Health Workforce Plan: Analyzing Kenya's Healthcare System (2019)
VerifiedAdded on 2022/11/28
|19
|4621
|432
Report
AI Summary
This report presents a health workforce plan for Kenya, addressing the critical shortage of healthcare workers. The executive summary highlights the context and environment, revealing a deficit of over 42,800 health workers, hindering the achievement of universal healthcare goals. The report analyzes the external environment, emphasizing the global challenge of health worker shortages, particularly in sub-Saharan Africa. It delves into the internal environment, assessing Kenya's capacity to train healthcare professionals. The current health workforce profile is examined, and a gap analysis is conducted, leading to proposed closing strategies, including investment in education. The report aims to reduce the health worker shortage by improving health worker density, as recommended by the WHO, and includes an evaluation strategy and next steps. The report also provides tables with detailed statistics on the gap of health workforce specialists in Kenya, and proposes strategies to improve the situation.

Running Head: HEALTH WORKFORCE PLAN, CASE STUDY OF KENYA 1
Health Workforce Plan, Case Study of Kenya
Student Name
Institution Affiliation
Course
Date
Health Workforce Plan, Case Study of Kenya
Student Name
Institution Affiliation
Course
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH WORKFORCE PLAN, CASE STUDY OF KENYA 2
Table of Contents
Introduction......................................................................................................................................3
Context and Environment................................................................................................................3
External Environment..................................................................................................................5
Internal Environment...................................................................................................................6
The Current Health Workforce Profile in Kenya............................................................................7
Future Workforce Profile in Kenya.................................................................................................8
Gap Analysis and Closing Strategies...............................................................................................9
Conclusion, Review, Evaluation Strategy and Next Steps............................................................10
References......................................................................................................................................11
Table of Contents
Introduction......................................................................................................................................3
Context and Environment................................................................................................................3
External Environment..................................................................................................................5
Internal Environment...................................................................................................................6
The Current Health Workforce Profile in Kenya............................................................................7
Future Workforce Profile in Kenya.................................................................................................8
Gap Analysis and Closing Strategies...............................................................................................9
Conclusion, Review, Evaluation Strategy and Next Steps............................................................10
References......................................................................................................................................11
HEALTH WORKFORCE PLAN, CASE STUDY OF KENYA 3
Executive summary
With the help of World Health Organization (WHO), this paper has identified Kenya as a
low-middle income country whose health sector has a lot to be done. For improvement
purposes, the paper has come up with a workforce plan. The outlined workforce place will
solve the problem of health worker shortage in the country. In the first subtitle, context and
environment, it has been revealed that Kenya has been grappling with a shortage of 42,800
health workers which has made it very hard for the country to meet its health goals. The
second subtitle, the external environment, has presented health worker shortage as a big
problem especially among the sub-Saharan African countries which has made it very hard for
them to achieve universal healthcare. In the current workforce profile of Kenya, the paper has
revealed that the country has enough institutions which can accommodate enough healthcare
workers for its market. To close the gap on healthcare worker shortage, the paper has
proposed that the government of Kenya should invest on its education system to encourage
more learners in the healthcare sector
Executive summary
With the help of World Health Organization (WHO), this paper has identified Kenya as a
low-middle income country whose health sector has a lot to be done. For improvement
purposes, the paper has come up with a workforce plan. The outlined workforce place will
solve the problem of health worker shortage in the country. In the first subtitle, context and
environment, it has been revealed that Kenya has been grappling with a shortage of 42,800
health workers which has made it very hard for the country to meet its health goals. The
second subtitle, the external environment, has presented health worker shortage as a big
problem especially among the sub-Saharan African countries which has made it very hard for
them to achieve universal healthcare. In the current workforce profile of Kenya, the paper has
revealed that the country has enough institutions which can accommodate enough healthcare
workers for its market. To close the gap on healthcare worker shortage, the paper has
proposed that the government of Kenya should invest on its education system to encourage
more learners in the healthcare sector
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTH WORKFORCE PLAN, CASE STUDY OF KENYA 4
Health Workforce Plan, Case Study of Kenya
Introduction
Currently, the shortage of health workers among the countries which have poor health
indicators has hit the headlines. This trend has brought about some far-reaching impacts on
the countries’ ability to provide essential health services, fight diseases and implement
effective life-saving interventions (Knevel, Gussy & Farmer, 2017). World Health
Organization (WHO) has estimated that the current workforce in most of the countries under
the poor health indicator category will need to be scaled up by as much as 140% in order to
attain the health development targets which have been set by the Millennium Declaration
(World Health Organization, 2016). Further, WHO revealed that shortage of healthcare
workforce has been very serious among those countries to an extent that there has not been
enough human capacity to absorb, deploy and efficiently utilize the substantial funds which
are considered necessary to improve health care sector. This paper proposes a health
workforce plan to solve the problem of health worker shortage in Kenya.
Context and Environment
According to a health report drafted on March 2018, Kenya was grappling with a
shortage of 42,800 health workers, a condition which made it hard for this sub-Saharan
African country to achieve universal healthcare (McMenamin & Mannion, 2017). According
to this report, the number of medics in the country was far below the standard recommended
by the World Health Organization which is 23 health workers per 10,000 people. The report
revealed that there were 63,000 health workers in the whole country, which included 405
dentists, 293 radiologists, 20,981 nurses, 2286 medical officers, 1104 pharmacists, 22
Health Workforce Plan, Case Study of Kenya
Introduction
Currently, the shortage of health workers among the countries which have poor health
indicators has hit the headlines. This trend has brought about some far-reaching impacts on
the countries’ ability to provide essential health services, fight diseases and implement
effective life-saving interventions (Knevel, Gussy & Farmer, 2017). World Health
Organization (WHO) has estimated that the current workforce in most of the countries under
the poor health indicator category will need to be scaled up by as much as 140% in order to
attain the health development targets which have been set by the Millennium Declaration
(World Health Organization, 2016). Further, WHO revealed that shortage of healthcare
workforce has been very serious among those countries to an extent that there has not been
enough human capacity to absorb, deploy and efficiently utilize the substantial funds which
are considered necessary to improve health care sector. This paper proposes a health
workforce plan to solve the problem of health worker shortage in Kenya.
Context and Environment
According to a health report drafted on March 2018, Kenya was grappling with a
shortage of 42,800 health workers, a condition which made it hard for this sub-Saharan
African country to achieve universal healthcare (McMenamin & Mannion, 2017). According
to this report, the number of medics in the country was far below the standard recommended
by the World Health Organization which is 23 health workers per 10,000 people. The report
revealed that there were 63,000 health workers in the whole country, which included 405
dentists, 293 radiologists, 20,981 nurses, 2286 medical officers, 1104 pharmacists, 22
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH WORKFORCE PLAN, CASE STUDY OF KENYA 5
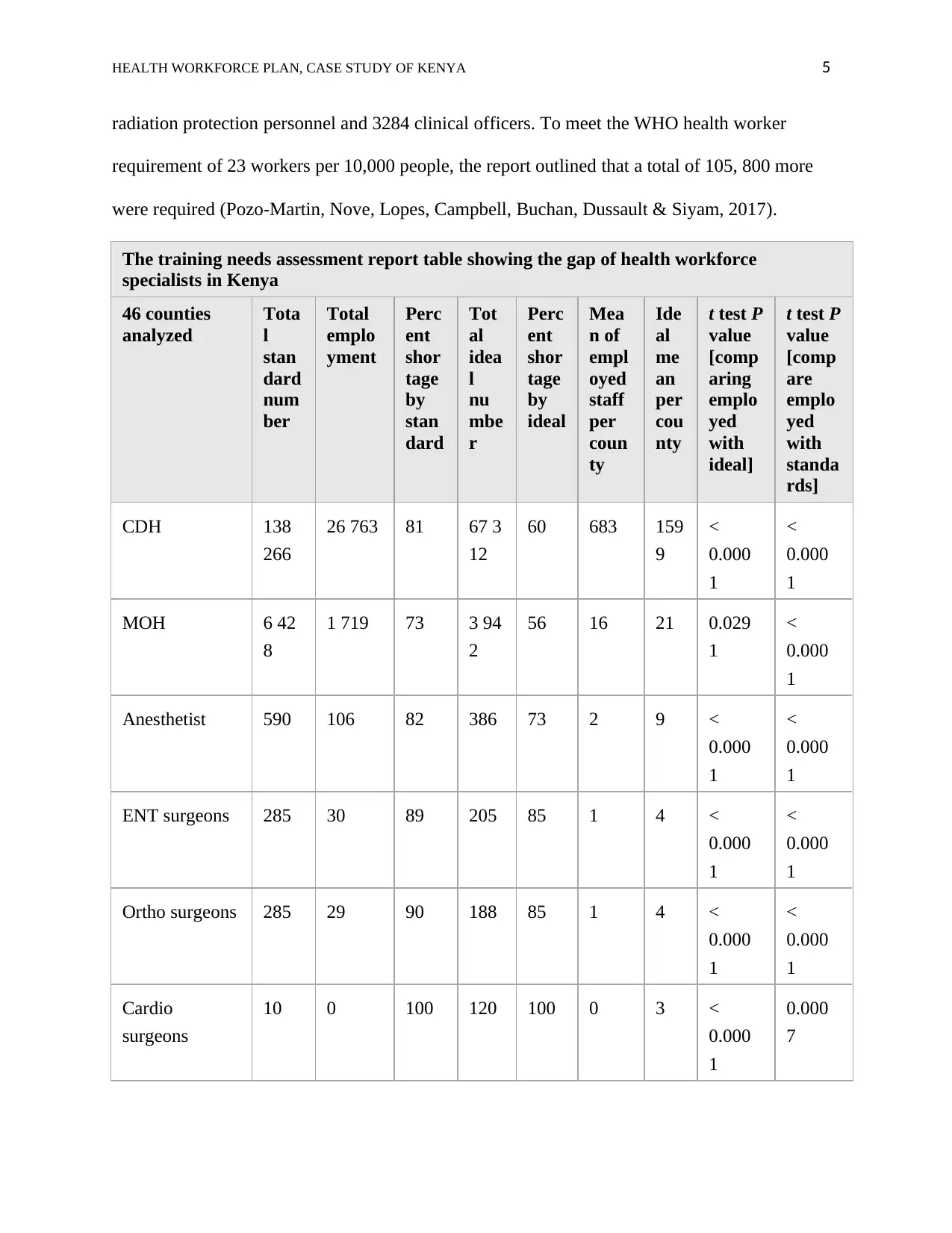
radiation protection personnel and 3284 clinical officers. To meet the WHO health worker
requirement of 23 workers per 10,000 people, the report outlined that a total of 105, 800 more
were required (Pozo-Martin, Nove, Lopes, Campbell, Buchan, Dussault & Siyam, 2017).
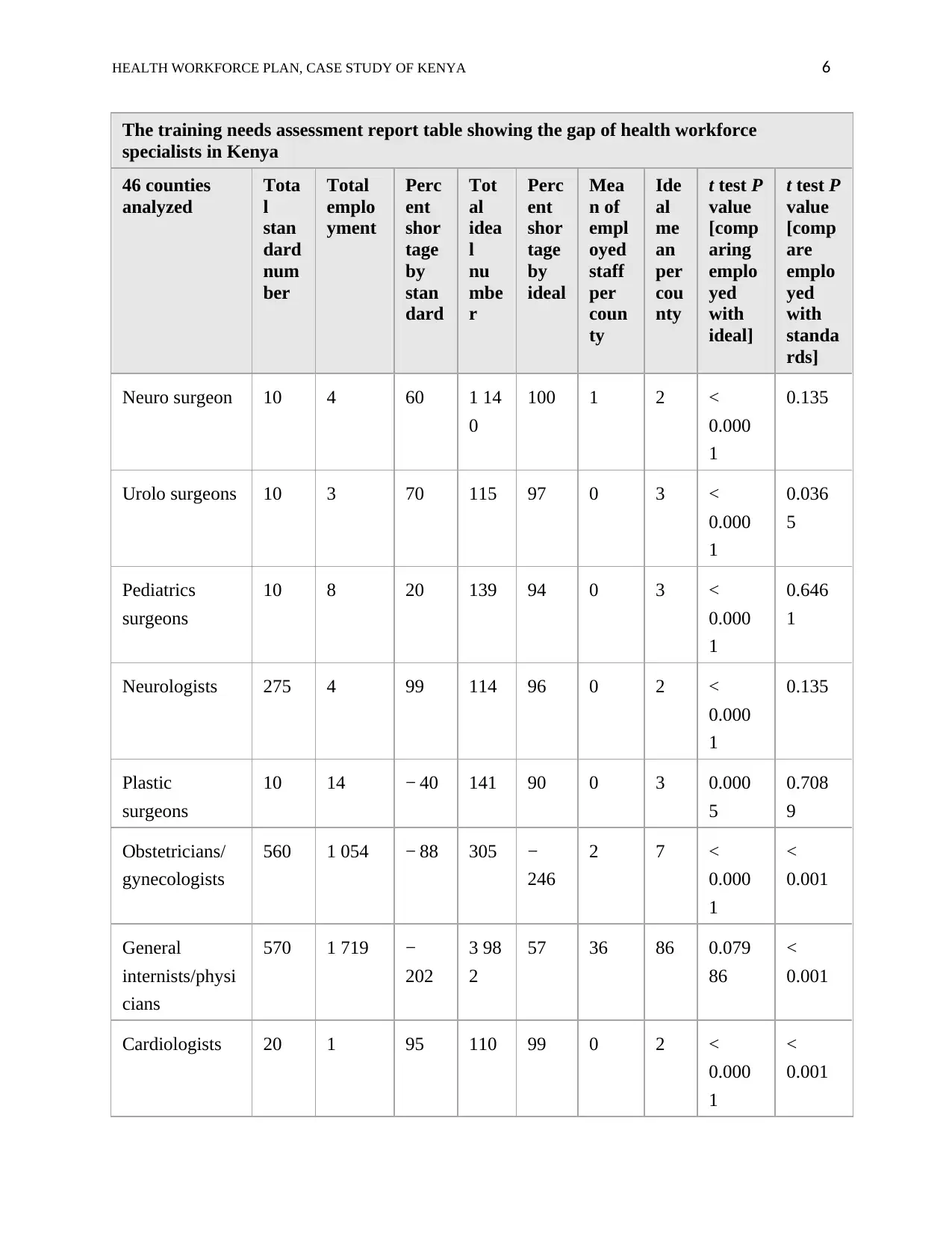
The training needs assessment report table showing the gap of health workforce
specialists in Kenya
46 counties
analyzed
Tota
l
stan
dard
num
ber
Total
emplo
yment
Perc
ent
shor
tage
by
stan
dard
Tot
al
idea
l
nu
mbe
r
Perc
ent
shor
tage
by
ideal
Mea
n of
empl
oyed
staff
per
coun
ty
Ide
al
me
an
per
cou
nty
t test P
value
[comp
aring
emplo
yed
with
ideal]
t test P
value
[comp
are
emplo
yed
with
standa
rds]
CDH 138
266
26 763 81 67 3
12
60 683 159
9
<
0.000
1
<
0.000
1
MOH 6 42
8
1 719 73 3 94
2
56 16 21 0.029
1
<
0.000
1
Anesthetist 590 106 82 386 73 2 9 <
0.000
1
<
0.000
1
ENT surgeons 285 30 89 205 85 1 4 <
0.000
1
<
0.000
1
Ortho surgeons 285 29 90 188 85 1 4 <
0.000
1
<
0.000
1
Cardio
surgeons
10 0 100 120 100 0 3 <
0.000
1
0.000
7
radiation protection personnel and 3284 clinical officers. To meet the WHO health worker
requirement of 23 workers per 10,000 people, the report outlined that a total of 105, 800 more
were required (Pozo-Martin, Nove, Lopes, Campbell, Buchan, Dussault & Siyam, 2017).
The training needs assessment report table showing the gap of health workforce
specialists in Kenya
46 counties
analyzed
Tota
l
stan
dard
num
ber
Total
emplo
yment
Perc
ent
shor
tage
by
stan
dard
Tot
al
idea
l
nu
mbe
r
Perc
ent
shor
tage
by
ideal
Mea
n of
empl
oyed
staff
per
coun
ty
Ide
al
me
an
per
cou
nty
t test P
value
[comp
aring
emplo
yed
with
ideal]
t test P
value
[comp
are
emplo
yed
with
standa
rds]
CDH 138
266
26 763 81 67 3
12
60 683 159
9
<
0.000
1
<
0.000
1
MOH 6 42
8
1 719 73 3 94
2
56 16 21 0.029
1
<
0.000
1
Anesthetist 590 106 82 386 73 2 9 <
0.000
1
<
0.000
1
ENT surgeons 285 30 89 205 85 1 4 <
0.000
1
<
0.000
1
Ortho surgeons 285 29 90 188 85 1 4 <
0.000
1
<
0.000
1
Cardio
surgeons
10 0 100 120 100 0 3 <
0.000
1
0.000
7
HEALTH WORKFORCE PLAN, CASE STUDY OF KENYA 6
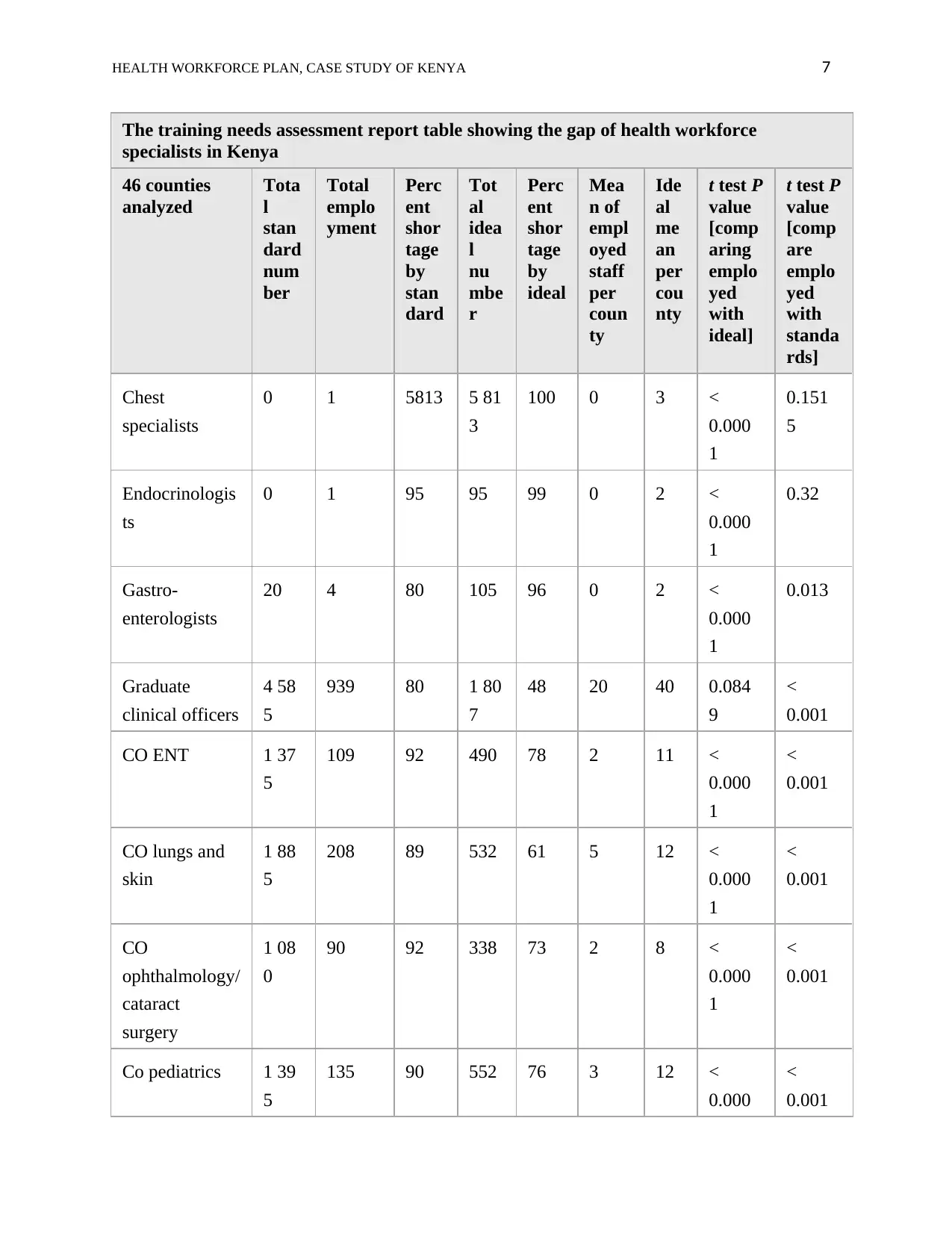
The training needs assessment report table showing the gap of health workforce
specialists in Kenya
46 counties
analyzed
Tota
l
stan
dard
num
ber
Total
emplo
yment
Perc
ent
shor
tage
by
stan
dard
Tot
al
idea
l
nu
mbe
r
Perc
ent
shor
tage
by
ideal
Mea
n of
empl
oyed
staff
per
coun
ty
Ide
al
me
an
per
cou
nty
t test P
value
[comp
aring
emplo
yed
with
ideal]
t test P
value
[comp
are
emplo
yed
with
standa
rds]
Neuro surgeon 10 4 60 1 14
0
100 1 2 <
0.000
1
0.135
Urolo surgeons 10 3 70 115 97 0 3 <
0.000
1
0.036
5
Pediatrics
surgeons
10 8 20 139 94 0 3 <
0.000
1
0.646
1
Neurologists 275 4 99 114 96 0 2 <
0.000
1
0.135
Plastic
surgeons
10 14 − 40 141 90 0 3 0.000
5
0.708
9
Obstetricians/
gynecologists
560 1 054 − 88 305 −
246
2 7 <
0.000
1
<
0.001
General
internists/physi
cians
570 1 719 −
202
3 98
2
57 36 86 0.079
86
<
0.001
Cardiologists 20 1 95 110 99 0 2 <
0.000
1
<
0.001
The training needs assessment report table showing the gap of health workforce
specialists in Kenya
46 counties
analyzed
Tota
l
stan
dard
num
ber
Total
emplo
yment
Perc
ent
shor
tage
by
stan
dard
Tot
al
idea
l
nu
mbe
r
Perc
ent
shor
tage
by
ideal
Mea
n of
empl
oyed
staff
per
coun
ty
Ide
al
me
an
per
cou
nty
t test P
value
[comp
aring
emplo
yed
with
ideal]
t test P
value
[comp
are
emplo
yed
with
standa
rds]
Neuro surgeon 10 4 60 1 14
0
100 1 2 <
0.000
1
0.135
Urolo surgeons 10 3 70 115 97 0 3 <
0.000
1
0.036
5
Pediatrics
surgeons
10 8 20 139 94 0 3 <
0.000
1
0.646
1
Neurologists 275 4 99 114 96 0 2 <
0.000
1
0.135
Plastic
surgeons
10 14 − 40 141 90 0 3 0.000
5
0.708
9
Obstetricians/
gynecologists
560 1 054 − 88 305 −
246
2 7 <
0.000
1
<
0.001
General
internists/physi
cians
570 1 719 −
202
3 98
2
57 36 86 0.079
86
<
0.001
Cardiologists 20 1 95 110 99 0 2 <
0.000
1
<
0.001
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTH WORKFORCE PLAN, CASE STUDY OF KENYA 7
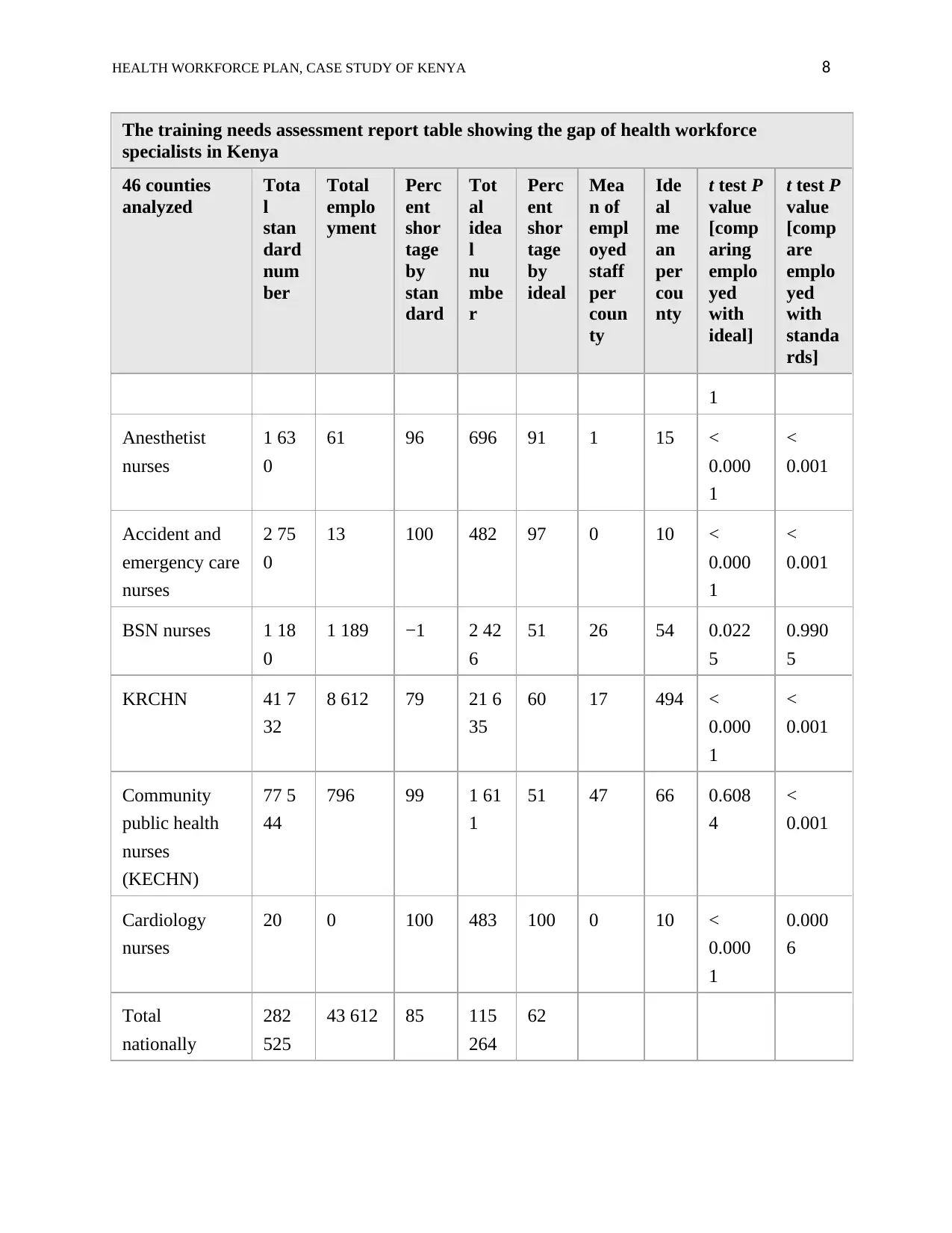
The training needs assessment report table showing the gap of health workforce
specialists in Kenya
46 counties
analyzed
Tota
l
stan
dard
num
ber
Total
emplo
yment
Perc
ent
shor
tage
by
stan
dard
Tot
al
idea
l
nu
mbe
r
Perc
ent
shor
tage
by
ideal
Mea
n of
empl
oyed
staff
per
coun
ty
Ide
al
me
an
per
cou
nty
t test P
value
[comp
aring
emplo
yed
with
ideal]
t test P
value
[comp
are
emplo
yed
with
standa
rds]
Chest
specialists
0 1 5813 5 81
3
100 0 3 <
0.000
1
0.151
5
Endocrinologis
ts
0 1 95 95 99 0 2 <
0.000
1
0.32
Gastro-
enterologists
20 4 80 105 96 0 2 <
0.000
1
0.013
Graduate
clinical officers
4 58
5
939 80 1 80
7
48 20 40 0.084
9
<
0.001
CO ENT 1 37
5
109 92 490 78 2 11 <
0.000
1
<
0.001
CO lungs and
skin
1 88
5
208 89 532 61 5 12 <
0.000
1
<
0.001
CO
ophthalmology/
cataract
surgery
1 08
0
90 92 338 73 2 8 <
0.000
1
<
0.001
Co pediatrics 1 39
5
135 90 552 76 3 12 <
0.000
<
0.001
The training needs assessment report table showing the gap of health workforce
specialists in Kenya
46 counties
analyzed
Tota
l
stan
dard
num
ber
Total
emplo
yment
Perc
ent
shor
tage
by
stan
dard
Tot
al
idea
l
nu
mbe
r
Perc
ent
shor
tage
by
ideal
Mea
n of
empl
oyed
staff
per
coun
ty
Ide
al
me
an
per
cou
nty
t test P
value
[comp
aring
emplo
yed
with
ideal]
t test P
value
[comp
are
emplo
yed
with
standa
rds]
Chest
specialists
0 1 5813 5 81
3
100 0 3 <
0.000
1
0.151
5
Endocrinologis
ts
0 1 95 95 99 0 2 <
0.000
1
0.32
Gastro-
enterologists
20 4 80 105 96 0 2 <
0.000
1
0.013
Graduate
clinical officers
4 58
5
939 80 1 80
7
48 20 40 0.084
9
<
0.001
CO ENT 1 37
5
109 92 490 78 2 11 <
0.000
1
<
0.001
CO lungs and
skin
1 88
5
208 89 532 61 5 12 <
0.000
1
<
0.001
CO
ophthalmology/
cataract
surgery
1 08
0
90 92 338 73 2 8 <
0.000
1
<
0.001
Co pediatrics 1 39
5
135 90 552 76 3 12 <
0.000
<
0.001
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH WORKFORCE PLAN, CASE STUDY OF KENYA 8
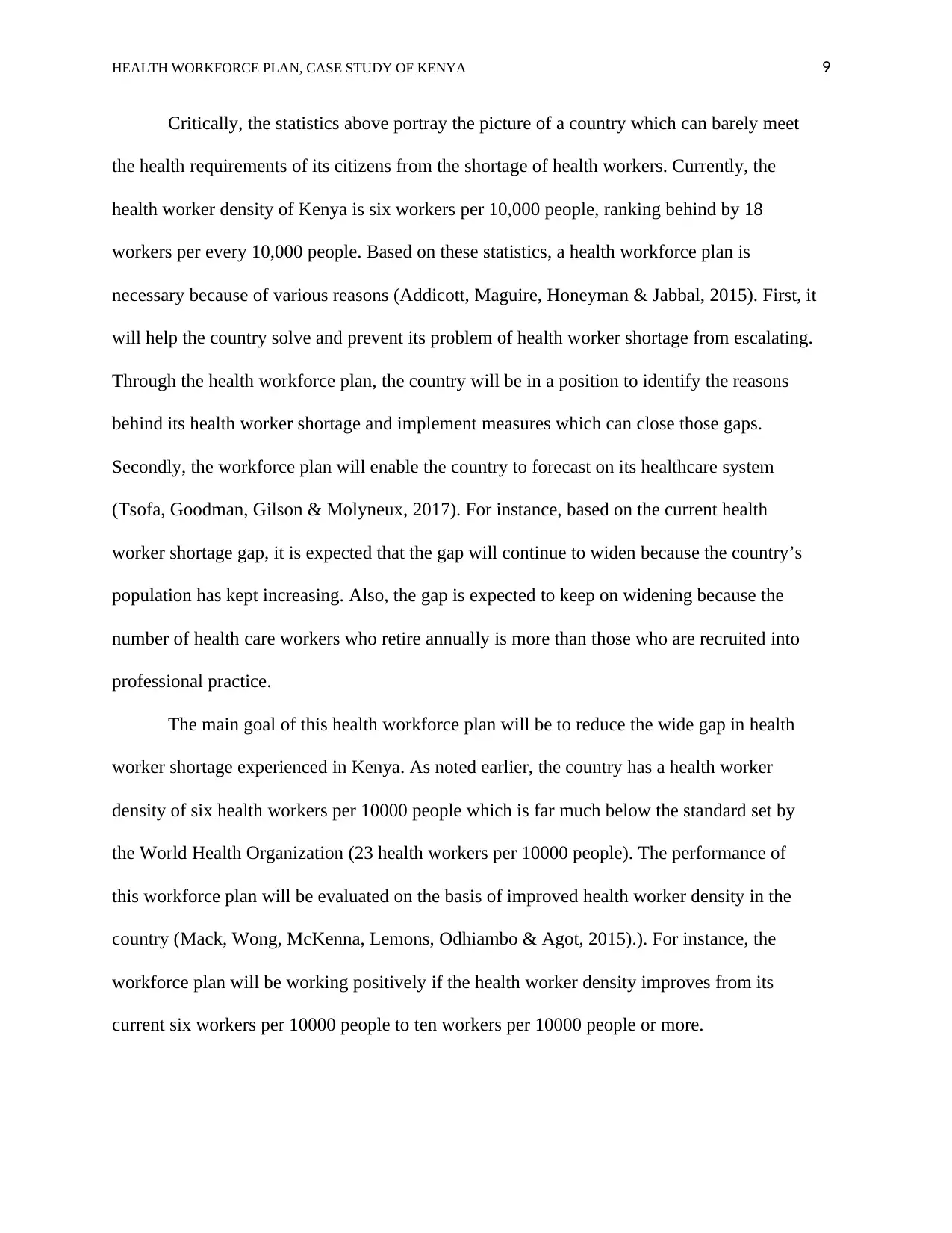
The training needs assessment report table showing the gap of health workforce
specialists in Kenya
46 counties
analyzed
Tota
l
stan
dard
num
ber
Total
emplo
yment
Perc
ent
shor
tage
by
stan
dard
Tot
al
idea
l
nu
mbe
r
Perc
ent
shor
tage
by
ideal
Mea
n of
empl
oyed
staff
per
coun
ty
Ide
al
me
an
per
cou
nty
t test P
value
[comp
aring
emplo
yed
with
ideal]
t test P
value
[comp
are
emplo
yed
with
standa
rds]
1
Anesthetist
nurses
1 63
0
61 96 696 91 1 15 <
0.000
1
<
0.001
Accident and
emergency care
nurses
2 75
0
13 100 482 97 0 10 <
0.000
1
<
0.001
BSN nurses 1 18
0
1 189 −1 2 42
6
51 26 54 0.022
5
0.990
5
KRCHN 41 7
32
8 612 79 21 6
35
60 17 494 <
0.000
1
<
0.001
Community
public health
nurses
(KECHN)
77 5
44
796 99 1 61
1
51 47 66 0.608
4
<
0.001
Cardiology
nurses
20 0 100 483 100 0 10 <
0.000
1
0.000
6
Total
nationally
282
525
43 612 85 115
264
62
The training needs assessment report table showing the gap of health workforce
specialists in Kenya
46 counties
analyzed
Tota
l
stan
dard
num
ber
Total
emplo
yment
Perc
ent
shor
tage
by
stan
dard
Tot
al
idea
l
nu
mbe
r
Perc
ent
shor
tage
by
ideal
Mea
n of
empl
oyed
staff
per
coun
ty
Ide
al
me
an
per
cou
nty
t test P
value
[comp
aring
emplo
yed
with
ideal]
t test P
value
[comp
are
emplo
yed
with
standa
rds]
1
Anesthetist
nurses
1 63
0
61 96 696 91 1 15 <
0.000
1
<
0.001
Accident and
emergency care
nurses
2 75
0
13 100 482 97 0 10 <
0.000
1
<
0.001
BSN nurses 1 18
0
1 189 −1 2 42
6
51 26 54 0.022
5
0.990
5
KRCHN 41 7
32
8 612 79 21 6
35
60 17 494 <
0.000
1
<
0.001
Community
public health
nurses
(KECHN)
77 5
44
796 99 1 61
1
51 47 66 0.608
4
<
0.001
Cardiology
nurses
20 0 100 483 100 0 10 <
0.000
1
0.000
6
Total
nationally
282
525
43 612 85 115
264
62
HEALTH WORKFORCE PLAN, CASE STUDY OF KENYA 9
Critically, the statistics above portray the picture of a country which can barely meet
the health requirements of its citizens from the shortage of health workers. Currently, the
health worker density of Kenya is six workers per 10,000 people, ranking behind by 18
workers per every 10,000 people. Based on these statistics, a health workforce plan is
necessary because of various reasons (Addicott, Maguire, Honeyman & Jabbal, 2015). First, it
will help the country solve and prevent its problem of health worker shortage from escalating.
Through the health workforce plan, the country will be in a position to identify the reasons
behind its health worker shortage and implement measures which can close those gaps.
Secondly, the workforce plan will enable the country to forecast on its healthcare system
(Tsofa, Goodman, Gilson & Molyneux, 2017). For instance, based on the current health
worker shortage gap, it is expected that the gap will continue to widen because the country’s
population has kept increasing. Also, the gap is expected to keep on widening because the
number of health care workers who retire annually is more than those who are recruited into
professional practice.
The main goal of this health workforce plan will be to reduce the wide gap in health
worker shortage experienced in Kenya. As noted earlier, the country has a health worker
density of six health workers per 10000 people which is far much below the standard set by
the World Health Organization (23 health workers per 10000 people). The performance of
this workforce plan will be evaluated on the basis of improved health worker density in the
country (Mack, Wong, McKenna, Lemons, Odhiambo & Agot, 2015).). For instance, the
workforce plan will be working positively if the health worker density improves from its
current six workers per 10000 people to ten workers per 10000 people or more.
Critically, the statistics above portray the picture of a country which can barely meet
the health requirements of its citizens from the shortage of health workers. Currently, the
health worker density of Kenya is six workers per 10,000 people, ranking behind by 18
workers per every 10,000 people. Based on these statistics, a health workforce plan is
necessary because of various reasons (Addicott, Maguire, Honeyman & Jabbal, 2015). First, it
will help the country solve and prevent its problem of health worker shortage from escalating.
Through the health workforce plan, the country will be in a position to identify the reasons
behind its health worker shortage and implement measures which can close those gaps.
Secondly, the workforce plan will enable the country to forecast on its healthcare system
(Tsofa, Goodman, Gilson & Molyneux, 2017). For instance, based on the current health
worker shortage gap, it is expected that the gap will continue to widen because the country’s
population has kept increasing. Also, the gap is expected to keep on widening because the
number of health care workers who retire annually is more than those who are recruited into
professional practice.
The main goal of this health workforce plan will be to reduce the wide gap in health
worker shortage experienced in Kenya. As noted earlier, the country has a health worker
density of six health workers per 10000 people which is far much below the standard set by
the World Health Organization (23 health workers per 10000 people). The performance of
this workforce plan will be evaluated on the basis of improved health worker density in the
country (Mack, Wong, McKenna, Lemons, Odhiambo & Agot, 2015).). For instance, the
workforce plan will be working positively if the health worker density improves from its
current six workers per 10000 people to ten workers per 10000 people or more.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTH WORKFORCE PLAN, CASE STUDY OF KENYA 10
In a report drafted in 2013, the government of Kenya stipulated its strategic objective
to increase health worker density from five workers per 10000 people to seven workers per
10000 people in 2016. The number was significantly improved to six per 10000 as reported
by another report in 2016. Measures which were put in place to achieve that included, scaling
up the recruitment of health workers, reviewing the salaries and benefits according to health
care workers and strengthening the human resource policies and practices (Miseda, Were,
Murianki, Mutuku & Mutwiwa, 2017). However, the health worker density in Kenya has
remained low, leading to a re-enactment of the same strategic objective in order to see the
density improve further. This strategic objective will strengthen and promote the workforce
plan by providing a favorable environment which can help alleviate the gap in the health
sector of the country. The workforce will focus on encouraging enrollment of more health
professional students in the country’s universities, colleges and tertiary institutions (Peter,
Rose & Carol, 2018).
External Environment
Health workers shortage has proved to be a global challenge, even among the
developed countries like the United States. However, proper strategies have enabled those
countries to overcome the problem. For instance, a report by the U.S census data indicated
that the country’s senior population will continue to experience unprecedented growth in the
years to come. This is in consideration of its aging population. According to the report,
growth of senior population and the rise of insured people under the Affordable Care Act is
expected to pose opportunities as well as challenges on the health sector of the country
(World Health Organization, 2016). The demand for healthcare services within the country is
In a report drafted in 2013, the government of Kenya stipulated its strategic objective
to increase health worker density from five workers per 10000 people to seven workers per
10000 people in 2016. The number was significantly improved to six per 10000 as reported
by another report in 2016. Measures which were put in place to achieve that included, scaling
up the recruitment of health workers, reviewing the salaries and benefits according to health
care workers and strengthening the human resource policies and practices (Miseda, Were,
Murianki, Mutuku & Mutwiwa, 2017). However, the health worker density in Kenya has
remained low, leading to a re-enactment of the same strategic objective in order to see the
density improve further. This strategic objective will strengthen and promote the workforce
plan by providing a favorable environment which can help alleviate the gap in the health
sector of the country. The workforce will focus on encouraging enrollment of more health
professional students in the country’s universities, colleges and tertiary institutions (Peter,
Rose & Carol, 2018).
External Environment
Health workers shortage has proved to be a global challenge, even among the
developed countries like the United States. However, proper strategies have enabled those
countries to overcome the problem. For instance, a report by the U.S census data indicated
that the country’s senior population will continue to experience unprecedented growth in the
years to come. This is in consideration of its aging population. According to the report,
growth of senior population and the rise of insured people under the Affordable Care Act is
expected to pose opportunities as well as challenges on the health sector of the country
(World Health Organization, 2016). The demand for healthcare services within the country is
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTH WORKFORCE PLAN, CASE STUDY OF KENYA 11
expected to surpass the available healthcare workforce and hence the country has proactively
continued to plan for its future health demands.
To close the gap, the US has outlined several steps to take towards healthcare
workforce planning to ensure that the country is well equipped to withstand the changes and
health worker challenges in its healthcare sector. For instance, the country has invested in
education programs such as Medicare and Medicaid programs by subsidizing them to
encourage enrollment of more healthcare practitioners (World Health Organization, 2018).
However, despite the efforts to come up with a sustainable health workforce, the country has
continued to face challenges. The American Hospital Association Committee on Performance
Improvement identified that rural communities continue to face the challenge of providing
education and training on potential healthcare practitioners and recruiting healthcare
professionals. Also, educational pipeline and partnership between academic and medical
institutions have not been strengthened.
Internal Environment
Currently, Kenya has enough institutions which can produce enough healthcare
practitioners in the future. Unlike before when the only institutions where healthcare training
could be done were the universities, several medical training colleges have been established
across the whole country. This implies that the country has the capability of recruiting
medical practitioners required for its health sector (Were, Jere, Lanyo, Mburu, Kiriinya,
Waudo & Rodgers, 2019). Also, the government has come up with initiatives such as
universal health care which are aimed at ensuring that all citizens receive healthcare services
regardless of their social economic backgrounds. Such initiatives have encouraged many
students to enroll in learning institutions to pursue nursing professions. However, it has
expected to surpass the available healthcare workforce and hence the country has proactively
continued to plan for its future health demands.
To close the gap, the US has outlined several steps to take towards healthcare
workforce planning to ensure that the country is well equipped to withstand the changes and
health worker challenges in its healthcare sector. For instance, the country has invested in
education programs such as Medicare and Medicaid programs by subsidizing them to
encourage enrollment of more healthcare practitioners (World Health Organization, 2018).
However, despite the efforts to come up with a sustainable health workforce, the country has
continued to face challenges. The American Hospital Association Committee on Performance
Improvement identified that rural communities continue to face the challenge of providing
education and training on potential healthcare practitioners and recruiting healthcare
professionals. Also, educational pipeline and partnership between academic and medical
institutions have not been strengthened.
Internal Environment
Currently, Kenya has enough institutions which can produce enough healthcare
practitioners in the future. Unlike before when the only institutions where healthcare training
could be done were the universities, several medical training colleges have been established
across the whole country. This implies that the country has the capability of recruiting
medical practitioners required for its health sector (Were, Jere, Lanyo, Mburu, Kiriinya,
Waudo & Rodgers, 2019). Also, the government has come up with initiatives such as
universal health care which are aimed at ensuring that all citizens receive healthcare services
regardless of their social economic backgrounds. Such initiatives have encouraged many
students to enroll in learning institutions to pursue nursing professions. However, it has
HEALTH WORKFORCE PLAN, CASE STUDY OF KENYA 12
remained a challenge for many who would wish to pursue health professionals because
institutions are offering those courses at a very high cost when compared to other courses
such as business (Sander, Holtzman, Pauly & Cohn, 2015). Health care workers are also
underpaid in the country and that has discouraged many potential health students from
pursuing health-related courses at the learning institutions.
The Current Health Workforce Profile in Kenya
As identified in the sub-section above, currently Kenya has enough institutions which
can accommodate the potential health professionals it requires as a country. This is in
consideration of the fact that apart from its universities, medical training colleges have been
launched almost in all its counties. Also, the number of students who qualify to pursue health-
related professionals is enough to fill the positions in those institutions (Fort, Mwarey,
Mbindyo & Yang, 2015).). However, for those institutions to be in a position to accommodate
the number of potential health practitioners required to fill the shortage gap in the country’s
healthcare sector, enough facilities to facilitate the training of those students will be required.
Enough lecturers and tutors will also be required in order to accommodate the high intake of
medical students on those institutions. This raises the concern on the ability of those
institutions financially to support a large number of medical students. Also, the cost of
acquiring a degree or a diploma in the country is high to an extent that most of the potential
students cannot afford (Siyam, Diallo, Lopes, & Campbell, 2019).
In addition, Kenya is among the countries whose nursing practitioners are underpaid
and that has discouraged many potential healthcare students from pursuing healthcare related
courses. The Kenyan government should, therefore, channel more funds to improve the
learning institutions which offer medical related courses in the sector such as laboratories and
remained a challenge for many who would wish to pursue health professionals because
institutions are offering those courses at a very high cost when compared to other courses
such as business (Sander, Holtzman, Pauly & Cohn, 2015). Health care workers are also
underpaid in the country and that has discouraged many potential health students from
pursuing health-related courses at the learning institutions.
The Current Health Workforce Profile in Kenya
As identified in the sub-section above, currently Kenya has enough institutions which
can accommodate the potential health professionals it requires as a country. This is in
consideration of the fact that apart from its universities, medical training colleges have been
launched almost in all its counties. Also, the number of students who qualify to pursue health-
related professionals is enough to fill the positions in those institutions (Fort, Mwarey,
Mbindyo & Yang, 2015).). However, for those institutions to be in a position to accommodate
the number of potential health practitioners required to fill the shortage gap in the country’s
healthcare sector, enough facilities to facilitate the training of those students will be required.
Enough lecturers and tutors will also be required in order to accommodate the high intake of
medical students on those institutions. This raises the concern on the ability of those
institutions financially to support a large number of medical students. Also, the cost of
acquiring a degree or a diploma in the country is high to an extent that most of the potential
students cannot afford (Siyam, Diallo, Lopes, & Campbell, 2019).
In addition, Kenya is among the countries whose nursing practitioners are underpaid
and that has discouraged many potential healthcare students from pursuing healthcare related
courses. The Kenyan government should, therefore, channel more funds to improve the
learning institutions which offer medical related courses in the sector such as laboratories and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 19
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





