Health Economics Report: Evaluating NSW's E-health Digital Strategy
VerifiedAdded on 2023/06/07
|11
|1902
|459
Report
AI Summary
This report provides an analysis of the New South Wales (NSW) e-health strategy, focusing on the digitalization of healthcare services. It highlights the NSW government's initiative to build a healthcare system that delivers the 'Right Care, Right Place, Right Time' through the integration of digital technology. The report identifies key e-health priorities, including building a consistent foundation, integration, and personalization, which aim to improve patient-provider interaction, secure information sharing, and enhance overall healthcare quality. It also discusses the potential benefits of e-health, such as reduced staff stress, efficient patient records, and improved patient care outcomes, while addressing challenges like computer literacy among citizens. The report concludes with recommendations for successful e-health implementation, emphasizing interdisciplinary collaboration, simplified application design, and a focus on essential dimensions of health services. Desklib offers a platform for students to access similar solved assignments and study resources.

Running head: HEALTH ECONOMICS
NSW E-health report
Name of the Student
Name of the University
Author Note
NSW E-health report
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1HEALTH ECONOMICS
Table of Contents
Introduction......................................................................................................................................3
E-health priorities............................................................................................................................4
Discussion of findings.....................................................................................................................7
Recommendations............................................................................................................................8
References........................................................................................................................................9
Table of Contents
Introduction......................................................................................................................................3
E-health priorities............................................................................................................................4
Discussion of findings.....................................................................................................................7
Recommendations............................................................................................................................8
References........................................................................................................................................9
2HEALTH ECONOMICS
Executive Summary
E-health has been identified as an emerging field in recent years that involves the intersection of
public health, medical informatics, and business, in regards to health services, delivered through
the internet. In a broader sense, E-health describes a technical development and a commitment
for global and networked thinking, to improve healthcare. The report found that he NSW
Government started changing the healthcare service in 2011 for building a healthcare system that
delivers on the promise of ‘Right Care, Right Place, Right Time’. The NSW is working towards
digitalization of the healthcare system with the aim of improving patient-provider interaction,
secured sharing of electronic information, effective diagnosis of diseases, reducing medical
errors, and improving productivity.
Executive Summary
E-health has been identified as an emerging field in recent years that involves the intersection of
public health, medical informatics, and business, in regards to health services, delivered through
the internet. In a broader sense, E-health describes a technical development and a commitment
for global and networked thinking, to improve healthcare. The report found that he NSW
Government started changing the healthcare service in 2011 for building a healthcare system that
delivers on the promise of ‘Right Care, Right Place, Right Time’. The NSW is working towards
digitalization of the healthcare system with the aim of improving patient-provider interaction,
secured sharing of electronic information, effective diagnosis of diseases, reducing medical
errors, and improving productivity.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3HEALTH ECONOMICS
Introduction
The term E-health is a recent healthcare practice option supported by electronic
communication and processes and dates back to 1999. Although the term is often
interchangeably used with health informatics, it generally refers to the practice of healthcare with
the use of internet. This umbrella term often encompasses electronic health record, clinical
decision support systems, computerised physician order entries, telemedicine, e-prescribing,
consumer health informatics, and medical research with the use of grids (Kontos et al., 2014).
NSW health has been identified to deliver world class person-centred healthcare that is digitally
enabled for all people of NSW. It takes essential steps for incorporating the latest health
technology advances and ICT infrastructure, with the aim of delivering integrated accessible and
high quality healthcare (NSW Ministry of Health, 2014). The E-health strategy of NSW
comprises of using digital technology for transforming the way it delivers healthcare to all
patients, and takes into account the recent advances, policy directions, and ongoing
enhancement, for ensuring quality safety and performance of the health system. E-health will
help in reducing staff stress, make an accessible and efficient patient record, and reduce the
indirect work (Mohr et al., 2014). Moreover the procedure is time saving and also guarantees
best outcome for patient care. This report will analyse the NSW health state plan that aims to
digitalise healthcare.
Introduction
The term E-health is a recent healthcare practice option supported by electronic
communication and processes and dates back to 1999. Although the term is often
interchangeably used with health informatics, it generally refers to the practice of healthcare with
the use of internet. This umbrella term often encompasses electronic health record, clinical
decision support systems, computerised physician order entries, telemedicine, e-prescribing,
consumer health informatics, and medical research with the use of grids (Kontos et al., 2014).
NSW health has been identified to deliver world class person-centred healthcare that is digitally
enabled for all people of NSW. It takes essential steps for incorporating the latest health
technology advances and ICT infrastructure, with the aim of delivering integrated accessible and
high quality healthcare (NSW Ministry of Health, 2014). The E-health strategy of NSW
comprises of using digital technology for transforming the way it delivers healthcare to all
patients, and takes into account the recent advances, policy directions, and ongoing
enhancement, for ensuring quality safety and performance of the health system. E-health will
help in reducing staff stress, make an accessible and efficient patient record, and reduce the
indirect work (Mohr et al., 2014). Moreover the procedure is time saving and also guarantees
best outcome for patient care. This report will analyse the NSW health state plan that aims to
digitalise healthcare.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

4HEALTH ECONOMICS
Figure 1- E-health usage
Source- (NSW Ministry of Health, 2014)
E-health priorities
Typically E-health applications have the role of using the internet for transmitting and
storing patient data that can be used either by a provider or buy a service user. Digitalization of
the health care service by NSW will be achieved by utilisation of services and software that
allow to transmit, manage, record or store information, record keeping or payment. The three E-
health priorities as identified in the strategic plan are namely, (1) building consistent foundation,
(2) integration, and (3) personalization. Thus, NSW health will help in delivering integrated and
digitally enabled healthcare services to all clients (NSW Ministry of Health, 2016). The system
will focus on building the already existing processes in a way that the patients are provided the
opportunity to consistently interact with service providers, regardless of the region where they
Figure 1- E-health usage
Source- (NSW Ministry of Health, 2014)
E-health priorities
Typically E-health applications have the role of using the internet for transmitting and
storing patient data that can be used either by a provider or buy a service user. Digitalization of
the health care service by NSW will be achieved by utilisation of services and software that
allow to transmit, manage, record or store information, record keeping or payment. The three E-
health priorities as identified in the strategic plan are namely, (1) building consistent foundation,
(2) integration, and (3) personalization. Thus, NSW health will help in delivering integrated and
digitally enabled healthcare services to all clients (NSW Ministry of Health, 2016). The system
will focus on building the already existing processes in a way that the patients are provided the
opportunity to consistently interact with service providers, regardless of the region where they
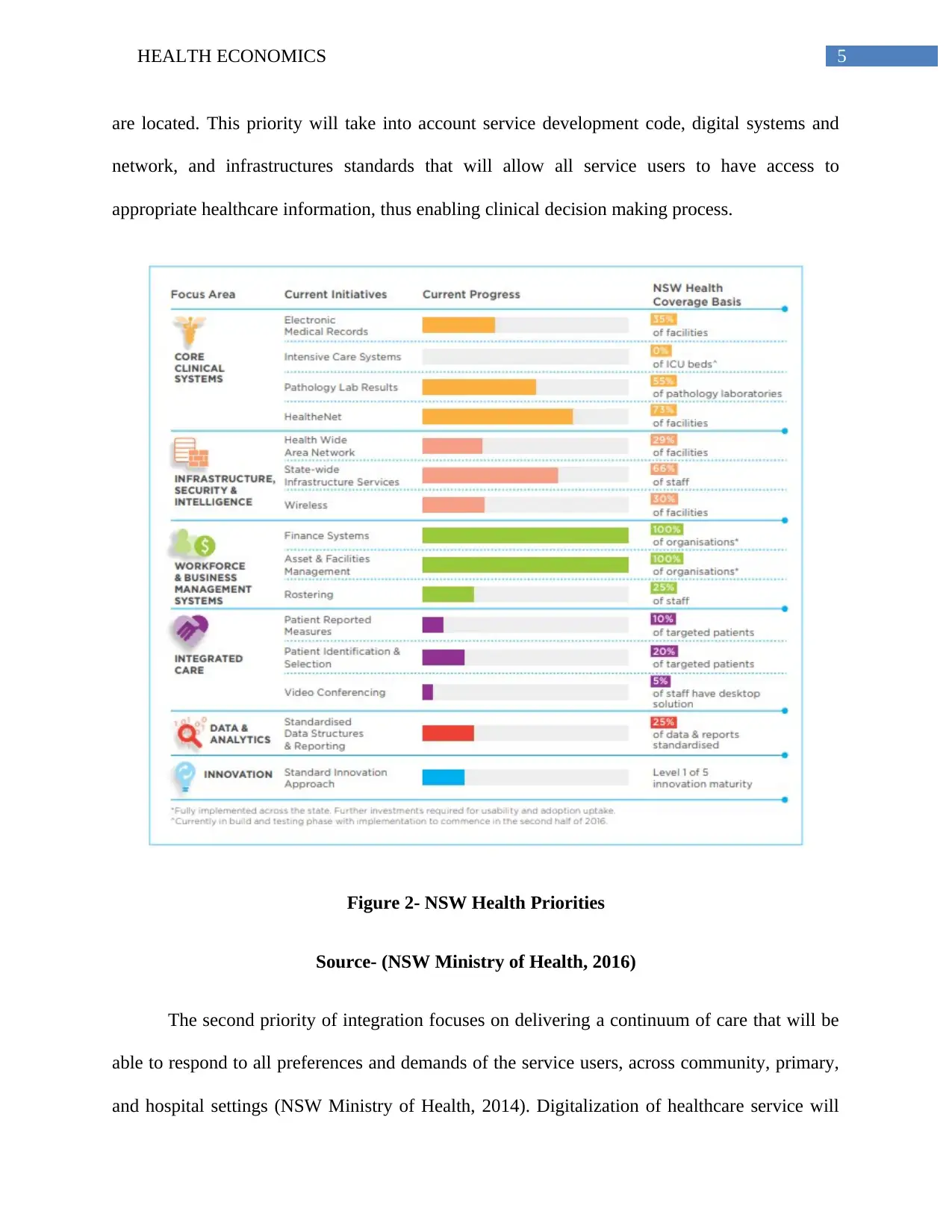
5HEALTH ECONOMICS
are located. This priority will take into account service development code, digital systems and
network, and infrastructures standards that will allow all service users to have access to
appropriate healthcare information, thus enabling clinical decision making process.
Figure 2- NSW Health Priorities
Source- (NSW Ministry of Health, 2016)
The second priority of integration focuses on delivering a continuum of care that will be
able to respond to all preferences and demands of the service users, across community, primary,
and hospital settings (NSW Ministry of Health, 2014). Digitalization of healthcare service will
are located. This priority will take into account service development code, digital systems and
network, and infrastructures standards that will allow all service users to have access to
appropriate healthcare information, thus enabling clinical decision making process.
Figure 2- NSW Health Priorities
Source- (NSW Ministry of Health, 2016)
The second priority of integration focuses on delivering a continuum of care that will be
able to respond to all preferences and demands of the service users, across community, primary,
and hospital settings (NSW Ministry of Health, 2014). Digitalization of healthcare service will
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

6HEALTH ECONOMICS
provide benefits to the patient and foster partnership with the providers, thereby delivering
integrated services. The third priority of personalization emphasizes on tailoring the services in
response to the needs of the patient that will allow them to play the role of active participants in
decision making and enhancing their wellbeing. An analysis of the priorities suggests that the
NSW plan will be beneficial for all patients in the long-run due to the advantages that E-health
will provide such as, increased safety, improved communication, reduced hospitalisation,
enhanced medication management, and access to electronic media (Bergmo, 2015).
Figure 3- Key initiatives
Source- (NSW Ministry of Health, 2016)
provide benefits to the patient and foster partnership with the providers, thereby delivering
integrated services. The third priority of personalization emphasizes on tailoring the services in
response to the needs of the patient that will allow them to play the role of active participants in
decision making and enhancing their wellbeing. An analysis of the priorities suggests that the
NSW plan will be beneficial for all patients in the long-run due to the advantages that E-health
will provide such as, increased safety, improved communication, reduced hospitalisation,
enhanced medication management, and access to electronic media (Bergmo, 2015).
Figure 3- Key initiatives
Source- (NSW Ministry of Health, 2016)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7HEALTH ECONOMICS
Discussion of findings
Upon analysing the E-health strategy it can be suggested that NSW should focus more on
allocating resources for digitalizing healthcare services across the state. This can be attributed to
the fact that spending resources on this emerging field of medical informatics will effectively
help in tackling the prevalence and spread of infectious diseases such as, tuberculosis, malaria,
and HIV (Tennant et al., 2015). It will also help in meeting the long-term care demands for an
aging population of the state and will improve the quality of treatment by broadening access to
medical care services. Spending more resources on digitalisation of health will reduce the
pressure on different public health care budget and lower the administrative burden by allowing
sharing of information in a secured manner (Bergmo, 2015).
NSW can produce digital infrastructure by the effective utilisation of digital community
based healthcare services such as, mobile health, health information technology, telemedicine,
personalized medicine, telehealth, and wearables (Mohr et al., 2014). Digitalizing an entire
hospital would take up huge amount of resources, when compared to the aforementioned
strategy. 70% of the supply needs must be addressed now, and the rest 30% should be kept for
future.
The digitalised healthcare services are used by healthcare professionals, patients and
family carers. Owing to the growing healthcare demands that is often governed by demographic
changes and a shortage of healthcare professionals, all service providers, patients, and citizens
can effectively use this means for exchanging or providing information, in order to improve
healthcare status, enhance person-centred care, increase equity of excess and foster cross-border
healthcare (Li et al., 2013). However, citizens of the state having limited computer literacy will
Discussion of findings
Upon analysing the E-health strategy it can be suggested that NSW should focus more on
allocating resources for digitalizing healthcare services across the state. This can be attributed to
the fact that spending resources on this emerging field of medical informatics will effectively
help in tackling the prevalence and spread of infectious diseases such as, tuberculosis, malaria,
and HIV (Tennant et al., 2015). It will also help in meeting the long-term care demands for an
aging population of the state and will improve the quality of treatment by broadening access to
medical care services. Spending more resources on digitalisation of health will reduce the
pressure on different public health care budget and lower the administrative burden by allowing
sharing of information in a secured manner (Bergmo, 2015).
NSW can produce digital infrastructure by the effective utilisation of digital community
based healthcare services such as, mobile health, health information technology, telemedicine,
personalized medicine, telehealth, and wearables (Mohr et al., 2014). Digitalizing an entire
hospital would take up huge amount of resources, when compared to the aforementioned
strategy. 70% of the supply needs must be addressed now, and the rest 30% should be kept for
future.
The digitalised healthcare services are used by healthcare professionals, patients and
family carers. Owing to the growing healthcare demands that is often governed by demographic
changes and a shortage of healthcare professionals, all service providers, patients, and citizens
can effectively use this means for exchanging or providing information, in order to improve
healthcare status, enhance person-centred care, increase equity of excess and foster cross-border
healthcare (Li et al., 2013). However, citizens of the state having limited computer literacy will
8HEALTH ECONOMICS
be unable to utilise the digitalised service efficiently, thereby not receiving quantifiable benefits
(Choi & DiNitto, 2013).
Recommendations
One major recommendation would be to involve and interdisciplinary team in the
development and enforcement of E-health services in the community. One of the prime
challenges would be to ensure a sound understanding of the complexities that are associated with
digitalization of health. Hence, all team members should be able to meet for discussions
approvals and clarifications to get them on the same board, before the application developers are
involved. The NSW should take attempts at minimising the requirement of user input into the
applications for keeping them relatively simple, while delivering personalized and safe messages
to all service users and providers as and when appropriate (Li et al., 2013). Digitalization of
health care service will show an increased likelihood to succeed when the NSW focuses on four
essential dimensions of health services such as, identifying and prioritising the essential sources
of values, building service delivery capabilities, modernizing foundations, and strengthening the
code management capabilities (Meier, Fitzgerald & Smith, 2013). Increasing access of patient
outcome, cost-to-care data, and satisfaction scores would also help in devising a new risk sharing
model with all the service providers. This should be followed by examination of the IT
infrastructure of all healthcare companies that will formulate the E-health applications (Van
Velsen, Wentzel & Van Gemert-Pijnen, 2013). Connectivity should also be incorporated into the
IT architecture with the use of monitoring technologies and sensors, for effectively generating
and managing data that are collected from the medical applications.
be unable to utilise the digitalised service efficiently, thereby not receiving quantifiable benefits
(Choi & DiNitto, 2013).
Recommendations
One major recommendation would be to involve and interdisciplinary team in the
development and enforcement of E-health services in the community. One of the prime
challenges would be to ensure a sound understanding of the complexities that are associated with
digitalization of health. Hence, all team members should be able to meet for discussions
approvals and clarifications to get them on the same board, before the application developers are
involved. The NSW should take attempts at minimising the requirement of user input into the
applications for keeping them relatively simple, while delivering personalized and safe messages
to all service users and providers as and when appropriate (Li et al., 2013). Digitalization of
health care service will show an increased likelihood to succeed when the NSW focuses on four
essential dimensions of health services such as, identifying and prioritising the essential sources
of values, building service delivery capabilities, modernizing foundations, and strengthening the
code management capabilities (Meier, Fitzgerald & Smith, 2013). Increasing access of patient
outcome, cost-to-care data, and satisfaction scores would also help in devising a new risk sharing
model with all the service providers. This should be followed by examination of the IT
infrastructure of all healthcare companies that will formulate the E-health applications (Van
Velsen, Wentzel & Van Gemert-Pijnen, 2013). Connectivity should also be incorporated into the
IT architecture with the use of monitoring technologies and sensors, for effectively generating
and managing data that are collected from the medical applications.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9HEALTH ECONOMICS
References
Bergmo, T. S. (2015). How to measure costs and benefits of eHealth interventions: an overview
of methods and frameworks. Journal of medical Internet research, 17(11), e254.
Choi, N. G., & DiNitto, D. M. (2013). The digital divide among low-income homebound older
adults: Internet use patterns, eHealth literacy, and attitudes toward computer/Internet
use. Journal of medical Internet research, 15(5), e93.
Kontos, E., Blake, K. D., Chou, W. Y. S., & Prestin, A. (2014). Predictors of eHealth usage:
insights on the digital divide from the Health Information National Trends Survey
2012. Journal of medical Internet research, 16(7), e172.
Li, J., Talaei-Khoei, A., Seale, H., Ray, P., & MacIntyre, C. R. (2013). Health care provider
adoption of eHealth: systematic literature review. Interactive journal of medical
research, 2(1), e7.
Meier, C. A., Fitzgerald, M. C., & Smith, J. M. (2013). eHealth: extending, enhancing, and
evolving health care. Annual review of biomedical engineering, 15, 359-382.
Mohr, D. C., Schueller, S. M., Montague, E., Burns, M. N., & Rashidi, P. (2014). The behavioral
intervention technology model: an integrated conceptual and technological framework for
eHealth and mHealth interventions. Journal of medical Internet research, 16(6), e146.
NSW Ministry of Health. (2014). NSW STATE HEALTH PLAN TOWARDS 2021. Retrieved
from https://www.health.nsw.gov.au/statehealthplan/Publications/NSW-State-Health-
Plan-Towards-2021.pdf.
References
Bergmo, T. S. (2015). How to measure costs and benefits of eHealth interventions: an overview
of methods and frameworks. Journal of medical Internet research, 17(11), e254.
Choi, N. G., & DiNitto, D. M. (2013). The digital divide among low-income homebound older
adults: Internet use patterns, eHealth literacy, and attitudes toward computer/Internet
use. Journal of medical Internet research, 15(5), e93.
Kontos, E., Blake, K. D., Chou, W. Y. S., & Prestin, A. (2014). Predictors of eHealth usage:
insights on the digital divide from the Health Information National Trends Survey
2012. Journal of medical Internet research, 16(7), e172.
Li, J., Talaei-Khoei, A., Seale, H., Ray, P., & MacIntyre, C. R. (2013). Health care provider
adoption of eHealth: systematic literature review. Interactive journal of medical
research, 2(1), e7.
Meier, C. A., Fitzgerald, M. C., & Smith, J. M. (2013). eHealth: extending, enhancing, and
evolving health care. Annual review of biomedical engineering, 15, 359-382.
Mohr, D. C., Schueller, S. M., Montague, E., Burns, M. N., & Rashidi, P. (2014). The behavioral
intervention technology model: an integrated conceptual and technological framework for
eHealth and mHealth interventions. Journal of medical Internet research, 16(6), e146.
NSW Ministry of Health. (2014). NSW STATE HEALTH PLAN TOWARDS 2021. Retrieved
from https://www.health.nsw.gov.au/statehealthplan/Publications/NSW-State-Health-
Plan-Towards-2021.pdf.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10HEALTH ECONOMICS
NSW Ministry of Health. (2016). eHealth Strategy for NSW Health 2016-2026. Retrieved from
https://www.health.nsw.gov.au/ehealth/documents/ehealth-strategy-for-nsw-health-2016-
2026.pdf.
Tennant, B., Stellefson, M., Dodd, V., Chaney, B., Chaney, D., Paige, S., & Alber, J. (2015).
eHealth literacy and Web 2.0 health information seeking behaviors among baby boomers
and older adults. Journal of medical Internet research, 17(3), e70.
Van Velsen, L., Wentzel, J., & Van Gemert-Pijnen, J. E. (2013). Designing eHealth that matters
via a multidisciplinary requirements development approach. JMIR research
protocols, 2(1), e21.
NSW Ministry of Health. (2016). eHealth Strategy for NSW Health 2016-2026. Retrieved from
https://www.health.nsw.gov.au/ehealth/documents/ehealth-strategy-for-nsw-health-2016-
2026.pdf.
Tennant, B., Stellefson, M., Dodd, V., Chaney, B., Chaney, D., Paige, S., & Alber, J. (2015).
eHealth literacy and Web 2.0 health information seeking behaviors among baby boomers
and older adults. Journal of medical Internet research, 17(3), e70.
Van Velsen, L., Wentzel, J., & Van Gemert-Pijnen, J. E. (2013). Designing eHealth that matters
via a multidisciplinary requirements development approach. JMIR research
protocols, 2(1), e21.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




