University Hospice Care Report: Evidence-Based Practice for Nurses
VerifiedAdded on 2022/08/15
|7
|1463
|16
Report
AI Summary
This report focuses on evidence-based practices in hospice care, addressing the challenges faced by nurses and family caregivers. The research problem centers on caregiver withdrawal and the need for nurses to support and empower them. The PICO question explores whether empowerment and advocacy by nurses increase caregiver participation and reduce withdrawal. The report details a search strategy using PubMed Central, including keywords and filters to identify relevant literature. Two studies are synthesized, highlighting the stressors faced by caregivers and the importance of institutional support. The report recommends that nurses adopt advocacy and empowerment strategies to boost caregiver confidence and prevent withdrawal. Nurses must advocate for the thought process of the caregivers to improve their emotional condition and maintain their confidence in providing care to the patient. The goal is to improve the quality of palliative care by supporting both patients and their families. The report concludes by emphasizing the crucial role of nurses in palliative care, particularly in supporting caregivers.

Running head: HOSPICE CARE
Evidence Based Practice for Hospice Care
Name of the Student
Name of the University
Author Note
Evidence Based Practice for Hospice Care
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HOSPICE CARE
Introduction
All across the world, nursing professionals represent the largest group of health care
professionals and play a crucial role in service provisions from the health care sector. Nursing
professionals are a vital resource that helps in ensuring effective and safe health care delivery
to the community. In the special case scenarios of end-of-life situations, the nurses help an
optimization of the quality of life for the patients as well as their family members using
curated measures to prevent, anticipate and treat suffering. Palliative care encompasses the
continuum of suffering including spiritual, emotional, psychosocial, and physical needs of the
terminally ill patients. The following section of the paper will synthesize information
collected from a search of literature conducted to follow the research problem and PICOT
question.
Research Problem
In scenarios of end-of-life situation, family members in addition to the patients, also
suffer, mostly from emotional and mental aspects of health. In grave situations, where the
health of the patient deteriorates to critical levels, the caregivers or the family members of the
patient receiving palliative care may get withdrawn. The nursing professionals have to ensure
proper addressing to this issue, as family members and informal caregivers play a crucial role
during the palliative care of a patient.
PICO Question
Does empowerment and advocacy of the informal caregivers by the nursing
professionals help to increase the participation of informal caregivers in palliative care and
reduce the incidence of withdrawing from care, in comparison to no such interaction between
the nursing professionals and informal caregivers?
Population: Intervention
Introduction
All across the world, nursing professionals represent the largest group of health care
professionals and play a crucial role in service provisions from the health care sector. Nursing
professionals are a vital resource that helps in ensuring effective and safe health care delivery
to the community. In the special case scenarios of end-of-life situations, the nurses help an
optimization of the quality of life for the patients as well as their family members using
curated measures to prevent, anticipate and treat suffering. Palliative care encompasses the
continuum of suffering including spiritual, emotional, psychosocial, and physical needs of the
terminally ill patients. The following section of the paper will synthesize information
collected from a search of literature conducted to follow the research problem and PICOT
question.
Research Problem
In scenarios of end-of-life situation, family members in addition to the patients, also
suffer, mostly from emotional and mental aspects of health. In grave situations, where the
health of the patient deteriorates to critical levels, the caregivers or the family members of the
patient receiving palliative care may get withdrawn. The nursing professionals have to ensure
proper addressing to this issue, as family members and informal caregivers play a crucial role
during the palliative care of a patient.
PICO Question
Does empowerment and advocacy of the informal caregivers by the nursing
professionals help to increase the participation of informal caregivers in palliative care and
reduce the incidence of withdrawing from care, in comparison to no such interaction between
the nursing professionals and informal caregivers?
Population: Intervention
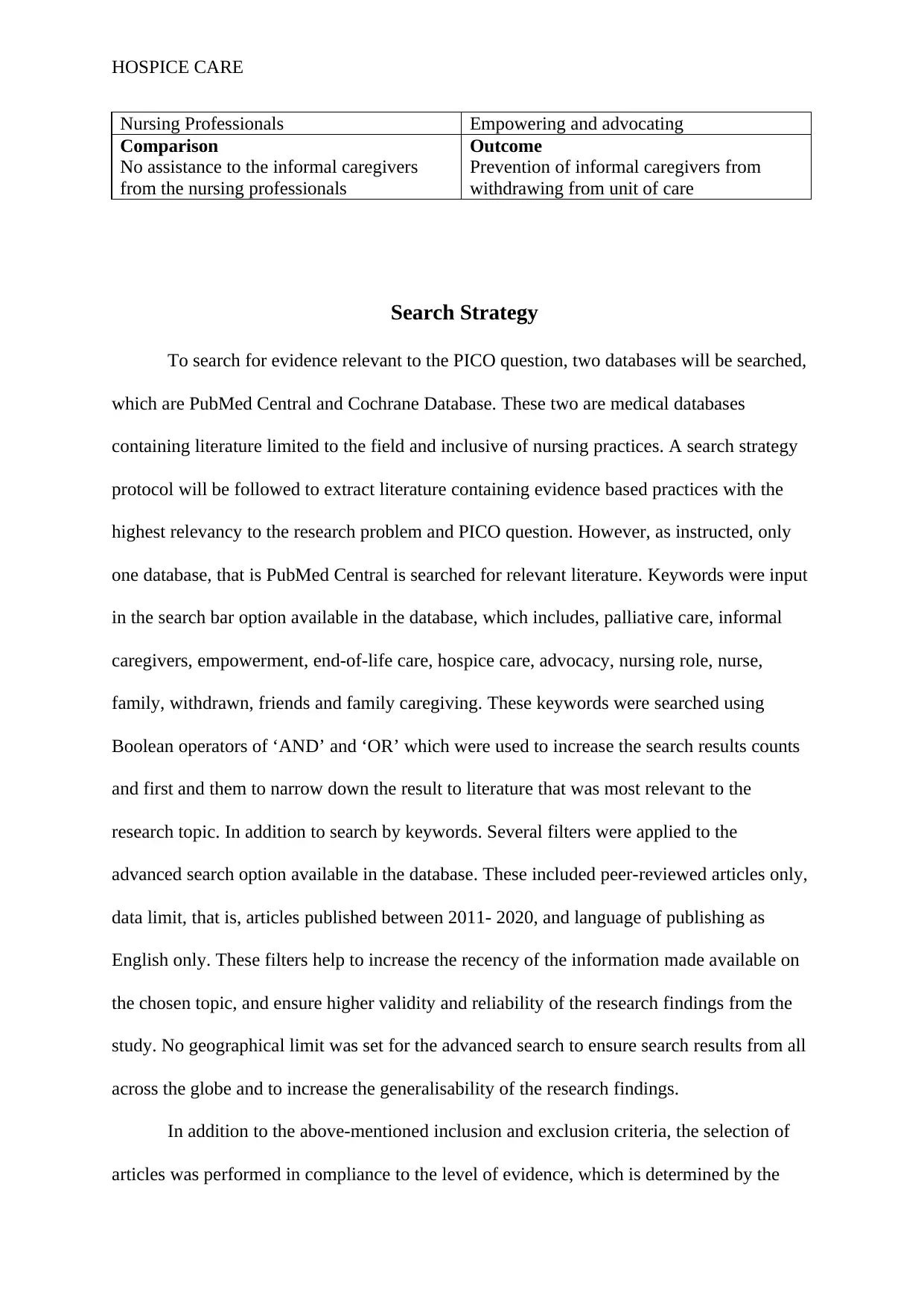
HOSPICE CARE
Nursing Professionals Empowering and advocating
Comparison
No assistance to the informal caregivers
from the nursing professionals
Outcome
Prevention of informal caregivers from
withdrawing from unit of care
Search Strategy
To search for evidence relevant to the PICO question, two databases will be searched,
which are PubMed Central and Cochrane Database. These two are medical databases
containing literature limited to the field and inclusive of nursing practices. A search strategy
protocol will be followed to extract literature containing evidence based practices with the
highest relevancy to the research problem and PICO question. However, as instructed, only
one database, that is PubMed Central is searched for relevant literature. Keywords were input
in the search bar option available in the database, which includes, palliative care, informal
caregivers, empowerment, end-of-life care, hospice care, advocacy, nursing role, nurse,
family, withdrawn, friends and family caregiving. These keywords were searched using
Boolean operators of ‘AND’ and ‘OR’ which were used to increase the search results counts
and first and them to narrow down the result to literature that was most relevant to the
research topic. In addition to search by keywords. Several filters were applied to the
advanced search option available in the database. These included peer-reviewed articles only,
data limit, that is, articles published between 2011- 2020, and language of publishing as
English only. These filters help to increase the recency of the information made available on
the chosen topic, and ensure higher validity and reliability of the research findings from the
study. No geographical limit was set for the advanced search to ensure search results from all
across the globe and to increase the generalisability of the research findings.
In addition to the above-mentioned inclusion and exclusion criteria, the selection of
articles was performed in compliance to the level of evidence, which is determined by the
Nursing Professionals Empowering and advocating
Comparison
No assistance to the informal caregivers
from the nursing professionals
Outcome
Prevention of informal caregivers from
withdrawing from unit of care
Search Strategy
To search for evidence relevant to the PICO question, two databases will be searched,
which are PubMed Central and Cochrane Database. These two are medical databases
containing literature limited to the field and inclusive of nursing practices. A search strategy
protocol will be followed to extract literature containing evidence based practices with the
highest relevancy to the research problem and PICO question. However, as instructed, only
one database, that is PubMed Central is searched for relevant literature. Keywords were input
in the search bar option available in the database, which includes, palliative care, informal
caregivers, empowerment, end-of-life care, hospice care, advocacy, nursing role, nurse,
family, withdrawn, friends and family caregiving. These keywords were searched using
Boolean operators of ‘AND’ and ‘OR’ which were used to increase the search results counts
and first and them to narrow down the result to literature that was most relevant to the
research topic. In addition to search by keywords. Several filters were applied to the
advanced search option available in the database. These included peer-reviewed articles only,
data limit, that is, articles published between 2011- 2020, and language of publishing as
English only. These filters help to increase the recency of the information made available on
the chosen topic, and ensure higher validity and reliability of the research findings from the
study. No geographical limit was set for the advanced search to ensure search results from all
across the globe and to increase the generalisability of the research findings.
In addition to the above-mentioned inclusion and exclusion criteria, the selection of
articles was performed in compliance to the level of evidence, which is determined by the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HOSPICE CARE
type of study design employed in the research for data collection and analysis. The highest
preferred level of evidence includes research studies that have conducted systematic reviews,
randomized control trials and cohort studies.
Furthermore, the final step of the search strategy included the synthesis of information
by analyzing the abstracts and title of the research articles with the highest relevancy to the
research question.
Evidence Synthesis
From the aforementioned search strategy, two articles were selected for further
evaluation and synthesis of the information to extract evidence based practices to guide
nursing professionals during the clinical problem of informal caregivers withdrawing
themselves from a unit of care and the support for the patient receiving palliative care in a
clinical setting. The first study is conducted by Hampton and Newcomb (2018) focuses on
determining the stressors in providing informal care to the patient and identify the existence
of any potential factors that can prevent or buffer stress. The primary objective of the study
was to determine the relationship between stress and self-efficacy in the informal caregivers
that are currently providing palliative care to their loved ones. This research study is
important for the nursing professionals to have an in-depth insight into the stressing factors in
the informal caregivers and play their advocacy role to support the informal caregivers and
prevent them from stressing out. The study conducted by Hampton and Newcomb (2018) was
a cross-sectional study in which questionnaire was used to get data on the perceived health,
stress and self-efficacy of the caregiver. The research findings concluded that informal
caregivers who had greater confidence in managing the demands of the patient were less
likely to get stressed and had lower levels of perceived stress.
Another study conducted by Ateş et al. (2018), aimed at evaluating the responsibilities
of the informal caregivers during the delivery of palliative care to the patient. Further
type of study design employed in the research for data collection and analysis. The highest
preferred level of evidence includes research studies that have conducted systematic reviews,
randomized control trials and cohort studies.
Furthermore, the final step of the search strategy included the synthesis of information
by analyzing the abstracts and title of the research articles with the highest relevancy to the
research question.
Evidence Synthesis
From the aforementioned search strategy, two articles were selected for further
evaluation and synthesis of the information to extract evidence based practices to guide
nursing professionals during the clinical problem of informal caregivers withdrawing
themselves from a unit of care and the support for the patient receiving palliative care in a
clinical setting. The first study is conducted by Hampton and Newcomb (2018) focuses on
determining the stressors in providing informal care to the patient and identify the existence
of any potential factors that can prevent or buffer stress. The primary objective of the study
was to determine the relationship between stress and self-efficacy in the informal caregivers
that are currently providing palliative care to their loved ones. This research study is
important for the nursing professionals to have an in-depth insight into the stressing factors in
the informal caregivers and play their advocacy role to support the informal caregivers and
prevent them from stressing out. The study conducted by Hampton and Newcomb (2018) was
a cross-sectional study in which questionnaire was used to get data on the perceived health,
stress and self-efficacy of the caregiver. The research findings concluded that informal
caregivers who had greater confidence in managing the demands of the patient were less
likely to get stressed and had lower levels of perceived stress.
Another study conducted by Ateş et al. (2018), aimed at evaluating the responsibilities
of the informal caregivers during the delivery of palliative care to the patient. Further
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HOSPICE CARE
investigation on the burdens, rewards, and provisions from the healthcare professionals that
help in assisting the informal caregivers are also performed. The researchers conducted a
multinational mixed-method study to collect data on these objectives and perform analysis to
conclude the results. For the qualitative part, semi-structured interviews were conducted
which were analysed with the help of transnationally agreed thematic codes of NVivo or
MAXQDA. Another quantitative part of the study included questionnaires on which
statistical tests using SPSS were performed to analyse data. The research findings showed
that lack of institutionalised or systematic support structures in the integrated palliative care
units was the most significant determinant of caregivers withdrawing themselves from a unit
of care. This information can be critically analysed by the nursing professionals to ensure
greater psychological support for the informal caregivers to empower them and ensure their
participation and contribution in palliative care.
Recommendation
From the above analysis and synthesis of information extracted from the two selected
research studies, it was determined that the nursing professionals and their clinical practices
require modification to increase support and assistance of the informal caregivers. The two
primary evidence based practices that the nursing professionals need to incur in their daily
clinical setting and provision of palliative care are playing to role of advocacy and
empowering the informal caregivers to increase their confidence in managing the health care
of the patients in the end-of-life situation. Nurses have to advocate for the thought process of
the caregivers to improve their emotional condition and maintain their confidence in
providing care to the patient. By empowering the informal caregivers, the nursing
professionals can ensure psychological support to the caregivers and to prevent themselves
from withdrawing from the unit care of care.
investigation on the burdens, rewards, and provisions from the healthcare professionals that
help in assisting the informal caregivers are also performed. The researchers conducted a
multinational mixed-method study to collect data on these objectives and perform analysis to
conclude the results. For the qualitative part, semi-structured interviews were conducted
which were analysed with the help of transnationally agreed thematic codes of NVivo or
MAXQDA. Another quantitative part of the study included questionnaires on which
statistical tests using SPSS were performed to analyse data. The research findings showed
that lack of institutionalised or systematic support structures in the integrated palliative care
units was the most significant determinant of caregivers withdrawing themselves from a unit
of care. This information can be critically analysed by the nursing professionals to ensure
greater psychological support for the informal caregivers to empower them and ensure their
participation and contribution in palliative care.
Recommendation
From the above analysis and synthesis of information extracted from the two selected
research studies, it was determined that the nursing professionals and their clinical practices
require modification to increase support and assistance of the informal caregivers. The two
primary evidence based practices that the nursing professionals need to incur in their daily
clinical setting and provision of palliative care are playing to role of advocacy and
empowering the informal caregivers to increase their confidence in managing the health care
of the patients in the end-of-life situation. Nurses have to advocate for the thought process of
the caregivers to improve their emotional condition and maintain their confidence in
providing care to the patient. By empowering the informal caregivers, the nursing
professionals can ensure psychological support to the caregivers and to prevent themselves
from withdrawing from the unit care of care.
HOSPICE CARE
Conclusion
Nurses have a crucial role to play in the provision of palliative care which requires an
emphasis on the health of the informal caregivers in addition to the patient. Nurses can ensure
empowerment and advocacy to the informal caregivers who will essentially boost up their
confidence in maintaining demands of the patient receiving palliative care and critically
provide them with the much needed psychological support to prevent them from withdrawing
from the unit of care.
Conclusion
Nurses have a crucial role to play in the provision of palliative care which requires an
emphasis on the health of the informal caregivers in addition to the patient. Nurses can ensure
empowerment and advocacy to the informal caregivers who will essentially boost up their
confidence in maintaining demands of the patient receiving palliative care and critically
provide them with the much needed psychological support to prevent them from withdrawing
from the unit of care.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HOSPICE CARE
References
Ateş, G., Ebenau, A. F., Busa, C., Csikos, Á., Hasselaar, J., Jaspers, B., ... & Groot, M.
(2018). “Never at ease”–family carers within integrated palliative care: a
multinational, mixed method study. BMC palliative care, 17(1), 39. doi:
10.1186/s12904-018-0291-7
Hampton, M. M., & Newcomb, P. (2018). Self-efficacy and Stress Among Informal
Caregivers of Individuals at End of Life. Journal of Hospice & Palliative
Nursing, 20(5), 471-477. doi: 10.1097/NJH.0000000000000464
References
Ateş, G., Ebenau, A. F., Busa, C., Csikos, Á., Hasselaar, J., Jaspers, B., ... & Groot, M.
(2018). “Never at ease”–family carers within integrated palliative care: a
multinational, mixed method study. BMC palliative care, 17(1), 39. doi:
10.1186/s12904-018-0291-7
Hampton, M. M., & Newcomb, P. (2018). Self-efficacy and Stress Among Informal
Caregivers of Individuals at End of Life. Journal of Hospice & Palliative
Nursing, 20(5), 471-477. doi: 10.1097/NJH.0000000000000464
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





