Hand Hygiene Project: Infection Prevention in Acute Care Unit
VerifiedAdded on 2022/08/22
|12
|1927
|24
Project
AI Summary
This project plan focuses on the critical role of hand hygiene in preventing hospital-acquired infections within an acute care unit. The student, drawing from personal experience and relevant literature, identifies the significance of hand hygiene in reducing healthcare-associated infections, referencing WHO guidelines and statistics on infection rates. The project includes a detailed proposal for a hand hygiene training program and the implementation of an automated evaluation system to monitor compliance among healthcare providers. A comparative analysis will be performed to assess the effectiveness of the intervention. The plan incorporates a literature review supporting the importance of hand hygiene, along with evidence from various studies on the impact of different hand hygiene strategies. The proposed service innovation aims to improve hand hygiene compliance and ultimately decrease infection rates, with an emphasis on evaluation and outcome measures to assess the project's success. The project adheres to the guidelines provided in the assignment brief, outlining the problem identification, background evidence, implementation plan, evaluation methods, and recommendations.

Running Head : Hand hygiene
Hand hygiene
Name of the Student
Name of the University
Authors Note
Hand hygiene
Name of the Student
Name of the University
Authors Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2Hand hygiene
Problem Identification and Background Evidence
Introduction
The project plan will be focused on importance of Hand Hygiene in infection
prevention in an acute care unit of hospital. In section1, the evidence of effectiveness of the
hand-washing will be discussed. The section 2 will be represented with the proposal in detail
and summary of implementation of the plan. Evaluation and measurements will be shown in
section 3 which will help in the assessment of proposed plan. Finally, recommendations and
learning out comes will be described in the section 4.
Topic choice –rationale and reflection on practice
In my experience as healthcare assistant and during my placement of first and
second year , I have observed that the hospital acquired infection can be controlled by
hand hygiene and to control the infection among the patient and longer hospital stay .
300,000 healthcare-acquired infections are reported annually and among them 5,000 cases
outcome in mortality (Zilberberg et al., 2017). WHO has invented a hand hygiene protocol
called “5 moments of hand hygiene” which has been proven as an effective intervention for
preventing nosocomial infection in the hospital setting (www.who.int, 2020). The five steps
consist the following steps such as; “Before patient contact”, “Before aseptic task ”, “After
body fluid exposure risk”, “After touching a patient” and “After touching patient’s
surrounding”.
Background evidence
Problem Identification and Background Evidence
Introduction
The project plan will be focused on importance of Hand Hygiene in infection
prevention in an acute care unit of hospital. In section1, the evidence of effectiveness of the
hand-washing will be discussed. The section 2 will be represented with the proposal in detail
and summary of implementation of the plan. Evaluation and measurements will be shown in
section 3 which will help in the assessment of proposed plan. Finally, recommendations and
learning out comes will be described in the section 4.
Topic choice –rationale and reflection on practice
In my experience as healthcare assistant and during my placement of first and
second year , I have observed that the hospital acquired infection can be controlled by
hand hygiene and to control the infection among the patient and longer hospital stay .
300,000 healthcare-acquired infections are reported annually and among them 5,000 cases
outcome in mortality (Zilberberg et al., 2017). WHO has invented a hand hygiene protocol
called “5 moments of hand hygiene” which has been proven as an effective intervention for
preventing nosocomial infection in the hospital setting (www.who.int, 2020). The five steps
consist the following steps such as; “Before patient contact”, “Before aseptic task ”, “After
body fluid exposure risk”, “After touching a patient” and “After touching patient’s
surrounding”.
Background evidence
3Hand hygiene
I have investigated the usefulness of hand hygiene in preventing infection among the
patients admitted in the acute care unit in my literature review. Practice of Hand-washing
can reduce MRSA infections among the patients. Hand hygiene can prevent flu and food
poison with other diseases. There are different types of hand hygiene such as routine hand
wash, antiseptic hand wash, antiseptic hand-rub and surgical antisepsis (Bolon, 2016).
According to Gould et al., 2017, in acute care setting the highest rate of morbidity
and mortality is responsible for health care‐associated infection . Hand hygiene is one of the
most effective preventive measure to reduce Healthcare associated infection among the
patient. According to a systematic review short and long-term success policies recover the
compliance regarding Commendation of hand hygiene can determine whether hand hygiene
is effective acquiescence for reducing the rate of Health Care associated infection in in
hospitals or not. In the systematic review different studies were taken for evaluate the
effectiveness of hand hygiene compliances in Healthcare associated infection reduction. The
different strategies are education, verbal and written reminders, various performance
responses, organisational support with staff involvement and placement of alcohol based
hand rub in acute care settings.After reviewing 26 studies Systematic review state that
multimodal strategies are useful in improving hand hygiene compliances and reduce the
infection rate. The interventions are also effective in lowering methicillin-resistant
Staphylococcus aureus infection rate. The systematic review has stated that enhancing the
interventions of WHO can slightly improve hand hygiene compliances or reduce the
colonisation of bacteria and germs. However there is no use difference after executing the
WHO compliances in action of infection rate control.
Another study was conducted to evaluate the effectiveness of hand hygiene depending
upon the patient health condition and care environment(Okada, Yamamizu, and Fukai, 2016).
The study that in hemodialysis patient hand contamination rate is highest followed by the
I have investigated the usefulness of hand hygiene in preventing infection among the
patients admitted in the acute care unit in my literature review. Practice of Hand-washing
can reduce MRSA infections among the patients. Hand hygiene can prevent flu and food
poison with other diseases. There are different types of hand hygiene such as routine hand
wash, antiseptic hand wash, antiseptic hand-rub and surgical antisepsis (Bolon, 2016).
According to Gould et al., 2017, in acute care setting the highest rate of morbidity
and mortality is responsible for health care‐associated infection . Hand hygiene is one of the
most effective preventive measure to reduce Healthcare associated infection among the
patient. According to a systematic review short and long-term success policies recover the
compliance regarding Commendation of hand hygiene can determine whether hand hygiene
is effective acquiescence for reducing the rate of Health Care associated infection in in
hospitals or not. In the systematic review different studies were taken for evaluate the
effectiveness of hand hygiene compliances in Healthcare associated infection reduction. The
different strategies are education, verbal and written reminders, various performance
responses, organisational support with staff involvement and placement of alcohol based
hand rub in acute care settings.After reviewing 26 studies Systematic review state that
multimodal strategies are useful in improving hand hygiene compliances and reduce the
infection rate. The interventions are also effective in lowering methicillin-resistant
Staphylococcus aureus infection rate. The systematic review has stated that enhancing the
interventions of WHO can slightly improve hand hygiene compliances or reduce the
colonisation of bacteria and germs. However there is no use difference after executing the
WHO compliances in action of infection rate control.
Another study was conducted to evaluate the effectiveness of hand hygiene depending
upon the patient health condition and care environment(Okada, Yamamizu, and Fukai, 2016).
The study that in hemodialysis patient hand contamination rate is highest followed by the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4Hand hygiene
resident of of nursing homes patient with cancer postoperative patient and the patient of
hematological malignancies. The samples were taken from inpatient and outpatient and
individuals living in nursing home. The participants of the study perform hand hygiene and
bacteria samples were collected from the palm of the participants before and after performing
the hand hygiene procedure. The researcher collected the samples of smear from contralateral
Palm and measured the adenosine triphosphate levels to calculate the bacterial colonization.
Hand washing was more effective than using wet wipes to reduce infection rate. Regardless
the care environment and health condition of the patient hand hygiene is effective in reducing
methicillin-resistant staphylococcus aureus.
Relation between surface contact of Health Care worker and hand hygiene was studied in bye
observational study in a single bed hospital of UK. This study evaluate our relationship
between handwriting and the frequency of touching surface by Healthcare workers in a
patient room. Often the surface contact was non-random and the hygiene was deferred before
and after the patient contact (King et al.,2016). However the study showed that hand hygiene
was not related to spending time in patient room. The study represent that subconscious need
for hand hygiene has been increased among the Healthcare workers. This consciousness with
the help to support and focus on future and hygiene educational programs which will help in
patient care.
A reprospective cohort study investigated that application of hand hygiene complaints
system can resulted in to improve hand hygiene compliance and reduction in common
Hospital acquired infection rate. The trial was conducted in an Intensive Care Unit and
Intensive Care step down unit in hospital facility. The study was conducted to understand the
effectiveness of automated hand hygiene complement system in monitoring Healthcare
workers and the hand hygiene practices in in hospital care setting. The Complaints system
collected 623 404 events in comparison of 480 human observed events (McCalla et al.,
resident of of nursing homes patient with cancer postoperative patient and the patient of
hematological malignancies. The samples were taken from inpatient and outpatient and
individuals living in nursing home. The participants of the study perform hand hygiene and
bacteria samples were collected from the palm of the participants before and after performing
the hand hygiene procedure. The researcher collected the samples of smear from contralateral
Palm and measured the adenosine triphosphate levels to calculate the bacterial colonization.
Hand washing was more effective than using wet wipes to reduce infection rate. Regardless
the care environment and health condition of the patient hand hygiene is effective in reducing
methicillin-resistant staphylococcus aureus.
Relation between surface contact of Health Care worker and hand hygiene was studied in bye
observational study in a single bed hospital of UK. This study evaluate our relationship
between handwriting and the frequency of touching surface by Healthcare workers in a
patient room. Often the surface contact was non-random and the hygiene was deferred before
and after the patient contact (King et al.,2016). However the study showed that hand hygiene
was not related to spending time in patient room. The study represent that subconscious need
for hand hygiene has been increased among the Healthcare workers. This consciousness with
the help to support and focus on future and hygiene educational programs which will help in
patient care.
A reprospective cohort study investigated that application of hand hygiene complaints
system can resulted in to improve hand hygiene compliance and reduction in common
Hospital acquired infection rate. The trial was conducted in an Intensive Care Unit and
Intensive Care step down unit in hospital facility. The study was conducted to understand the
effectiveness of automated hand hygiene complement system in monitoring Healthcare
workers and the hand hygiene practices in in hospital care setting. The Complaints system
collected 623 404 events in comparison of 480 human observed events (McCalla et al.,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5Hand hygiene
2017). This result can ensure Hospital that automatic hand hygiene complaints system can
monitor the hand hygiene practices effectively. However the result showed that multidrug-
resistant organism Central Line associated bloodstream infection and catheter associated in
urinary tract infection rates were are not affected very much by HH compliances. Therefore
more awareness and researches are needed to control these infections.
Study criticized who promoted hand hygiene recommendations save lives clean our
hands and showed that no significant difference was observed in hospital acquired infection
before and after the implementation of the interventions (Bolton and McCulloch, 2018). The
study showed that in Australia MRSA bacteraemia was observed linear regression before and
after the intervention. The graph shows almost an identical slow with represent the
insignificance of hand hygiene compliances.
The principle evidences regarding effectiveness of hand hygiene has been presented
in the Table 1.
Proposed service innovation
The evidence above show the recommendation for controlling the hospital acquired
infections by Hand Hygiene Compliances. The recommendations will support to maintain
hand hygiene compliances, to implement automatic evaluating system to check whether the
healthcare worker has washed their hands or used sanitizers. Aim of my research is to
organise a hand hygiene training program among the healthcare providers and check the rate
of compliance among them with the help of automatic evaluating system . A comparative
analysis will be done to check the helpfulness of hand hygiene compliances in infection
control.
2017). This result can ensure Hospital that automatic hand hygiene complaints system can
monitor the hand hygiene practices effectively. However the result showed that multidrug-
resistant organism Central Line associated bloodstream infection and catheter associated in
urinary tract infection rates were are not affected very much by HH compliances. Therefore
more awareness and researches are needed to control these infections.
Study criticized who promoted hand hygiene recommendations save lives clean our
hands and showed that no significant difference was observed in hospital acquired infection
before and after the implementation of the interventions (Bolton and McCulloch, 2018). The
study showed that in Australia MRSA bacteraemia was observed linear regression before and
after the intervention. The graph shows almost an identical slow with represent the
insignificance of hand hygiene compliances.
The principle evidences regarding effectiveness of hand hygiene has been presented
in the Table 1.
Proposed service innovation
The evidence above show the recommendation for controlling the hospital acquired
infections by Hand Hygiene Compliances. The recommendations will support to maintain
hand hygiene compliances, to implement automatic evaluating system to check whether the
healthcare worker has washed their hands or used sanitizers. Aim of my research is to
organise a hand hygiene training program among the healthcare providers and check the rate
of compliance among them with the help of automatic evaluating system . A comparative
analysis will be done to check the helpfulness of hand hygiene compliances in infection
control.
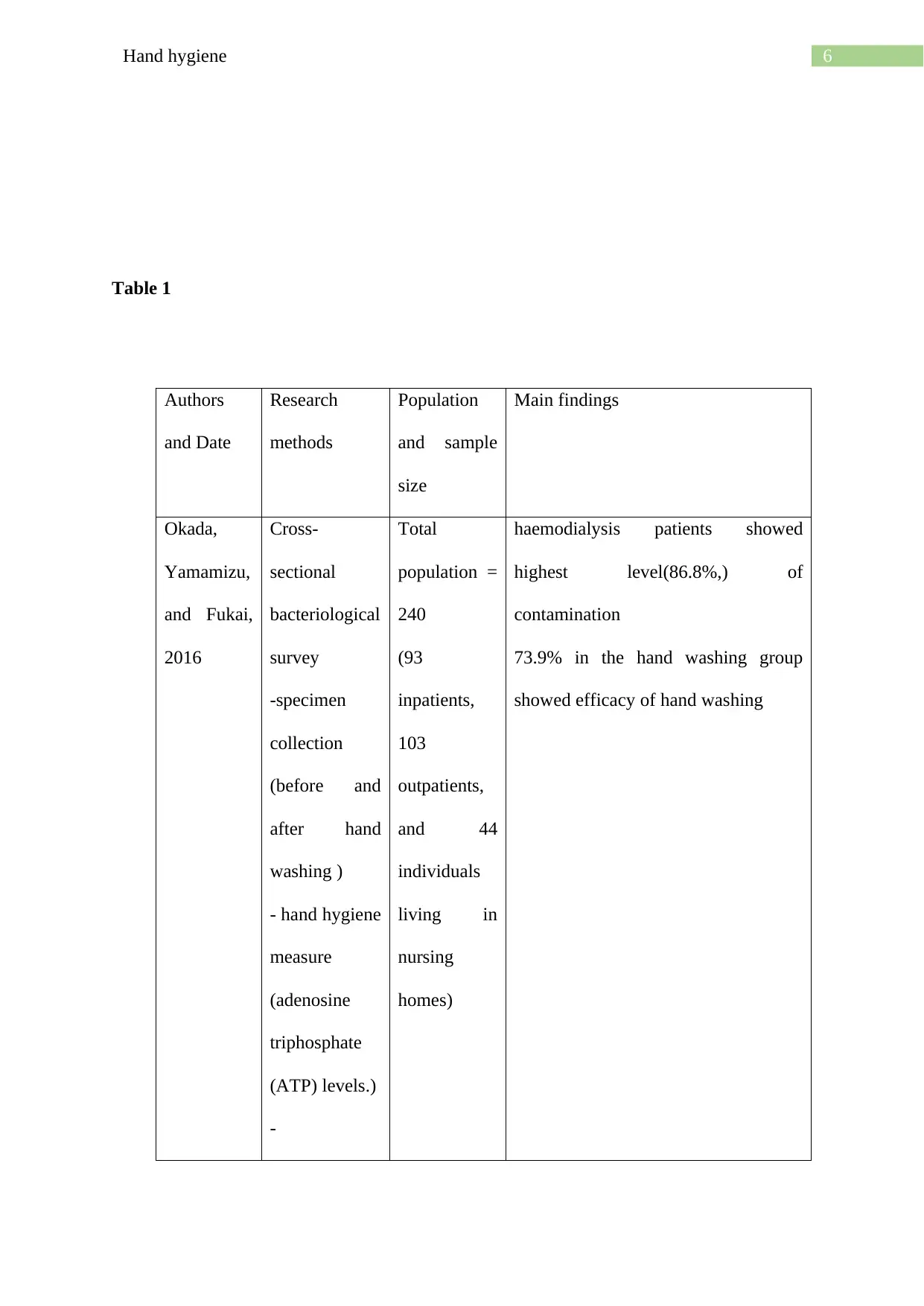
6Hand hygiene
Table 1
Authors
and Date
Research
methods
Population
and sample
size
Main findings
Okada,
Yamamizu,
and Fukai,
2016
Cross-
sectional
bacteriological
survey
-specimen
collection
(before and
after hand
washing )
- hand hygiene
measure
(adenosine
triphosphate
(ATP) levels.)
-
Total
population =
240
(93
inpatients,
103
outpatients,
and 44
individuals
living in
nursing
homes)
haemodialysis patients showed
highest level(86.8%,) of
contamination
73.9% in the hand washing group
showed efficacy of hand washing
Table 1
Authors
and Date
Research
methods
Population
and sample
size
Main findings
Okada,
Yamamizu,
and Fukai,
2016
Cross-
sectional
bacteriological
survey
-specimen
collection
(before and
after hand
washing )
- hand hygiene
measure
(adenosine
triphosphate
(ATP) levels.)
-
Total
population =
240
(93
inpatients,
103
outpatients,
and 44
individuals
living in
nursing
homes)
haemodialysis patients showed
highest level(86.8%,) of
contamination
73.9% in the hand washing group
showed efficacy of hand washing
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
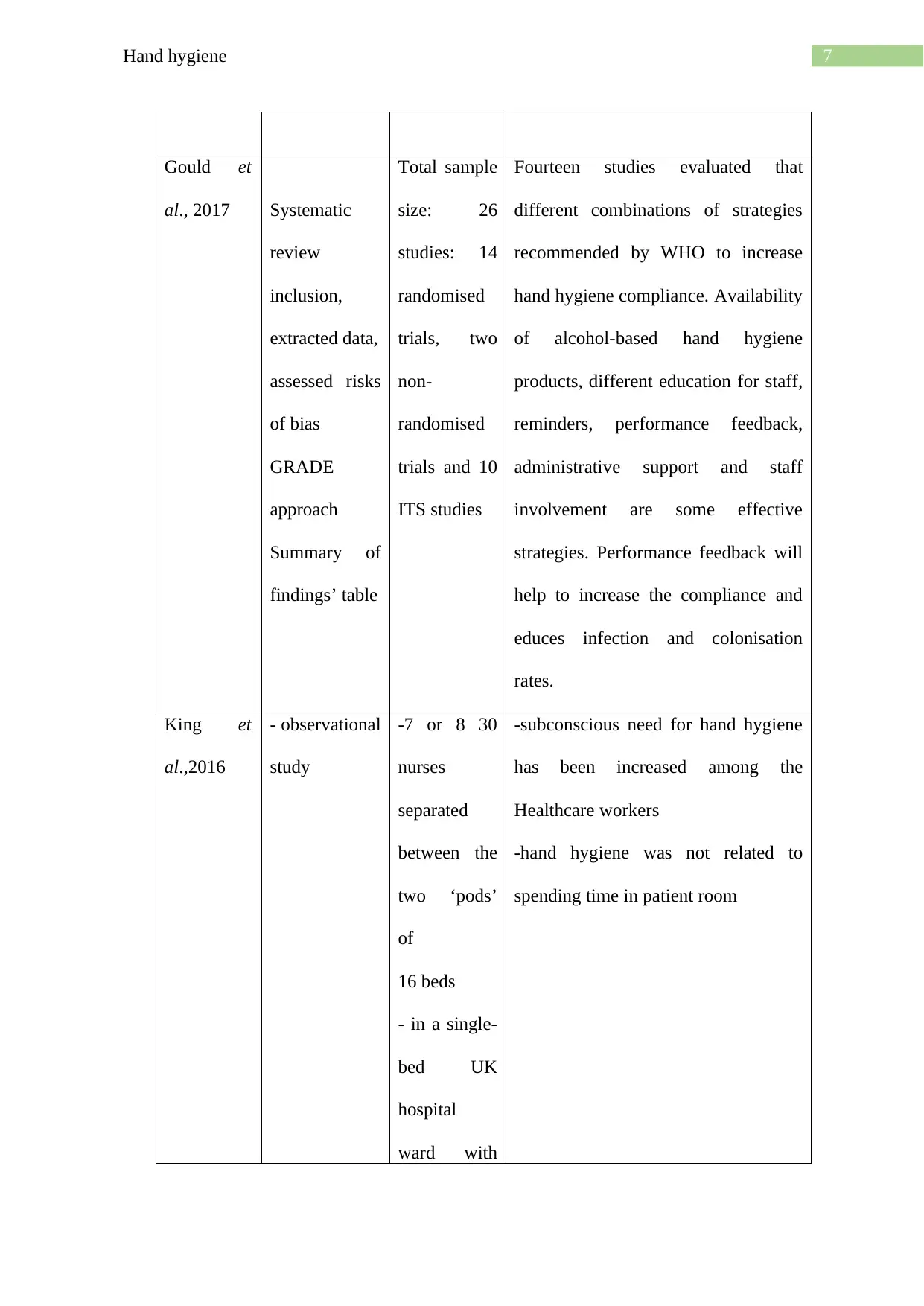
7Hand hygiene
Gould et
al., 2017 Systematic
review
inclusion,
extracted data,
assessed risks
of bias
GRADE
approach
Summary of
findings’ table
Total sample
size: 26
studies: 14
randomised
trials, two
non-
randomised
trials and 10
ITS studies
Fourteen studies evaluated that
different combinations of strategies
recommended by WHO to increase
hand hygiene compliance. Availability
of alcohol-based hand hygiene
products, different education for staff,
reminders, performance feedback,
administrative support and staff
involvement are some effective
strategies. Performance feedback will
help to increase the compliance and
educes infection and colonisation
rates.
King et
al.,2016
- observational
study
-7 or 8 30
nurses
separated
between the
two ‘pods’
of
16 beds
- in a single-
bed UK
hospital
ward with
-subconscious need for hand hygiene
has been increased among the
Healthcare workers
-hand hygiene was not related to
spending time in patient room
Gould et
al., 2017 Systematic
review
inclusion,
extracted data,
assessed risks
of bias
GRADE
approach
Summary of
findings’ table
Total sample
size: 26
studies: 14
randomised
trials, two
non-
randomised
trials and 10
ITS studies
Fourteen studies evaluated that
different combinations of strategies
recommended by WHO to increase
hand hygiene compliance. Availability
of alcohol-based hand hygiene
products, different education for staff,
reminders, performance feedback,
administrative support and staff
involvement are some effective
strategies. Performance feedback will
help to increase the compliance and
educes infection and colonisation
rates.
King et
al.,2016
- observational
study
-7 or 8 30
nurses
separated
between the
two ‘pods’
of
16 beds
- in a single-
bed UK
hospital
ward with
-subconscious need for hand hygiene
has been increased among the
Healthcare workers
-hand hygiene was not related to
spending time in patient room
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
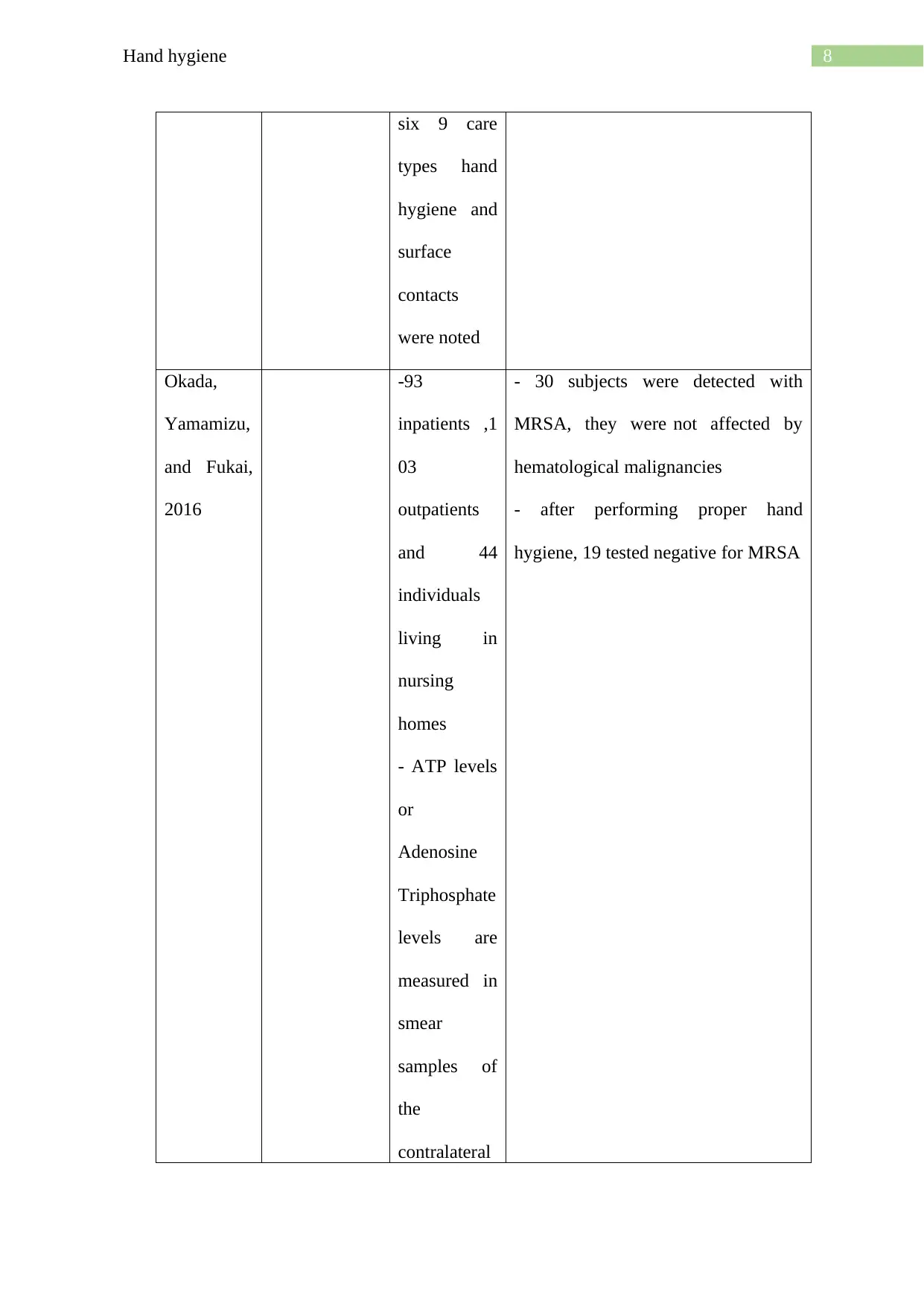
8Hand hygiene
six 9 care
types hand
hygiene and
surface
contacts
were noted
Okada,
Yamamizu,
and Fukai,
2016
-93
inpatients ,1
03
outpatients
and 44
individuals
living in
nursing
homes
- ATP levels
or
Adenosine
Triphosphate
levels are
measured in
smear
samples of
the
contralateral
- 30 subjects were detected with
MRSA, they were not affected by
hematological malignancies
- after performing proper hand
hygiene, 19 tested negative for MRSA
six 9 care
types hand
hygiene and
surface
contacts
were noted
Okada,
Yamamizu,
and Fukai,
2016
-93
inpatients ,1
03
outpatients
and 44
individuals
living in
nursing
homes
- ATP levels
or
Adenosine
Triphosphate
levels are
measured in
smear
samples of
the
contralateral
- 30 subjects were detected with
MRSA, they were not affected by
hematological malignancies
- after performing proper hand
hygiene, 19 tested negative for MRSA
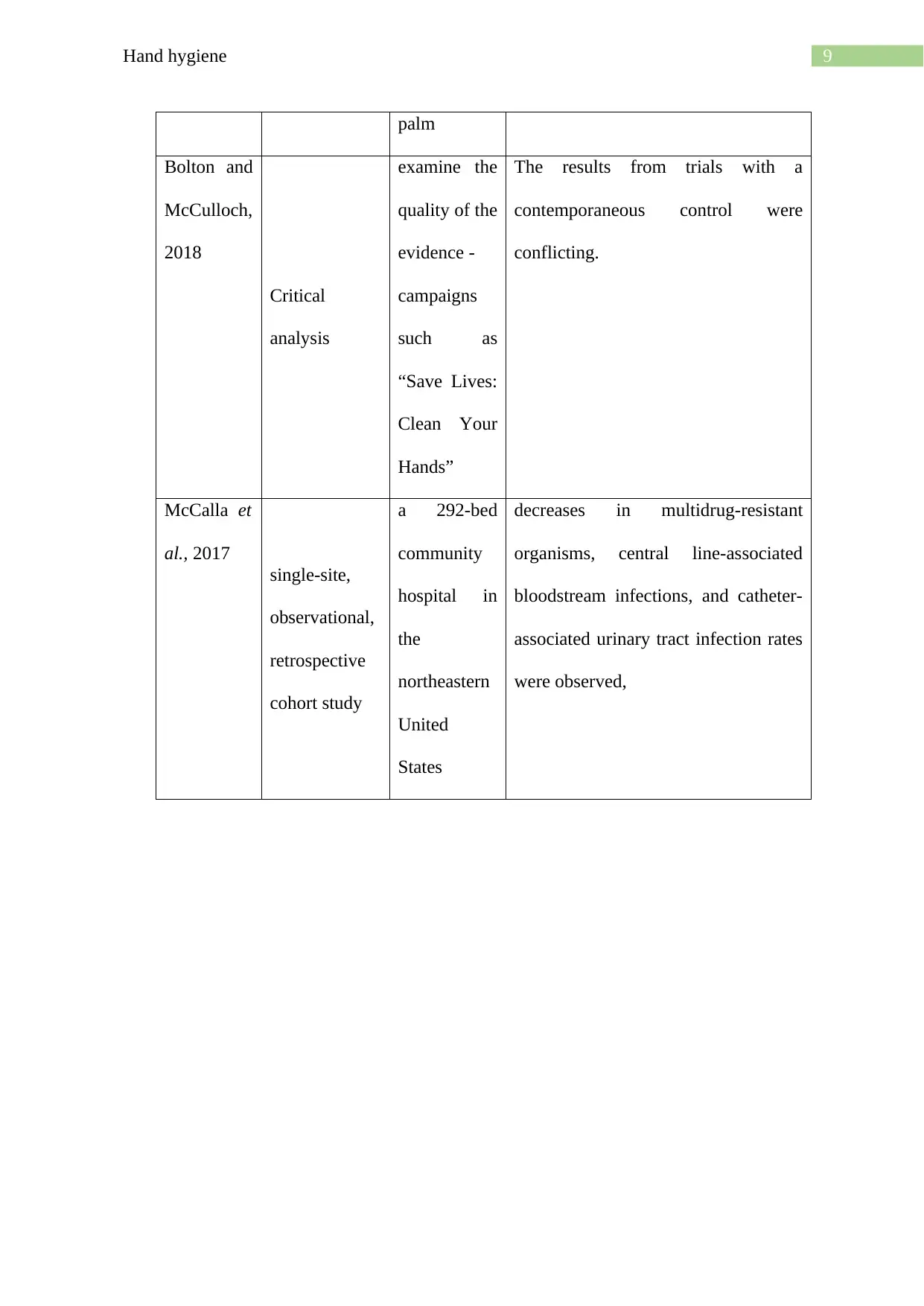
9Hand hygiene
palm
Bolton and
McCulloch,
2018
Critical
analysis
examine the
quality of the
evidence -
campaigns
such as
“Save Lives:
Clean Your
Hands”
The results from trials with a
contemporaneous control were
conflicting.
McCalla et
al., 2017
single-site,
observational,
retrospective
cohort study
a 292-bed
community
hospital in
the
northeastern
United
States
decreases in multidrug-resistant
organisms, central line-associated
bloodstream infections, and catheter-
associated urinary tract infection rates
were observed,
palm
Bolton and
McCulloch,
2018
Critical
analysis
examine the
quality of the
evidence -
campaigns
such as
“Save Lives:
Clean Your
Hands”
The results from trials with a
contemporaneous control were
conflicting.
McCalla et
al., 2017
single-site,
observational,
retrospective
cohort study
a 292-bed
community
hospital in
the
northeastern
United
States
decreases in multidrug-resistant
organisms, central line-associated
bloodstream infections, and catheter-
associated urinary tract infection rates
were observed,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10Hand hygiene
References
Bolon, M. K. (2016). Hand hygiene: an update. Infectious Disease Clinics, 30(3), 591-607.
Bolton, P. and McCulloch, T.J., 2018. The evidence supporting WHO recommendations on
the promotion of hand hygiene: a critique. BMC research notes, 11(1), pp.1-4.
Gould, D.J., Moralejo, D., Drey, N., Chudleigh, J.H. and Taljaard, M., 2017. Interventions to
improve hand hygiene compliance in patient care. Cochrane database of systematic reviews,
(9).
King, M.F., Noakes, C.J., Sleigh, P.A., Bale, S. and Waters, L., 2016. The relationship
between HCW surface contacts, care type and hand hygiene: An observational study in a
single-bed hospital ward. Journal of Hospital Infection May, 13.
McCalla, S., Reilly, M., Thomas, R. and McSpedon-Rai, D., 2017. An automated hand
hygiene compliance system is associated with improved monitoring of hand hygiene.
American journal of infection control, 45(5), pp.492-497.
Okada, J., Yamamizu, Y. and Fukai, K., 2016. Effectiveness of hand hygiene depends on the
patient's health condition and care environment. Japan Journal of Nursing Science, 13(4),
pp.413-423.
www.who.int, 2020. WHO | About SAVE LIVES: Clean Your Hands. [online] Who.int.
Available at: <https://www.who.int/gpsc/5may/background/5moments/en/> [Accessed 25
March 2020].
Zilberberg, M.D., Nathanson, B.H., Sulham, K., Fan, W. and Shorr, A.F., 2017. Carbapenem
resistance, inappropriate empiric treatment and outcomes among patients hospitalized with
Enterobacteriaceae urinary tract infection, pneumonia and sepsis. BMC infectious
diseases, 17(1), p.279.
References
Bolon, M. K. (2016). Hand hygiene: an update. Infectious Disease Clinics, 30(3), 591-607.
Bolton, P. and McCulloch, T.J., 2018. The evidence supporting WHO recommendations on
the promotion of hand hygiene: a critique. BMC research notes, 11(1), pp.1-4.
Gould, D.J., Moralejo, D., Drey, N., Chudleigh, J.H. and Taljaard, M., 2017. Interventions to
improve hand hygiene compliance in patient care. Cochrane database of systematic reviews,
(9).
King, M.F., Noakes, C.J., Sleigh, P.A., Bale, S. and Waters, L., 2016. The relationship
between HCW surface contacts, care type and hand hygiene: An observational study in a
single-bed hospital ward. Journal of Hospital Infection May, 13.
McCalla, S., Reilly, M., Thomas, R. and McSpedon-Rai, D., 2017. An automated hand
hygiene compliance system is associated with improved monitoring of hand hygiene.
American journal of infection control, 45(5), pp.492-497.
Okada, J., Yamamizu, Y. and Fukai, K., 2016. Effectiveness of hand hygiene depends on the
patient's health condition and care environment. Japan Journal of Nursing Science, 13(4),
pp.413-423.
www.who.int, 2020. WHO | About SAVE LIVES: Clean Your Hands. [online] Who.int.
Available at: <https://www.who.int/gpsc/5may/background/5moments/en/> [Accessed 25
March 2020].
Zilberberg, M.D., Nathanson, B.H., Sulham, K., Fan, W. and Shorr, A.F., 2017. Carbapenem
resistance, inappropriate empiric treatment and outcomes among patients hospitalized with
Enterobacteriaceae urinary tract infection, pneumonia and sepsis. BMC infectious
diseases, 17(1), p.279.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Running Head : Hand hygiene

12Hand hygiene
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





