Research on Health Effects of Recreational Cannabis Use (1993-2013)
VerifiedAdded on 2023/06/14
|17
|17731
|204
Literature Review
AI Summary
This literature review examines the evidence on the adverse health effects of cannabis use, comparing findings from 1993 with those from 2013. It highlights that driving under the influence of cannabis approximately doubles the risk of car crashes, and about one in ten regular users develop dependence. Regular cannabis use during adolescence is associated with increased risks of early school leaving, cognitive impairment, and psychosis in adulthood, as well as the use of other illicit drugs. While cannabis smoking likely increases cardiovascular disease risk in middle-aged adults, its effects on respiratory function and cancer remain unclear due to concurrent tobacco use. The review concludes that cannabis use elevates the risk of accidents and dependence, with consistent links to poor psychosocial outcomes and mental health, emphasizing the need for continued research and informed public health strategies. Desklib provides access to similar documents and study tools for students.
What has research over the past two decades revealed
about the adverse health effects of recreational
cannabis use?
Wayne Hall1,2,3
The University of Queensland Centre for Youth Substance Abuse Research and The UQ Centre for ClinicalResearch, Herston, Australia,1 The National Addiction
Centre,Kings College London,London,UK2 and NationalDrug and AlcoholResearch Centre,University ofNew South Wales,New South Wales,Australia3
ABSTRACT
Aims To examine changes in the evidence on the adverse health effects ofcannabis since 1993.MethodsA
comparison ofthe evidence in 1993 with the evidence and interpretation ofthe same health outcomes in 2013.
ResultsResearch in the past 20 years has shown that driving while cannabis-impaired approximately doubles car
crash risk and that around one in 10 regular cannabis users develop dependence. Regular cannabis use in adolesce
approximately doubles the risks ofearly school-leaving and ofcognitive impairment and psychoses in adulthood.
Regular cannabis use in adolescence is also associated strongly with the use ofother illicit drugs. These associations
persist after controlling for plausible confounding variables in longitudinal studies. This suggests that cannabis use i
a contributory cause ofthese outcomes but some researchers stillargue that these relationships are explained by
shared causes or risk factors. Cannabis smoking probably increases cardiovascular disease risk in middle-aged adul
but its effects on respiratory function and respiratory cancer remain unclear, because most cannabis smokers have
smoked or still smoke tobacco. ConclusionsThe epidemiological literature in the past 20 years shows that cannabis
use increases the risk ofaccidents and can produce dependence, and that there are consistent associations between
regular cannabis use and poor psychosocial outcomes and mental health in adulthood.
Keywords Cannabis, dependence, drug-related harms, epidemiology, health risks, mental health.
Correspondence to: Wayne Hall, The University ofQueensland Centre for Youth Substance Abuse Research, Herston 4006, Australia. E-mail: w.hall@
uq.edu.au
Submitted 6 April 2014; initial review completed 21 May 2014; final version accepted 4 August 2014
WHY ARE WE CONCERNED ABOUT
RECREATIONAL CANNABIS USE?
During the past half-century,recreationalcannabis use
has become almost as common as tobacco use among
adolescents and young adults.Since its use was first
reported more than 40 years ago in the United States,
recreationalcannabis use has spread globally to other
developed countries and, more recently, low- and middle-
income countries [1,2].
The effects sought by cannabis users—euphoria and
increased sociability—seem to be produced primarily
by delta-9-tetrahydrocannabinol(THC) [3]. These
effects may be modulated by cannabidiol(CBD),a non-
psychoactive cannabinoid found in many cannabis prod-
ucts [3]. THC content is highest in the flowering tops of
the female cannabis plant. During the past 30 years the
THC contentof cannabis has increased in the United
States from <2% in 1980 to 8.5% in 2006 [4].THC
content has also increased in the Netherlands and prob-
ably in other developed countries [5].
Cannabis is usually smoked in a ‘joint’ or with a water
pipe (sometimes with tobacco added) because smoking is
the most efficient way to achieve the desired psychoactive
effects [3]. A dose of 2–3 mg of THC will produce a ‘high’
in occasional users who typically share a single joint with
others. Regular users may smoke up to three to five joints
of potent cannabis a day [6].
Paper presented atThrough the Maze:Cannabis and Health InternationalDrug Policy Symposium Auckland,New Zealand,
November 2013.
MONOGRAPH
bs_bs_banner
doi:10.1111/add.12703
© 2014 Society for the Study ofAddiction Addiction
about the adverse health effects of recreational
cannabis use?
Wayne Hall1,2,3
The University of Queensland Centre for Youth Substance Abuse Research and The UQ Centre for ClinicalResearch, Herston, Australia,1 The National Addiction
Centre,Kings College London,London,UK2 and NationalDrug and AlcoholResearch Centre,University ofNew South Wales,New South Wales,Australia3
ABSTRACT
Aims To examine changes in the evidence on the adverse health effects ofcannabis since 1993.MethodsA
comparison ofthe evidence in 1993 with the evidence and interpretation ofthe same health outcomes in 2013.
ResultsResearch in the past 20 years has shown that driving while cannabis-impaired approximately doubles car
crash risk and that around one in 10 regular cannabis users develop dependence. Regular cannabis use in adolesce
approximately doubles the risks ofearly school-leaving and ofcognitive impairment and psychoses in adulthood.
Regular cannabis use in adolescence is also associated strongly with the use ofother illicit drugs. These associations
persist after controlling for plausible confounding variables in longitudinal studies. This suggests that cannabis use i
a contributory cause ofthese outcomes but some researchers stillargue that these relationships are explained by
shared causes or risk factors. Cannabis smoking probably increases cardiovascular disease risk in middle-aged adul
but its effects on respiratory function and respiratory cancer remain unclear, because most cannabis smokers have
smoked or still smoke tobacco. ConclusionsThe epidemiological literature in the past 20 years shows that cannabis
use increases the risk ofaccidents and can produce dependence, and that there are consistent associations between
regular cannabis use and poor psychosocial outcomes and mental health in adulthood.
Keywords Cannabis, dependence, drug-related harms, epidemiology, health risks, mental health.
Correspondence to: Wayne Hall, The University ofQueensland Centre for Youth Substance Abuse Research, Herston 4006, Australia. E-mail: w.hall@
uq.edu.au
Submitted 6 April 2014; initial review completed 21 May 2014; final version accepted 4 August 2014
WHY ARE WE CONCERNED ABOUT
RECREATIONAL CANNABIS USE?
During the past half-century,recreationalcannabis use
has become almost as common as tobacco use among
adolescents and young adults.Since its use was first
reported more than 40 years ago in the United States,
recreationalcannabis use has spread globally to other
developed countries and, more recently, low- and middle-
income countries [1,2].
The effects sought by cannabis users—euphoria and
increased sociability—seem to be produced primarily
by delta-9-tetrahydrocannabinol(THC) [3]. These
effects may be modulated by cannabidiol(CBD),a non-
psychoactive cannabinoid found in many cannabis prod-
ucts [3]. THC content is highest in the flowering tops of
the female cannabis plant. During the past 30 years the
THC contentof cannabis has increased in the United
States from <2% in 1980 to 8.5% in 2006 [4].THC
content has also increased in the Netherlands and prob-
ably in other developed countries [5].
Cannabis is usually smoked in a ‘joint’ or with a water
pipe (sometimes with tobacco added) because smoking is
the most efficient way to achieve the desired psychoactive
effects [3]. A dose of 2–3 mg of THC will produce a ‘high’
in occasional users who typically share a single joint with
others. Regular users may smoke up to three to five joints
of potent cannabis a day [6].
Paper presented atThrough the Maze:Cannabis and Health InternationalDrug Policy Symposium Auckland,New Zealand,
November 2013.
MONOGRAPH
bs_bs_banner
doi:10.1111/add.12703
© 2014 Society for the Study ofAddiction Addiction
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
In epidemiological studies, ‘heavy’ or ‘regular’ canna-
bis use is usually defined as daily or near-daily use [6].
This pattern,when continued over years and decades,
predicts increased risk ofmany ofthe adverse health
effects attributed to cannabis that are reviewed below [6].
Unless stated otherwise, the remainder of this paper deals
with the adverse effects ofcannabis smoking, especially
the adverse health effects ofregular, typically daily, can-
nabis smoking.
OUR APPROACH TO THE LITERATURE
IN 1993
In 1993 there were very few epidemiological studies of the
health effects ofcannabis. The literature was dominated
by (i) animalstudies from the 1970s on the toxicity,
teratogenicity and carcinogenicity ofcannabis and THC;
and (ii) human laboratory studies from the late 1970s and
early 1980s on the effects ofsustained cannabis use over
7–35 days on the health ofcollege students. There was a
small number ofclinical studies ofadverse health effects
in heavy cannabis users from the same period [7,8].
In the early 1990s in Australia (as elsewhere) there
were strongly polarized views on the health effects of
cannabis.The published appraisals ofthe limited evi-
dence were refracted through the prism of the appraisers’
preferred policies towards cannabis (decriminalization or
legalization ofpersonal use versus intensified public edu-
cation and law enforcementcampaigns to discourage
use). We adopted the following approaches to maximize
the chances that our review would be seen as credible by
advocates ofthese very different competing public poli-
cies towards cannabis use.
First, Nadia Solowij,Jim Lemon and Iapplied the
standard rules for making causalinferences about the
health effects ofany drug to cannabis. That is, we looked
for: (i) epidemiologicalevidenceof an association
between cannabis use and the health outcome in case–
control and prospective studies; (ii) evidence that reverse
causation was an implausible explanation (e.g. evidence
from prospective studies that cannabis use preceded the
outcome); (iii) evidence from prospective studies that had
controlled for potentialconfounding variables (such as
other drug use and characteristics on which cannabis
usersdiffered from non-users);and (iv) clinical and
experimentalevidence which supported the biological
plausibility ofa causal relationship [9].
Secondly, we specified the standard ofproofthat we
would use in inferring thatcannabis was a probable
cause ofan adverse health effect; namely, evidence that
made it more likely than not that cannabis was a cause
of the adverse health effect. As we pointed out, very few
conclusionscould be drawn if we demanded proof
beyond reasonable doubt.We also identified possible
adverse health effects that required further investigation,
e.g. ifanimal and/or human evidence indicated an asso-
ciation between cannabis use and an adverse health effect
which was biologically plausible.
Thirdly,we were prepared to inferthat cannabis
could have adverse health effects when it: shared a route
of administration with cigarette smoking,e.g.respira-
tory disease,or produced similar acute effects to those
of alcohol,e.g.on driving and crash risk;and had
similar pharmacologicaleffectsto other long-acting
centralnervoussystem (CNS)depressantdrugs,e.g.
benzodiazepines.
Fourthly,we compared the probable adverse health
effects ofcannabis with the known adverse health effects
of alcohol and tobacco. We aimed to do so in a way that
used the same evidentialstandards in drawing causal
inferences about the probable adverse health effects ofall
three drugs.
In the following analysis I apply these criteria to the
more substantialresearch evidence thathas accumu-
lated over the past 20 years on the adverse health effects
of cannabis.For each type ofadverse health effect,I
(i) briefly summarize the conclusions drawn in 1993;
(ii) explain the reasons given for these conclusions; and
(iii) compare the conclusions reached in 1993 with the
inferences that may reasonably be drawn in 2013. The
review begins with acute adverse health effects,those
that may arise from a single episode ofintoxication.It
then considersthe adverse health and psychological
effects ofregular cannabis use over periods ofyears and
decades.
ADVERSE ACUTE HEALTH EFFECTS
In 1993 the evidence indicated that the risk ofa fatal
overdose from using cannabis was extremely small. This
remains an uncontroversial conclusion, because the dose
of THC that kills rodents is extremely high. The estimated
fatal dose in humansderived from animalstudiesis
between 15 [10]and 70 g [3].This is a far greater
amount of cannabis that even a very heavy cannabis user
could use in a day [10]. There are also no reports offatal
overdoses in the epidemiologicalliterature [11].There
have been case reportsof cardiovascularfatalitiesin
seemingly otherwise healthy young men after smoking
cannabis [12] that are discussed below under ‘Cardiovas-
cular effects’ ofcannabis smoking.
In 1993 we identified the following adverse acute
effects of cannabis use: (i) unpleasant experiences such as
anxiety, dysphoria and paranoia, especially among naive
users;(ii) cognitive impairment,especially ofattention
and memory;(iii) psychomotor impairment that could
impair a person’s ability to drive a motor vehicle while
intoxicated; (iv) an increased risk ofpsychotic symptoms
2 Wayne Hall
© 2014 Society for the Study ofAddiction Addiction
bis use is usually defined as daily or near-daily use [6].
This pattern,when continued over years and decades,
predicts increased risk ofmany ofthe adverse health
effects attributed to cannabis that are reviewed below [6].
Unless stated otherwise, the remainder of this paper deals
with the adverse effects ofcannabis smoking, especially
the adverse health effects ofregular, typically daily, can-
nabis smoking.
OUR APPROACH TO THE LITERATURE
IN 1993
In 1993 there were very few epidemiological studies of the
health effects ofcannabis. The literature was dominated
by (i) animalstudies from the 1970s on the toxicity,
teratogenicity and carcinogenicity ofcannabis and THC;
and (ii) human laboratory studies from the late 1970s and
early 1980s on the effects ofsustained cannabis use over
7–35 days on the health ofcollege students. There was a
small number ofclinical studies ofadverse health effects
in heavy cannabis users from the same period [7,8].
In the early 1990s in Australia (as elsewhere) there
were strongly polarized views on the health effects of
cannabis.The published appraisals ofthe limited evi-
dence were refracted through the prism of the appraisers’
preferred policies towards cannabis (decriminalization or
legalization ofpersonal use versus intensified public edu-
cation and law enforcementcampaigns to discourage
use). We adopted the following approaches to maximize
the chances that our review would be seen as credible by
advocates ofthese very different competing public poli-
cies towards cannabis use.
First, Nadia Solowij,Jim Lemon and Iapplied the
standard rules for making causalinferences about the
health effects ofany drug to cannabis. That is, we looked
for: (i) epidemiologicalevidenceof an association
between cannabis use and the health outcome in case–
control and prospective studies; (ii) evidence that reverse
causation was an implausible explanation (e.g. evidence
from prospective studies that cannabis use preceded the
outcome); (iii) evidence from prospective studies that had
controlled for potentialconfounding variables (such as
other drug use and characteristics on which cannabis
usersdiffered from non-users);and (iv) clinical and
experimentalevidence which supported the biological
plausibility ofa causal relationship [9].
Secondly, we specified the standard ofproofthat we
would use in inferring thatcannabis was a probable
cause ofan adverse health effect; namely, evidence that
made it more likely than not that cannabis was a cause
of the adverse health effect. As we pointed out, very few
conclusionscould be drawn if we demanded proof
beyond reasonable doubt.We also identified possible
adverse health effects that required further investigation,
e.g. ifanimal and/or human evidence indicated an asso-
ciation between cannabis use and an adverse health effect
which was biologically plausible.
Thirdly,we were prepared to inferthat cannabis
could have adverse health effects when it: shared a route
of administration with cigarette smoking,e.g.respira-
tory disease,or produced similar acute effects to those
of alcohol,e.g.on driving and crash risk;and had
similar pharmacologicaleffectsto other long-acting
centralnervoussystem (CNS)depressantdrugs,e.g.
benzodiazepines.
Fourthly,we compared the probable adverse health
effects ofcannabis with the known adverse health effects
of alcohol and tobacco. We aimed to do so in a way that
used the same evidentialstandards in drawing causal
inferences about the probable adverse health effects ofall
three drugs.
In the following analysis I apply these criteria to the
more substantialresearch evidence thathas accumu-
lated over the past 20 years on the adverse health effects
of cannabis.For each type ofadverse health effect,I
(i) briefly summarize the conclusions drawn in 1993;
(ii) explain the reasons given for these conclusions; and
(iii) compare the conclusions reached in 1993 with the
inferences that may reasonably be drawn in 2013. The
review begins with acute adverse health effects,those
that may arise from a single episode ofintoxication.It
then considersthe adverse health and psychological
effects ofregular cannabis use over periods ofyears and
decades.
ADVERSE ACUTE HEALTH EFFECTS
In 1993 the evidence indicated that the risk ofa fatal
overdose from using cannabis was extremely small. This
remains an uncontroversial conclusion, because the dose
of THC that kills rodents is extremely high. The estimated
fatal dose in humansderived from animalstudiesis
between 15 [10]and 70 g [3].This is a far greater
amount of cannabis that even a very heavy cannabis user
could use in a day [10]. There are also no reports offatal
overdoses in the epidemiologicalliterature [11].There
have been case reportsof cardiovascularfatalitiesin
seemingly otherwise healthy young men after smoking
cannabis [12] that are discussed below under ‘Cardiovas-
cular effects’ ofcannabis smoking.
In 1993 we identified the following adverse acute
effects of cannabis use: (i) unpleasant experiences such as
anxiety, dysphoria and paranoia, especially among naive
users;(ii) cognitive impairment,especially ofattention
and memory;(iii) psychomotor impairment that could
impair a person’s ability to drive a motor vehicle while
intoxicated; (iv) an increased risk ofpsychotic symptoms
2 Wayne Hall
© 2014 Society for the Study ofAddiction Addiction
in high doses, especially among those with a personal or
family history ofpsychosis; and (v) an increased risk of
low birth weightbabies,if cannabis was used during
pregnancy.
The acute adverse effects ofanxiety, panic reactions
and psychotic symptoms continue to be reported,espe-
cially by naive users [6]. During the past decade there has
been an increase in the number ofattendances at hospi-
tal emergency rooms in the United States in which can-
nabis is ‘mentioned’ [13]. This could reflect an increase in
acute adverse effects in naive users as the average THC
content ofcannabis products has risen, an issue that is
discussed further below.
Car crash injuries and deaths
In 1993 it was clear from laboratory studies that canna-
bis and THC produced dose-related impairmentsin
reaction-time, information-processing, perceptual-motor
coordination, motor performance, attention and tracking
behaviour. This suggested that cannabis could potentially
cause car crashes ifusers drove while intoxicated, but it
was unclear whether in fact cannabis use did so. Studies
in driving simulators suggested that cannabis-impaired
drivers were aware of their impairment and compensated
for these effects by slowing down and taking fewer risks.
There were similar findings in the few studies on the
effects of cannabis use on driving on the road (see [14] for
a review).
In 1993 there were major problems in interpreting
the few epidemiological studies ofcannabis use in fatal
car crashes.Most reported on cannabismetabolites,
which indicated only that cannabis had been used in the
days before the accident;they did notshow thatthe
drivers were cannabis-impaired at the time ofthe acci-
dent.Moreover,in many ofthese studies a substantial
proportion ofdrivers with cannabis in their blood also
had high blood alcohol levels, making it difficult to distin-
guish between the effects of cannabis and alcohol on acci-
dent risk [9].
In the pastdecade,better-designed epidemiological
studies have found that cannabis users who drive while
intoxicated approximately double their risk of a car crash.
Gerberich et al.[15],for example,found that cannabis
users had higher rates ofhospitalization for injury from
all causes than former cannabis users or non-users in
64 657 patients from a Health Maintenance Organiza-
tion (HMO). The relative risk (RR) ofmotor vehicle acci-
dents (RR = 1.96) persisted after statisticaladjustment
for confounding in men. Mura et al. [16] found a similar
relationship in a case–control study of THC in the serum
of 900 people hospitalized in France with motor vehicle
injuries and 900 age- and sex-matched controls admitted
to the same hospitals for reasons other than trauma.
A meta-analysis ofnine case–control and culpability
studies [17] found that recent cannabis use (indicated
by THC in blood or self-reported cannabis use) doubled
the risk ofa car crash [odds ratio (OR) = 1.92 95% con-
fidence interval (CI) = 1.35, 2.73]. The risk was margin-
ally higher in: better-designed studies (2.21 versus 1.78),
in case–controlratherthan driverculpability studies
(2.79 versus 1.65) and in studies offatalities rather than
injuries (2.10 versus 1.74).Very similar results were
reported in another meta-analysis [18](pooled risk of
2.66) and in a systematic review oflaboratory and epi-
demiological studies [19].
In summary, the epidemiological and laboratory evi-
dence on the acute effects ofcannabis suggests strongly
that cannabis users who drive while intoxicated increase
their risk ofmotor vehicle crashes 2–3 times [20]as
against 6–15 times for comparable intoxicating doses of
alcohol. Cannabis use was estimated to account for 2.5%
of traffic deaths in France as against 29% for alcohol. The
risk of an accidentincreases substantially ifcannabis
users also have elevated blood alcohol levels [19].
Reproductive effects ofcannabis use
Fetal development and birth defects
In 1993 animal studies suggested that high doses of can-
nabis extract caused growth retardation and birth mal-
formations[21], but epidemiologicalstudiesdid not
consistently find an increased risk ofbirth defects among
women who reported using cannabis during pregnancy.
It was also difficultto interpretthe few studiesthat
reported increased ratesof birth defects(e.g.[22]),
becausecannabisusers were more likely to smoke
tobacco and use alcoholand other illicit drugs during
pregnancy [23]. They were also less likely to seek antena-
tal care and had poorer nutrition than women who did
not use cannabis [24]. Zuckerman et al. [25] reported the
most convincing failure to find an increased risk ofbirth
defects in a study ofa large sample ofwomen among
whom there was a substantial rate ofcannabis use that
was measured by urinalysis rather than self-report.
A meta-analysis [26]of studies in the 1980s and
1990s suggested that regular cannabis use during preg-
nancy reduced birth weight,although the effectwas
smaller than that for tobacco smoking. Several large epi-
demiologicalstudies have since reported that cannabis
use in pregnancyis associatedwith reducedbirth
weight (e.g. [27,28]). This effect has generally persisted
aftercontrolling statistically forother drug use (e.g.
[25,28,29]).Severalof these studies also reported that
women who used cannabis had a shorter duration of
labour and an increased risk ofbabies smallfor gesta-
tional age [27].
Cannabis health effects3
© 2014 Society for the Study ofAddiction Addiction
family history ofpsychosis; and (v) an increased risk of
low birth weightbabies,if cannabis was used during
pregnancy.
The acute adverse effects ofanxiety, panic reactions
and psychotic symptoms continue to be reported,espe-
cially by naive users [6]. During the past decade there has
been an increase in the number ofattendances at hospi-
tal emergency rooms in the United States in which can-
nabis is ‘mentioned’ [13]. This could reflect an increase in
acute adverse effects in naive users as the average THC
content ofcannabis products has risen, an issue that is
discussed further below.
Car crash injuries and deaths
In 1993 it was clear from laboratory studies that canna-
bis and THC produced dose-related impairmentsin
reaction-time, information-processing, perceptual-motor
coordination, motor performance, attention and tracking
behaviour. This suggested that cannabis could potentially
cause car crashes ifusers drove while intoxicated, but it
was unclear whether in fact cannabis use did so. Studies
in driving simulators suggested that cannabis-impaired
drivers were aware of their impairment and compensated
for these effects by slowing down and taking fewer risks.
There were similar findings in the few studies on the
effects of cannabis use on driving on the road (see [14] for
a review).
In 1993 there were major problems in interpreting
the few epidemiological studies ofcannabis use in fatal
car crashes.Most reported on cannabismetabolites,
which indicated only that cannabis had been used in the
days before the accident;they did notshow thatthe
drivers were cannabis-impaired at the time ofthe acci-
dent.Moreover,in many ofthese studies a substantial
proportion ofdrivers with cannabis in their blood also
had high blood alcohol levels, making it difficult to distin-
guish between the effects of cannabis and alcohol on acci-
dent risk [9].
In the pastdecade,better-designed epidemiological
studies have found that cannabis users who drive while
intoxicated approximately double their risk of a car crash.
Gerberich et al.[15],for example,found that cannabis
users had higher rates ofhospitalization for injury from
all causes than former cannabis users or non-users in
64 657 patients from a Health Maintenance Organiza-
tion (HMO). The relative risk (RR) ofmotor vehicle acci-
dents (RR = 1.96) persisted after statisticaladjustment
for confounding in men. Mura et al. [16] found a similar
relationship in a case–control study of THC in the serum
of 900 people hospitalized in France with motor vehicle
injuries and 900 age- and sex-matched controls admitted
to the same hospitals for reasons other than trauma.
A meta-analysis ofnine case–control and culpability
studies [17] found that recent cannabis use (indicated
by THC in blood or self-reported cannabis use) doubled
the risk ofa car crash [odds ratio (OR) = 1.92 95% con-
fidence interval (CI) = 1.35, 2.73]. The risk was margin-
ally higher in: better-designed studies (2.21 versus 1.78),
in case–controlratherthan driverculpability studies
(2.79 versus 1.65) and in studies offatalities rather than
injuries (2.10 versus 1.74).Very similar results were
reported in another meta-analysis [18](pooled risk of
2.66) and in a systematic review oflaboratory and epi-
demiological studies [19].
In summary, the epidemiological and laboratory evi-
dence on the acute effects ofcannabis suggests strongly
that cannabis users who drive while intoxicated increase
their risk ofmotor vehicle crashes 2–3 times [20]as
against 6–15 times for comparable intoxicating doses of
alcohol. Cannabis use was estimated to account for 2.5%
of traffic deaths in France as against 29% for alcohol. The
risk of an accidentincreases substantially ifcannabis
users also have elevated blood alcohol levels [19].
Reproductive effects ofcannabis use
Fetal development and birth defects
In 1993 animal studies suggested that high doses of can-
nabis extract caused growth retardation and birth mal-
formations[21], but epidemiologicalstudiesdid not
consistently find an increased risk ofbirth defects among
women who reported using cannabis during pregnancy.
It was also difficultto interpretthe few studiesthat
reported increased ratesof birth defects(e.g.[22]),
becausecannabisusers were more likely to smoke
tobacco and use alcoholand other illicit drugs during
pregnancy [23]. They were also less likely to seek antena-
tal care and had poorer nutrition than women who did
not use cannabis [24]. Zuckerman et al. [25] reported the
most convincing failure to find an increased risk ofbirth
defects in a study ofa large sample ofwomen among
whom there was a substantial rate ofcannabis use that
was measured by urinalysis rather than self-report.
A meta-analysis [26]of studies in the 1980s and
1990s suggested that regular cannabis use during preg-
nancy reduced birth weight,although the effectwas
smaller than that for tobacco smoking. Several large epi-
demiologicalstudies have since reported that cannabis
use in pregnancyis associatedwith reducedbirth
weight (e.g. [27,28]). This effect has generally persisted
aftercontrolling statistically forother drug use (e.g.
[25,28,29]).Severalof these studies also reported that
women who used cannabis had a shorter duration of
labour and an increased risk ofbabies smallfor gesta-
tional age [27].
Cannabis health effects3
© 2014 Society for the Study ofAddiction Addiction
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
These studies have a number oflimitations. First, self-
reported rates of cannabis use during pregnancy are typi-
cally low (2–6%). Studies that have measured cannabis
use using urinalyses suggest that there is considerable
under-reporting ofuse, which probably attenuates asso-
ciations between cannabis use and poor birth outcomes.
Secondly, it has often been difficult to fully adjust for the
effects ofmajor confounders such as cigarette smoking
in analyses of the effects of cannabis use on birth weight.
None the less,there is a good case on the grounds of
prudence for recommending that women should avoid
using cannabis while pregnant,or while attempting to
become pregnant.
Postnatal effects ofmaternal cannabis use
In 1993 a smallnumber ofstudies reported increased
rates ofdevelopmental abnormalities in children born to
women who used cannabis during pregnancy,such as
developmental delays in the visual system and increased
tremor and startle shortly after birth [30]. These effects
were not reported consistently in later assessments; e.g.
some were notdetected atthe age of1 month or on
ability tests at 6 and 12 months. Others were reported at
36 and 48 months, but not at 60 and 72 months [30]. As
these children entered adolescence,maternalcannabis
was associated with poorer cognitive performance. In the
Ontario study, at age 12 years, there were no differences
in full-scale IQ scores between children who were and
were not exposed to cannabis, but there were differences
in perceptual organization and higher cognitive processes
[30]. Tennes et al. [24], by contrast, found no IQ differ-
ences at 1 year between the children ofusers and nonus-
ers in 756 women, a third of whom used cannabis during
pregnancy.
In the past 20 years another cohort oflow-income
women with higher rates ofregular cannabis use [31]
has reported lower scores on memory and verbal scales of
the Stanford–Binet Intelligence Scale at age 3 in children
born to 655 low-income women (halfAfrican American
and halfCaucasian) in Pittsburgh between 1990 and
1995. By age 10, maternal cannabis use at all stages of
pregnancy was associated with delinquency and problem
behaviour[32]. Cannabis-exposed children also per-
formed more poorly on reading and spelling tests and
were rated loweron academic achievementby their
teachers [33]. These findings were confirmed at age 14,
when the association between prenatal cannabis use and
poorer schoolperformance was shown to be mediated
by the child’slower cognitive ability,higherratesof
attentional and mood disorders and by these children ini-
tiating cannabis use before the age of14 [34].
The behavioural effects of prenatal cannabis exposure
have been reported in only two cohort studies, and the
effects have been most consistent in the cohort oflower-
income women with higher rates ofuse [35]. The dose–
response relationship in one ofthese studies is suggestive
of a causal role for cannabis.Uncertainty remains
because of the small number of studies, the small samples
of women in each and the researchers’ limited ability to
controlfor the confounding effects ofother drug use
during pregnancy,maternaldrug use post-birth and
poor parenting. These studies have also been unable to
control for a plausible explanation ofsome ofthe effects
of maternal cannabis use, namely, genetic differences in
IQ and in the risks ofconduct and substance use disor-
ders between cannabis-using mothers and their non-
using peers [35]. None the less, as with the evidence on
birth weight,it is prudentto counselwomen against
using cannabis during pregnancy.
ADVERSE HEALTH EFFECTS OF
CHRONIC CANNABIS USE
Epidemiologicalstudiesof cannabisuse are usually
unable to measurethe dosesof THC and other
cannabinoids (e.g.cannabidiol)that regular cannabis
users receive [36]. In the absence of these data, epidemio-
logical studies have defined ‘heavy’ or ‘regular’ cannabis
use as daily or near-daily use [6]. This is the pattern of use
that has been associated most consistently with adverse
health and psychological outcomes.
A major challengein interpretingassociations
between regular cannabis use and adverse health out-
comes in epidemiological studies is that regular cannabis
users differ from non-users in a variety ofways that may
reflect baseline differences in their risks ofadverse out-
comes.Regular cannabis users,for example,are more
likely to use alcohol, tobacco and other illicit drugs, and
they differ from non-users in their risk-taking and other
behaviour [6]. Statistical methods ofcontrol have been
used to test the plausibility ofconfounding as an expla-
nation ofthese relationships and fixed-effects regression
has been used to testfor unknown fixed differences
between users and non-users (e.g. [37]). Some research-
ers have expressed doubts about whether the first strategy
can be wholly successful [38].
Cannabis dependence
The conclusions of our 1993 review on cannabis depend-
ence provoked some scepticism. We used the DSM-III defi-
nition of cannabis dependence thatincluded impaired
controlover cannabisuse and difficulty ceasing use
despite harmscaused by it.DSM-III cannabisabuse
and/or dependence had been the most common type of
illicit substance use disorderidentified in US mental
health surveys of the 1980s and 1990s [9]. Critics of this
epidemiological evidence argued that very few cannabis
4 Wayne Hall
© 2014 Society for the Study ofAddiction Addiction
reported rates of cannabis use during pregnancy are typi-
cally low (2–6%). Studies that have measured cannabis
use using urinalyses suggest that there is considerable
under-reporting ofuse, which probably attenuates asso-
ciations between cannabis use and poor birth outcomes.
Secondly, it has often been difficult to fully adjust for the
effects ofmajor confounders such as cigarette smoking
in analyses of the effects of cannabis use on birth weight.
None the less,there is a good case on the grounds of
prudence for recommending that women should avoid
using cannabis while pregnant,or while attempting to
become pregnant.
Postnatal effects ofmaternal cannabis use
In 1993 a smallnumber ofstudies reported increased
rates ofdevelopmental abnormalities in children born to
women who used cannabis during pregnancy,such as
developmental delays in the visual system and increased
tremor and startle shortly after birth [30]. These effects
were not reported consistently in later assessments; e.g.
some were notdetected atthe age of1 month or on
ability tests at 6 and 12 months. Others were reported at
36 and 48 months, but not at 60 and 72 months [30]. As
these children entered adolescence,maternalcannabis
was associated with poorer cognitive performance. In the
Ontario study, at age 12 years, there were no differences
in full-scale IQ scores between children who were and
were not exposed to cannabis, but there were differences
in perceptual organization and higher cognitive processes
[30]. Tennes et al. [24], by contrast, found no IQ differ-
ences at 1 year between the children ofusers and nonus-
ers in 756 women, a third of whom used cannabis during
pregnancy.
In the past 20 years another cohort oflow-income
women with higher rates ofregular cannabis use [31]
has reported lower scores on memory and verbal scales of
the Stanford–Binet Intelligence Scale at age 3 in children
born to 655 low-income women (halfAfrican American
and halfCaucasian) in Pittsburgh between 1990 and
1995. By age 10, maternal cannabis use at all stages of
pregnancy was associated with delinquency and problem
behaviour[32]. Cannabis-exposed children also per-
formed more poorly on reading and spelling tests and
were rated loweron academic achievementby their
teachers [33]. These findings were confirmed at age 14,
when the association between prenatal cannabis use and
poorer schoolperformance was shown to be mediated
by the child’slower cognitive ability,higherratesof
attentional and mood disorders and by these children ini-
tiating cannabis use before the age of14 [34].
The behavioural effects of prenatal cannabis exposure
have been reported in only two cohort studies, and the
effects have been most consistent in the cohort oflower-
income women with higher rates ofuse [35]. The dose–
response relationship in one ofthese studies is suggestive
of a causal role for cannabis.Uncertainty remains
because of the small number of studies, the small samples
of women in each and the researchers’ limited ability to
controlfor the confounding effects ofother drug use
during pregnancy,maternaldrug use post-birth and
poor parenting. These studies have also been unable to
control for a plausible explanation ofsome ofthe effects
of maternal cannabis use, namely, genetic differences in
IQ and in the risks ofconduct and substance use disor-
ders between cannabis-using mothers and their non-
using peers [35]. None the less, as with the evidence on
birth weight,it is prudentto counselwomen against
using cannabis during pregnancy.
ADVERSE HEALTH EFFECTS OF
CHRONIC CANNABIS USE
Epidemiologicalstudiesof cannabisuse are usually
unable to measurethe dosesof THC and other
cannabinoids (e.g.cannabidiol)that regular cannabis
users receive [36]. In the absence of these data, epidemio-
logical studies have defined ‘heavy’ or ‘regular’ cannabis
use as daily or near-daily use [6]. This is the pattern of use
that has been associated most consistently with adverse
health and psychological outcomes.
A major challengein interpretingassociations
between regular cannabis use and adverse health out-
comes in epidemiological studies is that regular cannabis
users differ from non-users in a variety ofways that may
reflect baseline differences in their risks ofadverse out-
comes.Regular cannabis users,for example,are more
likely to use alcohol, tobacco and other illicit drugs, and
they differ from non-users in their risk-taking and other
behaviour [6]. Statistical methods ofcontrol have been
used to test the plausibility ofconfounding as an expla-
nation ofthese relationships and fixed-effects regression
has been used to testfor unknown fixed differences
between users and non-users (e.g. [37]). Some research-
ers have expressed doubts about whether the first strategy
can be wholly successful [38].
Cannabis dependence
The conclusions of our 1993 review on cannabis depend-
ence provoked some scepticism. We used the DSM-III defi-
nition of cannabis dependence thatincluded impaired
controlover cannabisuse and difficulty ceasing use
despite harmscaused by it.DSM-III cannabisabuse
and/or dependence had been the most common type of
illicit substance use disorderidentified in US mental
health surveys of the 1980s and 1990s [9]. Critics of this
epidemiological evidence argued that very few cannabis
4 Wayne Hall
© 2014 Society for the Study ofAddiction Addiction
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
users defined by DSM-III had a problem that warranted
professional help.
During the past 20 years, cannabis abuse and depend-
ence have remained the mostcommon form ofdrug
dependence after alcohol and tobacco in epidemiological
surveys in Australia, Canada and the United States. These
disorders have affected an estimated 1–2% of adults in the
past year, and 4–8% of adults during their life-time [6,39].
The life-time risk ofdeveloping dependence among those
who have ever used cannabis was estimated at 9% in the
United States in the early 1990s [39] as against 32% for
nicotine, 23% for heroin, 17% for cocaine, 15% for alcohol
and 11% for stimulants [40,41]. In longitudinal studies,
the risk of developing cannabis dependence has been esti-
mated as one in six among those users who initiated in
adolescence [39] and halfof daily cannabis users [42].
The evidence for a cannabis withdrawal syndrome has
strengthened since 1993. In laboratory studies, humans
develop tolerance to THC [43] and cannabis users who
seek help often report withdrawal symptoms that make it
more difficult to achieve abstinence. The most common
withdrawalsymptoms include anxiety,insomnia,appe-
tite disturbance and depression [44],often ofsufficient
severity to impair everyday functioning [45].A recent
double-blind controlled clinicaltrial showed that these
withdrawalsymptoms were markedly attenuated by an
oral cannabis extract (Sativex) [46].
It is now difficult to argue that cannabis dependence
does not require professionalattention. The number of
cannabis users seeking help to quit or control their can-
nabis use has increased during the past two decades in
the United States, Europe [47] and Australia [6,48,49].
The increase has usually occurred a decade or so after
increased cannabis use among young adults [49]. This
increase is not explained by increased court diversion of
users into treatmentin countries thatretain criminal
penaltiesfor cannabisuse: the same increasehas
occurred in the Netherlands,where cannabis use was
decriminalized more than 40 years ago [50].In 2011
cannabis was the primary drug problem for 48% ofindi-
viduals entering drug treatment,and for 58% ofnew
treatment entrants in the Netherlands.
The adverse health and social consequences ofcan-
nabis use reported by cannabis users who seek treatment
for dependence appearto be less severe than those
reported by alcohol and opioid-dependent people [6,51],
but rates ofrecovery from cannabis dependence among
those seeking treatment are similar to those for alcohol
[52]. Clinicaltrials ofcognitive behaviour therapy for
cannabis dependence show that only a minority remain
abstinent 6 and 12 months after treatment,but treat-
ment substantially reduces the severity ofproblems and
the frequency oftheir cannabis use in most who receive
treatment [53,54].
Chronic cannabis use and cognitive and brain function
Cognitive impairment
In 1993 case–control studies reported that regular can-
nabis users had poorer cognitive performance than non-
cannabis-using controls, but it was unclear whether this
was because cannabisuse impaired cognitive perfor-
mance,people with poorer cognitive functioning were
more likely to become regular cannabis users,or some
combination of the two [9]. Very few studies had matched
users and non-users on estimated intellectualfunction
before using cannabis [55], and only one study had meas-
ured cognitive performance before cannabis use [56].
Both these studies found greater cognitive impairments
in frequent and/or long-term cannabis users after con-
trolling for differences in baseline cognitive ability.
The increased numberof better-controlled studies
that have been reported since 1993 (see [57,58]for
reviews) have consistently found deficits in verbal learn-
ing, memory and attention in regular cannabis users,
and these deficitshave usually butnot alwaysbeen
related to the duration and frequency of cannabis use, the
age ofinitiation and the estimated cumulative dose of
THC received [59,60].It still remains unclear whether
cognitive function recovers fully after cessation oflong-
term cannabis use. Solowij [55,60] found partial recov-
ery after2 years’abstinence,but brain event-related
potentials stillshowed impaired information processing
that was correlated with years of cannabis use. Bolla et al.
[61] found persistentdose-relatedimpairmentin
neurocognitive performance after 28 days ofabstinence
in young heavy users (who had used on average for 5
years). Pope et al. [62], by contrast, reported full recovery
after 28 days’ abstinence.It also remainsunclear
whether any cognitive impairment reflects the residual
effectsof chronic cannabisuse, or more enduring
changes in brain function produced by the cumulative
effects ofTHC exposure [59].
A longitudinal study from the Dunedin birth cohort
has suggested recently that sustained heavy cannabis use
over several decades can produce substantial differences
in cognitive performance that may not be wholly revers-
ible. This study assessed changes in IQ between age 13
(before cannabis was used) and at age 38 in 1037 New
Zealanders born in 1972 or 1973 [63]. It found that early
and persistent cannabis users showed an average decline
in IQ of8 points compared with those who had not used
cannabis at all,and cannabis users who had not used
cannabis in this sustained way.
Detailed analyses pointed to persistent cannabis use as
the most plausible explanation for the cognitive decline.
First,the decline in IQ was largest in those who began
using cannabis in adolescence and continued near-daily
use throughoutadulthood.Secondly,it persisted after
Cannabis health effects5
© 2014 Society for the Study ofAddiction Addiction
professional help.
During the past 20 years, cannabis abuse and depend-
ence have remained the mostcommon form ofdrug
dependence after alcohol and tobacco in epidemiological
surveys in Australia, Canada and the United States. These
disorders have affected an estimated 1–2% of adults in the
past year, and 4–8% of adults during their life-time [6,39].
The life-time risk ofdeveloping dependence among those
who have ever used cannabis was estimated at 9% in the
United States in the early 1990s [39] as against 32% for
nicotine, 23% for heroin, 17% for cocaine, 15% for alcohol
and 11% for stimulants [40,41]. In longitudinal studies,
the risk of developing cannabis dependence has been esti-
mated as one in six among those users who initiated in
adolescence [39] and halfof daily cannabis users [42].
The evidence for a cannabis withdrawal syndrome has
strengthened since 1993. In laboratory studies, humans
develop tolerance to THC [43] and cannabis users who
seek help often report withdrawal symptoms that make it
more difficult to achieve abstinence. The most common
withdrawalsymptoms include anxiety,insomnia,appe-
tite disturbance and depression [44],often ofsufficient
severity to impair everyday functioning [45].A recent
double-blind controlled clinicaltrial showed that these
withdrawalsymptoms were markedly attenuated by an
oral cannabis extract (Sativex) [46].
It is now difficult to argue that cannabis dependence
does not require professionalattention. The number of
cannabis users seeking help to quit or control their can-
nabis use has increased during the past two decades in
the United States, Europe [47] and Australia [6,48,49].
The increase has usually occurred a decade or so after
increased cannabis use among young adults [49]. This
increase is not explained by increased court diversion of
users into treatmentin countries thatretain criminal
penaltiesfor cannabisuse: the same increasehas
occurred in the Netherlands,where cannabis use was
decriminalized more than 40 years ago [50].In 2011
cannabis was the primary drug problem for 48% ofindi-
viduals entering drug treatment,and for 58% ofnew
treatment entrants in the Netherlands.
The adverse health and social consequences ofcan-
nabis use reported by cannabis users who seek treatment
for dependence appearto be less severe than those
reported by alcohol and opioid-dependent people [6,51],
but rates ofrecovery from cannabis dependence among
those seeking treatment are similar to those for alcohol
[52]. Clinicaltrials ofcognitive behaviour therapy for
cannabis dependence show that only a minority remain
abstinent 6 and 12 months after treatment,but treat-
ment substantially reduces the severity ofproblems and
the frequency oftheir cannabis use in most who receive
treatment [53,54].
Chronic cannabis use and cognitive and brain function
Cognitive impairment
In 1993 case–control studies reported that regular can-
nabis users had poorer cognitive performance than non-
cannabis-using controls, but it was unclear whether this
was because cannabisuse impaired cognitive perfor-
mance,people with poorer cognitive functioning were
more likely to become regular cannabis users,or some
combination of the two [9]. Very few studies had matched
users and non-users on estimated intellectualfunction
before using cannabis [55], and only one study had meas-
ured cognitive performance before cannabis use [56].
Both these studies found greater cognitive impairments
in frequent and/or long-term cannabis users after con-
trolling for differences in baseline cognitive ability.
The increased numberof better-controlled studies
that have been reported since 1993 (see [57,58]for
reviews) have consistently found deficits in verbal learn-
ing, memory and attention in regular cannabis users,
and these deficitshave usually butnot alwaysbeen
related to the duration and frequency of cannabis use, the
age ofinitiation and the estimated cumulative dose of
THC received [59,60].It still remains unclear whether
cognitive function recovers fully after cessation oflong-
term cannabis use. Solowij [55,60] found partial recov-
ery after2 years’abstinence,but brain event-related
potentials stillshowed impaired information processing
that was correlated with years of cannabis use. Bolla et al.
[61] found persistentdose-relatedimpairmentin
neurocognitive performance after 28 days ofabstinence
in young heavy users (who had used on average for 5
years). Pope et al. [62], by contrast, reported full recovery
after 28 days’ abstinence.It also remainsunclear
whether any cognitive impairment reflects the residual
effectsof chronic cannabisuse, or more enduring
changes in brain function produced by the cumulative
effects ofTHC exposure [59].
A longitudinal study from the Dunedin birth cohort
has suggested recently that sustained heavy cannabis use
over several decades can produce substantial differences
in cognitive performance that may not be wholly revers-
ible. This study assessed changes in IQ between age 13
(before cannabis was used) and at age 38 in 1037 New
Zealanders born in 1972 or 1973 [63]. It found that early
and persistent cannabis users showed an average decline
in IQ of8 points compared with those who had not used
cannabis at all,and cannabis users who had not used
cannabis in this sustained way.
Detailed analyses pointed to persistent cannabis use as
the most plausible explanation for the cognitive decline.
First,the decline in IQ was largest in those who began
using cannabis in adolescence and continued near-daily
use throughoutadulthood.Secondly,it persisted after
Cannabis health effects5
© 2014 Society for the Study ofAddiction Addiction
statistical adjustment for recent cannabis use, for alcohol,
tobacco and other drug use, and for symptoms ofschizo-
phrenia. Thirdly, the same effects were observed in canna-
bis users who finished high school, in whom the decline
also persisted after statistically controlling for educational
level attained. Fourthly, there was some recovery ifusers
quit using for a year or more. There was no IQ decline in
cannabis users who started in young adulthood and had
not used for a year or more before follow-up.
It is worth stressing two things about this study. First,
these effects on IQ were found only in the small propor-
tion ofcannabis users who initiated in adolescence and
persisted in daily use throughout their 20s and into their
30s. No effects were found in those who initiated later or
in daily users who ceased use earlier in adulthood. Sec-
ondly,the 8-point decline in IQ in the heavy sustained
users was not trivial:it was halfa standard deviation
lower than their peers. This means that the average IQ of
these heavy users was below 70% oftheir peer group.
These cognitive effects were evident to close acquaint-
ances ofthe study participants.Heavy cannabis users
were rated as having more problems with memory and
attention in everyday life than peers who did notuse
cannabis in this way.
Brain structure and function
In our 1993 review, we found a 22-year-old study using
air encephalography which suggested that heavy canna-
bis use produced structuralbrain damage [64].This
study was heavily criticized because it involved a small
number ofusers, the effects ofother drug use were not
well controlled and therewere major doubtsabout
the validity ofair encephalography.Since then,better
methods ofbrain imaging studies have reported changes
in brain function and structure in heavy cannabis users.
Positron emission tomography (PET)studieshave
shown a down-regulation ofcannabinoid receptors in
regular cannabis users which persisted for up to a month
after abstinence[65]. Functionalimaging studiesof
chronic cannabis users (e.g.[66]) have shown reduced
activity in brain regions that are involved in memory and
attention after 28 days of abstinence [56]. Magnetic reso-
nance imaging studies have reported structural changes
in the hippocampus, prefrontal cortex and cerebellum in
chronic cannabis users.Yücel et al.[67], for example,
reported reduced hippocampal and amygdala volumes in
15 long-term users who had smoked five or more joints a
day for 10 or more years. These reductions were largest in
users with the longest duration ofuse.
Reviews offunctionaland structuralneuroimaging
studies ofchronic cannabis users [68,69] indicate that
there is a need for larger, better-controlled neuroimaging
studies that use standardized tasks and measures.The
potential cognitive effects ofchronic cannabis use are of
specialconcern because itis the leastcognitively able
young people who are most likely to begin early cannabis
use and to use regularly throughout young adulthood.
The psychosocial consequences ofadolescent
cannabis use
Educational outcomes
In 1993, cross-sectional studies found that regular can-
nabis users had poorer educationalattainments than
non-using peers [70],but it was uncertain which was
cause and which effect. That is, we could not tell whether
this association arose because: (i) cannabis use was a con-
tributory cause ofpoor school performance; (ii) cannabis
use was more likely in young people with poor educa-
tional attainment; or (iii) that cannabis use and poor edu-
cationalattainmentwere caused by common factors
[70]. Explanations (i) and (ii) could both be true ifpoor
schoolperformance made young people more likely to
become regular cannabis users,and regular cannabis
use, in turn, further impaired school performance.
Longitudinalstudies have found that a relationship
between cannabis use before the age of15 and early
school-leaving persisted after adjustment for confounders
(e.g.[71]).A recent meta-analysis ofthree Australian
and New Zealand longitudinal studies [72] showed that
the earlier the age offirst cannabis use,the lower the
chancesof completing schooland undertaking post-
secondary training. These effects persisted after adjust-
mentfor parentalsocialclass and other measures of
disadvantage.The authors estimated thatearly use of
cannabis contributed to 17% of the risk of failing to com-
plete high school or post-secondary training. The adverse
effects ofcannabis use on educational outcomes may be
amplified by school policies that exclude students who are
caught using cannabis from secondary school.
It is plausible that educationaloutcomes in regular
cannabis users are impaired as a result ofa combination
of: a higher pre-existing risk ofeducational problems in
those who become regular cannabis users,the adverse
effects ofregular cannabis use on learning in school,
increased affiliation ofregular cannabis users with other
cannabis-using peers who rejectschooland a strong
desire among younger cannabis users to make a prema-
ture transition to adulthood by leaving school [70].
A recent analysis ofAustralian twin-study data has
raised some doubtsabout whetherthe association
between adolescentcannabisuse and early school-
leaving is causal[73].An analysis oftwins who were
discordant for early cannabis use found no difference in
risk ofearly school-leaving between the twins who did
and did not use cannabis, suggesting that the association
was explained by shared genetic and environmental risk
6 Wayne Hall
© 2014 Society for the Study ofAddiction Addiction
tobacco and other drug use, and for symptoms ofschizo-
phrenia. Thirdly, the same effects were observed in canna-
bis users who finished high school, in whom the decline
also persisted after statistically controlling for educational
level attained. Fourthly, there was some recovery ifusers
quit using for a year or more. There was no IQ decline in
cannabis users who started in young adulthood and had
not used for a year or more before follow-up.
It is worth stressing two things about this study. First,
these effects on IQ were found only in the small propor-
tion ofcannabis users who initiated in adolescence and
persisted in daily use throughout their 20s and into their
30s. No effects were found in those who initiated later or
in daily users who ceased use earlier in adulthood. Sec-
ondly,the 8-point decline in IQ in the heavy sustained
users was not trivial:it was halfa standard deviation
lower than their peers. This means that the average IQ of
these heavy users was below 70% oftheir peer group.
These cognitive effects were evident to close acquaint-
ances ofthe study participants.Heavy cannabis users
were rated as having more problems with memory and
attention in everyday life than peers who did notuse
cannabis in this way.
Brain structure and function
In our 1993 review, we found a 22-year-old study using
air encephalography which suggested that heavy canna-
bis use produced structuralbrain damage [64].This
study was heavily criticized because it involved a small
number ofusers, the effects ofother drug use were not
well controlled and therewere major doubtsabout
the validity ofair encephalography.Since then,better
methods ofbrain imaging studies have reported changes
in brain function and structure in heavy cannabis users.
Positron emission tomography (PET)studieshave
shown a down-regulation ofcannabinoid receptors in
regular cannabis users which persisted for up to a month
after abstinence[65]. Functionalimaging studiesof
chronic cannabis users (e.g.[66]) have shown reduced
activity in brain regions that are involved in memory and
attention after 28 days of abstinence [56]. Magnetic reso-
nance imaging studies have reported structural changes
in the hippocampus, prefrontal cortex and cerebellum in
chronic cannabis users.Yücel et al.[67], for example,
reported reduced hippocampal and amygdala volumes in
15 long-term users who had smoked five or more joints a
day for 10 or more years. These reductions were largest in
users with the longest duration ofuse.
Reviews offunctionaland structuralneuroimaging
studies ofchronic cannabis users [68,69] indicate that
there is a need for larger, better-controlled neuroimaging
studies that use standardized tasks and measures.The
potential cognitive effects ofchronic cannabis use are of
specialconcern because itis the leastcognitively able
young people who are most likely to begin early cannabis
use and to use regularly throughout young adulthood.
The psychosocial consequences ofadolescent
cannabis use
Educational outcomes
In 1993, cross-sectional studies found that regular can-
nabis users had poorer educationalattainments than
non-using peers [70],but it was uncertain which was
cause and which effect. That is, we could not tell whether
this association arose because: (i) cannabis use was a con-
tributory cause ofpoor school performance; (ii) cannabis
use was more likely in young people with poor educa-
tional attainment; or (iii) that cannabis use and poor edu-
cationalattainmentwere caused by common factors
[70]. Explanations (i) and (ii) could both be true ifpoor
schoolperformance made young people more likely to
become regular cannabis users,and regular cannabis
use, in turn, further impaired school performance.
Longitudinalstudies have found that a relationship
between cannabis use before the age of15 and early
school-leaving persisted after adjustment for confounders
(e.g.[71]).A recent meta-analysis ofthree Australian
and New Zealand longitudinal studies [72] showed that
the earlier the age offirst cannabis use,the lower the
chancesof completing schooland undertaking post-
secondary training. These effects persisted after adjust-
mentfor parentalsocialclass and other measures of
disadvantage.The authors estimated thatearly use of
cannabis contributed to 17% of the risk of failing to com-
plete high school or post-secondary training. The adverse
effects ofcannabis use on educational outcomes may be
amplified by school policies that exclude students who are
caught using cannabis from secondary school.
It is plausible that educationaloutcomes in regular
cannabis users are impaired as a result ofa combination
of: a higher pre-existing risk ofeducational problems in
those who become regular cannabis users,the adverse
effects ofregular cannabis use on learning in school,
increased affiliation ofregular cannabis users with other
cannabis-using peers who rejectschooland a strong
desire among younger cannabis users to make a prema-
ture transition to adulthood by leaving school [70].
A recent analysis ofAustralian twin-study data has
raised some doubtsabout whetherthe association
between adolescentcannabisuse and early school-
leaving is causal[73].An analysis oftwins who were
discordant for early cannabis use found no difference in
risk ofearly school-leaving between the twins who did
and did not use cannabis, suggesting that the association
was explained by shared genetic and environmental risk
6 Wayne Hall
© 2014 Society for the Study ofAddiction Addiction
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
factors. These findings are supported by two earlier analy-
ses ofUS twin-study data [74,75].
Other drug use
In 1993 in the United States, Australia and New Zealand
epidemiologicalstudies reported consistentlythat:
(i) regular cannabis users were more likely to use heroin
and cocaine; and (ii) the younger a person was when they
first used cannabis,the more likely they were to do so
[76]. Three explanations were offered for these patterns:
(i) that cannabis users have more opportunities to use
other illicit drugs because these are supplied by the same
black market as cannabis; (ii) that early cannabis users
were more likely to use other illicit drugs for reasons that
are unrelated to their cannabis use (e.g.risk-taking or
sensation-seeking);and (iii) that the pharmacological
effects of cannabis increased a young person’s propensity
to use other illicit drugs [6].
Epidemiologicalresearch since 1993 hasreported
similar patterns ofdrug involvementin a number of
countries (e.g. [77]), although the order in which drugs
are used can vary with the prevalence of different types of
illicit drug use in the adult population [78]. Research has
also supported the first two hypotheses,in that young
people in the United Stateswho have used cannabis
report more opportunities to use cocaine at an earlier age
[79],and socially deviant young people (who are also
more likely to use cocaine and heroin) start using canna-
bis at an earlier age than their peers [80]. A simulation
study [81] indicated that shared risk factors could explain
the observed relationships between cannabis and other
illicit drug use in the United States.
The shared risk factor hypothesis has been tested in
longitudinalstudiesby assessingwhethercannabis
users are more likely to report heroin and cocaine use
after controlling statistically for plausible confounding
factors (e.g. [82]). Adjustment for confounders (including
unmeasured fixed onesusing fixed-effectsregression)
[83] has not eliminated the relationship between regular
cannabis use and the use ofother illicit drugs [84].
Studies oftwins who are discordant for cannabis use
(i.e. one used cannabis and the other did not) have tested
whether the relationship between cannabis use and the
use ofother illicit drugs is explained by a shared genetic
vulnerability to use drugs. Lynskey et al. [85] found that
the twin who had used cannabis was more likely to have
used other illicit drugs than the co-twin who had not.
This relationship persisted aftercontrolling fornon-
shared environmental factors. Similar results have been
reported in discordant twin studies in the United States
[86] and the Netherlands [86].
The order ofinvolvement with cannabis and other
illicit drugs, and the increased likelihood ofusing other
illicit drugs, are the most consistent findings in epidemio-
logical studies ofdrug use in young adults. The interpre-
tation ofthese relationships remains contested, but the
relationships between regular cannabis use and other
illicit drug use have persisted after statistical adjustment
for the effects ofconfounding variables in both longitudi-
nal studies and discordant twin studies.
Research over the past 20 years has revealed a chang-
ing relationship between cannabis and other drug use. In
1993, cigarette smoking wasgenerally initiated well
before cannabis use and regular tobacco smoking was
a predictor ofregular cannabis use.As a result ofthe
successin the 2000s of public health campaignsto
prevent tobacco smoking among young people, cannabis
smoking is initiated increasingly by young people who
have not smoked tobacco.A number ofrecent studies
have reported that these cannabis smokers are now more
likely to become tobacco smokers after using cannabis, a
pattern described as a ‘reverse gateway’ [87]. This finding
probably reflects a combination of:a shared route of
administration (smoking)[88], cannabis users mixing
with tobacco smokers, and possibly the effects ofmixing
tobacco and cannabis in joints. There is suggestive evi-
dence for the latter in the fact that the effect was much
strongerin an Australian study ofadolescents[87],
where it is common to combine tobacco and cannabis,
than in a US study where this practice seems to be less
common [89].
Cannabis use and mental health
Psychosis and schizophrenia
In 1993, there were reports that regular cannabis use
was associated with psychoticsymptoms(disordered
thinking, hallucinations and delusions) and that regular
cannabis use occurred athigher rates among people
with schizophrenia,a disorderin which individuals
report severe psychotic symptoms over months, and often
experience substantial social disability, a loss ofmotiva-
tion, disturbed behaviour and cognitive deficits [90].
In 1993 our review found one large prospective study
that supported a causalrole for cannabis,a 15-year
follow-up study ofrates ofschizophrenia among 50 465
Swedish male conscripts. Conscripts who had tried can-
nabis by age 18 were 2.4 times more likely to be diag-
nosed with schizophrenia over the next 15 years than
those who had not [91]. After statistical adjustment for
a personal history ofpsychiatric disorder by age 18 and
parentaldivorce,those who had used cannabis 10 or
more times by age 18 were 2.3 times more likely to receive
a diagnosis ofschizophrenia than those who had not
used cannabis.
Critics argued that this study had not addressed con-
founding and reverse causation. Studies since then have
attempted to do so. Zammit et al.’s [92] 27-year follow-up
Cannabis health effects7
© 2014 Society for the Study ofAddiction Addiction
ses ofUS twin-study data [74,75].
Other drug use
In 1993 in the United States, Australia and New Zealand
epidemiologicalstudies reported consistentlythat:
(i) regular cannabis users were more likely to use heroin
and cocaine; and (ii) the younger a person was when they
first used cannabis,the more likely they were to do so
[76]. Three explanations were offered for these patterns:
(i) that cannabis users have more opportunities to use
other illicit drugs because these are supplied by the same
black market as cannabis; (ii) that early cannabis users
were more likely to use other illicit drugs for reasons that
are unrelated to their cannabis use (e.g.risk-taking or
sensation-seeking);and (iii) that the pharmacological
effects of cannabis increased a young person’s propensity
to use other illicit drugs [6].
Epidemiologicalresearch since 1993 hasreported
similar patterns ofdrug involvementin a number of
countries (e.g. [77]), although the order in which drugs
are used can vary with the prevalence of different types of
illicit drug use in the adult population [78]. Research has
also supported the first two hypotheses,in that young
people in the United Stateswho have used cannabis
report more opportunities to use cocaine at an earlier age
[79],and socially deviant young people (who are also
more likely to use cocaine and heroin) start using canna-
bis at an earlier age than their peers [80]. A simulation
study [81] indicated that shared risk factors could explain
the observed relationships between cannabis and other
illicit drug use in the United States.
The shared risk factor hypothesis has been tested in
longitudinalstudiesby assessingwhethercannabis
users are more likely to report heroin and cocaine use
after controlling statistically for plausible confounding
factors (e.g. [82]). Adjustment for confounders (including
unmeasured fixed onesusing fixed-effectsregression)
[83] has not eliminated the relationship between regular
cannabis use and the use ofother illicit drugs [84].
Studies oftwins who are discordant for cannabis use
(i.e. one used cannabis and the other did not) have tested
whether the relationship between cannabis use and the
use ofother illicit drugs is explained by a shared genetic
vulnerability to use drugs. Lynskey et al. [85] found that
the twin who had used cannabis was more likely to have
used other illicit drugs than the co-twin who had not.
This relationship persisted aftercontrolling fornon-
shared environmental factors. Similar results have been
reported in discordant twin studies in the United States
[86] and the Netherlands [86].
The order ofinvolvement with cannabis and other
illicit drugs, and the increased likelihood ofusing other
illicit drugs, are the most consistent findings in epidemio-
logical studies ofdrug use in young adults. The interpre-
tation ofthese relationships remains contested, but the
relationships between regular cannabis use and other
illicit drug use have persisted after statistical adjustment
for the effects ofconfounding variables in both longitudi-
nal studies and discordant twin studies.
Research over the past 20 years has revealed a chang-
ing relationship between cannabis and other drug use. In
1993, cigarette smoking wasgenerally initiated well
before cannabis use and regular tobacco smoking was
a predictor ofregular cannabis use.As a result ofthe
successin the 2000s of public health campaignsto
prevent tobacco smoking among young people, cannabis
smoking is initiated increasingly by young people who
have not smoked tobacco.A number ofrecent studies
have reported that these cannabis smokers are now more
likely to become tobacco smokers after using cannabis, a
pattern described as a ‘reverse gateway’ [87]. This finding
probably reflects a combination of:a shared route of
administration (smoking)[88], cannabis users mixing
with tobacco smokers, and possibly the effects ofmixing
tobacco and cannabis in joints. There is suggestive evi-
dence for the latter in the fact that the effect was much
strongerin an Australian study ofadolescents[87],
where it is common to combine tobacco and cannabis,
than in a US study where this practice seems to be less
common [89].
Cannabis use and mental health
Psychosis and schizophrenia
In 1993, there were reports that regular cannabis use
was associated with psychoticsymptoms(disordered
thinking, hallucinations and delusions) and that regular
cannabis use occurred athigher rates among people
with schizophrenia,a disorderin which individuals
report severe psychotic symptoms over months, and often
experience substantial social disability, a loss ofmotiva-
tion, disturbed behaviour and cognitive deficits [90].
In 1993 our review found one large prospective study
that supported a causalrole for cannabis,a 15-year
follow-up study ofrates ofschizophrenia among 50 465
Swedish male conscripts. Conscripts who had tried can-
nabis by age 18 were 2.4 times more likely to be diag-
nosed with schizophrenia over the next 15 years than
those who had not [91]. After statistical adjustment for
a personal history ofpsychiatric disorder by age 18 and
parentaldivorce,those who had used cannabis 10 or
more times by age 18 were 2.3 times more likely to receive
a diagnosis ofschizophrenia than those who had not
used cannabis.
Critics argued that this study had not addressed con-
founding and reverse causation. Studies since then have
attempted to do so. Zammit et al.’s [92] 27-year follow-up
Cannabis health effects7
© 2014 Society for the Study ofAddiction Addiction
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
of the Swedish cohort found a dose–response relationship
between frequency ofcannabis use at age 18 and risk of
schizophrenia during the whole follow-up period.This
effect persisted after controlling statistically for confound-
ing factors. They estimated that 13% ofcases ofschizo-
phrenia could be averted ifall cannabis use had been
prevented in the cohort.The Swedish cohortfindings
have been supported by the results ofsmaller longitudi-
nal studies in the Netherlands [93],Germany [94] and
New Zealand [95,96]. All these studies have found a rela-
tionship between cannabis use and psychotic disorders or
psychotic symptoms,and these relationships persisted
after adjustment for confounders.
A meta-analysis of these longitudinal studies reported
that psychotic symptomsor psychotic disorderswere
more common among those who had ever used cannabis
(a pooled OR of1.4, 95% CI = 1.20, 1.65) [97]. The risk
of psychotic symptoms or psychotic disorders was higher
in regular users (OR of2.09, 95% CI = 1.54,2.84).
Reverse causation was addressed in some of these studies
by excluding cases who reported psychotic symptoms at
baseline, or by statistically adjusting for pre-existing psy-
chotic symptoms.The common cause hypothesis was
harder to exclude, because the association between can-
nabis use and psychosis was attenuated after statistical
adjustmentfor potentialconfounders,and no study
assessed all confounders.
Researcherswho remain scepticalabouta casual
explanation often argue that a causal hypothesis is incon-
sistent with the absence ofany increase in the incidence
of schizophrenia, as cannabis use has increased among
young adults.There is mixed evidence on trendsin
schizophrenia incidence. An Australian modelling study
did not find any increased psychosis incidence after steep
increases in cannabis use during the 1980s and 1990s
[98],but a similar British modelling study [99] argued
that it was too early to detect any increase in psychosis
incidence in Britain. Two case register studies in Britain
[100] and Switzerland [101] reported an increased inci-
dence ofpsychoses in recent birth cohorts, but a British
study ofpeople treated for schizophrenia in general prac-
tice failed to do so [90].
It is difficult to decide whether cannabis use has had
any effects on psychosis incidence,because even ifthe
relationship were causal, cannabis use would produce a
very modest increase in incidence. The detection ofany
such increases is complicated by changes in diagnostic
criteria and psychiatric services for psychosis,the poor
quality of administrative data on the treated cases of psy-
chosis, and possibly by social improvements (e.g. in ante-
natal care) that may have reduced incidence ofpsychosis
during the period in which cannabis use increased.
Our best estimate is that the risk ofdeveloping a psy-
chosis doubles from approximately 7 in 1000 in non-
users [102] to 14 in 1000 among regular cannabis users.
If we assume that cannabis use plays a causalrole in
psychosis, it will be difficult to reduce psychosis incidence
by preventing cannabis uptake in the whole population:
an estimated 4700 young men in the United Kingdom
aged 20–24 yearswould have to be dissuaded from
smoking cannabis to prevent one case ofschizophrenia
[99].If the risks ofcannabis use are independent and
multiplicative with genetic risk, then a doubling ofrisk
would be an important piece ofinformation for people
who have an affected first-degree relative: it would mean
that their risk would increase from 10 to 20% if they used
cannabis regularly [103].
There are also important risk messages about canna-
bis use for young peoplewho experiencepsychotic
symptoms.Young people with psychoses or psychotic
symptoms who use cannabis have an earlier average age
of first-episode psychosis [104].More positively,young
people with a first episode ofpsychosis who stop using
cannabis use have better clinicaloutcomes than those
who persistin using,as measured by fewer psychotic
symptoms and better social functioning [105,106].
Cannabis use and other mental disorders
In 1993, epidemiological studies such as the Epidemio-
logic Catchment Area Study and NationalComorbidity
Study found high rates ofcomorbidity between cannabis
use disorders and anxiety and depressive disorders, other
substance use disorders and antisocial personality disor-
ders [9]. There were,however,few longitudinalstudies
available in 1993 to decide on the best explanations of
these relationships.
In longitudinalstudies conducted since our earlier
review,the relationship between regular cannabis use
and depression has been weaker than that for cannabis
and psychosis [107]. A follow-up ofthe Swedish cohort
by Manrique-Garcia and colleagues found that depres-
sion was 1.5 times more common in those who reported
the heaviest cannabis use at age 18 than in non-users,
but the association was no longer significant after adjust-
ment for confounders [108]. Fergusson & Horwood [109]
found a dose–response relationship between frequency of
cannabis use by age 16 and depressive disorder, but the
relationship was no longer statistically significant after
adjusting forconfounders.A meta-analysisof these
studies [97] reported a modest association between can-
nabis use and depressivedisorders(OR = 1.49,95%
CI = 1.15, 1.94) and concluded that support for a causal
hypothesis was weak, because most ofthese studies had
not controlled adequately for confounders or excluded
the possibility that depressed young people were more
likely to use cannabis.Similar conclusions were drawn
from a combined analysis ofdata from four Australasian
birth cohorts [110].
8 Wayne Hall
© 2014 Society for the Study ofAddiction Addiction
between frequency ofcannabis use at age 18 and risk of
schizophrenia during the whole follow-up period.This
effect persisted after controlling statistically for confound-
ing factors. They estimated that 13% ofcases ofschizo-
phrenia could be averted ifall cannabis use had been
prevented in the cohort.The Swedish cohortfindings
have been supported by the results ofsmaller longitudi-
nal studies in the Netherlands [93],Germany [94] and
New Zealand [95,96]. All these studies have found a rela-
tionship between cannabis use and psychotic disorders or
psychotic symptoms,and these relationships persisted
after adjustment for confounders.
A meta-analysis of these longitudinal studies reported
that psychotic symptomsor psychotic disorderswere
more common among those who had ever used cannabis
(a pooled OR of1.4, 95% CI = 1.20, 1.65) [97]. The risk
of psychotic symptoms or psychotic disorders was higher
in regular users (OR of2.09, 95% CI = 1.54,2.84).
Reverse causation was addressed in some of these studies
by excluding cases who reported psychotic symptoms at
baseline, or by statistically adjusting for pre-existing psy-
chotic symptoms.The common cause hypothesis was
harder to exclude, because the association between can-
nabis use and psychosis was attenuated after statistical
adjustmentfor potentialconfounders,and no study
assessed all confounders.
Researcherswho remain scepticalabouta casual
explanation often argue that a causal hypothesis is incon-
sistent with the absence ofany increase in the incidence
of schizophrenia, as cannabis use has increased among
young adults.There is mixed evidence on trendsin
schizophrenia incidence. An Australian modelling study
did not find any increased psychosis incidence after steep
increases in cannabis use during the 1980s and 1990s
[98],but a similar British modelling study [99] argued
that it was too early to detect any increase in psychosis
incidence in Britain. Two case register studies in Britain
[100] and Switzerland [101] reported an increased inci-
dence ofpsychoses in recent birth cohorts, but a British
study ofpeople treated for schizophrenia in general prac-
tice failed to do so [90].
It is difficult to decide whether cannabis use has had
any effects on psychosis incidence,because even ifthe
relationship were causal, cannabis use would produce a
very modest increase in incidence. The detection ofany
such increases is complicated by changes in diagnostic
criteria and psychiatric services for psychosis,the poor
quality of administrative data on the treated cases of psy-
chosis, and possibly by social improvements (e.g. in ante-
natal care) that may have reduced incidence ofpsychosis
during the period in which cannabis use increased.
Our best estimate is that the risk ofdeveloping a psy-
chosis doubles from approximately 7 in 1000 in non-
users [102] to 14 in 1000 among regular cannabis users.
If we assume that cannabis use plays a causalrole in
psychosis, it will be difficult to reduce psychosis incidence
by preventing cannabis uptake in the whole population:
an estimated 4700 young men in the United Kingdom
aged 20–24 yearswould have to be dissuaded from
smoking cannabis to prevent one case ofschizophrenia
[99].If the risks ofcannabis use are independent and
multiplicative with genetic risk, then a doubling ofrisk
would be an important piece ofinformation for people
who have an affected first-degree relative: it would mean
that their risk would increase from 10 to 20% if they used
cannabis regularly [103].
There are also important risk messages about canna-
bis use for young peoplewho experiencepsychotic
symptoms.Young people with psychoses or psychotic
symptoms who use cannabis have an earlier average age
of first-episode psychosis [104].More positively,young
people with a first episode ofpsychosis who stop using
cannabis use have better clinicaloutcomes than those
who persistin using,as measured by fewer psychotic
symptoms and better social functioning [105,106].
Cannabis use and other mental disorders
In 1993, epidemiological studies such as the Epidemio-
logic Catchment Area Study and NationalComorbidity
Study found high rates ofcomorbidity between cannabis
use disorders and anxiety and depressive disorders, other
substance use disorders and antisocial personality disor-
ders [9]. There were,however,few longitudinalstudies
available in 1993 to decide on the best explanations of
these relationships.
In longitudinalstudies conducted since our earlier
review,the relationship between regular cannabis use
and depression has been weaker than that for cannabis
and psychosis [107]. A follow-up ofthe Swedish cohort
by Manrique-Garcia and colleagues found that depres-
sion was 1.5 times more common in those who reported
the heaviest cannabis use at age 18 than in non-users,
but the association was no longer significant after adjust-
ment for confounders [108]. Fergusson & Horwood [109]
found a dose–response relationship between frequency of
cannabis use by age 16 and depressive disorder, but the
relationship was no longer statistically significant after
adjusting forconfounders.A meta-analysisof these
studies [97] reported a modest association between can-
nabis use and depressivedisorders(OR = 1.49,95%
CI = 1.15, 1.94) and concluded that support for a causal
hypothesis was weak, because most ofthese studies had
not controlled adequately for confounders or excluded
the possibility that depressed young people were more
likely to use cannabis.Similar conclusions were drawn
from a combined analysis ofdata from four Australasian
birth cohorts [110].
8 Wayne Hall
© 2014 Society for the Study ofAddiction Addiction
In clinicalsamples there are much higher rates of
cannabis use disorders among people diagnosed with
bipolar disorders than in the generalpopulation (e.g.
[111–114]).In one longitudinalstudy,cannabis use at
baseline predicted an increased risk ofmanic symptoms
in a 3-year follow-up [115].In some clinicalstudies,
people with bipolar disorders who continue to use canna-
bis have more manic episodes and are less satisfied with
their lives than bipolar peers who do not use cannabis
[113]. These findings suggest that regular cannabis use
may play a contributory causal role in bipolar disorders,
but the case is not yet proved because these studies have
not controlled adequately for confounding variables or
ruled out reverse causation [113].
Several case–control and cohort studies have reported
associations between cannabis use and suicide in adoles-
cents and young adults.For example,a New Zealand
case–controlstudy [116] of suicide attemptsthat
resulted in hospitalization found that 16% ofthe 302
suicide attempters had a cannabis disorder compared
with 2% of1028 community controls.Controlling for
social disadvantage, depression and alcohol dependence
substantially reduced but did not eliminate the associa-
tion (adjusted OR of2).
The evidencefrom prospectivestudiesis mixed.
Fergusson & Horwood [109], for example, found a dose–
response relationship between frequency ofcannabis use
by age 16 and self-reported suicide attempts,but the
association did not persist after controlling for confound-
ers. A recent analysis ofthe data from this cohort [117]
using econometricmethodsfound that more than
weekly cannabis use increased the likelihood ofreport-
ing suicidalideation,but only in males.Patton et al.
[118],by contrast,found that cannabis was associated
with self-harm only in females. Rasic et al. [119]
reported that heavy cannabis use increased the risk of
depression but did not affect suicide risk. An attempted
meta-analysis ofsimilar studies [97] concluded that the
designs ofthese studies and measures used were too
varied to quantify risk meaningfully,and mostof the
studies had not excluded reverse causation or controlled
adequately for confounding.
A recent study of mortality among 6445 people
treated for a cannabis use disorder in Norway found an
elevated risk ofsuicide (OR = 5.3, CI = 3.3, 7.79) [120].
This sample included much heavier problematic cannabis
usersthan have been studied in the cohortstudies.
Moreover, a substantial proportion ofthese problem can-
nabis users had also injected illicit drugs,a behaviour
that substantially increases suicide mortality [51]. Exclu-
sion of cannabis users who were known to be injectors at
the time oftreatment marginally reduced the suicide risk
(OR = 4.8, 95% CI = 2.4, 8.9). The study relied upon case
registers so there was a limited ability to control for other
possible confounders,but it suggests thatpre-existing
suicide risk may be elevated among heavy cannabis users
who seek treatment.
Adverse health effects oflong-term cannabis smoking
Respiratory system
In 1993 there were studiesreporting thatregular
cannabis smokers reported more symptoms ofchronic
bronchitis(wheeze,sputum production and chronic
coughs)than non-smokers(see [121]for a review).
Follow-up studies ofregular cannabis-only smokers also
found impaired respiratory function and pathological
changes in lung tissue like those preceding the develop-
ment ofchronic obstructive pulmonary disease [121].
Since 1993 epidemiologicalstudies have raised con-
cerns about the respiratory risks ofcannabis smoking
without producing a clear picture, because most canna-
bis smokers also smoke tobacco or are former smokers
(see [122] for a review). A cohort study of members of an
HMO reported thatcannabis-only smokershad more
health service use for respiratory infections than non-
users ofcannabis [123].In other cohortstudies,the
effects oflong-term cannabis smoking on respiratory
function were less clear [121].A longitudinalstudy of
1037 New Zealand youths followed until the age of26
[124] reported impaired respiratory function in depend-
ent cannabis users,but a longer-term follow-up ofa
larger sample ofUS cannabis users did not replicate this
finding [123]. Chronic cannabis smoking did not increase
the risk ofemphysema in follow-up studies ofcannabis
smokers in the United States [125,126] and New Zealand
[127].
The large US cohort study that followed more than
5000 young adults for 20 years [125]found a dose–
response relationship between cigarette smoking and
poor respiratory function, but the relationship with can-
nabis smoking was more complicated: low levels ofcan-
nabis smoking (a median ofthree to five joints each
month)appeared to increase respiratory function,but
respiratory function declined in daily cannabis smokers.
The authors hypothesized thatthe effects ofcannabis
smoking may depend upon the frequency ofuse:at a
lower frequency ofuse it increases respiratory volume,
either because offrequent deep inhalation and breath-
holding or possibly because THC has bronchodilatory
effects;at higher frequencies ofuse,these effects were
over-ridden by the cumulative adverse effects ofcannabis
smoke on lung function.
Cardiovascular effects
In 1993, we found that laboratory studies had reported
that cannabissmoking increasedheart rate in a
Cannabis health effects9
© 2014 Society for the Study ofAddiction Addiction
cannabis use disorders among people diagnosed with
bipolar disorders than in the generalpopulation (e.g.
[111–114]).In one longitudinalstudy,cannabis use at
baseline predicted an increased risk ofmanic symptoms
in a 3-year follow-up [115].In some clinicalstudies,
people with bipolar disorders who continue to use canna-
bis have more manic episodes and are less satisfied with
their lives than bipolar peers who do not use cannabis
[113]. These findings suggest that regular cannabis use
may play a contributory causal role in bipolar disorders,
but the case is not yet proved because these studies have
not controlled adequately for confounding variables or
ruled out reverse causation [113].
Several case–control and cohort studies have reported
associations between cannabis use and suicide in adoles-
cents and young adults.For example,a New Zealand
case–controlstudy [116] of suicide attemptsthat
resulted in hospitalization found that 16% ofthe 302
suicide attempters had a cannabis disorder compared
with 2% of1028 community controls.Controlling for
social disadvantage, depression and alcohol dependence
substantially reduced but did not eliminate the associa-
tion (adjusted OR of2).
The evidencefrom prospectivestudiesis mixed.
Fergusson & Horwood [109], for example, found a dose–
response relationship between frequency ofcannabis use
by age 16 and self-reported suicide attempts,but the
association did not persist after controlling for confound-
ers. A recent analysis ofthe data from this cohort [117]
using econometricmethodsfound that more than
weekly cannabis use increased the likelihood ofreport-
ing suicidalideation,but only in males.Patton et al.
[118],by contrast,found that cannabis was associated
with self-harm only in females. Rasic et al. [119]
reported that heavy cannabis use increased the risk of
depression but did not affect suicide risk. An attempted
meta-analysis ofsimilar studies [97] concluded that the
designs ofthese studies and measures used were too
varied to quantify risk meaningfully,and mostof the
studies had not excluded reverse causation or controlled
adequately for confounding.
A recent study of mortality among 6445 people
treated for a cannabis use disorder in Norway found an
elevated risk ofsuicide (OR = 5.3, CI = 3.3, 7.79) [120].
This sample included much heavier problematic cannabis
usersthan have been studied in the cohortstudies.
Moreover, a substantial proportion ofthese problem can-
nabis users had also injected illicit drugs,a behaviour
that substantially increases suicide mortality [51]. Exclu-
sion of cannabis users who were known to be injectors at
the time oftreatment marginally reduced the suicide risk
(OR = 4.8, 95% CI = 2.4, 8.9). The study relied upon case
registers so there was a limited ability to control for other
possible confounders,but it suggests thatpre-existing
suicide risk may be elevated among heavy cannabis users
who seek treatment.
Adverse health effects oflong-term cannabis smoking
Respiratory system
In 1993 there were studiesreporting thatregular
cannabis smokers reported more symptoms ofchronic
bronchitis(wheeze,sputum production and chronic
coughs)than non-smokers(see [121]for a review).
Follow-up studies ofregular cannabis-only smokers also
found impaired respiratory function and pathological
changes in lung tissue like those preceding the develop-
ment ofchronic obstructive pulmonary disease [121].
Since 1993 epidemiologicalstudies have raised con-
cerns about the respiratory risks ofcannabis smoking
without producing a clear picture, because most canna-
bis smokers also smoke tobacco or are former smokers
(see [122] for a review). A cohort study of members of an
HMO reported thatcannabis-only smokershad more
health service use for respiratory infections than non-
users ofcannabis [123].In other cohortstudies,the
effects oflong-term cannabis smoking on respiratory
function were less clear [121].A longitudinalstudy of
1037 New Zealand youths followed until the age of26
[124] reported impaired respiratory function in depend-
ent cannabis users,but a longer-term follow-up ofa
larger sample ofUS cannabis users did not replicate this
finding [123]. Chronic cannabis smoking did not increase
the risk ofemphysema in follow-up studies ofcannabis
smokers in the United States [125,126] and New Zealand
[127].
The large US cohort study that followed more than
5000 young adults for 20 years [125]found a dose–
response relationship between cigarette smoking and
poor respiratory function, but the relationship with can-
nabis smoking was more complicated: low levels ofcan-
nabis smoking (a median ofthree to five joints each
month)appeared to increase respiratory function,but
respiratory function declined in daily cannabis smokers.
The authors hypothesized thatthe effects ofcannabis
smoking may depend upon the frequency ofuse:at a
lower frequency ofuse it increases respiratory volume,
either because offrequent deep inhalation and breath-
holding or possibly because THC has bronchodilatory
effects;at higher frequencies ofuse,these effects were
over-ridden by the cumulative adverse effects ofcannabis
smoke on lung function.
Cardiovascular effects
In 1993, we found that laboratory studies had reported
that cannabissmoking increasedheart rate in a
Cannabis health effects9
© 2014 Society for the Study ofAddiction Addiction
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
dose-related way (see reviews [128,129]), but that toler-
ance to these effects developed rapidly in healthy young
adults. There was clinical evidencethat cannabis
smoking could produce symptoms ofangina in older
adults with cardiovascular disease who used cannabis
[130].
The evidence has notincreased a greatdealsince
1993, but it is consistent with cannabis smoking having
adverse cardiovascular effects in middle-aged and older
adults.A case–cross-over study [131] of3882 patients
who had had a myocardial infarction found that cannabis
use acutely increased the risk ofa myocardial infarction:
it quadrupled the risk in the hour after smoking cannabis.
A prospective study of1913 of these patients found a
dose–response relationship between frequency ofcanna-
bis use and mortality over 3.8 years [132]. These findings
support the older laboratory studies showing that canna-
bis smoking can produce angina in patients with heart
disease [130].
The cardiovascularrisks of cannabissmoking are
probably highest in older adults, but younger adults with
undiagnosed cardiovascular disease may also be at risk.
A French study,for example,of 200 cannabis-related
hospitalizations in the Toulouse area between January
2004 and December 2007 included several cases of myo-
cardial infarction and a fatal stroke in young adults who
had recently used cannabis and had no other known risk
factorsfor these disorders[133]. These case reports
suggest that cannabis smoking can provoke fatal cardio-
vascular events in young individuals with undiagnosed
cardiovascular disease.
Cannabis and cancer
THC and other cannabinoids are not potentialcarcino-
gens in microbial assays, such as the Ames test [134,135]
or testsusing ratsand mice [136].Cannabissmoke
is carcinogenic in standard laboratory assays
[134,135,137]. The fact that it is cannabis smoke that is
carcinogenic [21] suggests that cannabis smoking may be
a cause of cancers of the lung and the upper aerodigestive
tract (mouth, tongue, oesophagus) and bladder [134].
Respiratory cancers
In 1993 the main reasons for suspecting that cannabis
use could cause lung and upper respiratory tract cancers
was that cannabis smoke contained many ofthe same
carcinogens as tobacco smoke [138].In a few case–
controlstudies,regular cannabis smokers had shown
pathologicalchangesin lung cells of the type that
precede lung cancer in tobacco smokers [139].There
were also case reports of lung cancer in young adults who
did not smoke tobacco, but there were no case–control or
prospective studies showing higher rates ofany ofthese
cancers among cannabis smokers [9].
Epidemiologicalstudiessince 1993 have produced
inconsistent results.Sidney et al.[140] did not find an
increased risk ofrespiratory cancerin an 8.6-year
follow-up of64 855 members ofthe Kaiser Permanente
Medical Care Program, but rates ofregular cannabis use
were low and follow-up stopped at age 42.Zhang et al.
[141] reported an increased risk (OR of2) ofsquamous
cellcarcinoma ofthe head and neck among cannabis
users in 173 cases and 176 controls. The effect persisted
after adjusting for cigarette smoking,alcoholuse and
other risk factors;but three other case–controlstudies
failed to find any association between cannabis use and
these cancers [142].
Case–controlstudies oflung cancer have produced
more consistent associations, but in all these studies can-
nabis smoking has been confounded by cigarette smoking
[143].A Tunisian case–controlstudy of110 cases of
hospital diagnosed lung cancer and 110 community con-
trols found an association with cannabis use (OR = 8.2)
that persisted after adjustment for cigarette smoking. A
pooled analysis ofthree Moroccan case–controlstudies
also found an elevated risk oflung cancer among canna-
bis smokers,but all their cannabis users also smoked
tobacco [144]. A New Zealand case–control study of lung
cancer in 79 adults under the age of55 years and 324
community controls [145] found a dose–response rela-
tionship between frequency ofcannabis use and lung
cancer risk. A US case–control study found an association
between cannabis smoking and head and neck and lung
cancers, but the associations were no longer significant
after controlling for tobacco use [146].
A recent 40-year follow-up of lung cancer cases in the
Swedish conscript cohort [147] found a doubling ofthe
risk oflung cancer among conscripts who had smoked
cannabis 50 or more times by age 18.This survived
adjustmentfor cigarette smoking (which showed the
expected dose–response relationship to lung cancer), but
the ability to adjust fully for tobacco smoking was limited
because 91% ofheavy cannabis smokers at age 18 also
smoked tobacco. Larger cohort and better-designed case–
controlstudies thatcontrolfor cigarette smoking are
needed to clarify lung cancerrisk among long-term
regular cannabis smokers [142].
Maternal cannabis use and childhood cancers
Cannabis smoking during pregnancy has been associated
with cancers among children. Three case–control studies
examined cannabis use as one ofmany risk factors for
thesecancersand found an association [148–150].
Unlike respiratory cancers, there was no a priori reason to
expect a relationship between cannabis use and the risk of
developing any ofthese cancers. We concluded in 1993
that these associations were unlikely to be causal. Since
then, there have been no further studies replicating these
10 Wayne Hall
© 2014 Society for the Study ofAddiction Addiction
ance to these effects developed rapidly in healthy young
adults. There was clinical evidencethat cannabis
smoking could produce symptoms ofangina in older
adults with cardiovascular disease who used cannabis
[130].
The evidence has notincreased a greatdealsince
1993, but it is consistent with cannabis smoking having
adverse cardiovascular effects in middle-aged and older
adults.A case–cross-over study [131] of3882 patients
who had had a myocardial infarction found that cannabis
use acutely increased the risk ofa myocardial infarction:
it quadrupled the risk in the hour after smoking cannabis.
A prospective study of1913 of these patients found a
dose–response relationship between frequency ofcanna-
bis use and mortality over 3.8 years [132]. These findings
support the older laboratory studies showing that canna-
bis smoking can produce angina in patients with heart
disease [130].
The cardiovascularrisks of cannabissmoking are
probably highest in older adults, but younger adults with
undiagnosed cardiovascular disease may also be at risk.
A French study,for example,of 200 cannabis-related
hospitalizations in the Toulouse area between January
2004 and December 2007 included several cases of myo-
cardial infarction and a fatal stroke in young adults who
had recently used cannabis and had no other known risk
factorsfor these disorders[133]. These case reports
suggest that cannabis smoking can provoke fatal cardio-
vascular events in young individuals with undiagnosed
cardiovascular disease.
Cannabis and cancer
THC and other cannabinoids are not potentialcarcino-
gens in microbial assays, such as the Ames test [134,135]
or testsusing ratsand mice [136].Cannabissmoke
is carcinogenic in standard laboratory assays
[134,135,137]. The fact that it is cannabis smoke that is
carcinogenic [21] suggests that cannabis smoking may be
a cause of cancers of the lung and the upper aerodigestive
tract (mouth, tongue, oesophagus) and bladder [134].
Respiratory cancers
In 1993 the main reasons for suspecting that cannabis
use could cause lung and upper respiratory tract cancers
was that cannabis smoke contained many ofthe same
carcinogens as tobacco smoke [138].In a few case–
controlstudies,regular cannabis smokers had shown
pathologicalchangesin lung cells of the type that
precede lung cancer in tobacco smokers [139].There
were also case reports of lung cancer in young adults who
did not smoke tobacco, but there were no case–control or
prospective studies showing higher rates ofany ofthese
cancers among cannabis smokers [9].
Epidemiologicalstudiessince 1993 have produced
inconsistent results.Sidney et al.[140] did not find an
increased risk ofrespiratory cancerin an 8.6-year
follow-up of64 855 members ofthe Kaiser Permanente
Medical Care Program, but rates ofregular cannabis use
were low and follow-up stopped at age 42.Zhang et al.
[141] reported an increased risk (OR of2) ofsquamous
cellcarcinoma ofthe head and neck among cannabis
users in 173 cases and 176 controls. The effect persisted
after adjusting for cigarette smoking,alcoholuse and
other risk factors;but three other case–controlstudies
failed to find any association between cannabis use and
these cancers [142].
Case–controlstudies oflung cancer have produced
more consistent associations, but in all these studies can-
nabis smoking has been confounded by cigarette smoking
[143].A Tunisian case–controlstudy of110 cases of
hospital diagnosed lung cancer and 110 community con-
trols found an association with cannabis use (OR = 8.2)
that persisted after adjustment for cigarette smoking. A
pooled analysis ofthree Moroccan case–controlstudies
also found an elevated risk oflung cancer among canna-
bis smokers,but all their cannabis users also smoked
tobacco [144]. A New Zealand case–control study of lung
cancer in 79 adults under the age of55 years and 324
community controls [145] found a dose–response rela-
tionship between frequency ofcannabis use and lung
cancer risk. A US case–control study found an association
between cannabis smoking and head and neck and lung
cancers, but the associations were no longer significant
after controlling for tobacco use [146].
A recent 40-year follow-up of lung cancer cases in the
Swedish conscript cohort [147] found a doubling ofthe
risk oflung cancer among conscripts who had smoked
cannabis 50 or more times by age 18.This survived
adjustmentfor cigarette smoking (which showed the
expected dose–response relationship to lung cancer), but
the ability to adjust fully for tobacco smoking was limited
because 91% ofheavy cannabis smokers at age 18 also
smoked tobacco. Larger cohort and better-designed case–
controlstudies thatcontrolfor cigarette smoking are
needed to clarify lung cancerrisk among long-term
regular cannabis smokers [142].
Maternal cannabis use and childhood cancers
Cannabis smoking during pregnancy has been associated
with cancers among children. Three case–control studies
examined cannabis use as one ofmany risk factors for
thesecancersand found an association [148–150].
Unlike respiratory cancers, there was no a priori reason to
expect a relationship between cannabis use and the risk of
developing any ofthese cancers. We concluded in 1993
that these associations were unlikely to be causal. Since
then, there have been no further studies replicating these
10 Wayne Hall
© 2014 Society for the Study ofAddiction Addiction
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
findingsand the incidence ofthese cancersdid not
increase over the period 1979–95 in the United States
[151–153].
Male cancers
An elevated risk of prostatecancer was reported
among cannabis smokers in Sidney et al.’s study [140]
of cancerincidence during an 8.6-yearfollow-up of
64 855 members ofthe Kaiser Permanente Medical Care
Program.There was no overallexcess ofcancer when
those who had ever used cannabis or who were current
users were compared to those who were non-users at
study entry (RR = 0.9,95% CI = 0.7,1.2). However,
males who smoked cannabis had an increased risk of pros-
tate cancer,as did males who were currentcannabis
smokers [140]. Confounding by other life-style factors was
a possible explanation ofthe finding,because AIDS-
related deaths were higher among cannabis users in this
study.
There is more cause for concern about recent reports
of an increased risk oftesticular cancer among cannabis
users. Daling et al. [154] reported a case–control study of
cannabis use among 369 men diagnosed with a testicular
germ cell tumour and 979 age-matchedcontrols.
They found a higher rate ofcannabis use among cases
(OR = 1.7,95% CI = 1.1,2.5).The risk was higher for
a non-seminoma (OR = 2.3,95% CI = 1.4,4.0) and
increased for those who began to use cannabis before the
age of 18 and those who used cannabismore than
weekly. These findings have since been replicated in two
further US case–control studies [155,156]. These studies
found a doubling ofrisk of non-seminoma testicular
tumours among cannabis users and suggestive evidence
that risk increased with earlier initiation and more fre-
quent use of cannabis. The replication of these findings in
three case–controlstudies indicates an effect requiring
further investigation.It is also a biologically plausible
effect, given that cannabinoid receptors are found in the
male reproductive system.
THE HEALTH EFFECTS OF INCREASED
THC IN CANNABIS PRODUCTS
In 1993 there were claims that the THC content ofcan-
nabis had increased sharply. Analyses of US cannabis sei-
zures reported a 30% increase in THC content, but there
were no good time trend data on THC levels in cannabis
outside the United States as late as 1999 [157].Since
2000 it has become clearer that the THC content ofcan-
nabis products increased during the 1990s and early
2000s in the United States and in many other developed
countries[5,158,159].It is less clear whetherthe
increased THC content has been accompanied by sub-
stantialreductions in CBD content,a cannabinoid that
some researchers argue may moderate the adverse effects
of THC [160].
How may the use of cannabis products with increased
THC content affect the likelihood of adverse health effects?
Some argue that the effects will be minimal, because users
titrate their doses ofTHC to achieve the desired level of
intoxication,but recent evidence suggests that regular
cannabis users titrate their THC doses incompletely when
given more potent cannabis products [161].
The impacts ofincreased potency on cannabis use
should be a research priority.The following are some
plausible hypotheses which assume thatthe effects of
increased cannabis potency will depend upon the extent of
users’ experience with cannabis. A higher THC content
may increase anxiety, depression and psychotic symptoms
in naive users. This may explain the increased emergency
room attendances for cannabis in the United States. It may
also deter continued use in those who experience these
effects. More potent cannabis products may also increase
the risks of dependence and psychotic symptomsin
regular users. Adverse effects on the respiratory and car-
diovascular systems may be reduced to the extent that
regular users titrate their THC dose by smoking less.
WHAT HAVE WE LEARNED IN 20 YEARS?
We know much more in 2013 about the adverse psycho-
socialeffects ofcannabis than we did in 1993.This is
largely because many more epidemiological studies have
been conducted on the effects ofcannabis use in adoles-
cence and young adulthood on psychosocial outcomes in
the late 20s and early 30s (e.g. [63,162,163]). The best-
designed and most informative of these studies have been
two New Zealand birth cohort studies whose members
lived through a historicalperiod during which a large
proportion used cannabis during adolescence and young
adulthood; sufficient numbers of these had used cannabis
often enough, and for long enough, to provide informa-
tion about the adverse effects ofregular and sustained
cannabisuse. Confidence in the resultsof the New
Zealand studies has been increased by the replication of
their results in cohort studies in Australia (e.g.[164]),
Germany [165] and the Netherlands [93]. The fact that
cannabis dependence and some ofthese adverse effects
have also been reported in the Netherlands (where can-
nabis has been decriminalized for nearly 40 years) makes
it unlikely that these adverse psychosocial effects can be
attributed to legal policies towards cannabis.
The epidemiologicalevidence has strengthened for
many ofthe probable adverse health effects that we iden-
tified in 1993. There have been consistent associations
found between regular (especially daily) cannabis use and
adverse health and psychosocial outcomes, relationships
Cannabis health effects11
© 2014 Society for the Study ofAddiction Addiction
increase over the period 1979–95 in the United States
[151–153].
Male cancers
An elevated risk of prostatecancer was reported
among cannabis smokers in Sidney et al.’s study [140]
of cancerincidence during an 8.6-yearfollow-up of
64 855 members ofthe Kaiser Permanente Medical Care
Program.There was no overallexcess ofcancer when
those who had ever used cannabis or who were current
users were compared to those who were non-users at
study entry (RR = 0.9,95% CI = 0.7,1.2). However,
males who smoked cannabis had an increased risk of pros-
tate cancer,as did males who were currentcannabis
smokers [140]. Confounding by other life-style factors was
a possible explanation ofthe finding,because AIDS-
related deaths were higher among cannabis users in this
study.
There is more cause for concern about recent reports
of an increased risk oftesticular cancer among cannabis
users. Daling et al. [154] reported a case–control study of
cannabis use among 369 men diagnosed with a testicular
germ cell tumour and 979 age-matchedcontrols.
They found a higher rate ofcannabis use among cases
(OR = 1.7,95% CI = 1.1,2.5).The risk was higher for
a non-seminoma (OR = 2.3,95% CI = 1.4,4.0) and
increased for those who began to use cannabis before the
age of 18 and those who used cannabismore than
weekly. These findings have since been replicated in two
further US case–control studies [155,156]. These studies
found a doubling ofrisk of non-seminoma testicular
tumours among cannabis users and suggestive evidence
that risk increased with earlier initiation and more fre-
quent use of cannabis. The replication of these findings in
three case–controlstudies indicates an effect requiring
further investigation.It is also a biologically plausible
effect, given that cannabinoid receptors are found in the
male reproductive system.
THE HEALTH EFFECTS OF INCREASED
THC IN CANNABIS PRODUCTS
In 1993 there were claims that the THC content ofcan-
nabis had increased sharply. Analyses of US cannabis sei-
zures reported a 30% increase in THC content, but there
were no good time trend data on THC levels in cannabis
outside the United States as late as 1999 [157].Since
2000 it has become clearer that the THC content ofcan-
nabis products increased during the 1990s and early
2000s in the United States and in many other developed
countries[5,158,159].It is less clear whetherthe
increased THC content has been accompanied by sub-
stantialreductions in CBD content,a cannabinoid that
some researchers argue may moderate the adverse effects
of THC [160].
How may the use of cannabis products with increased
THC content affect the likelihood of adverse health effects?
Some argue that the effects will be minimal, because users
titrate their doses ofTHC to achieve the desired level of
intoxication,but recent evidence suggests that regular
cannabis users titrate their THC doses incompletely when
given more potent cannabis products [161].
The impacts ofincreased potency on cannabis use
should be a research priority.The following are some
plausible hypotheses which assume thatthe effects of
increased cannabis potency will depend upon the extent of
users’ experience with cannabis. A higher THC content
may increase anxiety, depression and psychotic symptoms
in naive users. This may explain the increased emergency
room attendances for cannabis in the United States. It may
also deter continued use in those who experience these
effects. More potent cannabis products may also increase
the risks of dependence and psychotic symptomsin
regular users. Adverse effects on the respiratory and car-
diovascular systems may be reduced to the extent that
regular users titrate their THC dose by smoking less.
WHAT HAVE WE LEARNED IN 20 YEARS?
We know much more in 2013 about the adverse psycho-
socialeffects ofcannabis than we did in 1993.This is
largely because many more epidemiological studies have
been conducted on the effects ofcannabis use in adoles-
cence and young adulthood on psychosocial outcomes in
the late 20s and early 30s (e.g. [63,162,163]). The best-
designed and most informative of these studies have been
two New Zealand birth cohort studies whose members
lived through a historicalperiod during which a large
proportion used cannabis during adolescence and young
adulthood; sufficient numbers of these had used cannabis
often enough, and for long enough, to provide informa-
tion about the adverse effects ofregular and sustained
cannabisuse. Confidence in the resultsof the New
Zealand studies has been increased by the replication of
their results in cohort studies in Australia (e.g.[164]),
Germany [165] and the Netherlands [93]. The fact that
cannabis dependence and some ofthese adverse effects
have also been reported in the Netherlands (where can-
nabis has been decriminalized for nearly 40 years) makes
it unlikely that these adverse psychosocial effects can be
attributed to legal policies towards cannabis.
The epidemiologicalevidence has strengthened for
many ofthe probable adverse health effects that we iden-
tified in 1993. There have been consistent associations
found between regular (especially daily) cannabis use and
adverse health and psychosocial outcomes, relationships
Cannabis health effects11
© 2014 Society for the Study ofAddiction Addiction
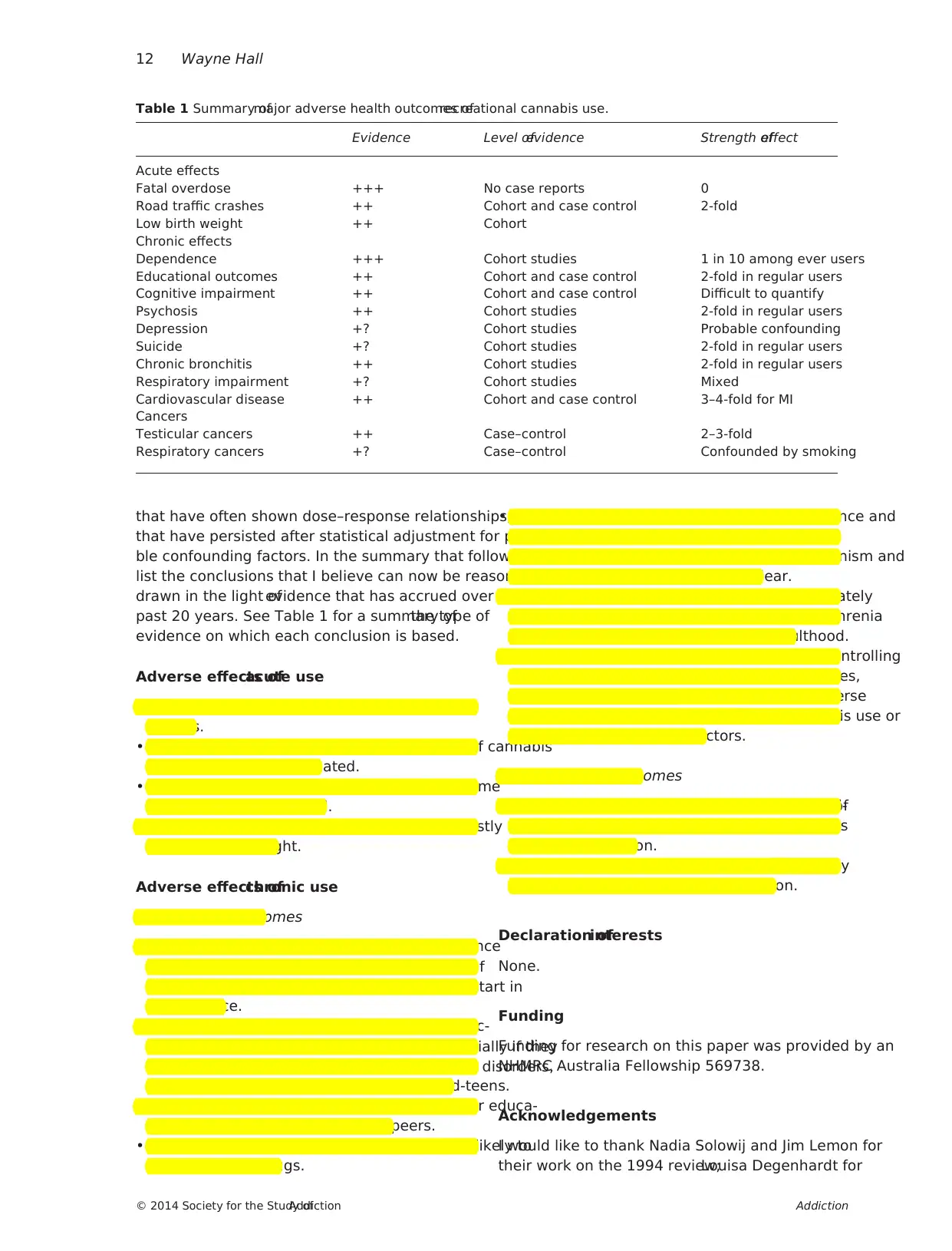
that have often shown dose–response relationships, and
that have persisted after statistical adjustment for plausi-
ble confounding factors. In the summary that follows, I
list the conclusions that I believe can now be reasonably
drawn in the light ofevidence that has accrued over the
past 20 years. See Table 1 for a summary ofthe type of
evidence on which each conclusion is based.
Adverse effects ofacute use
• Cannabisdoesnot producefatal overdosesas do
opioids.
• There is a doubling of the risk of car crashes if cannabis
users drive while intoxicated.
• This risk increases substantially ifusers also consume
intoxicating doses ofalcohol.
• Maternalcannabisuse during pregnancy modestly
reduces birth weight.
Adverse effects ofchronic use
Psychosocial outcomes
• Regularcannabisuserscan develop a dependence
syndrome, the risks ofwhich are around 1 in 10 ofall
cannabis users and 1 in 6 among those who start in
adolescence.
• Regular cannabis users double their risks ofexperienc-
ing psychotic symptoms and disorders, especially if they
have a personal or family history of psychotic disorders,
and ifthey initiate cannabis use in their mid-teens.
• Regular adolescent cannabis users have lower educa-
tional attainment than non-using peers.
• Regular adolescent cannabis users are more likely to
use other illicit drugs.
• Regular cannabis use that begins in adolescence and
continuesthroughoutyoung adulthood appearsto
produce cognitive impairment but the mechanism and
reversibility ofthe impairment is unclear.
• Regularcannabisuse in adolescence approximately
doubles the risk ofbeing diagnosed with schizophrenia
or reporting psychotic symptoms in adulthood.
• All these relationships have persisted after controlling
for plausibleconfoundersin well-designed studies,
but some researchers stillquestion whether adverse
effects are related causally to regular cannabis use or
explained by shared risk factors.
Physical health outcomes
• Regular cannabis smokers have higher risks ofdevel-
oping chronic bronchitis, but it is unclear ifit impairs
respiratory function.
• Cannabissmoking by middle-aged adultsprobably
increases the risks ofmyocardial infarction.
Declaration ofinterests
None.
Funding
Funding for research on this paper was provided by an
NHMRC Australia Fellowship 569738.
Acknowledgements
I would like to thank Nadia Solowij and Jim Lemon for
their work on the 1994 review;Louisa Degenhardt for
Table 1 Summary ofmajor adverse health outcomes ofrecreational cannabis use.
Evidence Level ofevidence Strength ofeffect
Acute effects
Fatal overdose +++ No case reports 0
Road traffic crashes ++ Cohort and case control 2-fold
Low birth weight ++ Cohort
Chronic effects
Dependence +++ Cohort studies 1 in 10 among ever users
Educational outcomes ++ Cohort and case control 2-fold in regular users
Cognitive impairment ++ Cohort and case control Difficult to quantify
Psychosis ++ Cohort studies 2-fold in regular users
Depression +? Cohort studies Probable confounding
Suicide +? Cohort studies 2-fold in regular users
Chronic bronchitis ++ Cohort studies 2-fold in regular users
Respiratory impairment +? Cohort studies Mixed
Cardiovascular disease ++ Cohort and case control 3–4-fold for MI
Cancers
Testicular cancers ++ Case–control 2–3-fold
Respiratory cancers +? Case–control Confounded by smoking
12 Wayne Hall
© 2014 Society for the Study ofAddiction Addiction
that have persisted after statistical adjustment for plausi-
ble confounding factors. In the summary that follows, I
list the conclusions that I believe can now be reasonably
drawn in the light ofevidence that has accrued over the
past 20 years. See Table 1 for a summary ofthe type of
evidence on which each conclusion is based.
Adverse effects ofacute use
• Cannabisdoesnot producefatal overdosesas do
opioids.
• There is a doubling of the risk of car crashes if cannabis
users drive while intoxicated.
• This risk increases substantially ifusers also consume
intoxicating doses ofalcohol.
• Maternalcannabisuse during pregnancy modestly
reduces birth weight.
Adverse effects ofchronic use
Psychosocial outcomes
• Regularcannabisuserscan develop a dependence
syndrome, the risks ofwhich are around 1 in 10 ofall
cannabis users and 1 in 6 among those who start in
adolescence.
• Regular cannabis users double their risks ofexperienc-
ing psychotic symptoms and disorders, especially if they
have a personal or family history of psychotic disorders,
and ifthey initiate cannabis use in their mid-teens.
• Regular adolescent cannabis users have lower educa-
tional attainment than non-using peers.
• Regular adolescent cannabis users are more likely to
use other illicit drugs.
• Regular cannabis use that begins in adolescence and
continuesthroughoutyoung adulthood appearsto
produce cognitive impairment but the mechanism and
reversibility ofthe impairment is unclear.
• Regularcannabisuse in adolescence approximately
doubles the risk ofbeing diagnosed with schizophrenia
or reporting psychotic symptoms in adulthood.
• All these relationships have persisted after controlling
for plausibleconfoundersin well-designed studies,
but some researchers stillquestion whether adverse
effects are related causally to regular cannabis use or
explained by shared risk factors.
Physical health outcomes
• Regular cannabis smokers have higher risks ofdevel-
oping chronic bronchitis, but it is unclear ifit impairs
respiratory function.
• Cannabissmoking by middle-aged adultsprobably
increases the risks ofmyocardial infarction.
Declaration ofinterests
None.
Funding
Funding for research on this paper was provided by an
NHMRC Australia Fellowship 569738.
Acknowledgements
I would like to thank Nadia Solowij and Jim Lemon for
their work on the 1994 review;Louisa Degenhardt for
Table 1 Summary ofmajor adverse health outcomes ofrecreational cannabis use.
Evidence Level ofevidence Strength ofeffect
Acute effects
Fatal overdose +++ No case reports 0
Road traffic crashes ++ Cohort and case control 2-fold
Low birth weight ++ Cohort
Chronic effects
Dependence +++ Cohort studies 1 in 10 among ever users
Educational outcomes ++ Cohort and case control 2-fold in regular users
Cognitive impairment ++ Cohort and case control Difficult to quantify
Psychosis ++ Cohort studies 2-fold in regular users
Depression +? Cohort studies Probable confounding
Suicide +? Cohort studies 2-fold in regular users
Chronic bronchitis ++ Cohort studies 2-fold in regular users
Respiratory impairment +? Cohort studies Mixed
Cardiovascular disease ++ Cohort and case control 3–4-fold for MI
Cancers
Testicular cancers ++ Case–control 2–3-fold
Respiratory cancers +? Case–control Confounded by smoking
12 Wayne Hall
© 2014 Society for the Study ofAddiction Addiction
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
