Health Insurance Analysis: Case Study for Raj and Sangeeta, Australia
VerifiedAdded on 2023/06/08
|13
|2999
|396
Case Study
AI Summary
This case study analyzes the health insurance needs of Raj and Sangeeta, an older couple in Australia. The assignment reviews their existing insurance coverage, including term life, funeral, trauma, and income protection. It recommends suitable health insurance products, focusing on hospitality or elective surgery cover and exclusive policies. The study compares health insurance providers Latrobe and BUPA, detailing their benefits, exclusions, and add-on options. It suggests Latrobe as the more suitable option for the couple, given its benefits and the couple's specific needs, including travel & accommodation and GP visits. The assignment also outlines the application process and the principle of utmost good faith in insurance, considering Raj's health condition and age. The document is a student's case study on health insurance with recommendations.
ASSIGNMENT 1 CASE
STUDY 2
STUDY 2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
TASK 1............................................................................................................................................3
Reviewing the existing cover.......................................................................................................3
TASK 2............................................................................................................................................4
Recommendation of suitable health insurance products.............................................................4
TASK 3............................................................................................................................................5
TASK 4............................................................................................................................................8
TASK 5............................................................................................................................................9
a. Steps involved in the application process................................................................................9
TASK 6..........................................................................................................................................10
TASK 7..........................................................................................................................................10
REFERENCES..............................................................................................................................12
Books and Journals....................................................................................................................12
TASK 1............................................................................................................................................3
Reviewing the existing cover.......................................................................................................3
TASK 2............................................................................................................................................4
Recommendation of suitable health insurance products.............................................................4
TASK 3............................................................................................................................................5
TASK 4............................................................................................................................................8
TASK 5............................................................................................................................................9
a. Steps involved in the application process................................................................................9
TASK 6..........................................................................................................................................10
TASK 7..........................................................................................................................................10
REFERENCES..............................................................................................................................12
Books and Journals....................................................................................................................12
TASK 1
Reviewing the existing cover
Term life cover: The couple have taken term life cover of $300000 each which is meant for
covering the insurance coverage until the couple will reached their 80 years. This is means if any
of the couple would die then the beneficent mentioned in the policy would be going to have the
term life cover amount (Biggs, 2020). It is helpful for protecting children or other partner in the
event of the death of the person on whom the beneficent is dependent. Therefore, it would be
recommended to Raj & Sangeeta to retain their term life cover which would provide financial
support to other partner if any of them would die before arriving the age of 80 years. This
insurance cover was suggested to be retained because it has been assumed that the surviving
partner would be the only recipient of the proceedings of the insurance cover.
Funeral cover: The couple is having a funeral cover that should also be retained with
them in order to safeguard the surviving partner from spending their savings or taking on any
additional debts. This cover would be helpful in covering costs associated with the funeral
activities. At this point, the cover provides with the amount necessary for meeting the funeral
requirements and accordingly, there is no requirements for using the hard earned monies out of
savings.
Trauma cover: This cover taken by Raj & Sangeeta is reaching its maturity within a period of
one year and is meant for protecting them from any expenditure that the couple would be going
to made towards the incidence of any serious illness (Bilkey, Baynam and Molster, 2018). So, it
would be better for the couple to cancel out this cover as it has become expensive for them due
to reaching at an older age. The protection that this cover is offering could be availed through
private insurance cover as well that the couple is planning to get now.
Income protection cover: This cover is available with Raj only due to being provided by
their employer and is going to expire at the age of 65 which is about to arrive. Therefore, this
cover should be retained as it is. This is because it would be going to provide income protection
after the retirement on monthly basis to support financially.
Reviewing the existing cover
Term life cover: The couple have taken term life cover of $300000 each which is meant for
covering the insurance coverage until the couple will reached their 80 years. This is means if any
of the couple would die then the beneficent mentioned in the policy would be going to have the
term life cover amount (Biggs, 2020). It is helpful for protecting children or other partner in the
event of the death of the person on whom the beneficent is dependent. Therefore, it would be
recommended to Raj & Sangeeta to retain their term life cover which would provide financial
support to other partner if any of them would die before arriving the age of 80 years. This
insurance cover was suggested to be retained because it has been assumed that the surviving
partner would be the only recipient of the proceedings of the insurance cover.
Funeral cover: The couple is having a funeral cover that should also be retained with
them in order to safeguard the surviving partner from spending their savings or taking on any
additional debts. This cover would be helpful in covering costs associated with the funeral
activities. At this point, the cover provides with the amount necessary for meeting the funeral
requirements and accordingly, there is no requirements for using the hard earned monies out of
savings.
Trauma cover: This cover taken by Raj & Sangeeta is reaching its maturity within a period of
one year and is meant for protecting them from any expenditure that the couple would be going
to made towards the incidence of any serious illness (Bilkey, Baynam and Molster, 2018). So, it
would be better for the couple to cancel out this cover as it has become expensive for them due
to reaching at an older age. The protection that this cover is offering could be availed through
private insurance cover as well that the couple is planning to get now.
Income protection cover: This cover is available with Raj only due to being provided by
their employer and is going to expire at the age of 65 which is about to arrive. Therefore, this
cover should be retained as it is. This is because it would be going to provide income protection
after the retirement on monthly basis to support financially.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
TASK 2
Recommendation of suitable health insurance products
Type of cover recommended: For Raj & Sangeeta, the type of cover that would be recommended
involves the hospitality only or elective surgery cover because it is useful in covering the costs
associated with major medical expenses along with being considered cheaper than
comprehensive health insurance cover (Callander, Fox and Lindsay, 2019). This is policy
provides cover for surgical costs, various tests along with several add on benefits that are
available free of costs and making this type of cover equally advantageous as comprehensive
cover.
Inclusive / exclusive: The Policy that the couple would take is exclusive in order to cover the all
the conditions except those conditions that are specifically excluded from being covered. This
would be helpful for the client (Raj & Sangeeta) in reducing the risk of any condition that could
be covered through exclusive policies over inclusive policies. However, such policies are
comparatively cheaper than that of the inclusive policies because of the unlimited liability of
insurer.
Covering the cost of treatment: With regards to the covering of cost of treatment, there are
several ways in which the costs are covered by health insurance plans. The option of getting
payment as a percentage of treatment cost, or it is limited per treatment is considered to less
attractive against the option of getting maximum amount per policy per annum. Therefore, the
couple should opt for that health insurance cover providing maximum amount per annum under
the policy because the future costs of treatment are not easily predictable, so it better and even a
profitable option for the insured person.
Excess options: Such options are available with health insurance products facilitating insured to
claim for the treatment costs after their claimable amount gets exhausted or used up. Here the
insurer after charging a set excess undertakes to make full payment towards the treatment cost of
insured by keeping their coverage within the maximum limits of the policy (Erlangga and et.al.,
2019). In case of Raj & Sangeeta, this facility would help them in getting the entire amount of
the claim within their policy’s maximum limits after using up the maximum amount of the policy
per annum. For this, Raj & Sangeeta would require to pay for the excess charge on selecting the
“excess option” and in turn, the insurer reduced the amount that is required to be paid towards
Recommendation of suitable health insurance products
Type of cover recommended: For Raj & Sangeeta, the type of cover that would be recommended
involves the hospitality only or elective surgery cover because it is useful in covering the costs
associated with major medical expenses along with being considered cheaper than
comprehensive health insurance cover (Callander, Fox and Lindsay, 2019). This is policy
provides cover for surgical costs, various tests along with several add on benefits that are
available free of costs and making this type of cover equally advantageous as comprehensive
cover.
Inclusive / exclusive: The Policy that the couple would take is exclusive in order to cover the all
the conditions except those conditions that are specifically excluded from being covered. This
would be helpful for the client (Raj & Sangeeta) in reducing the risk of any condition that could
be covered through exclusive policies over inclusive policies. However, such policies are
comparatively cheaper than that of the inclusive policies because of the unlimited liability of
insurer.
Covering the cost of treatment: With regards to the covering of cost of treatment, there are
several ways in which the costs are covered by health insurance plans. The option of getting
payment as a percentage of treatment cost, or it is limited per treatment is considered to less
attractive against the option of getting maximum amount per policy per annum. Therefore, the
couple should opt for that health insurance cover providing maximum amount per annum under
the policy because the future costs of treatment are not easily predictable, so it better and even a
profitable option for the insured person.
Excess options: Such options are available with health insurance products facilitating insured to
claim for the treatment costs after their claimable amount gets exhausted or used up. Here the
insurer after charging a set excess undertakes to make full payment towards the treatment cost of
insured by keeping their coverage within the maximum limits of the policy (Erlangga and et.al.,
2019). In case of Raj & Sangeeta, this facility would help them in getting the entire amount of
the claim within their policy’s maximum limits after using up the maximum amount of the policy
per annum. For this, Raj & Sangeeta would require to pay for the excess charge on selecting the
“excess option” and in turn, the insurer reduced the amount that is required to be paid towards
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
the policy’s premium. There are two types of excess option available to Raj & Sangeeta that is,
fixed % per claim and fixed maximum excess per annum. It would be better for Raj & Sangeeta
to opt for fixed maximum excess per annum. Suppose, if the trauma surgery of Raj would cost
them $50000 and the fixed maximum excess per annum is $2000 per annum. In this case, the
policy would cover the amount of $48000 and the client (Raj & Sangeeta) would be having
limited liability of just $2000.
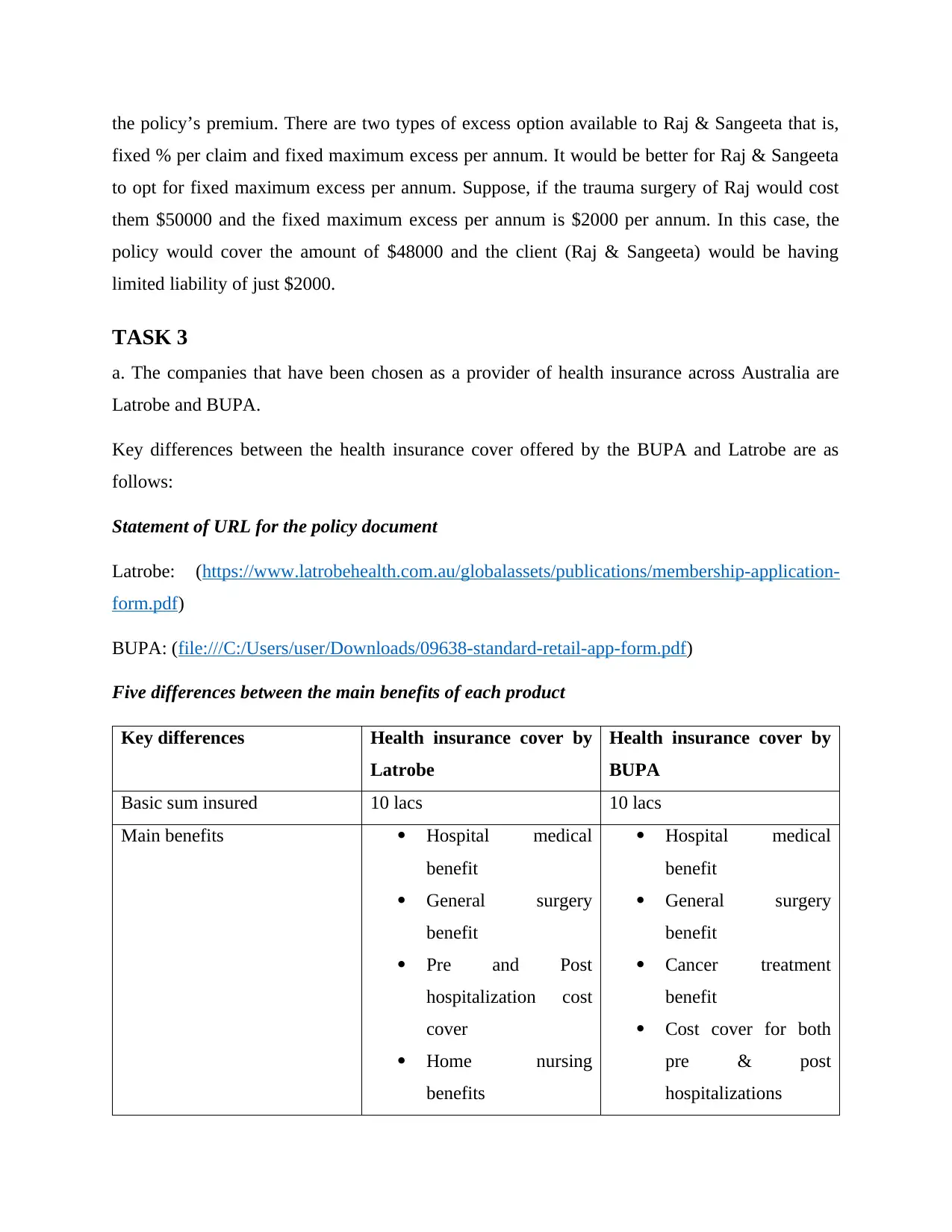
TASK 3
a. The companies that have been chosen as a provider of health insurance across Australia are
Latrobe and BUPA.
Key differences between the health insurance cover offered by the BUPA and Latrobe are as
follows:
Statement of URL for the policy document
Latrobe: (https://www.latrobehealth.com.au/globalassets/publications/membership-application-
form.pdf)
BUPA: (file:///C:/Users/user/Downloads/09638-standard-retail-app-form.pdf)
Five differences between the main benefits of each product
Key differences Health insurance cover by
Latrobe
Health insurance cover by
BUPA
Basic sum insured 10 lacs 10 lacs
Main benefits Hospital medical
benefit
General surgery
benefit
Pre and Post
hospitalization cost
cover
Home nursing
benefits
Hospital medical
benefit
General surgery
benefit
Cancer treatment
benefit
Cost cover for both
pre & post
hospitalizations
fixed % per claim and fixed maximum excess per annum. It would be better for Raj & Sangeeta
to opt for fixed maximum excess per annum. Suppose, if the trauma surgery of Raj would cost
them $50000 and the fixed maximum excess per annum is $2000 per annum. In this case, the
policy would cover the amount of $48000 and the client (Raj & Sangeeta) would be having
limited liability of just $2000.
TASK 3
a. The companies that have been chosen as a provider of health insurance across Australia are
Latrobe and BUPA.
Key differences between the health insurance cover offered by the BUPA and Latrobe are as
follows:
Statement of URL for the policy document
Latrobe: (https://www.latrobehealth.com.au/globalassets/publications/membership-application-
form.pdf)
BUPA: (file:///C:/Users/user/Downloads/09638-standard-retail-app-form.pdf)
Five differences between the main benefits of each product
Key differences Health insurance cover by
Latrobe
Health insurance cover by
BUPA
Basic sum insured 10 lacs 10 lacs
Main benefits Hospital medical
benefit
General surgery
benefit
Pre and Post
hospitalization cost
cover
Home nursing
benefits
Hospital medical
benefit
General surgery
benefit
Cancer treatment
benefit
Cost cover for both
pre & post
hospitalizations
There is no restriction
or sub limits
pertaining to hospital
accommodation.
Here the facility of
group insurance at
comparatively low
premiums is
available.
Premiums are
comparatively lower
in case of Latrobe
than BUPA.
Home nursing benefit
Additional amount at
a fixed rate can be
claimed to the extent
of $30000 for the
occurrence of medical
misadventure.
The cost associated
with hiring nurse for
home nursing care
after the treatment
has been covered
under the plan.
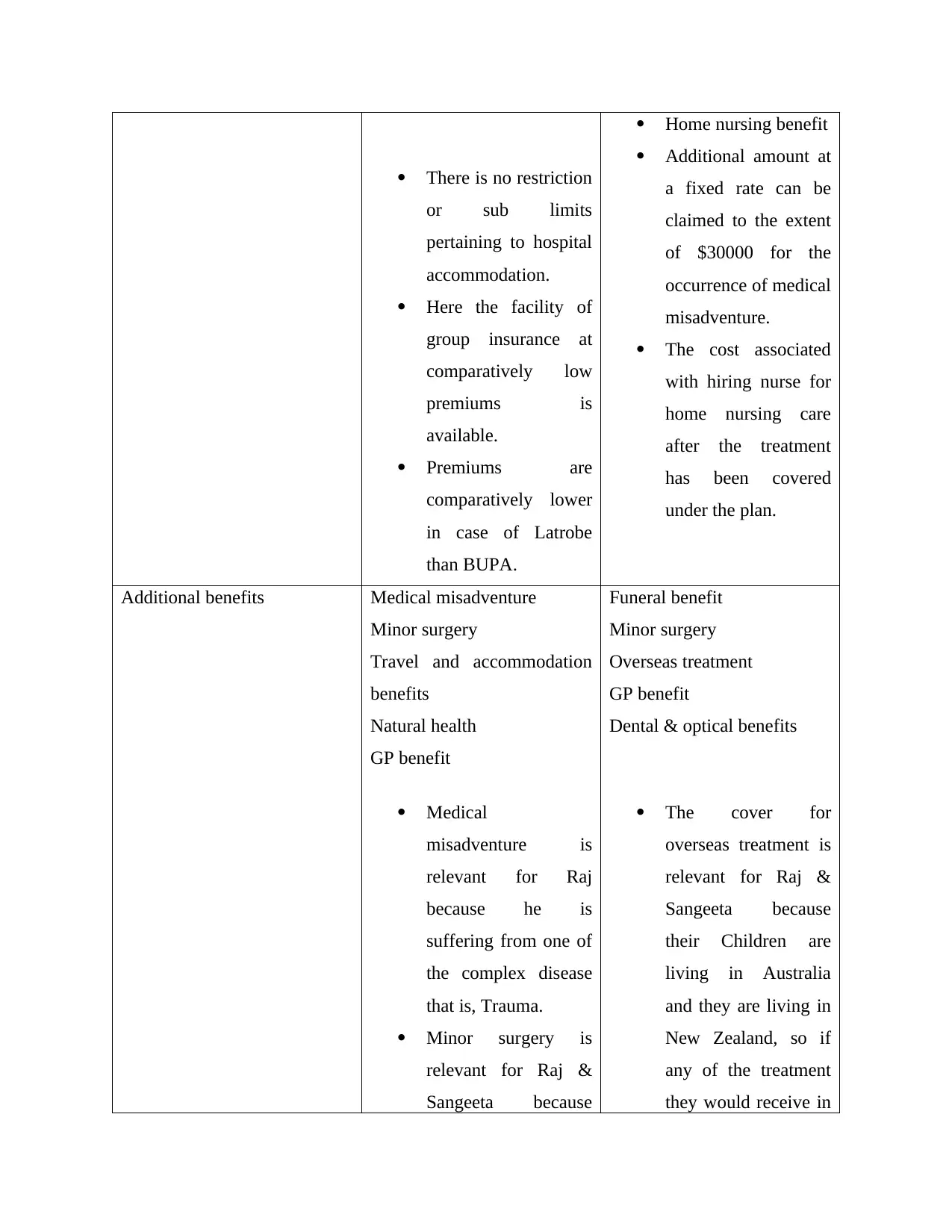
Additional benefits Medical misadventure
Minor surgery
Travel and accommodation
benefits
Natural health
GP benefit
Medical
misadventure is
relevant for Raj
because he is
suffering from one of
the complex disease
that is, Trauma.
Minor surgery is
relevant for Raj &
Sangeeta because
Funeral benefit
Minor surgery
Overseas treatment
GP benefit
Dental & optical benefits
The cover for
overseas treatment is
relevant for Raj &
Sangeeta because
their Children are
living in Australia
and they are living in
New Zealand, so if
any of the treatment
they would receive in
or sub limits
pertaining to hospital
accommodation.
Here the facility of
group insurance at
comparatively low
premiums is
available.
Premiums are
comparatively lower
in case of Latrobe
than BUPA.
Home nursing benefit
Additional amount at
a fixed rate can be
claimed to the extent
of $30000 for the
occurrence of medical
misadventure.
The cost associated
with hiring nurse for
home nursing care
after the treatment
has been covered
under the plan.
Additional benefits Medical misadventure
Minor surgery
Travel and accommodation
benefits
Natural health
GP benefit
Medical
misadventure is
relevant for Raj
because he is
suffering from one of
the complex disease
that is, Trauma.
Minor surgery is
relevant for Raj &
Sangeeta because
Funeral benefit
Minor surgery
Overseas treatment
GP benefit
Dental & optical benefits
The cover for
overseas treatment is
relevant for Raj &
Sangeeta because
their Children are
living in Australia
and they are living in
New Zealand, so if
any of the treatment
they would receive in
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
they are at older age
and the frequent visit
to GP for minor
surgery or treatment
is normal.
Australia can also be
covered under the
plan.
At an older age like
the one from which
Raj & Sangeeta are
passing through, there
usually seems a
random visit for
dental & optical care.
So, the health
insurance cover
should provide for the
same.
Policy exclusions The cover does not provide
for the pre – existing disease
under the health insurance
policy.
All the treatment arising
from or related to pregnancy
are not covered under the
insurance plan offered by
Latrobe (Duckett, Cowgill
and Nemet, 2019).
The cosmetic surgery or
therapies related to it are not
covered under this private
health cover.
There is also no cover
available for pre-existing
disease and surgeries related
to cosmetics.
Health screening is also not
covered under this plan.
The assistance obtained with
regards to infertility or
reproduction is not covered
under the health insurance
product offered by BUPA.
and the frequent visit
to GP for minor
surgery or treatment
is normal.
Australia can also be
covered under the
plan.
At an older age like
the one from which
Raj & Sangeeta are
passing through, there
usually seems a
random visit for
dental & optical care.
So, the health
insurance cover
should provide for the
same.
Policy exclusions The cover does not provide
for the pre – existing disease
under the health insurance
policy.
All the treatment arising
from or related to pregnancy
are not covered under the
insurance plan offered by
Latrobe (Duckett, Cowgill
and Nemet, 2019).
The cosmetic surgery or
therapies related to it are not
covered under this private
health cover.
There is also no cover
available for pre-existing
disease and surgeries related
to cosmetics.
Health screening is also not
covered under this plan.
The assistance obtained with
regards to infertility or
reproduction is not covered
under the health insurance
product offered by BUPA.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
b. Choosing a different Add on benefit
Latrobe: Travel & accommodation benefit
BUPA: Funeral benefit
The importance of these add on benefit to Raj & Sangeeta
The travel and accommodation benefit is important to Raj & Sangeeta because if they would
receive their treatment in Australia where their children are living, then this benefit would be
helpful in covering the cost of travel to the place of treatment in other country or city (Biggs,
2020).
Also, the funeral benefit provides the surviving partner with the facility of claiming the expenses
incurred for the funeral related activities.
TASK 4
From the discussion done in Task 3, the health insurance product offered by Latrobe is suitable
for Raj & Sangeeta. This is because it is providing more number of main benefits than BUPA
along with the facility of group insurance at lower premiums (Mooney, 2020). Further, the
additional benefits include the benefits like treatment related to natural health deterioration, GP
visits, cover for travel & accommodation costs, minor surgeries as well as the medical
misadventure which is possible in case of Raj due to suffering from trauma. The travel &
accommodation is beneficial in covering the additional costs associated with taking oversees
treatment while the GP visits on a frequent basis are normal in case of older people like Raj &
Sangeeta. The exclusions associated with this product is not of greater significance because
exclusion pertaining to pre-existing disease and cosmetic surgeries are common in all plans
while the coverage for pregnancy related costs would definitely not relevant in case of older
people like Raj & Sangeeta.
TASK 5
a. Steps involved in the application process
Usually different insurers have their own specific application process, the following are the key
steps that are necessarily required to be their while applying for the insurance policy (Dineen-
Griffin, Benrimoj and Garcia-Cardenas, 2020).
Latrobe: Travel & accommodation benefit
BUPA: Funeral benefit
The importance of these add on benefit to Raj & Sangeeta
The travel and accommodation benefit is important to Raj & Sangeeta because if they would
receive their treatment in Australia where their children are living, then this benefit would be
helpful in covering the cost of travel to the place of treatment in other country or city (Biggs,
2020).
Also, the funeral benefit provides the surviving partner with the facility of claiming the expenses
incurred for the funeral related activities.
TASK 4
From the discussion done in Task 3, the health insurance product offered by Latrobe is suitable
for Raj & Sangeeta. This is because it is providing more number of main benefits than BUPA
along with the facility of group insurance at lower premiums (Mooney, 2020). Further, the
additional benefits include the benefits like treatment related to natural health deterioration, GP
visits, cover for travel & accommodation costs, minor surgeries as well as the medical
misadventure which is possible in case of Raj due to suffering from trauma. The travel &
accommodation is beneficial in covering the additional costs associated with taking oversees
treatment while the GP visits on a frequent basis are normal in case of older people like Raj &
Sangeeta. The exclusions associated with this product is not of greater significance because
exclusion pertaining to pre-existing disease and cosmetic surgeries are common in all plans
while the coverage for pregnancy related costs would definitely not relevant in case of older
people like Raj & Sangeeta.
TASK 5
a. Steps involved in the application process
Usually different insurers have their own specific application process, the following are the key
steps that are necessarily required to be their while applying for the insurance policy (Dineen-
Griffin, Benrimoj and Garcia-Cardenas, 2020).
Step 1: Completion of the application form: After deciding the type of insurance product that Raj
& Sangeeta are planning to buy, they need to complete the application form that is being
provided by the insurer.
Step 2: Underwriting: Here the assessment & appropriate verification of the applicant is done by
the insurer to determine the risk associated with their client.
Step 3: Acceptance or amended terms: Here the application made by the client for the policy gets
accepted on the determined conditions & rates and the contract of insurance comes into place.
Step 4: Policy issue: After signing & accepting the terms by the clients, the policy is being
issued.
b.
The principle of utmost good faith: According to this principle, it is must for both the insurer as
well as the insured to act in a transparent manner and accordingly disclose all the material facts
and essential information to each other while signing up for the health insurance policy (Bilkey,
Baynam and Molster, 2018).
The purpose of declaration & consent section at the end of the application is to confirm that the
information provided by the client is complete & true. It gives rise to the insurer’s requirement of
getting notified of the changes taking place in the health of insured from the date of application
till the commencement of the policy.
The role of the underwriter includes the assessment of risk that is being posed by the applicants.
Based on the assessment, the applicants are classified as falling in the category of standard risk
sun-standard risk and deferred (Harvey and Campbell, 2020). Accordingly, the rates for the
premiums are determined. In case of Raj & Sangeeta, the private health insurance cover would
be fall in the category of sub-standard risk as they are at older age and Raj is having the risk of
getting suffered from trauma.
Insurer’s duty of disclosure:
The insurer’s duty of disclosure is such that they need to tell client about each and every
term and conditions of their insurance policy. They should provide client with the hard and soft
copy of term and conditions (Pradana, 2021).
& Sangeeta are planning to buy, they need to complete the application form that is being
provided by the insurer.
Step 2: Underwriting: Here the assessment & appropriate verification of the applicant is done by
the insurer to determine the risk associated with their client.
Step 3: Acceptance or amended terms: Here the application made by the client for the policy gets
accepted on the determined conditions & rates and the contract of insurance comes into place.
Step 4: Policy issue: After signing & accepting the terms by the clients, the policy is being
issued.
b.
The principle of utmost good faith: According to this principle, it is must for both the insurer as
well as the insured to act in a transparent manner and accordingly disclose all the material facts
and essential information to each other while signing up for the health insurance policy (Bilkey,
Baynam and Molster, 2018).
The purpose of declaration & consent section at the end of the application is to confirm that the
information provided by the client is complete & true. It gives rise to the insurer’s requirement of
getting notified of the changes taking place in the health of insured from the date of application
till the commencement of the policy.
The role of the underwriter includes the assessment of risk that is being posed by the applicants.
Based on the assessment, the applicants are classified as falling in the category of standard risk
sun-standard risk and deferred (Harvey and Campbell, 2020). Accordingly, the rates for the
premiums are determined. In case of Raj & Sangeeta, the private health insurance cover would
be fall in the category of sub-standard risk as they are at older age and Raj is having the risk of
getting suffered from trauma.
Insurer’s duty of disclosure:
The insurer’s duty of disclosure is such that they need to tell client about each and every
term and conditions of their insurance policy. They should provide client with the hard and soft
copy of term and conditions (Pradana, 2021).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
TASK 6
1.
After analyzing the case of Sangeeta, the best way to claim the health insurance under health
insurance policy is that Sangeeta should seek prior-approval from the health insurer. It is best for
the client who knows whether their medical issue cover under the insurance agreement terms and
condition or not. Under this way, the health insurer of Sangeeta will arrange to pay medical
provider directly which means less than any excess. But in case, if Sangeeta won’t know about
whether their medical issue covered under insurance or not than she can decide to pay the for the
treatment or can wait to know whether it have been done under the public system. Here,
Sangeeta is also required to ask for the referral to a specialist from its GP to file online form of
health insurance (Hick and Murphy, 2021). This helps the patient to claim the cost of treatment
from insurance company.
2.
The three insurer’s requirement that have to be follow by Sangeeta to settle the claim are as
follows:
A completed pre-approval claim form.
A copy of referral letter as well as the clinical notes of Sangeeta’s General Practitioner
(GP).
An estimate for cost of Sangeeta’s hip surgery.
TASK 7
1.
In the situation when the health policy of insurance was lapsed due to the non-payment of due
for more than 3 months and insured have adviser, in that case, insurance company make the
adviser aware of the non-payment and potential lapses (Unruh and et.al., 2022). The adviser
would initially try to contact insured to resolve this situation. They should also contact and hire
advocate to have the policy reinstated and the arrears paid.
2.
1.
After analyzing the case of Sangeeta, the best way to claim the health insurance under health
insurance policy is that Sangeeta should seek prior-approval from the health insurer. It is best for
the client who knows whether their medical issue cover under the insurance agreement terms and
condition or not. Under this way, the health insurer of Sangeeta will arrange to pay medical
provider directly which means less than any excess. But in case, if Sangeeta won’t know about
whether their medical issue covered under insurance or not than she can decide to pay the for the
treatment or can wait to know whether it have been done under the public system. Here,
Sangeeta is also required to ask for the referral to a specialist from its GP to file online form of
health insurance (Hick and Murphy, 2021). This helps the patient to claim the cost of treatment
from insurance company.
2.
The three insurer’s requirement that have to be follow by Sangeeta to settle the claim are as
follows:
A completed pre-approval claim form.
A copy of referral letter as well as the clinical notes of Sangeeta’s General Practitioner
(GP).
An estimate for cost of Sangeeta’s hip surgery.
TASK 7
1.
In the situation when the health policy of insurance was lapsed due to the non-payment of due
for more than 3 months and insured have adviser, in that case, insurance company make the
adviser aware of the non-payment and potential lapses (Unruh and et.al., 2022). The adviser
would initially try to contact insured to resolve this situation. They should also contact and hire
advocate to have the policy reinstated and the arrears paid.
2.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The risk arising from this situation is as follows:
Cancellation of policy.
The cover will not further restart until all missed payment was done by client.
Cancellation of policy.
The cover will not further restart until all missed payment was done by client.
REFERENCES
Books and Journals
Biggs, A., 2020. COVID-19 and private health insurance.
Bilkey, G. A., Baynam, G. and Molster, C., 2018. Changes to the employers' use of genetic
information and non-discrimination for health insurance in the USA: implications for
Australians. Frontiers in Public Health. 6. p.183.
Callander, E. J., Fox, H. and Lindsay, D., 2019. Out-of-pocket healthcare expenditure in
Australia: trends, inequalities and the impact on household living standards in a high-
income country with a universal health care system. Health economics review. 9(1). pp.1-
8.
Dineen-Griffin, S., Benrimoj, S. I. and Garcia-Cardenas, V., 2020. Primary health care policy
and vision for community pharmacy and pharmacists in Australia. Pharmacy Practice
(Granada). 18(2).
Duckett, S., Cowgill, M. and Nemet, K., 2019. Saving Private Health 2: Making private health
insurance viable.
Erlangga, D. and et.al., 2019. The impact of public health insurance on health care utilisation,
financial protection and health status in low-and middle-income countries: A systematic
review. PloS one. 14(8). p.e0219731.
Harvey, D. R. and Campbell, R., 2020. Private eyes…, hips, etc: Health insurance benefits
during the Covid crisis.
Hick, R. and Murphy, M. P., 2021. Common shock, different paths? Comparing social policy
responses to COVID‐19 in the UK and Ireland. Social Policy & Administration. 55(2).
pp.312-325.
Mooney, G., 2020. Economics and Australian health policy. Routledge.
Pradana, A. W., 2021. Policyholder protection for insurance companies with default claims:
comparative analysis in Indonesia and the UK. Borobudur Law Review. 3(1). pp.1-15.
Books and Journals
Biggs, A., 2020. COVID-19 and private health insurance.
Bilkey, G. A., Baynam, G. and Molster, C., 2018. Changes to the employers' use of genetic
information and non-discrimination for health insurance in the USA: implications for
Australians. Frontiers in Public Health. 6. p.183.
Callander, E. J., Fox, H. and Lindsay, D., 2019. Out-of-pocket healthcare expenditure in
Australia: trends, inequalities and the impact on household living standards in a high-
income country with a universal health care system. Health economics review. 9(1). pp.1-
8.
Dineen-Griffin, S., Benrimoj, S. I. and Garcia-Cardenas, V., 2020. Primary health care policy
and vision for community pharmacy and pharmacists in Australia. Pharmacy Practice
(Granada). 18(2).
Duckett, S., Cowgill, M. and Nemet, K., 2019. Saving Private Health 2: Making private health
insurance viable.
Erlangga, D. and et.al., 2019. The impact of public health insurance on health care utilisation,
financial protection and health status in low-and middle-income countries: A systematic
review. PloS one. 14(8). p.e0219731.
Harvey, D. R. and Campbell, R., 2020. Private eyes…, hips, etc: Health insurance benefits
during the Covid crisis.
Hick, R. and Murphy, M. P., 2021. Common shock, different paths? Comparing social policy
responses to COVID‐19 in the UK and Ireland. Social Policy & Administration. 55(2).
pp.312-325.
Mooney, G., 2020. Economics and Australian health policy. Routledge.
Pradana, A. W., 2021. Policyholder protection for insurance companies with default claims:
comparative analysis in Indonesia and the UK. Borobudur Law Review. 3(1). pp.1-15.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.