Health Information Management Virtual Tour Worksheet - University Name
VerifiedAdded on 2022/08/16
|6
|903
|9
Homework Assignment
AI Summary
This homework assignment presents a completed worksheet based on a virtual tour of a Health Information Management (HIM) department at a hospital. The student answers questions regarding ambulatory visits, outpatient diagnostics, medical record numbers, document scanning, electronic health records (EHR), paper record destruction, physician order completion, common medical record reports, electronic flags, coding, and credentialing. The assignment also covers topics such as delinquent records, HIPAA mandates, data breaches, transcription, cancer registry requirements, the Master Patient Index (MPI), data quality management, and data visualization. The answers are derived from a video tour of the Sinclair Memorial Hospital HIM department, providing a practical understanding of HIM processes and terminology.

Health Information Management Virtual Tour
Student Work Sheet
Work sheet- Health Information Management
Name of the student
Name of the University
Authors Note
Student Work Sheet
Work sheet- Health Information Management
Name of the student
Name of the University
Authors Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Health Information Management Virtual Tour
Student Work Sheet
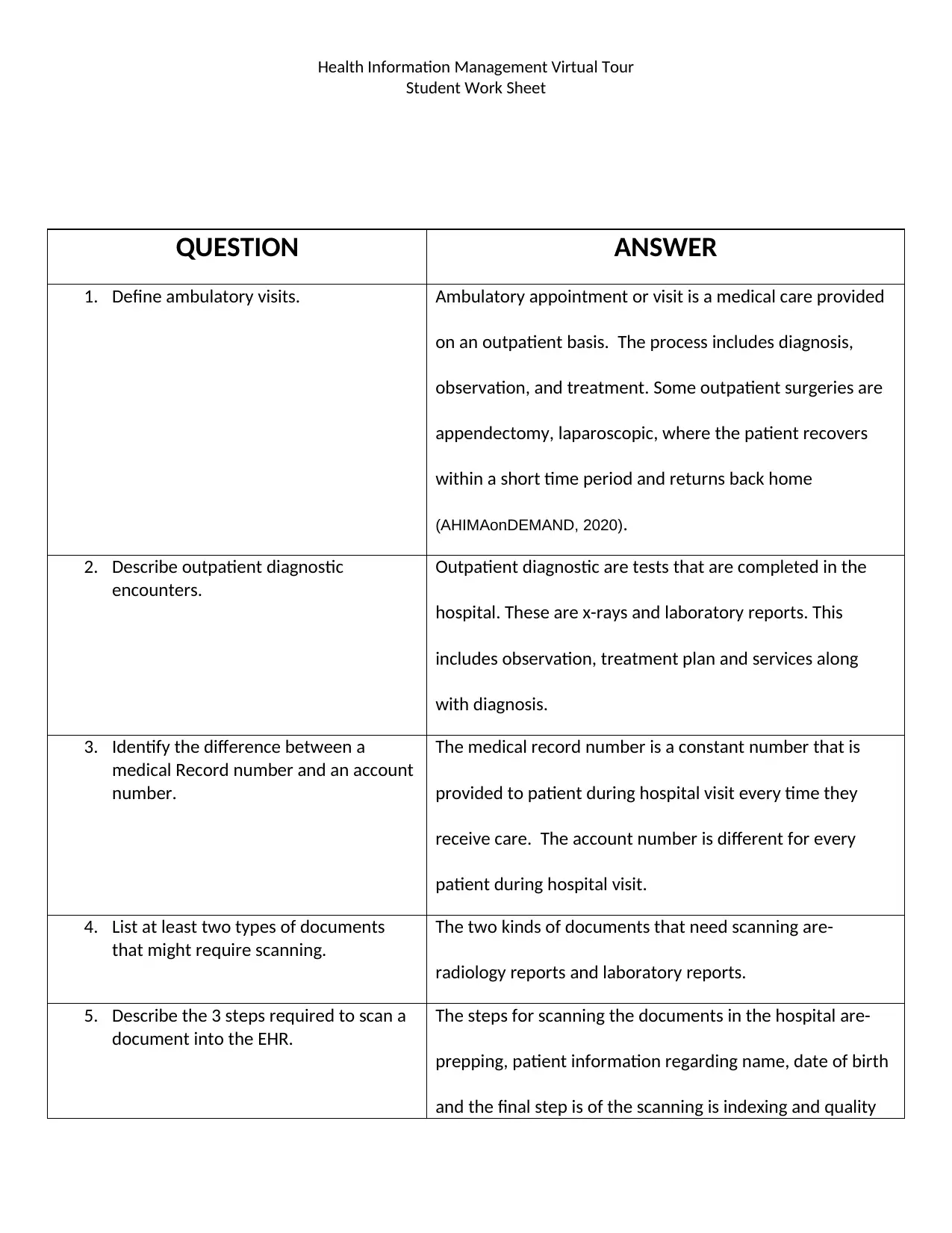
QUESTION ANSWER
1. Define ambulatory visits. Ambulatory appointment or visit is a medical care provided
on an outpatient basis. The process includes diagnosis,
observation, and treatment. Some outpatient surgeries are
appendectomy, laparoscopic, where the patient recovers
within a short time period and returns back home
(AHIMAonDEMAND, 2020).
2. Describe outpatient diagnostic
encounters.
Outpatient diagnostic are tests that are completed in the
hospital. These are x-rays and laboratory reports. This
includes observation, treatment plan and services along
with diagnosis.
3. Identify the difference between a
medical Record number and an account
number.
The medical record number is a constant number that is
provided to patient during hospital visit every time they
receive care. The account number is different for every
patient during hospital visit.
4. List at least two types of documents
that might require scanning.
The two kinds of documents that need scanning are-
radiology reports and laboratory reports.
5. Describe the 3 steps required to scan a
document into the EHR.
The steps for scanning the documents in the hospital are-
prepping, patient information regarding name, date of birth
and the final step is of the scanning is indexing and quality
Student Work Sheet
QUESTION ANSWER
1. Define ambulatory visits. Ambulatory appointment or visit is a medical care provided
on an outpatient basis. The process includes diagnosis,
observation, and treatment. Some outpatient surgeries are
appendectomy, laparoscopic, where the patient recovers
within a short time period and returns back home
(AHIMAonDEMAND, 2020).
2. Describe outpatient diagnostic
encounters.
Outpatient diagnostic are tests that are completed in the
hospital. These are x-rays and laboratory reports. This
includes observation, treatment plan and services along
with diagnosis.
3. Identify the difference between a
medical Record number and an account
number.
The medical record number is a constant number that is
provided to patient during hospital visit every time they
receive care. The account number is different for every
patient during hospital visit.
4. List at least two types of documents
that might require scanning.
The two kinds of documents that need scanning are-
radiology reports and laboratory reports.
5. Describe the 3 steps required to scan a
document into the EHR.
The steps for scanning the documents in the hospital are-
prepping, patient information regarding name, date of birth
and the final step is of the scanning is indexing and quality
Health Information Management Virtual Tour
Student Work Sheet
assurance.
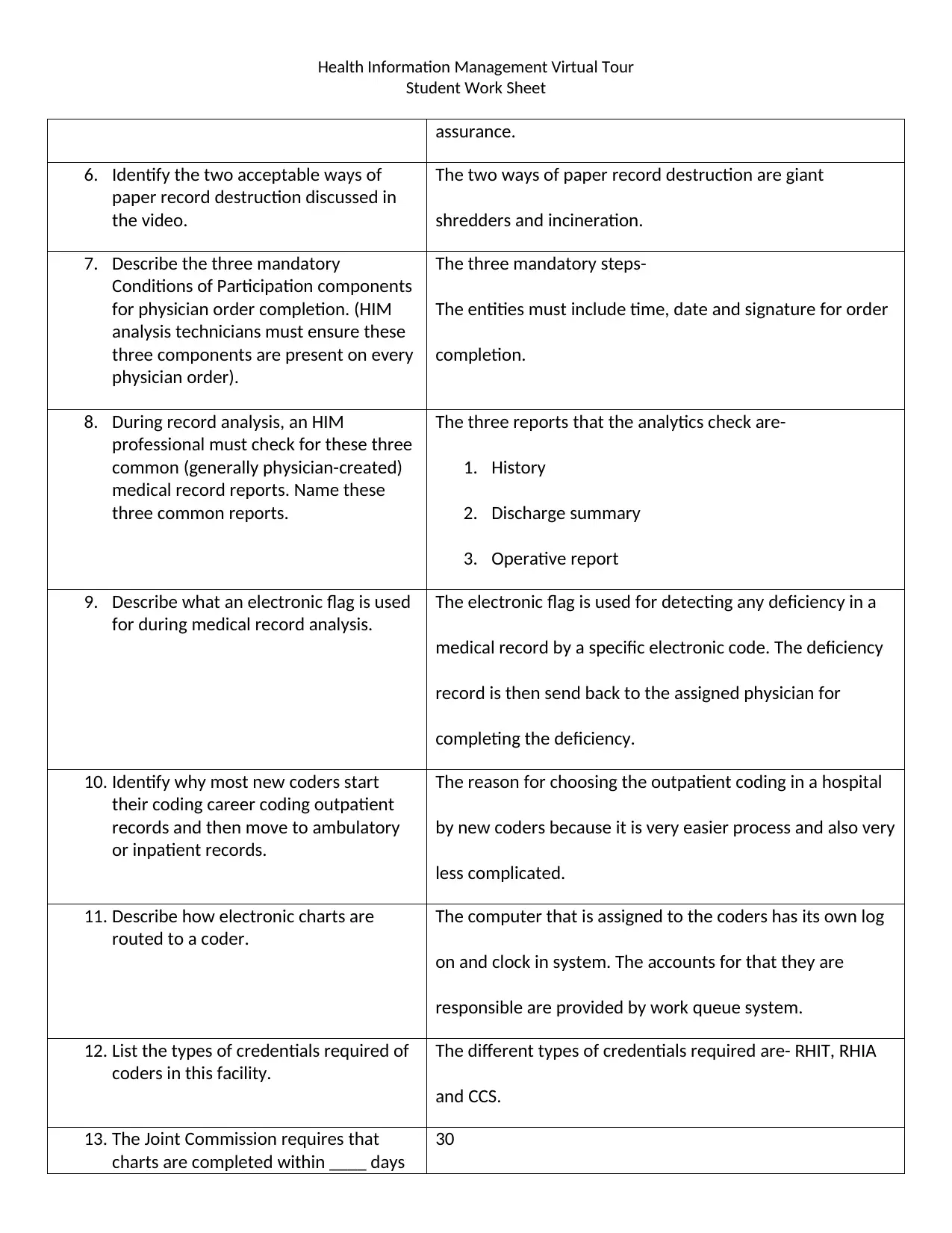
6. Identify the two acceptable ways of
paper record destruction discussed in
the video.
The two ways of paper record destruction are giant
shredders and incineration.
7. Describe the three mandatory
Conditions of Participation components
for physician order completion. (HIM
analysis technicians must ensure these
three components are present on every
physician order).
The three mandatory steps-
The entities must include time, date and signature for order
completion.
8. During record analysis, an HIM
professional must check for these three
common (generally physician-created)
medical record reports. Name these
three common reports.
The three reports that the analytics check are-
1. History
2. Discharge summary
3. Operative report
9. Describe what an electronic flag is used
for during medical record analysis.
The electronic flag is used for detecting any deficiency in a
medical record by a specific electronic code. The deficiency
record is then send back to the assigned physician for
completing the deficiency.
10. Identify why most new coders start
their coding career coding outpatient
records and then move to ambulatory
or inpatient records.
The reason for choosing the outpatient coding in a hospital
by new coders because it is very easier process and also very
less complicated.
11. Describe how electronic charts are
routed to a coder.
The computer that is assigned to the coders has its own log
on and clock in system. The accounts for that they are
responsible are provided by work queue system.
12. List the types of credentials required of
coders in this facility.
The different types of credentials required are- RHIT, RHIA
and CCS.
13. The Joint Commission requires that
charts are completed within ____ days
30
Student Work Sheet
assurance.
6. Identify the two acceptable ways of
paper record destruction discussed in
the video.
The two ways of paper record destruction are giant
shredders and incineration.
7. Describe the three mandatory
Conditions of Participation components
for physician order completion. (HIM
analysis technicians must ensure these
three components are present on every
physician order).
The three mandatory steps-
The entities must include time, date and signature for order
completion.
8. During record analysis, an HIM
professional must check for these three
common (generally physician-created)
medical record reports. Name these
three common reports.
The three reports that the analytics check are-
1. History
2. Discharge summary
3. Operative report
9. Describe what an electronic flag is used
for during medical record analysis.
The electronic flag is used for detecting any deficiency in a
medical record by a specific electronic code. The deficiency
record is then send back to the assigned physician for
completing the deficiency.
10. Identify why most new coders start
their coding career coding outpatient
records and then move to ambulatory
or inpatient records.
The reason for choosing the outpatient coding in a hospital
by new coders because it is very easier process and also very
less complicated.
11. Describe how electronic charts are
routed to a coder.
The computer that is assigned to the coders has its own log
on and clock in system. The accounts for that they are
responsible are provided by work queue system.
12. List the types of credentials required of
coders in this facility.
The different types of credentials required are- RHIT, RHIA
and CCS.
13. The Joint Commission requires that
charts are completed within ____ days
30
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Health Information Management Virtual Tour
Student Work Sheet
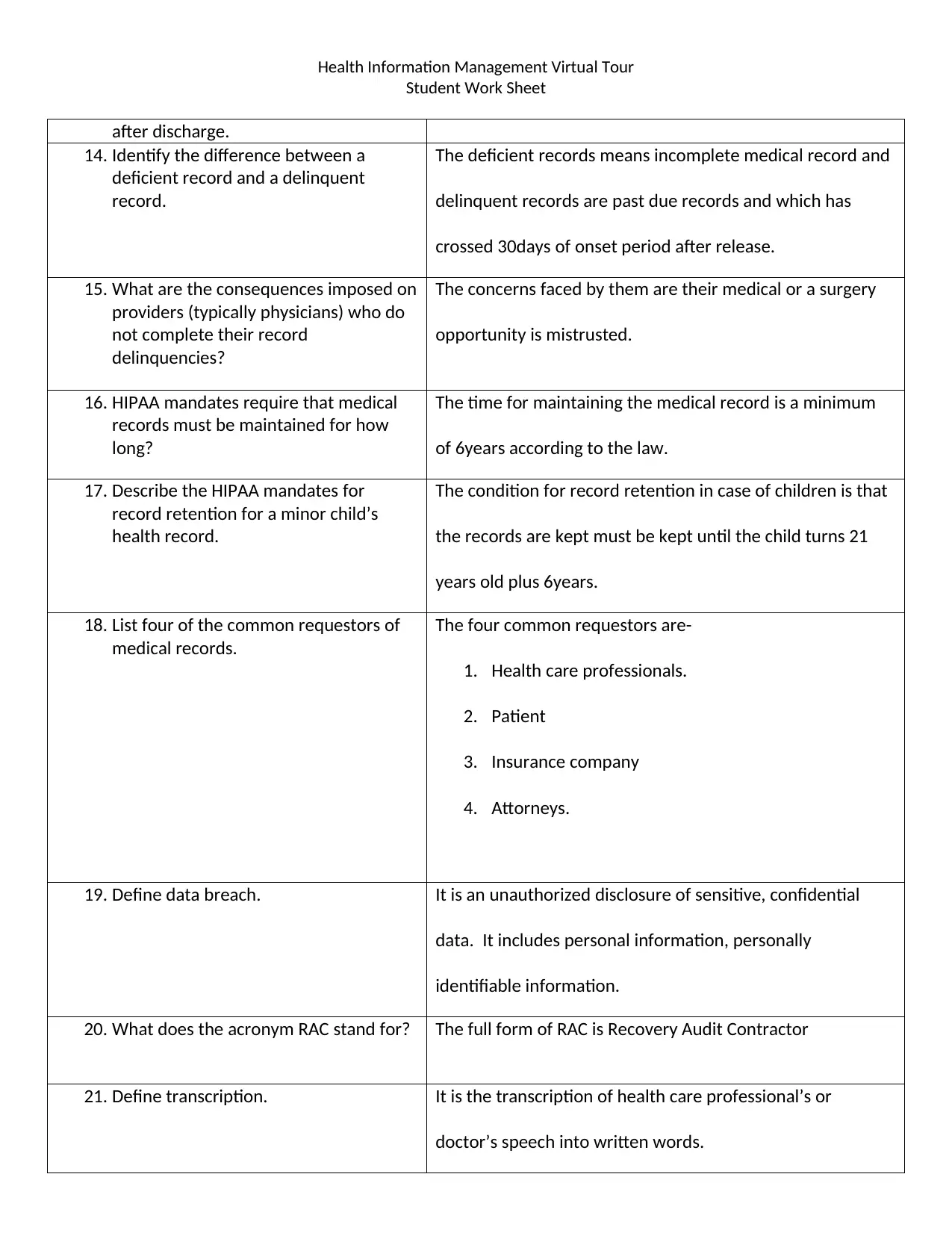
after discharge.
14. Identify the difference between a
deficient record and a delinquent
record.
The deficient records means incomplete medical record and
delinquent records are past due records and which has
crossed 30days of onset period after release.
15. What are the consequences imposed on
providers (typically physicians) who do
not complete their record
delinquencies?
The concerns faced by them are their medical or a surgery
opportunity is mistrusted.
16. HIPAA mandates require that medical
records must be maintained for how
long?
The time for maintaining the medical record is a minimum
of 6years according to the law.
17. Describe the HIPAA mandates for
record retention for a minor child’s
health record.
The condition for record retention in case of children is that
the records are kept must be kept until the child turns 21
years old plus 6years.
18. List four of the common requestors of
medical records.
The four common requestors are-
1. Health care professionals.
2. Patient
3. Insurance company
4. Attorneys.
19. Define data breach. It is an unauthorized disclosure of sensitive, confidential
data. It includes personal information, personally
identifiable information.
20. What does the acronym RAC stand for? The full form of RAC is Recovery Audit Contractor
21. Define transcription. It is the transcription of health care professional’s or
doctor’s speech into written words.
Student Work Sheet
after discharge.
14. Identify the difference between a
deficient record and a delinquent
record.
The deficient records means incomplete medical record and
delinquent records are past due records and which has
crossed 30days of onset period after release.
15. What are the consequences imposed on
providers (typically physicians) who do
not complete their record
delinquencies?
The concerns faced by them are their medical or a surgery
opportunity is mistrusted.
16. HIPAA mandates require that medical
records must be maintained for how
long?
The time for maintaining the medical record is a minimum
of 6years according to the law.
17. Describe the HIPAA mandates for
record retention for a minor child’s
health record.
The condition for record retention in case of children is that
the records are kept must be kept until the child turns 21
years old plus 6years.
18. List four of the common requestors of
medical records.
The four common requestors are-
1. Health care professionals.
2. Patient
3. Insurance company
4. Attorneys.
19. Define data breach. It is an unauthorized disclosure of sensitive, confidential
data. It includes personal information, personally
identifiable information.
20. What does the acronym RAC stand for? The full form of RAC is Recovery Audit Contractor
21. Define transcription. It is the transcription of health care professional’s or
doctor’s speech into written words.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Health Information Management Virtual Tour
Student Work Sheet
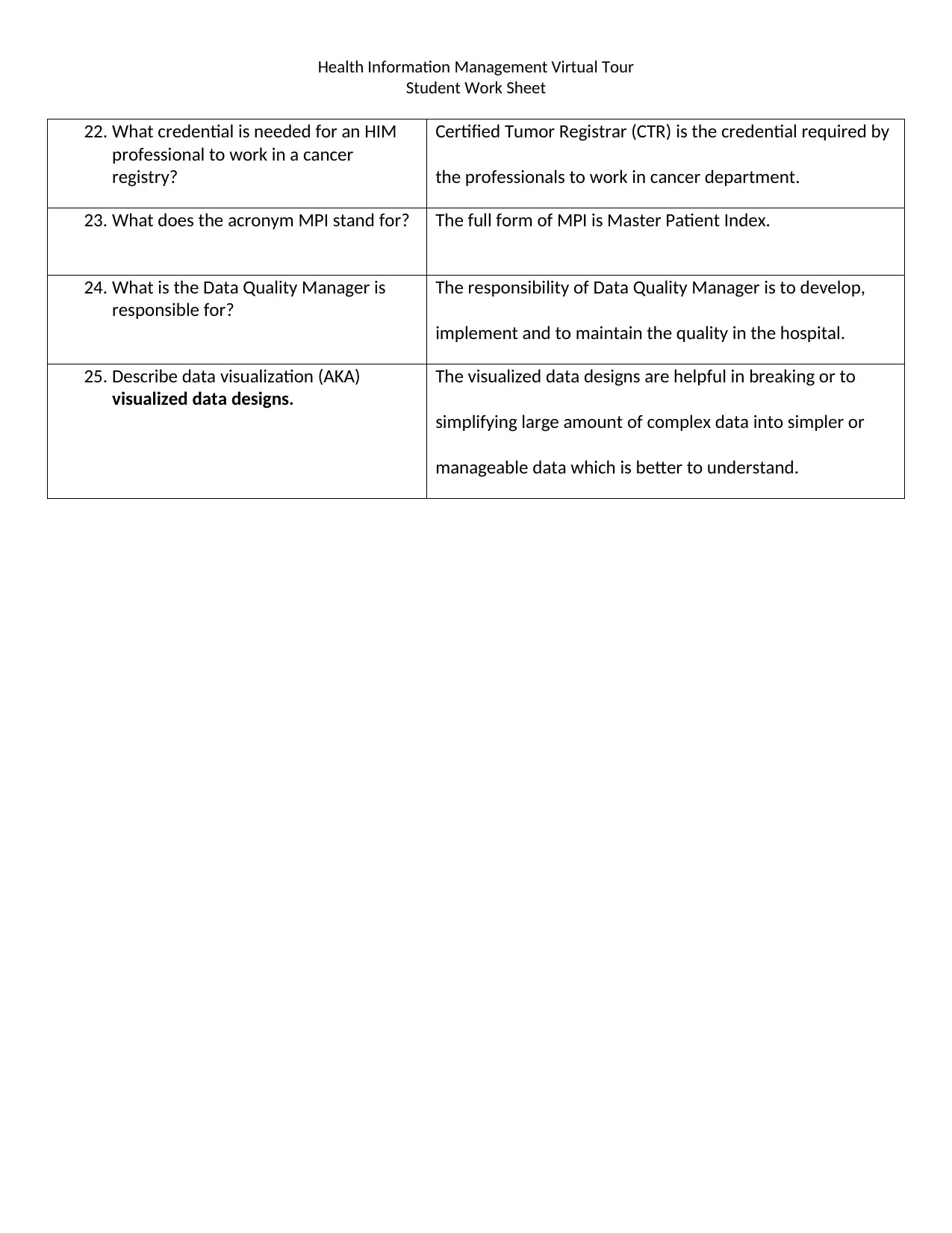
22. What credential is needed for an HIM
professional to work in a cancer
registry?
Certified Tumor Registrar (CTR) is the credential required by
the professionals to work in cancer department.
23. What does the acronym MPI stand for? The full form of MPI is Master Patient Index.
24. What is the Data Quality Manager is
responsible for?
The responsibility of Data Quality Manager is to develop,
implement and to maintain the quality in the hospital.
25. Describe data visualization (AKA)
visualized data designs.
The visualized data designs are helpful in breaking or to
simplifying large amount of complex data into simpler or
manageable data which is better to understand.
Student Work Sheet
22. What credential is needed for an HIM
professional to work in a cancer
registry?
Certified Tumor Registrar (CTR) is the credential required by
the professionals to work in cancer department.
23. What does the acronym MPI stand for? The full form of MPI is Master Patient Index.
24. What is the Data Quality Manager is
responsible for?
The responsibility of Data Quality Manager is to develop,
implement and to maintain the quality in the hospital.
25. Describe data visualization (AKA)
visualized data designs.
The visualized data designs are helpful in breaking or to
simplifying large amount of complex data into simpler or
manageable data which is better to understand.
Health Information Management Virtual Tour
Student Work Sheet
References
AHIMAonDEMAND. (2020). HIM Department Tour - Full Version [Video]. Retrieved from https://www.youtube.com/watch?
v=fI6tuW3-tek&feature=yout
Student Work Sheet
References
AHIMAonDEMAND. (2020). HIM Department Tour - Full Version [Video]. Retrieved from https://www.youtube.com/watch?
v=fI6tuW3-tek&feature=yout
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


