Health & Social Care: Partnership Working - NHS Foundation Trust
VerifiedAdded on 2024/04/25
|16
|5460
|133
Report
AI Summary
This report provides a comprehensive analysis of partnership working within health and social care settings, emphasizing its philosophical underpinnings, practical implementation, and potential outcomes. It begins by elucidating the core philosophies of partnership, including ethics, beneficence, autonomy, and respect, highlighting their importance in fostering effective collaborative relationships. The report evaluates partnership relationships at various levels, from interpersonal interactions between care providers and service users to strategic alliances between healthcare facilities and local authorities. It also analyzes models of partnership working, reviews relevant legislation and organizational practices, and explains how differences in working practices can affect collaboration. Furthermore, the report assesses potential barriers to partnership working and devises strategies to improve outcomes for service users, professionals, and organizations, using the case scenario of the Mid Staffordshire NHS Foundation Trust to illustrate the critical need for effective partnership approaches in healthcare.

HEALTH AND SOCIAL CARE WORKING IN PARTNERSHIP
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Table of Contents
Introduction................................................................................................................................3
LO 1: Understand partnership philosophies and relationships in “health and social care”
services.......................................................................................................................................3
1.1 Explain the philosophy of working in partnership in “health and social care”....................3
1.2 Evaluate partnership relationships within “health and social care” services.......................6
LO 2: Understand how to promote positive partnership working with users of services,
professionals and organizations in “health and social care” services........................................7
2.1 Analyze models of partnership working across the “health and social care” sector............7
2.2 Review current legislation and organizational practices and policies for partnership
working in “health and social care”...........................................................................................9
2.3 Explain how differences in working practices and policies affect collaborative working 10
LO 3: Be able to evaluate the outcomes of partnership working for users of services,
professionals and organizations in “health and social care” services......................................11
3.1 Evaluate possible outcomes of partnership working for users of services, professionals
and organizations.....................................................................................................................11
3.2 Analyze the potential barriers to partnership working in “health and social care” services.
..................................................................................................................................................12
3.3 Devise strategies to improve outcomes for partnership working in “health and social care”
services.....................................................................................................................................13
Conclusion................................................................................................................................14
Reference List..........................................................................................................................15
Introduction................................................................................................................................3
LO 1: Understand partnership philosophies and relationships in “health and social care”
services.......................................................................................................................................3
1.1 Explain the philosophy of working in partnership in “health and social care”....................3
1.2 Evaluate partnership relationships within “health and social care” services.......................6
LO 2: Understand how to promote positive partnership working with users of services,
professionals and organizations in “health and social care” services........................................7
2.1 Analyze models of partnership working across the “health and social care” sector............7
2.2 Review current legislation and organizational practices and policies for partnership
working in “health and social care”...........................................................................................9
2.3 Explain how differences in working practices and policies affect collaborative working 10
LO 3: Be able to evaluate the outcomes of partnership working for users of services,
professionals and organizations in “health and social care” services......................................11
3.1 Evaluate possible outcomes of partnership working for users of services, professionals
and organizations.....................................................................................................................11
3.2 Analyze the potential barriers to partnership working in “health and social care” services.
..................................................................................................................................................12
3.3 Devise strategies to improve outcomes for partnership working in “health and social care”
services.....................................................................................................................................13
Conclusion................................................................................................................................14
Reference List..........................................................................................................................15
Introduction
In “health and social care practice”, it is vital for the “health and social care” workers to
develop a healthy work environment, which can significantly promote the health outcomes of
the service care users. In this context, one of the key purposes of the “health and social care”
worker” is to offer satisfactory services to the clients and promote their overall wellbeing.
However, it is not possible for a care professional to promote the overall wellbeing of the
service users. Thus, it is important to promote the concept of working with others, like a team
in the “health and social care” setting’. In healthcare settings, the multidisciplinary care team
is common, where professionals from different disciplinary services work together to address
holistic needs of the patient as well as to improve the holistic wellbeing of the care service
users (Munn-Giddings and Winter, 2013). In the current assignment, the focus would be to
investigate the significance of “working in partnership’ in the ‘“health and social care”
settings. In this context, the assignment would help to know “partnership philosophies and
relationships” in “health and social care” services”; in the next section, the assignment would
focus on the ways of promoting “positive partnership working” with the clients, professionals
as well as “health and social care” service facilities or organizations. Finally, the assignment
would also help to evaluate the outcomes of partnership working for the service users,
professionals as well as organizations in “health and social care” services. In order to
demonstrate the above mentioned facts, the case scenario of the Mid Staffordshire NHS
Foundation Trust would be focused.
LO 1: Understand partnership philosophies and relationships in “health and social
care” services
1.1 Explain the philosophy of working in partnership in “health and social care”
In the case study of the Mid Staffordshire NHS Foundation Trust, the failure to develop and
provide a quality standard services have been highlighted, in several cases, which indicated
that patient’s voice have been neglected by the care authorities continuously, leading to a
poor care outcome. On the other hand, it has also been noticed that the management did not
attempted to look into these matters or did not listen to issues raised by staffs regarding the
improvement of facilities and services in the “health and social care” settings”. As a result,
the NHS associated trust is losing public trust due to low level of practice. A lack of
In “health and social care practice”, it is vital for the “health and social care” workers to
develop a healthy work environment, which can significantly promote the health outcomes of
the service care users. In this context, one of the key purposes of the “health and social care”
worker” is to offer satisfactory services to the clients and promote their overall wellbeing.
However, it is not possible for a care professional to promote the overall wellbeing of the
service users. Thus, it is important to promote the concept of working with others, like a team
in the “health and social care” setting’. In healthcare settings, the multidisciplinary care team
is common, where professionals from different disciplinary services work together to address
holistic needs of the patient as well as to improve the holistic wellbeing of the care service
users (Munn-Giddings and Winter, 2013). In the current assignment, the focus would be to
investigate the significance of “working in partnership’ in the ‘“health and social care”
settings. In this context, the assignment would help to know “partnership philosophies and
relationships” in “health and social care” services”; in the next section, the assignment would
focus on the ways of promoting “positive partnership working” with the clients, professionals
as well as “health and social care” service facilities or organizations. Finally, the assignment
would also help to evaluate the outcomes of partnership working for the service users,
professionals as well as organizations in “health and social care” services. In order to
demonstrate the above mentioned facts, the case scenario of the Mid Staffordshire NHS
Foundation Trust would be focused.
LO 1: Understand partnership philosophies and relationships in “health and social
care” services
1.1 Explain the philosophy of working in partnership in “health and social care”
In the case study of the Mid Staffordshire NHS Foundation Trust, the failure to develop and
provide a quality standard services have been highlighted, in several cases, which indicated
that patient’s voice have been neglected by the care authorities continuously, leading to a
poor care outcome. On the other hand, it has also been noticed that the management did not
attempted to look into these matters or did not listen to issues raised by staffs regarding the
improvement of facilities and services in the “health and social care” settings”. As a result,
the NHS associated trust is losing public trust due to low level of practice. A lack of
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
partnership working has been highlighted in the practice indicating huge improvements
needed in the care setting as soon as possible.
According to Aveyard (2014), “working in partnership” is the key part of practice in “health
and social care” context. The notions of “power sharing, consultation and cooperative ways
of working” are vital for efficient service provision in “health and social care” setting. In the
partnership-working environment, “health and social care” professionals must involve the
care service user in the partnership working, which would empower the patient by enhancing
their self esteem, which in turn promote his overall wellbeing. Promoting autonomy of
service users is a key responsibility and “philosophy of working” in the “health and social
care” settings, while being attentive of their own roles and responsibilities. In the current
settings, the National Health Service promoted the urgency of working in partnership in
healthcare sector. It is important for developing supportive relationships for providing good
health service. In this context, considering patients as a crucial part of the partnership
working is needed, as patient preference is not a “reflection of good practice”, rather it is a
“government policy”.
In this context, several philosophy of working should be followed by the Mid Staffordshire
NHS Foundation Trust, for several reasons. For instance, it helps to provide equity in service,
helps to improve efficiency as well as quality of services provided. In addition, it is also
needed to improve the power balance within the care settings, as well as to build a good inter-
professional relationship culture in the care settings. The key philosophies used in “health and
social care” settings for promoting partnership in working is demonstrated in the following
part.
Ethics: Ethics is a key issue in the “health and social care” settings. The professionals must
understand and make decision by considering what is right and wrong to the patient.
However, several dilemmas arises for making decisions in several contexts, especially in case
of aged care, end life care as well as supporting patient’s choice. In this context, Deontology
and utilitarianism theories are followed, where the first one highlights the moral duties of the
care professionals to be maintained during the care provision and the second one focuses
upon utility, i.e. creating maximal balance of positive value over disvalue to the patients’
wellbeing (Lowes and Hulatt, 2013). In addition, ethics is important for promoting the human
rights of the patients, workers as well as the employers. In this context, paternalism is also a
key issue of professional ethics in “health and social care” settings. The other ethical
needed in the care setting as soon as possible.
According to Aveyard (2014), “working in partnership” is the key part of practice in “health
and social care” context. The notions of “power sharing, consultation and cooperative ways
of working” are vital for efficient service provision in “health and social care” setting. In the
partnership-working environment, “health and social care” professionals must involve the
care service user in the partnership working, which would empower the patient by enhancing
their self esteem, which in turn promote his overall wellbeing. Promoting autonomy of
service users is a key responsibility and “philosophy of working” in the “health and social
care” settings, while being attentive of their own roles and responsibilities. In the current
settings, the National Health Service promoted the urgency of working in partnership in
healthcare sector. It is important for developing supportive relationships for providing good
health service. In this context, considering patients as a crucial part of the partnership
working is needed, as patient preference is not a “reflection of good practice”, rather it is a
“government policy”.
In this context, several philosophy of working should be followed by the Mid Staffordshire
NHS Foundation Trust, for several reasons. For instance, it helps to provide equity in service,
helps to improve efficiency as well as quality of services provided. In addition, it is also
needed to improve the power balance within the care settings, as well as to build a good inter-
professional relationship culture in the care settings. The key philosophies used in “health and
social care” settings for promoting partnership in working is demonstrated in the following
part.
Ethics: Ethics is a key issue in the “health and social care” settings. The professionals must
understand and make decision by considering what is right and wrong to the patient.
However, several dilemmas arises for making decisions in several contexts, especially in case
of aged care, end life care as well as supporting patient’s choice. In this context, Deontology
and utilitarianism theories are followed, where the first one highlights the moral duties of the
care professionals to be maintained during the care provision and the second one focuses
upon utility, i.e. creating maximal balance of positive value over disvalue to the patients’
wellbeing (Lowes and Hulatt, 2013). In addition, ethics is important for promoting the human
rights of the patients, workers as well as the employers. In this context, paternalism is also a
key issue of professional ethics in “health and social care” settings. The other ethical
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
philosophies are followed by the “health and social care” workers, which include the
following ones, for promoting the overall wellbeing of the patients as well as the care
workers.
Beneficence: Beneficence indicates that “health and social care” workers must promote such
activities, which have benefits over the health care service users. In this context, it is
necessary for the health care professionals to consider benefits for a particular service user.
Non-maleficience: Another key ethical philosophy in health care setting is non-maleficience,
which indicates that the “health and social care” professionals must ensure that they are not
harming the care user, i.e. services are provided after ensuring that these are not harmful for
the care user.
Autonomy and independence: In care setting, while involving care users in the care team, it
needs to be ensured that the patient’ choice and rights are being promoted. In this is context,
care workers must show respect to their autonomy and independence. The patients must
promote to take their own decision regarding care services (Village and Hooper, 2015).
Empowerment: Empowering is referred to the process of determining, facilitating and
increasing individual’s capabilities to meet their own needs, to resolve their own issues and
organize the important resources for feeling that they can manage their own lives. It helps to
enrich experience, develop the sense of satisfaction throughout their own realization, which is
ultimately leading to smooth partnership relationship building.
Respect: Respect is crucial in “health and social care” setting, for promoting relationship as
well as for improving the quality of outcomes. It is important to respect patient’s culture and
dignity, in order to protect patient’s autonomy. Moreover, showing unconditional positive
regard helps patients to be felt values, which in turn promotes the health outcomes.
Justice: Providing fair treatment is important for enhancing patient’s trust towards the care
system, which influences the health progress and overall wellbeing.
Power sharing: “Power sharing” in “health and social care” setting involves significant
negotiation in for arriving at a mutual understanding of the roles and liabilities of each team
members beyond the multidisciplinary boundaries, while eliminating power relationships.
Making informed choice: This philosophy ensures that “health and social care” professionals
are promoting the ethical considerations, by making the service users aware about the “health
following ones, for promoting the overall wellbeing of the patients as well as the care
workers.
Beneficence: Beneficence indicates that “health and social care” workers must promote such
activities, which have benefits over the health care service users. In this context, it is
necessary for the health care professionals to consider benefits for a particular service user.
Non-maleficience: Another key ethical philosophy in health care setting is non-maleficience,
which indicates that the “health and social care” professionals must ensure that they are not
harming the care user, i.e. services are provided after ensuring that these are not harmful for
the care user.
Autonomy and independence: In care setting, while involving care users in the care team, it
needs to be ensured that the patient’ choice and rights are being promoted. In this is context,
care workers must show respect to their autonomy and independence. The patients must
promote to take their own decision regarding care services (Village and Hooper, 2015).
Empowerment: Empowering is referred to the process of determining, facilitating and
increasing individual’s capabilities to meet their own needs, to resolve their own issues and
organize the important resources for feeling that they can manage their own lives. It helps to
enrich experience, develop the sense of satisfaction throughout their own realization, which is
ultimately leading to smooth partnership relationship building.
Respect: Respect is crucial in “health and social care” setting, for promoting relationship as
well as for improving the quality of outcomes. It is important to respect patient’s culture and
dignity, in order to protect patient’s autonomy. Moreover, showing unconditional positive
regard helps patients to be felt values, which in turn promotes the health outcomes.
Justice: Providing fair treatment is important for enhancing patient’s trust towards the care
system, which influences the health progress and overall wellbeing.
Power sharing: “Power sharing” in “health and social care” setting involves significant
negotiation in for arriving at a mutual understanding of the roles and liabilities of each team
members beyond the multidisciplinary boundaries, while eliminating power relationships.
Making informed choice: This philosophy ensures that “health and social care” professionals
are promoting the ethical considerations, by making the service users aware about the “health

and social care services” provided to them. It also helps to eliminate the risk of further
conflicts in the care settings (Armstrong and Rauch, 2017).
Reviewing the key philosophies in “health and social care” settings, it has been revealed that
in the Mid Staffordshire NHS Foundation Trust, these philosophies need to be implemented
in all the operational units.
1.2 Evaluate partnership relationships within “health and social care” services
In ““health and social care”” working, partnership could be implemented at various levels,
including the internal as well as external settings. For instance, within the professionals and
care users to the partnership within health service facilities and the social care service
facilities. Strategic partnership is crucial for the success of the teamwork done by the
partners. The partnership relationships can be evaluated in terms of the service users’
outcomes as well as the standards or targets met by the organizations. In the case of the Mid
Staffordshire NHS Foundation Trust, ineffective approaches of partnership has led to
negative outcomes of the service users, which in turn reduced the overall trust of general
public on the care setting. Thus, while evaluating partnership relations in the “health and
social care” settings, the following aspects need to be considered. The goal of these
partnership relationships are prevention, early intervention, improved quality and efficiency,
meeting service user’s needs and provision of seamless services.
Interpersonal working: Partnership between independent service provider and service users:
It is highly crucial for empowering the care service users. The service users usually feel
comfortable, if the care providers attempt to show positive regards and try to establish a
positive relationship within the care framework. Nowadays, the partnership in HSC
philosophies indicates that the patients are placed at the centre position of the care team,
where their perception and values are being promoted. This can only be done when a strong
positive relationship is built within the care professional and care user (Dickinson and
O'Flynn, 2016).
Interdisciplinary teamwork: Partnership between professionals of multidisciplinary care
team: Multidisciplinary teamwork or interdisciplinary teamwork is referred to the teamwork
between professionals from different disciplinary services, for ensuring the overall wellbeing
of the care users. Nowadays, the holistic approach of wellbeing is followed in care setting,
where, the assessment of care user is done not only looking into the issue, for which he is
conflicts in the care settings (Armstrong and Rauch, 2017).
Reviewing the key philosophies in “health and social care” settings, it has been revealed that
in the Mid Staffordshire NHS Foundation Trust, these philosophies need to be implemented
in all the operational units.
1.2 Evaluate partnership relationships within “health and social care” services
In ““health and social care”” working, partnership could be implemented at various levels,
including the internal as well as external settings. For instance, within the professionals and
care users to the partnership within health service facilities and the social care service
facilities. Strategic partnership is crucial for the success of the teamwork done by the
partners. The partnership relationships can be evaluated in terms of the service users’
outcomes as well as the standards or targets met by the organizations. In the case of the Mid
Staffordshire NHS Foundation Trust, ineffective approaches of partnership has led to
negative outcomes of the service users, which in turn reduced the overall trust of general
public on the care setting. Thus, while evaluating partnership relations in the “health and
social care” settings, the following aspects need to be considered. The goal of these
partnership relationships are prevention, early intervention, improved quality and efficiency,
meeting service user’s needs and provision of seamless services.
Interpersonal working: Partnership between independent service provider and service users:
It is highly crucial for empowering the care service users. The service users usually feel
comfortable, if the care providers attempt to show positive regards and try to establish a
positive relationship within the care framework. Nowadays, the partnership in HSC
philosophies indicates that the patients are placed at the centre position of the care team,
where their perception and values are being promoted. This can only be done when a strong
positive relationship is built within the care professional and care user (Dickinson and
O'Flynn, 2016).
Interdisciplinary teamwork: Partnership between professionals of multidisciplinary care
team: Multidisciplinary teamwork or interdisciplinary teamwork is referred to the teamwork
between professionals from different disciplinary services, for ensuring the overall wellbeing
of the care users. Nowadays, the holistic approach of wellbeing is followed in care setting,
where, the assessment of care user is done not only looking into the issue, for which he is
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
seeking service, rather the other domains of health and wellbeing are also being addressed,
and adequate care services are included in the care plan by the professionals from different
domains, in order to improve the patient’s overall health and wellbeing.
Inter-agency working: Partnership between health care and others organizations: It is also
important for “health and social care” organizations to establish partnership relations with
other agencies, for working in wider context. For instance, in case of the “Mid Staffordshire
NHS Foundation Trust”, the trust has established a partnership relationship with the NHS
trust. In addition, the partnership relationship could also be developed with the other private
and voluntary organizations, like diagnostic centres, mental health support, primary care,
social service centres, aged care, care home or residencies as well as rehabilitation centre
(Carpenter et al. 2017).
Strategic partnership: Partnership between local authorities and health care facilities: It is
also important for promoting the quality of services provided to the “health and social care”
service users. The involvement or development of partnership with the local authorities or
government agencies would help the organization to get funds and implement strategic
policies and standards to improve the overall outcomes.
LO 2: Understand how to promote positive partnership working with users of services,
professionals and organizations in “health and social care” services.
2.1 Analyze models of partnership working across the “health and social care” sector
There are several partnership models used in “health and social care” for getting a guideline
of partnership in the organizational context. It has been revealed that the management system
of the Mid Staffordshire NHS Foundation Trust has not followed any partnership models for
addressing and improving the partnership working and positive consequences of the service
users’ outcomes. The key models, which they can use to develop partnership relationship in
the care settings, are discussed below:
The Unified model- This model has been indicated as one of the most structurally integrated
and comprehensive models of health and personal social services in Europe. It promotes the
development and implementation of single integrated system of HSC service delivery. Under
this model, a single unified trust provides all the “health and social care” services, while each
trust consist a financial system and uses a single strategic approach with common goals and
and adequate care services are included in the care plan by the professionals from different
domains, in order to improve the patient’s overall health and wellbeing.
Inter-agency working: Partnership between health care and others organizations: It is also
important for “health and social care” organizations to establish partnership relations with
other agencies, for working in wider context. For instance, in case of the “Mid Staffordshire
NHS Foundation Trust”, the trust has established a partnership relationship with the NHS
trust. In addition, the partnership relationship could also be developed with the other private
and voluntary organizations, like diagnostic centres, mental health support, primary care,
social service centres, aged care, care home or residencies as well as rehabilitation centre
(Carpenter et al. 2017).
Strategic partnership: Partnership between local authorities and health care facilities: It is
also important for promoting the quality of services provided to the “health and social care”
service users. The involvement or development of partnership with the local authorities or
government agencies would help the organization to get funds and implement strategic
policies and standards to improve the overall outcomes.
LO 2: Understand how to promote positive partnership working with users of services,
professionals and organizations in “health and social care” services.
2.1 Analyze models of partnership working across the “health and social care” sector
There are several partnership models used in “health and social care” for getting a guideline
of partnership in the organizational context. It has been revealed that the management system
of the Mid Staffordshire NHS Foundation Trust has not followed any partnership models for
addressing and improving the partnership working and positive consequences of the service
users’ outcomes. The key models, which they can use to develop partnership relationship in
the care settings, are discussed below:
The Unified model- This model has been indicated as one of the most structurally integrated
and comprehensive models of health and personal social services in Europe. It promotes the
development and implementation of single integrated system of HSC service delivery. Under
this model, a single unified trust provides all the “health and social care” services, while each
trust consist a financial system and uses a single strategic approach with common goals and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
objectives. This model helps to reduce delay in services, develop integrated teams and
enhance integrated working within the system. However, the model promotes the continued
dominance by the agenda and integration has not realised its maximum potential (Green,
2015).
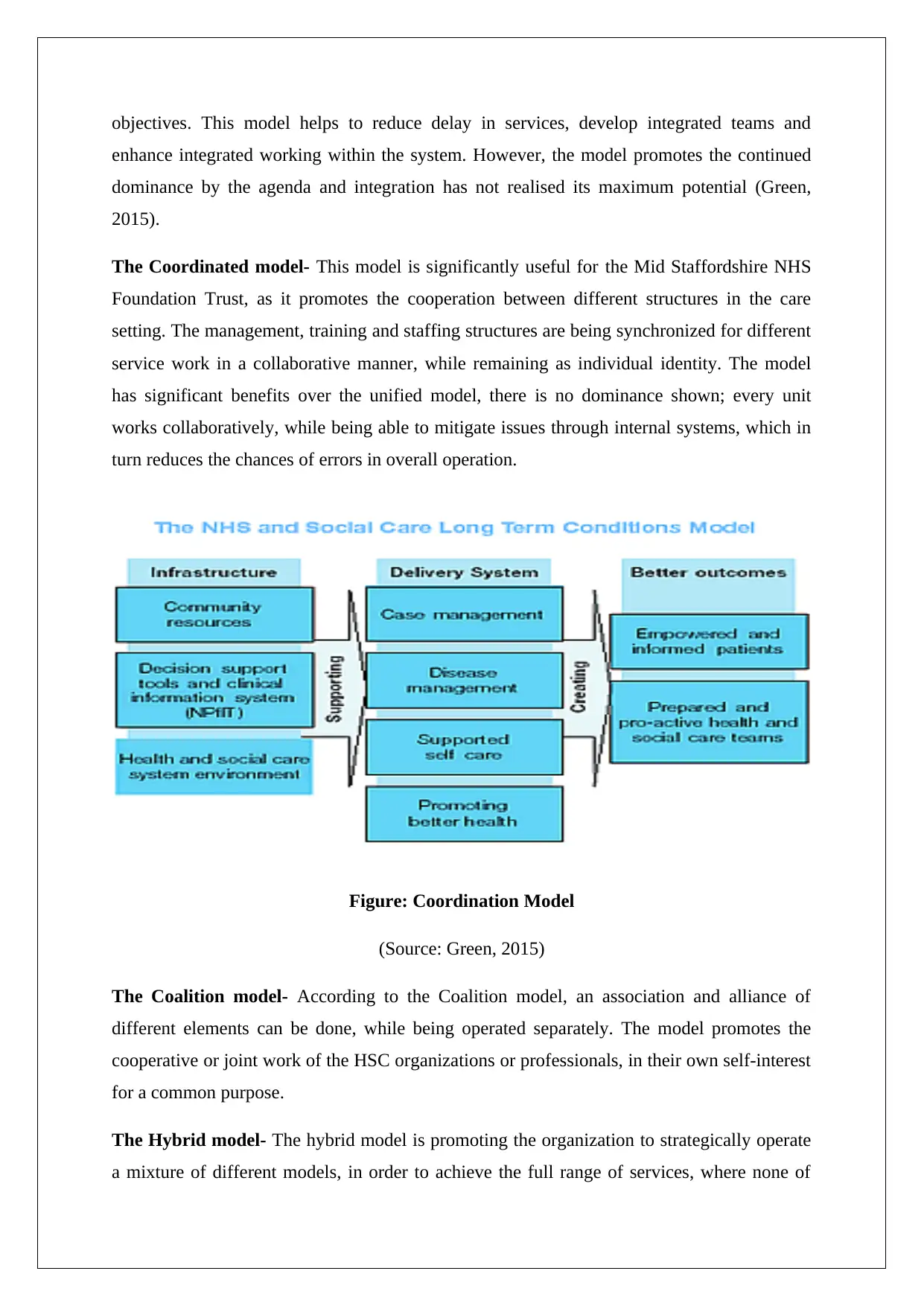
The Coordinated model- This model is significantly useful for the Mid Staffordshire NHS
Foundation Trust, as it promotes the cooperation between different structures in the care
setting. The management, training and staffing structures are being synchronized for different
service work in a collaborative manner, while remaining as individual identity. The model
has significant benefits over the unified model, there is no dominance shown; every unit
works collaboratively, while being able to mitigate issues through internal systems, which in
turn reduces the chances of errors in overall operation.
Figure: Coordination Model
(Source: Green, 2015)
The Coalition model- According to the Coalition model, an association and alliance of
different elements can be done, while being operated separately. The model promotes the
cooperative or joint work of the HSC organizations or professionals, in their own self-interest
for a common purpose.
The Hybrid model- The hybrid model is promoting the organization to strategically operate
a mixture of different models, in order to achieve the full range of services, where none of
enhance integrated working within the system. However, the model promotes the continued
dominance by the agenda and integration has not realised its maximum potential (Green,
2015).
The Coordinated model- This model is significantly useful for the Mid Staffordshire NHS
Foundation Trust, as it promotes the cooperation between different structures in the care
setting. The management, training and staffing structures are being synchronized for different
service work in a collaborative manner, while remaining as individual identity. The model
has significant benefits over the unified model, there is no dominance shown; every unit
works collaboratively, while being able to mitigate issues through internal systems, which in
turn reduces the chances of errors in overall operation.
Figure: Coordination Model
(Source: Green, 2015)
The Coalition model- According to the Coalition model, an association and alliance of
different elements can be done, while being operated separately. The model promotes the
cooperative or joint work of the HSC organizations or professionals, in their own self-interest
for a common purpose.
The Hybrid model- The hybrid model is promoting the organization to strategically operate
a mixture of different models, in order to achieve the full range of services, where none of
these model could dominate the other, rather includes the perspectives in a collaborative
fashion.
2.2 Review current legislation and organizational practices and policies for partnership
working in “health and social care”.
In “health and social care” settings, several legislations and partnership policies guide the
practices in the care settings. According to McLaughlin et al. (2014), care provision is
significantly affected by laws and guides the organization to operate in a certain way. On the
other hand, the government has introduced some policies, for guiding the practices in “health
and social care” settings. The key legislations, policies and organizational practices those are
affecting the partnership working in “health and social care” context include:
“health and social care” Act 2012- The act has reinforced the “National Health Service Act
2006” (NHS Act). According to this act, four key aspect of NHS are “clinical commissioning
groups, health and wellbeing boards, economic regulation and providers”. The act promotes
development of “Clinical commissioning groups” and “Health and wellbeing boards”, which
would review the performance of partner organizations (Care Quality Commission, 2012).
The act aims to improve accountability and patient voice, which the Mid Staffordshire NHS
Foundation Trust needs to follow for improving their practices.
Care standard act 2000- This act has reformed the regulatory system of care in England and
Wales. This act regulates the effectiveness of care provision, by reviewing and inspecting the
effectiveness of partnership developed within different health care agencies.
NHS Act, Section 75- Section 75 in NHS Act 2006 highlighted partnership, which has
enabled partners to collaboratively perform for designing and delivering services to care users
based on their needs, which would allow service users to get overall care services, instead of
worrying about boundaries of organizations (Aveyard, 2014).
Mental health acts 1983 and 2007- This act has focused on strengthening user’s rights
beyond their mental health status, indicating the rights to get fair treatment by the mentally ill
patients. In partnership work, partners would include risk management strategies to focus on
this matter.
Mental capacity act 2005- The act promotes the requirement of collaborative working
between all agencies as well as professionals from different disciplines, who affect the
fashion.
2.2 Review current legislation and organizational practices and policies for partnership
working in “health and social care”.
In “health and social care” settings, several legislations and partnership policies guide the
practices in the care settings. According to McLaughlin et al. (2014), care provision is
significantly affected by laws and guides the organization to operate in a certain way. On the
other hand, the government has introduced some policies, for guiding the practices in “health
and social care” settings. The key legislations, policies and organizational practices those are
affecting the partnership working in “health and social care” context include:
“health and social care” Act 2012- The act has reinforced the “National Health Service Act
2006” (NHS Act). According to this act, four key aspect of NHS are “clinical commissioning
groups, health and wellbeing boards, economic regulation and providers”. The act promotes
development of “Clinical commissioning groups” and “Health and wellbeing boards”, which
would review the performance of partner organizations (Care Quality Commission, 2012).
The act aims to improve accountability and patient voice, which the Mid Staffordshire NHS
Foundation Trust needs to follow for improving their practices.
Care standard act 2000- This act has reformed the regulatory system of care in England and
Wales. This act regulates the effectiveness of care provision, by reviewing and inspecting the
effectiveness of partnership developed within different health care agencies.
NHS Act, Section 75- Section 75 in NHS Act 2006 highlighted partnership, which has
enabled partners to collaboratively perform for designing and delivering services to care users
based on their needs, which would allow service users to get overall care services, instead of
worrying about boundaries of organizations (Aveyard, 2014).
Mental health acts 1983 and 2007- This act has focused on strengthening user’s rights
beyond their mental health status, indicating the rights to get fair treatment by the mentally ill
patients. In partnership work, partners would include risk management strategies to focus on
this matter.
Mental capacity act 2005- The act promotes the requirement of collaborative working
between all agencies as well as professionals from different disciplines, who affect the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

service user, in order to empower and protect service user, lacking the capacity to make
decisions for him.
National Health Service and Community Care Act 1990- The act has introduced an
internal market within the supply of healthcare, which indicates the duty of local authorities
to assess the service users for social care support. Thus, this act is actually promoting
collaborative work within local authorities and other agencies (Dickinson and O'Flynn,
2016).
Organizational practices and policies- In addition to the above mentioned legislations, the
organizational policies and practices are also affecting the outcomes of the “health and social
care” organizations. For instance, the Mid Staffordshire NHS Foundation Trust have not
implemented appropriate policies, while not adhering to the local, regional and national legal
frameworks, which led to reduced care standards. Thus, the organization needs to implement
agreed ways of working, aligning with statutory policies and legal framework. On the other
hand, while establishing inter-agency partnership, the organizations must show respect to the
partner’s organizational policies and practices (Green, 2015). The adherence to local, regional
and national policy documents introduced by the national government should also be done. In
addition, policies for specialist units, voluntary agencies, risk assessment procedures and
employment practices must be produced.
2.3 Explain how differences in working practices and policies affect collaborative
working
Differences in working practices and policies significantly affect the establishment of
effective partnership. The differences among the local authorizes, different disciplinary
“health and social care” services, NHS and government bodies could affect the development
of partnership. The differences that hinder effective partnership formation in HSC settings
are, different purpose, different goals or outcomes specification, different professional
perspectives and training, different monitoring, regulatory and governing bodies, different
focus regarding legal, professional and ethical codes of practices in the care settings (Lowes
and Hulatt, 2013).
decisions for him.
National Health Service and Community Care Act 1990- The act has introduced an
internal market within the supply of healthcare, which indicates the duty of local authorities
to assess the service users for social care support. Thus, this act is actually promoting
collaborative work within local authorities and other agencies (Dickinson and O'Flynn,
2016).
Organizational practices and policies- In addition to the above mentioned legislations, the
organizational policies and practices are also affecting the outcomes of the “health and social
care” organizations. For instance, the Mid Staffordshire NHS Foundation Trust have not
implemented appropriate policies, while not adhering to the local, regional and national legal
frameworks, which led to reduced care standards. Thus, the organization needs to implement
agreed ways of working, aligning with statutory policies and legal framework. On the other
hand, while establishing inter-agency partnership, the organizations must show respect to the
partner’s organizational policies and practices (Green, 2015). The adherence to local, regional
and national policy documents introduced by the national government should also be done. In
addition, policies for specialist units, voluntary agencies, risk assessment procedures and
employment practices must be produced.
2.3 Explain how differences in working practices and policies affect collaborative
working
Differences in working practices and policies significantly affect the establishment of
effective partnership. The differences among the local authorizes, different disciplinary
“health and social care” services, NHS and government bodies could affect the development
of partnership. The differences that hinder effective partnership formation in HSC settings
are, different purpose, different goals or outcomes specification, different professional
perspectives and training, different monitoring, regulatory and governing bodies, different
focus regarding legal, professional and ethical codes of practices in the care settings (Lowes
and Hulatt, 2013).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
LO 3: Be able to evaluate the outcomes of partnership working for users of services,
professionals and organizations in “health and social care” services.
3.1 Evaluate possible outcomes of partnership working for users of services,
professionals and organizations
According to Thomas (2015), the Francis Report, there was an awful and unnecessary
suffering of hundreds of people due to neglecting warning signs and put cost controlled as
well as corporate self-interest ahead of their patients and their safety. This causes Mid
Staffordshire NHS Foundation Trust a serious damage in their brand image. The negative
results are listed below,
Neglect: From the above case study, it is identified that this organizational faculty is not
serious about their patient care services. A serious lacking of concentration as well as
responsibility is focused due to this type of incident.
Miscommunication: From the above case study, it is evident that there is a serious
miscommunication between the organizational faculties and members while taking care of
patients. The organizational management and communication structure is not productive to
perform difficult tasks (Cameron et al., 2014).
Anger and Frustration: Due to this kind of incident there is an increase of frustration level
and anger among the relatives of patients who are dead and affected along with other patients
present in the organization.
Harm: Serious damage to the human property happen due to this kind of negligence in work.
Moreover, this incident has exhibited the fact that patients’ trust over the organization is
damaged to some extent, which is not welcome for the “health and social care” organizations
and could be more harmful in future. On the other hand, if this organization follows
procedures effectively, then the organizational management could notice that there is
immense change in possible outcomes, which will be centred round Empowerment, perfect
autonomy, development in services as well as a structure and informed decision-making
procedure (Cameron et al., 2014).
professionals and organizations in “health and social care” services.
3.1 Evaluate possible outcomes of partnership working for users of services,
professionals and organizations
According to Thomas (2015), the Francis Report, there was an awful and unnecessary
suffering of hundreds of people due to neglecting warning signs and put cost controlled as
well as corporate self-interest ahead of their patients and their safety. This causes Mid
Staffordshire NHS Foundation Trust a serious damage in their brand image. The negative
results are listed below,
Neglect: From the above case study, it is identified that this organizational faculty is not
serious about their patient care services. A serious lacking of concentration as well as
responsibility is focused due to this type of incident.
Miscommunication: From the above case study, it is evident that there is a serious
miscommunication between the organizational faculties and members while taking care of
patients. The organizational management and communication structure is not productive to
perform difficult tasks (Cameron et al., 2014).
Anger and Frustration: Due to this kind of incident there is an increase of frustration level
and anger among the relatives of patients who are dead and affected along with other patients
present in the organization.
Harm: Serious damage to the human property happen due to this kind of negligence in work.
Moreover, this incident has exhibited the fact that patients’ trust over the organization is
damaged to some extent, which is not welcome for the “health and social care” organizations
and could be more harmful in future. On the other hand, if this organization follows
procedures effectively, then the organizational management could notice that there is
immense change in possible outcomes, which will be centred round Empowerment, perfect
autonomy, development in services as well as a structure and informed decision-making
procedure (Cameron et al., 2014).
3.2 Analyze the potential barriers to partnership working in “health and social care”
services.
The potential barriers involved in partnership working in “health and social care” services are
explained below,
Different angels in attitudes and business objectives
Working with one partner or more than one partner will cause various angels in business
attitudes and objectives. Some business objectives will cause unintended consequences for
the patients and families under guidance of organizations of this type. Partners involved in
business should plan and analyze possible outcomes of any kind of business initiatives such
as equipment resourcing in “health and social care” (Glasby and Dickinson, 2014). According
to the case study, negligence may be happen due to different angels in attitudes involved with
this organization.
Incomplete systems
Due to lack in compact business management policies as well as objectives “health and social
care” companies often confront incompatible or incomplete systems. There should be
common system present for electronic collection and evaluation of data regarding patients
and families involved in “health and social care” organizations so that all the agencies are
become aware of these information and work according to it (Glasby and Dickinson, 2014).
Otherwise, serious communication would be happen due to this.
Lack of collective decision-making process
A collective decision-making process should be developed within all the partners involved in
a project about enhancing facilities for “health and social care” patients. Otherwise, lack of
decision-making could cause serious damage to organizational property, value, fame and
most importantly loss of patients’ lives (Glasby, 2017). The collective decision-making
process is not effective enough in this case with Mid Staffordshire NHS Foundation Trust and
they neglect alarm regarding warning signs. That is why they put corporate self-interest before
consumer safety.
services.
The potential barriers involved in partnership working in “health and social care” services are
explained below,
Different angels in attitudes and business objectives
Working with one partner or more than one partner will cause various angels in business
attitudes and objectives. Some business objectives will cause unintended consequences for
the patients and families under guidance of organizations of this type. Partners involved in
business should plan and analyze possible outcomes of any kind of business initiatives such
as equipment resourcing in “health and social care” (Glasby and Dickinson, 2014). According
to the case study, negligence may be happen due to different angels in attitudes involved with
this organization.
Incomplete systems
Due to lack in compact business management policies as well as objectives “health and social
care” companies often confront incompatible or incomplete systems. There should be
common system present for electronic collection and evaluation of data regarding patients
and families involved in “health and social care” organizations so that all the agencies are
become aware of these information and work according to it (Glasby and Dickinson, 2014).
Otherwise, serious communication would be happen due to this.
Lack of collective decision-making process
A collective decision-making process should be developed within all the partners involved in
a project about enhancing facilities for “health and social care” patients. Otherwise, lack of
decision-making could cause serious damage to organizational property, value, fame and
most importantly loss of patients’ lives (Glasby, 2017). The collective decision-making
process is not effective enough in this case with Mid Staffordshire NHS Foundation Trust and
they neglect alarm regarding warning signs. That is why they put corporate self-interest before
consumer safety.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





