Review of Literature: End-of-Life Care and Family Support in Dementia
VerifiedAdded on 2022/10/15
|20
|5372
|467
Report
AI Summary
This report provides a comprehensive review of the literature concerning end-of-life care and family support for patients with dementia. It explores the definition of dementia, search strategies used in the study, and a critical evaluation of various research papers and guidelines. The report emphasizes the importance of palliative care, the roles of family members and healthcare professionals, and effective communication strategies in managing the disease. Key topics include the impact of dementia on individuals, the significance of advance care planning, and the need for a collaborative approach involving families, caregivers, and healthcare providers. The report highlights the importance of guidelines for providing care, the value of communication between older people and their families, and the crucial role families play in directing care. It also discusses the benefits of palliative care in improving the quality of life for dementia patients and the need for awareness and understanding within society. The report concludes by summarizing the key findings and implications of the research, emphasizing the need for a holistic approach to dementia care that prioritizes patient well-being and family support.
Running Head: End of life care and family support for patients with dementia.
END OF LIFE CARE AND FAMILY SUPPORT FOR PATIENTS
WITH DEMENTIA
END OF LIFE CARE AND FAMILY SUPPORT FOR PATIENTS
WITH DEMENTIA
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
End of life care and family support for patients with dementia.
Table of Contents
1.1 Introduction................................................................................................................................3
1.2 Definition of the topic................................................................................................................4
1.3 Search strategy...........................................................................................................................5
1.4 Evaluation and critical discussion of literature..........................................................................6
1.4.1 Dementia is everybody's business......................................................................................6
1.4.2 Palliative aged residential care guideline...........................................................................7
1.4.3 Guideline for providing care to people with dementia.......................................................8
1.4.4 Importance of communication between older people and their family..............................8
1.4.5 Role played by family in directing care..............................................................................9
1.4.6 Palliative care for dementia patients in New Zealand......................................................10
1.5 Discussion and Conclusion......................................................................................................13
Reference list.................................................................................................................................17
End of life care and family support for patients with dementia.
Table of Contents
1.1 Introduction................................................................................................................................3
1.2 Definition of the topic................................................................................................................4
1.3 Search strategy...........................................................................................................................5
1.4 Evaluation and critical discussion of literature..........................................................................6
1.4.1 Dementia is everybody's business......................................................................................6
1.4.2 Palliative aged residential care guideline...........................................................................7
1.4.3 Guideline for providing care to people with dementia.......................................................8
1.4.4 Importance of communication between older people and their family..............................8
1.4.5 Role played by family in directing care..............................................................................9
1.4.6 Palliative care for dementia patients in New Zealand......................................................10
1.5 Discussion and Conclusion......................................................................................................13
Reference list.................................................................................................................................17
3
End of life care and family support for patients with dementia.
1.1 Introduction
Dementia is considered as a progressive condition that has no cure and it is essential to get
prepared for the final stage. As stages of this disease progress, patients get more dependent on
conducting daily activities and care. Advance care planning is essential that helps to gather
knowledge about essential steps that can be taken during advanced stage of dementia
(Alzheimers.org.nz, 2018). Planning includes collection of evidence regarding different
requirements of dementia patients, which must be provided through external support. A power of
attorney is essential that is a legal document, which enables other people to look after the
interests of a person if that person is unable to perform. Palliative care is about providing relief to
a dying person and providing them the best quality of life (Moh.govt.nz, 2017). This process of
care is not about curing the disease but to provide some relief from suffering of the disease and
maintaining comfort level.
This study has been selected because knowledge about palliative care can help to increase
expertise in this sector. Different knowledge about care process, formalities, and required
resources is essential to plan and design the care process. Moreover, knowledge regarding the
role of family needs to be gained. Family plays an essential role in this process because they
have prompt knowledge about different requirements of the patients. Hence, care process can be
planned well through inclusion of family members. In this study, different kinds of literature
have been collected that has knowledge regarding the topic. Hence, different lessons like
planning information, role of caregiver and family can be earned from this study.
End of life care and family support for patients with dementia.
1.1 Introduction
Dementia is considered as a progressive condition that has no cure and it is essential to get
prepared for the final stage. As stages of this disease progress, patients get more dependent on
conducting daily activities and care. Advance care planning is essential that helps to gather
knowledge about essential steps that can be taken during advanced stage of dementia
(Alzheimers.org.nz, 2018). Planning includes collection of evidence regarding different
requirements of dementia patients, which must be provided through external support. A power of
attorney is essential that is a legal document, which enables other people to look after the
interests of a person if that person is unable to perform. Palliative care is about providing relief to
a dying person and providing them the best quality of life (Moh.govt.nz, 2017). This process of
care is not about curing the disease but to provide some relief from suffering of the disease and
maintaining comfort level.
This study has been selected because knowledge about palliative care can help to increase
expertise in this sector. Different knowledge about care process, formalities, and required
resources is essential to plan and design the care process. Moreover, knowledge regarding the
role of family needs to be gained. Family plays an essential role in this process because they
have prompt knowledge about different requirements of the patients. Hence, care process can be
planned well through inclusion of family members. In this study, different kinds of literature
have been collected that has knowledge regarding the topic. Hence, different lessons like
planning information, role of caregiver and family can be earned from this study.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
End of life care and family support for patients with dementia.
1.2 Definition of the topic
Aim of this study is to review literature based on palliative care for older adults with dementia
and develop findings from the review, which can help in improving the process of providing care
to older dementia patients.
Discussion of the topic
Dementia is very common in older people and this mental disorder makes people dependent on
others. This is not a disease and this term refers to a set of activities that prevent a person to do
their daily activities. In this mental situation, people lose their ability to think and make decisions
of their own. As mentioned by Sternberg et al. (2019), partial memory loss is one of the main
symptoms of dementia. In this kind of situation, older people must get palliative care from
healthcare professionals like nurses and their family members. Family support at this point may
encourage people to cooperate with the medical process for their wellbeing. Providing care to
older people with dementia is considered as end-of-life care and healthcare organizations provide
training to their staff regarding the process of handling older dementia patients.
Family members of these patients need to communicate with them for understanding their issues.
It is important to help them to cope up with this mental condition at the end of their life. Positive
attitude towards these patients enhance their confidence level and they start trusting the medical
system. This approach is good for their wellbeing. Healthcare professionals are liable to educate
others, including patients and their relatives regarding dementia. Palliative care and family
support are two important aspects that can help in dementia. Patients must share their problems
with family members to help them to get possible solutions. On the other hand, Amador,
End of life care and family support for patients with dementia.
1.2 Definition of the topic
Aim of this study is to review literature based on palliative care for older adults with dementia
and develop findings from the review, which can help in improving the process of providing care
to older dementia patients.
Discussion of the topic
Dementia is very common in older people and this mental disorder makes people dependent on
others. This is not a disease and this term refers to a set of activities that prevent a person to do
their daily activities. In this mental situation, people lose their ability to think and make decisions
of their own. As mentioned by Sternberg et al. (2019), partial memory loss is one of the main
symptoms of dementia. In this kind of situation, older people must get palliative care from
healthcare professionals like nurses and their family members. Family support at this point may
encourage people to cooperate with the medical process for their wellbeing. Providing care to
older people with dementia is considered as end-of-life care and healthcare organizations provide
training to their staff regarding the process of handling older dementia patients.
Family members of these patients need to communicate with them for understanding their issues.
It is important to help them to cope up with this mental condition at the end of their life. Positive
attitude towards these patients enhance their confidence level and they start trusting the medical
system. This approach is good for their wellbeing. Healthcare professionals are liable to educate
others, including patients and their relatives regarding dementia. Palliative care and family
support are two important aspects that can help in dementia. Patients must share their problems
with family members to help them to get possible solutions. On the other hand, Amador,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
End of life care and family support for patients with dementia.
Sampson, Goodman, and Robinson (2019) have stated that family members must have good
listening and communication skills along with a higher rate of patience. Behavior of family
members has a great impact on the mind of patients with dementia and positive behavior
encourages them to be calm and happy. For this study, relevant literature is being searched and
reviewed. These reviewing reveal different perspectives of the selected topic. Importance of
effective communication between family members and dementia patients are being discussed.
On the other hand, different potential processes that can be considered to improve patient care
quality are being presented in this study. Providing palliative care and family support can help
older people to fight with dementia.
1.3 Search strategy
A proper search strategy is used for accomplishing the task. Different relevant articles and
journals are researched from various sources that have proper information about the subject area.
A proper search strategy can help to increase the chance of a researcher to gain proper
information about a selected topic. In this research, different sources of data are explored and
appropriate articles are chosen for review.
Keywords: Different keywords like palliative care, end of life care, dementia are used to search
relevant information from specific sites. Different government websites like health department of
New Zealand are searched with keywords like guidelines, palliative care framework and others.
Settings: For searching, relevant articles settings of databases are managed. Time frame is
selected from 2009 that has enabled to select only those articles or journals that are published
after 2009. Language is set in English and only peer-reviewed articles are collected.
End of life care and family support for patients with dementia.
Sampson, Goodman, and Robinson (2019) have stated that family members must have good
listening and communication skills along with a higher rate of patience. Behavior of family
members has a great impact on the mind of patients with dementia and positive behavior
encourages them to be calm and happy. For this study, relevant literature is being searched and
reviewed. These reviewing reveal different perspectives of the selected topic. Importance of
effective communication between family members and dementia patients are being discussed.
On the other hand, different potential processes that can be considered to improve patient care
quality are being presented in this study. Providing palliative care and family support can help
older people to fight with dementia.
1.3 Search strategy
A proper search strategy is used for accomplishing the task. Different relevant articles and
journals are researched from various sources that have proper information about the subject area.
A proper search strategy can help to increase the chance of a researcher to gain proper
information about a selected topic. In this research, different sources of data are explored and
appropriate articles are chosen for review.
Keywords: Different keywords like palliative care, end of life care, dementia are used to search
relevant information from specific sites. Different government websites like health department of
New Zealand are searched with keywords like guidelines, palliative care framework and others.
Settings: For searching, relevant articles settings of databases are managed. Time frame is
selected from 2009 that has enabled to select only those articles or journals that are published
after 2009. Language is set in English and only peer-reviewed articles are collected.
6
End of life care and family support for patients with dementia.
Databases: Various databases like Google scholar is used. Hits number in this site is 150. Other
sites like ProQuest are used and hits number in this site is 80. Total hits are 230 and different
ways are adopted to reduce the hits. More, specific keywords like end of life care for aged
patients and policies for home care staff are used to sort the proper articles. Total selected
journals are 12, which are used to critically analyze the topic under literature review portion.
1.4 Evaluation and critical discussion of literature
1.4.1 Dementia is everybody's business
Dementia has become one of the common problems of today's world and it is important to
eradicate this issue from society with a collaborative approach from all levels of society. In New
Zealand, the Health of older persons (HOP) is taking initiatives to influence people in taking care
of older adults, who are suffering from Dementia. As opined by Sampson et al. (2018), people
with dementia must get palliative care from healthcare professionals and their family members.
Sampson et al. (2018) have evaluated psychological and physical symptoms of dementia,
utilization of the services of the health and social care and the care received by these older
people in their end-of-life in UK. They have found that service provision is not fulfilling the
needs of these patients and longitudinal multidisciplinary input may help in optimizing quality of
life and control of symptom. On the contrary, Ashton, Roe, Jack and McClelland (2016) have
mentioned that everybody related to dementia patient must implement advanced care planning
(ACP). Especially, these findings of this research paper have considered that family carers are
allowed to take part in this planning for providing better quality palliative care to older dementia
patients in their end-of-life. The collaborative effort of caregivers and family members can
ensure a comfortable environment for older adults with dementia. Harrop, Nelson, Rees, Harris
End of life care and family support for patients with dementia.
Databases: Various databases like Google scholar is used. Hits number in this site is 150. Other
sites like ProQuest are used and hits number in this site is 80. Total hits are 230 and different
ways are adopted to reduce the hits. More, specific keywords like end of life care for aged
patients and policies for home care staff are used to sort the proper articles. Total selected
journals are 12, which are used to critically analyze the topic under literature review portion.
1.4 Evaluation and critical discussion of literature
1.4.1 Dementia is everybody's business
Dementia has become one of the common problems of today's world and it is important to
eradicate this issue from society with a collaborative approach from all levels of society. In New
Zealand, the Health of older persons (HOP) is taking initiatives to influence people in taking care
of older adults, who are suffering from Dementia. As opined by Sampson et al. (2018), people
with dementia must get palliative care from healthcare professionals and their family members.
Sampson et al. (2018) have evaluated psychological and physical symptoms of dementia,
utilization of the services of the health and social care and the care received by these older
people in their end-of-life in UK. They have found that service provision is not fulfilling the
needs of these patients and longitudinal multidisciplinary input may help in optimizing quality of
life and control of symptom. On the contrary, Ashton, Roe, Jack and McClelland (2016) have
mentioned that everybody related to dementia patient must implement advanced care planning
(ACP). Especially, these findings of this research paper have considered that family carers are
allowed to take part in this planning for providing better quality palliative care to older dementia
patients in their end-of-life. The collaborative effort of caregivers and family members can
ensure a comfortable environment for older adults with dementia. Harrop, Nelson, Rees, Harris
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
End of life care and family support for patients with dementia.
and Noble (2018) have argued that everyone in the society must understand this aspect of
palliative care for older dementia patients and treat them accordingly. Spreading awareness about
dementia and palliative care among society can help in this regard.
1.4.2 Palliative aged residential care guideline
Sampson et al. (2018) have stated that for it is important to consult with a general practitioner to
provide palliative residential care. In addition, note the importance of collect contacts of all
emergency services for providing palliative care (Sampson et al. 2018). On the other hand, Poole
et al. (2018) have stated that different barriers like pressure from different service provider and
other healthcare facilities need to be eliminated. In many cases, it can be seen that service
provides often pressure families of patients to move the person from a home-based setting to an
organizational care setting. In addition, it is stated that care staff need to maintain proper
communication with family regarding essential decisions that will be made about the patient
achieving end of life care (Poole et al. 2018). Hence, in both articles, one common aspect has
been highlighted and that is communication. The caregiver must maintain proper communication
with families and simultaneously with emergency service providers. This approach can help to
improve the quality of palliative aged care. In addition to this Boogaard et al. (2018) argued that
feedback can be used to improve the quality of palliative aged care. Caregivers need to translate
the feedback into care improvement approaches.
1.4.3 Guideline for providing care to people with dementia
There are different guidelines that can be maintained by nurses to offer care to people with
dementia. As opined by Harrop, Nelson, Rees, Harris, and Noble (2018), care to the people with
End of life care and family support for patients with dementia.
and Noble (2018) have argued that everyone in the society must understand this aspect of
palliative care for older dementia patients and treat them accordingly. Spreading awareness about
dementia and palliative care among society can help in this regard.
1.4.2 Palliative aged residential care guideline
Sampson et al. (2018) have stated that for it is important to consult with a general practitioner to
provide palliative residential care. In addition, note the importance of collect contacts of all
emergency services for providing palliative care (Sampson et al. 2018). On the other hand, Poole
et al. (2018) have stated that different barriers like pressure from different service provider and
other healthcare facilities need to be eliminated. In many cases, it can be seen that service
provides often pressure families of patients to move the person from a home-based setting to an
organizational care setting. In addition, it is stated that care staff need to maintain proper
communication with family regarding essential decisions that will be made about the patient
achieving end of life care (Poole et al. 2018). Hence, in both articles, one common aspect has
been highlighted and that is communication. The caregiver must maintain proper communication
with families and simultaneously with emergency service providers. This approach can help to
improve the quality of palliative aged care. In addition to this Boogaard et al. (2018) argued that
feedback can be used to improve the quality of palliative aged care. Caregivers need to translate
the feedback into care improvement approaches.
1.4.3 Guideline for providing care to people with dementia
There are different guidelines that can be maintained by nurses to offer care to people with
dementia. As opined by Harrop, Nelson, Rees, Harris, and Noble (2018), care to the people with
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
End of life care and family support for patients with dementia.
dementia must be evidence-based. Palliative care must be designed on the basis of information
gained about the stage of disease and different needs of patients. And following policies like
gathering knowledge about the appropriate service for the patient and maintaining proper
communication needs to be followed. Different information retrieval strategies like accessing
documents from patients, communicating with family and the physician must be adopted to gain
knowledge. Moreover, Jones et al. (2016) noted that care providers need to learn some skills that
are included in the guideline. For providing proper care to the person suffering from dementia, it
is essential for the caregiver to be compassionate, patient and attentive. This can help to increase
the quality of person-centered care. In addition, for application of intervention, it is essential for
caregivers to have a proper theoretical understanding (Jones et al. 2016). This can help to devise
appropriate strategy to mitigate different needs of patients.
1.4.4 Importance of communication between older people and their family
Effective communication between older dementia patients and their relatives helps in directing
the palliative care. As argued by Johnson and Bott (2016), dementia patients lose their ability to
think and make decisions of their own. Due to this, their family members look after them and
make decisions on their behalf. At the same time nurses must communicate with the family
members of older patients with dementia for understanding the patients’ physical and mental
condition (Harrop, Nelson, Rees, Harris, and Noble, 2018). Percival and Johnson (2013) argued
that nurses must be trained to provide palliative care to older people with dementia by involving
their family members in the care process. This kind of patients become sensitive and they seek
care from their family members. Due to their loss of memory and thinking process, dementia
patients become increasingly dependent on their family members. In that situation, their family
End of life care and family support for patients with dementia.
dementia must be evidence-based. Palliative care must be designed on the basis of information
gained about the stage of disease and different needs of patients. And following policies like
gathering knowledge about the appropriate service for the patient and maintaining proper
communication needs to be followed. Different information retrieval strategies like accessing
documents from patients, communicating with family and the physician must be adopted to gain
knowledge. Moreover, Jones et al. (2016) noted that care providers need to learn some skills that
are included in the guideline. For providing proper care to the person suffering from dementia, it
is essential for the caregiver to be compassionate, patient and attentive. This can help to increase
the quality of person-centered care. In addition, for application of intervention, it is essential for
caregivers to have a proper theoretical understanding (Jones et al. 2016). This can help to devise
appropriate strategy to mitigate different needs of patients.
1.4.4 Importance of communication between older people and their family
Effective communication between older dementia patients and their relatives helps in directing
the palliative care. As argued by Johnson and Bott (2016), dementia patients lose their ability to
think and make decisions of their own. Due to this, their family members look after them and
make decisions on their behalf. At the same time nurses must communicate with the family
members of older patients with dementia for understanding the patients’ physical and mental
condition (Harrop, Nelson, Rees, Harris, and Noble, 2018). Percival and Johnson (2013) argued
that nurses must be trained to provide palliative care to older people with dementia by involving
their family members in the care process. This kind of patients become sensitive and they seek
care from their family members. Due to their loss of memory and thinking process, dementia
patients become increasingly dependent on their family members. In that situation, their family
9
End of life care and family support for patients with dementia.
members need to communicate with them politely to gain their trust. D'astous, Abrams,
Vandrevala, Samsi and Manthorpe (2019) have supported this view following research findings
that often homecare workers fail to understand the needs of this kind of patients. As a result,
gaps in caregiving take place and create discomfort for the patient (Sampson et al. 2018).
1.4.5 Role played by family in directing care
Gott et al. (2018) recognized that not one health professionals but family and friends also play an
essential role in directing palliative care. Input regarding different needs of a patient is provided
by family members as they have closely observed the person. Hence, in the process of data
collection regarding patient's needs, family plays an important role. In addition, family members
also play a key part in eliminating patient loneliness and this support increases patient’s mental
strength (Morgan et al. 2016). Percival and Johnson (2013) agree that collaboration of family
with care staff is essential. Family can provide support to accomplish different daily activities of
the patient like washing and shaving. Moreover, family members need to assist the care
providers to select a proper place to provide end of life care. Family and friends need to create a
positive bond with palliative care provider for sharing different information about life history.
This communication can facilitate the process of care support (Jones et al. 2016). In general, it
can be said that family plays different roles that include healthcare expert, spokesperson, an
essential decision-maker, and expert to manage patient's wishes (Quinn et al. 2012). The health
care professional’s formal role includes communication with caregivers and supporting the care
process that helps to increase the quality and pace of care. Each role of family members is
considered as a part of potentially complicated family dynamics in the end of life decision-
making process (Johnson and Bott, 2016).
End of life care and family support for patients with dementia.
members need to communicate with them politely to gain their trust. D'astous, Abrams,
Vandrevala, Samsi and Manthorpe (2019) have supported this view following research findings
that often homecare workers fail to understand the needs of this kind of patients. As a result,
gaps in caregiving take place and create discomfort for the patient (Sampson et al. 2018).
1.4.5 Role played by family in directing care
Gott et al. (2018) recognized that not one health professionals but family and friends also play an
essential role in directing palliative care. Input regarding different needs of a patient is provided
by family members as they have closely observed the person. Hence, in the process of data
collection regarding patient's needs, family plays an important role. In addition, family members
also play a key part in eliminating patient loneliness and this support increases patient’s mental
strength (Morgan et al. 2016). Percival and Johnson (2013) agree that collaboration of family
with care staff is essential. Family can provide support to accomplish different daily activities of
the patient like washing and shaving. Moreover, family members need to assist the care
providers to select a proper place to provide end of life care. Family and friends need to create a
positive bond with palliative care provider for sharing different information about life history.
This communication can facilitate the process of care support (Jones et al. 2016). In general, it
can be said that family plays different roles that include healthcare expert, spokesperson, an
essential decision-maker, and expert to manage patient's wishes (Quinn et al. 2012). The health
care professional’s formal role includes communication with caregivers and supporting the care
process that helps to increase the quality and pace of care. Each role of family members is
considered as a part of potentially complicated family dynamics in the end of life decision-
making process (Johnson and Bott, 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

10
End of life care and family support for patients with dementia.
1.4.6 Palliative care for dementia patients in New Zealand
Framework for palliative care in case of dementia
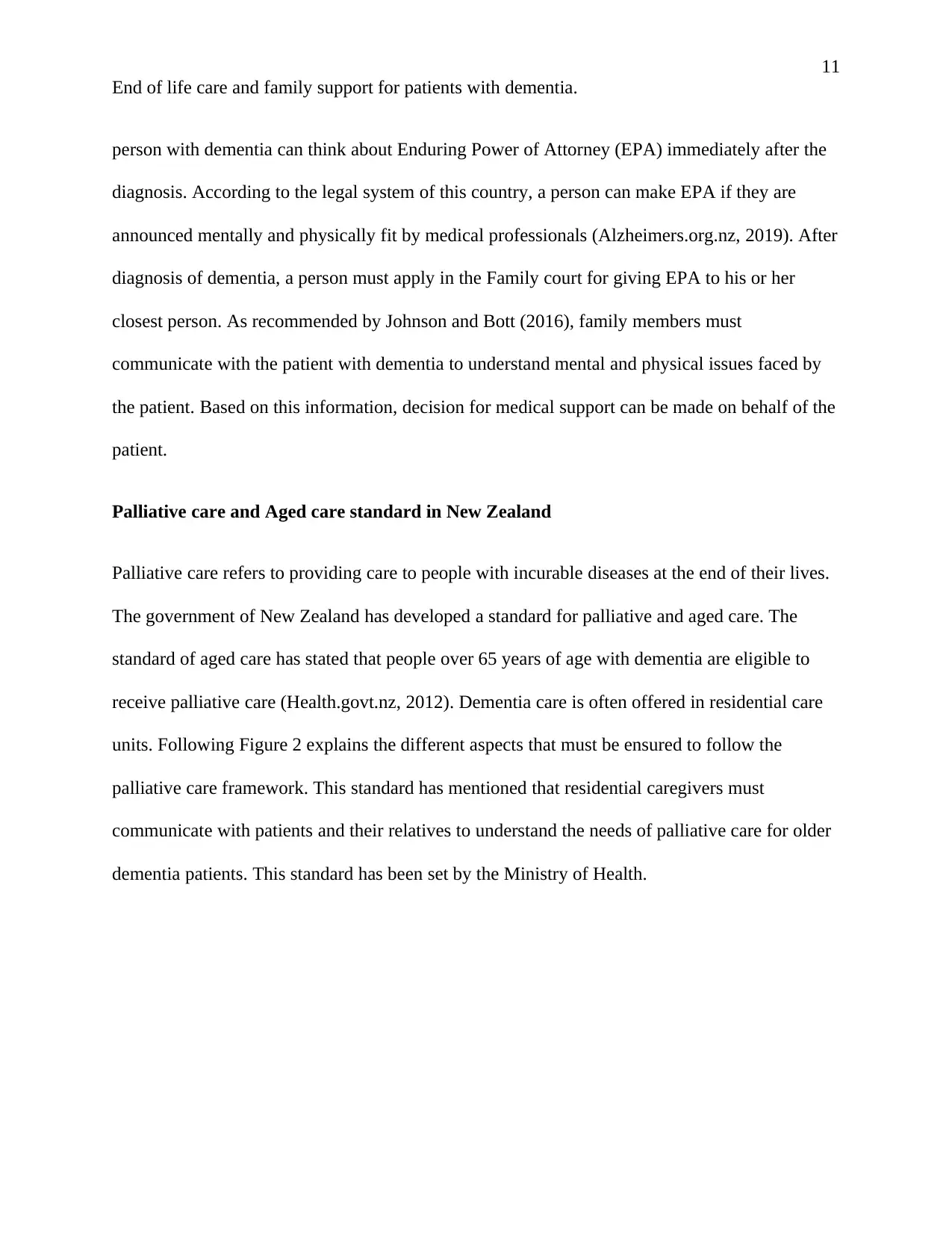
In New Zealand, older people are growing in number. Main vision for this framework of
dementia is to provide proper support to the patients and families. The health policy on dementia
has been developed by the Ministry of Health (Health.govt.nz, 2018). Main principles of this
framework include, following a person-centered as well as a people directed approach. Another
principle is to provide integrated, proactive services, which are flexible and meet different needs
of patients. Key elements of this framework include assessment and diagnosis of the disease and
providing early intervention, and meeting different barriers to increase well being and end of life
care.
Figure1: Key elements of framework
(Source: Health.govt.nz, 2018)
Power of attorney for making decisions in New Zealand
People often arrange for the closest person to them to have a power of attorney to make a
decision on their behalf in case they are not fit to make decisions of their own. In New Zealand, a
End of life care and family support for patients with dementia.
1.4.6 Palliative care for dementia patients in New Zealand
Framework for palliative care in case of dementia
In New Zealand, older people are growing in number. Main vision for this framework of
dementia is to provide proper support to the patients and families. The health policy on dementia
has been developed by the Ministry of Health (Health.govt.nz, 2018). Main principles of this
framework include, following a person-centered as well as a people directed approach. Another
principle is to provide integrated, proactive services, which are flexible and meet different needs
of patients. Key elements of this framework include assessment and diagnosis of the disease and
providing early intervention, and meeting different barriers to increase well being and end of life
care.
Figure1: Key elements of framework
(Source: Health.govt.nz, 2018)
Power of attorney for making decisions in New Zealand
People often arrange for the closest person to them to have a power of attorney to make a
decision on their behalf in case they are not fit to make decisions of their own. In New Zealand, a
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11
End of life care and family support for patients with dementia.
person with dementia can think about Enduring Power of Attorney (EPA) immediately after the
diagnosis. According to the legal system of this country, a person can make EPA if they are
announced mentally and physically fit by medical professionals (Alzheimers.org.nz, 2019). After
diagnosis of dementia, a person must apply in the Family court for giving EPA to his or her
closest person. As recommended by Johnson and Bott (2016), family members must
communicate with the patient with dementia to understand mental and physical issues faced by
the patient. Based on this information, decision for medical support can be made on behalf of the
patient.
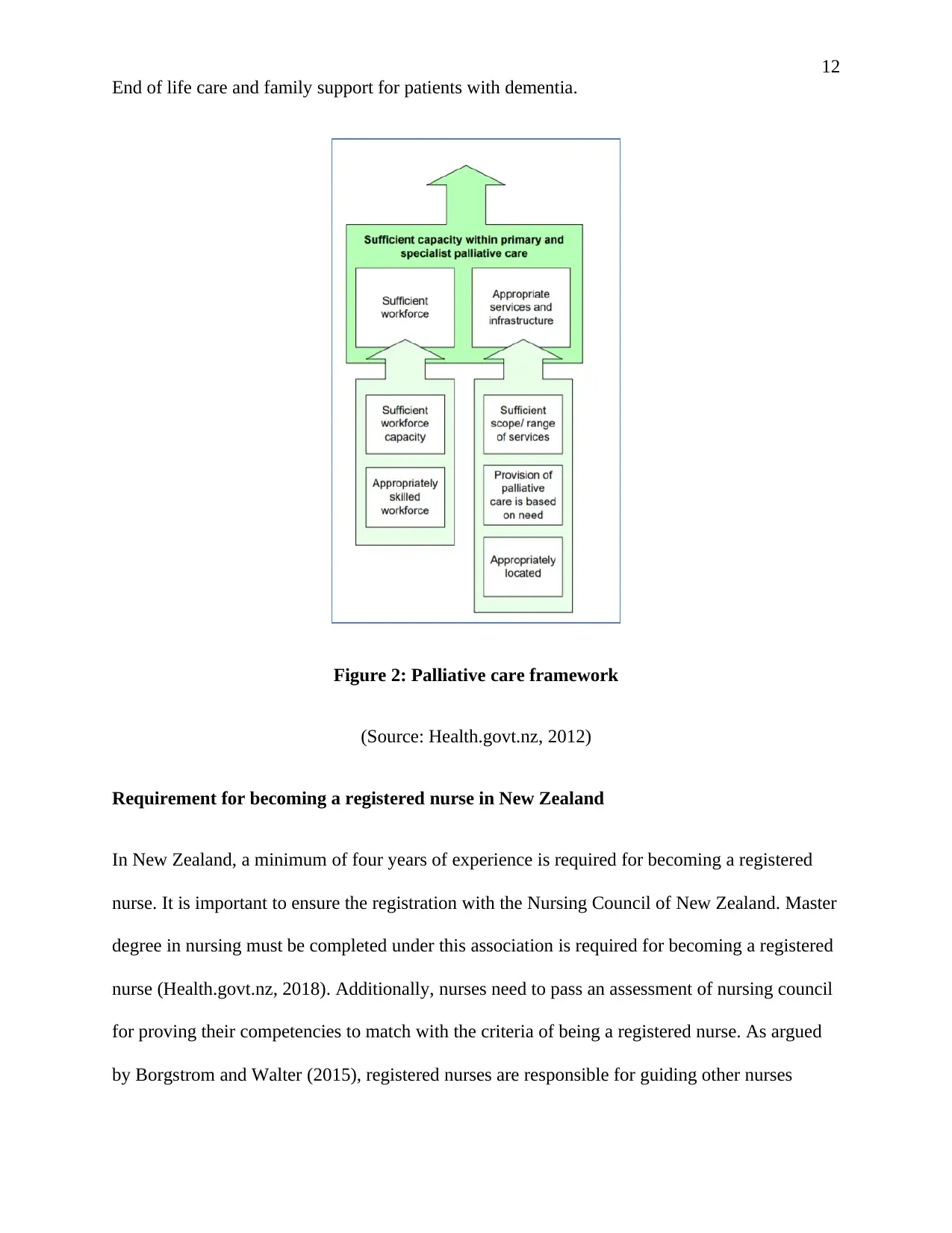
Palliative care and Aged care standard in New Zealand
Palliative care refers to providing care to people with incurable diseases at the end of their lives.
The government of New Zealand has developed a standard for palliative and aged care. The
standard of aged care has stated that people over 65 years of age with dementia are eligible to
receive palliative care (Health.govt.nz, 2012). Dementia care is often offered in residential care
units. Following Figure 2 explains the different aspects that must be ensured to follow the
palliative care framework. This standard has mentioned that residential caregivers must
communicate with patients and their relatives to understand the needs of palliative care for older
dementia patients. This standard has been set by the Ministry of Health.
End of life care and family support for patients with dementia.
person with dementia can think about Enduring Power of Attorney (EPA) immediately after the
diagnosis. According to the legal system of this country, a person can make EPA if they are
announced mentally and physically fit by medical professionals (Alzheimers.org.nz, 2019). After
diagnosis of dementia, a person must apply in the Family court for giving EPA to his or her
closest person. As recommended by Johnson and Bott (2016), family members must
communicate with the patient with dementia to understand mental and physical issues faced by
the patient. Based on this information, decision for medical support can be made on behalf of the
patient.
Palliative care and Aged care standard in New Zealand
Palliative care refers to providing care to people with incurable diseases at the end of their lives.
The government of New Zealand has developed a standard for palliative and aged care. The
standard of aged care has stated that people over 65 years of age with dementia are eligible to
receive palliative care (Health.govt.nz, 2012). Dementia care is often offered in residential care
units. Following Figure 2 explains the different aspects that must be ensured to follow the
palliative care framework. This standard has mentioned that residential caregivers must
communicate with patients and their relatives to understand the needs of palliative care for older
dementia patients. This standard has been set by the Ministry of Health.
12
End of life care and family support for patients with dementia.
Figure 2: Palliative care framework
(Source: Health.govt.nz, 2012)
Requirement for becoming a registered nurse in New Zealand
In New Zealand, a minimum of four years of experience is required for becoming a registered
nurse. It is important to ensure the registration with the Nursing Council of New Zealand. Master
degree in nursing must be completed under this association is required for becoming a registered
nurse (Health.govt.nz, 2018). Additionally, nurses need to pass an assessment of nursing council
for proving their competencies to match with the criteria of being a registered nurse. As argued
by Borgstrom and Walter (2015), registered nurses are responsible for guiding other nurses
End of life care and family support for patients with dementia.
Figure 2: Palliative care framework
(Source: Health.govt.nz, 2012)
Requirement for becoming a registered nurse in New Zealand
In New Zealand, a minimum of four years of experience is required for becoming a registered
nurse. It is important to ensure the registration with the Nursing Council of New Zealand. Master
degree in nursing must be completed under this association is required for becoming a registered
nurse (Health.govt.nz, 2018). Additionally, nurses need to pass an assessment of nursing council
for proving their competencies to match with the criteria of being a registered nurse. As argued
by Borgstrom and Walter (2015), registered nurses are responsible for guiding other nurses
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 20
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





