the NICE guidelines, would help
me better the behavioral (Escott-Price et al. 2019) cognitive, emotional, hallucinatory,
MENTAL HEALTH NURSING
this step of CBT should treat the hallucination (Jauhar, Laws & McKenna, 2019). Then, I will
teach him coping strategies such as listening to songs, talking with others, having a social group,
exercise and taking care of himself (self-hygiene) as important tools to counter and cope with the
hallucinations. Explaining briefly the neurobiology (revealed from stress vulnerability model) to
Tom, would help him realize the presenting symptom by himself as well. On a weekly basis, to
keep Tom distracted, I decided to take him to music classes and art classes as art therapy and
music therapy has been reported by many researches to synchronize the brain waves and return
sanity to the subject with development of personal skills such as stress management, emotional
intelligence, patience, endurance and calmness. Other than that, my nursing plan will also have a
morning and evening walk for Tom where he can be in touch with the healing environment of
therapeutic gardens in our hospital, under my supervision. Distracting the patient from evoking
the noxious stimuli present within and then making the negative and distressing emotions
reconcile with his positive and profound side – shall be an important part of my nursing
intervention. Acting with empathy, politeness and talk therapy as a psycho therapeutic tool – I
would be able to gain Tom’s trust and help him get better, clinically and psychosocially.
Forgetting the medications can lead to array of other aggravated problems and care has to
be taken to ensure that Tom is adhering to the prescribed medications (Shattock et al. 2018).
Providing memory support by usage of memory aids and memory tracking exercises, I will be
able to help Tom adhere to the activities of daily life like eating, sleeping and hygiene needs, in a
more effective manner for addressing the self-care deficits (Wang et al. 2015). Incorporating a
therapeutic counselling such as CBT (cognitive behavioral therapy), talk therapy will be the
other important mental health nursing tools that according to the NICE guidelines, would help
me better the behavioral (Escott-Price et al. 2019) cognitive, emotional, hallucinatory,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
MENTAL HEALTH NURSING
delusionary and social distortions of the patient’s thought patterns (Selten, van Os and Cantor‐
Graae 2016). It is increasingly important that as a psychiatric intensive care nurse, I shall be re-
evoking hope and positivism in the patient through reconciliation of his social and emotional
relationship with his mother. The agitation and distress will be addressed by managing his
sleeping and eating habits (Degnan et al. 2018). These are the major symptoms of schizophrenia
that has to be addressed, in a nursing care plan. Strengthening the social framework of Tom with
fostering of better meaningful relationships with his friends and family is important and the
nursing care plan would also monitor Tom for dangerous self-harm behavior and eliminating the
same. The auditory hallucinations are reported by Tom as he has been hearing voices can be
treated by helping the subject attach back with the social environment more firmly and being
fully aware of himself and the physical, social environment. Promoting hope, trust and
confidence in the patient is critical and it is important my nursing intervention shall be able to
foster it.
EVALUATION
Daily evaluation as well as taking weekly assessments is critical to proper management and
faster recovery of the patient. As suggested by different research studies, the art and the music
therapies are very beneficial to the recovery of a schizophrenia case but it has also been
emphasized that the programs should be continued for a period of time in order to aid the patient
receive the full benefits of the therapy. I would check the behavioral patterns of Tom in order to
evaluate the process of recovery and level of improvement achieved by the patient at the end of
the day. I can collaborate my nursing care plan with a psychologist’s support for the essence of
understanding the recovery and prognosis of Tom from a behavioral and cognitive point of view.
MENTAL HEALTH NURSING
delusionary and social distortions of the patient’s thought patterns (Selten, van Os and Cantor‐
Graae 2016). It is increasingly important that as a psychiatric intensive care nurse, I shall be re-
evoking hope and positivism in the patient through reconciliation of his social and emotional
relationship with his mother. The agitation and distress will be addressed by managing his
sleeping and eating habits (Degnan et al. 2018). These are the major symptoms of schizophrenia
that has to be addressed, in a nursing care plan. Strengthening the social framework of Tom with
fostering of better meaningful relationships with his friends and family is important and the
nursing care plan would also monitor Tom for dangerous self-harm behavior and eliminating the
same. The auditory hallucinations are reported by Tom as he has been hearing voices can be
treated by helping the subject attach back with the social environment more firmly and being
fully aware of himself and the physical, social environment. Promoting hope, trust and
confidence in the patient is critical and it is important my nursing intervention shall be able to
foster it.
EVALUATION
Daily evaluation as well as taking weekly assessments is critical to proper management and
faster recovery of the patient. As suggested by different research studies, the art and the music
therapies are very beneficial to the recovery of a schizophrenia case but it has also been
emphasized that the programs should be continued for a period of time in order to aid the patient
receive the full benefits of the therapy. I would check the behavioral patterns of Tom in order to
evaluate the process of recovery and level of improvement achieved by the patient at the end of
the day. I can collaborate my nursing care plan with a psychologist’s support for the essence of
understanding the recovery and prognosis of Tom from a behavioral and cognitive point of view.
8
MENTAL HEALTH NURSING
A psychological evaluation after every one week is important that would reveal the cognitive,
behavioral, emotional and personality parameters of the patient (Hagen, Knizek and Hjelmeland
2017). Looking at the progress, the nursing care plan take add new interventions such as
recreational activities like keeping a journal by the patient where he would monitor his own
feelings and emotions, thus becoming aware of it and being able to manage his emotions in a
more profound way. New self-management strategies will be incorporated in the psychiatric
acute care nursing plan while the old stress management and self-management strategies (such as
emotional quotient strategies) will be extended, after the evaluation of the patient’s state. The
family support framework shall be strengthened in order to foster an effective psychosocial care.
Based on evaluation of the available evidence and clinical reasoning cycle – the housing, family,
work support will be integrated in the mental nursing care. The functional independence has to
be measured on a daily basis and Tom’s activities of daily life practices should be monitored on
a regular basis. The food, thirst and sleep drives should be made rhythmic and more balanced so
that Tom refrains from any aggressive, unusual and violent exhibition of behaviors.
I have learned that reducing agitation and anxiety disorder is a critical nursing
intervention and care must be taken – that any approach (psychological, behavioral or
psychosocial) if does not proves to be that effective as expected – then it should be immediately
changed and alternate approaches must be planned on a critical note. Helping the patient with the
right medications at the right time would increase medication adherence and rapid recovery.
Through counselling sessions and talk therapies – the stimulus that is irritating or triggering a
negative response out of the patient – must be recognized. Next, the nursing plan should take
care of preventing the noxious stimuli (which can be a memory, a behavior, a particular object,
person or environment) from presenting itself in fromt of the subject. If presented by any chance,
MENTAL HEALTH NURSING
A psychological evaluation after every one week is important that would reveal the cognitive,
behavioral, emotional and personality parameters of the patient (Hagen, Knizek and Hjelmeland
2017). Looking at the progress, the nursing care plan take add new interventions such as
recreational activities like keeping a journal by the patient where he would monitor his own
feelings and emotions, thus becoming aware of it and being able to manage his emotions in a
more profound way. New self-management strategies will be incorporated in the psychiatric
acute care nursing plan while the old stress management and self-management strategies (such as
emotional quotient strategies) will be extended, after the evaluation of the patient’s state. The
family support framework shall be strengthened in order to foster an effective psychosocial care.
Based on evaluation of the available evidence and clinical reasoning cycle – the housing, family,
work support will be integrated in the mental nursing care. The functional independence has to
be measured on a daily basis and Tom’s activities of daily life practices should be monitored on
a regular basis. The food, thirst and sleep drives should be made rhythmic and more balanced so
that Tom refrains from any aggressive, unusual and violent exhibition of behaviors.
I have learned that reducing agitation and anxiety disorder is a critical nursing
intervention and care must be taken – that any approach (psychological, behavioral or
psychosocial) if does not proves to be that effective as expected – then it should be immediately
changed and alternate approaches must be planned on a critical note. Helping the patient with the
right medications at the right time would increase medication adherence and rapid recovery.
Through counselling sessions and talk therapies – the stimulus that is irritating or triggering a
negative response out of the patient – must be recognized. Next, the nursing plan should take
care of preventing the noxious stimuli (which can be a memory, a behavior, a particular object,
person or environment) from presenting itself in fromt of the subject. If presented by any chance,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
MENTAL HEALTH NURSING
care must be taken to ‘desensitize’ the patient with the correct psychosocial approaches. I would
like to apply the same in my future approaches.
CONCLUSION
Hence it can be concluded saying that in schizophrenic and related cases, the nursing care of plan
must be directed towards a humanistic approach where the patient’s hygiene, esteem and social
needs should be addressed with complete integrity, totality and autonomy. The nursing
intervention must start with assessment of the patient’s symptoms such as apathy, social
withdrawal and detachment, aggression, hallucination and the underlying causes that might have
triggered it. Recreational activities along with ADL activities adherence should be promoted in
the patient and the mental health care nurse must take care of the defense mechanisms and
emotional outbursts of the subject pertinently. Medication adherence should be improved and
self-harm behaviors should be checked.
CARE PLAN FOR TOM
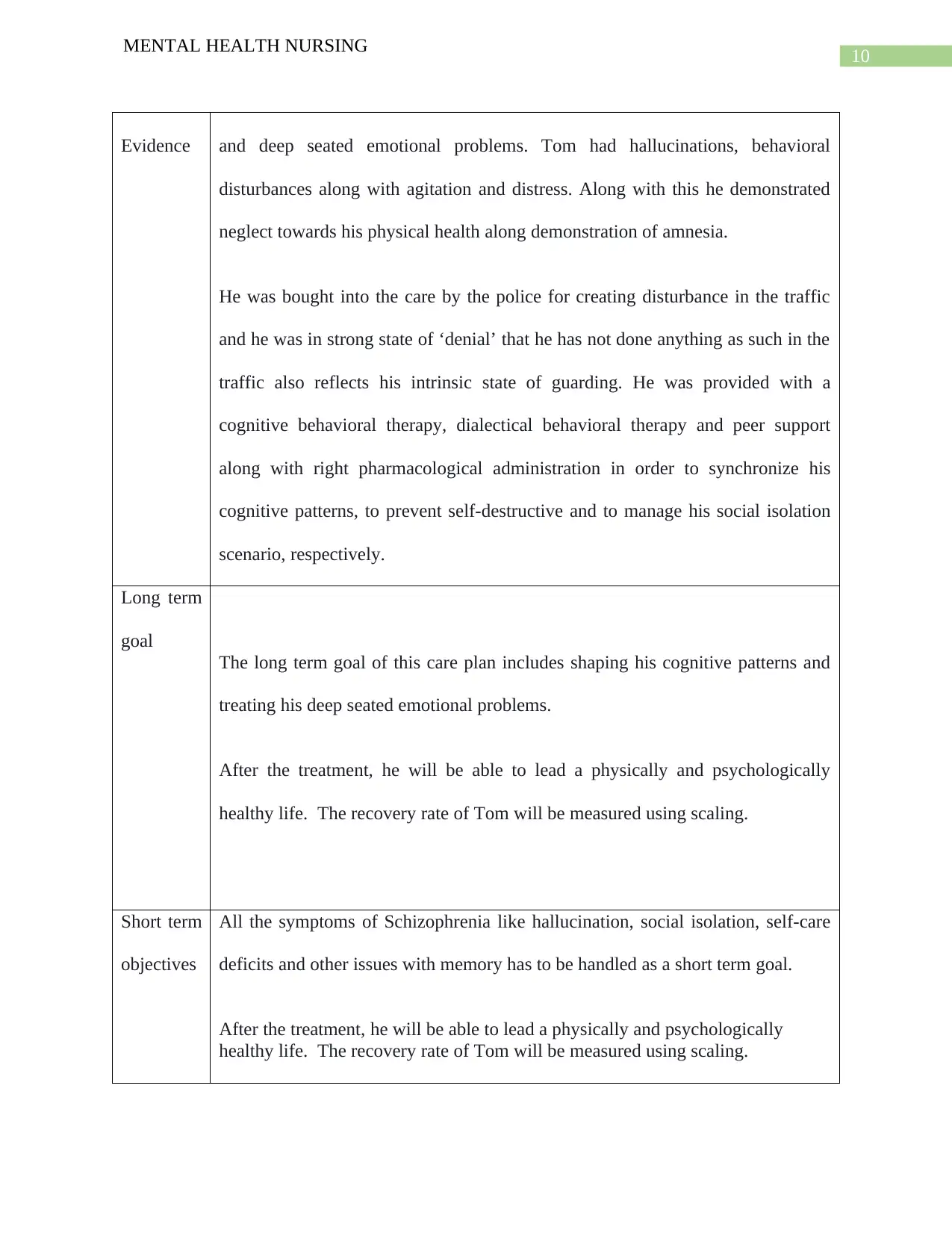
Problem
Evidence
SCHIZOPHRENIA
Hallucination, Social isolation, self-care deficits, sleep disorder and ineffective
coping mechanism.
Initially, Tom has auditory hallucination (as he reports hearing voices) along self-
care deficits, unusual behavior with memory problems. He also has possibly self-
harm behavior which might have resulted from a prolonged social withdrawal
MENTAL HEALTH NURSING
care must be taken to ‘desensitize’ the patient with the correct psychosocial approaches. I would
like to apply the same in my future approaches.
CONCLUSION
Hence it can be concluded saying that in schizophrenic and related cases, the nursing care of plan
must be directed towards a humanistic approach where the patient’s hygiene, esteem and social
needs should be addressed with complete integrity, totality and autonomy. The nursing
intervention must start with assessment of the patient’s symptoms such as apathy, social
withdrawal and detachment, aggression, hallucination and the underlying causes that might have
triggered it. Recreational activities along with ADL activities adherence should be promoted in
the patient and the mental health care nurse must take care of the defense mechanisms and
emotional outbursts of the subject pertinently. Medication adherence should be improved and
self-harm behaviors should be checked.
CARE PLAN FOR TOM
Problem
Evidence
SCHIZOPHRENIA
Hallucination, Social isolation, self-care deficits, sleep disorder and ineffective
coping mechanism.
Initially, Tom has auditory hallucination (as he reports hearing voices) along self-
care deficits, unusual behavior with memory problems. He also has possibly self-
harm behavior which might have resulted from a prolonged social withdrawal
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
MENTAL HEALTH NURSING
Evidence and deep seated emotional problems. Tom had hallucinations, behavioral
disturbances along with agitation and distress. Along with this he demonstrated
neglect towards his physical health along demonstration of amnesia.
He was bought into the care by the police for creating disturbance in the traffic
and he was in strong state of ‘denial’ that he has not done anything as such in the
traffic also reflects his intrinsic state of guarding. He was provided with a
cognitive behavioral therapy, dialectical behavioral therapy and peer support
along with right pharmacological administration in order to synchronize his
cognitive patterns, to prevent self-destructive and to manage his social isolation
scenario, respectively.
Long term
goal
The long term goal of this care plan includes shaping his cognitive patterns and
treating his deep seated emotional problems.
After the treatment, he will be able to lead a physically and psychologically
healthy life. The recovery rate of Tom will be measured using scaling.
Short term
objectives
All the symptoms of Schizophrenia like hallucination, social isolation, self-care
deficits and other issues with memory has to be handled as a short term goal.
After the treatment, he will be able to lead a physically and psychologically
healthy life. The recovery rate of Tom will be measured using scaling.
MENTAL HEALTH NURSING
Evidence and deep seated emotional problems. Tom had hallucinations, behavioral
disturbances along with agitation and distress. Along with this he demonstrated
neglect towards his physical health along demonstration of amnesia.
He was bought into the care by the police for creating disturbance in the traffic
and he was in strong state of ‘denial’ that he has not done anything as such in the
traffic also reflects his intrinsic state of guarding. He was provided with a
cognitive behavioral therapy, dialectical behavioral therapy and peer support
along with right pharmacological administration in order to synchronize his
cognitive patterns, to prevent self-destructive and to manage his social isolation
scenario, respectively.
Long term
goal
The long term goal of this care plan includes shaping his cognitive patterns and
treating his deep seated emotional problems.
After the treatment, he will be able to lead a physically and psychologically
healthy life. The recovery rate of Tom will be measured using scaling.
Short term
objectives
All the symptoms of Schizophrenia like hallucination, social isolation, self-care
deficits and other issues with memory has to be handled as a short term goal.
After the treatment, he will be able to lead a physically and psychologically
healthy life. The recovery rate of Tom will be measured using scaling.
11
MENTAL HEALTH NURSING
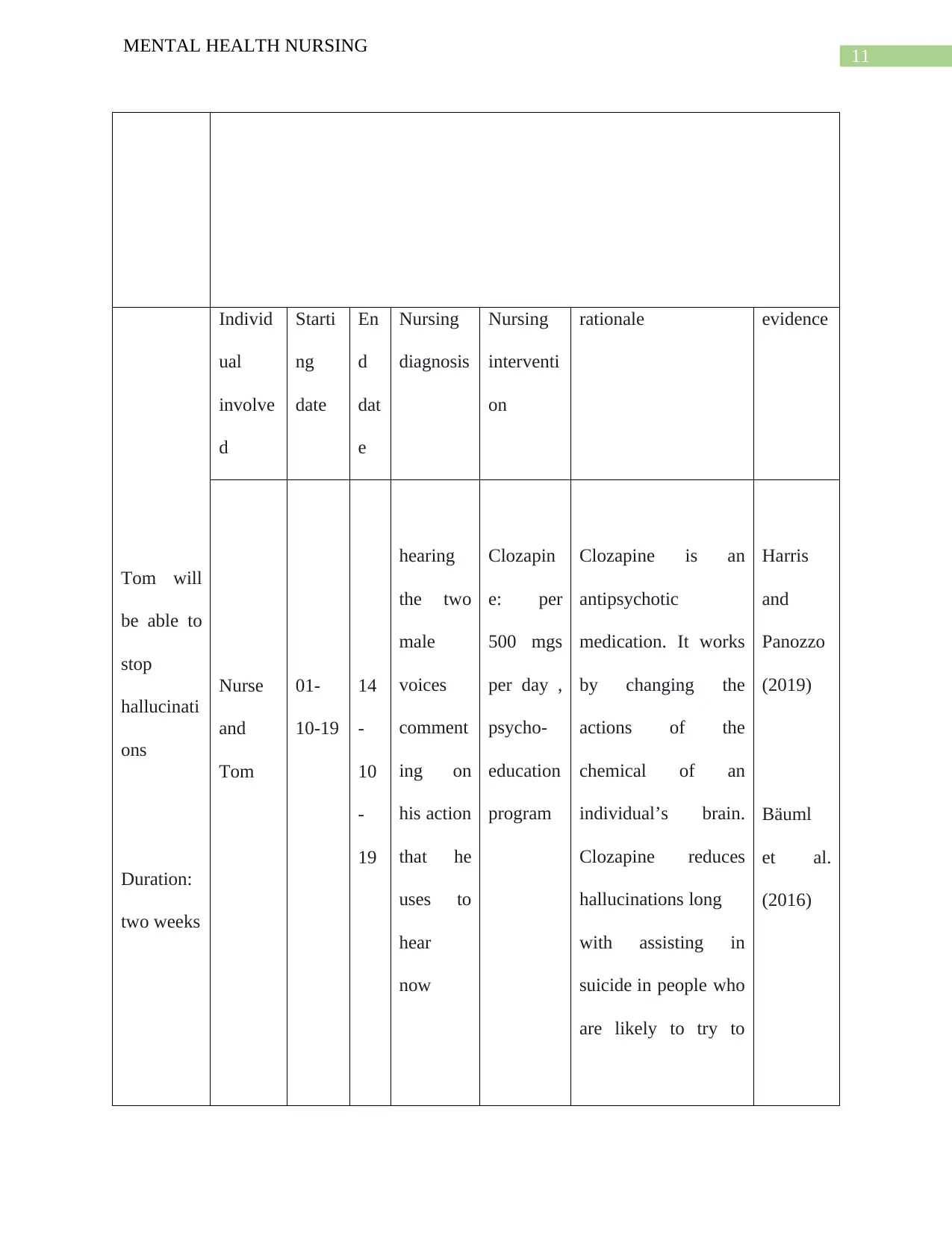
Tom will
be able to
stop
hallucinati
ons
Duration:
two weeks
Individ
ual
involve
d
Starti
ng
date
En
d
dat
e
Nursing
diagnosis
Nursing
interventi
on
rationale evidence
Nurse
and
Tom
01-
10-19
14
-
10
-
19
hearing
the two
male
voices
comment
ing on
his action
that he
uses to
hear
now
Clozapin
e: per
500 mgs
per day ,
psycho-
education
program
Clozapine is an
antipsychotic
medication. It works
by changing the
actions of the
chemical of an
individual’s brain.
Clozapine reduces
hallucinations long
with assisting in
suicide in people who
are likely to try to
Harris
and
Panozzo
(2019)
Bäuml
et al.
(2016)
MENTAL HEALTH NURSING
Tom will
be able to
stop
hallucinati
ons
Duration:
two weeks
Individ
ual
involve
d
Starti
ng
date
En
d
dat
e
Nursing
diagnosis
Nursing
interventi
on
rationale evidence
Nurse
and
Tom
01-
10-19
14
-
10
-
19
hearing
the two
male
voices
comment
ing on
his action
that he
uses to
hear
now
Clozapin
e: per
500 mgs
per day ,
psycho-
education
program
Clozapine is an
antipsychotic
medication. It works
by changing the
actions of the
chemical of an
individual’s brain.
Clozapine reduces
hallucinations long
with assisting in
suicide in people who
are likely to try to
Harris
and
Panozzo
(2019)
Bäuml
et al.
(2016)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 26
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





