The Hartford Institute: Geriatric Depression Scale in Nursing Care
VerifiedAdded on 2023/04/25
|2
|1486
|73
Practical Assignment
AI Summary
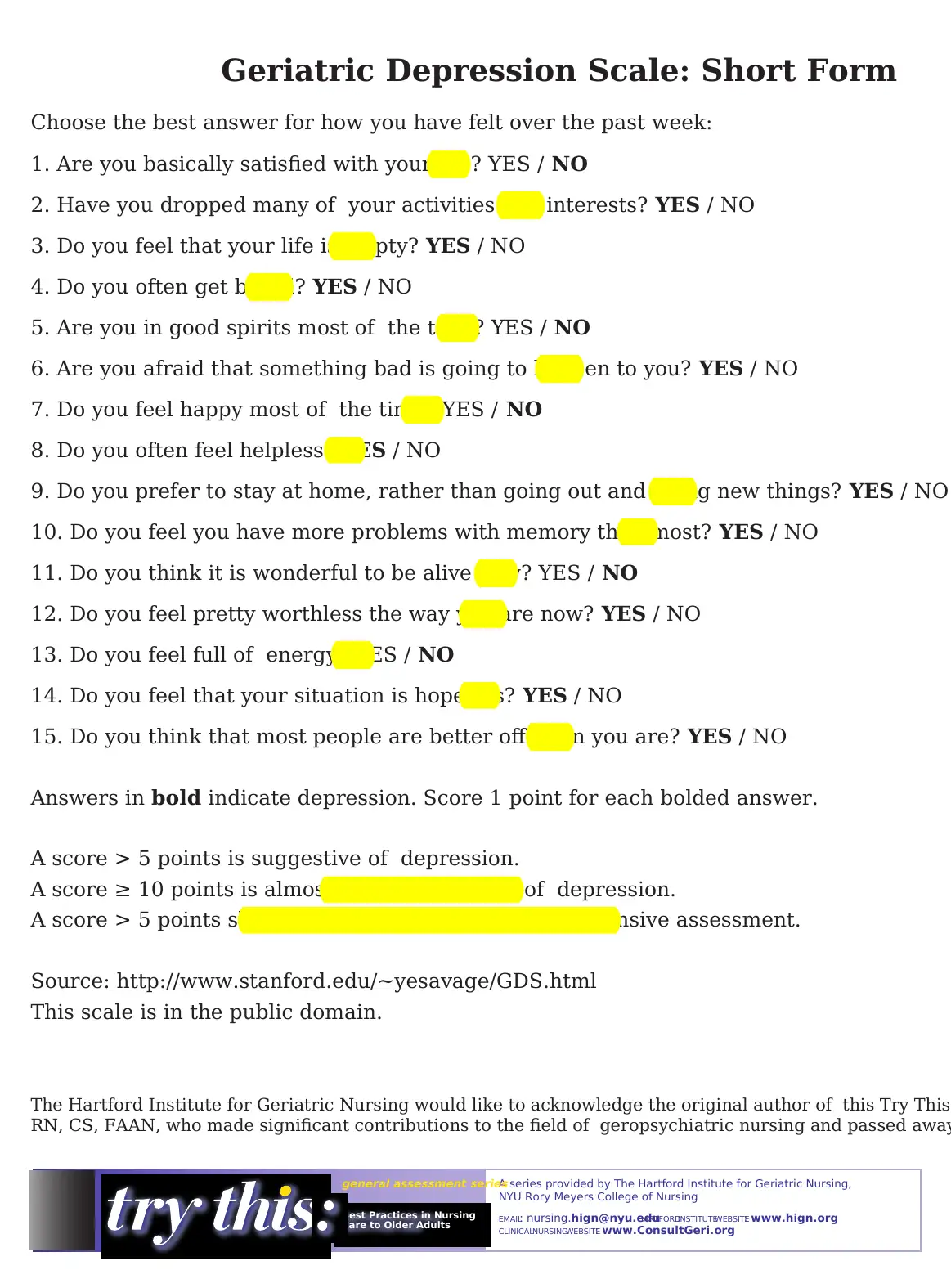
This document presents the Geriatric Depression Scale (GDS), a crucial tool for assessing depression in older adults. Developed by Yesavage et al., the GDS is a brief questionnaire designed to identify depressive symptoms in various settings, including community, acute care, and long-term care. The document highlights the GDS's strengths, such as its ease of use and established validity and reliability, while acknowledging its limitations, including its role as a screening tool rather than a diagnostic interview. It provides detailed instructions on scoring and interpreting the GDS, differentiating between normal, mild, moderate, and severe depression levels. Furthermore, the document emphasizes the importance of prompt intervention and treatment for depression, suggesting the GDS as a valuable tool for monitoring patients over time and guiding further psychological assessment when necessary. The resource includes the GDS Short Form and references to related materials and websites, underscoring its value for nursing professionals and students seeking to improve their geriatric care practices.
1 out of 2

![[object Object]](/_next/static/media/star-bottom.7253800d.svg)