Evidence-Based Nursing Research: Hand Hygiene Education Impact
VerifiedAdded on 2023/06/15
|15
|4127
|393
Literature Review
AI Summary
This literature review examines the critical issue of hand hygiene in healthcare settings, focusing on the problem of inadequate hand hygiene practices and its significant impact on the spread of infections, including antibiotic-resistant microorganisms. It highlights the importance of hand hygiene in preventing healthcare-associated infections (HAIs) and discusses the current practices and multi-modal strategies for promoting hand hygiene, such as in-service education, workshops, and the implementation of national and facility-based guidelines. The review also explores the potential impact of hand hygiene education programs on improving healthcare quality, reducing hospital-acquired infections, and enhancing patient safety. It includes a PICO question addressing the effectiveness of enhanced theory education on hand hygiene and details the search strategy used to identify relevant research articles, including keywords and selection criteria. The review summarizes the findings of several research articles and non-research articles, emphasizing the importance of multimodal strategies, educational interventions, and quality improvement programs in promoting hand hygiene compliance among healthcare workers. Desklib offers a wealth of similar solved assignments and study resources for students.
Evidence Based Nursing Research
1
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
A
A1 Problem:
Hand hygiene is a general term which can be used for the activities related to the hand
cleansing. World Health Organization (WHO) published guidelines on hand hygiene which
comprises of scientific data on hand hygiene rationale and practices in health care. Hand
hygiene is required in five instances like prior to touching to the patient, prior to carrying out
aseptic and clean procedures, at the time of risk of exposure to body fluids, after touching
patient and after touching patient’s belongings and surroundings. Dynamic behavioural
change is required for maintaining hand hygiene. Infection prevention and control
programme should be implemented through healthcare related training and education for
maintaining hand hygiene. All the healthcare workers should incorporate hand hygiene as the
integral part of their practice. However, it was evident that medical and nursing students are
shortfall in education about hand hygiene. Education about hand hygiene should be initiated
from the first year of their curricula (Srigley et al., 2016).
Patients and healthcare providers are more susceptible to the methicillin resistant
Staphylococcus Aureus (MRSA). Precautions should be taken during hand hygiene because
frequent hand wash is associated with certain adverse events like dryness and irritation.
Successful implementation of the system change in the hospital can be achieved by education
to the staff members. It is evident that less support from the management and insufficient
resources for hand hygiene are the main hurdles for implementing hand hygiene. Scarcity of
resources is mainly evident in the developing countries. Behavioural changes among
healthcare professionals are required for implementing hand hygiene. Education, awareness
and training can bring positive behavioural changes among healthcare professionals. Lack of
adherence to the hand hygiene policy implementation is one of the main reasons identified for
increased infections through hands. Continuous monitoring for successful implementation of
hand hygiene is difficult because observation of hand hygiene is associated with error and
bias. There are more chances of false positive results during evaluation of hand hygiene
implementation programme. There is no validated method available for monitoring hand
hygiene, hence surrogate methods should be used to monitor it. It is necessary to develop
robust method for monitoring hand hygiene. It is difficult to get direct and observable results
in case of hand hygiene (Goldberg, 2017).
2
A1 Problem:
Hand hygiene is a general term which can be used for the activities related to the hand
cleansing. World Health Organization (WHO) published guidelines on hand hygiene which
comprises of scientific data on hand hygiene rationale and practices in health care. Hand
hygiene is required in five instances like prior to touching to the patient, prior to carrying out
aseptic and clean procedures, at the time of risk of exposure to body fluids, after touching
patient and after touching patient’s belongings and surroundings. Dynamic behavioural
change is required for maintaining hand hygiene. Infection prevention and control
programme should be implemented through healthcare related training and education for
maintaining hand hygiene. All the healthcare workers should incorporate hand hygiene as the
integral part of their practice. However, it was evident that medical and nursing students are
shortfall in education about hand hygiene. Education about hand hygiene should be initiated
from the first year of their curricula (Srigley et al., 2016).
Patients and healthcare providers are more susceptible to the methicillin resistant
Staphylococcus Aureus (MRSA). Precautions should be taken during hand hygiene because
frequent hand wash is associated with certain adverse events like dryness and irritation.
Successful implementation of the system change in the hospital can be achieved by education
to the staff members. It is evident that less support from the management and insufficient
resources for hand hygiene are the main hurdles for implementing hand hygiene. Scarcity of
resources is mainly evident in the developing countries. Behavioural changes among
healthcare professionals are required for implementing hand hygiene. Education, awareness
and training can bring positive behavioural changes among healthcare professionals. Lack of
adherence to the hand hygiene policy implementation is one of the main reasons identified for
increased infections through hands. Continuous monitoring for successful implementation of
hand hygiene is difficult because observation of hand hygiene is associated with error and
bias. There are more chances of false positive results during evaluation of hand hygiene
implementation programme. There is no validated method available for monitoring hand
hygiene, hence surrogate methods should be used to monitor it. It is necessary to develop
robust method for monitoring hand hygiene. It is difficult to get direct and observable results
in case of hand hygiene (Goldberg, 2017).
2
A2 Significance of the problem:
Cleaning of hands can be helpful in preventing spread of microorganisms including those are
resistant to antibiotics. It is evident that healthcare professionals clean their hands
approximately 50 % of the times as compared to its requirement. Approximately 0.4 %
patients get infected due to healthcare related microorganisms. Thousands of people die daily
due to infection spread through hand at the time of receiving healthcare services. During
healthcare practices, hands are the most important route of transmission of microorganisms.
In developed countries, approximately 7 % hospitalised patients and 20 % intensive care unit
patients encounter hospital related infections. In developing countries approximately 10 %
hospitalised patient and 30 % intensive care unit patients encounter hospital related
infections.
There is measurable difference among developed and developing countries in terms of
infection due to hands. Patients in the developing countries are more susceptible for infection
as compared to the developing countries. Healthcare providers need to be in constant touch
with the patients which can spread infections to other people. Hand contamination can spread
infection in both direct and indirect way and it is more prevalent in the intensive care unit and
hemodialysis unit. Most of the healthcare workers are following hand decontamination
procedures, however it is evident that there are very less chances of successful
decontamination of the hand. Ideal method for the hand decontamination can be provided
through educational and training programme. Hand hygiene is more significant in healthcare
facility because in healthcare facility hand infection can affect patient health. Health care
providers need to use disinfectant for their hands for at least 100 times in a 12 hrs shift.
Selection of disinfectant is also important for hand hygiene because alcohol based
disinfectants are not useful for few microorganisms like C. difficile. It is evident that there is
progress in promotion of education and training for controlling hand associated infection
hygiene however, there is less progress in monitoring hand hygiene and behavioural changes
for improving hand hygiene. Patients can carry microorganisms to larger population, hence
hand hygiene should be maintained for all type of patients (Winship, and McClunie-Trust,
2016).
A3: Current practice :
Hand hygiene can be maintained by implementing multi-modal strategies. Hand hygiene can
be maintained by promoting its importance. It can be achieved through in-service education,
3
Cleaning of hands can be helpful in preventing spread of microorganisms including those are
resistant to antibiotics. It is evident that healthcare professionals clean their hands
approximately 50 % of the times as compared to its requirement. Approximately 0.4 %
patients get infected due to healthcare related microorganisms. Thousands of people die daily
due to infection spread through hand at the time of receiving healthcare services. During
healthcare practices, hands are the most important route of transmission of microorganisms.
In developed countries, approximately 7 % hospitalised patients and 20 % intensive care unit
patients encounter hospital related infections. In developing countries approximately 10 %
hospitalised patient and 30 % intensive care unit patients encounter hospital related
infections.
There is measurable difference among developed and developing countries in terms of
infection due to hands. Patients in the developing countries are more susceptible for infection
as compared to the developing countries. Healthcare providers need to be in constant touch
with the patients which can spread infections to other people. Hand contamination can spread
infection in both direct and indirect way and it is more prevalent in the intensive care unit and
hemodialysis unit. Most of the healthcare workers are following hand decontamination
procedures, however it is evident that there are very less chances of successful
decontamination of the hand. Ideal method for the hand decontamination can be provided
through educational and training programme. Hand hygiene is more significant in healthcare
facility because in healthcare facility hand infection can affect patient health. Health care
providers need to use disinfectant for their hands for at least 100 times in a 12 hrs shift.
Selection of disinfectant is also important for hand hygiene because alcohol based
disinfectants are not useful for few microorganisms like C. difficile. It is evident that there is
progress in promotion of education and training for controlling hand associated infection
hygiene however, there is less progress in monitoring hand hygiene and behavioural changes
for improving hand hygiene. Patients can carry microorganisms to larger population, hence
hand hygiene should be maintained for all type of patients (Winship, and McClunie-Trust,
2016).
A3: Current practice :
Hand hygiene can be maintained by implementing multi-modal strategies. Hand hygiene can
be maintained by promoting its importance. It can be achieved through in-service education,
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
information leaflets, workshops and lectures. Hand hygiene adherence for the healthcare staff
should be maintained and rewards should be given to the staff with highest adherence rate for
hand hygiene. The Occupational Safety and Health Administration (OSHA) guidelines stated
to wear gloves during the all the activities related to the patients care. It is evident that freshly
applied nail polish can prevent growth of microorganisms, hence prior to nursing intervention
nail polish can be applied. National policies and plans should be implemented. Facility based
guidelines and laws should be prepared for maintaining hand hygiene and these should be
strictly implemented. Management of healthcare facility should allocate special budget to
prevent hand originated infection. Surveillance of resistant microorganisms should be
improved. Alcohol based hand-rub should be provided to all the health workers at the place
of practice. There should be monitoring and feedback on compliance of hand hygiene. Visual
reminders about hand hygiene should be displayed at the workplace. Organisational culture
should be created for maintaining hand hygiene at the workplace (Winship, and McClunie-
Trust, 2016).
A4: Impact:
Hand hygiene education programme would be helpful in bringing behavioural changes
among healthcare staff. Education about the hand hygiene can improve quality standard of
the healthcare facility. It would be helpful in improving overall healthcare services to the
patients. It would be helpful in reducing hospital acquired and blood borne infections. It
would be helpful in improving ranking of the healthcare facilities as compared to other
competitive healthcare facilities. It would also be helpful in developing healthy and safety
culture in the facility. Hence, preferences of the patients for the hospital would be increased.
Along with the health impact, hand hygiene can also affect financial condition of patient and
hospital. Catheter associated infection like methicillin-resistant Staphylococcus aureus
(MRSA) may cost upto US$ 38 000 per episode. Infections due to infected hand can lead to
readmissions to the hospital. It can lead to financial burden both to hospitals and to the
patient. Hospital need to make separate arrangement for the infected patients, which can have
extra financial burden on the hospital. It would be helpful in developing protocols for hand
hygeine and standardising the methods for hand hygiene. It would also reduce risk of
infection to the healthcare workers, hence it would be helpful in improving productivity of
the organisation. Implementation of hand hygiene practices would also be helpful in
improving overall infection control strategy of the hospital. Education programme would
also be useful in developing leadership qualities for infection control and monitoring staff for
4
should be maintained and rewards should be given to the staff with highest adherence rate for
hand hygiene. The Occupational Safety and Health Administration (OSHA) guidelines stated
to wear gloves during the all the activities related to the patients care. It is evident that freshly
applied nail polish can prevent growth of microorganisms, hence prior to nursing intervention
nail polish can be applied. National policies and plans should be implemented. Facility based
guidelines and laws should be prepared for maintaining hand hygiene and these should be
strictly implemented. Management of healthcare facility should allocate special budget to
prevent hand originated infection. Surveillance of resistant microorganisms should be
improved. Alcohol based hand-rub should be provided to all the health workers at the place
of practice. There should be monitoring and feedback on compliance of hand hygiene. Visual
reminders about hand hygiene should be displayed at the workplace. Organisational culture
should be created for maintaining hand hygiene at the workplace (Winship, and McClunie-
Trust, 2016).
A4: Impact:
Hand hygiene education programme would be helpful in bringing behavioural changes
among healthcare staff. Education about the hand hygiene can improve quality standard of
the healthcare facility. It would be helpful in improving overall healthcare services to the
patients. It would be helpful in reducing hospital acquired and blood borne infections. It
would be helpful in improving ranking of the healthcare facilities as compared to other
competitive healthcare facilities. It would also be helpful in developing healthy and safety
culture in the facility. Hence, preferences of the patients for the hospital would be increased.
Along with the health impact, hand hygiene can also affect financial condition of patient and
hospital. Catheter associated infection like methicillin-resistant Staphylococcus aureus
(MRSA) may cost upto US$ 38 000 per episode. Infections due to infected hand can lead to
readmissions to the hospital. It can lead to financial burden both to hospitals and to the
patient. Hospital need to make separate arrangement for the infected patients, which can have
extra financial burden on the hospital. It would be helpful in developing protocols for hand
hygeine and standardising the methods for hand hygiene. It would also reduce risk of
infection to the healthcare workers, hence it would be helpful in improving productivity of
the organisation. Implementation of hand hygiene practices would also be helpful in
improving overall infection control strategy of the hospital. Education programme would
also be useful in developing leadership qualities for infection control and monitoring staff for
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
implementing hand hygiene. It would be helpful in performing audit of hand hygiene and
getting feedback for its implementation. It facilitates sustainable changes for implementing
hand hygiene programme in the hospital (Srigley et al., 2016).
B
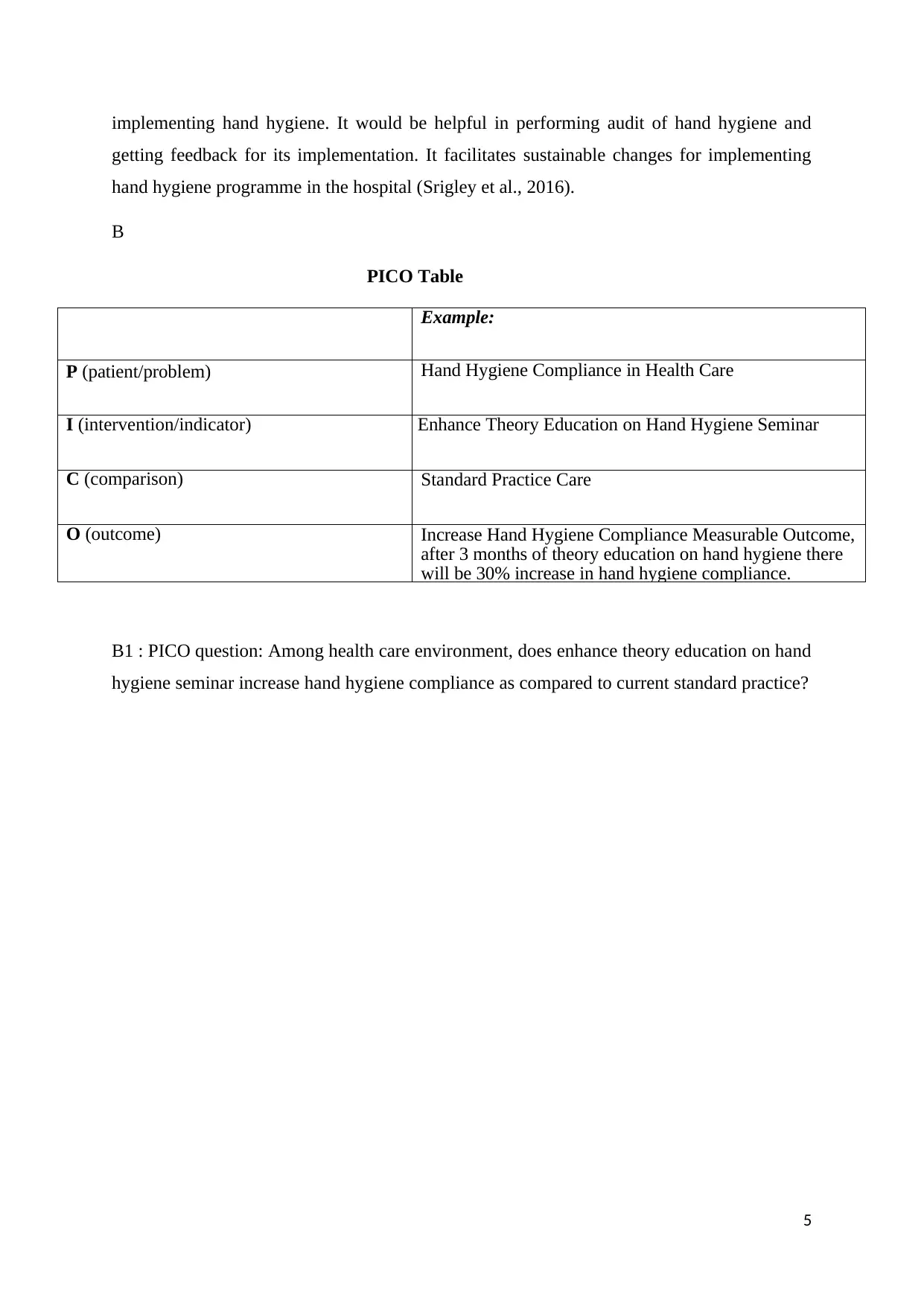
PICO Table
Example:
P (patient/problem) Hand Hygiene Compliance in Health Care
I (intervention/indicator) Enhance Theory Education on Hand Hygiene Seminar
C (comparison) Standard Practice Care
O (outcome) Increase Hand Hygiene Compliance Measurable Outcome,
after 3 months of theory education on hand hygiene there
will be 30% increase in hand hygiene compliance.
B1 : PICO question: Among health care environment, does enhance theory education on hand
hygiene seminar increase hand hygiene compliance as compared to current standard practice?
5
getting feedback for its implementation. It facilitates sustainable changes for implementing
hand hygiene programme in the hospital (Srigley et al., 2016).
B
PICO Table
Example:
P (patient/problem) Hand Hygiene Compliance in Health Care
I (intervention/indicator) Enhance Theory Education on Hand Hygiene Seminar
C (comparison) Standard Practice Care
O (outcome) Increase Hand Hygiene Compliance Measurable Outcome,
after 3 months of theory education on hand hygiene there
will be 30% increase in hand hygiene compliance.
B1 : PICO question: Among health care environment, does enhance theory education on hand
hygiene seminar increase hand hygiene compliance as compared to current standard practice?
5
C
Articles related to hand hygiene interventions and education were searched. Hand hygiene
interventions for healthcare staff were selected. Interventions were selected which were
directed towards prevention of spread of infection to patients. Comparators in the
interventions were either placebo or comparison among standard handwashing procedure
with soap and different hand sanitizers. Educational programme for hand hygiene carried out
at hospital facilities for the healthcare staff were selected. Targeted outcomes for the selection
of the articles were respiratory tract infection, gastrointestinal tract infection, absenteeism
rate, hospital readmissions, changes in behaviour, attitude, belief and knowledge of
healthcare staff. More focus was given to healthcare staff outcome.
C1 : Key words for search strategy were divided in three classes like hand hygiene,
healthcare facilities and study type. Date restrictions were not applied however, language for
articles was restricted to English. Data from the studies was extracted by using a standard
template. Extracted data comprise of study details; intervention description, study
recruitment, random allocation, study baseline data, follow-up, process evaluation, outcomes
and analysis. Following were the key words used for the search strategy : handwashing or
hand washing, hand or hands, health education, health education and hand or hands, hand or
hands hygiene, hand or hands and cleansing or cleaning, hand antisepsis, hand or hands
disinfect, communicable disease control, communicable disease control and hand or hands,
infection control and hand or hands, soap or soaps, soap or soaps and hand or hands, alcohol
gel, anti-microbial gel, disinfectant gel, sanitizer, infection control and randomized controlled
trial or infection control and controlled clinical trial, hand hygiene intervention or hand
hygiene experiment, hand hygiene and nursing research or clinical nursing research or
nursing evaluation research or nursing methodology research.
C2 : Search strategy was applied under four categories like identification, screening,
eligibility and inclusion. 6256 articles were found in the electronic database searches in the
identification step. These 6256 articles comprise of research articles, editorials and review
articles. Information in these articles comprise of research evidence, quality improvement,
national and international practice guidelines, WHO guidelines and expert opinion. From
these 6256 articles, 1868 duplicate articles were removed. After removing duplicate articles,
4388 articles were screened for eligibility. Out of 4388 articles, 4122 articles were excluded
based on the title of the article. These articles were removed because these were editorials,
guidelines and expert opinion. Remaining 266 articles were screened for abstracts. These
6
Articles related to hand hygiene interventions and education were searched. Hand hygiene
interventions for healthcare staff were selected. Interventions were selected which were
directed towards prevention of spread of infection to patients. Comparators in the
interventions were either placebo or comparison among standard handwashing procedure
with soap and different hand sanitizers. Educational programme for hand hygiene carried out
at hospital facilities for the healthcare staff were selected. Targeted outcomes for the selection
of the articles were respiratory tract infection, gastrointestinal tract infection, absenteeism
rate, hospital readmissions, changes in behaviour, attitude, belief and knowledge of
healthcare staff. More focus was given to healthcare staff outcome.
C1 : Key words for search strategy were divided in three classes like hand hygiene,
healthcare facilities and study type. Date restrictions were not applied however, language for
articles was restricted to English. Data from the studies was extracted by using a standard
template. Extracted data comprise of study details; intervention description, study
recruitment, random allocation, study baseline data, follow-up, process evaluation, outcomes
and analysis. Following were the key words used for the search strategy : handwashing or
hand washing, hand or hands, health education, health education and hand or hands, hand or
hands hygiene, hand or hands and cleansing or cleaning, hand antisepsis, hand or hands
disinfect, communicable disease control, communicable disease control and hand or hands,
infection control and hand or hands, soap or soaps, soap or soaps and hand or hands, alcohol
gel, anti-microbial gel, disinfectant gel, sanitizer, infection control and randomized controlled
trial or infection control and controlled clinical trial, hand hygiene intervention or hand
hygiene experiment, hand hygiene and nursing research or clinical nursing research or
nursing evaluation research or nursing methodology research.
C2 : Search strategy was applied under four categories like identification, screening,
eligibility and inclusion. 6256 articles were found in the electronic database searches in the
identification step. These 6256 articles comprise of research articles, editorials and review
articles. Information in these articles comprise of research evidence, quality improvement,
national and international practice guidelines, WHO guidelines and expert opinion. From
these 6256 articles, 1868 duplicate articles were removed. After removing duplicate articles,
4388 articles were screened for eligibility. Out of 4388 articles, 4122 articles were excluded
based on the title of the article. These articles were removed because these were editorials,
guidelines and expert opinion. Remaining 266 articles were screened for abstracts. These
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
remaining articles comprise of randomised controlled trials and informative review articles.
Out of these 266 abstracts, 212 abstracts were excluded. Remaining 54 articles were included
in the full paper screening. Out of these 54 full text articles, 47 were excluded and finally 5
research articles and 2 non-research articles were selected.
C2a :
Research article : Shen et al., (2017), implemented quasi experimental study using
questionaries’ to evaluate implementation of WHO multimodal hand hygiene strategy. Hand
hygiene multimodal strategy was implemented comprising of different factors like
environmental, individual and management. Hand hygiene compliance and correctness of the
health workers for following hand hygiene were the evaluated outcomes in this research. This
study was conducted in the hospital of traditional Chinese medicine. 553 participants were
participated in this study. After implementation of the multimodal strategy, there was
statistically significant improvement in the compliance and correctness of hand hygiene as
compared to the baseline. Compliance was met for all other criterias except “after body fluid
exposure risk” and “after touching patient surroundings”’. Compliance was more for doctors
as compared to the nurses and other health workers.
Research article : O’Donoghue et al., (2016), implemented quasi experimental study to
evaluate educational programme for hand hygiene. Questionnaires comprised of knowledge
and attitude of healthcare professionals about hand hygiene. This study was implemented in
the radiography department. 76 radiographers, 17 nurses, and 9 healthcare assistants were
participated in this study. Educational intervention was provided for the duration of 2 months
in the form of talks and visual aids. Hand hygiene compliance was observed for 3 weeks for
all these participants. Educational intervention programme proved useful in improving hand
hygiene compliance by approximately 50 % as compared to the compliance prior to the
educational intervention.
Non - Research article : Whitcomb, (2014) implemented quality improvement programme
with the objective to bring BSN students of school of nursing with hospital’s target of 90 %
hand hygiene compliance. Data was collected in the form of direct observations and missed
opportunities. From the study, it is evident that implementation of multidimensional quality
improvement programme can be helpful in improving hand hygiene quality of nursing school
students.
Non - Research article : Glodberg, (2017) focused on guidelines of hand hygiene. Association
7
Out of these 266 abstracts, 212 abstracts were excluded. Remaining 54 articles were included
in the full paper screening. Out of these 54 full text articles, 47 were excluded and finally 5
research articles and 2 non-research articles were selected.
C2a :
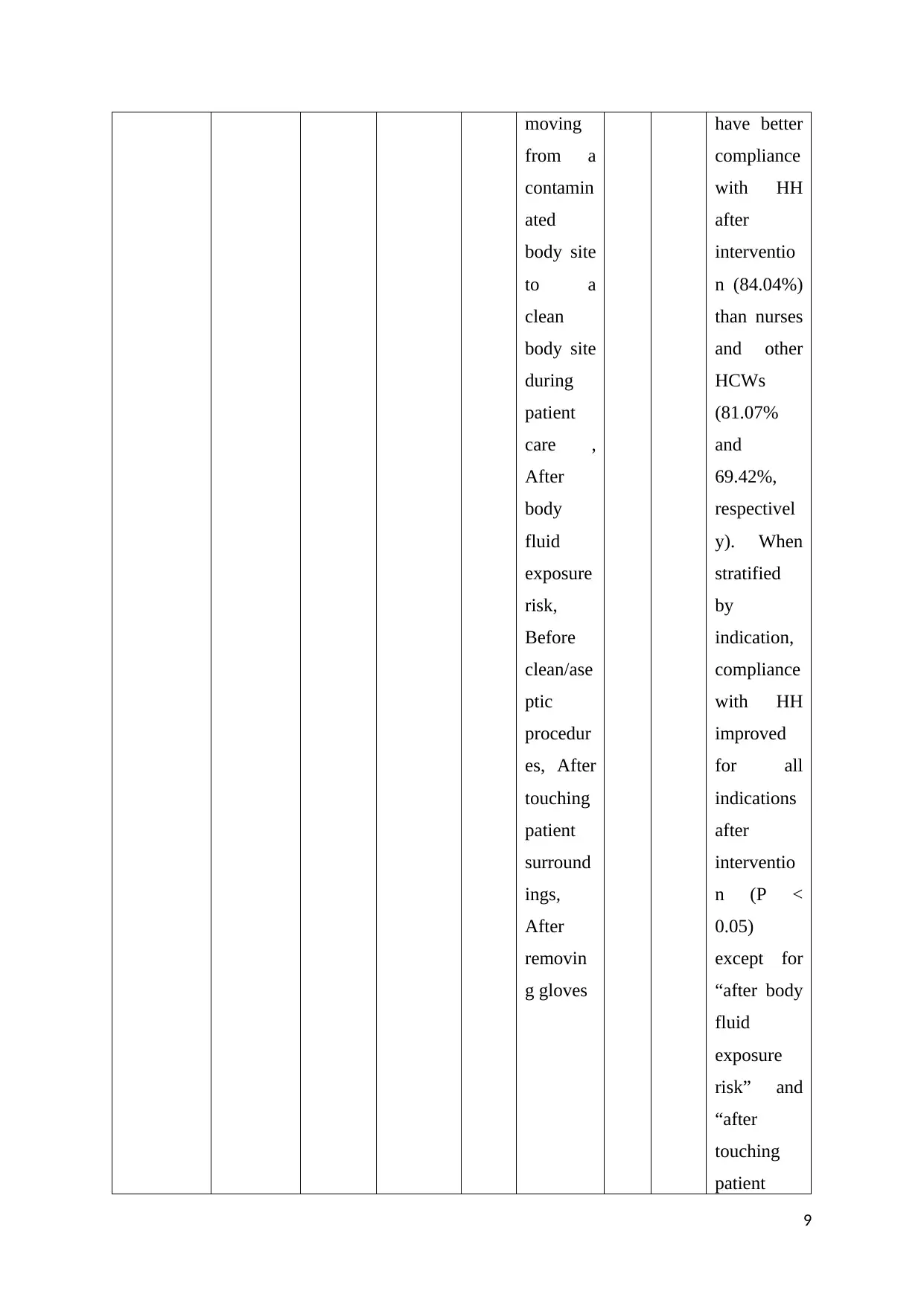
Research article : Shen et al., (2017), implemented quasi experimental study using
questionaries’ to evaluate implementation of WHO multimodal hand hygiene strategy. Hand
hygiene multimodal strategy was implemented comprising of different factors like
environmental, individual and management. Hand hygiene compliance and correctness of the
health workers for following hand hygiene were the evaluated outcomes in this research. This
study was conducted in the hospital of traditional Chinese medicine. 553 participants were
participated in this study. After implementation of the multimodal strategy, there was
statistically significant improvement in the compliance and correctness of hand hygiene as
compared to the baseline. Compliance was met for all other criterias except “after body fluid
exposure risk” and “after touching patient surroundings”’. Compliance was more for doctors
as compared to the nurses and other health workers.
Research article : O’Donoghue et al., (2016), implemented quasi experimental study to
evaluate educational programme for hand hygiene. Questionnaires comprised of knowledge
and attitude of healthcare professionals about hand hygiene. This study was implemented in
the radiography department. 76 radiographers, 17 nurses, and 9 healthcare assistants were
participated in this study. Educational intervention was provided for the duration of 2 months
in the form of talks and visual aids. Hand hygiene compliance was observed for 3 weeks for
all these participants. Educational intervention programme proved useful in improving hand
hygiene compliance by approximately 50 % as compared to the compliance prior to the
educational intervention.
Non - Research article : Whitcomb, (2014) implemented quality improvement programme
with the objective to bring BSN students of school of nursing with hospital’s target of 90 %
hand hygiene compliance. Data was collected in the form of direct observations and missed
opportunities. From the study, it is evident that implementation of multidimensional quality
improvement programme can be helpful in improving hand hygiene quality of nursing school
students.
Non - Research article : Glodberg, (2017) focused on guidelines of hand hygiene. Association
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
of periOperative Registered Nurses (AORN) guidelines give information about the hand
hygiene, surgical hand antisepsis, nail polish, artificial nails, and skin care. According to
these guidelines perioperative personal make aware of the hand hygiene and surgical hand
antisepsis. Patients undergoing surgery and invasive procedure might be at higher risk of
infection and they come in close contact with the perioperative nurses. Hence, perioperative
nurse should be aware if these guidelines, implement it and incorporate these guidelines
while preparing policies and procedures for hand hygiene.
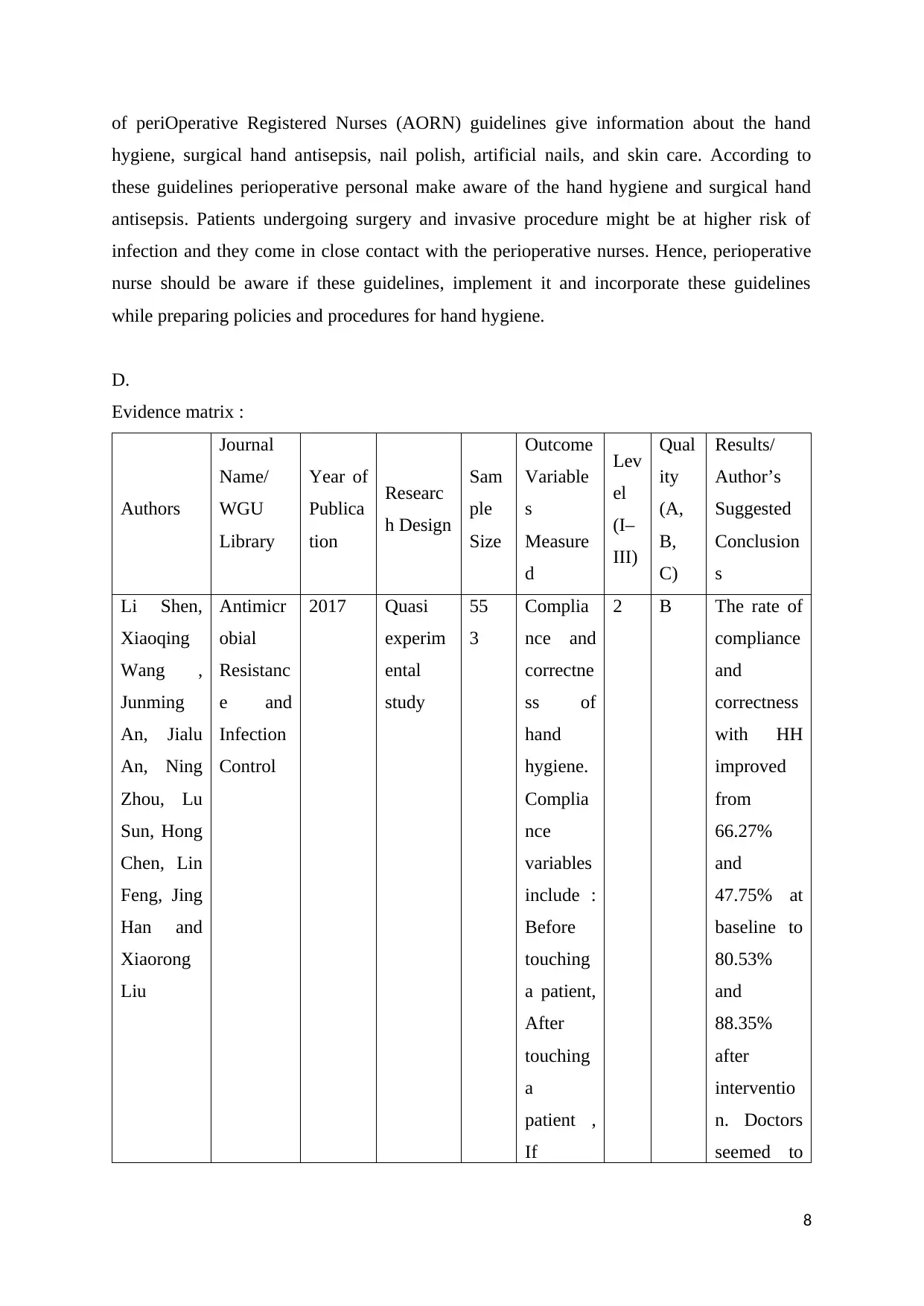
D.
Evidence matrix :
Authors
Journal
Name/
WGU
Library
Year of
Publica
tion
Researc
h Design
Sam
ple
Size
Outcome
Variable
s
Measure
d
Lev
el
(I–
III)
Qual
ity
(A,
B,
C)
Results/
Author’s
Suggested
Conclusion
s
Li Shen,
Xiaoqing
Wang ,
Junming
An, Jialu
An, Ning
Zhou, Lu
Sun, Hong
Chen, Lin
Feng, Jing
Han and
Xiaorong
Liu
Antimicr
obial
Resistanc
e and
Infection
Control
2017 Quasi
experim
ental
study
55
3
Complia
nce and
correctne
ss of
hand
hygiene.
Complia
nce
variables
include :
Before
touching
a patient,
After
touching
a
patient ,
If
2 B The rate of
compliance
and
correctness
with HH
improved
from
66.27%
and
47.75% at
baseline to
80.53%
and
88.35%
after
interventio
n. Doctors
seemed to
8
hygiene, surgical hand antisepsis, nail polish, artificial nails, and skin care. According to
these guidelines perioperative personal make aware of the hand hygiene and surgical hand
antisepsis. Patients undergoing surgery and invasive procedure might be at higher risk of
infection and they come in close contact with the perioperative nurses. Hence, perioperative
nurse should be aware if these guidelines, implement it and incorporate these guidelines
while preparing policies and procedures for hand hygiene.
D.
Evidence matrix :
Authors
Journal
Name/
WGU
Library
Year of
Publica
tion
Researc
h Design
Sam
ple
Size
Outcome
Variable
s
Measure
d
Lev
el
(I–
III)
Qual
ity
(A,
B,
C)
Results/
Author’s
Suggested
Conclusion
s
Li Shen,
Xiaoqing
Wang ,
Junming
An, Jialu
An, Ning
Zhou, Lu
Sun, Hong
Chen, Lin
Feng, Jing
Han and
Xiaorong
Liu
Antimicr
obial
Resistanc
e and
Infection
Control
2017 Quasi
experim
ental
study
55
3
Complia
nce and
correctne
ss of
hand
hygiene.
Complia
nce
variables
include :
Before
touching
a patient,
After
touching
a
patient ,
If
2 B The rate of
compliance
and
correctness
with HH
improved
from
66.27%
and
47.75% at
baseline to
80.53%
and
88.35%
after
interventio
n. Doctors
seemed to
8
moving
from a
contamin
ated
body site
to a
clean
body site
during
patient
care ,
After
body
fluid
exposure
risk,
Before
clean/ase
ptic
procedur
es, After
touching
patient
surround
ings,
After
removin
g gloves
have better
compliance
with HH
after
interventio
n (84.04%)
than nurses
and other
HCWs
(81.07%
and
69.42%,
respectivel
y). When
stratified
by
indication,
compliance
with HH
improved
for all
indications
after
interventio
n (P <
0.05)
except for
“after body
fluid
exposure
risk” and
“after
touching
patient
9
from a
contamin
ated
body site
to a
clean
body site
during
patient
care ,
After
body
fluid
exposure
risk,
Before
clean/ase
ptic
procedur
es, After
touching
patient
surround
ings,
After
removin
g gloves
have better
compliance
with HH
after
interventio
n (84.04%)
than nurses
and other
HCWs
(81.07%
and
69.42%,
respectivel
y). When
stratified
by
indication,
compliance
with HH
improved
for all
indications
after
interventio
n (P <
0.05)
except for
“after body
fluid
exposure
risk” and
“after
touching
patient
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
surroundin
gs”.
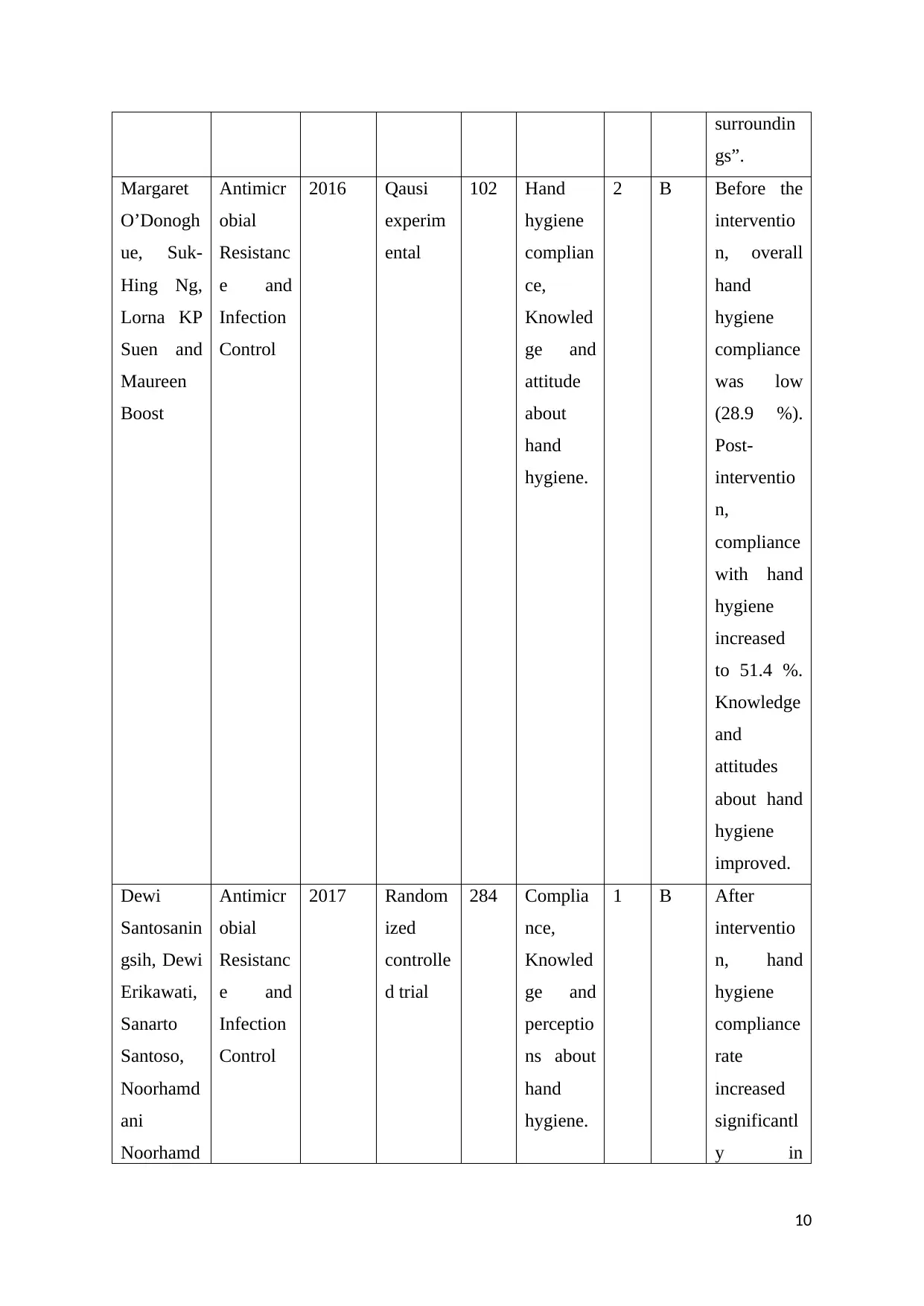
Margaret
O’Donogh
ue, Suk-
Hing Ng,
Lorna KP
Suen and
Maureen
Boost
Antimicr
obial
Resistanc
e and
Infection
Control
2016 Qausi
experim
ental
102 Hand
hygiene
complian
ce,
Knowled
ge and
attitude
about
hand
hygiene.
2 B Before the
interventio
n, overall
hand
hygiene
compliance
was low
(28.9 %).
Post-
interventio
n,
compliance
with hand
hygiene
increased
to 51.4 %.
Knowledge
and
attitudes
about hand
hygiene
improved.
Dewi
Santosanin
gsih, Dewi
Erikawati,
Sanarto
Santoso,
Noorhamd
ani
Noorhamd
Antimicr
obial
Resistanc
e and
Infection
Control
2017 Random
ized
controlle
d trial
284 Complia
nce,
Knowled
ge and
perceptio
ns about
hand
hygiene.
1 B After
interventio
n, hand
hygiene
compliance
rate
increased
significantl
y in
10
gs”.
Margaret
O’Donogh
ue, Suk-
Hing Ng,
Lorna KP
Suen and
Maureen
Boost
Antimicr
obial
Resistanc
e and
Infection
Control
2016 Qausi
experim
ental
102 Hand
hygiene
complian
ce,
Knowled
ge and
attitude
about
hand
hygiene.
2 B Before the
interventio
n, overall
hand
hygiene
compliance
was low
(28.9 %).
Post-
interventio
n,
compliance
with hand
hygiene
increased
to 51.4 %.
Knowledge
and
attitudes
about hand
hygiene
improved.
Dewi
Santosanin
gsih, Dewi
Erikawati,
Sanarto
Santoso,
Noorhamd
ani
Noorhamd
Antimicr
obial
Resistanc
e and
Infection
Control
2017 Random
ized
controlle
d trial
284 Complia
nce,
Knowled
ge and
perceptio
ns about
hand
hygiene.
1 B After
interventio
n, hand
hygiene
compliance
rate
increased
significantl
y in
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ani et al. pediatrics,
internal
medicine
and
obstetrics-
gynecology
. The
nurses’
incorrect
use of hand
rub while
wearing
gloves
increased.
Average
knowledge
score also
improved.
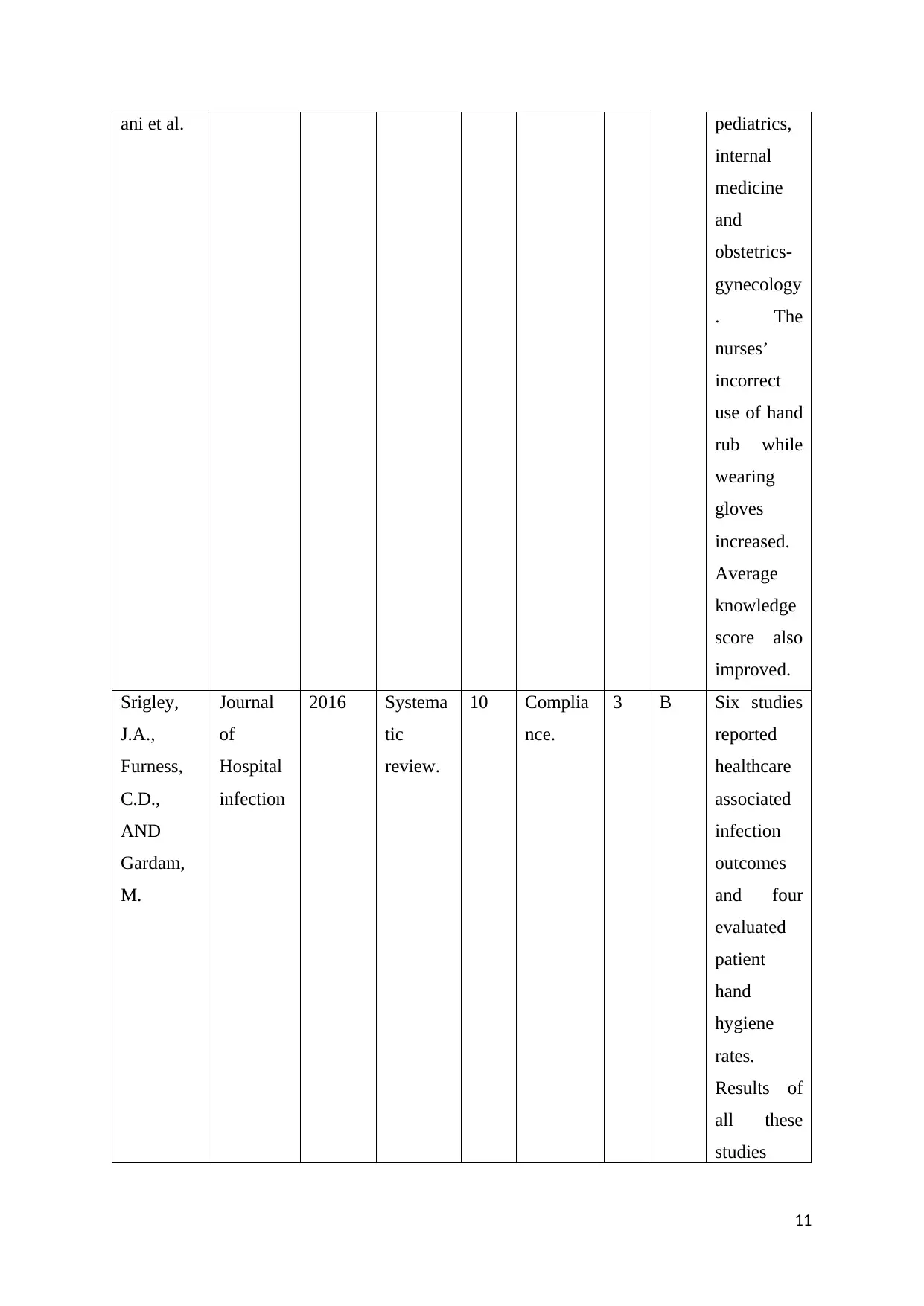
Srigley,
J.A.,
Furness,
C.D.,
AND
Gardam,
M.
Journal
of
Hospital
infection
2016 Systema
tic
review.
10 Complia
nce.
3 B Six studies
reported
healthcare
associated
infection
outcomes
and four
evaluated
patient
hand
hygiene
rates.
Results of
all these
studies
11
internal
medicine
and
obstetrics-
gynecology
. The
nurses’
incorrect
use of hand
rub while
wearing
gloves
increased.
Average
knowledge
score also
improved.
Srigley,
J.A.,
Furness,
C.D.,
AND
Gardam,
M.
Journal
of
Hospital
infection
2016 Systema
tic
review.
10 Complia
nce.
3 B Six studies
reported
healthcare
associated
infection
outcomes
and four
evaluated
patient
hand
hygiene
rates.
Results of
all these
studies
11
were
moderate
and risk to
bias.
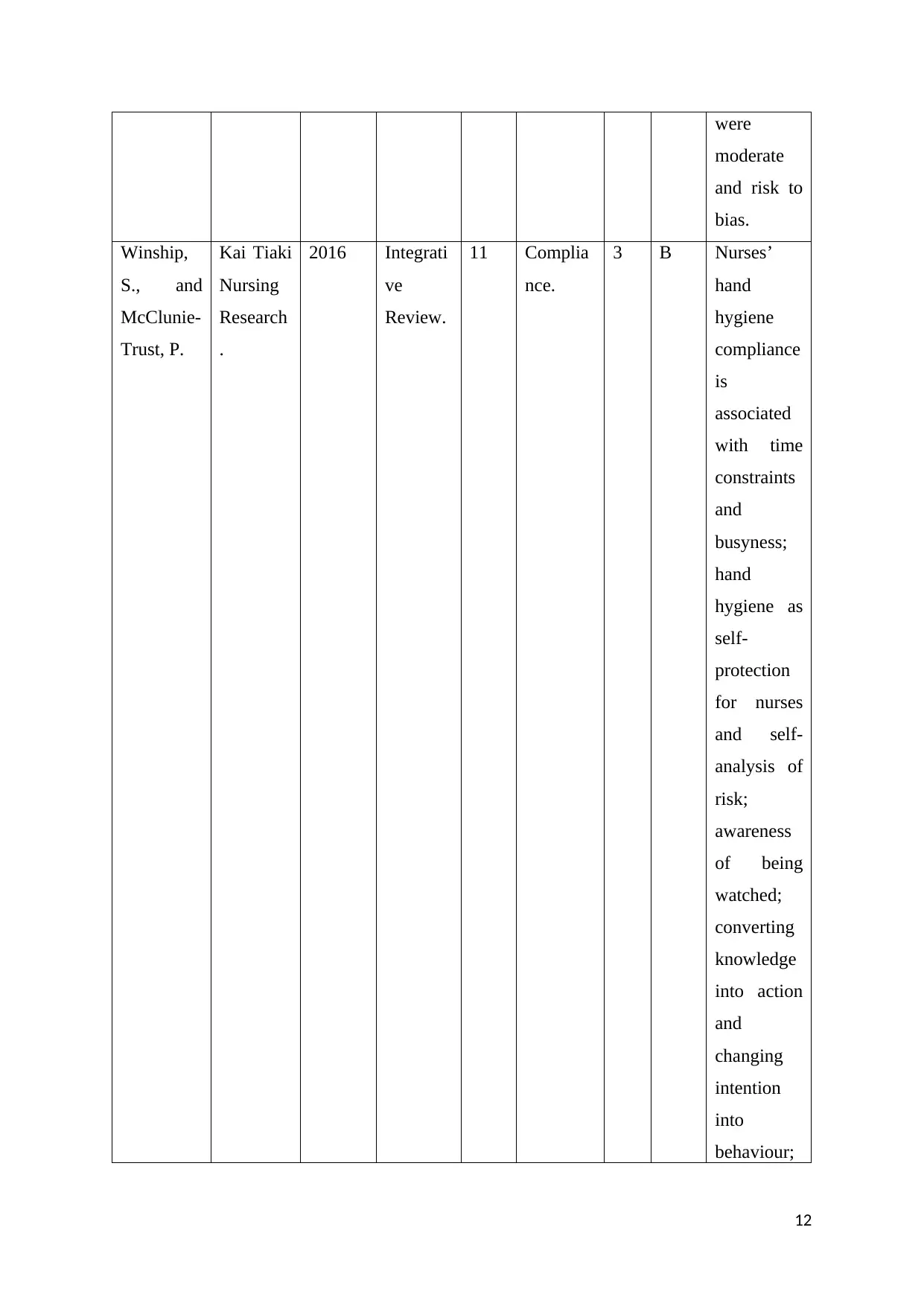
Winship,
S., and
McClunie-
Trust, P.
Kai Tiaki
Nursing
Research
.
2016 Integrati
ve
Review.
11 Complia
nce.
3 B Nurses’
hand
hygiene
compliance
is
associated
with time
constraints
and
busyness;
hand
hygiene as
self-
protection
for nurses
and self-
analysis of
risk;
awareness
of being
watched;
converting
knowledge
into action
and
changing
intention
into
behaviour;
12
moderate
and risk to
bias.
Winship,
S., and
McClunie-
Trust, P.
Kai Tiaki
Nursing
Research
.
2016 Integrati
ve
Review.
11 Complia
nce.
3 B Nurses’
hand
hygiene
compliance
is
associated
with time
constraints
and
busyness;
hand
hygiene as
self-
protection
for nurses
and self-
analysis of
risk;
awareness
of being
watched;
converting
knowledge
into action
and
changing
intention
into
behaviour;
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





