Medical Ward Case Study: Gastroenteritis and Dehydration Nursing
VerifiedAdded on 2023/06/03
|13
|3157
|483
Case Study
AI Summary
This case study examines the nursing care provided to an 86-year-old male, Mr. Keith Manor, admitted to the medical ward with gastroenteritis and dehydration. The study explores how gastroenteritis affects activities of living such as eating and drinking, personal cleansing and dressing, and elimination. It details the assessment methods used to identify dehydration and malnutrition, including monitoring vital signs, fluid input/output, and skin turgor. The care plan includes interventions like encouraging fluid intake, administering intravenous fluids, providing a BRAT diet, and administering medications such as bismuth salicylate and loperamide. The study also addresses personal hygiene challenges due to vomiting, diarrhea, and lethargy, emphasizing the importance of frequent cleansing and environmental control to prevent infection spread. Finally, the case study discusses how diarrhea and vomiting affect elimination, detailing assessment and care strategies to manage fluid and electrolyte imbalances and maintain kidney function.

Nursing
Student’s name:
Institutional:
Student’s name:
Institutional:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction
GASTROENTERITIS AND DEHYDRATION
Gastroenteritis is an infection that targets the lower part of the digestive system (Payne et.al,
2013). It keeps the intestines from absorbing food and water properly. It results from poorly
sanitized source and spread to the host after eating an apparently unsafe food. This infection in
adults is caused by Norovirus (Payne et.al, 2013) which is characterized by its habitat, that is,
fecal contaminated water and food. It spread by contact and therefore, it can easily be transmitted
from one person to another. Once the virus is contracted, it targets the small intestines. When
particle is at the small intestines, it behaves like a normal virus and latches itself into a cell
nearby immediately. From there, the virus goes through cell wall and insert itself into the cells
enzyme, in essence hijacking them. The virus then put in the genetic information that it contains
into the enzyme making it to produce another virulent particle (Koo, Ajami, Atmar, & DuPont,
2010). Vomiting, diarrhea and stomach pains take over the intestinal cells. Due to vomiting and
diarrhea, the amount of fluid that is lost become more than the one taken in. This leads to
dehydration which is a life threatening condition to the patient. (Blinderman, & Billings, 2015).
Older people are at high risk of getting dehydrated. The reduction in total body water leads to
decrease in both extracellular and intracellular fluid volume as dehydration ensues. Hypovolemic
shock ultimately develops causing organ failure and finally death (Chaithongdi, Subauste, Koch,
& Geraci, 2011). Neurologic complications may develop in hyponatremic and hypernatremia
states. Symptoms include low urine output, dry or sticky mouth eating and drinking
ACTIVITIES OF LIFE AFFECTED
Eating and drinking
How it has been altered for Manor
GASTROENTERITIS AND DEHYDRATION
Gastroenteritis is an infection that targets the lower part of the digestive system (Payne et.al,
2013). It keeps the intestines from absorbing food and water properly. It results from poorly
sanitized source and spread to the host after eating an apparently unsafe food. This infection in
adults is caused by Norovirus (Payne et.al, 2013) which is characterized by its habitat, that is,
fecal contaminated water and food. It spread by contact and therefore, it can easily be transmitted
from one person to another. Once the virus is contracted, it targets the small intestines. When
particle is at the small intestines, it behaves like a normal virus and latches itself into a cell
nearby immediately. From there, the virus goes through cell wall and insert itself into the cells
enzyme, in essence hijacking them. The virus then put in the genetic information that it contains
into the enzyme making it to produce another virulent particle (Koo, Ajami, Atmar, & DuPont,
2010). Vomiting, diarrhea and stomach pains take over the intestinal cells. Due to vomiting and
diarrhea, the amount of fluid that is lost become more than the one taken in. This leads to
dehydration which is a life threatening condition to the patient. (Blinderman, & Billings, 2015).
Older people are at high risk of getting dehydrated. The reduction in total body water leads to
decrease in both extracellular and intracellular fluid volume as dehydration ensues. Hypovolemic
shock ultimately develops causing organ failure and finally death (Chaithongdi, Subauste, Koch,
& Geraci, 2011). Neurologic complications may develop in hyponatremic and hypernatremia
states. Symptoms include low urine output, dry or sticky mouth eating and drinking
ACTIVITIES OF LIFE AFFECTED
Eating and drinking
How it has been altered for Manor
Gastroenteritis causes vomiting, diarrhea and abdominal cramping (Humphries, & Linscott,
2015). Vomiting come as a result of rapid release of serotonin by the virus. When copious
amount of serotonin rush into bloodstream, the body tries to eliminate serotonin through
vomiting which lead to loss of more water and electrolytes in the body leading to fluid and
electrolyte disequilibrium. Abdominal cramping is as a result of the body immune system.
Immune system makes white blood cells to attack the virus and in turn the body undergoes
inflammation which is an attempt by the body to destroy the virus by filling the part infected area
blood. Flooding the blood around the virus makes the infected cells washed away through the
bloodstream and eliminated from the body. The lower abdomen becomes very sensitive to touch
and this cuases cramps and pain causing discomfort and nausea this reduces the amount of food
intake by the patient leading to malnutrition (Surena, 2010). Diarrhea causes loss of water
electrolytes and nutrients in the body (Field, 2016). It come as result of small intestines unable to
absorb water and essential nutrients from the food, they do not take in much water from the food
that is passing, so the passing food is almost fully liquid and excreted as watery stool. Vomiting
and diarrhea affects drinking in that the patient will need more of fluids and become thirsty
frequently, while abdominal cramping affects eating because the patient will not have the desire
to eat food.
How to assess
This can be assessed by checking the signs of both dehydration and malnutrition. For
dehydration, the clinical signs that are assessed include weight loss, thirst, dry mucous
membrane, sunken-appearing eyes and decreased skin turgor. Monitoring the vital signs four
hourly to check signs of hypotension, monitoring his fluid input and output each shift and
balancing daily. Ask patient if he is frequently feeling headaches.
2015). Vomiting come as a result of rapid release of serotonin by the virus. When copious
amount of serotonin rush into bloodstream, the body tries to eliminate serotonin through
vomiting which lead to loss of more water and electrolytes in the body leading to fluid and
electrolyte disequilibrium. Abdominal cramping is as a result of the body immune system.
Immune system makes white blood cells to attack the virus and in turn the body undergoes
inflammation which is an attempt by the body to destroy the virus by filling the part infected area
blood. Flooding the blood around the virus makes the infected cells washed away through the
bloodstream and eliminated from the body. The lower abdomen becomes very sensitive to touch
and this cuases cramps and pain causing discomfort and nausea this reduces the amount of food
intake by the patient leading to malnutrition (Surena, 2010). Diarrhea causes loss of water
electrolytes and nutrients in the body (Field, 2016). It come as result of small intestines unable to
absorb water and essential nutrients from the food, they do not take in much water from the food
that is passing, so the passing food is almost fully liquid and excreted as watery stool. Vomiting
and diarrhea affects drinking in that the patient will need more of fluids and become thirsty
frequently, while abdominal cramping affects eating because the patient will not have the desire
to eat food.
How to assess
This can be assessed by checking the signs of both dehydration and malnutrition. For
dehydration, the clinical signs that are assessed include weight loss, thirst, dry mucous
membrane, sunken-appearing eyes and decreased skin turgor. Monitoring the vital signs four
hourly to check signs of hypotension, monitoring his fluid input and output each shift and
balancing daily. Ask patient if he is frequently feeling headaches.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
How to care
Patient is cared by encouraging him to drink clear liquids such water or diluted juice at regular
interval and small amounts each time. Patient to avoid undiluted juice and soft drinks because it
will worsen diarrhea (Yunus, 2011). Patient to take fruit juice during the day about 8-12 cups to
avoid vomiting and diarrhea. Encourage sips of water in between the meals. Use sports drink to
replace potassium and sodium, salt and other electrolytes the body lost during diarrhea and if
nausea is present encourage the patient to take sips of water and to eat slowly, drink ice –cold
drinks, avoid activity after eating and to avoid fried and greasy food. Administer normal saline
intravenous 500mls. It comprises of sodium and chlorine (Floss, & Borthwick, 2018) so that it
replaces lost fluid and prevent or corrects some type of electrolyte imbalance alternating with
ringer’s lactate six hourly, ringers lactate contains mixture of sodium chloride, sodium lactate
and calcium chloride. It also contains microbial agents also antimicrobial agents for prevention
of infection. you check signs of fluid overload and give the patient soft foods, BRAT diet which
are high in potassium and help replace nutrients lost including bananas, rice, applesauce, dry
toast and soda crackers this reduces vomiting and diarrhea. Another alternative food are potatoes,
peanut butter, skinless chicken and yoghurt, this food help recover from upset of diarrhea.
Administer bismuth salicylate 525mg 2 tablets every 30minutes as needed 16tablets 24 hours
which treat discomforts of stomach and diarrhea. Administer paracetamol 100mg if the patient is
in more discomfort of abdominal cramps. Administer loperamide which slows movement of food
through the intestines and allows the body absorbs more liquid (Brunner, 2010), 4mg orally after
first stool then 2mg after each unformed stool. It should be 16mg per day.
Patient is cared by encouraging him to drink clear liquids such water or diluted juice at regular
interval and small amounts each time. Patient to avoid undiluted juice and soft drinks because it
will worsen diarrhea (Yunus, 2011). Patient to take fruit juice during the day about 8-12 cups to
avoid vomiting and diarrhea. Encourage sips of water in between the meals. Use sports drink to
replace potassium and sodium, salt and other electrolytes the body lost during diarrhea and if
nausea is present encourage the patient to take sips of water and to eat slowly, drink ice –cold
drinks, avoid activity after eating and to avoid fried and greasy food. Administer normal saline
intravenous 500mls. It comprises of sodium and chlorine (Floss, & Borthwick, 2018) so that it
replaces lost fluid and prevent or corrects some type of electrolyte imbalance alternating with
ringer’s lactate six hourly, ringers lactate contains mixture of sodium chloride, sodium lactate
and calcium chloride. It also contains microbial agents also antimicrobial agents for prevention
of infection. you check signs of fluid overload and give the patient soft foods, BRAT diet which
are high in potassium and help replace nutrients lost including bananas, rice, applesauce, dry
toast and soda crackers this reduces vomiting and diarrhea. Another alternative food are potatoes,
peanut butter, skinless chicken and yoghurt, this food help recover from upset of diarrhea.
Administer bismuth salicylate 525mg 2 tablets every 30minutes as needed 16tablets 24 hours
which treat discomforts of stomach and diarrhea. Administer paracetamol 100mg if the patient is
in more discomfort of abdominal cramps. Administer loperamide which slows movement of food
through the intestines and allows the body absorbs more liquid (Brunner, 2010), 4mg orally after
first stool then 2mg after each unformed stool. It should be 16mg per day.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Personal cleansing and dressing
How it is affected
This affected by vomiting, diarrhea and lethargy. Vomiting and episodes of watery diarrhea is
unpredictable and it can cause soiling of oneself and also the clothing’s and beddings. It also
causes transfer of the disease if there is improper hand washing and hygiene also especially after
using the toilet or being in contact with vomitus, equipment and environmental surfaces can be
contaminated and lead to further spread. It can further cause urinary tract infection if poor
cleaning technique of genitals after diarrhea is done. Lethargy makes the patient unable to
change the soiled clothes and maintain personal hygiene
How to asses
It can be assessed by examining patient's clothing if it is wet soiled, smelling or are wet, skin if it
oily, greasy has acne or rashes especially the genital regions, assess the mouth if it has smell due
to vomitus, has gingivitis, cavities if the lips are dry and cracked, check the nails if they are well
kept and not dirty, check the hair if they are unkempt, smelly and oily.
How to care
Ensure the clothing are changed whenever soiled if diaper is soiled and washed separately with
hot water and detergent and allow to dry thoroughly. Ensure the patient wash his hands properly
and frequently with soap and water, wash hands before contact meals and other people and after
using the toilet. Do sponge bath daily or bathe the patient normally to prevent smell and spread
of the infection, ensure enhanced cleaning of environment and equipment, control the source of
the disease if water or food and also isolate the patient to prevent spread of the infection to other
people, this precaution should continue for 48hours. Use the adult diapers in case of increased
frequency of diarrhea and change it when it is soiled and ensure it is disposed well. Administer
How it is affected
This affected by vomiting, diarrhea and lethargy. Vomiting and episodes of watery diarrhea is
unpredictable and it can cause soiling of oneself and also the clothing’s and beddings. It also
causes transfer of the disease if there is improper hand washing and hygiene also especially after
using the toilet or being in contact with vomitus, equipment and environmental surfaces can be
contaminated and lead to further spread. It can further cause urinary tract infection if poor
cleaning technique of genitals after diarrhea is done. Lethargy makes the patient unable to
change the soiled clothes and maintain personal hygiene
How to asses
It can be assessed by examining patient's clothing if it is wet soiled, smelling or are wet, skin if it
oily, greasy has acne or rashes especially the genital regions, assess the mouth if it has smell due
to vomitus, has gingivitis, cavities if the lips are dry and cracked, check the nails if they are well
kept and not dirty, check the hair if they are unkempt, smelly and oily.
How to care
Ensure the clothing are changed whenever soiled if diaper is soiled and washed separately with
hot water and detergent and allow to dry thoroughly. Ensure the patient wash his hands properly
and frequently with soap and water, wash hands before contact meals and other people and after
using the toilet. Do sponge bath daily or bathe the patient normally to prevent smell and spread
of the infection, ensure enhanced cleaning of environment and equipment, control the source of
the disease if water or food and also isolate the patient to prevent spread of the infection to other
people, this precaution should continue for 48hours. Use the adult diapers in case of increased
frequency of diarrhea and change it when it is soiled and ensure it is disposed well. Administer
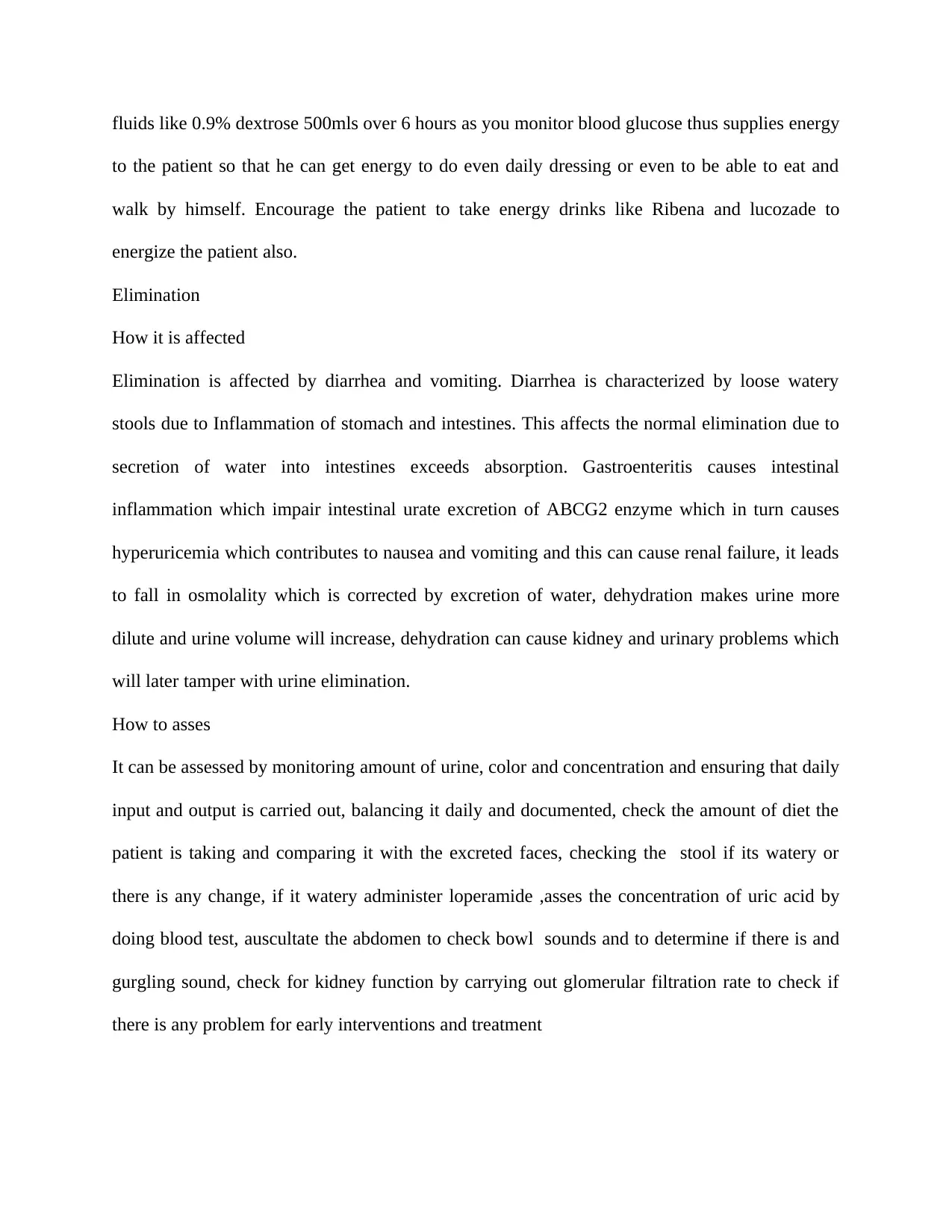
fluids like 0.9% dextrose 500mls over 6 hours as you monitor blood glucose thus supplies energy
to the patient so that he can get energy to do even daily dressing or even to be able to eat and
walk by himself. Encourage the patient to take energy drinks like Ribena and lucozade to
energize the patient also.
Elimination
How it is affected
Elimination is affected by diarrhea and vomiting. Diarrhea is characterized by loose watery
stools due to Inflammation of stomach and intestines. This affects the normal elimination due to
secretion of water into intestines exceeds absorption. Gastroenteritis causes intestinal
inflammation which impair intestinal urate excretion of ABCG2 enzyme which in turn causes
hyperuricemia which contributes to nausea and vomiting and this can cause renal failure, it leads
to fall in osmolality which is corrected by excretion of water, dehydration makes urine more
dilute and urine volume will increase, dehydration can cause kidney and urinary problems which
will later tamper with urine elimination.
How to asses
It can be assessed by monitoring amount of urine, color and concentration and ensuring that daily
input and output is carried out, balancing it daily and documented, check the amount of diet the
patient is taking and comparing it with the excreted faces, checking the stool if its watery or
there is any change, if it watery administer loperamide ,asses the concentration of uric acid by
doing blood test, auscultate the abdomen to check bowl sounds and to determine if there is and
gurgling sound, check for kidney function by carrying out glomerular filtration rate to check if
there is any problem for early interventions and treatment
to the patient so that he can get energy to do even daily dressing or even to be able to eat and
walk by himself. Encourage the patient to take energy drinks like Ribena and lucozade to
energize the patient also.
Elimination
How it is affected
Elimination is affected by diarrhea and vomiting. Diarrhea is characterized by loose watery
stools due to Inflammation of stomach and intestines. This affects the normal elimination due to
secretion of water into intestines exceeds absorption. Gastroenteritis causes intestinal
inflammation which impair intestinal urate excretion of ABCG2 enzyme which in turn causes
hyperuricemia which contributes to nausea and vomiting and this can cause renal failure, it leads
to fall in osmolality which is corrected by excretion of water, dehydration makes urine more
dilute and urine volume will increase, dehydration can cause kidney and urinary problems which
will later tamper with urine elimination.
How to asses
It can be assessed by monitoring amount of urine, color and concentration and ensuring that daily
input and output is carried out, balancing it daily and documented, check the amount of diet the
patient is taking and comparing it with the excreted faces, checking the stool if its watery or
there is any change, if it watery administer loperamide ,asses the concentration of uric acid by
doing blood test, auscultate the abdomen to check bowl sounds and to determine if there is and
gurgling sound, check for kidney function by carrying out glomerular filtration rate to check if
there is any problem for early interventions and treatment
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

How to care
Monitoring fluid intake and output to evaluate patient’s fluid and electrolyte imbalance and also
to allow for prompt intervention to correct the imbalance this is done at regular interval of 4
hours and recording it in fluid chart (Metheny, N., & Metheny, N. M. 2011). The normal urine
output range for 24 hours is of 800-2000 liters with normal fluid intake of 2litres per day.
Monitor temperature, inflammation of intestinal lining causes increase in temperature due to
infection and administer antipyretic such as paracetamol, hyperuricemia can be treated by giving
non- steroidal anti-inflammatory such as ibuprofen and diclofenac which can prevent its severity,
osmolality can be corrected by giving electrolyte balance drugs or fluids such as ringers lactate,
polyuria is corrected by desmopressin which increase permeability of renal tubules which
increases water reabsorption (Rahnama’i, Vrijens, & Marcelissen, 2018).
Assess Plan Implement Evaluate
Vomiting
Diarrhea
Lethargy
To administer normal saline
500mls to run alternatively
with Ringer's lactate 500mls
To administer lower amide
4mg orally
To ensure patient drinks
clear fluid sip by sip slowly
To administer bismuth
subsalicylate 525mg
To administer 0.9%dextrose
give the patient water slowl,y sip
by sip
Patient also was given sports
drink at 3pm to replace
potassium
Nurse to also administer
loperamide 4mg at 9 am orally
Administered bismuth
subsalicylate 525mg 2 tablets
every 30 minutes, administered
After 24 hours;
Patient skin turgor improved
patient became active and
was able to do daily
activities
On assessing patient stool, it
was hard and normal
On repeat of urea electrolyte
and creatinine test it was at
normal range
Monitoring fluid intake and output to evaluate patient’s fluid and electrolyte imbalance and also
to allow for prompt intervention to correct the imbalance this is done at regular interval of 4
hours and recording it in fluid chart (Metheny, N., & Metheny, N. M. 2011). The normal urine
output range for 24 hours is of 800-2000 liters with normal fluid intake of 2litres per day.
Monitor temperature, inflammation of intestinal lining causes increase in temperature due to
infection and administer antipyretic such as paracetamol, hyperuricemia can be treated by giving
non- steroidal anti-inflammatory such as ibuprofen and diclofenac which can prevent its severity,
osmolality can be corrected by giving electrolyte balance drugs or fluids such as ringers lactate,
polyuria is corrected by desmopressin which increase permeability of renal tubules which
increases water reabsorption (Rahnama’i, Vrijens, & Marcelissen, 2018).
Assess Plan Implement Evaluate
Vomiting
Diarrhea
Lethargy
To administer normal saline
500mls to run alternatively
with Ringer's lactate 500mls
To administer lower amide
4mg orally
To ensure patient drinks
clear fluid sip by sip slowly
To administer bismuth
subsalicylate 525mg
To administer 0.9%dextrose
give the patient water slowl,y sip
by sip
Patient also was given sports
drink at 3pm to replace
potassium
Nurse to also administer
loperamide 4mg at 9 am orally
Administered bismuth
subsalicylate 525mg 2 tablets
every 30 minutes, administered
After 24 hours;
Patient skin turgor improved
patient became active and
was able to do daily
activities
On assessing patient stool, it
was hard and normal
On repeat of urea electrolyte
and creatinine test it was at
normal range
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
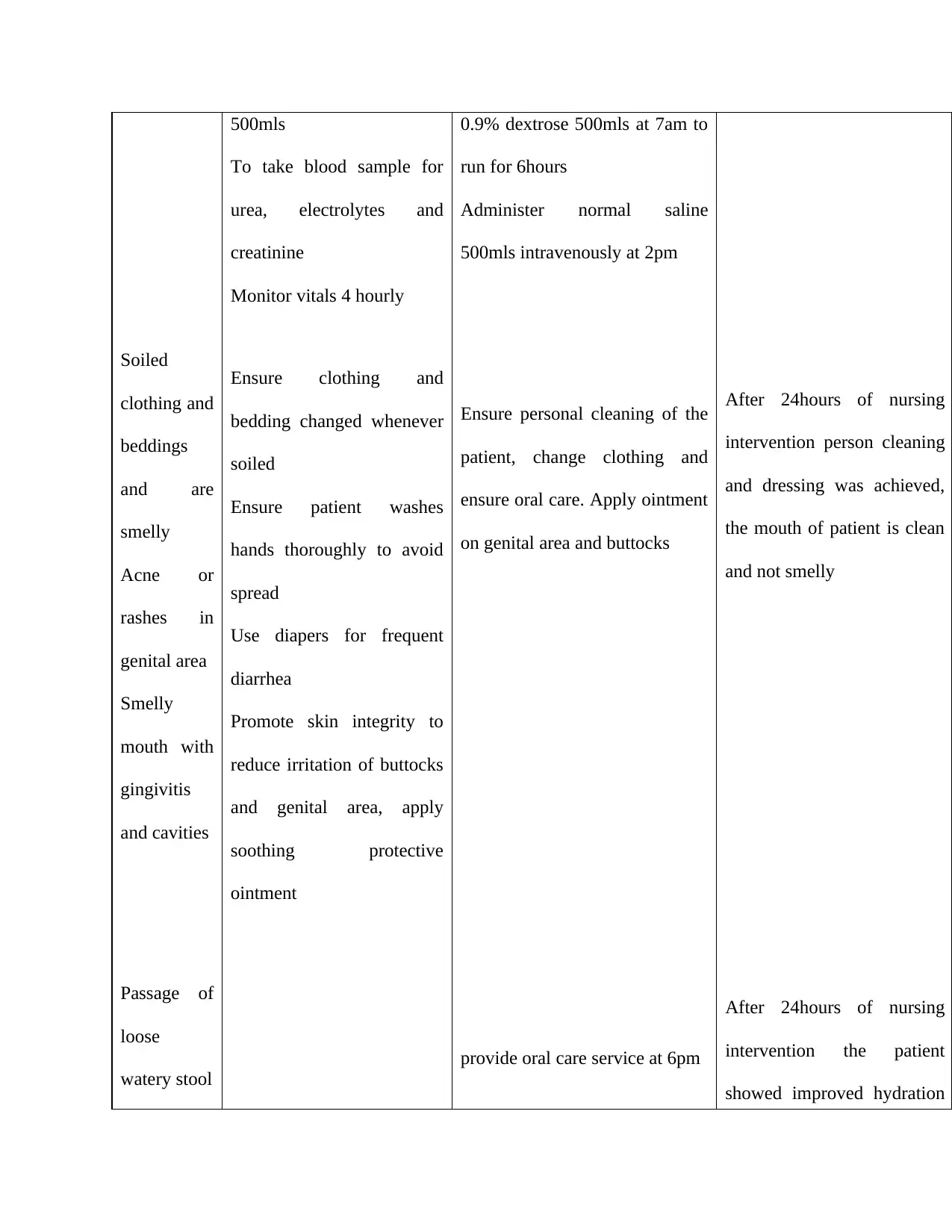
Soiled
clothing and
beddings
and are
smelly
Acne or
rashes in
genital area
Smelly
mouth with
gingivitis
and cavities
Passage of
loose
watery stool
500mls
To take blood sample for
urea, electrolytes and
creatinine
Monitor vitals 4 hourly
Ensure clothing and
bedding changed whenever
soiled
Ensure patient washes
hands thoroughly to avoid
spread
Use diapers for frequent
diarrhea
Promote skin integrity to
reduce irritation of buttocks
and genital area, apply
soothing protective
ointment
0.9% dextrose 500mls at 7am to
run for 6hours
Administer normal saline
500mls intravenously at 2pm
Ensure personal cleaning of the
patient, change clothing and
ensure oral care. Apply ointment
on genital area and buttocks
provide oral care service at 6pm
After 24hours of nursing
intervention person cleaning
and dressing was achieved,
the mouth of patient is clean
and not smelly
After 24hours of nursing
intervention the patient
showed improved hydration
clothing and
beddings
and are
smelly
Acne or
rashes in
genital area
Smelly
mouth with
gingivitis
and cavities
Passage of
loose
watery stool
500mls
To take blood sample for
urea, electrolytes and
creatinine
Monitor vitals 4 hourly
Ensure clothing and
bedding changed whenever
soiled
Ensure patient washes
hands thoroughly to avoid
spread
Use diapers for frequent
diarrhea
Promote skin integrity to
reduce irritation of buttocks
and genital area, apply
soothing protective
ointment
0.9% dextrose 500mls at 7am to
run for 6hours
Administer normal saline
500mls intravenously at 2pm
Ensure personal cleaning of the
patient, change clothing and
ensure oral care. Apply ointment
on genital area and buttocks
provide oral care service at 6pm
After 24hours of nursing
intervention person cleaning
and dressing was achieved,
the mouth of patient is clean
and not smelly
After 24hours of nursing
intervention the patient
showed improved hydration
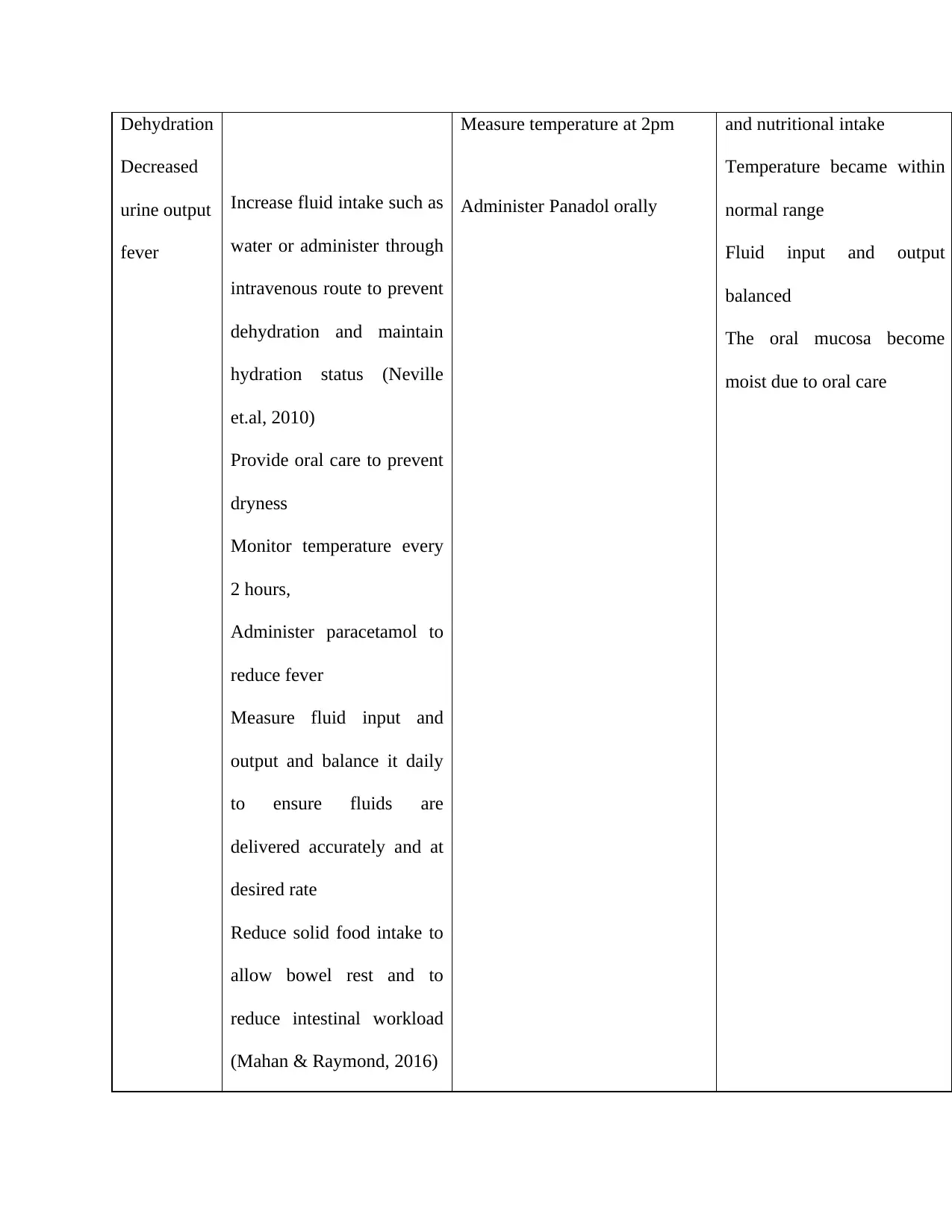
Dehydration
Decreased
urine output
fever
Increase fluid intake such as
water or administer through
intravenous route to prevent
dehydration and maintain
hydration status (Neville
et.al, 2010)
Provide oral care to prevent
dryness
Monitor temperature every
2 hours,
Administer paracetamol to
reduce fever
Measure fluid input and
output and balance it daily
to ensure fluids are
delivered accurately and at
desired rate
Reduce solid food intake to
allow bowel rest and to
reduce intestinal workload
(Mahan & Raymond, 2016)
Measure temperature at 2pm
Administer Panadol orally
and nutritional intake
Temperature became within
normal range
Fluid input and output
balanced
The oral mucosa become
moist due to oral care
Decreased
urine output
fever
Increase fluid intake such as
water or administer through
intravenous route to prevent
dehydration and maintain
hydration status (Neville
et.al, 2010)
Provide oral care to prevent
dryness
Monitor temperature every
2 hours,
Administer paracetamol to
reduce fever
Measure fluid input and
output and balance it daily
to ensure fluids are
delivered accurately and at
desired rate
Reduce solid food intake to
allow bowel rest and to
reduce intestinal workload
(Mahan & Raymond, 2016)
Measure temperature at 2pm
Administer Panadol orally
and nutritional intake
Temperature became within
normal range
Fluid input and output
balanced
The oral mucosa become
moist due to oral care
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
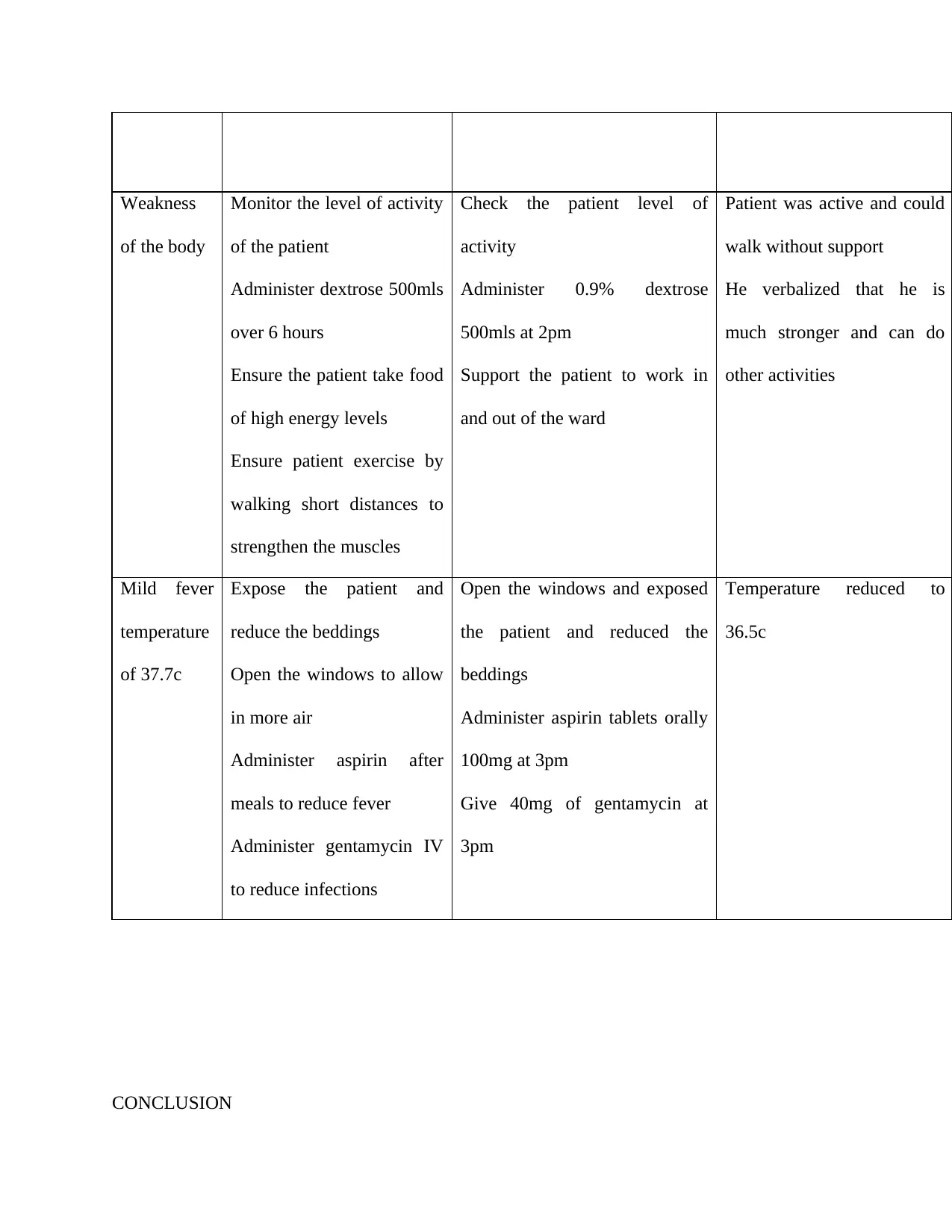
Weakness
of the body
Monitor the level of activity
of the patient
Administer dextrose 500mls
over 6 hours
Ensure the patient take food
of high energy levels
Ensure patient exercise by
walking short distances to
strengthen the muscles
Check the patient level of
activity
Administer 0.9% dextrose
500mls at 2pm
Support the patient to work in
and out of the ward
Patient was active and could
walk without support
He verbalized that he is
much stronger and can do
other activities
Mild fever
temperature
of 37.7c
Expose the patient and
reduce the beddings
Open the windows to allow
in more air
Administer aspirin after
meals to reduce fever
Administer gentamycin IV
to reduce infections
Open the windows and exposed
the patient and reduced the
beddings
Administer aspirin tablets orally
100mg at 3pm
Give 40mg of gentamycin at
3pm
Temperature reduced to
36.5c
CONCLUSION
of the body
Monitor the level of activity
of the patient
Administer dextrose 500mls
over 6 hours
Ensure the patient take food
of high energy levels
Ensure patient exercise by
walking short distances to
strengthen the muscles
Check the patient level of
activity
Administer 0.9% dextrose
500mls at 2pm
Support the patient to work in
and out of the ward
Patient was active and could
walk without support
He verbalized that he is
much stronger and can do
other activities
Mild fever
temperature
of 37.7c
Expose the patient and
reduce the beddings
Open the windows to allow
in more air
Administer aspirin after
meals to reduce fever
Administer gentamycin IV
to reduce infections
Open the windows and exposed
the patient and reduced the
beddings
Administer aspirin tablets orally
100mg at 3pm
Give 40mg of gentamycin at
3pm
Temperature reduced to
36.5c
CONCLUSION
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Viral gastroenteritis is the most common illness since affects many people. The paths that it
follows is simple. It starts from fecal contaminated substance where the body contracts the virus,
enabling it to travel to small intestines (Cutler, 2013). After causing touble on the lower digestive
system, the virus gets attacked by the white blood cells of the immune system which is powerful.
Understanding the life cycle of can help in diagnoses, elimination and prevention of the disease
(Tille, 2015). It can be prevented by washing hands, cooking meat thoroughly and drinking
plenty of water daily. Dehydration occurs when the fluid amount leaving the body is higher than
the amount going back to the body (Roberts, 2016). In case of dehydration and signs like
extreme thirst, confusion, little or no urine output, notify the doctor because it’s an emergency.
Certain individuals with heart or kidney disease many need less fluid to correct dehydration ( Ter
Maaten, 2015)
follows is simple. It starts from fecal contaminated substance where the body contracts the virus,
enabling it to travel to small intestines (Cutler, 2013). After causing touble on the lower digestive
system, the virus gets attacked by the white blood cells of the immune system which is powerful.
Understanding the life cycle of can help in diagnoses, elimination and prevention of the disease
(Tille, 2015). It can be prevented by washing hands, cooking meat thoroughly and drinking
plenty of water daily. Dehydration occurs when the fluid amount leaving the body is higher than
the amount going back to the body (Roberts, 2016). In case of dehydration and signs like
extreme thirst, confusion, little or no urine output, notify the doctor because it’s an emergency.
Certain individuals with heart or kidney disease many need less fluid to correct dehydration ( Ter
Maaten, 2015)
References
Blinderman, C. D., & Billings, J. A. (2015). Comfort care for patients dying in the hospital. New
England Journal of Medicine, 373(26), 2549-2561.
Brunner, L. S. (2010). Brunner & Suddarth's textbook of medical-surgical nursing (Vol. 1). Lippincott
Williams & Wilkins.
Chaithongdi, N., Subauste, J. S., Koch, C. A., & Geraci, S. A. (2011). Diagnosis and management of
hyperglycemic emergencies. Hormones (Athens), 10(4), 250-60.
Cutler, E. (2013). Clearing the Way to Health and Wellness: Reversing Chronic Conditions by Freeing
the Body of Food, Environmental, and Other Sensitivities. iUniverse.
Field, L. (2016). Nursing & Health Survival Guide: Nutrition and Hydration. Routledge.
Floss, K., & Borthwick, M. (2018). Intravenous fluid therapy—background and principles. Lung
cancer, 15, 05.
Humphries, R. M., & Linscott, A. J. (2015). Laboratory diagnosis of bacterial gastroenteritis. Clinical
microbiology reviews, 28(1), 3-31.
Koo, H. L., Ajami, N., Atmar, R. L., & DuPont, H. L. (2010). Noroviruses: The leading cause of
gastroenteritis worldwide. Discovery medicine, 10(50), 61-70.
Mahan, L. K., & Raymond, J. L. (2016). Krause's food & the nutrition care process-e-book. Elsevier
Health Sciences.
Metheny, N., & Metheny, N. M. (2011). Fluid and electrolyte balance. Jones & Bartlett Publishers.
Neville, K. A., Sandeman, D. J., Rubinstein, A., Henry, G. M., McGlynn, M., & Walker, J. L. (2010).
Prevention of hyponatremia during maintenance intravenous fluid administration: a prospective
randomized study of fluid type versus fluid rate. The Journal of pediatrics, 156(2), 313-319.
Blinderman, C. D., & Billings, J. A. (2015). Comfort care for patients dying in the hospital. New
England Journal of Medicine, 373(26), 2549-2561.
Brunner, L. S. (2010). Brunner & Suddarth's textbook of medical-surgical nursing (Vol. 1). Lippincott
Williams & Wilkins.
Chaithongdi, N., Subauste, J. S., Koch, C. A., & Geraci, S. A. (2011). Diagnosis and management of
hyperglycemic emergencies. Hormones (Athens), 10(4), 250-60.
Cutler, E. (2013). Clearing the Way to Health and Wellness: Reversing Chronic Conditions by Freeing
the Body of Food, Environmental, and Other Sensitivities. iUniverse.
Field, L. (2016). Nursing & Health Survival Guide: Nutrition and Hydration. Routledge.
Floss, K., & Borthwick, M. (2018). Intravenous fluid therapy—background and principles. Lung
cancer, 15, 05.
Humphries, R. M., & Linscott, A. J. (2015). Laboratory diagnosis of bacterial gastroenteritis. Clinical
microbiology reviews, 28(1), 3-31.
Koo, H. L., Ajami, N., Atmar, R. L., & DuPont, H. L. (2010). Noroviruses: The leading cause of
gastroenteritis worldwide. Discovery medicine, 10(50), 61-70.
Mahan, L. K., & Raymond, J. L. (2016). Krause's food & the nutrition care process-e-book. Elsevier
Health Sciences.
Metheny, N., & Metheny, N. M. (2011). Fluid and electrolyte balance. Jones & Bartlett Publishers.
Neville, K. A., Sandeman, D. J., Rubinstein, A., Henry, G. M., McGlynn, M., & Walker, J. L. (2010).
Prevention of hyponatremia during maintenance intravenous fluid administration: a prospective
randomized study of fluid type versus fluid rate. The Journal of pediatrics, 156(2), 313-319.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





