Analyzing Family Presence During Resuscitation: Clinical Implications
VerifiedAdded on 2023/06/12
|7
|1954
|88
Essay
AI Summary
This essay critically examines the practice of allowing family members to be present during cardiopulmonary resuscitation (CPR) in acute settings. It explores the debate surrounding family presence, weighing the potential benefits such as emotional comfort, information sharing, and facilitating grief, against the risks of interference with medical procedures, psychological trauma to family members, and potential legal implications for healthcare professionals. The essay references research from databases like Medline and Cinhal, utilizing systematic reviews and randomized controlled trials to argue that while family presence may seem beneficial, the potential negative consequences, including increased anxiety, post-traumatic stress, and disruption of resuscitation efforts, outweigh the advantages. Ultimately, the essay concludes that, to protect both the efficiency of resuscitation teams and the mental well-being of family members, their presence should be discouraged during these critical procedures. Desklib offers this essay along with a wide range of study resources for students.

Running head: SCENARIO 3
SCENARIO 3
Name of the student:
Name of the university:
Author note:
SCENARIO 3
Name of the student:
Name of the university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
SCENARIO 3
Cardiopulmonary resuscitation also called CPR is mainly seen to be comprising of the
use of chest compressions as well as artificial ventilation. This is mainly done to maintain
circulatory flow as well as oxygenation during cardiac arrest. Researchers are of the opinion that
survival rates and neurologic outcomes are found to be poor in most of the cases in patients with
cardiac arrest (hill, Knafl &Santacroce, 2017). However, there are also studies which state that
early appropriate resuscitation that involve early defibrillation as well as appropriate
implementation of the post cardiac arrest result in improved survival as well as neurologic
outcomes. Often there are many instances where professionals allow the family members to be
present with their loved patients in their critical times. Often different types of negative
consequences remain associated with the presence of the family members. However, there have
been many debates about the allowance of the family members. It would be represented in the
essay and would be supported by different evidence based articles to show whether such
decisions are clinically correct or not.
The main database that I have used for the literature search is Medline and Cinhal. The
search terms that I have used are “resuscitation presence of family”, “family presence in
resuscitation of loved one”, “presence of family members in end moments of patients”,” should
families be allowed during resuscitation” and others. The level of evidences used is the first level
of evidences like systematic reviews and second level of evidences like randomized control
trials. Hence, the evidences are high of quality and content. I have mainly used an argumentative
approach proving the point.
SCENARIO 3
Cardiopulmonary resuscitation also called CPR is mainly seen to be comprising of the
use of chest compressions as well as artificial ventilation. This is mainly done to maintain
circulatory flow as well as oxygenation during cardiac arrest. Researchers are of the opinion that
survival rates and neurologic outcomes are found to be poor in most of the cases in patients with
cardiac arrest (hill, Knafl &Santacroce, 2017). However, there are also studies which state that
early appropriate resuscitation that involve early defibrillation as well as appropriate
implementation of the post cardiac arrest result in improved survival as well as neurologic
outcomes. Often there are many instances where professionals allow the family members to be
present with their loved patients in their critical times. Often different types of negative
consequences remain associated with the presence of the family members. However, there have
been many debates about the allowance of the family members. It would be represented in the
essay and would be supported by different evidence based articles to show whether such
decisions are clinically correct or not.
The main database that I have used for the literature search is Medline and Cinhal. The
search terms that I have used are “resuscitation presence of family”, “family presence in
resuscitation of loved one”, “presence of family members in end moments of patients”,” should
families be allowed during resuscitation” and others. The level of evidences used is the first level
of evidences like systematic reviews and second level of evidences like randomized control
trials. Hence, the evidences are high of quality and content. I have mainly used an argumentative
approach proving the point.
2
SCENARIO 3
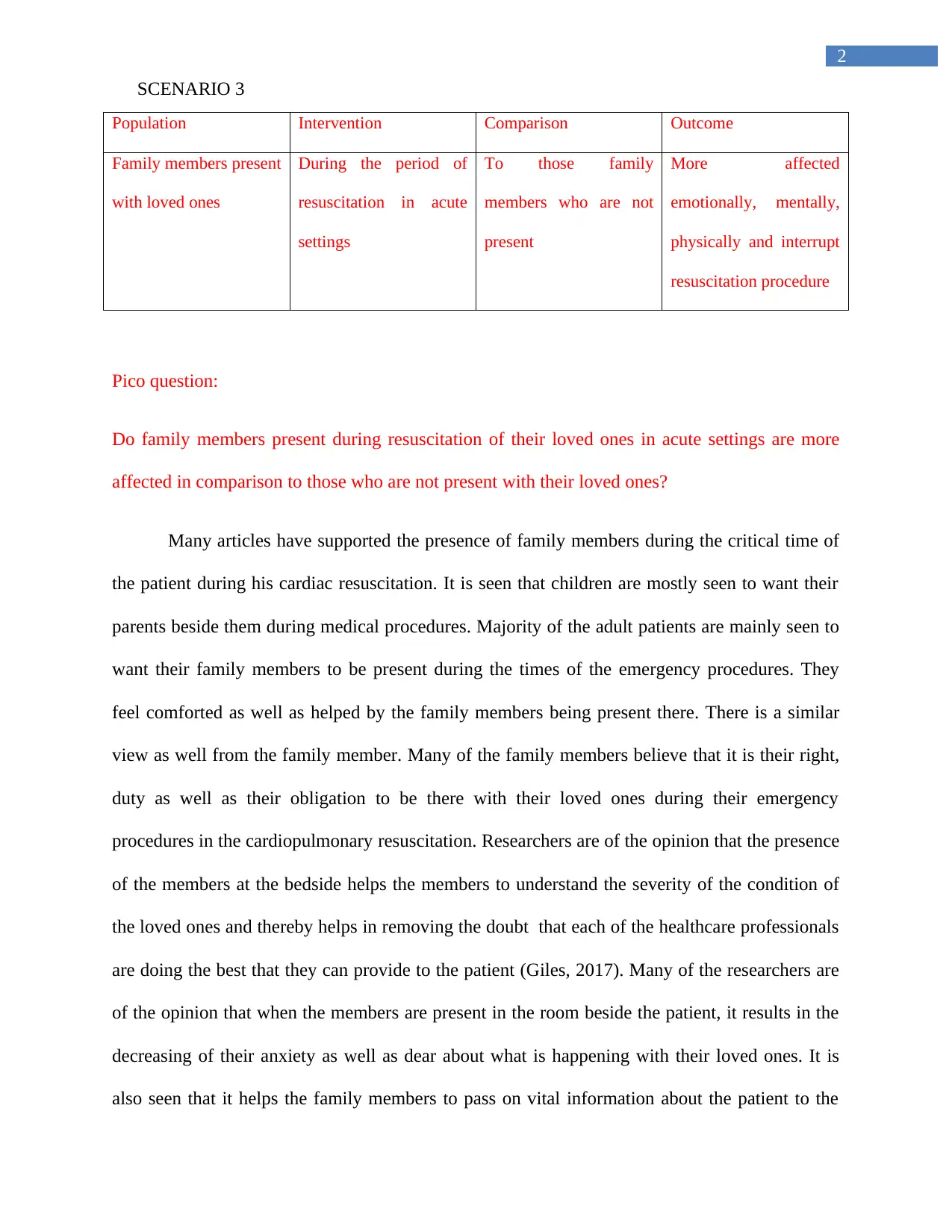
Population Intervention Comparison Outcome
Family members present
with loved ones
During the period of
resuscitation in acute
settings
To those family
members who are not
present
More affected
emotionally, mentally,
physically and interrupt
resuscitation procedure
Pico question:
Do family members present during resuscitation of their loved ones in acute settings are more
affected in comparison to those who are not present with their loved ones?
Many articles have supported the presence of family members during the critical time of
the patient during his cardiac resuscitation. It is seen that children are mostly seen to want their
parents beside them during medical procedures. Majority of the adult patients are mainly seen to
want their family members to be present during the times of the emergency procedures. They
feel comforted as well as helped by the family members being present there. There is a similar
view as well from the family member. Many of the family members believe that it is their right,
duty as well as their obligation to be there with their loved ones during their emergency
procedures in the cardiopulmonary resuscitation. Researchers are of the opinion that the presence
of the members at the bedside helps the members to understand the severity of the condition of
the loved ones and thereby helps in removing the doubt that each of the healthcare professionals
are doing the best that they can provide to the patient (Giles, 2017). Many of the researchers are
of the opinion that when the members are present in the room beside the patient, it results in the
decreasing of their anxiety as well as dear about what is happening with their loved ones. It is
also seen that it helps the family members to pass on vital information about the patient to the
SCENARIO 3
Population Intervention Comparison Outcome
Family members present
with loved ones
During the period of
resuscitation in acute
settings
To those family
members who are not
present
More affected
emotionally, mentally,
physically and interrupt
resuscitation procedure
Pico question:
Do family members present during resuscitation of their loved ones in acute settings are more
affected in comparison to those who are not present with their loved ones?
Many articles have supported the presence of family members during the critical time of
the patient during his cardiac resuscitation. It is seen that children are mostly seen to want their
parents beside them during medical procedures. Majority of the adult patients are mainly seen to
want their family members to be present during the times of the emergency procedures. They
feel comforted as well as helped by the family members being present there. There is a similar
view as well from the family member. Many of the family members believe that it is their right,
duty as well as their obligation to be there with their loved ones during their emergency
procedures in the cardiopulmonary resuscitation. Researchers are of the opinion that the presence
of the members at the bedside helps the members to understand the severity of the condition of
the loved ones and thereby helps in removing the doubt that each of the healthcare professionals
are doing the best that they can provide to the patient (Giles, 2017). Many of the researchers are
of the opinion that when the members are present in the room beside the patient, it results in the
decreasing of their anxiety as well as dear about what is happening with their loved ones. It is
also seen that it helps the family members to pass on vital information about the patient to the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
SCENARIO 3
healthcare providers. It helps in the facilitation of their needs to be together as well as their
opportunity to be with their loved one, advocate for them, comfort them, protect, and support
their loved ones (Olding et al., 2016). It has been also seen that the presence of the family
members allows them to experience a sense of closure as well as help in facilitation of the grief
procedure should death occur.
However, a large number of negative aspects are highly associated about the presence of
the family members in the room of resuscitation of the loved ones. In many of the cases,
researchers have observed in their observational studies that the family members have interfered
with the resuscitation efforts of the healthcare professionals. Different types of interruptions
from the family members are thereby seen to increase the increase the risk of death for the
patients. They are also seen to go through different types of physical, psychological as well as
legal obligations for the members who are working in the resuscitation teams. Therefore, in order
to allow the resuscitation team members to concentrate on their actions and helps the patient to
overcome the situation, interruptions from family members cannot be tolerated and hence they
should not be allowed in the rooms (Twibell et al., 2018). Many of the researchers have again
concentrated on the psychological trauma that family members witness during the resuscitation
efforts. Often many researchers have supported the presence of family members during
resuscitation at home where there were no significant posttraumatic stress disorders noticed
among the members. However this articles cannot be supported in the essay as cardiac arrests
that occur at home are entirely different from the cardiac arrests that had taken place in the acute
care emergency wards (Porter et al., 2017). This is mainly because the cardiac arrests that occur
in the homes are different in the sense as the emergency resuscitation the family embers summon
teams only where they have already noticed cardiac arrest situation of the patient. Many families
SCENARIO 3
healthcare providers. It helps in the facilitation of their needs to be together as well as their
opportunity to be with their loved one, advocate for them, comfort them, protect, and support
their loved ones (Olding et al., 2016). It has been also seen that the presence of the family
members allows them to experience a sense of closure as well as help in facilitation of the grief
procedure should death occur.
However, a large number of negative aspects are highly associated about the presence of
the family members in the room of resuscitation of the loved ones. In many of the cases,
researchers have observed in their observational studies that the family members have interfered
with the resuscitation efforts of the healthcare professionals. Different types of interruptions
from the family members are thereby seen to increase the increase the risk of death for the
patients. They are also seen to go through different types of physical, psychological as well as
legal obligations for the members who are working in the resuscitation teams. Therefore, in order
to allow the resuscitation team members to concentrate on their actions and helps the patient to
overcome the situation, interruptions from family members cannot be tolerated and hence they
should not be allowed in the rooms (Twibell et al., 2018). Many of the researchers have again
concentrated on the psychological trauma that family members witness during the resuscitation
efforts. Often many researchers have supported the presence of family members during
resuscitation at home where there were no significant posttraumatic stress disorders noticed
among the members. However this articles cannot be supported in the essay as cardiac arrests
that occur at home are entirely different from the cardiac arrests that had taken place in the acute
care emergency wards (Porter et al., 2017). This is mainly because the cardiac arrests that occur
in the homes are different in the sense as the emergency resuscitation the family embers summon
teams only where they have already noticed cardiac arrest situation of the patient. Many families
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
SCENARIO 3
were seen to conduct the resuscitations on their family members themselves. However, in case of
the emergency rooms resuscitations, the nursing professionals only notice most of the cardiac
arrests (Frivold et al., 2015). They then call for the resuscitation teams to immediately respond
and the family members only learn about the vent after the resuscitation is being carried on. This
sudden scenario of the professionals resuscitating their loved one result in many kinds of
questions and concerns among the members that might affect their mental stability and for this
the members should not be allowed in the rooms. In the inpatient cases of cardiac resuscitation,
social supports are usually not available and therefore family members who are present can
undergo severe psychological trauma when they are not given proper social support. Moreover,
inpatient acute settings mainly contains cases of the interventions that include visible bleeding
which may include insertion of central venous catheter and many others witnessing such
interventions may prove to be traumatic to the family members (Powers & Candela, 2017). It
should be kept in mind that not all members of the family have equal reaction to particular
psychological trauma. Many of the researchers have stated that many people who checked the
resuscitation of their loved ones were 11% less likely than their controls to have developed
symptoms of depression. However, there are also studies which have shown that 1% of the
witnesses accounting to about 5 people have committed suicides after such situations. Therefore,
it clearly states many individuals in a population are at a higher risk for the development for
depression and posttraumatic stress disorders after watching resuscitations. At the time of the
event, it can never be possible for the professionals to find out how the members would react
after watching their loved ones go through the critical phase (McLean, 2016). Therefore, by
analyzing the cost benefit ratio, it can be stated that keeping the family members out of the
rooms will not affect their mental stability to patient at which they can self harm themselves or
SCENARIO 3
were seen to conduct the resuscitations on their family members themselves. However, in case of
the emergency rooms resuscitations, the nursing professionals only notice most of the cardiac
arrests (Frivold et al., 2015). They then call for the resuscitation teams to immediately respond
and the family members only learn about the vent after the resuscitation is being carried on. This
sudden scenario of the professionals resuscitating their loved one result in many kinds of
questions and concerns among the members that might affect their mental stability and for this
the members should not be allowed in the rooms. In the inpatient cases of cardiac resuscitation,
social supports are usually not available and therefore family members who are present can
undergo severe psychological trauma when they are not given proper social support. Moreover,
inpatient acute settings mainly contains cases of the interventions that include visible bleeding
which may include insertion of central venous catheter and many others witnessing such
interventions may prove to be traumatic to the family members (Powers & Candela, 2017). It
should be kept in mind that not all members of the family have equal reaction to particular
psychological trauma. Many of the researchers have stated that many people who checked the
resuscitation of their loved ones were 11% less likely than their controls to have developed
symptoms of depression. However, there are also studies which have shown that 1% of the
witnesses accounting to about 5 people have committed suicides after such situations. Therefore,
it clearly states many individuals in a population are at a higher risk for the development for
depression and posttraumatic stress disorders after watching resuscitations. At the time of the
event, it can never be possible for the professionals to find out how the members would react
after watching their loved ones go through the critical phase (McLean, 2016). Therefore, by
analyzing the cost benefit ratio, it can be stated that keeping the family members out of the
rooms will not affect their mental stability to patient at which they can self harm themselves or
5
SCENARIO 3
develop PTSD as in cases where they may develop so when resuscitations are witnessed (Giles et
al., 2018). Therefore, family members should not be allowed in the rooms of resuscitation of
their loved ones.
Conclusion:
From the above discussion, it is clear that being present with loved one may be the duty
and right of the family members and make the patient comfortable it is not the correct decision. It
is important for the members to be outside the rooms so that they do not interrupt the
resuscitation process, do not develop depression and PTSD and do not lose mental stability.
Therefore, nursing professionals should try to advise the members to be outside the rooms while
such strategies are being carried on the patients.
References:
Frivold, G., Dale, B., & Slettebø, Å. (2015). Family members’ experiences of being cared for by
nurses and physicians in Norwegian intensive care units: A phenomenological
hermeneutical study. Intensive and Critical Care Nursing, 31(4), 232-240.
Giles, T., de Lacey, S., & Muir‐Cochrane, E. (2018). How do clinicians practise the principles of
beneficence when deciding to allow or deny family presence during
resuscitation?. Journal of clinical nursing, 27(5-6), e1214-e1224.
Giles, T. (2017). Caring for people at deaths door during resuscitation events. Australian Nursing
and Midwifery Journal, 25(6), 36-36.
SCENARIO 3
develop PTSD as in cases where they may develop so when resuscitations are witnessed (Giles et
al., 2018). Therefore, family members should not be allowed in the rooms of resuscitation of
their loved ones.
Conclusion:
From the above discussion, it is clear that being present with loved one may be the duty
and right of the family members and make the patient comfortable it is not the correct decision. It
is important for the members to be outside the rooms so that they do not interrupt the
resuscitation process, do not develop depression and PTSD and do not lose mental stability.
Therefore, nursing professionals should try to advise the members to be outside the rooms while
such strategies are being carried on the patients.
References:
Frivold, G., Dale, B., & Slettebø, Å. (2015). Family members’ experiences of being cared for by
nurses and physicians in Norwegian intensive care units: A phenomenological
hermeneutical study. Intensive and Critical Care Nursing, 31(4), 232-240.
Giles, T., de Lacey, S., & Muir‐Cochrane, E. (2018). How do clinicians practise the principles of
beneficence when deciding to allow or deny family presence during
resuscitation?. Journal of clinical nursing, 27(5-6), e1214-e1224.
Giles, T. (2017). Caring for people at deaths door during resuscitation events. Australian Nursing
and Midwifery Journal, 25(6), 36-36.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

6
SCENARIO 3
Hill, C., Knafl, K. A., & Santacroce, S. J. (2017). Family-Centered Care From the Perspective of
Parents of Children Cared for in a Pediatric Intensive Care Unit: An Integrative
Review. Journal of pediatric nursing.
McLean, J., Gill, F. J., & Shields, L. (2016). Family presence during resuscitation in a paediatric
hospital: health professionals’ confidence and perceptions. Journal of clinical
nursing, 25(7-8), 1045-1052.
Olding, M., McMillan, S. E., Reeves, S., Schmitt, M. H., Puntillo, K., & Kitto, S. (2016). Patient
and family involvement in adult critical and intensive care settings: a scoping
review. Health Expectations, 19(6), 1183-1202.
Powers, K. A., & Candela, L. (2017). Nursing Practices and Policies Related to Family Presence
During Resuscitation. Dimensions of Critical Care Nursing, 36(1), 53-59.
Porter, J. E., Miller, N., Giannis, A., & Coombs, N. (2017). Family Presence During
Resuscitation (FPDR): Observational case studies of emergency personnel in Victoria,
Australia. International emergency nursing, 33, 37-42.
Twibell, R., Siela, D., Riwitis, C., Neal, A., & Waters, N. (2018). A qualitative study of factors
in nurses' and physicians' decision‐making related to family presence during
resuscitation. Journal of clinical nursing, 27(1-2), e320-e334.
SCENARIO 3
Hill, C., Knafl, K. A., & Santacroce, S. J. (2017). Family-Centered Care From the Perspective of
Parents of Children Cared for in a Pediatric Intensive Care Unit: An Integrative
Review. Journal of pediatric nursing.
McLean, J., Gill, F. J., & Shields, L. (2016). Family presence during resuscitation in a paediatric
hospital: health professionals’ confidence and perceptions. Journal of clinical
nursing, 25(7-8), 1045-1052.
Olding, M., McMillan, S. E., Reeves, S., Schmitt, M. H., Puntillo, K., & Kitto, S. (2016). Patient
and family involvement in adult critical and intensive care settings: a scoping
review. Health Expectations, 19(6), 1183-1202.
Powers, K. A., & Candela, L. (2017). Nursing Practices and Policies Related to Family Presence
During Resuscitation. Dimensions of Critical Care Nursing, 36(1), 53-59.
Porter, J. E., Miller, N., Giannis, A., & Coombs, N. (2017). Family Presence During
Resuscitation (FPDR): Observational case studies of emergency personnel in Victoria,
Australia. International emergency nursing, 33, 37-42.
Twibell, R., Siela, D., Riwitis, C., Neal, A., & Waters, N. (2018). A qualitative study of factors
in nurses' and physicians' decision‐making related to family presence during
resuscitation. Journal of clinical nursing, 27(1-2), e320-e334.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





