Financial Control, Budgeting, and Financial Constraints in Health Care
VerifiedAdded on 2023/06/12
|16
|5188
|408
Report
AI Summary
This report explores financial control and budgeting within the health and social care sector, focusing on the NHS. It examines the impact of legal, financial, and regulatory developments, the usefulness of alternative funding options like PFI, and the application of agency theory in the NHS context. Key stakeholders are identified, along with communication strategies. The report critically discusses the effects of financial constraints, costs, and budgets on health and social care services. Challenges in public sector budgeting, advantages and disadvantages of incremental and zero-based budgeting, and the calculation of break-even points are analyzed. The report concludes with a discussion of the key assumptions associated with the break-even model in today's business environment.

FINANCIAL CONTROL
AND BUDGETING
AND BUDGETING
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
INTRODUCTION...........................................................................................................................3
MAIN BODY...................................................................................................................................3
Recent Development In Health And Social Care In Terms Of Legal, Financial And Regulatory
Environment.................................................................................................................................3
Usefulness of alternate funding options:......................................................................................5
Agency Theory of NHS AND Importance of Stakeholders Of Social And Health Care And
The Ways Of Communication With Them..................................................................................6
Impact Of Financial Constraints, Costs And Budgets On Health And Social Care....................8
Challenges Of Budgeting In Public Sector Organization............................................................9
Advantages And Disadvantages Of Incremental And Zero-Based Budgeting............................9
Calculation of BEP and Margin of Safety.................................................................................11
Key assumptions attached to the breakeven model...................................................................13
CONCLUSION..............................................................................................................................13
REFERENCES................................................................................................................................1
INTRODUCTION...........................................................................................................................3
MAIN BODY...................................................................................................................................3
Recent Development In Health And Social Care In Terms Of Legal, Financial And Regulatory
Environment.................................................................................................................................3
Usefulness of alternate funding options:......................................................................................5
Agency Theory of NHS AND Importance of Stakeholders Of Social And Health Care And
The Ways Of Communication With Them..................................................................................6
Impact Of Financial Constraints, Costs And Budgets On Health And Social Care....................8
Challenges Of Budgeting In Public Sector Organization............................................................9
Advantages And Disadvantages Of Incremental And Zero-Based Budgeting............................9
Calculation of BEP and Margin of Safety.................................................................................11
Key assumptions attached to the breakeven model...................................................................13
CONCLUSION..............................................................................................................................13
REFERENCES................................................................................................................................1
INTRODUCTION
Financial control includes the procedures, policies and ways using which monitoring and
controlling the direction, allocation, and usage of financial resources is done by the organization.
Through budgeting firm creates a spending plan for its money to achieve its short and long term
goals. This report will discuss how the developments in the legal, financial and regulatory
aspects affects the environment of health and social care. Usefulness of various funding options
with respect to NHS will be discussed. Understanding of agency theory in context of NHS will
be done in this study. Corporate governance and accountability issues of NHS will be addressed.
Identification of key stakeholders of NHS and channels by which it communicates with these
stakeholders will be clarified. Critical discussion on the impact of financial constraints, costs and
budget on health and social care services of NHS and its stakeholders will be highlighted. In
addition, challenges in public sector budgeting will be studied. Various advantages and
disadvantages of incremental and zero-based budgeting will be analysed. Discussion on the key
assumptions associated with break-even model in context of today's business environment's
reality will be done.
MAIN BODY
Recent Development In Health And Social Care In Terms Of Legal, Financial And Regulatory
Environment
Health and social care is effected by varied external factors in its environment.
Legal:
There are various laws that abides the working of Health and Social Care. The Health and
Social Care Act, 2012 specifies the duties for health bodies. It covers all health bodies including
the Department of Health, Public Health England, Clinical Commissioning Groups, and NHS
England. This act brought changes on public health functions by local authorities in regard to
reduce health inequalities among the people of England (Kloss, 2020). The Equality Act, 2010
states equality duties concerning all public sector bodies with the aim to incorporate
consideration relating to equality in everyday business. The Social Value Act, 2012 considers
economic, social and environmental wellness in acquisition of services by public sector
commissioners including local authorities and health sector bodies.
Financial control includes the procedures, policies and ways using which monitoring and
controlling the direction, allocation, and usage of financial resources is done by the organization.
Through budgeting firm creates a spending plan for its money to achieve its short and long term
goals. This report will discuss how the developments in the legal, financial and regulatory
aspects affects the environment of health and social care. Usefulness of various funding options
with respect to NHS will be discussed. Understanding of agency theory in context of NHS will
be done in this study. Corporate governance and accountability issues of NHS will be addressed.
Identification of key stakeholders of NHS and channels by which it communicates with these
stakeholders will be clarified. Critical discussion on the impact of financial constraints, costs and
budget on health and social care services of NHS and its stakeholders will be highlighted. In
addition, challenges in public sector budgeting will be studied. Various advantages and
disadvantages of incremental and zero-based budgeting will be analysed. Discussion on the key
assumptions associated with break-even model in context of today's business environment's
reality will be done.
MAIN BODY
Recent Development In Health And Social Care In Terms Of Legal, Financial And Regulatory
Environment
Health and social care is effected by varied external factors in its environment.
Legal:
There are various laws that abides the working of Health and Social Care. The Health and
Social Care Act, 2012 specifies the duties for health bodies. It covers all health bodies including
the Department of Health, Public Health England, Clinical Commissioning Groups, and NHS
England. This act brought changes on public health functions by local authorities in regard to
reduce health inequalities among the people of England (Kloss, 2020). The Equality Act, 2010
states equality duties concerning all public sector bodies with the aim to incorporate
consideration relating to equality in everyday business. The Social Value Act, 2012 considers
economic, social and environmental wellness in acquisition of services by public sector
commissioners including local authorities and health sector bodies.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Financial:
In the recent years capital spending of NHS has been cut down to meet the rising
requirements of the day to day operating costs. Cutting down capital expenditure resulted in poor
maintenance of building, outdated machines and inadequate services in primary care. Capital
projects take years for completion so NHS requires long term settlements for the capital projects.
In the recent health care bill plans have been proposed to change NHS rules (Pinedo-Villanueva
and et.al., 2019). The changes propose to ease the tension between the rules that are in the form,
written in the Health and Social Care Act 2012 and the rules that are in use in present times.
Integrated care system will cover all the parts of England.
Regulation:
The way health care is managed and regulated in England, Scotland and Wales is
different. The General Medical Council (GMC) and Nursing And Midwifery Council (NMC) are
the two regulatory bodies playing great roles to secure professional standards are to be
maintained. A range of powers is exercised by the varied regulators across the Great Britain to
ensure the betterment and justice. The Health and Safety Executive (HSE) is national regulator
ensuring workplace health and safety in Britain (Bolton, and Gillett, 2019). It sets the public
safety policy and priorities for compel. There are two aspects of regulation of health and social
care that Care Quality Commission (CQO) assures in England. First to regulate the quality and
safety areas of care that is offered to the public. Second regulation is to regulate the market in
health care services. This consists of care regulation that NHS, local authorities, independent
providers and registered voluntary organizations provides, social care service providers in care
homes for adults and service providers to those whose rights are restricted under the Mental
Health Act. Regulators operating in Scotland comprises three parts: (i) Healthcare Improvement
Scotland (HIS) -the Healthcare Environment Inspectorate (HEI) is a part of HIS. HIS focuses on
reduction of infection risk associated to health care of patients, improvement in the care provided
to elderly patients, inspection framework to regulate the independent healthcare services, (ii)
Care inspectorate -in order to scrutinize social care and work, and child protection services The
Social Care Work Improvement Scotland (SCSWIS), commonly known as care inspectorate
operates, (iii) Mental Welfare Commission for Scotland (MWC) -it promotes the welfare of
those with mental illness, learning disability and related conditions. There are two regulators in
In the recent years capital spending of NHS has been cut down to meet the rising
requirements of the day to day operating costs. Cutting down capital expenditure resulted in poor
maintenance of building, outdated machines and inadequate services in primary care. Capital
projects take years for completion so NHS requires long term settlements for the capital projects.
In the recent health care bill plans have been proposed to change NHS rules (Pinedo-Villanueva
and et.al., 2019). The changes propose to ease the tension between the rules that are in the form,
written in the Health and Social Care Act 2012 and the rules that are in use in present times.
Integrated care system will cover all the parts of England.
Regulation:
The way health care is managed and regulated in England, Scotland and Wales is
different. The General Medical Council (GMC) and Nursing And Midwifery Council (NMC) are
the two regulatory bodies playing great roles to secure professional standards are to be
maintained. A range of powers is exercised by the varied regulators across the Great Britain to
ensure the betterment and justice. The Health and Safety Executive (HSE) is national regulator
ensuring workplace health and safety in Britain (Bolton, and Gillett, 2019). It sets the public
safety policy and priorities for compel. There are two aspects of regulation of health and social
care that Care Quality Commission (CQO) assures in England. First to regulate the quality and
safety areas of care that is offered to the public. Second regulation is to regulate the market in
health care services. This consists of care regulation that NHS, local authorities, independent
providers and registered voluntary organizations provides, social care service providers in care
homes for adults and service providers to those whose rights are restricted under the Mental
Health Act. Regulators operating in Scotland comprises three parts: (i) Healthcare Improvement
Scotland (HIS) -the Healthcare Environment Inspectorate (HEI) is a part of HIS. HIS focuses on
reduction of infection risk associated to health care of patients, improvement in the care provided
to elderly patients, inspection framework to regulate the independent healthcare services, (ii)
Care inspectorate -in order to scrutinize social care and work, and child protection services The
Social Care Work Improvement Scotland (SCSWIS), commonly known as care inspectorate
operates, (iii) Mental Welfare Commission for Scotland (MWC) -it promotes the welfare of
those with mental illness, learning disability and related conditions. There are two regulators in
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Wales. First, Care Inspectorate Wales (CIW), regulates social care, early years services and local
authority care support services (Agarwal and et.al., 2019). Second, Healthcare Inspectorate
Wales (HIW) -its role is to inspect NHS and independent healthcare organizations. Medicines
and Healthcare Products Regulatory Agency (MHRA) is a government agency accountable for
regulating medicines and medical devices and tools in healthcare in whole United Kingdom.
Usefulness of alternate funding options:
Private Finance Initiatives(PFI) -risk connected with modernizing health care facilities is
shifted to private sector. All the expenses incurred to build the system, buying of equipments,
related operating costs and performance are included. Previously health care services were
underinvested which resulted in poor maintenance. PFI projects have started resolving the issue
(Whiteside, 2020). This also provides professionals with the opportunities to explore new career
pathways. The PFI hospitals are more accountable to provide quality services and better
environment to patients. The score of cleanliness has increased.
Agency partnerships -it focuses at enhancing the efficiency and quality of services
available at health care centres and hospitals. It establishes the one stop building for all the
patients. Care is available nearer to patients' homes. Greater choices and autonomy provided to
users along with the support to the service providers (Mell, 2018). Duplication of facilities
provided to users eliminates. Team roles are made clear for better understanding. Volunteers and
professionals have higher job satisfaction. It facilitates multi-skill development of the manpower.
Reduction in overlapping of activities resulting in better usage of calibre of front-line workers.
Early and safe discharge of patient rate increased. Role of generic health and social care
strengthened. Improvement in retention of support workers.
Competitive tendering -more choices and diversified provisions available to those who
use the services. It represents more potential opportunities for approaches to be applied for
service provisions for more people (Zhang and et.al., 2019). Social care and support members
can use it to stimulate market of lively labour providing them the best exchange for the skills and
experience they have. It acts as a key tool in the diversification of local market that promotes
innovations in cost and quality.
authority care support services (Agarwal and et.al., 2019). Second, Healthcare Inspectorate
Wales (HIW) -its role is to inspect NHS and independent healthcare organizations. Medicines
and Healthcare Products Regulatory Agency (MHRA) is a government agency accountable for
regulating medicines and medical devices and tools in healthcare in whole United Kingdom.
Usefulness of alternate funding options:
Private Finance Initiatives(PFI) -risk connected with modernizing health care facilities is
shifted to private sector. All the expenses incurred to build the system, buying of equipments,
related operating costs and performance are included. Previously health care services were
underinvested which resulted in poor maintenance. PFI projects have started resolving the issue
(Whiteside, 2020). This also provides professionals with the opportunities to explore new career
pathways. The PFI hospitals are more accountable to provide quality services and better
environment to patients. The score of cleanliness has increased.
Agency partnerships -it focuses at enhancing the efficiency and quality of services
available at health care centres and hospitals. It establishes the one stop building for all the
patients. Care is available nearer to patients' homes. Greater choices and autonomy provided to
users along with the support to the service providers (Mell, 2018). Duplication of facilities
provided to users eliminates. Team roles are made clear for better understanding. Volunteers and
professionals have higher job satisfaction. It facilitates multi-skill development of the manpower.
Reduction in overlapping of activities resulting in better usage of calibre of front-line workers.
Early and safe discharge of patient rate increased. Role of generic health and social care
strengthened. Improvement in retention of support workers.
Competitive tendering -more choices and diversified provisions available to those who
use the services. It represents more potential opportunities for approaches to be applied for
service provisions for more people (Zhang and et.al., 2019). Social care and support members
can use it to stimulate market of lively labour providing them the best exchange for the skills and
experience they have. It acts as a key tool in the diversification of local market that promotes
innovations in cost and quality.
Outsourcing –results in better HR services that helps in managing human resource
administration and benefits the overall assistance. Outsourcing of HR team can provide better
value of packages and health insurance. It assists varied facilities like creating manuals and
handbooks of employees, hiring and training workforce at improved costs. Outsourcing of
activities is (cost-effective) than appointing highly-qualified staff for the performance of
activities. Management of payroll is good, timely and accurate. It keeps a check on operational
costs (Šeba, 2018). Outsourcing of activities like service call centres, technical helpdesks, IT
systems, etc. saves infrastructural investments. Movement to new technologies is possible with
minimal downtime, increased productivity and quality. Benefits of the best services and
infrastructure can be exploited to improve performance of operations. Outsourcing of one time
activities that require manpower resources removes unnecessary burden. Risk management is
enhanced and hence it takes less time to respond to situations of calamities.
Agency Theory of NHS AND Importance of Stakeholders Of Social And Health Care And The
Ways Of Communication With Them.
The agency theory is a principal that explains and resolves the issues that arises in the relation
ship between the principal and their agents. The relationship arises when the principal engages
agent for the performance of certain work on the behalf of the principal thus there is involvement
of delegating the authorities. In respect of NHS, it is agent and various shareholders investing in
it are the principal. The focus is to allocate the available resources in such a way the health of the
population improves assuring maximum outcomes. But the resources are managed by the people
so optimum allocation is not possible unless decision makers are motivated to do so. Allocation
of resources relied on the decisions made by physicians largely. The behavioural characteristics
of the physician is the key issue of health economics (Pepper, PEPPER and Barlow, 2019). The
main goal of the physician is to make an efficient health care system. Effectiveness of the
decision made by motivated physician reflect in the facilities at hospitals and health care centres.
Fee for the services reflects the coordination of the interests of both the physician and the patient.
This ensures at the physician provides everything essential with the influence of any external
constraint. Three types of incentives are created for the motivation of the physicians. An
incentive to accept and retain all patients, incentive to regulate the use to resources to avoid
administration and benefits the overall assistance. Outsourcing of HR team can provide better
value of packages and health insurance. It assists varied facilities like creating manuals and
handbooks of employees, hiring and training workforce at improved costs. Outsourcing of
activities is (cost-effective) than appointing highly-qualified staff for the performance of
activities. Management of payroll is good, timely and accurate. It keeps a check on operational
costs (Šeba, 2018). Outsourcing of activities like service call centres, technical helpdesks, IT
systems, etc. saves infrastructural investments. Movement to new technologies is possible with
minimal downtime, increased productivity and quality. Benefits of the best services and
infrastructure can be exploited to improve performance of operations. Outsourcing of one time
activities that require manpower resources removes unnecessary burden. Risk management is
enhanced and hence it takes less time to respond to situations of calamities.
Agency Theory of NHS AND Importance of Stakeholders Of Social And Health Care And The
Ways Of Communication With Them.
The agency theory is a principal that explains and resolves the issues that arises in the relation
ship between the principal and their agents. The relationship arises when the principal engages
agent for the performance of certain work on the behalf of the principal thus there is involvement
of delegating the authorities. In respect of NHS, it is agent and various shareholders investing in
it are the principal. The focus is to allocate the available resources in such a way the health of the
population improves assuring maximum outcomes. But the resources are managed by the people
so optimum allocation is not possible unless decision makers are motivated to do so. Allocation
of resources relied on the decisions made by physicians largely. The behavioural characteristics
of the physician is the key issue of health economics (Pepper, PEPPER and Barlow, 2019). The
main goal of the physician is to make an efficient health care system. Effectiveness of the
decision made by motivated physician reflect in the facilities at hospitals and health care centres.
Fee for the services reflects the coordination of the interests of both the physician and the patient.
This ensures at the physician provides everything essential with the influence of any external
constraint. Three types of incentives are created for the motivation of the physicians. An
incentive to accept and retain all patients, incentive to regulate the use to resources to avoid
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

wastage of resources, an incentive to choose patient with low health risk, for avoidance of
consumption of medical services in larger amount.
Patients, caregivers, doctors, nurses, employees, employers, government, universities,
insurance companies, communities, and pharmaceutical firms are the stakeholders of health and
social care. Stakeholders are very vital for health and social care industry, their support provides
funds, skills and knowledge for the effective performance of the health care system.
Corporate governance is the system by which board-led organizations are directed and
governed at the senior levels to achieve its objectives and meet the necessary benchmark of
accountability and probity. NHS boards consist of a crowded organizational landscape that
includes a range of public, private, and community organizations serving widely to the citizens.
Accountability is a challenge for NHS. There is lack of accountability in NHS because of
varied reasons. Freedom of information NHS organizations including trusts, CCGs and NHS
itself have freedom of regulations (Hyndman and McKillop, 2018). Commercial confidentiality
is often cited by NHS organization and council as a result for non disclose full and detailed
information on contracts between the NHS.
Ways of communication:
NHS uses its own strategies to communicate to its stakeholders. It sets proposals with
respect to the Francis report. Clinicians follow Francis Report principles stated in the guidelines
for better communication, ensuring quality services and care being delivered to the citizens. In
addition, it sets proposals in the context of agile that is a 21st century model for collaborative
functioning. It focuses on the value that organizational boundaries must not ever show
carelessness in providing commitment to deliver best of services at scale in the partnership.
Lastly it also sets proposals for specialized care with the view to give better outcomes (Albury
and et.al., 2020). To reduce the proactive and open communication methods have been deployed.
Varied channels are used communicating firstly targeted communications are development to
communicate with the key stakeholders this consists targeted letters to shareholders, briefings for
teams inside the organization. Face to face communications are generally preferred in this type,
telephonic conversations and emails are secondary methods here. Next way of communication is
through using printed, electronic and face to face communication with partner firms in this part
internal mediums such as intranets, electronic bulletins, management briefing are used. Further
certain external channels like UCL partners' website, trust website and GP newsletters are used
consumption of medical services in larger amount.
Patients, caregivers, doctors, nurses, employees, employers, government, universities,
insurance companies, communities, and pharmaceutical firms are the stakeholders of health and
social care. Stakeholders are very vital for health and social care industry, their support provides
funds, skills and knowledge for the effective performance of the health care system.
Corporate governance is the system by which board-led organizations are directed and
governed at the senior levels to achieve its objectives and meet the necessary benchmark of
accountability and probity. NHS boards consist of a crowded organizational landscape that
includes a range of public, private, and community organizations serving widely to the citizens.
Accountability is a challenge for NHS. There is lack of accountability in NHS because of
varied reasons. Freedom of information NHS organizations including trusts, CCGs and NHS
itself have freedom of regulations (Hyndman and McKillop, 2018). Commercial confidentiality
is often cited by NHS organization and council as a result for non disclose full and detailed
information on contracts between the NHS.
Ways of communication:
NHS uses its own strategies to communicate to its stakeholders. It sets proposals with
respect to the Francis report. Clinicians follow Francis Report principles stated in the guidelines
for better communication, ensuring quality services and care being delivered to the citizens. In
addition, it sets proposals in the context of agile that is a 21st century model for collaborative
functioning. It focuses on the value that organizational boundaries must not ever show
carelessness in providing commitment to deliver best of services at scale in the partnership.
Lastly it also sets proposals for specialized care with the view to give better outcomes (Albury
and et.al., 2020). To reduce the proactive and open communication methods have been deployed.
Varied channels are used communicating firstly targeted communications are development to
communicate with the key stakeholders this consists targeted letters to shareholders, briefings for
teams inside the organization. Face to face communications are generally preferred in this type,
telephonic conversations and emails are secondary methods here. Next way of communication is
through using printed, electronic and face to face communication with partner firms in this part
internal mediums such as intranets, electronic bulletins, management briefing are used. Further
certain external channels like UCL partners' website, trust website and GP newsletters are used
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

(Barnes, 2019). Meetings and events are organized for the commissioner consultation
engagement processes, this includes workshops for stakeholders.
Impact Of Financial Constraints, Costs And Budgets On Health And Social Care.
United Kingdom has seen mortality trends recently. There have been slow and gradual
reductions in mortality rates. UK have experienced the smallest gains in terms of life expectancy
for both males and females. These changes in mortality rate have affected the whole population
of the Scotland. These changes in mortality rate has increased pressure on health and social care.
Responding to the financial crash of 2007 and the following recession UK adopted austerity
policies, that leads to shortfall in many areas of public spending. Government healthcare
spending supported NHS in its times of financial crises. Proportion of healthcare spending
changed and England experienced most spending and spendings were lowest the Scotland.
Constraints have also been imposed on social care. Local Authorities spending on social care and
work reduced. The Greatest cuts were in England that had very low per capita spending. These
financial pressure resulted in the introduction of the national living wage. The national wage
estimates to result in additional costing to care system to a great extent (Gaughan and et.al.,
2019). As a result of financial constraints social care services are facing a lot of challenges
across the country. For instance major demographic changes are occurring in Scotland. Studies'
estimates clearly show that there will be very low working age population as compared to the of
retired population. This reflects that there will be increasing ratio of population that relies on
adult social care facilities and working age population proportion will reduce significantly.
Privatisation of the health and social care services have seen an increase with the Health
and Social Care Act. This led to alterations in working of regulation in regards of NHS
provisions and purchase. Positive competition is assumed as it leads to improved quality of care
services. The differences in the extent to which the NHS is privatized in different parts of UK
have increased the costs without relatable improvements in services (Le Grand and Robinson,
2018). When talked about private funding much of adult social care is funded in this way.
Percentage of home beds at nursing has drastically fell over the decades. The estimation of The
National Audit Office(NAO) says that the cost of informal care of adult social care facilities is
equal to six times of public spending. Some evidences show that the increased privatization of
social care service provision resulted in reduced social care service quality.
engagement processes, this includes workshops for stakeholders.
Impact Of Financial Constraints, Costs And Budgets On Health And Social Care.
United Kingdom has seen mortality trends recently. There have been slow and gradual
reductions in mortality rates. UK have experienced the smallest gains in terms of life expectancy
for both males and females. These changes in mortality rate have affected the whole population
of the Scotland. These changes in mortality rate has increased pressure on health and social care.
Responding to the financial crash of 2007 and the following recession UK adopted austerity
policies, that leads to shortfall in many areas of public spending. Government healthcare
spending supported NHS in its times of financial crises. Proportion of healthcare spending
changed and England experienced most spending and spendings were lowest the Scotland.
Constraints have also been imposed on social care. Local Authorities spending on social care and
work reduced. The Greatest cuts were in England that had very low per capita spending. These
financial pressure resulted in the introduction of the national living wage. The national wage
estimates to result in additional costing to care system to a great extent (Gaughan and et.al.,
2019). As a result of financial constraints social care services are facing a lot of challenges
across the country. For instance major demographic changes are occurring in Scotland. Studies'
estimates clearly show that there will be very low working age population as compared to the of
retired population. This reflects that there will be increasing ratio of population that relies on
adult social care facilities and working age population proportion will reduce significantly.
Privatisation of the health and social care services have seen an increase with the Health
and Social Care Act. This led to alterations in working of regulation in regards of NHS
provisions and purchase. Positive competition is assumed as it leads to improved quality of care
services. The differences in the extent to which the NHS is privatized in different parts of UK
have increased the costs without relatable improvements in services (Le Grand and Robinson,
2018). When talked about private funding much of adult social care is funded in this way.
Percentage of home beds at nursing has drastically fell over the decades. The estimation of The
National Audit Office(NAO) says that the cost of informal care of adult social care facilities is
equal to six times of public spending. Some evidences show that the increased privatization of
social care service provision resulted in reduced social care service quality.
All the residents are entitled to public health care through National Health Service at free
of cost. The NHS budget is funded primarily through general taxation. NHS is a government
agency that look after and allocates funds to 191 Clinical Commissioning Groups, which govern
and pay for availability of care at local level. NHS England manages NHS budget. NHS pays for
preventive services, that consists screenings, immunizations and vaccination programs, inpatient
and outpatient medical care, maternity care, services provided by physician, necessary dental and
eye care, mental health care, palliative care, long term care, rehabilitation, wheelchairs, hearing
aids.
Challenges Of Budgeting In Public Sector Organization.
Ever since the establishment of NHS its allocated budget rises every year but the rate of
the rise is lower than it used to be. Use of private companies for funding has increased over the
years. The three key targets of health care namely accident and emergency(A & E), cancer care
and routine operations are getting worse and whole UK is struggling to improve the situation
(Siverbo, Cäker and Åkesson, 2019). The population is getting old, ageing of population is one
of the main problem system is suffering with. Care for older population is costly. Expenses for
care of ninety plus age section of population is seven times the expense incurred on those
belonging to thirty plus section. As a result of low budget nearly 100k jobs of NHS are vacant.
Out of the total money put in by the government a large part is kept aside for capital projects,
that provides for the infrastructural costs like IT and construction or maintenance of the buildings
(Hijal-Moghrabi, 2019). Free care is not accessible to all older people. Problems in the social
care system implies pressure on NHS. Social care includes day centres, in house help in
household chores, and quality care in the final years of life. Shortfall in budget have resulted in
over workloads on staff members, pay has been curbed, declined morale in stakeholders, these
factors' consequences are reflected in A&E crises, increased waiting time, and inferior patient
experience.
Advantages And Disadvantages Of Incremental And Zero-Based Budgeting.
Incremental budgeting is a type of preparing budget that is based on the idea that new
budget is best prepared on the basis of alteration made to the previous financial year's budget.
Commonly incremental budgeting use inflation rate as a guide for the adjustment factor in
creation of incremental budget.
Pros:
of cost. The NHS budget is funded primarily through general taxation. NHS is a government
agency that look after and allocates funds to 191 Clinical Commissioning Groups, which govern
and pay for availability of care at local level. NHS England manages NHS budget. NHS pays for
preventive services, that consists screenings, immunizations and vaccination programs, inpatient
and outpatient medical care, maternity care, services provided by physician, necessary dental and
eye care, mental health care, palliative care, long term care, rehabilitation, wheelchairs, hearing
aids.
Challenges Of Budgeting In Public Sector Organization.
Ever since the establishment of NHS its allocated budget rises every year but the rate of
the rise is lower than it used to be. Use of private companies for funding has increased over the
years. The three key targets of health care namely accident and emergency(A & E), cancer care
and routine operations are getting worse and whole UK is struggling to improve the situation
(Siverbo, Cäker and Åkesson, 2019). The population is getting old, ageing of population is one
of the main problem system is suffering with. Care for older population is costly. Expenses for
care of ninety plus age section of population is seven times the expense incurred on those
belonging to thirty plus section. As a result of low budget nearly 100k jobs of NHS are vacant.
Out of the total money put in by the government a large part is kept aside for capital projects,
that provides for the infrastructural costs like IT and construction or maintenance of the buildings
(Hijal-Moghrabi, 2019). Free care is not accessible to all older people. Problems in the social
care system implies pressure on NHS. Social care includes day centres, in house help in
household chores, and quality care in the final years of life. Shortfall in budget have resulted in
over workloads on staff members, pay has been curbed, declined morale in stakeholders, these
factors' consequences are reflected in A&E crises, increased waiting time, and inferior patient
experience.
Advantages And Disadvantages Of Incremental And Zero-Based Budgeting.
Incremental budgeting is a type of preparing budget that is based on the idea that new
budget is best prepared on the basis of alteration made to the previous financial year's budget.
Commonly incremental budgeting use inflation rate as a guide for the adjustment factor in
creation of incremental budget.
Pros:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
It is easy to implement as detailed analysis is not needed while preparing budget in this
type of budget preparation. It favours the projects or programs that requires funding for multiple
years ensuring availability of stable funds all during the program. Consistent operation of
departments. Similar treatment to departments resulting in fewer inter departmental conflicts.
Budgets same year after year so if any change is made it can be easily identified by seeing last
budget (Beredugo, Azubike and Okon, 2019). It is a very flexible approach for instance, it can be
done every month and all changes are clearly visible. This approach is widely used and adopted
in the modern business world.
Cons:
Each department's allocated budget gets increased every year but not all departments
actually needs increment very year. Departments tend to spend whole budget allotted to them
just to get more budget next year. This results in unnecessary promotion of spending by the
departments. Hence, this process can be wasteful and slightly inefficient for the company.
Making same budget year after year kills the scope for allocation of budget for innovative
activities or processes (Tahar and Eltweri, 2018). Discouragement to innovations and new ideas
creates conservative environment inside the business. The approach is based on the idea of
stability in the operations of the company. Thus, it can result in failure in competitively
encountering the unforeseen changes in external environment of the business. This type of
budgeting does not provide for incentives to the management.
Zero-Based budgeting in an approach to form budget in which budget is made starting
from zero every year. In this type of method all the expenses incurred in last financial are
justified in that period only the idea in this is to allot finance to important areas of concern.
Advantages:
All the items that results in cash inflow and outflow are carefully checked, so there is
accuracy of data while preparing budget using this approach. Zero based budgeting keeps the
firm completely aware about the actual amount that is going in and out of the accounts every
month. Historic figures are overlooked and focus is on actual numbers this leads to efficient
allocation of resources to each department (Al-attara, Mashkourb and Hassanc, 2020). As
allotment of resources between different departments is entirely based on the efficiency of the
department conflicts are less.
type of budget preparation. It favours the projects or programs that requires funding for multiple
years ensuring availability of stable funds all during the program. Consistent operation of
departments. Similar treatment to departments resulting in fewer inter departmental conflicts.
Budgets same year after year so if any change is made it can be easily identified by seeing last
budget (Beredugo, Azubike and Okon, 2019). It is a very flexible approach for instance, it can be
done every month and all changes are clearly visible. This approach is widely used and adopted
in the modern business world.
Cons:
Each department's allocated budget gets increased every year but not all departments
actually needs increment very year. Departments tend to spend whole budget allotted to them
just to get more budget next year. This results in unnecessary promotion of spending by the
departments. Hence, this process can be wasteful and slightly inefficient for the company.
Making same budget year after year kills the scope for allocation of budget for innovative
activities or processes (Tahar and Eltweri, 2018). Discouragement to innovations and new ideas
creates conservative environment inside the business. The approach is based on the idea of
stability in the operations of the company. Thus, it can result in failure in competitively
encountering the unforeseen changes in external environment of the business. This type of
budgeting does not provide for incentives to the management.
Zero-Based budgeting in an approach to form budget in which budget is made starting
from zero every year. In this type of method all the expenses incurred in last financial are
justified in that period only the idea in this is to allot finance to important areas of concern.
Advantages:
All the items that results in cash inflow and outflow are carefully checked, so there is
accuracy of data while preparing budget using this approach. Zero based budgeting keeps the
firm completely aware about the actual amount that is going in and out of the accounts every
month. Historic figures are overlooked and focus is on actual numbers this leads to efficient
allocation of resources to each department (Al-attara, Mashkourb and Hassanc, 2020). As
allotment of resources between different departments is entirely based on the efficiency of the
department conflicts are less.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
It leads to discontinuation of obsolete processes as all the activities that are inefficient are
eliminated. This help business to improve its costs and prices. Benefits of minimal operating
expenses as managers must provide justification for all the expenses incurred, as a result they
think about the worthiness of every penny that will be spent before actual expense is made.
Budget can be customized by the organization depending upon the needs.
Zero-Based budgeting accounting ensures a way to manage the expenses most efficiently.
Any changes that relates to the line-item needed every month can be made. So firm always
knows where its cash is going and it is easy to cut back the expenses in order to make emergency
funds. It allows to keep a check on legacy expenses (Miller, 2018). The traditional budgeting
processes focus on the amount that is spent every time an expense occurs while zero-based
budgeting also considers the reason behind making spending decision. The goal of this method
of budgeting is to correct the current spending habits that lead to drain out finances of the
company.
Disadvantages:
Justifying every expense is time-intensive activity. Close monitoring of every expense is
need to be done every month. That makes the event more time-consuming activity. It can reward
short term thinking, areas where revenue will generate in next financial year will be preferred
and those areas where benefits will generate in long run are neglected. Example- research and
development. Manipulation is also a crucial disadvantage. Savvy managers can manipulate the
budget to get more resources.
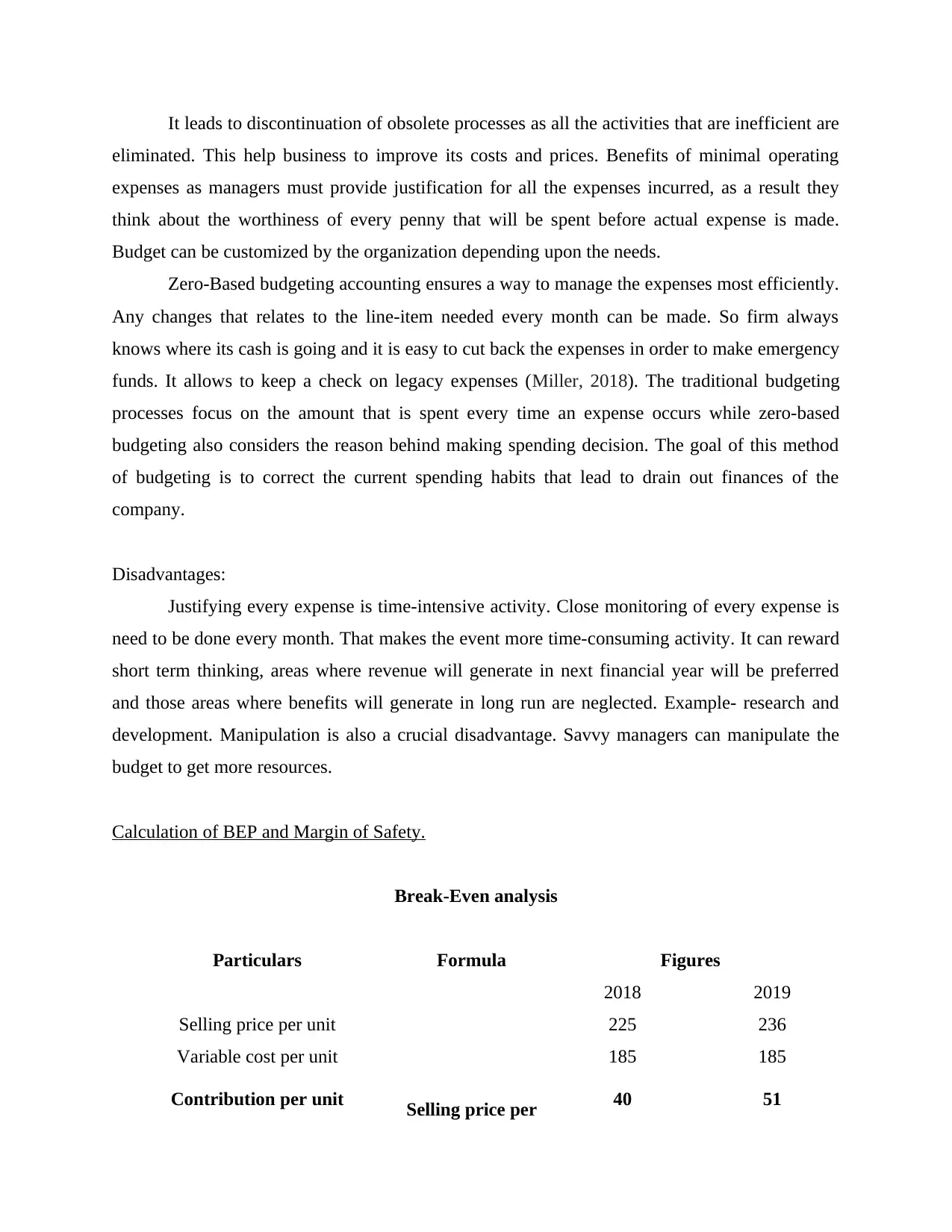
Calculation of BEP and Margin of Safety.
Break-Even analysis
Particulars Formula Figures
2018 2019
Selling price per unit 225 236
Variable cost per unit 185 185
Contribution per unit Selling price per 40 51
eliminated. This help business to improve its costs and prices. Benefits of minimal operating
expenses as managers must provide justification for all the expenses incurred, as a result they
think about the worthiness of every penny that will be spent before actual expense is made.
Budget can be customized by the organization depending upon the needs.
Zero-Based budgeting accounting ensures a way to manage the expenses most efficiently.
Any changes that relates to the line-item needed every month can be made. So firm always
knows where its cash is going and it is easy to cut back the expenses in order to make emergency
funds. It allows to keep a check on legacy expenses (Miller, 2018). The traditional budgeting
processes focus on the amount that is spent every time an expense occurs while zero-based
budgeting also considers the reason behind making spending decision. The goal of this method
of budgeting is to correct the current spending habits that lead to drain out finances of the
company.
Disadvantages:
Justifying every expense is time-intensive activity. Close monitoring of every expense is
need to be done every month. That makes the event more time-consuming activity. It can reward
short term thinking, areas where revenue will generate in next financial year will be preferred
and those areas where benefits will generate in long run are neglected. Example- research and
development. Manipulation is also a crucial disadvantage. Savvy managers can manipulate the
budget to get more resources.
Calculation of BEP and Margin of Safety.
Break-Even analysis
Particulars Formula Figures
2018 2019
Selling price per unit 225 236
Variable cost per unit 185 185
Contribution per unit Selling price per 40 51

unit - variable
cost per unit
Fixed cost 3225000 4675000
BEP (in units)
Fixed cost /
contribution per
unit 80625 91666.67
BEP (in value or monetary terms)
BEP (in units) *
selling price per
unit 18140625 21633333.33
Margin of Safety (in monetary terms)
Particulars Formula Figures
2018 2019
Sales 49500000 51920000
BEP 18140625 21633333.33
Sales Unit 220000 220000
Margin of safety (in %)
(Current Sales
Level – Break-
even Point) /
Current Sales
Level x 100 63.35 58.33
Margin of Safety (in units)
Current Sales
Units – Break-
even Point 139375 128333.33
Margin of Safety (in monetary
terms)
Current Sales –
Break-even
Sales 31359375 30286666.67
cost per unit
Fixed cost 3225000 4675000
BEP (in units)
Fixed cost /
contribution per
unit 80625 91666.67
BEP (in value or monetary terms)
BEP (in units) *
selling price per
unit 18140625 21633333.33
Margin of Safety (in monetary terms)
Particulars Formula Figures
2018 2019
Sales 49500000 51920000
BEP 18140625 21633333.33
Sales Unit 220000 220000
Margin of safety (in %)
(Current Sales
Level – Break-
even Point) /
Current Sales
Level x 100 63.35 58.33
Margin of Safety (in units)
Current Sales
Units – Break-
even Point 139375 128333.33
Margin of Safety (in monetary
terms)
Current Sales –
Break-even
Sales 31359375 30286666.67
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




