HSN713 Assignment: Critiquing the Health Belief Model for Food Choice
VerifiedAdded on 2023/01/19
|13
|3562
|1
Report
AI Summary
This report critically examines the Health Belief Model (HBM), a psychological model used to predict health-related behaviors, with a specific focus on its application to human food choices. The report analyzes the HBM's constructs, including perceived susceptibility, severity, benefits, and barriers, and discusses its limitations in explaining complex food choice behaviors. The assignment then proposes an alternative model, the Stages of Change Model (Transtheoretical Model), and argues for its superior ability to understand and influence human food choices. The report highlights the stages of the Transtheoretical Model, including pre-contemplation, contemplation, preparation, action, and maintenance, emphasizing its potential for promoting healthier eating habits. The analysis includes discussion of factors influencing food choices like palatability, cost, accessibility, and social setting, alongside the limitations of HBM. The report concludes by advocating for the Transtheoretical Model's usefulness in fostering behavior change, providing insights into how interventions based on this model can improve food choices.

Student’s Name
Affiliate Institution
Date
Affiliate Institution
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Health Belief Model (HBM)
Being a psychological model, the Health Belief Model endeavors to predict and explicate
health-related behaviors, particularly regarding the endorsement of health services.(1) HBM
focusses on people’s beliefs and attitudes which it uses to explain and forecast their health
behaviors. It is one of the first health behavior models, established in the 1950s by social
psychologists at the United States Public Health Service who were seeking a better
understanding of the prevalent failure of screening services for tuberculosis.(3)HBM is still one of
the preeminent and most extensively used theories in the research of human health behavior.(2)
The model proposes that factors such as people’s beliefs concerning health issues, their self-
efficacy, barriers to taking action as well as perceived advantages of acting determine their
engagement or lack of it towards health-upholding behavior.(10)
HBM Constructs
Perceived susceptibility: this is a person’s assessment of the risks involved in
developing a problem with their health. The health belief model denotes that persons who
recognize that they are vulnerable to a specified healthiness problem will involve themselves in
healthy behaviors that prevent the development of that issue. For instance, people who perceive a
high risk of suffering from type 2 diabetes probably due to their genetics will most likely try
their best to keep away from too much sugar or sugary foodstuffs and drinks. Sugar itself may
not lead to type 2 diabetes but the individual may become overweight or develop obesity which
increases their probability of developing type 2 diabetes.(7)On the other hand, folks with low
perceived vulnerability may not agree that they are at risk of contracting a certain illness. These
individuals are more likely to indulge in risky or unhealthy behaviors just like those who believe
Being a psychological model, the Health Belief Model endeavors to predict and explicate
health-related behaviors, particularly regarding the endorsement of health services.(1) HBM
focusses on people’s beliefs and attitudes which it uses to explain and forecast their health
behaviors. It is one of the first health behavior models, established in the 1950s by social
psychologists at the United States Public Health Service who were seeking a better
understanding of the prevalent failure of screening services for tuberculosis.(3)HBM is still one of
the preeminent and most extensively used theories in the research of human health behavior.(2)
The model proposes that factors such as people’s beliefs concerning health issues, their self-
efficacy, barriers to taking action as well as perceived advantages of acting determine their
engagement or lack of it towards health-upholding behavior.(10)
HBM Constructs
Perceived susceptibility: this is a person’s assessment of the risks involved in
developing a problem with their health. The health belief model denotes that persons who
recognize that they are vulnerable to a specified healthiness problem will involve themselves in
healthy behaviors that prevent the development of that issue. For instance, people who perceive a
high risk of suffering from type 2 diabetes probably due to their genetics will most likely try
their best to keep away from too much sugar or sugary foodstuffs and drinks. Sugar itself may
not lead to type 2 diabetes but the individual may become overweight or develop obesity which
increases their probability of developing type 2 diabetes.(7)On the other hand, folks with low
perceived vulnerability may not agree that they are at risk of contracting a certain illness. These
individuals are more likely to indulge in risky or unhealthy behaviors just like those who believe
that they might develop an ailment but it is unlikely. If there is no one in one’s family or among
close relatives who have ever suffered or is suffering from type 2 diabetes, for example, the
individual might not be too cautious of their sugar intake because they believe that there is the
low possibility of them developing the illness.
Perceived severity: This states to the subjective valuation of the austerity of a health
issue as well as that of its consequences. This element mentions that people who view a given
health problem or illness as serious are more probable to engage in health-promoting actions that
will help them prevent or avoid those problems. Perceiving obesity as a serious condition that
brings about other health problems will make the person be more careful about their food choice.
They will indulge in healthy eating habits and do regular physical exercises that will enable them
to prevent the onset of obesity or lessen its severity. The perceived harshness of a diseases
embraces subjective beliefs about the illness itself, for instance as causing disability, pain or
being life-threatening as well as its effects on individual functioning in their life, that is socially
and at work. Perceived severity and susceptibility lead to the perceived threat which depends on
individual knowledge about the condition. HBM forecasts that a greater perceived threat leads to
engagement in behaviors that promote health.
Perceived benefits: a party’s assessment of the value of taking action towards bettering
their health also influences health-promoting behavior. A person will presumably carry out an act
to benefit their health if they believe that it will reduce the susceptibility to a particular illness or
reduce its austerity. People who believe sunscreen will prevent skin cancer, for example, are
more likely to wear sunscreen as opposed to those who do not.(14) Believing that eating a
balanced diet and exercising regularly prevents the occurrence of certain diseases encourages one
to observe their diet and keep healthy.
close relatives who have ever suffered or is suffering from type 2 diabetes, for example, the
individual might not be too cautious of their sugar intake because they believe that there is the
low possibility of them developing the illness.
Perceived severity: This states to the subjective valuation of the austerity of a health
issue as well as that of its consequences. This element mentions that people who view a given
health problem or illness as serious are more probable to engage in health-promoting actions that
will help them prevent or avoid those problems. Perceiving obesity as a serious condition that
brings about other health problems will make the person be more careful about their food choice.
They will indulge in healthy eating habits and do regular physical exercises that will enable them
to prevent the onset of obesity or lessen its severity. The perceived harshness of a diseases
embraces subjective beliefs about the illness itself, for instance as causing disability, pain or
being life-threatening as well as its effects on individual functioning in their life, that is socially
and at work. Perceived severity and susceptibility lead to the perceived threat which depends on
individual knowledge about the condition. HBM forecasts that a greater perceived threat leads to
engagement in behaviors that promote health.
Perceived benefits: a party’s assessment of the value of taking action towards bettering
their health also influences health-promoting behavior. A person will presumably carry out an act
to benefit their health if they believe that it will reduce the susceptibility to a particular illness or
reduce its austerity. People who believe sunscreen will prevent skin cancer, for example, are
more likely to wear sunscreen as opposed to those who do not.(14) Believing that eating a
balanced diet and exercising regularly prevents the occurrence of certain diseases encourages one
to observe their diet and keep healthy.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Perceived barriers: behaviors related to health are also a function of hindrances to
action, which refer to the subjective valuation of the hurdles to change in behavior. Certain
obstacles may prevent one to take action in promoting their health even though they believe that
these actions will prevent certain health issues or reduce their seriousness. These hindrances
include certain aspects such as side effects to a medical procedure, danger, expenditure or even
discomforts such as pain which may be a result of engaging in those behaviors.(11)The benefits of
taking action toward health-enhancing behavior should, therefore, be more than the barriers
involved in the same. For example, the emotional upset brought about by giving up sugary drinks
and foods may prevent one from making a healthy choice in the foods they ingest. The individual
may not view it as worth the trouble especially if they trust that they are unlikely to develop any
illnesses related to sugar. Similarly, people who acquire great benefits from regular exercise and
healthy eating such as fitness professionals, for instance, will definitely be more enthusiastic
about overcoming the emotional upset of giving up unhealthy foods.
Cues to Action: Health Belief Model suggests that a trigger, either external or internal is
necessary for instigating engagement in behaviors associated with health. Internal cues of action
include psychological facets such as symptoms of a disease and pain while external cues are
other triggers such as the media and info from other people.(3) Examples of cues of action in the
case of food choice include illness of a family member or friend as a result of unhealthy eating, a
reminder from one’s fitness trainer as well as warnings indicated on purchased products.
Modifying variables: Individual perceptions are impacted by certain psychosocial,
demographic and structural characteristics. HBM suggests that variables such as age, race, and
knowledge about a particular illness, social class and peer pressure influence the perceived
severity, susceptibility barriers and benefits thus affect health-related behavior indirectly.(16)
action, which refer to the subjective valuation of the hurdles to change in behavior. Certain
obstacles may prevent one to take action in promoting their health even though they believe that
these actions will prevent certain health issues or reduce their seriousness. These hindrances
include certain aspects such as side effects to a medical procedure, danger, expenditure or even
discomforts such as pain which may be a result of engaging in those behaviors.(11)The benefits of
taking action toward health-enhancing behavior should, therefore, be more than the barriers
involved in the same. For example, the emotional upset brought about by giving up sugary drinks
and foods may prevent one from making a healthy choice in the foods they ingest. The individual
may not view it as worth the trouble especially if they trust that they are unlikely to develop any
illnesses related to sugar. Similarly, people who acquire great benefits from regular exercise and
healthy eating such as fitness professionals, for instance, will definitely be more enthusiastic
about overcoming the emotional upset of giving up unhealthy foods.
Cues to Action: Health Belief Model suggests that a trigger, either external or internal is
necessary for instigating engagement in behaviors associated with health. Internal cues of action
include psychological facets such as symptoms of a disease and pain while external cues are
other triggers such as the media and info from other people.(3) Examples of cues of action in the
case of food choice include illness of a family member or friend as a result of unhealthy eating, a
reminder from one’s fitness trainer as well as warnings indicated on purchased products.
Modifying variables: Individual perceptions are impacted by certain psychosocial,
demographic and structural characteristics. HBM suggests that variables such as age, race, and
knowledge about a particular illness, social class and peer pressure influence the perceived
severity, susceptibility barriers and benefits thus affect health-related behavior indirectly.(16)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Self-efficacy: in general, this is an entity’s belief in their natural aptitude to accomplish
goals. Self-efficacy was initially added to the above-mentioned model to better elucidate a one-
time behavior related to health such as obtaining immunization or screening for cancer. It was
later on applied to other matters such as diet modification. Strong belief in one’s ability to
achieve a certain goal brings about change in behavior. If one has great confidence that they can
live in good health through better food choice, then the individual is more likely to start eating a
healthier diet.
HBM is a useful model in promoting health through food choice. Interventions based on
this model aim to enhance apparent vulnerability as well as the seriousness of a health condition
through education of disease incidence, risk estimates, and information on financial, medical as
well as social consequences.(6) This model can thus be used to create awareness on the
relationship between diet and disease and the importance of healthy food choices in preventing
certain ailments.(9)(13) These interventions may also provide cues to action as well as improve self-
efficacy by delivering training in particular health-related behaviors.(8) However, in relation to
human food choice, relying on people’s beliefs and attitudes is not sufficient to stimulate them to
choose healthy meals. Most people know exactly what they should be eating but habitual
behaviors such as addiction to sugary foods and drinks become relatively independent of
conscious decision making in regard to health over time. In addition, individuals indulge in
healthy eating for other reasons other than the prevention of diseases or slowing their severity,
which HBM is all about. For example, many people in the modern world are engaged in healthy
living for aesthetic purposes which have nothing to do with illnesses. Also, the model does not
put into account the effects of emotions on health-related behavior. For instance, some people
may be propelled into indulging in eating unhealthy foods when they are experiencing
goals. Self-efficacy was initially added to the above-mentioned model to better elucidate a one-
time behavior related to health such as obtaining immunization or screening for cancer. It was
later on applied to other matters such as diet modification. Strong belief in one’s ability to
achieve a certain goal brings about change in behavior. If one has great confidence that they can
live in good health through better food choice, then the individual is more likely to start eating a
healthier diet.
HBM is a useful model in promoting health through food choice. Interventions based on
this model aim to enhance apparent vulnerability as well as the seriousness of a health condition
through education of disease incidence, risk estimates, and information on financial, medical as
well as social consequences.(6) This model can thus be used to create awareness on the
relationship between diet and disease and the importance of healthy food choices in preventing
certain ailments.(9)(13) These interventions may also provide cues to action as well as improve self-
efficacy by delivering training in particular health-related behaviors.(8) However, in relation to
human food choice, relying on people’s beliefs and attitudes is not sufficient to stimulate them to
choose healthy meals. Most people know exactly what they should be eating but habitual
behaviors such as addiction to sugary foods and drinks become relatively independent of
conscious decision making in regard to health over time. In addition, individuals indulge in
healthy eating for other reasons other than the prevention of diseases or slowing their severity,
which HBM is all about. For example, many people in the modern world are engaged in healthy
living for aesthetic purposes which have nothing to do with illnesses. Also, the model does not
put into account the effects of emotions on health-related behavior. For instance, some people
may be propelled into indulging in eating unhealthy foods when they are experiencing
psychological stress. A person’s mood also affects the choice of food he or she eats. In return,
food modifies temperament. Depressed moods increase severity for cravings which then
enhances the desire for those foodstuffs.
Drivers of Human Food Choice
Palatability
This describes the pleasure a specified individual derives from eating a specified food.
Each person has a certain type of food they enjoy eating the most. This has nothing to do with
their attitudes or beliefs as it is reliant on sensory properties such as smell, appearance, and taste.
(12)
Cost and accessibility
Cost is a major determinant of food choice among human beings. It depends on an
individual’s income and economic status. Low-income persons are more likely to eat unbalanced
diets that lack lots of fruits and vegetables which are often more expensive. Accessibility to
sources of foods such as shops and markets also determine the type of meals that a person eats.(15)
Social setting
Unlike years ago when almost all food was eaten at home, a continuously increasing
amount is eaten at work, in schools and restaurants today. The venue in which the food is eaten
affects one’s choice of food, particularly depending on which food is on offer. Unlike in homes,
access to healthy meals in schools and workplaces is limited. Social setting in relation to human
food choice majorly affects those with a special need, for example, vegetarians as well as those
with very tight work schedules.
Alternative Model of Food Choice
food modifies temperament. Depressed moods increase severity for cravings which then
enhances the desire for those foodstuffs.
Drivers of Human Food Choice
Palatability
This describes the pleasure a specified individual derives from eating a specified food.
Each person has a certain type of food they enjoy eating the most. This has nothing to do with
their attitudes or beliefs as it is reliant on sensory properties such as smell, appearance, and taste.
(12)
Cost and accessibility
Cost is a major determinant of food choice among human beings. It depends on an
individual’s income and economic status. Low-income persons are more likely to eat unbalanced
diets that lack lots of fruits and vegetables which are often more expensive. Accessibility to
sources of foods such as shops and markets also determine the type of meals that a person eats.(15)
Social setting
Unlike years ago when almost all food was eaten at home, a continuously increasing
amount is eaten at work, in schools and restaurants today. The venue in which the food is eaten
affects one’s choice of food, particularly depending on which food is on offer. Unlike in homes,
access to healthy meals in schools and workplaces is limited. Social setting in relation to human
food choice majorly affects those with a special need, for example, vegetarians as well as those
with very tight work schedules.
Alternative Model of Food Choice
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Stages of Change Model
Also referred to as the Transtheoretical Model, this is an interactive psychotherapeutic
theory that works toward change in behavior. The model evaluates the person’s readiness to
adopt new improved behavior and then provides processes and strategies that are meant to guide
the person on his or her new journey.(20) The transtheoretical model suggests that dissimilar
people are at different stages in relation to change in behavior. Some may not be set to attempt
changes whereas others may have already begun to implement modifications in their diet or other
aspects of life.(2) The model is based on various theories of psychotherapy, the Social Cognitive
Theory for instance, as well as the Learning Theory, hence the name transtheoretical. It was
developed by Carlo Di Clemente and the University of Rhode Island’s James O. Prochaska after
noticing that people differ in regard to motivational readiness to quit smoking.(17) They observed
that individuals pass along specific phases of readiness when trying to change their behavior.
The techniques and strategies that people employ to advance from one stage to the next along the
path of change in behavior were termed as processes of change.(4)
In this paper, the stages of change model was chosen based on its possible effectiveness
in the assimilation of healthy eating habits. Making a decision to start eating healthier can be
very difficult for many people, especially those used to eating unhealthy foods. Adoption of
healthy food choices should, therefore, be a process in which people are emboldened to keep
going and not give up. As indicated in the figure below, there are 5 stages of change portrayed by
the transtheoretical model.
Also referred to as the Transtheoretical Model, this is an interactive psychotherapeutic
theory that works toward change in behavior. The model evaluates the person’s readiness to
adopt new improved behavior and then provides processes and strategies that are meant to guide
the person on his or her new journey.(20) The transtheoretical model suggests that dissimilar
people are at different stages in relation to change in behavior. Some may not be set to attempt
changes whereas others may have already begun to implement modifications in their diet or other
aspects of life.(2) The model is based on various theories of psychotherapy, the Social Cognitive
Theory for instance, as well as the Learning Theory, hence the name transtheoretical. It was
developed by Carlo Di Clemente and the University of Rhode Island’s James O. Prochaska after
noticing that people differ in regard to motivational readiness to quit smoking.(17) They observed
that individuals pass along specific phases of readiness when trying to change their behavior.
The techniques and strategies that people employ to advance from one stage to the next along the
path of change in behavior were termed as processes of change.(4)
In this paper, the stages of change model was chosen based on its possible effectiveness
in the assimilation of healthy eating habits. Making a decision to start eating healthier can be
very difficult for many people, especially those used to eating unhealthy foods. Adoption of
healthy food choices should, therefore, be a process in which people are emboldened to keep
going and not give up. As indicated in the figure below, there are 5 stages of change portrayed by
the transtheoretical model.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
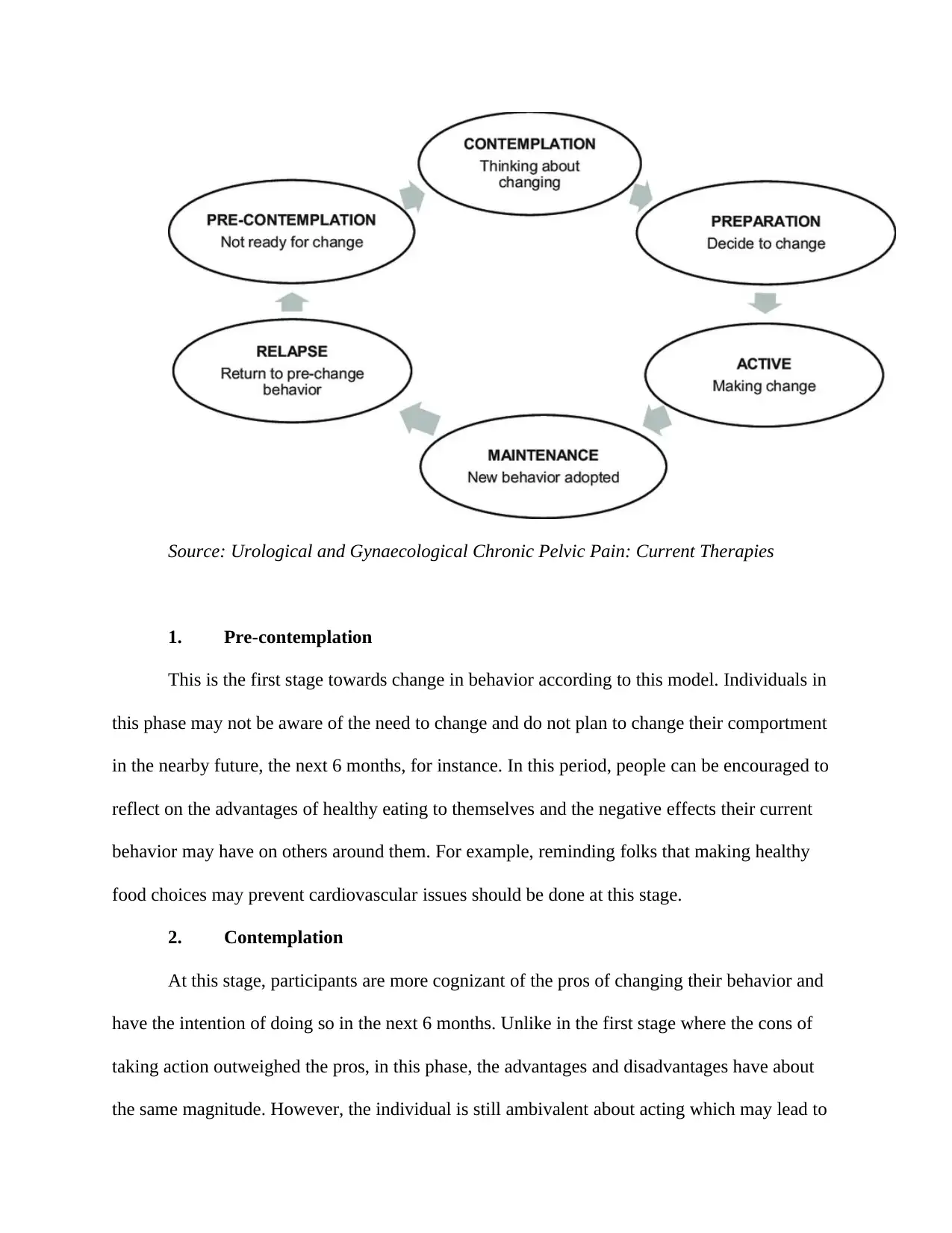
Source: Urological and Gynaecological Chronic Pelvic Pain: Current Therapies
1. Pre-contemplation
This is the first stage towards change in behavior according to this model. Individuals in
this phase may not be aware of the need to change and do not plan to change their comportment
in the nearby future, the next 6 months, for instance. In this period, people can be encouraged to
reflect on the advantages of healthy eating to themselves and the negative effects their current
behavior may have on others around them. For example, reminding folks that making healthy
food choices may prevent cardiovascular issues should be done at this stage.
2. Contemplation
At this stage, participants are more cognizant of the pros of changing their behavior and
have the intention of doing so in the next 6 months. Unlike in the first stage where the cons of
taking action outweighed the pros, in this phase, the advantages and disadvantages have about
the same magnitude. However, the individual is still ambivalent about acting which may lead to
1. Pre-contemplation
This is the first stage towards change in behavior according to this model. Individuals in
this phase may not be aware of the need to change and do not plan to change their comportment
in the nearby future, the next 6 months, for instance. In this period, people can be encouraged to
reflect on the advantages of healthy eating to themselves and the negative effects their current
behavior may have on others around them. For example, reminding folks that making healthy
food choices may prevent cardiovascular issues should be done at this stage.
2. Contemplation
At this stage, participants are more cognizant of the pros of changing their behavior and
have the intention of doing so in the next 6 months. Unlike in the first stage where the cons of
taking action outweighed the pros, in this phase, the advantages and disadvantages have about
the same magnitude. However, the individual is still ambivalent about acting which may lead to
constant postponing of the decision. In this instance, an individual meaning to start eating
healthier may be keeping off purchasing healthy meals time after time. In this stage, participants
learn about the kind of individuals they would be if they incorporated healthy behavior as well as
from other people who are already doing the same.
3. Preparation
People in the preparation stage are ready to take action toward adopting the new healthier
behavior in the very near future, for example, the following 30 days. They start small by taking
some steps which they believe will aid them in implementing the new behavior in their lives. An
example of making a healthy food choice in this stage is trying to make home-cooked meals as
often as possible so as to have a variety which may not be always on the menu. In this phase,
people should seek support from trusted friend and family and keep preparing themselves better.
4. Action
In this stage, the participants have changed their behavior recently and need to be
motivated to keep moving forward. In this case, individuals should strengthen their commitments
and keep checking their progress so as not to slip back. For instance, a person trying to avoid too
much sugar and sugary foodstuffs should avoid places that have lots of these sweet meals which
may keep them off track.(17) They should also develop substitutes to these meals and reward
themselves occasionally for the advancements they are making.
5. Maintenance
Individuals in this stage reformed their behavior a while ago (6 months). They should be
conscious of circumstances that may lure them into slipping back to their unhealthy behavior.
People should spend more time with others who eat healthily and focus more on healthy
healthier may be keeping off purchasing healthy meals time after time. In this stage, participants
learn about the kind of individuals they would be if they incorporated healthy behavior as well as
from other people who are already doing the same.
3. Preparation
People in the preparation stage are ready to take action toward adopting the new healthier
behavior in the very near future, for example, the following 30 days. They start small by taking
some steps which they believe will aid them in implementing the new behavior in their lives. An
example of making a healthy food choice in this stage is trying to make home-cooked meals as
often as possible so as to have a variety which may not be always on the menu. In this phase,
people should seek support from trusted friend and family and keep preparing themselves better.
4. Action
In this stage, the participants have changed their behavior recently and need to be
motivated to keep moving forward. In this case, individuals should strengthen their commitments
and keep checking their progress so as not to slip back. For instance, a person trying to avoid too
much sugar and sugary foodstuffs should avoid places that have lots of these sweet meals which
may keep them off track.(17) They should also develop substitutes to these meals and reward
themselves occasionally for the advancements they are making.
5. Maintenance
Individuals in this stage reformed their behavior a while ago (6 months). They should be
conscious of circumstances that may lure them into slipping back to their unhealthy behavior.
People should spend more time with others who eat healthily and focus more on healthy
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
behavior.(18) To do this, they should come up with better ways to cope with stress, for example,
exercising other than relying on food to improve their mood.
Relapse
This is not a stage of the transtheoretical model but only applies to individuals who
managed to change their behavior but then went back to the same old habits. Successful behavior
change requires ongoing support from trustworthy family and friends.
Discussion and Criticism of the Transtheoretical Model
Though arguably, the transtheoretical model has been termed the dominant theory in
behavior change.(5) The model can be employed to help people manage stress, prevent
depression, manage their weight as well as quit smoking.(19) However, no model is perfect and
thus this one has its cons as well depending on the field of application. In practice, the stages of
change model is difficult to assimilate and thus is implemented inadequately. Also, the model
does not have a distinguishable definition between the stages. Binding the stages on the basis of
time could be misleading as some people may take longer or a shorter period of time to be ready.
There is also no continuous version of the model that is applicable to all fields. Additionally, the
transtheoretical model assumes that individuals make stable, definite and coherent plans which
are often untrue.
References
1. Siddiqui TR, Ghazal S, Bibi S, Ahmed W, Sajjad SF. Use of the health belief
model for the assessment of public knowledge and household preventive practices in Karachi,
exercising other than relying on food to improve their mood.
Relapse
This is not a stage of the transtheoretical model but only applies to individuals who
managed to change their behavior but then went back to the same old habits. Successful behavior
change requires ongoing support from trustworthy family and friends.
Discussion and Criticism of the Transtheoretical Model
Though arguably, the transtheoretical model has been termed the dominant theory in
behavior change.(5) The model can be employed to help people manage stress, prevent
depression, manage their weight as well as quit smoking.(19) However, no model is perfect and
thus this one has its cons as well depending on the field of application. In practice, the stages of
change model is difficult to assimilate and thus is implemented inadequately. Also, the model
does not have a distinguishable definition between the stages. Binding the stages on the basis of
time could be misleading as some people may take longer or a shorter period of time to be ready.
There is also no continuous version of the model that is applicable to all fields. Additionally, the
transtheoretical model assumes that individuals make stable, definite and coherent plans which
are often untrue.
References
1. Siddiqui TR, Ghazal S, Bibi S, Ahmed W, Sajjad SF. Use of the health belief
model for the assessment of public knowledge and household preventive practices in Karachi,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Pakistan, a dengue-endemic city. PLoS neglected tropical diseases. 2016 Nov
10;10(11):e0005129.
2. Glanz K, Bishop DB. The role of behavioral science theory in development and
implementation of public health interventions. Annual review of public health. 2010 Apr
21;31:399-418.
3. Carpenter CJ. A meta-analysis of the effectiveness of health belief model
variables in predicting behavior. Health communication. 2010 Nov 30;25(8):661-9.
4. Pekmezi D, Barbera B, Marcus BH. Using the transtheoretical model to promote
physical activity. ACSM's Health & Fitness Journal. 2010 Jul 1;14(4):8-13.
5. Armitage CJ. Is there utility in the transtheoretical model?. British journal of
health psychology. 2009 May;14(2):195-210.
6. Zare M, Ghodsbin F, Jahanbin I, Ariafar A, Keshavarzi S, Izadi T. The effect of
health belief model-based education on knowledge and prostate cancer screening behaviors: a
randomized controlled trial. International journal of community based nursing and midwifery.
2016 Jan;4(1):57.
7. Shabibi P, Zavareh MS, Sayehmiri K, Qorbani M, Safari O, Rastegarimehr B,
Mansourian M. Effect of educational intervention based on the Health Belief Model on
promoting self-care behaviors of type-2 diabetes patients. Electronic physician. 2017
Dec;9(12):5960.
8. Orji R, Vassileva J, Mandryk R. Towards an effective health interventions design:
an extension of the health belief model. Online journal of public health informatics. 2012;4(3).
9. Kim HS, Ahn J, No JK. Applying the Health Belief Model to college students'
health behavior. Nutrition research and practice. 2012 Dec 1;6(6):551-8.
10;10(11):e0005129.
2. Glanz K, Bishop DB. The role of behavioral science theory in development and
implementation of public health interventions. Annual review of public health. 2010 Apr
21;31:399-418.
3. Carpenter CJ. A meta-analysis of the effectiveness of health belief model
variables in predicting behavior. Health communication. 2010 Nov 30;25(8):661-9.
4. Pekmezi D, Barbera B, Marcus BH. Using the transtheoretical model to promote
physical activity. ACSM's Health & Fitness Journal. 2010 Jul 1;14(4):8-13.
5. Armitage CJ. Is there utility in the transtheoretical model?. British journal of
health psychology. 2009 May;14(2):195-210.
6. Zare M, Ghodsbin F, Jahanbin I, Ariafar A, Keshavarzi S, Izadi T. The effect of
health belief model-based education on knowledge and prostate cancer screening behaviors: a
randomized controlled trial. International journal of community based nursing and midwifery.
2016 Jan;4(1):57.
7. Shabibi P, Zavareh MS, Sayehmiri K, Qorbani M, Safari O, Rastegarimehr B,
Mansourian M. Effect of educational intervention based on the Health Belief Model on
promoting self-care behaviors of type-2 diabetes patients. Electronic physician. 2017
Dec;9(12):5960.
8. Orji R, Vassileva J, Mandryk R. Towards an effective health interventions design:
an extension of the health belief model. Online journal of public health informatics. 2012;4(3).
9. Kim HS, Ahn J, No JK. Applying the Health Belief Model to college students'
health behavior. Nutrition research and practice. 2012 Dec 1;6(6):551-8.
10. Green EC, Murphy E. Health belief model. The Wiley Blackwell encyclopedia of
health, illness, behavior, and society. 2014 Jan 6:766-9.
11. Deshpande S, Basil MD, Basil DZ. Factors influencing healthy eating habits
among college students: An application of the health belief model. Health marketing quarterly.
2009 May 8;26(2):145-64.
12. Jones CJ, Smith H, Llewellyn C. Evaluating the effectiveness of health belief
model interventions in improving adherence: a systematic review. Health psychology review.
2014 Jul 3;8(3):253-69.
13. Sulat JS, Prabandari YS, Sanusi R, Hapsari ED, Santoso B. The validity of health
belief model variables in predicting behavioral change: A scoping review. Health Education.
2018 Oct 1;118(6):499-512.
14. McWhirter JE, Hoffman-Goetz L. Application of the health belief model to US
magazine text and image coverage of skin cancer and recreational tanning (2000–2012). Journal
of health communication. 2016 Apr 2;21(4):424-38.
15. Rawlett KE. Analytical evaluation of the health belief model and the vulnerable
populations conceptual model applied to a medically underserved rural population. International
Journal of Applied Science and Technology. 2011 Apr;1(2).
16. Gong F, Takeuchi DT. Ethnicity and health. InHandbook of Asian American
Health 2013 (pp. 3-9). Springer, New York, NY.
17. Prochaska JO, Norcross JC, DiClemente CC. Applying the stages of change.
Psychotherapy in Australia. 2013 Feb;19(2):10.
18. Norcross JC, Wampold BE. Adapting the relationship to the individual patient.
Evidence-based therapy relationships. 2010 Nov:27.
health, illness, behavior, and society. 2014 Jan 6:766-9.
11. Deshpande S, Basil MD, Basil DZ. Factors influencing healthy eating habits
among college students: An application of the health belief model. Health marketing quarterly.
2009 May 8;26(2):145-64.
12. Jones CJ, Smith H, Llewellyn C. Evaluating the effectiveness of health belief
model interventions in improving adherence: a systematic review. Health psychology review.
2014 Jul 3;8(3):253-69.
13. Sulat JS, Prabandari YS, Sanusi R, Hapsari ED, Santoso B. The validity of health
belief model variables in predicting behavioral change: A scoping review. Health Education.
2018 Oct 1;118(6):499-512.
14. McWhirter JE, Hoffman-Goetz L. Application of the health belief model to US
magazine text and image coverage of skin cancer and recreational tanning (2000–2012). Journal
of health communication. 2016 Apr 2;21(4):424-38.
15. Rawlett KE. Analytical evaluation of the health belief model and the vulnerable
populations conceptual model applied to a medically underserved rural population. International
Journal of Applied Science and Technology. 2011 Apr;1(2).
16. Gong F, Takeuchi DT. Ethnicity and health. InHandbook of Asian American
Health 2013 (pp. 3-9). Springer, New York, NY.
17. Prochaska JO, Norcross JC, DiClemente CC. Applying the stages of change.
Psychotherapy in Australia. 2013 Feb;19(2):10.
18. Norcross JC, Wampold BE. Adapting the relationship to the individual patient.
Evidence-based therapy relationships. 2010 Nov:27.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





