Health Policy Analysis of the Bonded Medical Program (BMP) - 401363
VerifiedAdded on 2022/09/11
|6
|1370
|27
Report
AI Summary
This report provides an in-depth analysis of the Bonded Medical Program (BMP), a health policy implemented in Australia to encourage healthcare professionals to work in rural and remote areas. The report examines the risks associated with the BMP, including the potential for poor health outcomes among providers and patients due to inadequate living conditions and limited resources. A risk analysis matrix is utilized to assess the impact and likelihood of these risks, along with proposed mitigation strategies such as stipends, funding, and subsidized medical facilities. The analysis further explores the BMP's impact on the overall healthcare system and vulnerable populations, highlighting potential violations of universal health coverage principles. The report concludes by emphasizing the need for government incentives and funding to address these risks and improve healthcare access and quality in rural and remote regions. References from the Department of Health and other scholarly articles are included to support the analysis.

Running head: HEALTH POLICY ANALYSIS: BONDED MEDICAL PROGRAM
HEALTH POLICY ANALYSIS: BONDED MEDICAL PROGRAM
Name of the Student:
Name of the University:
Author note:
HEALTH POLICY ANALYSIS: BONDED MEDICAL PROGRAM
Name of the Student:
Name of the University:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1HEALTH POLICY ANALYSIS: BONDED MEDICAL PROGRAM
Introduction
The Bonded Medical Program (BMP) was established for the purpose of encouraging
future healthcare professionals to work in regions of limited public health workforce capacity,
such as in rural and remote locations of Australia (Department of Health, 2020). The following
paper will briefly expound upon the risks associated with the BMP using a risk analysis matrix as
well as its potential impacts on the overall healthcare system and possible mitigations for the
same.
Discussion
Bonded Medical Program
The Bonded Medical Program (BMP), was established by the Department of Health
(2020) in the year 2001, with the aim of increasing the influx of qualified healthcare
professionals to places of healthcare workforce shortage, namely rural and remote locations of
Australia. As per this scheme, the government will arrange for a Commonwealth Supported
Place (CSP) at a reputed medical or healthcare university in Australia to interested candidates. A
CSP is a special educational place at higher medical education providers or universities where
the government will subsidize student’s educational costs by providing coverage for a part of the
same. In return for this subsidy, students are obliged to commit to a 3 to 18 year period of service
across remote or rural areas. These include: a Bonded Medical Place (BMP) (districts where
there is a shortage of workforce where students must work for a period equal to the time of their
course) and Medical Rural Bonded Scholarship (MRBS) (Remote or rural areas with a standard
service period of 3 to 6 years). As per recent alterations in policy, the government will offer no
Introduction
The Bonded Medical Program (BMP) was established for the purpose of encouraging
future healthcare professionals to work in regions of limited public health workforce capacity,
such as in rural and remote locations of Australia (Department of Health, 2020). The following
paper will briefly expound upon the risks associated with the BMP using a risk analysis matrix as
well as its potential impacts on the overall healthcare system and possible mitigations for the
same.
Discussion
Bonded Medical Program
The Bonded Medical Program (BMP), was established by the Department of Health
(2020) in the year 2001, with the aim of increasing the influx of qualified healthcare
professionals to places of healthcare workforce shortage, namely rural and remote locations of
Australia. As per this scheme, the government will arrange for a Commonwealth Supported
Place (CSP) at a reputed medical or healthcare university in Australia to interested candidates. A
CSP is a special educational place at higher medical education providers or universities where
the government will subsidize student’s educational costs by providing coverage for a part of the
same. In return for this subsidy, students are obliged to commit to a 3 to 18 year period of service
across remote or rural areas. These include: a Bonded Medical Place (BMP) (districts where
there is a shortage of workforce where students must work for a period equal to the time of their
course) and Medical Rural Bonded Scholarship (MRBS) (Remote or rural areas with a standard
service period of 3 to 6 years). As per recent alterations in policy, the government will offer no
2HEALTH POLICY ANALYSIS: BONDED MEDICAL PROGRAM
form of scholarship for this service period except for the educational subsidy in the form of a
CSP (Department of Health, 2020).
The absence of a scholarship for healthcare professionals opting to work in remote and
rural regions is a major cause of criticism of the BMP. These have been expounded upon in the
following sections.
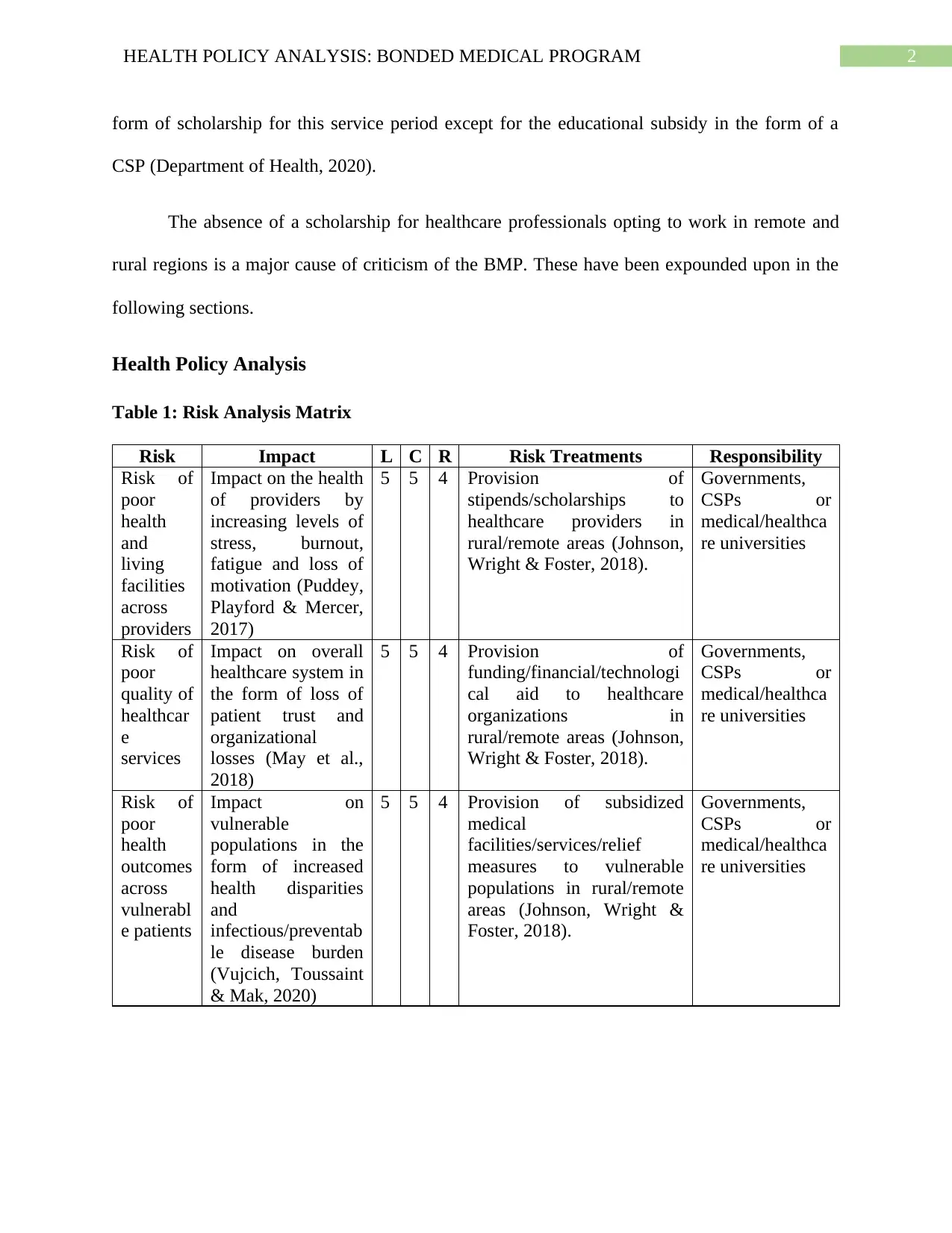
Health Policy Analysis
Table 1: Risk Analysis Matrix
Risk Impact L C R Risk Treatments Responsibility
Risk of
poor
health
and
living
facilities
across
providers
Impact on the health
of providers by
increasing levels of
stress, burnout,
fatigue and loss of
motivation (Puddey,
Playford & Mercer,
2017)
5 5 4 Provision of
stipends/scholarships to
healthcare providers in
rural/remote areas (Johnson,
Wright & Foster, 2018).
Governments,
CSPs or
medical/healthca
re universities
Risk of
poor
quality of
healthcar
e
services
Impact on overall
healthcare system in
the form of loss of
patient trust and
organizational
losses (May et al.,
2018)
5 5 4 Provision of
funding/financial/technologi
cal aid to healthcare
organizations in
rural/remote areas (Johnson,
Wright & Foster, 2018).
Governments,
CSPs or
medical/healthca
re universities
Risk of
poor
health
outcomes
across
vulnerabl
e patients
Impact on
vulnerable
populations in the
form of increased
health disparities
and
infectious/preventab
le disease burden
(Vujcich, Toussaint
& Mak, 2020)
5 5 4 Provision of subsidized
medical
facilities/services/relief
measures to vulnerable
populations in rural/remote
areas (Johnson, Wright &
Foster, 2018).
Governments,
CSPs or
medical/healthca
re universities
form of scholarship for this service period except for the educational subsidy in the form of a
CSP (Department of Health, 2020).
The absence of a scholarship for healthcare professionals opting to work in remote and
rural regions is a major cause of criticism of the BMP. These have been expounded upon in the
following sections.
Health Policy Analysis
Table 1: Risk Analysis Matrix
Risk Impact L C R Risk Treatments Responsibility
Risk of
poor
health
and
living
facilities
across
providers
Impact on the health
of providers by
increasing levels of
stress, burnout,
fatigue and loss of
motivation (Puddey,
Playford & Mercer,
2017)
5 5 4 Provision of
stipends/scholarships to
healthcare providers in
rural/remote areas (Johnson,
Wright & Foster, 2018).
Governments,
CSPs or
medical/healthca
re universities
Risk of
poor
quality of
healthcar
e
services
Impact on overall
healthcare system in
the form of loss of
patient trust and
organizational
losses (May et al.,
2018)
5 5 4 Provision of
funding/financial/technologi
cal aid to healthcare
organizations in
rural/remote areas (Johnson,
Wright & Foster, 2018).
Governments,
CSPs or
medical/healthca
re universities
Risk of
poor
health
outcomes
across
vulnerabl
e patients
Impact on
vulnerable
populations in the
form of increased
health disparities
and
infectious/preventab
le disease burden
(Vujcich, Toussaint
& Mak, 2020)
5 5 4 Provision of subsidized
medical
facilities/services/relief
measures to vulnerable
populations in rural/remote
areas (Johnson, Wright &
Foster, 2018).
Governments,
CSPs or
medical/healthca
re universities
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3HEALTH POLICY ANALYSIS: BONDED MEDICAL PROGRAM
Impact on Providers and Patients
Rural and remote regions are scare in resources required for maintaining basic standards
of living such as food, water, medications, hygiene, sanitation and even housing. Without any
scholarships or basic funding or relief measures by the BMP, it will be difficult for healthcare
providers stationed in these places to make arrangements for this facilities. This in turn will
contribute to poor health and increased levels of stress, fatigue, burnout and loss of motivation in
healthcare providers which will pave the way for deliverance of poor quality services to patients
and resultant poor patient health outcomes (Puddey, Playford & Mercer, 2017) (Table 1).
Impact on Health System
Rural and remote areas are generally impoverished and the scarcity and difficulty to
obtain basic technology, medications and care facilities will contribute to deliverance of poor
quality of healthcare services. Such problems maybe aggravated by the lack of scholarship in a
BMP. This in turn, will contribute to poor health outcomes in patients, increased medical errors,
loss of trust and financial losses in the healthcare system (May et al., 2018) (Table 1).
Impact on Vulnerable Populations
The impoverished conditions of rural and remote areas are key contributors to healthcare
disparities in populations living in these regions. The lack of funding by the BMP and resulting
poor quality of services delivered as mentioned above are likely to impact these vulnerable
populations in the form of increased healthcare disparities and disease burden of infectious
diseases (Vujcich, Toussaint & Mak, 2020) (Table 1).
Risk Management Plan
Governments and CSPs can provide of stipends or scholarships to improve living
conditions of healthcare providers in rural/remote areas.
Impact on Providers and Patients
Rural and remote regions are scare in resources required for maintaining basic standards
of living such as food, water, medications, hygiene, sanitation and even housing. Without any
scholarships or basic funding or relief measures by the BMP, it will be difficult for healthcare
providers stationed in these places to make arrangements for this facilities. This in turn will
contribute to poor health and increased levels of stress, fatigue, burnout and loss of motivation in
healthcare providers which will pave the way for deliverance of poor quality services to patients
and resultant poor patient health outcomes (Puddey, Playford & Mercer, 2017) (Table 1).
Impact on Health System
Rural and remote areas are generally impoverished and the scarcity and difficulty to
obtain basic technology, medications and care facilities will contribute to deliverance of poor
quality of healthcare services. Such problems maybe aggravated by the lack of scholarship in a
BMP. This in turn, will contribute to poor health outcomes in patients, increased medical errors,
loss of trust and financial losses in the healthcare system (May et al., 2018) (Table 1).
Impact on Vulnerable Populations
The impoverished conditions of rural and remote areas are key contributors to healthcare
disparities in populations living in these regions. The lack of funding by the BMP and resulting
poor quality of services delivered as mentioned above are likely to impact these vulnerable
populations in the form of increased healthcare disparities and disease burden of infectious
diseases (Vujcich, Toussaint & Mak, 2020) (Table 1).
Risk Management Plan
Governments and CSPs can provide of stipends or scholarships to improve living
conditions of healthcare providers in rural/remote areas.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4HEALTH POLICY ANALYSIS: BONDED MEDICAL PROGRAM
Governments and CSPs can provide of funding or financial or technological aid to
improve the quality of the healthcare system in rural/remote areas
Governments and CSPs can provide subsidized medical facilities and services/relief
measures to reduce healthcare disparities in vulnerable populations in rural/remote areas
(Johnson, Wright & Foster, 2018).
Universal Healthcare
By arranging for increased healthcare providers in rural areas, the BMP adheres to the
universal health coverage principle of ensuring accessibility to equitable healthcare
services for rural and remote populations.
By not providing sufficient funding and scholarships, the BMP violates universal health
coverage principles of the need to provide optimum quality healthcare services and
protection of individuals from financial harms (World Health Organization, 2020).
Conclusion
The rural and remote regions of Australia are not just limited in healthcare services but
also in basic standards of living, notwithstanding high rates of disease burden. To conclude, it is
expected that the government provides some form of incentives or funding to healthcare
professionals and organizations residing in rural and remote regions for the purpose of mitigation
of such risks.
Governments and CSPs can provide of funding or financial or technological aid to
improve the quality of the healthcare system in rural/remote areas
Governments and CSPs can provide subsidized medical facilities and services/relief
measures to reduce healthcare disparities in vulnerable populations in rural/remote areas
(Johnson, Wright & Foster, 2018).
Universal Healthcare
By arranging for increased healthcare providers in rural areas, the BMP adheres to the
universal health coverage principle of ensuring accessibility to equitable healthcare
services for rural and remote populations.
By not providing sufficient funding and scholarships, the BMP violates universal health
coverage principles of the need to provide optimum quality healthcare services and
protection of individuals from financial harms (World Health Organization, 2020).
Conclusion
The rural and remote regions of Australia are not just limited in healthcare services but
also in basic standards of living, notwithstanding high rates of disease burden. To conclude, it is
expected that the government provides some form of incentives or funding to healthcare
professionals and organizations residing in rural and remote regions for the purpose of mitigation
of such risks.
5HEALTH POLICY ANALYSIS: BONDED MEDICAL PROGRAM
References
Department of Health. (2020). Department of Health | The Bonded Medical Program New
Arrangement. Retrieved 1 April 2020, from
https://www1.health.gov.au/internet/main/publishing.nsf/Content/reformed-bonded-
programs.
Johnson, G. E., Wright, F. C., & Foster, K. (2018). The impact of rural outreach programs on
medical students’ future rural intentions and working locations: a systematic
review. BMC medical education, 18(1), 196.
May, J., Walker, J., McGrail, M., & Rolley, F. (2018). It’s more than money: policy options to
secure medical specialist workforce for regional centres. Australian Health
Review, 41(6), 698-706.
Puddey, I. B., Playford, D. E., & Mercer, A. (2017). Impact of medical student origins on the
likelihood of ultimately practicing in areas of low vs high socio-economic status. BMC
medical education, 17(1), 1.
Vujcich, D. L., Toussaint, S., & Mak, D. B. (2020). “[It’s] more than just medicine”: The value
and sustainability of mandatory, non-clinical, short-term rural placements in a Western
Australian medical school. Medical Teacher, 1-7.
World Health Organization. (2020). What is universal coverage?. Retrieved 1 April 2020, from
https://www.who.int/health_financing/universal_coverage_definition/en/.
References
Department of Health. (2020). Department of Health | The Bonded Medical Program New
Arrangement. Retrieved 1 April 2020, from
https://www1.health.gov.au/internet/main/publishing.nsf/Content/reformed-bonded-
programs.
Johnson, G. E., Wright, F. C., & Foster, K. (2018). The impact of rural outreach programs on
medical students’ future rural intentions and working locations: a systematic
review. BMC medical education, 18(1), 196.
May, J., Walker, J., McGrail, M., & Rolley, F. (2018). It’s more than money: policy options to
secure medical specialist workforce for regional centres. Australian Health
Review, 41(6), 698-706.
Puddey, I. B., Playford, D. E., & Mercer, A. (2017). Impact of medical student origins on the
likelihood of ultimately practicing in areas of low vs high socio-economic status. BMC
medical education, 17(1), 1.
Vujcich, D. L., Toussaint, S., & Mak, D. B. (2020). “[It’s] more than just medicine”: The value
and sustainability of mandatory, non-clinical, short-term rural placements in a Western
Australian medical school. Medical Teacher, 1-7.
World Health Organization. (2020). What is universal coverage?. Retrieved 1 April 2020, from
https://www.who.int/health_financing/universal_coverage_definition/en/.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





