Detailed Health Workforce Plan for Kenya: 2024 Analysis and Report
VerifiedAdded on 2022/11/17
|16
|3503
|360
Report
AI Summary
This report provides a detailed health workforce plan for Kenya, examining the country's healthcare system and workforce dynamics. It begins with an environmental scan, covering population characteristics, geographical regions, political and economic statuses, and the overall health context. The report then delves into the health workforce profile, including stakeholders, healthcare worker numbers, and ratios, highlighting critical issues such as uneven distribution and the impact of devolution. Recommendations are provided to address these challenges and improve the healthcare system. The report emphasizes the need for strategic planning to ensure an adequate, well-distributed, and well-supported health workforce to meet the needs of the Kenyan population. The report also highlights challenges in workforce distribution, the impact of devolution on healthcare workers, and proposes strategies to address these issues. The report is designed to inform policymakers, donors, researchers, and other stakeholders in the healthcare sector.

Running head: Health Workforce Planning 1
Health workforce Plan for Kenya 2024
(Author’s name)
(Institutional Affiliation)
Health workforce Plan for Kenya 2024
(Author’s name)
(Institutional Affiliation)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Health Workforce Planning 2
Table of Contents
Introduction......................................................................................................................................3
Environmental Scan.........................................................................................................................4
Population characteristics and geographical region....................................................................4
Political system............................................................................................................................5
Economic status...........................................................................................................................5
Health contest and status.............................................................................................................6
Health Systems............................................................................................................................6
Health Work Force Profile...............................................................................................................7
The Stakeholders.........................................................................................................................7
Health care workers numbers and ratio in Kenya........................................................................8
Other health workforce vital Statistics........................................................................................9
Critical issues.................................................................................................................................10
Recommendations..........................................................................................................................12
References......................................................................................................................................14
Table of Contents
Introduction......................................................................................................................................3
Environmental Scan.........................................................................................................................4
Population characteristics and geographical region....................................................................4
Political system............................................................................................................................5
Economic status...........................................................................................................................5
Health contest and status.............................................................................................................6
Health Systems............................................................................................................................6
Health Work Force Profile...............................................................................................................7
The Stakeholders.........................................................................................................................7
Health care workers numbers and ratio in Kenya........................................................................8
Other health workforce vital Statistics........................................................................................9
Critical issues.................................................................................................................................10
Recommendations..........................................................................................................................12
References......................................................................................................................................14
Health Workforce Planning 3
Introduction
The health workforce of a country simply means the actual number of medical care
providers offering medical services. According to the World Health Organization (WHO) 2013
report there are four major pillars on which determines the country’s health workforce. These are
having enough number of professionals in health care in regard to country’s cercus, even
distribution of health care providers and infrastructure based on, time of operation, accessibility
and the costs incurred in health care delivery either directly or indirectly(Campbell et al., 2013).
Another determinant of the health care system of a country is acceptability and quality of
services based on trained professionals, level of competency and continuity in
education(Tackling NCDs: the capacity of countries to respond, n.d.). The availability,
accessibility, and distribution of health workers at any particular time show the level of medical
services in a given country based on the recommended WHO medical workers to population
ratio and therefore giving the recommended health care for every citizen(MOH, 2013). There are
conditions that will determine the amount of the health workforce which constitute not less than
the following; change in population and demographics, policies, death and morbidity percentage,
the burden brought about by ailments and other related factors will have an influence on the
demand for medical services(WHO, 2016).
Therefore, in order for any country to avoid inconveniences brought about by healthcare
systems, it must come up with strategic plans on the healthcare workforce(Miseda, Were,
Murianki, Mutuku, & Mutwiwa, 2017). This plan will help determine the number of health
workers, the gap existing, how the development is done, how monitoring and implementation of
strategies in the health systems need to be carried out, control and management, improvement in
quality and policies needed to improve healthcare. A good health workforce plan should consider
Introduction
The health workforce of a country simply means the actual number of medical care
providers offering medical services. According to the World Health Organization (WHO) 2013
report there are four major pillars on which determines the country’s health workforce. These are
having enough number of professionals in health care in regard to country’s cercus, even
distribution of health care providers and infrastructure based on, time of operation, accessibility
and the costs incurred in health care delivery either directly or indirectly(Campbell et al., 2013).
Another determinant of the health care system of a country is acceptability and quality of
services based on trained professionals, level of competency and continuity in
education(Tackling NCDs: the capacity of countries to respond, n.d.). The availability,
accessibility, and distribution of health workers at any particular time show the level of medical
services in a given country based on the recommended WHO medical workers to population
ratio and therefore giving the recommended health care for every citizen(MOH, 2013). There are
conditions that will determine the amount of the health workforce which constitute not less than
the following; change in population and demographics, policies, death and morbidity percentage,
the burden brought about by ailments and other related factors will have an influence on the
demand for medical services(WHO, 2016).
Therefore, in order for any country to avoid inconveniences brought about by healthcare
systems, it must come up with strategic plans on the healthcare workforce(Miseda, Were,
Murianki, Mutuku, & Mutwiwa, 2017). This plan will help determine the number of health
workers, the gap existing, how the development is done, how monitoring and implementation of
strategies in the health systems need to be carried out, control and management, improvement in
quality and policies needed to improve healthcare. A good health workforce plan should consider
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Health Workforce Planning 4
the situational assessment needed by policymakers, donors, researchers, regulators, and world
financial institutions in order to enhance improvement in healthcare planning(Al-Sawai & Al-
Shishtawy, 2015). This study intends to provide a comprehensive health workforce plan for
Kenya. Kenya has been chosen for this assignment as the country is among the low middle-
income nations according to WHO statistic report of 2016. In this study, the environmental scan
on healthcare in Kenya, profile for the health workforce, critical issues arising, recommendations
will be provided.
Environmental Scan
Population characteristics and geographical region
Kenya is located on the Eastern part of Africa along the equator. It has around 43 ethnic
groups with Bantu subgroups forming the majority of the tribes, followed by the Kenyan
Highland Nilotes, Cushites, Plain Nilotes and Liver Lake Nilotes(HEALTH SITUATION, 2018).
The country has an area of around six thousand square kilometers. It contains seven geographical
regions and 47 counties. It has a coastline of around 540 kilometers on the shores of the Indian
Ocean. Kenya is bordered by Somalia, Ethiopia, South Sudan, Uganda, and Tanzania. Kenyan
Census put its population at around 47,681,779 people by 2016(Achoki et al., 2019). Out of this,
men accounted for 50% while the rest were women. The projections put the live birth rate at
5000 births daily while the mortality rate was 1200 deaths each day. Due to increase in
population, there will a likely reduction in the number of workforces in healthcare workers thus
increasing the demand for the health workforce(Muga, Kizito, Mbayah, & Gakuruh, 2018).
Kenya has an average population of around 69 individuals per square kilometers, 70 years in
expected average lifespan and a fertility rate of 5.0. In addition to this, the crude birth rate is put
at 35.8.
the situational assessment needed by policymakers, donors, researchers, regulators, and world
financial institutions in order to enhance improvement in healthcare planning(Al-Sawai & Al-
Shishtawy, 2015). This study intends to provide a comprehensive health workforce plan for
Kenya. Kenya has been chosen for this assignment as the country is among the low middle-
income nations according to WHO statistic report of 2016. In this study, the environmental scan
on healthcare in Kenya, profile for the health workforce, critical issues arising, recommendations
will be provided.
Environmental Scan
Population characteristics and geographical region
Kenya is located on the Eastern part of Africa along the equator. It has around 43 ethnic
groups with Bantu subgroups forming the majority of the tribes, followed by the Kenyan
Highland Nilotes, Cushites, Plain Nilotes and Liver Lake Nilotes(HEALTH SITUATION, 2018).
The country has an area of around six thousand square kilometers. It contains seven geographical
regions and 47 counties. It has a coastline of around 540 kilometers on the shores of the Indian
Ocean. Kenya is bordered by Somalia, Ethiopia, South Sudan, Uganda, and Tanzania. Kenyan
Census put its population at around 47,681,779 people by 2016(Achoki et al., 2019). Out of this,
men accounted for 50% while the rest were women. The projections put the live birth rate at
5000 births daily while the mortality rate was 1200 deaths each day. Due to increase in
population, there will a likely reduction in the number of workforces in healthcare workers thus
increasing the demand for the health workforce(Muga, Kizito, Mbayah, & Gakuruh, 2018).
Kenya has an average population of around 69 individuals per square kilometers, 70 years in
expected average lifespan and a fertility rate of 5.0. In addition to this, the crude birth rate is put
at 35.8.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Health Workforce Planning 5
Political system
The new constitution which came in place in 2010, changed the system of governance in
Kenya from purely central government to a mix of the central government and devolved
government in the 47 counties(Daniel, 2016). The central government consists of three arms
namely the executive, the legislature which consists of the Senate and the National Assembly
and the judiciary. The devolved part of government consists of governors each heading a county.
The devolvement of health sector has given county governments the responsibility of regulating
healthcare facilities, hiring and regulating all healthcare workers, for instance, the doctors,
nurses, clinical officers, laboratory technicians, and other professionals(Daniel, 2016). In
addition to this, counties are mandated with the regulation of ambulance services, pharmaceutical
services, and private health facilities that are within the county. County governments are also
responsible for the recruitment and retention of all healthcare workers in addition to the
distribution of health resources(“WHO | Kenya,” 2019).
Economic status
According to the World Bank report of 2015, with collaboration with the Ministry of
Finance, Kenya GDP was about KSH 7,000,000 in 2015(WHO, 2017). However, most of its
budgetary allocation in Kenya is used in the devolution process, Ministry of Trade, Ministry of
Education, central government current expenditure, Ministry of Defense and Internal Affairs,
The Ministry of Energy, Ministry of Transport, Ministry of Agriculture and lastly the Ministry
of Health sector having being allocated the least amount(WHO, 2017). The health sector was
given a budgetary allocation of about KSH 70 billion equivalent to 3.6% of the total budget in
the fiscal year of 2017/2018(WHO, 2017).
Political system
The new constitution which came in place in 2010, changed the system of governance in
Kenya from purely central government to a mix of the central government and devolved
government in the 47 counties(Daniel, 2016). The central government consists of three arms
namely the executive, the legislature which consists of the Senate and the National Assembly
and the judiciary. The devolved part of government consists of governors each heading a county.
The devolvement of health sector has given county governments the responsibility of regulating
healthcare facilities, hiring and regulating all healthcare workers, for instance, the doctors,
nurses, clinical officers, laboratory technicians, and other professionals(Daniel, 2016). In
addition to this, counties are mandated with the regulation of ambulance services, pharmaceutical
services, and private health facilities that are within the county. County governments are also
responsible for the recruitment and retention of all healthcare workers in addition to the
distribution of health resources(“WHO | Kenya,” 2019).
Economic status
According to the World Bank report of 2015, with collaboration with the Ministry of
Finance, Kenya GDP was about KSH 7,000,000 in 2015(WHO, 2017). However, most of its
budgetary allocation in Kenya is used in the devolution process, Ministry of Trade, Ministry of
Education, central government current expenditure, Ministry of Defense and Internal Affairs,
The Ministry of Energy, Ministry of Transport, Ministry of Agriculture and lastly the Ministry
of Health sector having being allocated the least amount(WHO, 2017). The health sector was
given a budgetary allocation of about KSH 70 billion equivalent to 3.6% of the total budget in
the fiscal year of 2017/2018(WHO, 2017).
Health Workforce Planning 6
Health contest and status
Life expectancy in Kenya was recorded to be around 62.8 years, the crude birth rate of
35.0 for every 1000 individual and fertility rate at about 5.0 per woman. Kenya has around 63 %
of the population who have access to clean water(WHO, 2018). The communicable and non-
communicable diseases contributed to the high burden of disease in addition to violence and
injuries. The high mortality rate and morbidity rate was brought about by major ailments like
HIV/AIDS, respiratory diseases, tuberculosis, and pregnancy complications(MOH, 2013).
HIV/AIDs, tuberculosis and malaria are the major communicable diseases affecting most of the
people in Kenya. However, the incidence rates of HIV/AIDs have reduced over the past
decade(UNICEF, 2018).
Health Systems
The Kenya Health Policy 2014-2030 guides the existing system in health care. It spells
out government intentions in providing high-quality services according to the law of the land and
guided by Vision 2030(Muga et al., 2018). The national government and county government
have a role in the administration of the Kenyan health system. The roles played by the national
government include financing, education, standards, and quality assurance, policy-making and
port health management, managing referral hospitals, administration of health care agencies on a
national level and medical professionals in the named departments(Muga et al., 2018). The
county government is responsible for county health facilities, public health, ambulance services,
surveillance, disaster mitigation, and waste disposal. The county government is also responsible
for the hiring of health care providers.
The private sectors facilitate a large percentage in health services provision in Kenya.
However, unlike government public hospitals, private hospitals are not grouped into levels by the
Kenya health care systems(KENYA MINISTRY OF HEALTH, 2015). Christian affiliated health
Health contest and status
Life expectancy in Kenya was recorded to be around 62.8 years, the crude birth rate of
35.0 for every 1000 individual and fertility rate at about 5.0 per woman. Kenya has around 63 %
of the population who have access to clean water(WHO, 2018). The communicable and non-
communicable diseases contributed to the high burden of disease in addition to violence and
injuries. The high mortality rate and morbidity rate was brought about by major ailments like
HIV/AIDS, respiratory diseases, tuberculosis, and pregnancy complications(MOH, 2013).
HIV/AIDs, tuberculosis and malaria are the major communicable diseases affecting most of the
people in Kenya. However, the incidence rates of HIV/AIDs have reduced over the past
decade(UNICEF, 2018).
Health Systems
The Kenya Health Policy 2014-2030 guides the existing system in health care. It spells
out government intentions in providing high-quality services according to the law of the land and
guided by Vision 2030(Muga et al., 2018). The national government and county government
have a role in the administration of the Kenyan health system. The roles played by the national
government include financing, education, standards, and quality assurance, policy-making and
port health management, managing referral hospitals, administration of health care agencies on a
national level and medical professionals in the named departments(Muga et al., 2018). The
county government is responsible for county health facilities, public health, ambulance services,
surveillance, disaster mitigation, and waste disposal. The county government is also responsible
for the hiring of health care providers.
The private sectors facilitate a large percentage in health services provision in Kenya.
However, unlike government public hospitals, private hospitals are not grouped into levels by the
Kenya health care systems(KENYA MINISTRY OF HEALTH, 2015). Christian affiliated health
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Health Workforce Planning 7
institution in Kenya are highly respected with some receiving government services. Hospitals in
Kenya are grouped into six levels depending on the type of care provided namely, level 1-
Community level services, level 2-Dispensaries, level 3- Health centers, level 4- District referral
hospitals, level 5- Provincial referral hospitals and last level which is level 6- National referral
hospitals(Muga et al., 2018). The funding of the health care system in Kenya primarily come
from both public and non-government sources. Public sources include government allocation,
loans, donations, grants, and mandatory insurance schemes. The private source, on the other
hand, includes direct funding, insurance companies, donors, loans, and international banks and
finance institutions(“WHO | Kenya,” 2019). The burden of disease determines the amount of
finance is allocated. Professional organizations register and control human resource in the health
sector.
Health Work Force Profile
The Stakeholders
In Kenya, the majority of health care providers include nurses, dentists, doctors,
pharmacists, clinical officers, medical laboratory technicians and practitioners, occupational
health personnel, community health workers and traditional medicines and herbalist
environmental and public health officers and technicians, and nutritionists and diabetics(WHO,
2017). Other than that, mostly in healthcare facilities and government administrative centers
including the County Commissioners Offices, health care workers work with security officers,
ambulance personnel, administrative officers, health communication and records officers,
subordinate staff and health district commissioners(Muga et al., 2018). In addition, Kenya
institution in Kenya are highly respected with some receiving government services. Hospitals in
Kenya are grouped into six levels depending on the type of care provided namely, level 1-
Community level services, level 2-Dispensaries, level 3- Health centers, level 4- District referral
hospitals, level 5- Provincial referral hospitals and last level which is level 6- National referral
hospitals(Muga et al., 2018). The funding of the health care system in Kenya primarily come
from both public and non-government sources. Public sources include government allocation,
loans, donations, grants, and mandatory insurance schemes. The private source, on the other
hand, includes direct funding, insurance companies, donors, loans, and international banks and
finance institutions(“WHO | Kenya,” 2019). The burden of disease determines the amount of
finance is allocated. Professional organizations register and control human resource in the health
sector.
Health Work Force Profile
The Stakeholders
In Kenya, the majority of health care providers include nurses, dentists, doctors,
pharmacists, clinical officers, medical laboratory technicians and practitioners, occupational
health personnel, community health workers and traditional medicines and herbalist
environmental and public health officers and technicians, and nutritionists and diabetics(WHO,
2017). Other than that, mostly in healthcare facilities and government administrative centers
including the County Commissioners Offices, health care workers work with security officers,
ambulance personnel, administrative officers, health communication and records officers,
subordinate staff and health district commissioners(Muga et al., 2018). In addition, Kenya
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Health Workforce Planning 8
medical workforce highly involves Research organizations including Kenya Research Institute,
international and domestic donors, Kenya Red Cross, International Monitory Fund, the World
Bank, non-governmental institutions, private sectors and highly the government of Kenya. Major
stakeholders from the government of Kenya include Kenya training institution including the
Kenya Medical Colleges and Universities, Ministry of Health, Ministry of Finance, National
Medical Boards, Ministry of Education and Salary and Remuneration Committee(Achoki et al.,
2019). Among other major stakeholders in Kenyan, health workforce includes the training
students who constitute about 30% of day to day working individuals in most of the Kenyan
public health system (Kenya Ministry of Health, 2015).
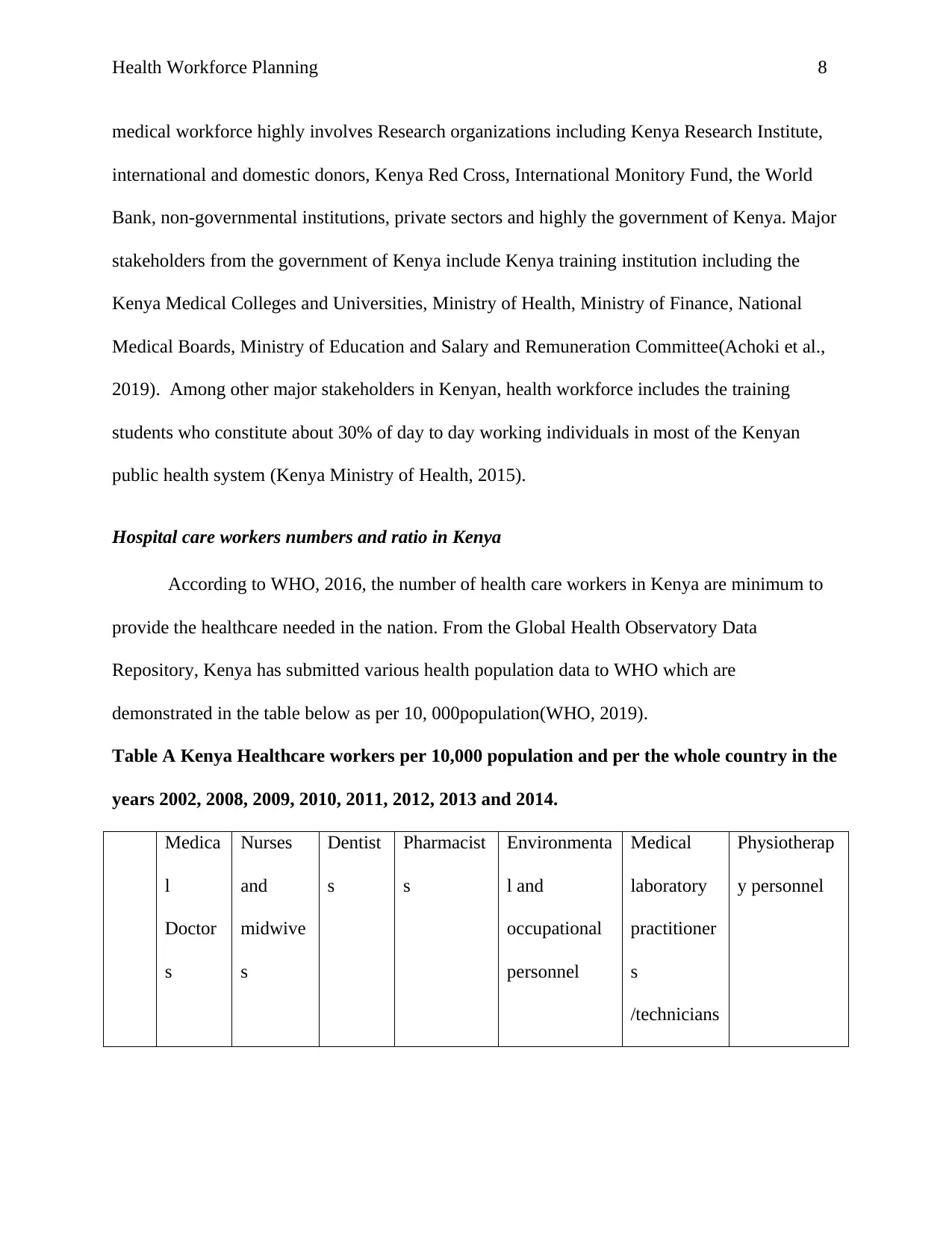
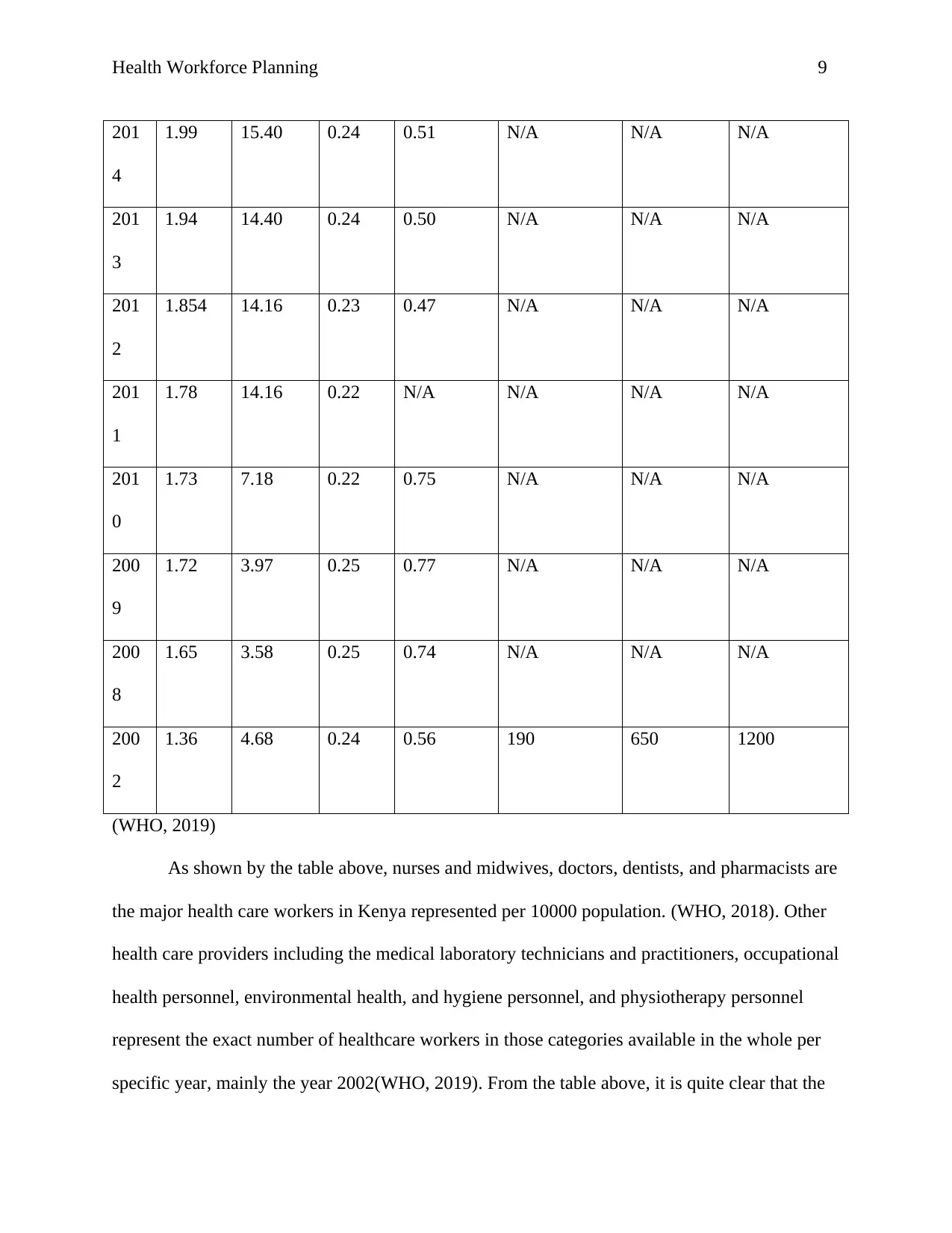
Hospital care workers numbers and ratio in Kenya
According to WHO, 2016, the number of health care workers in Kenya are minimum to
provide the healthcare needed in the nation. From the Global Health Observatory Data
Repository, Kenya has submitted various health population data to WHO which are
demonstrated in the table below as per 10, 000population(WHO, 2019).
Table A Kenya Healthcare workers per 10,000 population and per the whole country in the
years 2002, 2008, 2009, 2010, 2011, 2012, 2013 and 2014.
Medica
l
Doctor
s
Nurses
and
midwive
s
Dentist
s
Pharmacist
s
Environmenta
l and
occupational
personnel
Medical
laboratory
practitioner
s
/technicians
Physiotherap
y personnel
medical workforce highly involves Research organizations including Kenya Research Institute,
international and domestic donors, Kenya Red Cross, International Monitory Fund, the World
Bank, non-governmental institutions, private sectors and highly the government of Kenya. Major
stakeholders from the government of Kenya include Kenya training institution including the
Kenya Medical Colleges and Universities, Ministry of Health, Ministry of Finance, National
Medical Boards, Ministry of Education and Salary and Remuneration Committee(Achoki et al.,
2019). Among other major stakeholders in Kenyan, health workforce includes the training
students who constitute about 30% of day to day working individuals in most of the Kenyan
public health system (Kenya Ministry of Health, 2015).
Hospital care workers numbers and ratio in Kenya
According to WHO, 2016, the number of health care workers in Kenya are minimum to
provide the healthcare needed in the nation. From the Global Health Observatory Data
Repository, Kenya has submitted various health population data to WHO which are
demonstrated in the table below as per 10, 000population(WHO, 2019).
Table A Kenya Healthcare workers per 10,000 population and per the whole country in the
years 2002, 2008, 2009, 2010, 2011, 2012, 2013 and 2014.
Medica
l
Doctor
s
Nurses
and
midwive
s
Dentist
s
Pharmacist
s
Environmenta
l and
occupational
personnel
Medical
laboratory
practitioner
s
/technicians
Physiotherap
y personnel
Health Workforce Planning 9
201
4
1.99 15.40 0.24 0.51 N/A N/A N/A
201
3
1.94 14.40 0.24 0.50 N/A N/A N/A
201
2
1.854 14.16 0.23 0.47 N/A N/A N/A
201
1
1.78 14.16 0.22 N/A N/A N/A N/A
201
0
1.73 7.18 0.22 0.75 N/A N/A N/A
200
9
1.72 3.97 0.25 0.77 N/A N/A N/A
200
8
1.65 3.58 0.25 0.74 N/A N/A N/A
200
2
1.36 4.68 0.24 0.56 190 650 1200
(WHO, 2019)
As shown by the table above, nurses and midwives, doctors, dentists, and pharmacists are
the major health care workers in Kenya represented per 10000 population. (WHO, 2018). Other
health care providers including the medical laboratory technicians and practitioners, occupational
health personnel, environmental health, and hygiene personnel, and physiotherapy personnel
represent the exact number of healthcare workers in those categories available in the whole per
specific year, mainly the year 2002(WHO, 2019). From the table above, it is quite clear that the
201
4
1.99 15.40 0.24 0.51 N/A N/A N/A
201
3
1.94 14.40 0.24 0.50 N/A N/A N/A
201
2
1.854 14.16 0.23 0.47 N/A N/A N/A
201
1
1.78 14.16 0.22 N/A N/A N/A N/A
201
0
1.73 7.18 0.22 0.75 N/A N/A N/A
200
9
1.72 3.97 0.25 0.77 N/A N/A N/A
200
8
1.65 3.58 0.25 0.74 N/A N/A N/A
200
2
1.36 4.68 0.24 0.56 190 650 1200
(WHO, 2019)
As shown by the table above, nurses and midwives, doctors, dentists, and pharmacists are
the major health care workers in Kenya represented per 10000 population. (WHO, 2018). Other
health care providers including the medical laboratory technicians and practitioners, occupational
health personnel, environmental health, and hygiene personnel, and physiotherapy personnel
represent the exact number of healthcare workers in those categories available in the whole per
specific year, mainly the year 2002(WHO, 2019). From the table above, it is quite clear that the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Health Workforce Planning 10
nation has a deficit of healthcare workers and specifically, there are no registered herbalists,
complementary medicine personnel and traditional medicine men
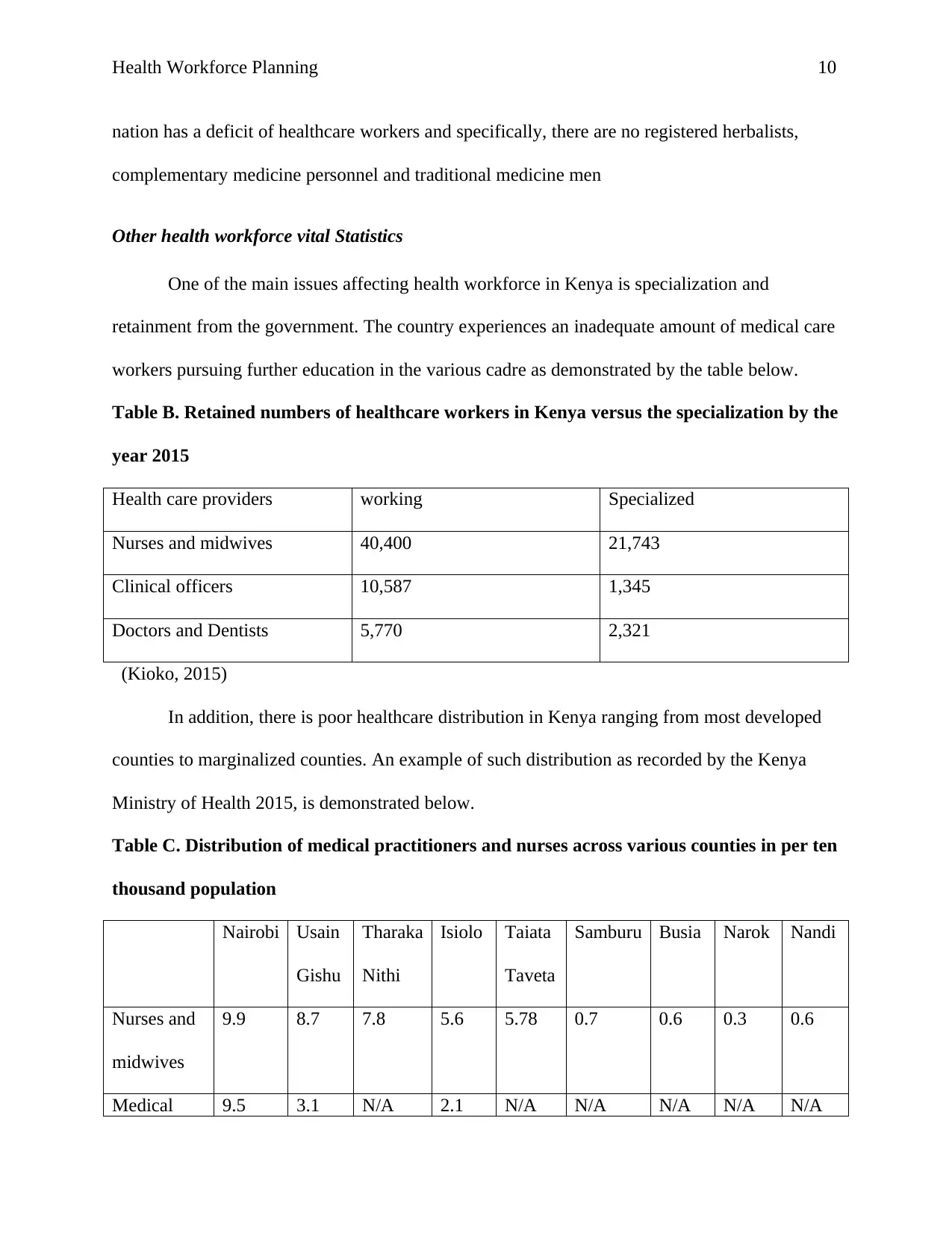
Other health workforce vital Statistics
One of the main issues affecting health workforce in Kenya is specialization and
retainment from the government. The country experiences an inadequate amount of medical care
workers pursuing further education in the various cadre as demonstrated by the table below.
Table B. Retained numbers of healthcare workers in Kenya versus the specialization by the
year 2015
Health care providers working Specialized
Nurses and midwives 40,400 21,743
Clinical officers 10,587 1,345
Doctors and Dentists 5,770 2,321
(Kioko, 2015)
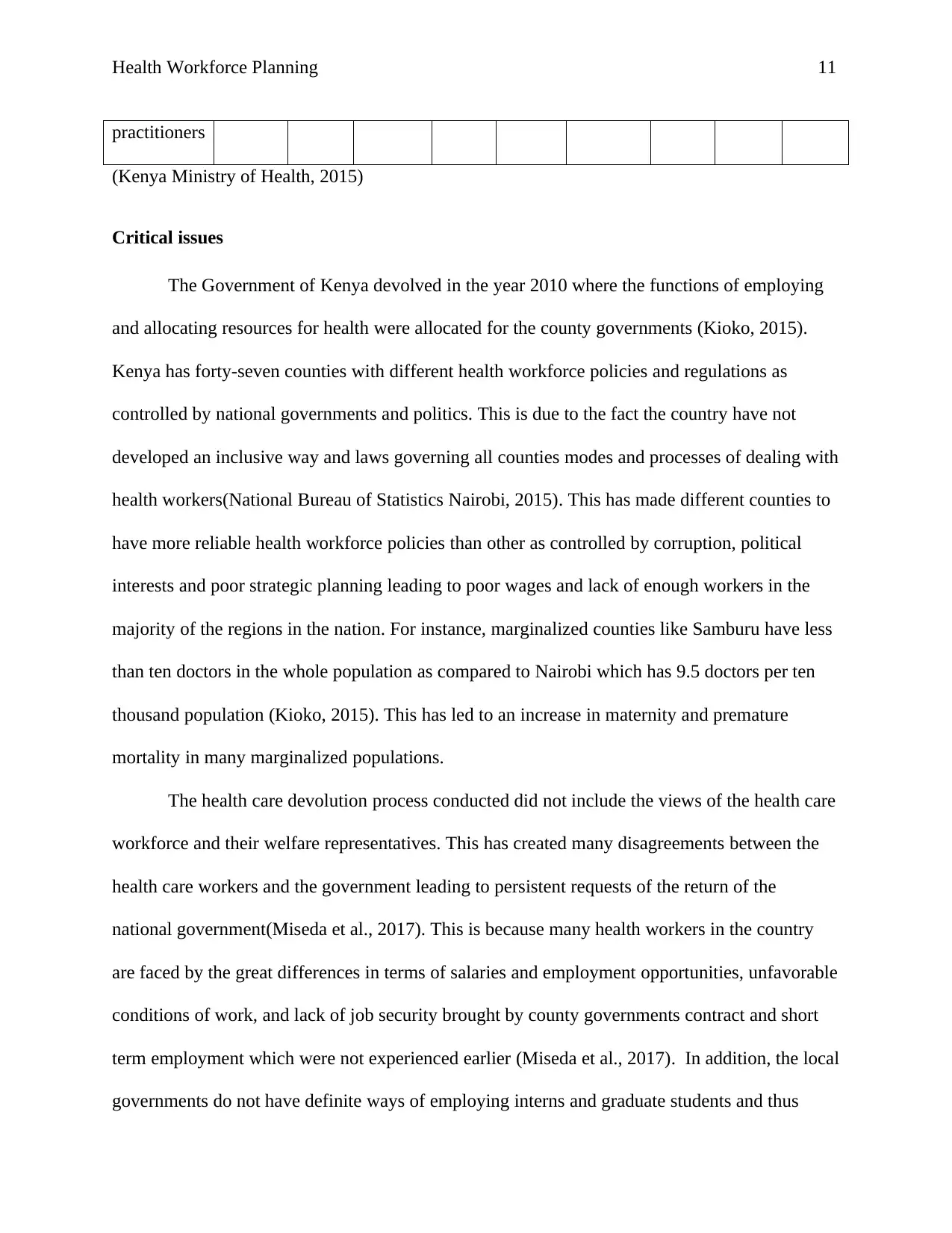
In addition, there is poor healthcare distribution in Kenya ranging from most developed
counties to marginalized counties. An example of such distribution as recorded by the Kenya
Ministry of Health 2015, is demonstrated below.
Table C. Distribution of medical practitioners and nurses across various counties in per ten
thousand population
Nairobi Usain
Gishu
Tharaka
Nithi
Isiolo Taiata
Taveta
Samburu Busia Narok Nandi
Nurses and
midwives
9.9 8.7 7.8 5.6 5.78 0.7 0.6 0.3 0.6
Medical 9.5 3.1 N/A 2.1 N/A N/A N/A N/A N/A
nation has a deficit of healthcare workers and specifically, there are no registered herbalists,
complementary medicine personnel and traditional medicine men
Other health workforce vital Statistics
One of the main issues affecting health workforce in Kenya is specialization and
retainment from the government. The country experiences an inadequate amount of medical care
workers pursuing further education in the various cadre as demonstrated by the table below.
Table B. Retained numbers of healthcare workers in Kenya versus the specialization by the
year 2015
Health care providers working Specialized
Nurses and midwives 40,400 21,743
Clinical officers 10,587 1,345
Doctors and Dentists 5,770 2,321
(Kioko, 2015)
In addition, there is poor healthcare distribution in Kenya ranging from most developed
counties to marginalized counties. An example of such distribution as recorded by the Kenya
Ministry of Health 2015, is demonstrated below.
Table C. Distribution of medical practitioners and nurses across various counties in per ten
thousand population
Nairobi Usain
Gishu
Tharaka
Nithi
Isiolo Taiata
Taveta
Samburu Busia Narok Nandi
Nurses and
midwives
9.9 8.7 7.8 5.6 5.78 0.7 0.6 0.3 0.6
Medical 9.5 3.1 N/A 2.1 N/A N/A N/A N/A N/A
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Health Workforce Planning 11
practitioners
(Kenya Ministry of Health, 2015)
Critical issues
The Government of Kenya devolved in the year 2010 where the functions of employing
and allocating resources for health were allocated for the county governments (Kioko, 2015).
Kenya has forty-seven counties with different health workforce policies and regulations as
controlled by national governments and politics. This is due to the fact the country have not
developed an inclusive way and laws governing all counties modes and processes of dealing with
health workers(National Bureau of Statistics Nairobi, 2015). This has made different counties to
have more reliable health workforce policies than other as controlled by corruption, political
interests and poor strategic planning leading to poor wages and lack of enough workers in the
majority of the regions in the nation. For instance, marginalized counties like Samburu have less
than ten doctors in the whole population as compared to Nairobi which has 9.5 doctors per ten
thousand population (Kioko, 2015). This has led to an increase in maternity and premature
mortality in many marginalized populations.
The health care devolution process conducted did not include the views of the health care
workforce and their welfare representatives. This has created many disagreements between the
health care workers and the government leading to persistent requests of the return of the
national government(Miseda et al., 2017). This is because many health workers in the country
are faced by the great differences in terms of salaries and employment opportunities, unfavorable
conditions of work, and lack of job security brought by county governments contract and short
term employment which were not experienced earlier (Miseda et al., 2017). In addition, the local
governments do not have definite ways of employing interns and graduate students and thus
practitioners
(Kenya Ministry of Health, 2015)
Critical issues
The Government of Kenya devolved in the year 2010 where the functions of employing
and allocating resources for health were allocated for the county governments (Kioko, 2015).
Kenya has forty-seven counties with different health workforce policies and regulations as
controlled by national governments and politics. This is due to the fact the country have not
developed an inclusive way and laws governing all counties modes and processes of dealing with
health workers(National Bureau of Statistics Nairobi, 2015). This has made different counties to
have more reliable health workforce policies than other as controlled by corruption, political
interests and poor strategic planning leading to poor wages and lack of enough workers in the
majority of the regions in the nation. For instance, marginalized counties like Samburu have less
than ten doctors in the whole population as compared to Nairobi which has 9.5 doctors per ten
thousand population (Kioko, 2015). This has led to an increase in maternity and premature
mortality in many marginalized populations.
The health care devolution process conducted did not include the views of the health care
workforce and their welfare representatives. This has created many disagreements between the
health care workers and the government leading to persistent requests of the return of the
national government(Miseda et al., 2017). This is because many health workers in the country
are faced by the great differences in terms of salaries and employment opportunities, unfavorable
conditions of work, and lack of job security brought by county governments contract and short
term employment which were not experienced earlier (Miseda et al., 2017). In addition, the local
governments do not have definite ways of employing interns and graduate students and thus
Health Workforce Planning 12
leading to work overload for working employers. Many health employers have been moving
overseas in search for better pay and some quitting jobs leading to decrease in a number of health
care workers as little or less are replaced (Miseda et al., 2017). However, the government of
Kenya with the collaboration with health care workers unions have recently been reviewing
Kenya health workforce plan in order to accomplish universal heal care for all and meet Kenya
Vision 2030 goals.
One of the major challenges affecting the Kenya health workforce is the collaboration
between health care workers unions welfares organizations, the national government, and the
county governments(HEALTH SITUATION, 2018). Despite so much persistent complaints and
poor working conditions by health care workers, little have been done over the time the
devolution processes began. This is due to the fact that the country is overwhelmed with much
corruption and political interests by county governments leading to little or no implementation of
nationally provided health workforce strategies( Kioko, 2015). In addition, there is a lack of
accountability, education, better women and youth representation and knowledge along with the
head of local governments. Other than that, health financing in Kenya is always allocate the
minimal budget as compared with other sectors. In the 2015/2016 fiscal year, the finance
allocated for health care was around three percent of the total budget making many county
governors to blame the Ministry of Finance and other political leaders for poor healthcare in
Kenya.
Recommendations
From the data health profile and the critical issues, Kenya surely needs to work on its
health workforce strategies. One of the most key elements that need to be addressed is
cooperation and partnership across all major and affiliated stakeholders related to health
leading to work overload for working employers. Many health employers have been moving
overseas in search for better pay and some quitting jobs leading to decrease in a number of health
care workers as little or less are replaced (Miseda et al., 2017). However, the government of
Kenya with the collaboration with health care workers unions have recently been reviewing
Kenya health workforce plan in order to accomplish universal heal care for all and meet Kenya
Vision 2030 goals.
One of the major challenges affecting the Kenya health workforce is the collaboration
between health care workers unions welfares organizations, the national government, and the
county governments(HEALTH SITUATION, 2018). Despite so much persistent complaints and
poor working conditions by health care workers, little have been done over the time the
devolution processes began. This is due to the fact that the country is overwhelmed with much
corruption and political interests by county governments leading to little or no implementation of
nationally provided health workforce strategies( Kioko, 2015). In addition, there is a lack of
accountability, education, better women and youth representation and knowledge along with the
head of local governments. Other than that, health financing in Kenya is always allocate the
minimal budget as compared with other sectors. In the 2015/2016 fiscal year, the finance
allocated for health care was around three percent of the total budget making many county
governors to blame the Ministry of Finance and other political leaders for poor healthcare in
Kenya.
Recommendations
From the data health profile and the critical issues, Kenya surely needs to work on its
health workforce strategies. One of the most key elements that need to be addressed is
cooperation and partnership across all major and affiliated stakeholders related to health
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





