Assessment and Care Plan for Patient with Cardiovascular Issues
VerifiedAdded on 2023/06/07
|15
|4343
|120
Report
AI Summary
This report presents a focused health assessment and care plan for a 64-year-old male patient, Rainey, who presented with flu-like symptoms and was later diagnosed with hypertension, dyslipidemia, and ultimately, a ST-elevation myocardial infarction (STEMI). The report begins with a detailed health history, including family history of heart disease and modifiable risk factors such as a sedentary lifestyle, poor diet, and obesity. The focused assessment includes cardiovascular, respiratory, and pain assessments, with specific questions and techniques outlined. The pathophysiology of the myocardial infarction is explained, including the role of atherosclerosis, risk factors, and the progression of the disease. Finally, the report outlines priority nursing interventions for acute pain, decreased cardiac output, ineffective tissue perfusion, anxiety, excess fluid volume, and activity intolerance, emphasizing evidence-based strategies to optimize patient outcomes. This analysis highlights the importance of comprehensive assessment and tailored care planning in managing cardiovascular disease.

Running Header: FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING 1
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING
Student’s name
Course
Institutional affiliation
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING
Student’s name
Course
Institutional affiliation
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING 2
Introduction
Health assessment through health history and examination is the cornerstone of nursing
diagnosis. Through a focused health assessment, proper diagnosis can be made, augmented by
various investigations. Nursing interventions can be formulated following identification of
priority issues in the care of the patient. The current paper is a discussion on the focused health
assessment and care plan of a patient, Rainey. The sequence of proposed assessment will be
discussed with an emphasis on the specific questions that should be asked and how they guide
the assessment. The findings of the health history and focused assessment will then be related to
the underlying disease pathophysiology. With the outline of the problem identified, evidence-
based nursing interventions will be discussed.
Health history
The case study refers to Rainey, a 64-year-old man of Maori descent. He had presented to
the GP with flu-like symptoms and on further evaluation found to have a hypertension of
160/100 mmHg. On follow-up a few days, he still had a hypertension of 160/100 and deranged
labs with a high serum cholesterol of 7.2 mmol/L, a high LDL of 6.2, a low HDL of 0.7 and a
high triglyceride level of 5.9 mmol/L. He was discharged on medication only to present three
months later with severe, crushing chest pain, radiating to the neck and jaw. Further inquiry at
the emergency department revealed that he had been experiencing similar episodes for the past
three months and the episodes were provoked by exercise lasting for up to 15 minutes. Relevant
family history shows a family history of heart disease with both parents dying in their 60’s due to
heart attacks, two of his four brothers had heart attacks and high blood pressure, and his
remaining uncle had two heart attacks and a stroke. His lifestyle is sedentary with a diet high in
sugars and fats. He is obese with a BMI of 31 Kg/m2 and a waist circumference of 101cm. An
Introduction
Health assessment through health history and examination is the cornerstone of nursing
diagnosis. Through a focused health assessment, proper diagnosis can be made, augmented by
various investigations. Nursing interventions can be formulated following identification of
priority issues in the care of the patient. The current paper is a discussion on the focused health
assessment and care plan of a patient, Rainey. The sequence of proposed assessment will be
discussed with an emphasis on the specific questions that should be asked and how they guide
the assessment. The findings of the health history and focused assessment will then be related to
the underlying disease pathophysiology. With the outline of the problem identified, evidence-
based nursing interventions will be discussed.
Health history
The case study refers to Rainey, a 64-year-old man of Maori descent. He had presented to
the GP with flu-like symptoms and on further evaluation found to have a hypertension of
160/100 mmHg. On follow-up a few days, he still had a hypertension of 160/100 and deranged
labs with a high serum cholesterol of 7.2 mmol/L, a high LDL of 6.2, a low HDL of 0.7 and a
high triglyceride level of 5.9 mmol/L. He was discharged on medication only to present three
months later with severe, crushing chest pain, radiating to the neck and jaw. Further inquiry at
the emergency department revealed that he had been experiencing similar episodes for the past
three months and the episodes were provoked by exercise lasting for up to 15 minutes. Relevant
family history shows a family history of heart disease with both parents dying in their 60’s due to
heart attacks, two of his four brothers had heart attacks and high blood pressure, and his
remaining uncle had two heart attacks and a stroke. His lifestyle is sedentary with a diet high in
sugars and fats. He is obese with a BMI of 31 Kg/m2 and a waist circumference of 101cm. An
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING 3
ECG done showed ST elevation. Serum markers were done and the results showed a slightly
decreased creatine kinase but grossly increased troponin I and T. A diagnosis of ST-elevation
myocardial infarction was made and coronary angioplasty with stenting done. He was discharged
to the ward for further monitoring and assessment.
Focused assessment
The sequence of assessment in this patient should include a cardiovascular assessment,
respiratory assessment and pain assessment (LeMone et al., 2015). This is a patient with an
established cardiovascular pathology presenting with chest pain. A cardiovascular assessment
with measurement of vital signs is therefore warranted (Glynn & Drake, 2017). Presentation of
chest pain and the close correlation between the respiratory system and cardiac pathology also
make a focused respiratory assessment needed (Glynn & Drake, 2017. Lastly, since the patient
presented with chest pain characteristic of angina, pain assessment, and monitoring should be
done (Goodlin et al., 2012).
The cardiovascular assessment begins with the measurement of vital signs (Lewis et al.,
2016). Blood pressure is an important measurement since the patient was previously
hypertensive with a blood pressure of 160/100. The questions in the health history should try to
rule out any complications of hypertension (Lewis et al., 2016). The patient should be asked
about blurring of vision to rule out hypertensive eye disease, history of loss of consciousness to
rule out transient ischemic attacks and palpitations to rule out hypertensive heart disease (Lewis
et al., 2016). The pulses should be measured including the radial, femoral, popliteal and dorsalis
pedis pulses. Tachycardia is a feature of heart failure and should be monitored in this patient.
Worsening vital signs show clinical deterioration and are a subject of inpatient monitoring to
guide clinical interventions (Lewis et al., 2016).
ECG done showed ST elevation. Serum markers were done and the results showed a slightly
decreased creatine kinase but grossly increased troponin I and T. A diagnosis of ST-elevation
myocardial infarction was made and coronary angioplasty with stenting done. He was discharged
to the ward for further monitoring and assessment.
Focused assessment
The sequence of assessment in this patient should include a cardiovascular assessment,
respiratory assessment and pain assessment (LeMone et al., 2015). This is a patient with an
established cardiovascular pathology presenting with chest pain. A cardiovascular assessment
with measurement of vital signs is therefore warranted (Glynn & Drake, 2017). Presentation of
chest pain and the close correlation between the respiratory system and cardiac pathology also
make a focused respiratory assessment needed (Glynn & Drake, 2017. Lastly, since the patient
presented with chest pain characteristic of angina, pain assessment, and monitoring should be
done (Goodlin et al., 2012).
The cardiovascular assessment begins with the measurement of vital signs (Lewis et al.,
2016). Blood pressure is an important measurement since the patient was previously
hypertensive with a blood pressure of 160/100. The questions in the health history should try to
rule out any complications of hypertension (Lewis et al., 2016). The patient should be asked
about blurring of vision to rule out hypertensive eye disease, history of loss of consciousness to
rule out transient ischemic attacks and palpitations to rule out hypertensive heart disease (Lewis
et al., 2016). The pulses should be measured including the radial, femoral, popliteal and dorsalis
pedis pulses. Tachycardia is a feature of heart failure and should be monitored in this patient.
Worsening vital signs show clinical deterioration and are a subject of inpatient monitoring to
guide clinical interventions (Lewis et al., 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING 4
The cardiac exam should be conducted by inspection, palpation, and percussion of the
precordium (Hinkle & Cheever, 2013). Relevant cardiac history should include questions
assessing for difficulty in breathing, dyspnea, palpitations, leg swelling, orthopnea, paroxysmal
nocturnal dyspnea, and chest pain. Dyspnea should be based on the level of exercise intolerance
experienced. Dyspnea that prevents one from lying supine is termed orthopnea and is a marker of
heart failure. Leg swelling is also a marker of heart failure (Hinkle & Cheever, 2013).
On inspection of the precordium, hyperactivity should be noted. A hyperactive
precordium denoted cardiomegaly which can occur in hypertension. Palpation for apex deviation
should be done. the normal apex beat in an adult is at the fifth intercostal space in the mid-
clavicular line. Apex deviation is also a sign of cardiomegaly. Auscultation of the heart sounds
should be done next. The first and second heart sounds should be heard and any murmurs noted
(Hinkle & Cheever, 2013). Murmurs represent turbulent blood flow and could point to other
cardiac pathology. This focused assessment aims at detecting cardiac pathology in this case of
myocardial infarction, identify comorbid conditions and complications such as heart failure and
cardiogenic shock (Hinkle & Cheever, 2013).
The respiratory assessment begins by assessing the breathing of the patient. This includes
signs of breathlessness, increased work of breathing, use of accessory muscles and cyanosis. This
is done on inspection (Lewis et al., 2016). The auscultation of the ling fields is done to assess for
added sounds such as wheeze, stridor, basal crepitations, rales or crackles. Signs of pulmonary
edema in this patient is warranted due to the setting of heart failure. Percussion notes over the
lung bases should be done to assess for fluid accumulation which is dull on percussion or a
pneumonic process (Lewis et al., 2016).
The cardiac exam should be conducted by inspection, palpation, and percussion of the
precordium (Hinkle & Cheever, 2013). Relevant cardiac history should include questions
assessing for difficulty in breathing, dyspnea, palpitations, leg swelling, orthopnea, paroxysmal
nocturnal dyspnea, and chest pain. Dyspnea should be based on the level of exercise intolerance
experienced. Dyspnea that prevents one from lying supine is termed orthopnea and is a marker of
heart failure. Leg swelling is also a marker of heart failure (Hinkle & Cheever, 2013).
On inspection of the precordium, hyperactivity should be noted. A hyperactive
precordium denoted cardiomegaly which can occur in hypertension. Palpation for apex deviation
should be done. the normal apex beat in an adult is at the fifth intercostal space in the mid-
clavicular line. Apex deviation is also a sign of cardiomegaly. Auscultation of the heart sounds
should be done next. The first and second heart sounds should be heard and any murmurs noted
(Hinkle & Cheever, 2013). Murmurs represent turbulent blood flow and could point to other
cardiac pathology. This focused assessment aims at detecting cardiac pathology in this case of
myocardial infarction, identify comorbid conditions and complications such as heart failure and
cardiogenic shock (Hinkle & Cheever, 2013).
The respiratory assessment begins by assessing the breathing of the patient. This includes
signs of breathlessness, increased work of breathing, use of accessory muscles and cyanosis. This
is done on inspection (Lewis et al., 2016). The auscultation of the ling fields is done to assess for
added sounds such as wheeze, stridor, basal crepitations, rales or crackles. Signs of pulmonary
edema in this patient is warranted due to the setting of heart failure. Percussion notes over the
lung bases should be done to assess for fluid accumulation which is dull on percussion or a
pneumonic process (Lewis et al., 2016).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING 5
The respiratory history should incorporate questions on cough, whether productive or
nonproduction, the color, and consistency of the sputum, variations of chest pain with respiration
and signs of respiratory distress. These questions are important in this assessment as they
differentiate respiratory from cardiac pathology and also identify respiratory manifestation of
cardiac pathology (Lewis et al., 2016).
Pain assessment is an important component of this patient’s assessment. This is because
the patient presented with chest pain (Goodlin et al., 2012). The pain was characteristic of
angina, which is a cardiac pain due to ischemia (Foreman, Garrett, & Blair, 2015). The patient is
an increased risk of recurrent ischemic attacks, monitoring the patient’s pain is important.
Assessment of pain involves asking questions that seek to guide one to the site of pain, the onset,
duration, aggravating factors, relieving factors, character and associated symptoms such as
vomiting (Turk & Melzack, 2011). The character of chest pain differentiates respiratory from
cardiovascular pain. respiratory pathology tends to result in pleuritic chest pain while the patient
presented with angina which is crushing in nature. The patient is then asked to rate their pain on
a scale of 1-10 with 1 being mild and 10 being unbearable. Monitoring for a similar episode
could prevent future attacks that might be fatal (Turk & Melzack, 2011).
Pathophysiology
Myocardial infarction is among a spectrum of cardiovascular diseases termed acute
coronary syndromes (Walker & Colledge, 2013). 90% of these acute coronary syndromes are
caused by atherosclerosis. Atherosclerotic plaque rupture and formation of an acute thrombus
lead to coronary artery obstruction, ischemia, and infarction (Thygesen et al., 2018). The risk
factors associated with atheroma formation and subsequent MI include both modifiable and non-
modifiable.
The respiratory history should incorporate questions on cough, whether productive or
nonproduction, the color, and consistency of the sputum, variations of chest pain with respiration
and signs of respiratory distress. These questions are important in this assessment as they
differentiate respiratory from cardiac pathology and also identify respiratory manifestation of
cardiac pathology (Lewis et al., 2016).
Pain assessment is an important component of this patient’s assessment. This is because
the patient presented with chest pain (Goodlin et al., 2012). The pain was characteristic of
angina, which is a cardiac pain due to ischemia (Foreman, Garrett, & Blair, 2015). The patient is
an increased risk of recurrent ischemic attacks, monitoring the patient’s pain is important.
Assessment of pain involves asking questions that seek to guide one to the site of pain, the onset,
duration, aggravating factors, relieving factors, character and associated symptoms such as
vomiting (Turk & Melzack, 2011). The character of chest pain differentiates respiratory from
cardiovascular pain. respiratory pathology tends to result in pleuritic chest pain while the patient
presented with angina which is crushing in nature. The patient is then asked to rate their pain on
a scale of 1-10 with 1 being mild and 10 being unbearable. Monitoring for a similar episode
could prevent future attacks that might be fatal (Turk & Melzack, 2011).
Pathophysiology
Myocardial infarction is among a spectrum of cardiovascular diseases termed acute
coronary syndromes (Walker & Colledge, 2013). 90% of these acute coronary syndromes are
caused by atherosclerosis. Atherosclerotic plaque rupture and formation of an acute thrombus
lead to coronary artery obstruction, ischemia, and infarction (Thygesen et al., 2018). The risk
factors associated with atheroma formation and subsequent MI include both modifiable and non-
modifiable.
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING 6
Non-modifiable risk factors include age, sex and family history of heart disease (Huma,
Tariq, Amin, & Mahmood, 2012). The patient has these risk factor as she is a 64-year-old female
with a family history of heart disease. Her advanced age is an independent risk factor for
cardiovascular disease (Dhingra & Vasan, 2012). The family history of heart disease include
both parents dying in their 60’s due to heart attacks, two of his four brothers had heart attacks
and high blood pressure, and his remaining uncle had two heart attacks and a stroke. The family
history of myocardial infarction is an independent risk factor with up to a double risk of MI if a
first-degree relative had MI (Ranthe et al., 2015).
Modifiable risk factors are those that can be altered to change the course of the disease
(Oliveira, Avezum, & Roever, 2015). They include smoking, diabetes mellitus, hypertension,
hypercholesterolemia, dyslipidemia, truncal obesity, stress, sedentary lifestyle and poor fatty diet
(Canto et al., 2011). The patient clearly has several modifiable risk factors as evidenced by the
health history. The patient leads a sedentary lifestyle with a diet high in sugars and fats. The
patient is hypertensive with a blood pressure of 160/100 and lab investigations relieved
dyslipidemia with high LDL, triglycerides, cholesterol and low HDL (Voight et al., 2012). The
patient is also obese with a BMI of 31 kg/m2 and a truncal obesity evidenced by a waist
circumference of 101 cm. All these risk factors increased the probability of developing acute
coronary syndrome and other cardiovascular pathology (Canto et al., 2011).
The pathology in acute coronary syndromes involves obstruction of coronary blood flow
leading to ischemia and infarction (Frangogiannis, 2011). Ischemia is due to hypoperfusion of
the myocardium and occurs in angina. The patient had symptoms of stable angina for three
months prior to the presentation. Myocardial infarction can be preceded by periods of stable or
Non-modifiable risk factors include age, sex and family history of heart disease (Huma,
Tariq, Amin, & Mahmood, 2012). The patient has these risk factor as she is a 64-year-old female
with a family history of heart disease. Her advanced age is an independent risk factor for
cardiovascular disease (Dhingra & Vasan, 2012). The family history of heart disease include
both parents dying in their 60’s due to heart attacks, two of his four brothers had heart attacks
and high blood pressure, and his remaining uncle had two heart attacks and a stroke. The family
history of myocardial infarction is an independent risk factor with up to a double risk of MI if a
first-degree relative had MI (Ranthe et al., 2015).
Modifiable risk factors are those that can be altered to change the course of the disease
(Oliveira, Avezum, & Roever, 2015). They include smoking, diabetes mellitus, hypertension,
hypercholesterolemia, dyslipidemia, truncal obesity, stress, sedentary lifestyle and poor fatty diet
(Canto et al., 2011). The patient clearly has several modifiable risk factors as evidenced by the
health history. The patient leads a sedentary lifestyle with a diet high in sugars and fats. The
patient is hypertensive with a blood pressure of 160/100 and lab investigations relieved
dyslipidemia with high LDL, triglycerides, cholesterol and low HDL (Voight et al., 2012). The
patient is also obese with a BMI of 31 kg/m2 and a truncal obesity evidenced by a waist
circumference of 101 cm. All these risk factors increased the probability of developing acute
coronary syndrome and other cardiovascular pathology (Canto et al., 2011).
The pathology in acute coronary syndromes involves obstruction of coronary blood flow
leading to ischemia and infarction (Frangogiannis, 2011). Ischemia is due to hypoperfusion of
the myocardium and occurs in angina. The patient had symptoms of stable angina for three
months prior to the presentation. Myocardial infarction can be preceded by periods of stable or
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING 7
unstable angina. It occurs when the obstruction becomes irreversible causing distal loss of
perfusion and eventual death of myocardium (Frangogiannis, 2011).
Acute myocardial infarction presents with chest a crushing chest pain, radiating to the
jaw or neck. The pathophysiology of angina is due to microvascular obstruction leading to an
imbalance between oxygen supply and demands (Heusch & Gersh,2016). Other presentations of
MI include autonomic symptoms due to activation of the sympathetic nervous system causing
nausea, vomiting, and pallor. The patient had an episode of vomiting on her way to the
emergency department.
Acute coronary syndromes include unstable angina which is angina even at rest, ST-
elevation myocardial infarction (STEMI) and non- ST-elevation myocardial infarction (NON-
STEMI) (Lewis et al., 2016). The patient had a STEMI evidenced by the ECG findings. An ECG
recording is therefore important in characterizing the type of MI and also diagnosing acute
coronary syndromes. Another needed requirement is an elevation in serum cardiac markers
(Lewis et al., 2016). This includes creatine kinase (CK-MB), and troponin I and T. These
enzymes are released from myocardium during infarction and are used to monitor the progress of
infarction, detect reinfarction and monitor treatment. The patient had elevated troponins with a
reduced creatine kinase.
unstable angina. It occurs when the obstruction becomes irreversible causing distal loss of
perfusion and eventual death of myocardium (Frangogiannis, 2011).
Acute myocardial infarction presents with chest a crushing chest pain, radiating to the
jaw or neck. The pathophysiology of angina is due to microvascular obstruction leading to an
imbalance between oxygen supply and demands (Heusch & Gersh,2016). Other presentations of
MI include autonomic symptoms due to activation of the sympathetic nervous system causing
nausea, vomiting, and pallor. The patient had an episode of vomiting on her way to the
emergency department.
Acute coronary syndromes include unstable angina which is angina even at rest, ST-
elevation myocardial infarction (STEMI) and non- ST-elevation myocardial infarction (NON-
STEMI) (Lewis et al., 2016). The patient had a STEMI evidenced by the ECG findings. An ECG
recording is therefore important in characterizing the type of MI and also diagnosing acute
coronary syndromes. Another needed requirement is an elevation in serum cardiac markers
(Lewis et al., 2016). This includes creatine kinase (CK-MB), and troponin I and T. These
enzymes are released from myocardium during infarction and are used to monitor the progress of
infarction, detect reinfarction and monitor treatment. The patient had elevated troponins with a
reduced creatine kinase.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING 8
Care planning and nursing interventions.
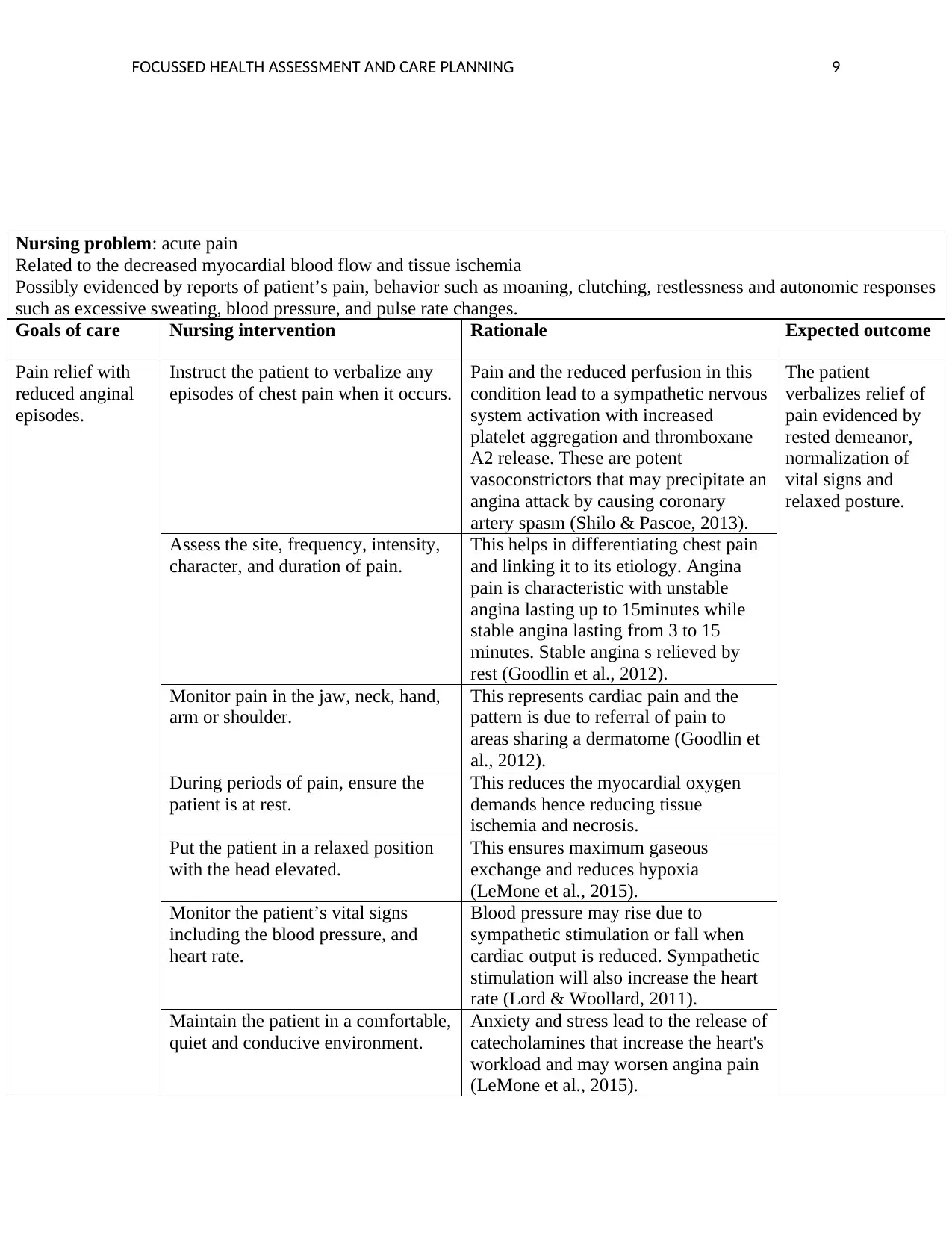
The priorities of care in this patient include acute pain, the risk of decreased cardiac
output, the risk of ineffective tissue perfusion, anxiety, the risk for excess fluid volume and
activity intolerance (Lewis et al., 2016). Nursing interventions should be centered around these
priority issues to ensure the optimal patient outcome.
Care planning and nursing interventions.
The priorities of care in this patient include acute pain, the risk of decreased cardiac
output, the risk of ineffective tissue perfusion, anxiety, the risk for excess fluid volume and
activity intolerance (Lewis et al., 2016). Nursing interventions should be centered around these
priority issues to ensure the optimal patient outcome.
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING 9
Nursing problem: acute pain
Related to the decreased myocardial blood flow and tissue ischemia
Possibly evidenced by reports of patient’s pain, behavior such as moaning, clutching, restlessness and autonomic responses
such as excessive sweating, blood pressure, and pulse rate changes.
Goals of care Nursing intervention Rationale Expected outcome
Pain relief with
reduced anginal
episodes.
Instruct the patient to verbalize any
episodes of chest pain when it occurs.
Pain and the reduced perfusion in this
condition lead to a sympathetic nervous
system activation with increased
platelet aggregation and thromboxane
A2 release. These are potent
vasoconstrictors that may precipitate an
angina attack by causing coronary
artery spasm (Shilo & Pascoe, 2013).
The patient
verbalizes relief of
pain evidenced by
rested demeanor,
normalization of
vital signs and
relaxed posture.
Assess the site, frequency, intensity,
character, and duration of pain.
This helps in differentiating chest pain
and linking it to its etiology. Angina
pain is characteristic with unstable
angina lasting up to 15minutes while
stable angina lasting from 3 to 15
minutes. Stable angina s relieved by
rest (Goodlin et al., 2012).
Monitor pain in the jaw, neck, hand,
arm or shoulder.
This represents cardiac pain and the
pattern is due to referral of pain to
areas sharing a dermatome (Goodlin et
al., 2012).
During periods of pain, ensure the
patient is at rest.
This reduces the myocardial oxygen
demands hence reducing tissue
ischemia and necrosis.
Put the patient in a relaxed position
with the head elevated.
This ensures maximum gaseous
exchange and reduces hypoxia
(LeMone et al., 2015).
Monitor the patient’s vital signs
including the blood pressure, and
heart rate.
Blood pressure may rise due to
sympathetic stimulation or fall when
cardiac output is reduced. Sympathetic
stimulation will also increase the heart
rate (Lord & Woollard, 2011).
Maintain the patient in a comfortable,
quiet and conducive environment.
Anxiety and stress lead to the release of
catecholamines that increase the heart's
workload and may worsen angina pain
(LeMone et al., 2015).
Nursing problem: acute pain
Related to the decreased myocardial blood flow and tissue ischemia
Possibly evidenced by reports of patient’s pain, behavior such as moaning, clutching, restlessness and autonomic responses
such as excessive sweating, blood pressure, and pulse rate changes.
Goals of care Nursing intervention Rationale Expected outcome
Pain relief with
reduced anginal
episodes.
Instruct the patient to verbalize any
episodes of chest pain when it occurs.
Pain and the reduced perfusion in this
condition lead to a sympathetic nervous
system activation with increased
platelet aggregation and thromboxane
A2 release. These are potent
vasoconstrictors that may precipitate an
angina attack by causing coronary
artery spasm (Shilo & Pascoe, 2013).
The patient
verbalizes relief of
pain evidenced by
rested demeanor,
normalization of
vital signs and
relaxed posture.
Assess the site, frequency, intensity,
character, and duration of pain.
This helps in differentiating chest pain
and linking it to its etiology. Angina
pain is characteristic with unstable
angina lasting up to 15minutes while
stable angina lasting from 3 to 15
minutes. Stable angina s relieved by
rest (Goodlin et al., 2012).
Monitor pain in the jaw, neck, hand,
arm or shoulder.
This represents cardiac pain and the
pattern is due to referral of pain to
areas sharing a dermatome (Goodlin et
al., 2012).
During periods of pain, ensure the
patient is at rest.
This reduces the myocardial oxygen
demands hence reducing tissue
ischemia and necrosis.
Put the patient in a relaxed position
with the head elevated.
This ensures maximum gaseous
exchange and reduces hypoxia
(LeMone et al., 2015).
Monitor the patient’s vital signs
including the blood pressure, and
heart rate.
Blood pressure may rise due to
sympathetic stimulation or fall when
cardiac output is reduced. Sympathetic
stimulation will also increase the heart
rate (Lord & Woollard, 2011).
Maintain the patient in a comfortable,
quiet and conducive environment.
Anxiety and stress lead to the release of
catecholamines that increase the heart's
workload and may worsen angina pain
(LeMone et al., 2015).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
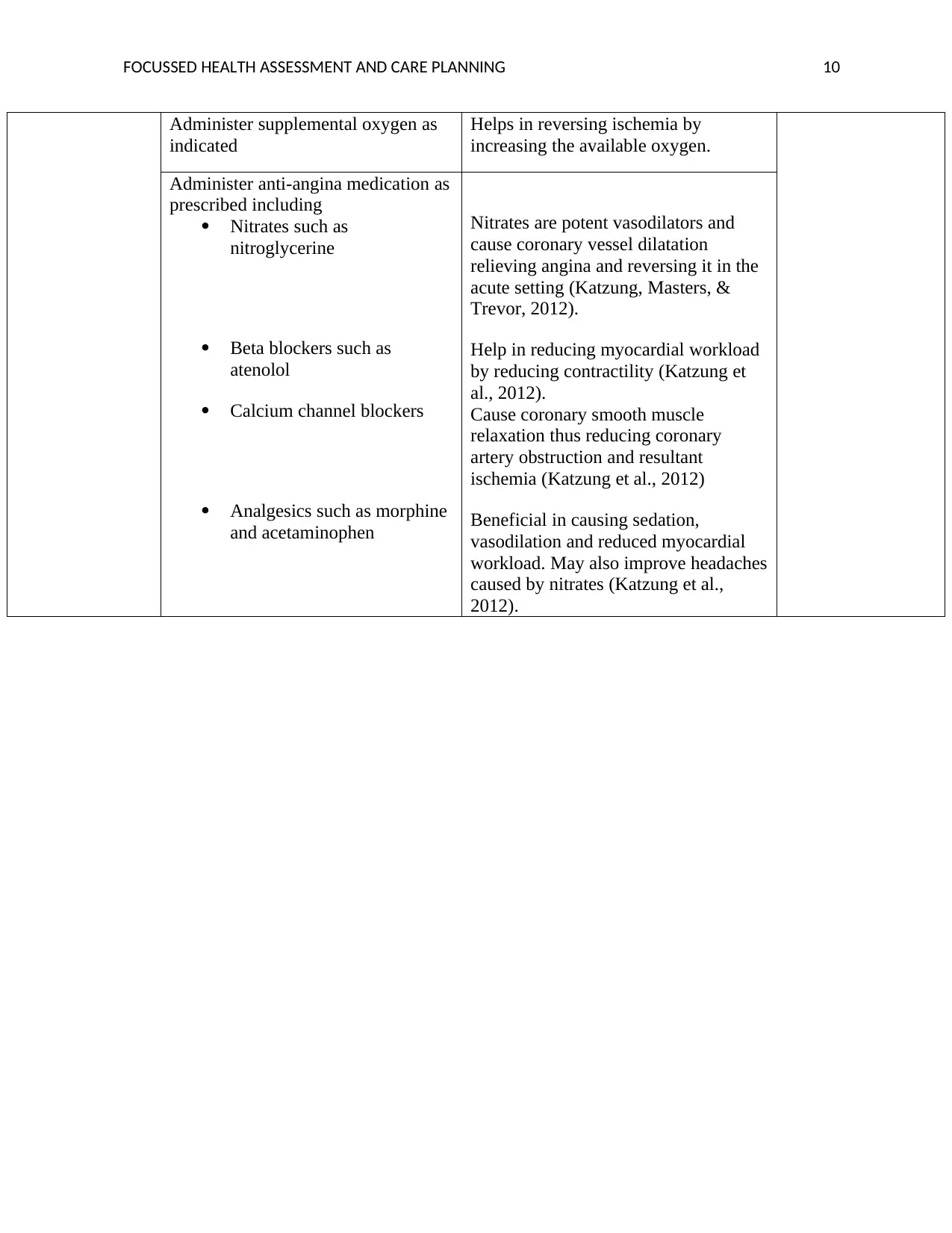
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING 10
Administer supplemental oxygen as
indicated
Helps in reversing ischemia by
increasing the available oxygen.
Administer anti-angina medication as
prescribed including
Nitrates such as
nitroglycerine
Beta blockers such as
atenolol
Calcium channel blockers
Analgesics such as morphine
and acetaminophen
Nitrates are potent vasodilators and
cause coronary vessel dilatation
relieving angina and reversing it in the
acute setting (Katzung, Masters, &
Trevor, 2012).
Help in reducing myocardial workload
by reducing contractility (Katzung et
al., 2012).
Cause coronary smooth muscle
relaxation thus reducing coronary
artery obstruction and resultant
ischemia (Katzung et al., 2012)
Beneficial in causing sedation,
vasodilation and reduced myocardial
workload. May also improve headaches
caused by nitrates (Katzung et al.,
2012).
Administer supplemental oxygen as
indicated
Helps in reversing ischemia by
increasing the available oxygen.
Administer anti-angina medication as
prescribed including
Nitrates such as
nitroglycerine
Beta blockers such as
atenolol
Calcium channel blockers
Analgesics such as morphine
and acetaminophen
Nitrates are potent vasodilators and
cause coronary vessel dilatation
relieving angina and reversing it in the
acute setting (Katzung, Masters, &
Trevor, 2012).
Help in reducing myocardial workload
by reducing contractility (Katzung et
al., 2012).
Cause coronary smooth muscle
relaxation thus reducing coronary
artery obstruction and resultant
ischemia (Katzung et al., 2012)
Beneficial in causing sedation,
vasodilation and reduced myocardial
workload. May also improve headaches
caused by nitrates (Katzung et al.,
2012).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
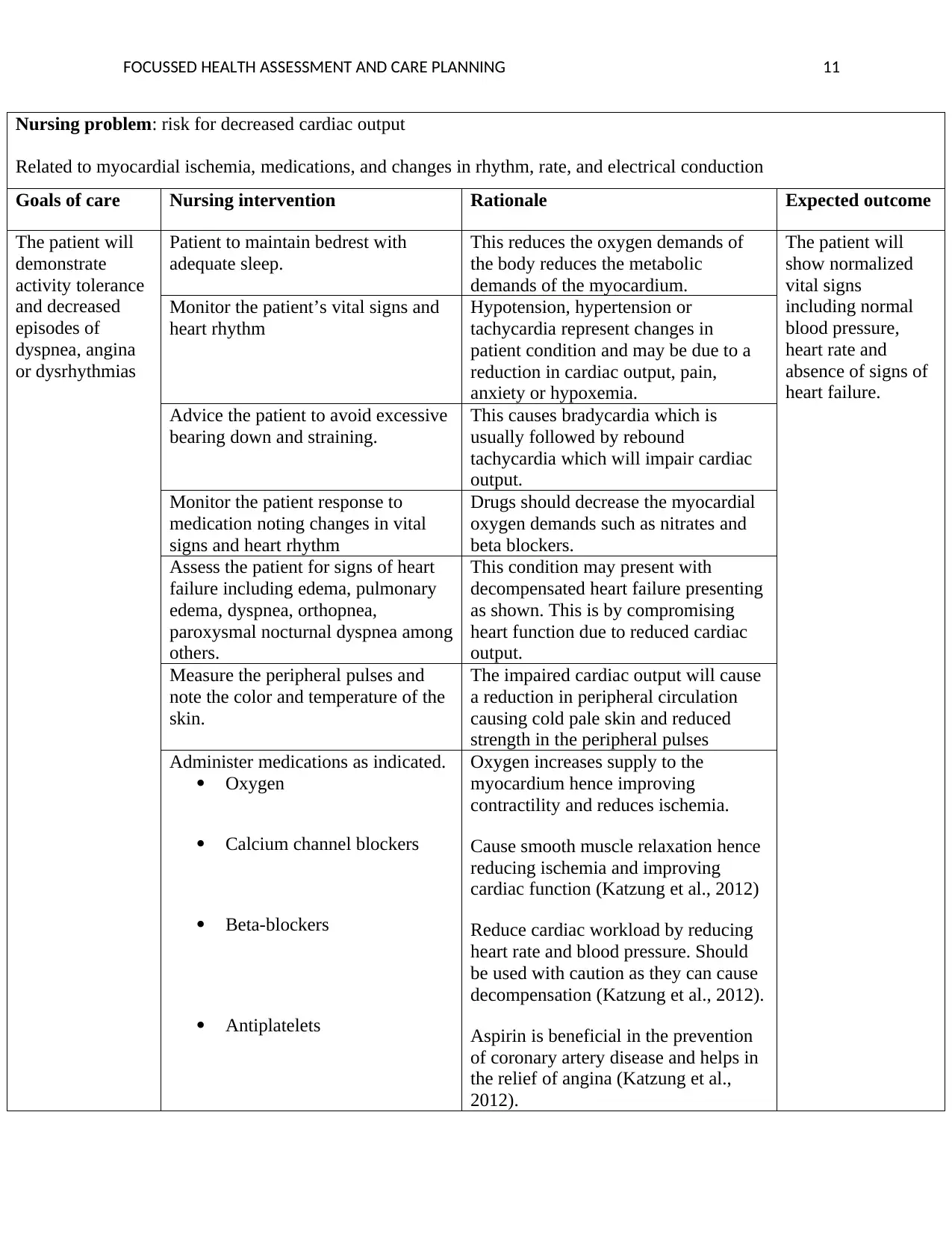
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING 11
Nursing problem: risk for decreased cardiac output
Related to myocardial ischemia, medications, and changes in rhythm, rate, and electrical conduction
Goals of care Nursing intervention Rationale Expected outcome
The patient will
demonstrate
activity tolerance
and decreased
episodes of
dyspnea, angina
or dysrhythmias
Patient to maintain bedrest with
adequate sleep.
This reduces the oxygen demands of
the body reduces the metabolic
demands of the myocardium.
The patient will
show normalized
vital signs
including normal
blood pressure,
heart rate and
absence of signs of
heart failure.
Monitor the patient’s vital signs and
heart rhythm
Hypotension, hypertension or
tachycardia represent changes in
patient condition and may be due to a
reduction in cardiac output, pain,
anxiety or hypoxemia.
Advice the patient to avoid excessive
bearing down and straining.
This causes bradycardia which is
usually followed by rebound
tachycardia which will impair cardiac
output.
Monitor the patient response to
medication noting changes in vital
signs and heart rhythm
Drugs should decrease the myocardial
oxygen demands such as nitrates and
beta blockers.
Assess the patient for signs of heart
failure including edema, pulmonary
edema, dyspnea, orthopnea,
paroxysmal nocturnal dyspnea among
others.
This condition may present with
decompensated heart failure presenting
as shown. This is by compromising
heart function due to reduced cardiac
output.
Measure the peripheral pulses and
note the color and temperature of the
skin.
The impaired cardiac output will cause
a reduction in peripheral circulation
causing cold pale skin and reduced
strength in the peripheral pulses
Administer medications as indicated.
Oxygen
Calcium channel blockers
Beta-blockers
Antiplatelets
Oxygen increases supply to the
myocardium hence improving
contractility and reduces ischemia.
Cause smooth muscle relaxation hence
reducing ischemia and improving
cardiac function (Katzung et al., 2012)
Reduce cardiac workload by reducing
heart rate and blood pressure. Should
be used with caution as they can cause
decompensation (Katzung et al., 2012).
Aspirin is beneficial in the prevention
of coronary artery disease and helps in
the relief of angina (Katzung et al.,
2012).
Nursing problem: risk for decreased cardiac output
Related to myocardial ischemia, medications, and changes in rhythm, rate, and electrical conduction
Goals of care Nursing intervention Rationale Expected outcome
The patient will
demonstrate
activity tolerance
and decreased
episodes of
dyspnea, angina
or dysrhythmias
Patient to maintain bedrest with
adequate sleep.
This reduces the oxygen demands of
the body reduces the metabolic
demands of the myocardium.
The patient will
show normalized
vital signs
including normal
blood pressure,
heart rate and
absence of signs of
heart failure.
Monitor the patient’s vital signs and
heart rhythm
Hypotension, hypertension or
tachycardia represent changes in
patient condition and may be due to a
reduction in cardiac output, pain,
anxiety or hypoxemia.
Advice the patient to avoid excessive
bearing down and straining.
This causes bradycardia which is
usually followed by rebound
tachycardia which will impair cardiac
output.
Monitor the patient response to
medication noting changes in vital
signs and heart rhythm
Drugs should decrease the myocardial
oxygen demands such as nitrates and
beta blockers.
Assess the patient for signs of heart
failure including edema, pulmonary
edema, dyspnea, orthopnea,
paroxysmal nocturnal dyspnea among
others.
This condition may present with
decompensated heart failure presenting
as shown. This is by compromising
heart function due to reduced cardiac
output.
Measure the peripheral pulses and
note the color and temperature of the
skin.
The impaired cardiac output will cause
a reduction in peripheral circulation
causing cold pale skin and reduced
strength in the peripheral pulses
Administer medications as indicated.
Oxygen
Calcium channel blockers
Beta-blockers
Antiplatelets
Oxygen increases supply to the
myocardium hence improving
contractility and reduces ischemia.
Cause smooth muscle relaxation hence
reducing ischemia and improving
cardiac function (Katzung et al., 2012)
Reduce cardiac workload by reducing
heart rate and blood pressure. Should
be used with caution as they can cause
decompensation (Katzung et al., 2012).
Aspirin is beneficial in the prevention
of coronary artery disease and helps in
the relief of angina (Katzung et al.,
2012).
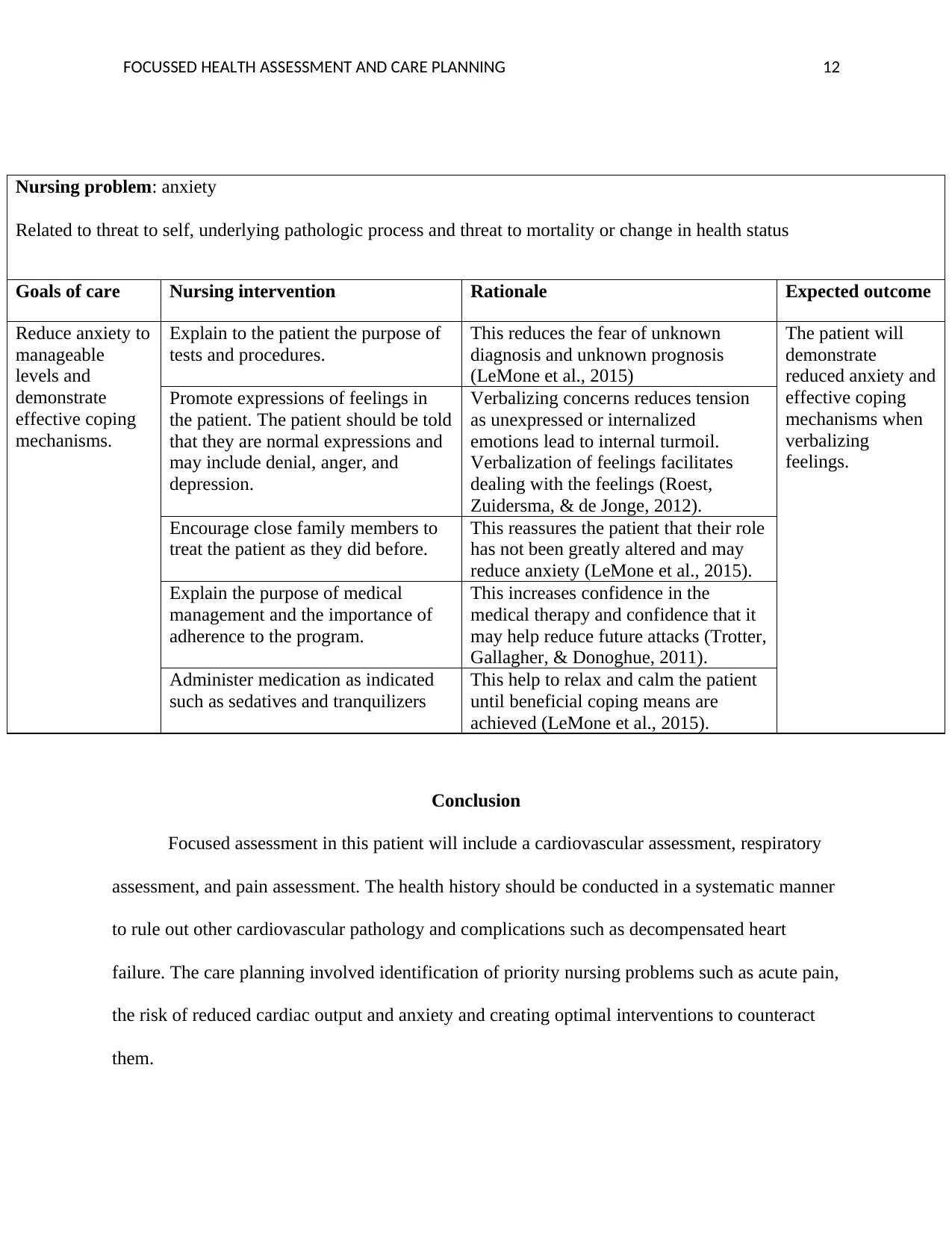
FOCUSSED HEALTH ASSESSMENT AND CARE PLANNING 12
Nursing problem: anxiety
Related to threat to self, underlying pathologic process and threat to mortality or change in health status
Goals of care Nursing intervention Rationale Expected outcome
Reduce anxiety to
manageable
levels and
demonstrate
effective coping
mechanisms.
Explain to the patient the purpose of
tests and procedures.
This reduces the fear of unknown
diagnosis and unknown prognosis
(LeMone et al., 2015)
The patient will
demonstrate
reduced anxiety and
effective coping
mechanisms when
verbalizing
feelings.
Promote expressions of feelings in
the patient. The patient should be told
that they are normal expressions and
may include denial, anger, and
depression.
Verbalizing concerns reduces tension
as unexpressed or internalized
emotions lead to internal turmoil.
Verbalization of feelings facilitates
dealing with the feelings (Roest,
Zuidersma, & de Jonge, 2012).
Encourage close family members to
treat the patient as they did before.
This reassures the patient that their role
has not been greatly altered and may
reduce anxiety (LeMone et al., 2015).
Explain the purpose of medical
management and the importance of
adherence to the program.
This increases confidence in the
medical therapy and confidence that it
may help reduce future attacks (Trotter,
Gallagher, & Donoghue, 2011).
Administer medication as indicated
such as sedatives and tranquilizers
This help to relax and calm the patient
until beneficial coping means are
achieved (LeMone et al., 2015).
Conclusion
Focused assessment in this patient will include a cardiovascular assessment, respiratory
assessment, and pain assessment. The health history should be conducted in a systematic manner
to rule out other cardiovascular pathology and complications such as decompensated heart
failure. The care planning involved identification of priority nursing problems such as acute pain,
the risk of reduced cardiac output and anxiety and creating optimal interventions to counteract
them.
Nursing problem: anxiety
Related to threat to self, underlying pathologic process and threat to mortality or change in health status
Goals of care Nursing intervention Rationale Expected outcome
Reduce anxiety to
manageable
levels and
demonstrate
effective coping
mechanisms.
Explain to the patient the purpose of
tests and procedures.
This reduces the fear of unknown
diagnosis and unknown prognosis
(LeMone et al., 2015)
The patient will
demonstrate
reduced anxiety and
effective coping
mechanisms when
verbalizing
feelings.
Promote expressions of feelings in
the patient. The patient should be told
that they are normal expressions and
may include denial, anger, and
depression.
Verbalizing concerns reduces tension
as unexpressed or internalized
emotions lead to internal turmoil.
Verbalization of feelings facilitates
dealing with the feelings (Roest,
Zuidersma, & de Jonge, 2012).
Encourage close family members to
treat the patient as they did before.
This reassures the patient that their role
has not been greatly altered and may
reduce anxiety (LeMone et al., 2015).
Explain the purpose of medical
management and the importance of
adherence to the program.
This increases confidence in the
medical therapy and confidence that it
may help reduce future attacks (Trotter,
Gallagher, & Donoghue, 2011).
Administer medication as indicated
such as sedatives and tranquilizers
This help to relax and calm the patient
until beneficial coping means are
achieved (LeMone et al., 2015).
Conclusion
Focused assessment in this patient will include a cardiovascular assessment, respiratory
assessment, and pain assessment. The health history should be conducted in a systematic manner
to rule out other cardiovascular pathology and complications such as decompensated heart
failure. The care planning involved identification of priority nursing problems such as acute pain,
the risk of reduced cardiac output and anxiety and creating optimal interventions to counteract
them.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




