Analyzing Disease Risk Among Indigenous Populations: Remote Areas
VerifiedAdded on 2022/09/28
|13
|3660
|21
Report
AI Summary
This report critically analyzes the health disparities and disease risks among indigenous populations residing in remote areas. It emphasizes the influence of social determinants of health, such as employment, education, and infrastructure, on physical and mental well-being, highlighting how these factors contribute to increased disease prevalence. The report explores health inequalities stemming from unequal access to quality healthcare, inadequate infrastructure, and socioeconomic disparities. It also examines health inequities, which are characterized by unequal distribution of resources and opportunities. The study underscores the impact of limited access to healthcare services, including vaccination and preventive care, and highlights the increased rates of chronic diseases, mental health disorders, and infectious diseases within these communities. The report advocates for policy interventions and recommendations, including increased healthcare access, culturally sensitive healthcare delivery, and educational programs to improve health outcomes and address systemic inequalities. This report is a valuable resource for understanding the complex health challenges faced by indigenous communities and the urgent need for targeted interventions.

Running head: RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
Name of Student:
Name of University:
Author’s Note:
RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
Name of Student:
Name of University:
Author’s Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
Introduction
The indigenous group of Australia living in a remote area are at the considerable risk of
disease due to following factors like a social determinant of health, health inequality, and health
inequities. It results in the emergence of various lethal disease impact the indigenous group of
population. According to the study of Azzopardi et al. (2018), the place where the people live
and play shapes their atmosphere and create their opportunities for good health. Indigenous
communities living in remote area lack access to adequate healthcare service, unhealthy
environment and poor education due to which there is a high prevalence of disease. Therefore,
the main aim of the paper is to critically analyse the health disparity and risk of disease among
the indigenous population of remote area.
The social determinant of health like employment, education, improper infrastructure,
poor sanitation, income, poverty and distribution of health resource has affected the physical and
mental health in various ways like increase in the risk of disease. The indigenous people living in
remote areas are affected by above mentioned social determinant of health. It is reported that
people living in remote area estimate to be 40% of the population below poverty line (Readin &
Greenwood, 2018). There is only 8% of people who have received adequate education, and 93%
of the total indigenous of remote area are unemployed (Greenwood et al., 2015). It is also
reported that people living in remote area do not have healthy eating habit due to their low
socioeconomic status that has made him in higher risk of disease.
The health inequalities are the difference in the status of health that is experienced by the
people living in remote area and urban area. The indigenous community of remote area undergo
health inequalities that have increased the risk of disease. According to the study of Möller et al.
Introduction
The indigenous group of Australia living in a remote area are at the considerable risk of
disease due to following factors like a social determinant of health, health inequality, and health
inequities. It results in the emergence of various lethal disease impact the indigenous group of
population. According to the study of Azzopardi et al. (2018), the place where the people live
and play shapes their atmosphere and create their opportunities for good health. Indigenous
communities living in remote area lack access to adequate healthcare service, unhealthy
environment and poor education due to which there is a high prevalence of disease. Therefore,
the main aim of the paper is to critically analyse the health disparity and risk of disease among
the indigenous population of remote area.
The social determinant of health like employment, education, improper infrastructure,
poor sanitation, income, poverty and distribution of health resource has affected the physical and
mental health in various ways like increase in the risk of disease. The indigenous people living in
remote areas are affected by above mentioned social determinant of health. It is reported that
people living in remote area estimate to be 40% of the population below poverty line (Readin &
Greenwood, 2018). There is only 8% of people who have received adequate education, and 93%
of the total indigenous of remote area are unemployed (Greenwood et al., 2015). It is also
reported that people living in remote area do not have healthy eating habit due to their low
socioeconomic status that has made him in higher risk of disease.
The health inequalities are the difference in the status of health that is experienced by the
people living in remote area and urban area. The indigenous community of remote area undergo
health inequalities that have increased the risk of disease. According to the study of Möller et al.
2RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
(2015), significant determinants of health inequality in Australia is concerned to the lack of equal
access to quality health care and low standard of the health and medical infrastructure in the
remote areas which includes food, sanitation and healthy housing compared to other non-
indigenous people living in urban area of Australia. The indigenous people living in remote areas
do not receive medical resource, have low-grade school and do not enjoy the facilities like the
non-indigenous people. According to Zhao, Vemuri and Arya (2016), 70.3% of health gap is
noticed between the indigenous and non-indigenous Australian, especially people living in
remote areas, which can be attributed by risk and incidence of disease. The government of
Australia spends an unequal amount of money in the health care sector in the remote area. It is
reported that 0.2% of the total health expenditure has relied upon in the remote regions and 5.6%
of the GDP is invested the health care sector in the urban areas (Angell et al., 2017). Thus, as the
outcome of the health inequalities, the life expectancy of indigenous group of people is low, and
the health outcome is worse than the non-indigenous counterpart.
The health inequity is the other terms which are the contributing factor for making the
indigenous communities at high risk of disease. According to the research of Rolfe et al. (2017),
it is known that people living in the remote area have inferior health status, and social
determinant of health is the leading cause of health inequity. It is evident from the research of
Lindert and Williamson (2016) that the unequal distribution of income, proper schooling and
employment in the indigenous and non-indigenous communities has resulted in emergence of
health inequity. According to the world health organisation, health equity infers a requirement
for justice in providing access to healthcare, irrespective of a person's social, demographic,
geographic or economic position (World Health Organization, 2016). The Healthcare inequity
occurs among indigenous and non-indigenous communities in Australia, and it obstructs their
(2015), significant determinants of health inequality in Australia is concerned to the lack of equal
access to quality health care and low standard of the health and medical infrastructure in the
remote areas which includes food, sanitation and healthy housing compared to other non-
indigenous people living in urban area of Australia. The indigenous people living in remote areas
do not receive medical resource, have low-grade school and do not enjoy the facilities like the
non-indigenous people. According to Zhao, Vemuri and Arya (2016), 70.3% of health gap is
noticed between the indigenous and non-indigenous Australian, especially people living in
remote areas, which can be attributed by risk and incidence of disease. The government of
Australia spends an unequal amount of money in the health care sector in the remote area. It is
reported that 0.2% of the total health expenditure has relied upon in the remote regions and 5.6%
of the GDP is invested the health care sector in the urban areas (Angell et al., 2017). Thus, as the
outcome of the health inequalities, the life expectancy of indigenous group of people is low, and
the health outcome is worse than the non-indigenous counterpart.
The health inequity is the other terms which are the contributing factor for making the
indigenous communities at high risk of disease. According to the research of Rolfe et al. (2017),
it is known that people living in the remote area have inferior health status, and social
determinant of health is the leading cause of health inequity. It is evident from the research of
Lindert and Williamson (2016) that the unequal distribution of income, proper schooling and
employment in the indigenous and non-indigenous communities has resulted in emergence of
health inequity. According to the world health organisation, health equity infers a requirement
for justice in providing access to healthcare, irrespective of a person's social, demographic,
geographic or economic position (World Health Organization, 2016). The Healthcare inequity
occurs among indigenous and non-indigenous communities in Australia, and it obstructs their
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
access to universal healthcare coverage. It is also reported that due to rural geographic
conditions, remote and social-economic disparity and cultural differences, the indigenous
populations living in remote area tends to undergo a significantly higher rate of child
mortality, infant and perinatal mortality, low birth weight, risk of disease and age-standardised
death rates. The accessibility and availability of health care not only need strong financial and
geographical healthcare system, but the culture and language is also a critical aspect. According
to the research of D'Antoine and Bower (2019), the racial discrimination is the other significant
factors which are contributing to unequal access to health service and lack of adequate facility
that is being given in the urban population. The difference in culture and belief has widened the
gap of health inequity.
As the outcome of the health inequalities and health inequity, the rate of the disease has
increased and made them more vulnerable. Research suggests that indigenous people living in
remote areas took part in health risk behaviour more than the non-indigenous population and
made them at higher risk of disease (Hoy et al., 2015). The health outcome of the target
population is negatively impacted and resulted in the prevalence of various disease like
cardiovascular complication, diabetes, and kidney failure and lung infection. The above-stated
factors have caused an increase in 1.7 times higher level of malnutrition than the non-indigenous
people. The rate of hospitalisation has also increased for the chronic disease by the rate of 11
times (Morris et al., 2018). The key health issue that is noticed in the people living in remote
areas are obesity, cardiovascular, diabetes, infection, and COPD and Alzheimer disease (Roberts
et al., 2015). Due to the racial discrimination and cultural disparity, there is huge mental pressure
and mental stress which is the leading cause of the mental disorder. It is evident from the
research of Roberts et al. (2018) major mental illness observed in the people living in remote
access to universal healthcare coverage. It is also reported that due to rural geographic
conditions, remote and social-economic disparity and cultural differences, the indigenous
populations living in remote area tends to undergo a significantly higher rate of child
mortality, infant and perinatal mortality, low birth weight, risk of disease and age-standardised
death rates. The accessibility and availability of health care not only need strong financial and
geographical healthcare system, but the culture and language is also a critical aspect. According
to the research of D'Antoine and Bower (2019), the racial discrimination is the other significant
factors which are contributing to unequal access to health service and lack of adequate facility
that is being given in the urban population. The difference in culture and belief has widened the
gap of health inequity.
As the outcome of the health inequalities and health inequity, the rate of the disease has
increased and made them more vulnerable. Research suggests that indigenous people living in
remote areas took part in health risk behaviour more than the non-indigenous population and
made them at higher risk of disease (Hoy et al., 2015). The health outcome of the target
population is negatively impacted and resulted in the prevalence of various disease like
cardiovascular complication, diabetes, and kidney failure and lung infection. The above-stated
factors have caused an increase in 1.7 times higher level of malnutrition than the non-indigenous
people. The rate of hospitalisation has also increased for the chronic disease by the rate of 11
times (Morris et al., 2018). The key health issue that is noticed in the people living in remote
areas are obesity, cardiovascular, diabetes, infection, and COPD and Alzheimer disease (Roberts
et al., 2015). Due to the racial discrimination and cultural disparity, there is huge mental pressure
and mental stress which is the leading cause of the mental disorder. It is evident from the
research of Roberts et al. (2018) major mental illness observed in the people living in remote
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
areas are depression, anxiety, mood change, schizophrenia and dementia. Thus, it can be said
that due to socio-economic status, low income, unemployment, lack of access to health care
service and poor education has resulted in huge health inequalities and health inequities in the
indigenous group of populations. Such factors have made the community more vulnerable to
higher risk of disease.
The health disparity impacting the indigenous group of people living in
remote area
The term access to health care service refers to the ability of the people to obtain the
service that they seek and it is the major social determinant of health. The people living in
remote areas experience major health disparity as they lack equal access to health care service
that the urban population have. It is evident that access to health care service is a huge problem
for the indigenous group of the population living in remote areas. The health service that is
delivered to the Australian is related to preventive health service, hospital care, and primary and
community health service. The data on the Australian Childhood ImmunisationImmunisation
Register (ACIR) reveals that there is only 0.7% of the indigenous people in the remote receive
immunisation and vaccination against pneumonia, BCG and other (McGrail & Humphreys,
2015). As the impact, there is 78.6% of the disease rate of pneumonia, 67.5% tuberculosis and
45.7% of skin infection. The socio-economic barrier, like a low level of education, low income
and high rate of poverty, has made the access difficult for the indigenous group of population
(Thomas, Wakerman & Humphreys, 2015). Due to low financial problem, the people are not
able to visit GP for a regular health check-up. The lack of adequate health education has made
undergo tradition treatment that has increased the risk of disease. It is reported that there are
more than 45% of women diagnosed by late stage breast cancer (Hunter et al., 2019). The major
areas are depression, anxiety, mood change, schizophrenia and dementia. Thus, it can be said
that due to socio-economic status, low income, unemployment, lack of access to health care
service and poor education has resulted in huge health inequalities and health inequities in the
indigenous group of populations. Such factors have made the community more vulnerable to
higher risk of disease.
The health disparity impacting the indigenous group of people living in
remote area
The term access to health care service refers to the ability of the people to obtain the
service that they seek and it is the major social determinant of health. The people living in
remote areas experience major health disparity as they lack equal access to health care service
that the urban population have. It is evident that access to health care service is a huge problem
for the indigenous group of the population living in remote areas. The health service that is
delivered to the Australian is related to preventive health service, hospital care, and primary and
community health service. The data on the Australian Childhood ImmunisationImmunisation
Register (ACIR) reveals that there is only 0.7% of the indigenous people in the remote receive
immunisation and vaccination against pneumonia, BCG and other (McGrail & Humphreys,
2015). As the impact, there is 78.6% of the disease rate of pneumonia, 67.5% tuberculosis and
45.7% of skin infection. The socio-economic barrier, like a low level of education, low income
and high rate of poverty, has made the access difficult for the indigenous group of population
(Thomas, Wakerman & Humphreys, 2015). Due to low financial problem, the people are not
able to visit GP for a regular health check-up. The lack of adequate health education has made
undergo tradition treatment that has increased the risk of disease. It is reported that there are
more than 45% of women diagnosed by late stage breast cancer (Hunter et al., 2019). The major
5RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
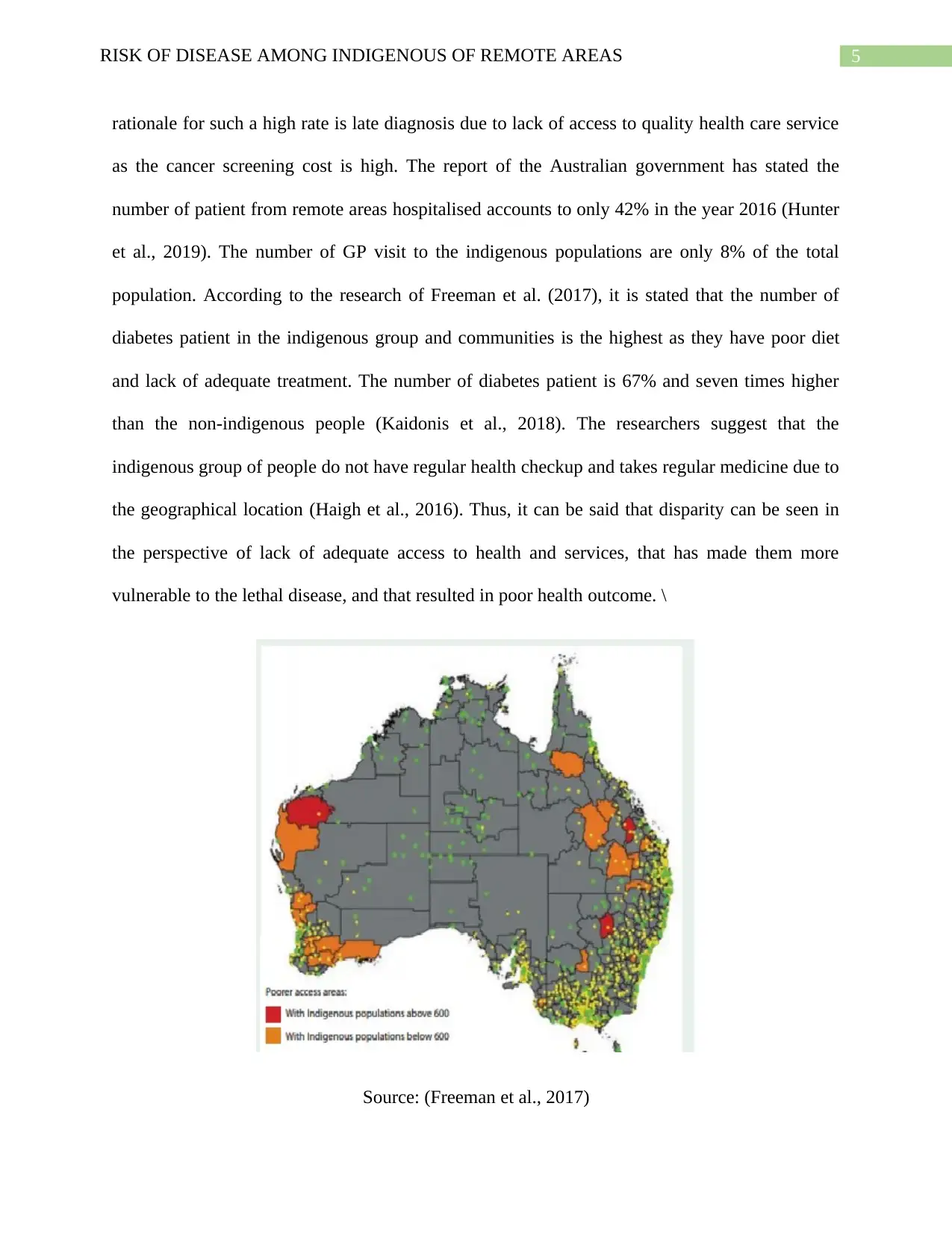
rationale for such a high rate is late diagnosis due to lack of access to quality health care service
as the cancer screening cost is high. The report of the Australian government has stated the
number of patient from remote areas hospitalised accounts to only 42% in the year 2016 (Hunter
et al., 2019). The number of GP visit to the indigenous populations are only 8% of the total
population. According to the research of Freeman et al. (2017), it is stated that the number of
diabetes patient in the indigenous group and communities is the highest as they have poor diet
and lack of adequate treatment. The number of diabetes patient is 67% and seven times higher
than the non-indigenous people (Kaidonis et al., 2018). The researchers suggest that the
indigenous group of people do not have regular health checkup and takes regular medicine due to
the geographical location (Haigh et al., 2016). Thus, it can be said that disparity can be seen in
the perspective of lack of adequate access to health and services, that has made them more
vulnerable to the lethal disease, and that resulted in poor health outcome. \
Source: (Freeman et al., 2017)
rationale for such a high rate is late diagnosis due to lack of access to quality health care service
as the cancer screening cost is high. The report of the Australian government has stated the
number of patient from remote areas hospitalised accounts to only 42% in the year 2016 (Hunter
et al., 2019). The number of GP visit to the indigenous populations are only 8% of the total
population. According to the research of Freeman et al. (2017), it is stated that the number of
diabetes patient in the indigenous group and communities is the highest as they have poor diet
and lack of adequate treatment. The number of diabetes patient is 67% and seven times higher
than the non-indigenous people (Kaidonis et al., 2018). The researchers suggest that the
indigenous group of people do not have regular health checkup and takes regular medicine due to
the geographical location (Haigh et al., 2016). Thus, it can be said that disparity can be seen in
the perspective of lack of adequate access to health and services, that has made them more
vulnerable to the lethal disease, and that resulted in poor health outcome. \
Source: (Freeman et al., 2017)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
The rate and risk of disease can conceptualise the impact of lack of access to health care
service. The effect on the health of the indigenous population of a remote area includes social,
environmental, economic and cultural factors. The remote area is having poor sanitation, high
rate of air and water pollution, that affect their health in negative manner. According to the study
of Reeve (2015), it is inferred that in 2017, the death rate of the indigenous population of remote
area was 13% due to coronary disease. The infection skin, borne disease and lung infection in
high among the indigenous population. The economic, social and cultural factors interconnected
that is known to affect the health of the population. Due to low purchasing power and low
income, they do not receive adequate health service and screening. It has increased the risk of
mental illness, cardiovascular complication and breast cancer (Belton et al., 2018). The cultural
belief of the indigenous population of the remote area, mainly focus on the traditional treatment,
that is not effective enough for faster recovery. Thus, it has also increased the risk of disease in
the indigenous population of the remote area.
Policy
To improve the health status of the indigenous population of the remote area, there is the
need to make a policy and make an advocacy program that will focus on to increase the access to
health care system, bridge the gap of health inequities and health inequalities (Kildea et al.,
2016). The health policy focus on the health promotion of the indigenous population of a remote
area by making the health care service accessible. Therefore, to bring it into action, local
foundation, health department and governmental body will be contacted for decision making.
The health care department is aware of the risk of disease-related to the community and a
possible way to address it. The nurses and health care professional provide evidence for the
widespread disease in the indigenous population of the remote area that will help in deciding for
The rate and risk of disease can conceptualise the impact of lack of access to health care
service. The effect on the health of the indigenous population of a remote area includes social,
environmental, economic and cultural factors. The remote area is having poor sanitation, high
rate of air and water pollution, that affect their health in negative manner. According to the study
of Reeve (2015), it is inferred that in 2017, the death rate of the indigenous population of remote
area was 13% due to coronary disease. The infection skin, borne disease and lung infection in
high among the indigenous population. The economic, social and cultural factors interconnected
that is known to affect the health of the population. Due to low purchasing power and low
income, they do not receive adequate health service and screening. It has increased the risk of
mental illness, cardiovascular complication and breast cancer (Belton et al., 2018). The cultural
belief of the indigenous population of the remote area, mainly focus on the traditional treatment,
that is not effective enough for faster recovery. Thus, it has also increased the risk of disease in
the indigenous population of the remote area.
Policy
To improve the health status of the indigenous population of the remote area, there is the
need to make a policy and make an advocacy program that will focus on to increase the access to
health care system, bridge the gap of health inequities and health inequalities (Kildea et al.,
2016). The health policy focus on the health promotion of the indigenous population of a remote
area by making the health care service accessible. Therefore, to bring it into action, local
foundation, health department and governmental body will be contacted for decision making.
The health care department is aware of the risk of disease-related to the community and a
possible way to address it. The nurses and health care professional provide evidence for the
widespread disease in the indigenous population of the remote area that will help in deciding for
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
the policy-making (White, Dudley-Brown & Terhaar, 2016). The local foundation of the remote
regions will give information about the health disparity and socio-economic issue that are
creating problem in accessing adequate health service. Such gathered information will be used by
the government and group of trustees for making the correct decision that will promote the health
of the indigenous population of remote area. It will require funds and approval from the
government for implementing the policy.
Recommendation
1. The nurse should provide evidence of the health issue and prevailing cause that will help
to make an adequate decision. They should visit the remote area and undertake regular
screening to evaluate the risk of disease in the population.
2. The project should focus on to deliver educational session in the native language of the
indigenous population of remote area.
3. The screening of the target population needs to be done efficiently by the volunteer to
access correct information.
Conclusion
Lastly, from the above discussion, it can be said that the policymaking and advocacy
program aims to promote the health of the indigenous population of the remote area, increase the
access to health care service and reduces the risk of disease. For this, the role of the registered
nurses is crucial to making the correct decision for policymaking. According to standard number
1 for RN by NMBA, they have the legal right for formulating decision with the goal of providing
equal health care and promoting health status. It is important to advocate for the indigenous
population of the remote area as the nurse, because of their legal responsibility of providing
the policy-making (White, Dudley-Brown & Terhaar, 2016). The local foundation of the remote
regions will give information about the health disparity and socio-economic issue that are
creating problem in accessing adequate health service. Such gathered information will be used by
the government and group of trustees for making the correct decision that will promote the health
of the indigenous population of remote area. It will require funds and approval from the
government for implementing the policy.
Recommendation
1. The nurse should provide evidence of the health issue and prevailing cause that will help
to make an adequate decision. They should visit the remote area and undertake regular
screening to evaluate the risk of disease in the population.
2. The project should focus on to deliver educational session in the native language of the
indigenous population of remote area.
3. The screening of the target population needs to be done efficiently by the volunteer to
access correct information.
Conclusion
Lastly, from the above discussion, it can be said that the policymaking and advocacy
program aims to promote the health of the indigenous population of the remote area, increase the
access to health care service and reduces the risk of disease. For this, the role of the registered
nurses is crucial to making the correct decision for policymaking. According to standard number
1 for RN by NMBA, they have the legal right for formulating decision with the goal of providing
equal health care and promoting health status. It is important to advocate for the indigenous
population of the remote area as the nurse, because of their legal responsibility of providing

8RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
adequate health care to the people as they can analyse and evaluate thoroughly the risk of
disease.
adequate health care to the people as they can analyse and evaluate thoroughly the risk of
disease.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
Reference
Angell, B., Laba, T. L., Lung, T., Brown, A., Eades, S., Usherwood, T., ... & Tonkin, A. (2017).
Healthcare expenditure on Indigenous and non-Indigenous Australians at high risk of
cardiovascular disease. International journal for equity in health, 16(1), 108.
Azzopardi, P. S., Sawyer, S. M., Carlin, J. B., Degenhardt, L., Brown, N., Brown, A. D., &
Patton, G. C. (2018). Health and wellbeing of Indigenous adolescents in Australia: a
systematic synthesis of population data. The Lancet, 391(10122), 766-782.
Belton, S., Kruske, S., Jackson Pulver, L., Sherwood, J., Tune, K., Carapetis, J., ... & Sullivan, E.
(2018). Rheumatic heart disease in pregnancy: How can health services adapt to the
needs of Indigenous women? A qualitative study. Australian and New Zealand Journal
of Obstetrics and Gynaecology, 58(4), 425-431.
D'Antoine, H., & Bower, C. (2019). Folate Status and Neural Tube Defects in Aboriginal
Australians: the Success of Mandatory Fortification in Reducing a Health
Disparity. Current developments in nutrition, 3(8), nzz071.
Freeman, C. R., Abdullah, N., Ford, P. J., & Taing, M. W. (2017). A national survey exploring
oral healthcare service provision across Australian community pharmacies. BMJ
open, 7(9), e017940.
Greenwood, M., De Leeuw, S., Lindsay, N. M., & Reading, C. (Eds.). (2015). Determinants of
Indigenous Peoples' Health. Canadian Scholars’ Press.
Reference
Angell, B., Laba, T. L., Lung, T., Brown, A., Eades, S., Usherwood, T., ... & Tonkin, A. (2017).
Healthcare expenditure on Indigenous and non-Indigenous Australians at high risk of
cardiovascular disease. International journal for equity in health, 16(1), 108.
Azzopardi, P. S., Sawyer, S. M., Carlin, J. B., Degenhardt, L., Brown, N., Brown, A. D., &
Patton, G. C. (2018). Health and wellbeing of Indigenous adolescents in Australia: a
systematic synthesis of population data. The Lancet, 391(10122), 766-782.
Belton, S., Kruske, S., Jackson Pulver, L., Sherwood, J., Tune, K., Carapetis, J., ... & Sullivan, E.
(2018). Rheumatic heart disease in pregnancy: How can health services adapt to the
needs of Indigenous women? A qualitative study. Australian and New Zealand Journal
of Obstetrics and Gynaecology, 58(4), 425-431.
D'Antoine, H., & Bower, C. (2019). Folate Status and Neural Tube Defects in Aboriginal
Australians: the Success of Mandatory Fortification in Reducing a Health
Disparity. Current developments in nutrition, 3(8), nzz071.
Freeman, C. R., Abdullah, N., Ford, P. J., & Taing, M. W. (2017). A national survey exploring
oral healthcare service provision across Australian community pharmacies. BMJ
open, 7(9), e017940.
Greenwood, M., De Leeuw, S., Lindsay, N. M., & Reading, C. (Eds.). (2015). Determinants of
Indigenous Peoples' Health. Canadian Scholars’ Press.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
Haigh, M., Shahid, S., O'Connor, K., & Thompson, S. C. (2016). Talking about the not talked
about: use of, and reactions to, a DVD promoting bowel cancer screening to Aboriginal
people. Australian and New Zealand journal of public health, 40(6), 548-552.
Hoy, W., White, A., Tipiloura, B., Singh, G., Sharma, S., Bloomfield, H., ... & McCredie, D.
(2015). The multideterminant model of renal disease in a remote Australian Aboriginal
population in the context of early life risk factors: lower birth weight, childhood post-
streptococcal glomerulonephritis, and current body mass index influence levels of
albuminuria in young Aboriginal adults. Clinical nephrology, 83(Supplement 1), 75-81.
Hunter, J., Smith, C., Delaney, G. P., Templeman, K., Grant, S., & Ussher, J. M. (2019).
Coverage of cancer services in Australia and providers’ views on service gaps: findings
from a national cross-sectional survey. BMC cancer, 19(1), 570.
Kaidonis, G., Hassall, M. M., Phillips, R., Raymond, G., Saha, N., Wong, G. H., ... & Newland,
H. (2018). Visual outcomes following vitrectomy for diabetic retinopathy amongst
Indigenous and non‐Indigenous Australians in South Australia and the Northern
Territory. Clinical & experimental ophthalmology, 46(4), 417-423.
Kildea, S., Tracy, S., Sherwood, J., Magick‐Dennis, F., & Barclay, L. (2016). Improving
maternity services for Indigenous women in Australia: moving from policy to
practice. Medical Journal of Australia, 205(8), 374-379.
Lindert, P. H., & Williamson, J. G. (2016). Unequal gains: American growth and inequality since
1700. Juncture, 22(4), 276-283.
McGrail, M. R., & Humphreys, J. S. (2015). Spatial access disparities to primary health care in
rural and remote Australia. Geospatial health.
Haigh, M., Shahid, S., O'Connor, K., & Thompson, S. C. (2016). Talking about the not talked
about: use of, and reactions to, a DVD promoting bowel cancer screening to Aboriginal
people. Australian and New Zealand journal of public health, 40(6), 548-552.
Hoy, W., White, A., Tipiloura, B., Singh, G., Sharma, S., Bloomfield, H., ... & McCredie, D.
(2015). The multideterminant model of renal disease in a remote Australian Aboriginal
population in the context of early life risk factors: lower birth weight, childhood post-
streptococcal glomerulonephritis, and current body mass index influence levels of
albuminuria in young Aboriginal adults. Clinical nephrology, 83(Supplement 1), 75-81.
Hunter, J., Smith, C., Delaney, G. P., Templeman, K., Grant, S., & Ussher, J. M. (2019).
Coverage of cancer services in Australia and providers’ views on service gaps: findings
from a national cross-sectional survey. BMC cancer, 19(1), 570.
Kaidonis, G., Hassall, M. M., Phillips, R., Raymond, G., Saha, N., Wong, G. H., ... & Newland,
H. (2018). Visual outcomes following vitrectomy for diabetic retinopathy amongst
Indigenous and non‐Indigenous Australians in South Australia and the Northern
Territory. Clinical & experimental ophthalmology, 46(4), 417-423.
Kildea, S., Tracy, S., Sherwood, J., Magick‐Dennis, F., & Barclay, L. (2016). Improving
maternity services for Indigenous women in Australia: moving from policy to
practice. Medical Journal of Australia, 205(8), 374-379.
Lindert, P. H., & Williamson, J. G. (2016). Unequal gains: American growth and inequality since
1700. Juncture, 22(4), 276-283.
McGrail, M. R., & Humphreys, J. S. (2015). Spatial access disparities to primary health care in
rural and remote Australia. Geospatial health.
11RISK OF DISEASE AMONG INDIGENOUS OF REMOTE AREAS
Möller, H., Falster, K., Ivers, R., & Jorm, L. (2015). Inequalities in unintentional injuries
between indigenous and non-indigenous children: a systematic review. Injury
prevention, 21(e1), e144-e152.
Morris, N. F., Stewart, S., Riley, M. D., & Maguire, G. P. (2018). The burden and nature of
malnutrition among patients in regional hospital settings: A cross-sectional
survey. Clinical nutrition ESPEN, 23, 1-9.
Reading, C., & Greenwood, M. (2018). Structural determinants of Aboriginal peoples’
health. Determinants of Indigenous Peoples' Health: Beyond the Social, 1.
Reeve, C., Humphreys, J., Wakerman, J., Carter, M., Carroll, V., & Reeve, D. (2015).
Strengthening primary health care: achieving health gains in a remote region of
Australia. Medical Journal of Australia, 202(9), 483-487.
Roberts, K. V., Maguire, G. P., Brown, A., Atkinson, D. N., Remenyi, B., Wheaton, G., ... &
Carapetis, J. (2015). Rheumatic heart disease in Indigenous children in northern
Australia: differences in prevalence and the challenges of screening. Medical Journal of
Australia, 203(5), 221-221.
Roberts, R., Lockett, H., Bagnall, C., Maylea, C., & Hopwood, M. (2018). Improving the
physical health of people living with mental illness in Australia and New
Zealand. Australian Journal of Rural Health, 26(5), 354-362.
Rolfe, M. I., Donoghue, D. A., Longman, J. M., Pilcher, J., Kildea, S., Kruske, S., ... & Morgan,
G. G. (2017). The distribution of maternity services across rural and remote Australia:
does it reflect population need?. BMC health services research, 17(1), 163.
Möller, H., Falster, K., Ivers, R., & Jorm, L. (2015). Inequalities in unintentional injuries
between indigenous and non-indigenous children: a systematic review. Injury
prevention, 21(e1), e144-e152.
Morris, N. F., Stewart, S., Riley, M. D., & Maguire, G. P. (2018). The burden and nature of
malnutrition among patients in regional hospital settings: A cross-sectional
survey. Clinical nutrition ESPEN, 23, 1-9.
Reading, C., & Greenwood, M. (2018). Structural determinants of Aboriginal peoples’
health. Determinants of Indigenous Peoples' Health: Beyond the Social, 1.
Reeve, C., Humphreys, J., Wakerman, J., Carter, M., Carroll, V., & Reeve, D. (2015).
Strengthening primary health care: achieving health gains in a remote region of
Australia. Medical Journal of Australia, 202(9), 483-487.
Roberts, K. V., Maguire, G. P., Brown, A., Atkinson, D. N., Remenyi, B., Wheaton, G., ... &
Carapetis, J. (2015). Rheumatic heart disease in Indigenous children in northern
Australia: differences in prevalence and the challenges of screening. Medical Journal of
Australia, 203(5), 221-221.
Roberts, R., Lockett, H., Bagnall, C., Maylea, C., & Hopwood, M. (2018). Improving the
physical health of people living with mental illness in Australia and New
Zealand. Australian Journal of Rural Health, 26(5), 354-362.
Rolfe, M. I., Donoghue, D. A., Longman, J. M., Pilcher, J., Kildea, S., Kruske, S., ... & Morgan,
G. G. (2017). The distribution of maternity services across rural and remote Australia:
does it reflect population need?. BMC health services research, 17(1), 163.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




