Comprehensive First Aid Report: Procedures and Emergency Treatment
VerifiedAdded on 2020/12/18
|16
|4163
|237
Report
AI Summary
This report provides a comprehensive overview of first aid, beginning with the roles and responsibilities of a first aider, including assessing casualties, providing appropriate first aid, and arranging further medical help. It emphasizes minimizing the risk of infection through the use of personal protective equipment and proper hygiene. The report highlights the importance of establishing consent before providing first aid, respecting cultural norms, and legal considerations. It lists essential first aid equipment, including gauze pads, bandages, scissors, and resuscitation equipment, and details the safe use of these items. The report also includes a table of drugs used in first aid, along with their uses, and a table outlining various medical conditions such as angina, asthma, heart attack, stroke, epilepsy, anaphylaxis, faints, and hyperventilation, including their signs, symptoms, and treatments. The report also covers CPR techniques, including how to manage CPR with one or two rescuers, and the importance of a firm base for compressions. The report also covers post-CPR care and the recovery position for unconscious, breathing casualties. Finally, it emphasizes the importance of providing paramedics with detailed information and the need for proper post-first aid procedures.
First Aid
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
INTRODUCTION...........................................................................................................................4
MAIN BODY...................................................................................................................................4
1.1 Roles and responsibilities of first aider............................................................................4
1.2 Minimise the risk of infection to self and others..............................................................4
1.3 Need for establishing consent to provide first aid............................................................5
1.4 Identify the first aid equipment that should be available.................................................5
1.5 Safe use of first aid equipment.........................................................................................5
Table 1....................................................................................................................................5
What is priority of life support?...........................................................................................11
What does D.R.A.B.C. Stand for?........................................................................................12
What is kept in your first aid box?.......................................................................................12
What should not be kept in you first aid box and why?.......................................................12
The Resuscitation Council (UK 2006) advise ABCDE assessment. What do the D & E stand
for?........................................................................................................................................12
What precautions, of possible would you take to protect yourself from the above infections?
..............................................................................................................................................12
When checking an unconscious casualty for breathing, how long would you take?...........12
What signs would you look for when checking casualty for evidence of breathing?..........13
At what stage would you send for help if other people are present?....................................13
How long should you take to assess before life supporting begins and how long before brain
damage occurs?....................................................................................................................13
Why is it important not to use the neck tilt technique when spinal neck or neck injury is
suspected?.............................................................................................................................13
Please complete the table below in CPR techniques:...........................................................13
When help has been sent for how long would you continue CPR?......................................13
INTRODUCTION...........................................................................................................................4
MAIN BODY...................................................................................................................................4
1.1 Roles and responsibilities of first aider............................................................................4
1.2 Minimise the risk of infection to self and others..............................................................4
1.3 Need for establishing consent to provide first aid............................................................5
1.4 Identify the first aid equipment that should be available.................................................5
1.5 Safe use of first aid equipment.........................................................................................5
Table 1....................................................................................................................................5
What is priority of life support?...........................................................................................11
What does D.R.A.B.C. Stand for?........................................................................................12
What is kept in your first aid box?.......................................................................................12
What should not be kept in you first aid box and why?.......................................................12
The Resuscitation Council (UK 2006) advise ABCDE assessment. What do the D & E stand
for?........................................................................................................................................12
What precautions, of possible would you take to protect yourself from the above infections?
..............................................................................................................................................12
When checking an unconscious casualty for breathing, how long would you take?...........12
What signs would you look for when checking casualty for evidence of breathing?..........13
At what stage would you send for help if other people are present?....................................13
How long should you take to assess before life supporting begins and how long before brain
damage occurs?....................................................................................................................13
Why is it important not to use the neck tilt technique when spinal neck or neck injury is
suspected?.............................................................................................................................13
Please complete the table below in CPR techniques:...........................................................13
When help has been sent for how long would you continue CPR?......................................13
How might you manage CPR if two people where available?.............................................14
Why is a firm base needed for compressions and what would you do if there wasn't one?.14
What details would you need to give to the paramedics when they arrived?.......................14
Following CPR in your surgery or after using any first aid equipment what would you need to
do?........................................................................................................................................14
What position would you place an unconscious, breathing casualty in?.............................14
Why is this position most important?...................................................................................14
State the treatment for:.........................................................................................................14
Describe the signs and symptoms of shock..........................................................................15
State the treatment for shock................................................................................................15
How would you control severe bleeding in a casualty?.......................................................15
Where is your Emergency Drug Kit stored?........................................................................15
Describe how to identify a casualty with partially blocked airway......................................15
Describe how to identify a casualty with completely blocked airway.................................15
First aid to a choking casualty..............................................................................................15
How long should you take to assess before life support begins?.........................................15
How long should you take to assess before brain damage occurs?......................................16
Post CPR on surgery or use of first aid equipments, what needs to be done?......................16
What position should you place an unconscious, breathing casualty in?.............................16
CONCLUSION..............................................................................................................................16
Why is a firm base needed for compressions and what would you do if there wasn't one?.14
What details would you need to give to the paramedics when they arrived?.......................14
Following CPR in your surgery or after using any first aid equipment what would you need to
do?........................................................................................................................................14
What position would you place an unconscious, breathing casualty in?.............................14
Why is this position most important?...................................................................................14
State the treatment for:.........................................................................................................14
Describe the signs and symptoms of shock..........................................................................15
State the treatment for shock................................................................................................15
How would you control severe bleeding in a casualty?.......................................................15
Where is your Emergency Drug Kit stored?........................................................................15
Describe how to identify a casualty with partially blocked airway......................................15
Describe how to identify a casualty with completely blocked airway.................................15
First aid to a choking casualty..............................................................................................15
How long should you take to assess before life support begins?.........................................15
How long should you take to assess before brain damage occurs?......................................16
Post CPR on surgery or use of first aid equipments, what needs to be done?......................16
What position should you place an unconscious, breathing casualty in?.............................16
CONCLUSION..............................................................................................................................16
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
INTRODUCTION
First aid refers to an emergency care or treatment given to an ill or injured person before
regular medical aid can be obtained. It include the fact that immediate first aid at correct time can
be considered much effective to reduce severe complications and even save a life of an
individual. The report will focus on roles of first aider and need of first aid including equipments.
It will also include safe use of first aid equipments and priority of life support.
MAIN BODY
1.1 Roles and responsibilities of first aider
Roles of first aider –
Placing an unconscious casualty into the recovery position
Performing cardiopulmonary resuscitation (CPR).
Using an automated external defibrillator (AED).
Stopping bleeding using pressure and elevation.
Keeping a fractured limb still.
Responsibilities –
Assess casualties and find out nature the nature & cause of victim's injuries.
Arrange the further medical help.
Provide appropriate first aid treated as trained.
1.2 Minimise the risk of infection to self and others
Methods to minimise risk of infection –
Always cover all open skin areas to avoid infection.
Wear desired personal protective equipments (PPE) such as gloves, mask, CPR barrier
mask and goggles.
Try to put barrier between you and another person's body fluids.
Minimise the splashing of body fluids (blood, urine, sputum and secretions).
Wash hand and other exposed area immediately with soap after providing care.
Handle sharp objects with caution.
Dispose contaminated PPE in appropriate place.
First aid refers to an emergency care or treatment given to an ill or injured person before
regular medical aid can be obtained. It include the fact that immediate first aid at correct time can
be considered much effective to reduce severe complications and even save a life of an
individual. The report will focus on roles of first aider and need of first aid including equipments.
It will also include safe use of first aid equipments and priority of life support.
MAIN BODY
1.1 Roles and responsibilities of first aider
Roles of first aider –
Placing an unconscious casualty into the recovery position
Performing cardiopulmonary resuscitation (CPR).
Using an automated external defibrillator (AED).
Stopping bleeding using pressure and elevation.
Keeping a fractured limb still.
Responsibilities –
Assess casualties and find out nature the nature & cause of victim's injuries.
Arrange the further medical help.
Provide appropriate first aid treated as trained.
1.2 Minimise the risk of infection to self and others
Methods to minimise risk of infection –
Always cover all open skin areas to avoid infection.
Wear desired personal protective equipments (PPE) such as gloves, mask, CPR barrier
mask and goggles.
Try to put barrier between you and another person's body fluids.
Minimise the splashing of body fluids (blood, urine, sputum and secretions).
Wash hand and other exposed area immediately with soap after providing care.
Handle sharp objects with caution.
Dispose contaminated PPE in appropriate place.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
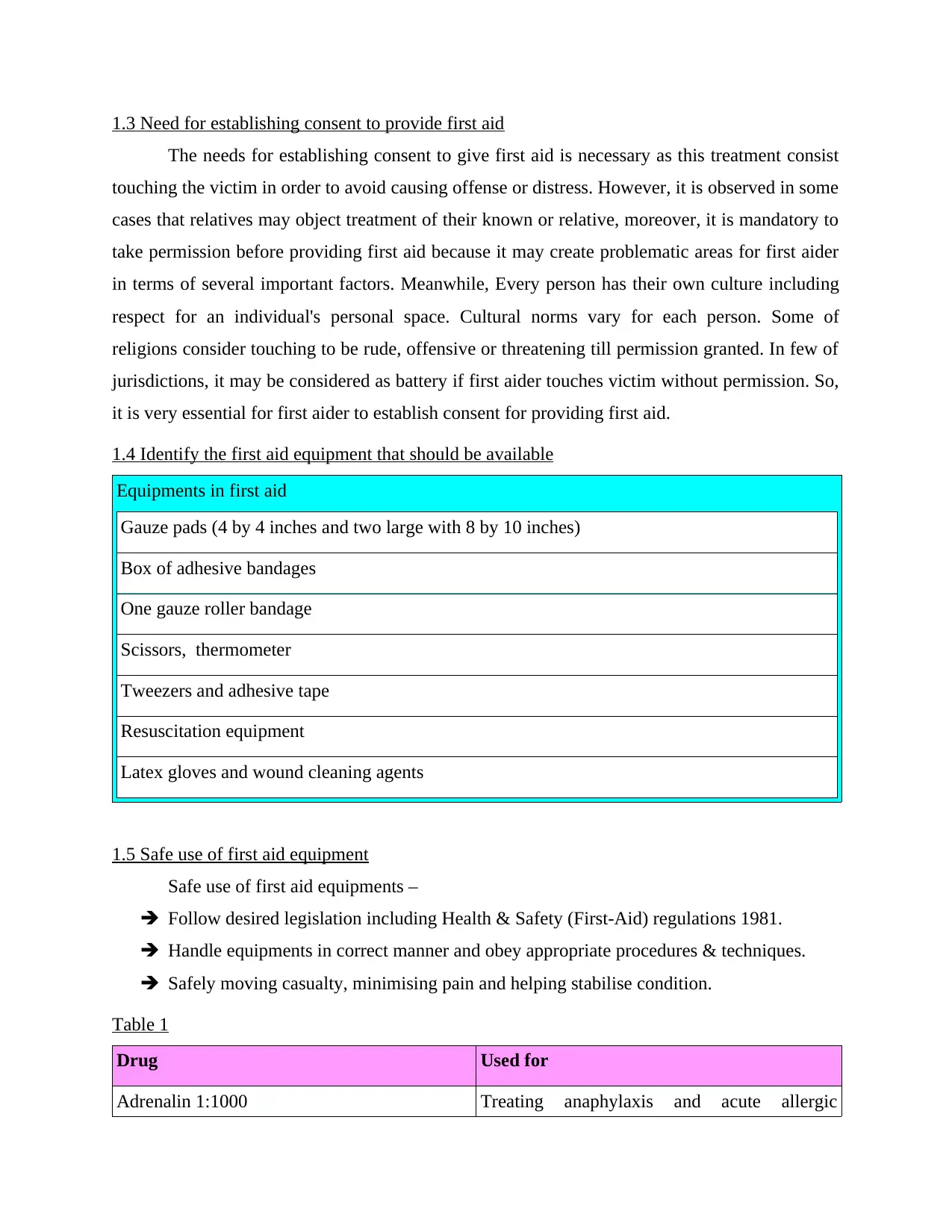
1.3 Need for establishing consent to provide first aid
The needs for establishing consent to give first aid is necessary as this treatment consist
touching the victim in order to avoid causing offense or distress. However, it is observed in some
cases that relatives may object treatment of their known or relative, moreover, it is mandatory to
take permission before providing first aid because it may create problematic areas for first aider
in terms of several important factors. Meanwhile, Every person has their own culture including
respect for an individual's personal space. Cultural norms vary for each person. Some of
religions consider touching to be rude, offensive or threatening till permission granted. In few of
jurisdictions, it may be considered as battery if first aider touches victim without permission. So,
it is very essential for first aider to establish consent for providing first aid.
1.4 Identify the first aid equipment that should be available
Equipments in first aid
Gauze pads (4 by 4 inches and two large with 8 by 10 inches)
Box of adhesive bandages
One gauze roller bandage
Scissors, thermometer
Tweezers and adhesive tape
Resuscitation equipment
Latex gloves and wound cleaning agents
1.5 Safe use of first aid equipment
Safe use of first aid equipments –
Follow desired legislation including Health & Safety (First-Aid) regulations 1981.
Handle equipments in correct manner and obey appropriate procedures & techniques.
Safely moving casualty, minimising pain and helping stabilise condition.
Table 1
Drug Used for
Adrenalin 1:1000 Treating anaphylaxis and acute allergic
The needs for establishing consent to give first aid is necessary as this treatment consist
touching the victim in order to avoid causing offense or distress. However, it is observed in some
cases that relatives may object treatment of their known or relative, moreover, it is mandatory to
take permission before providing first aid because it may create problematic areas for first aider
in terms of several important factors. Meanwhile, Every person has their own culture including
respect for an individual's personal space. Cultural norms vary for each person. Some of
religions consider touching to be rude, offensive or threatening till permission granted. In few of
jurisdictions, it may be considered as battery if first aider touches victim without permission. So,
it is very essential for first aider to establish consent for providing first aid.
1.4 Identify the first aid equipment that should be available
Equipments in first aid
Gauze pads (4 by 4 inches and two large with 8 by 10 inches)
Box of adhesive bandages
One gauze roller bandage
Scissors, thermometer
Tweezers and adhesive tape
Resuscitation equipment
Latex gloves and wound cleaning agents
1.5 Safe use of first aid equipment
Safe use of first aid equipments –
Follow desired legislation including Health & Safety (First-Aid) regulations 1981.
Handle equipments in correct manner and obey appropriate procedures & techniques.
Safely moving casualty, minimising pain and helping stabilise condition.
Table 1
Drug Used for
Adrenalin 1:1000 Treating anaphylaxis and acute allergic
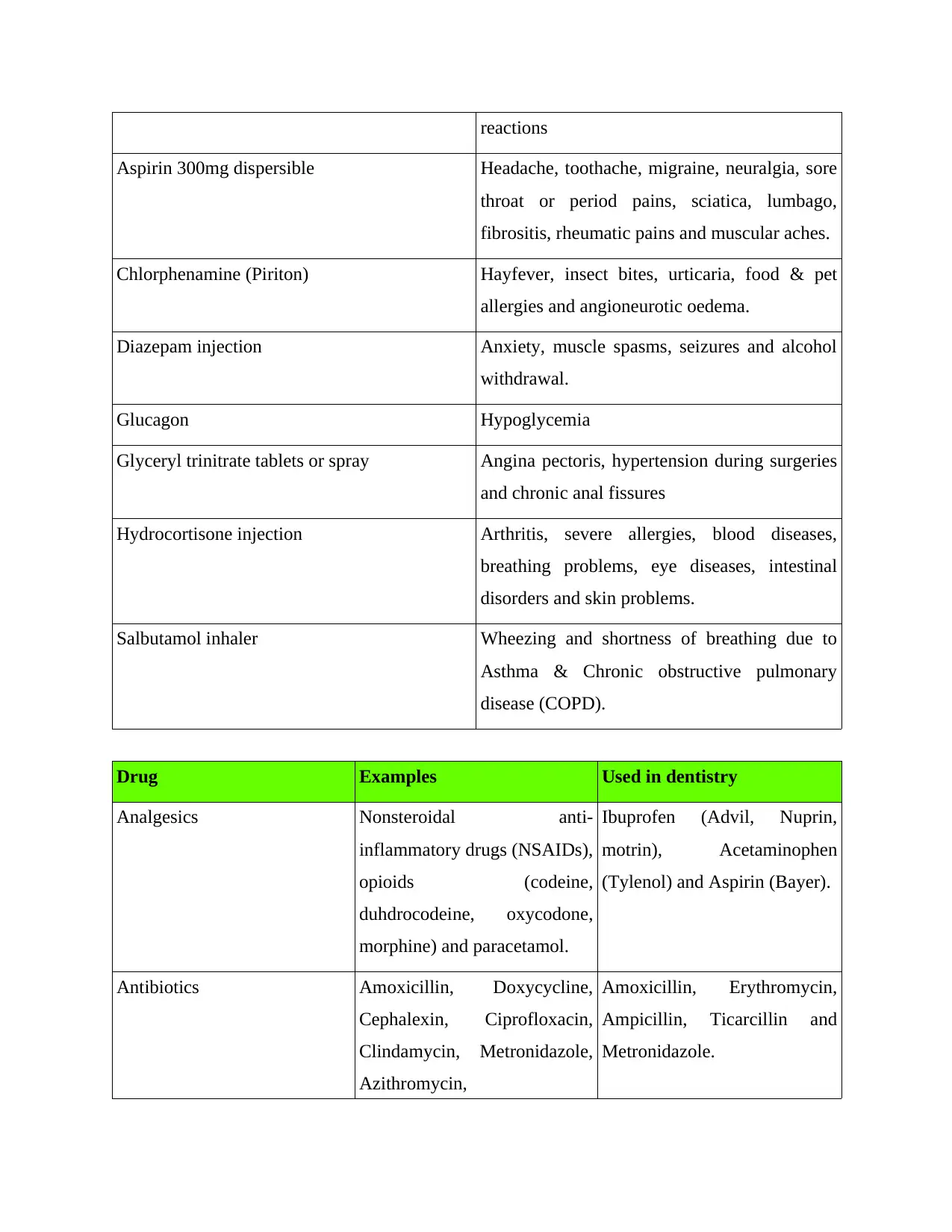
reactions
Aspirin 300mg dispersible Headache, toothache, migraine, neuralgia, sore
throat or period pains, sciatica, lumbago,
fibrositis, rheumatic pains and muscular aches.
Chlorphenamine (Piriton) Hayfever, insect bites, urticaria, food & pet
allergies and angioneurotic oedema.
Diazepam injection Anxiety, muscle spasms, seizures and alcohol
withdrawal.
Glucagon Hypoglycemia
Glyceryl trinitrate tablets or spray Angina pectoris, hypertension during surgeries
and chronic anal fissures
Hydrocortisone injection Arthritis, severe allergies, blood diseases,
breathing problems, eye diseases, intestinal
disorders and skin problems.
Salbutamol inhaler Wheezing and shortness of breathing due to
Asthma & Chronic obstructive pulmonary
disease (COPD).
Drug Examples Used in dentistry
Analgesics Nonsteroidal anti-
inflammatory drugs (NSAIDs),
opioids (codeine,
duhdrocodeine, oxycodone,
morphine) and paracetamol.
Ibuprofen (Advil, Nuprin,
motrin), Acetaminophen
(Tylenol) and Aspirin (Bayer).
Antibiotics Amoxicillin, Doxycycline,
Cephalexin, Ciprofloxacin,
Clindamycin, Metronidazole,
Azithromycin,
Amoxicillin, Erythromycin,
Ampicillin, Ticarcillin and
Metronidazole.
Aspirin 300mg dispersible Headache, toothache, migraine, neuralgia, sore
throat or period pains, sciatica, lumbago,
fibrositis, rheumatic pains and muscular aches.
Chlorphenamine (Piriton) Hayfever, insect bites, urticaria, food & pet
allergies and angioneurotic oedema.
Diazepam injection Anxiety, muscle spasms, seizures and alcohol
withdrawal.
Glucagon Hypoglycemia
Glyceryl trinitrate tablets or spray Angina pectoris, hypertension during surgeries
and chronic anal fissures
Hydrocortisone injection Arthritis, severe allergies, blood diseases,
breathing problems, eye diseases, intestinal
disorders and skin problems.
Salbutamol inhaler Wheezing and shortness of breathing due to
Asthma & Chronic obstructive pulmonary
disease (COPD).
Drug Examples Used in dentistry
Analgesics Nonsteroidal anti-
inflammatory drugs (NSAIDs),
opioids (codeine,
duhdrocodeine, oxycodone,
morphine) and paracetamol.
Ibuprofen (Advil, Nuprin,
motrin), Acetaminophen
(Tylenol) and Aspirin (Bayer).
Antibiotics Amoxicillin, Doxycycline,
Cephalexin, Ciprofloxacin,
Clindamycin, Metronidazole,
Azithromycin,
Amoxicillin, Erythromycin,
Ampicillin, Ticarcillin and
Metronidazole.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Sulfamethoxazole and
Levofloxacin.
Tranquillisers Hypnotics Diazepam, chlordiazepoxide,
phenothiazines, thioxanthines,
clozapine and rauwolfia
alkaloids.
Lorazepam, Diazepam,
Hydroxyzine, Zaleplon,
Triazolam and Nitrous oxide.
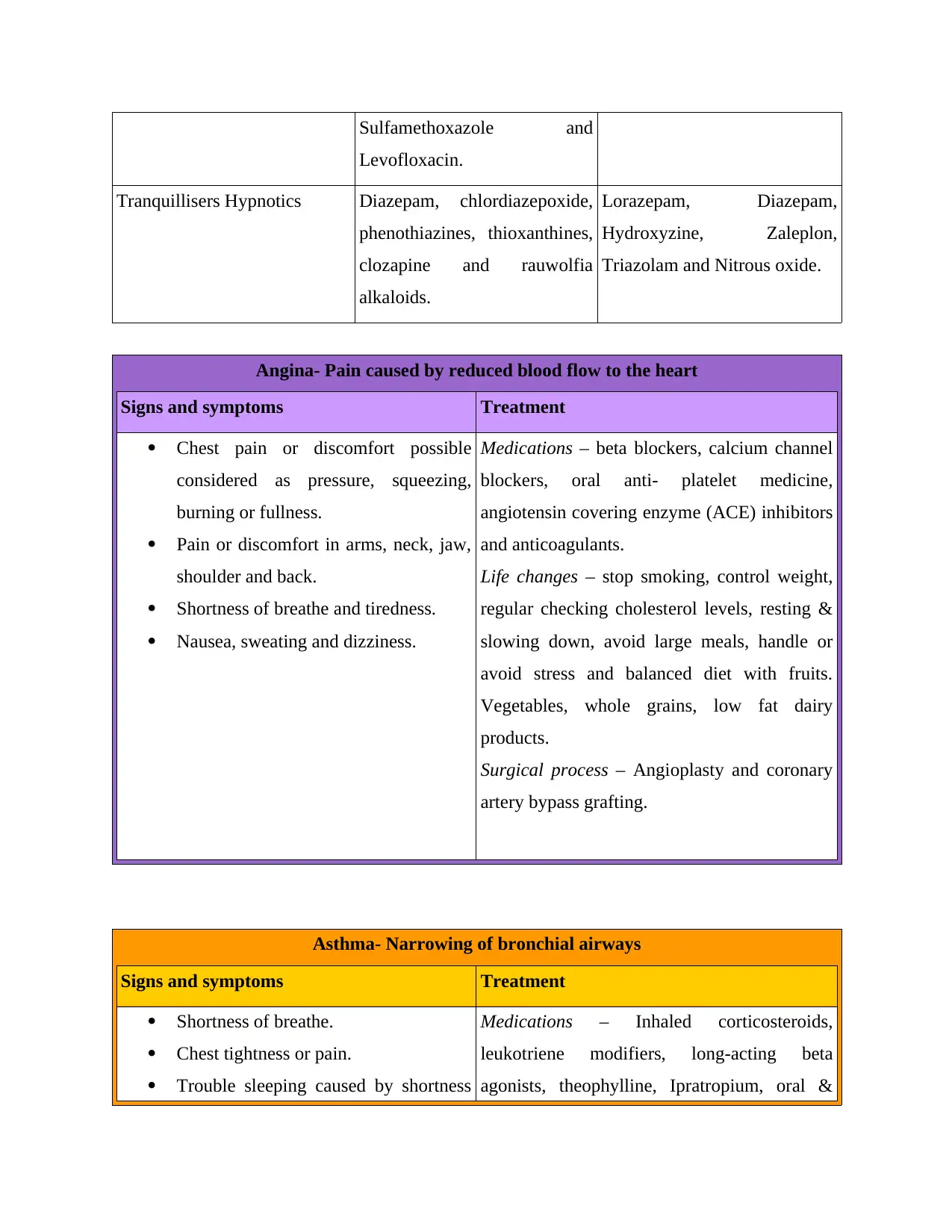
Angina- Pain caused by reduced blood flow to the heart
Signs and symptoms Treatment
Chest pain or discomfort possible
considered as pressure, squeezing,
burning or fullness.
Pain or discomfort in arms, neck, jaw,
shoulder and back.
Shortness of breathe and tiredness.
Nausea, sweating and dizziness.
Medications – beta blockers, calcium channel
blockers, oral anti- platelet medicine,
angiotensin covering enzyme (ACE) inhibitors
and anticoagulants.
Life changes – stop smoking, control weight,
regular checking cholesterol levels, resting &
slowing down, avoid large meals, handle or
avoid stress and balanced diet with fruits.
Vegetables, whole grains, low fat dairy
products.
Surgical process – Angioplasty and coronary
artery bypass grafting.
Asthma- Narrowing of bronchial airways
Signs and symptoms Treatment
Shortness of breathe.
Chest tightness or pain.
Trouble sleeping caused by shortness
Medications – Inhaled corticosteroids,
leukotriene modifiers, long-acting beta
agonists, theophylline, Ipratropium, oral &
Levofloxacin.
Tranquillisers Hypnotics Diazepam, chlordiazepoxide,
phenothiazines, thioxanthines,
clozapine and rauwolfia
alkaloids.
Lorazepam, Diazepam,
Hydroxyzine, Zaleplon,
Triazolam and Nitrous oxide.
Angina- Pain caused by reduced blood flow to the heart
Signs and symptoms Treatment
Chest pain or discomfort possible
considered as pressure, squeezing,
burning or fullness.
Pain or discomfort in arms, neck, jaw,
shoulder and back.
Shortness of breathe and tiredness.
Nausea, sweating and dizziness.
Medications – beta blockers, calcium channel
blockers, oral anti- platelet medicine,
angiotensin covering enzyme (ACE) inhibitors
and anticoagulants.
Life changes – stop smoking, control weight,
regular checking cholesterol levels, resting &
slowing down, avoid large meals, handle or
avoid stress and balanced diet with fruits.
Vegetables, whole grains, low fat dairy
products.
Surgical process – Angioplasty and coronary
artery bypass grafting.
Asthma- Narrowing of bronchial airways
Signs and symptoms Treatment
Shortness of breathe.
Chest tightness or pain.
Trouble sleeping caused by shortness
Medications – Inhaled corticosteroids,
leukotriene modifiers, long-acting beta
agonists, theophylline, Ipratropium, oral &
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
of breathe, coughing or wheezing.
A whistling or wheezing sign while
exhaling.
Coughing or wheezing attacks.
Signs of cold or allergies.
Decrease or changes in lung function.
Feeling tired, easily upset, grouchy or
moody.
intravenous corticosteriods.
Allergy medications – Immunotherapy and
Omalizumab.
Oxygen therapy.
Bronchial thermoplasty.
Breathing exercises.
Rescue or first aid treatment like inhalers and
nebulizers.
Asthma action plan.
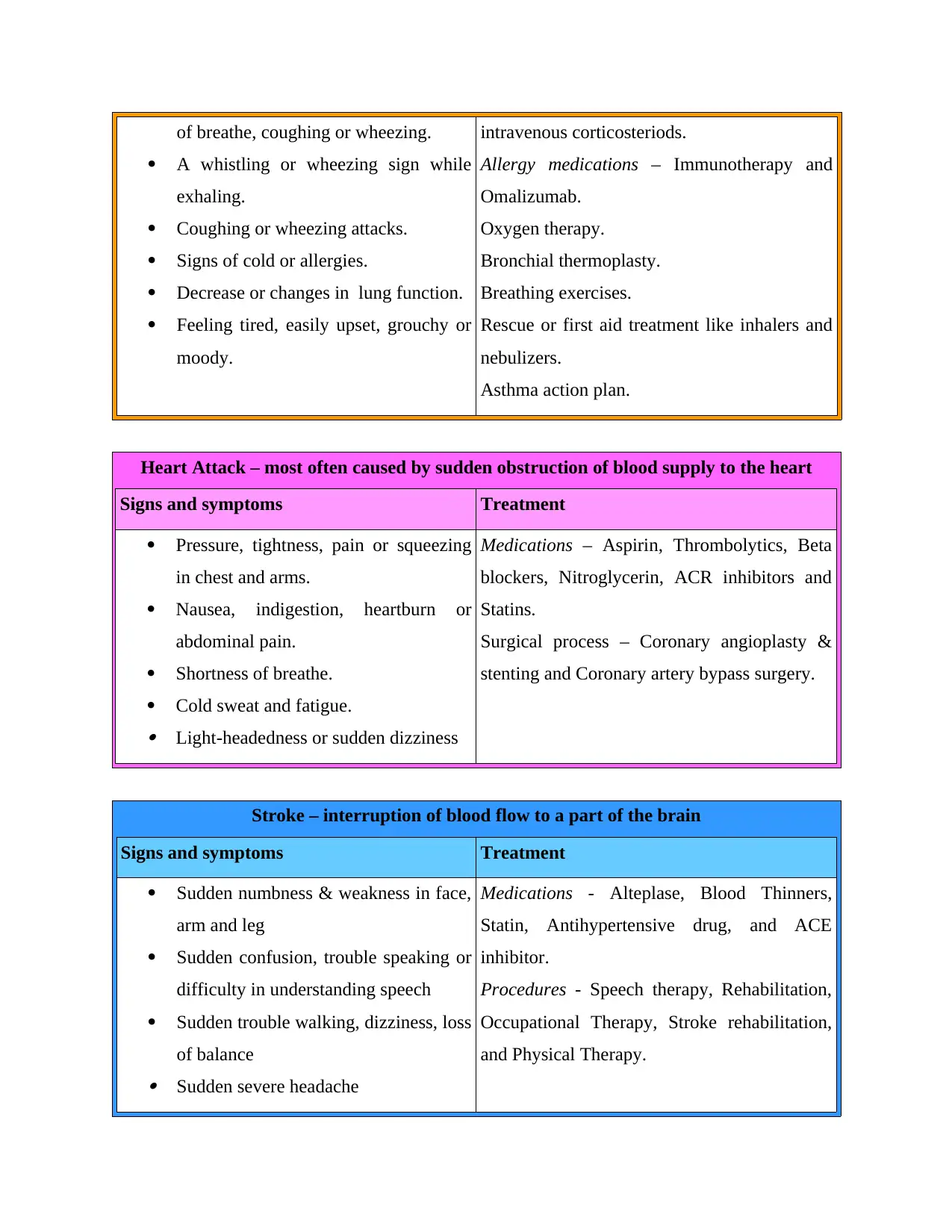
Heart Attack – most often caused by sudden obstruction of blood supply to the heart
Signs and symptoms Treatment
Pressure, tightness, pain or squeezing
in chest and arms.
Nausea, indigestion, heartburn or
abdominal pain.
Shortness of breathe.
Cold sweat and fatigue. Light-headedness or sudden dizziness
Medications – Aspirin, Thrombolytics, Beta
blockers, Nitroglycerin, ACR inhibitors and
Statins.
Surgical process – Coronary angioplasty &
stenting and Coronary artery bypass surgery.
Stroke – interruption of blood flow to a part of the brain
Signs and symptoms Treatment
Sudden numbness & weakness in face,
arm and leg
Sudden confusion, trouble speaking or
difficulty in understanding speech
Sudden trouble walking, dizziness, loss
of balance Sudden severe headache
Medications - Alteplase, Blood Thinners,
Statin, Antihypertensive drug, and ACE
inhibitor.
Procedures - Speech therapy, Rehabilitation,
Occupational Therapy, Stroke rehabilitation,
and Physical Therapy.
A whistling or wheezing sign while
exhaling.
Coughing or wheezing attacks.
Signs of cold or allergies.
Decrease or changes in lung function.
Feeling tired, easily upset, grouchy or
moody.
intravenous corticosteriods.
Allergy medications – Immunotherapy and
Omalizumab.
Oxygen therapy.
Bronchial thermoplasty.
Breathing exercises.
Rescue or first aid treatment like inhalers and
nebulizers.
Asthma action plan.
Heart Attack – most often caused by sudden obstruction of blood supply to the heart
Signs and symptoms Treatment
Pressure, tightness, pain or squeezing
in chest and arms.
Nausea, indigestion, heartburn or
abdominal pain.
Shortness of breathe.
Cold sweat and fatigue. Light-headedness or sudden dizziness
Medications – Aspirin, Thrombolytics, Beta
blockers, Nitroglycerin, ACR inhibitors and
Statins.
Surgical process – Coronary angioplasty &
stenting and Coronary artery bypass surgery.
Stroke – interruption of blood flow to a part of the brain
Signs and symptoms Treatment
Sudden numbness & weakness in face,
arm and leg
Sudden confusion, trouble speaking or
difficulty in understanding speech
Sudden trouble walking, dizziness, loss
of balance Sudden severe headache
Medications - Alteplase, Blood Thinners,
Statin, Antihypertensive drug, and ACE
inhibitor.
Procedures - Speech therapy, Rehabilitation,
Occupational Therapy, Stroke rehabilitation,
and Physical Therapy.
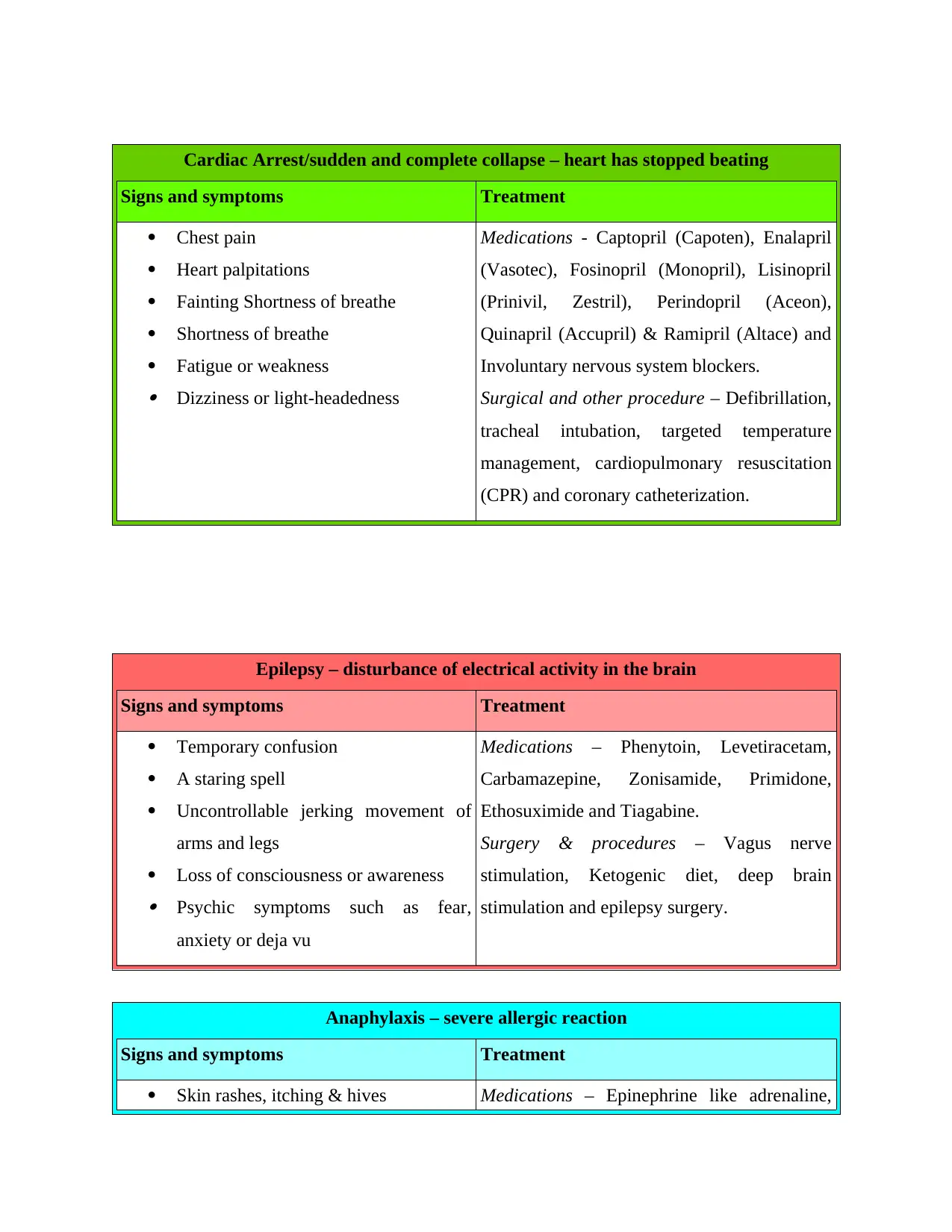
Cardiac Arrest/sudden and complete collapse – heart has stopped beating
Signs and symptoms Treatment
Chest pain
Heart palpitations
Fainting Shortness of breathe
Shortness of breathe
Fatigue or weakness Dizziness or light-headedness
Medications - Captopril (Capoten), Enalapril
(Vasotec), Fosinopril (Monopril), Lisinopril
(Prinivil, Zestril), Perindopril (Aceon),
Quinapril (Accupril) & Ramipril (Altace) and
Involuntary nervous system blockers.
Surgical and other procedure – Defibrillation,
tracheal intubation, targeted temperature
management, cardiopulmonary resuscitation
(CPR) and coronary catheterization.
Epilepsy – disturbance of electrical activity in the brain
Signs and symptoms Treatment
Temporary confusion
A staring spell
Uncontrollable jerking movement of
arms and legs
Loss of consciousness or awareness Psychic symptoms such as fear,
anxiety or deja vu
Medications – Phenytoin, Levetiracetam,
Carbamazepine, Zonisamide, Primidone,
Ethosuximide and Tiagabine.
Surgery & procedures – Vagus nerve
stimulation, Ketogenic diet, deep brain
stimulation and epilepsy surgery.
Anaphylaxis – severe allergic reaction
Signs and symptoms Treatment
Skin rashes, itching & hives Medications – Epinephrine like adrenaline,
Signs and symptoms Treatment
Chest pain
Heart palpitations
Fainting Shortness of breathe
Shortness of breathe
Fatigue or weakness Dizziness or light-headedness
Medications - Captopril (Capoten), Enalapril
(Vasotec), Fosinopril (Monopril), Lisinopril
(Prinivil, Zestril), Perindopril (Aceon),
Quinapril (Accupril) & Ramipril (Altace) and
Involuntary nervous system blockers.
Surgical and other procedure – Defibrillation,
tracheal intubation, targeted temperature
management, cardiopulmonary resuscitation
(CPR) and coronary catheterization.
Epilepsy – disturbance of electrical activity in the brain
Signs and symptoms Treatment
Temporary confusion
A staring spell
Uncontrollable jerking movement of
arms and legs
Loss of consciousness or awareness Psychic symptoms such as fear,
anxiety or deja vu
Medications – Phenytoin, Levetiracetam,
Carbamazepine, Zonisamide, Primidone,
Ethosuximide and Tiagabine.
Surgery & procedures – Vagus nerve
stimulation, Ketogenic diet, deep brain
stimulation and epilepsy surgery.
Anaphylaxis – severe allergic reaction
Signs and symptoms Treatment
Skin rashes, itching & hives Medications – Epinephrine like adrenaline,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Swelling of lips, tongue & throat
shortness of breathe, trouble in
breathing, wheezing
dizziness or fainting stomach pain, vomiting or diarrhoea
Intravenous (IV) antihistamines and cortisone
and A beta-agonist as albuterol.
Process - Oxygen therapy to facilitate
comfortable breathe.
Faints – loss of consciousness caused by temporary insufficient blood supply to brain
Signs and symptoms Treatment
Weakness and sweating
Blurred vision, seeing spots
Sensation that room is moving
Ringing of ears
Tingling or numbness of finger tips Bluish cast to the skin
Medications – Beta blockers and selective
serotonin inhibitors
Procedures – lifestyle alterations to intake
more water & salt by avoiding prolonged
standing. Angioplasty for cardiac syncope and
pacemaker implantation.
Hyperventilation or panic attack – rapid breathing
Signs and symptoms Treatment
Feeling light-headedness, dizzy, weak
Feeling of not catching breathe
Chest pain or fast & pounding
heartbeat
Belching and bloating
Dry mouth
Muscle spasms
Numbness and tingling Problem in sleeping
Medications – Selective serotonin reuptake
inhibitors (SSRIs) like fluoxetine (Prozac),
paroxetine (Paxil, Pexeva); Serotonin and
norepinephrine reuptake inhibitors (SNRIs)
and Benzodiazepines including alprazolam
(Xanax) and clonazepam (Klonopin).
Processes – Purse the lips, limit the airflow
and psychotherapy.
Hypoglycemia – abnormally low blood sugar level
shortness of breathe, trouble in
breathing, wheezing
dizziness or fainting stomach pain, vomiting or diarrhoea
Intravenous (IV) antihistamines and cortisone
and A beta-agonist as albuterol.
Process - Oxygen therapy to facilitate
comfortable breathe.
Faints – loss of consciousness caused by temporary insufficient blood supply to brain
Signs and symptoms Treatment
Weakness and sweating
Blurred vision, seeing spots
Sensation that room is moving
Ringing of ears
Tingling or numbness of finger tips Bluish cast to the skin
Medications – Beta blockers and selective
serotonin inhibitors
Procedures – lifestyle alterations to intake
more water & salt by avoiding prolonged
standing. Angioplasty for cardiac syncope and
pacemaker implantation.
Hyperventilation or panic attack – rapid breathing
Signs and symptoms Treatment
Feeling light-headedness, dizzy, weak
Feeling of not catching breathe
Chest pain or fast & pounding
heartbeat
Belching and bloating
Dry mouth
Muscle spasms
Numbness and tingling Problem in sleeping
Medications – Selective serotonin reuptake
inhibitors (SSRIs) like fluoxetine (Prozac),
paroxetine (Paxil, Pexeva); Serotonin and
norepinephrine reuptake inhibitors (SNRIs)
and Benzodiazepines including alprazolam
(Xanax) and clonazepam (Klonopin).
Processes – Purse the lips, limit the airflow
and psychotherapy.
Hypoglycemia – abnormally low blood sugar level
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
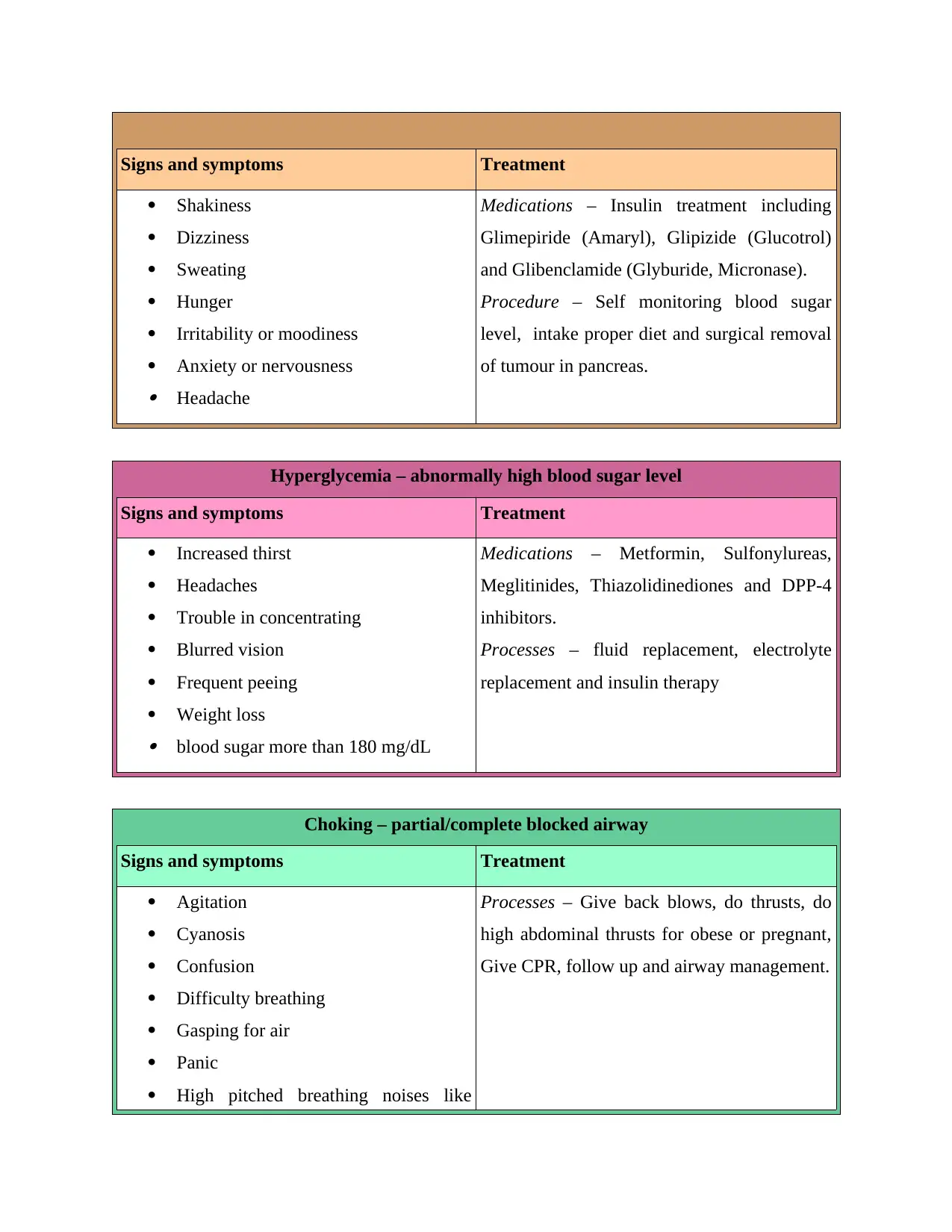
Signs and symptoms Treatment
Shakiness
Dizziness
Sweating
Hunger
Irritability or moodiness
Anxiety or nervousness Headache
Medications – Insulin treatment including
Glimepiride (Amaryl), Glipizide (Glucotrol)
and Glibenclamide (Glyburide, Micronase).
Procedure – Self monitoring blood sugar
level, intake proper diet and surgical removal
of tumour in pancreas.
Hyperglycemia – abnormally high blood sugar level
Signs and symptoms Treatment
Increased thirst
Headaches
Trouble in concentrating
Blurred vision
Frequent peeing
Weight loss blood sugar more than 180 mg/dL
Medications – Metformin, Sulfonylureas,
Meglitinides, Thiazolidinediones and DPP-4
inhibitors.
Processes – fluid replacement, electrolyte
replacement and insulin therapy
Choking – partial/complete blocked airway
Signs and symptoms Treatment
Agitation
Cyanosis
Confusion
Difficulty breathing
Gasping for air
Panic
High pitched breathing noises like
Processes – Give back blows, do thrusts, do
high abdominal thrusts for obese or pregnant,
Give CPR, follow up and airway management.
Shakiness
Dizziness
Sweating
Hunger
Irritability or moodiness
Anxiety or nervousness Headache
Medications – Insulin treatment including
Glimepiride (Amaryl), Glipizide (Glucotrol)
and Glibenclamide (Glyburide, Micronase).
Procedure – Self monitoring blood sugar
level, intake proper diet and surgical removal
of tumour in pancreas.
Hyperglycemia – abnormally high blood sugar level
Signs and symptoms Treatment
Increased thirst
Headaches
Trouble in concentrating
Blurred vision
Frequent peeing
Weight loss blood sugar more than 180 mg/dL
Medications – Metformin, Sulfonylureas,
Meglitinides, Thiazolidinediones and DPP-4
inhibitors.
Processes – fluid replacement, electrolyte
replacement and insulin therapy
Choking – partial/complete blocked airway
Signs and symptoms Treatment
Agitation
Cyanosis
Confusion
Difficulty breathing
Gasping for air
Panic
High pitched breathing noises like
Processes – Give back blows, do thrusts, do
high abdominal thrusts for obese or pregnant,
Give CPR, follow up and airway management.
wheezing Unconsciousness
What is priority of life support?
The basic priority of life support consist initial assessment, airway maintenance and
cardiopulmonary resuscitation (CPR). Apart from this, some of advance life support include
tracheal intubation, rapid sequence induction, cardiac monitoring, cardiac defibrillation,
transcutaneous pacing and many more. When the casualty is unconscious, first aider needs to
provide basic life support.
What does D.R.A.B.C. Stand for?
D – Danger
R – Response
A – Airway
B – Breathing
C – Circulation
What is kept in your first aid box?
A first aid box should contain small, medium and large sized sterile gauze dressings, eye
dressings, triangular bandages, crepe rolled bandages, safety pins and tweezers. Moreover. It
consist of scissors, alcohol free cleansing wipes, sticky tape, thermometer, gloves, antiseptic
cream, painkillers (paracetamol) and antihistamine cream (Gamelli and et. al., 2015).
What should not be kept in you first aid box and why?
Expired medicines should not kept in first aid box because if carer have mistaken to
evaluate their expiry date and provide to victim then it may create severe condition for them.
Meanwhile, critical specified device should be avoided as it is not helpful in emergency
situations and may generate severe situation.
The Resuscitation Council (UK 2006) advise ABCDE assessment. What do the D & E stand for?
D - Disability
E - Exposure
What is priority of life support?
The basic priority of life support consist initial assessment, airway maintenance and
cardiopulmonary resuscitation (CPR). Apart from this, some of advance life support include
tracheal intubation, rapid sequence induction, cardiac monitoring, cardiac defibrillation,
transcutaneous pacing and many more. When the casualty is unconscious, first aider needs to
provide basic life support.
What does D.R.A.B.C. Stand for?
D – Danger
R – Response
A – Airway
B – Breathing
C – Circulation
What is kept in your first aid box?
A first aid box should contain small, medium and large sized sterile gauze dressings, eye
dressings, triangular bandages, crepe rolled bandages, safety pins and tweezers. Moreover. It
consist of scissors, alcohol free cleansing wipes, sticky tape, thermometer, gloves, antiseptic
cream, painkillers (paracetamol) and antihistamine cream (Gamelli and et. al., 2015).
What should not be kept in you first aid box and why?
Expired medicines should not kept in first aid box because if carer have mistaken to
evaluate their expiry date and provide to victim then it may create severe condition for them.
Meanwhile, critical specified device should be avoided as it is not helpful in emergency
situations and may generate severe situation.
The Resuscitation Council (UK 2006) advise ABCDE assessment. What do the D & E stand for?
D - Disability
E - Exposure
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




