Comprehensive Discharge Plan for Angelo: Healthcare Report & Analysis
VerifiedAdded on 2021/04/16
|19
|4954
|141
Report
AI Summary
This report details the discharge plan for Angelo, focusing on his diagnosis of Lewy body dementia, hypertension, and hyperlipidaemia. It emphasizes a patient-centered approach, incorporating his medical and social history, and the involvement of a multidisciplinary team (MDT). The plan addresses potential complications, medication management, and the need for long-term care, including activities of daily living (ADL). The report highlights the importance of effective communication among stakeholders, patient empowerment, and clinical referrals to prevent hospital readmissions. It also considers the challenges associated with managing symptoms and the need for a supportive environment to ensure Angelo's well-being and successful transition back into the community. The report follows the Nursing and Midwifery Council's professional code of conduct and adheres to data protection guidelines.
Discharge Plan
1
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction :
In this essay, discharge planning of Angelo will be discussed. In planning and practicing
discharge for Angelo, different aspects like his medical and social history, also current
medical condition will be considered. Multidisciplinary team (MDT) will be incorporated in
his discharge planning and Angelo and his family members will be encouraged to actively
participate in the discharge planning. Coordination among all the stakeholders can be
effectively maintained through communication. Exact condition of the Angelo will be
considered and also possible complications also will be considered while designing discharge
plan. Smooth transition of Angelo to the society can be achieved by providing holistic care by
incorporating interventions for physical, physiological, pathological and psychological
condition of Angelo. Requirements of Angelo and his family members will be considered and
preference will be given to fulfil these requirements. Family members of Angelo should be
informed about all the aspects of Angelo. These aspects include, medical condition of
Angelo, diagnosis, schedule of medication administration, adherence to medication and
nutritional requirements of Angelo. Discharge planning for Angelo will be planned and
executed according to Nursing and Midwifery Council's (NMC) professional code of conduct
(2015). All the information related to Angelo will be kept confidential according to
guidelines of Data Protection Act (1998). Discharge planning foe Angelo should be initiated
since he got admitted to the hospital. Based on the, health status of Angelo discharge
planning can be changed to provide effective discharge to Angelo. Family members should
be educated about the care to be taken at the home. Prior to discharge, it should be sure that
Angelo is with improved medical condition and all the requirements for the discharge are
fulfilled. Continued care after discharge should be arranged for Angelo after discharge from
the hospital. Prepared discharge plan for Angelo should be person centred (Heath et al., 2015;
Orlu-Gul et al., 2014).
During preparation of discharge plan, patient should be assessed based on the current health
status and potential complications. Based on the assessment, some of the patients require
simple discharge plan. On the other hand, few patients require complex discharge plan.
Angelo requires complex discharge plan because he is associated with multiple health issues
like hypertension, hyperlipidaemia and Lewy body dementia. LBD patients are associated
with symptoms like visual hallucination, movement disorder, poor regulation of body
functions, cognitive problems, sleep difficulties and depression. Hence, Angelo should be
provided with care from multiple professionals like doctors, nurses, occupational therapist,
2
In this essay, discharge planning of Angelo will be discussed. In planning and practicing
discharge for Angelo, different aspects like his medical and social history, also current
medical condition will be considered. Multidisciplinary team (MDT) will be incorporated in
his discharge planning and Angelo and his family members will be encouraged to actively
participate in the discharge planning. Coordination among all the stakeholders can be
effectively maintained through communication. Exact condition of the Angelo will be
considered and also possible complications also will be considered while designing discharge
plan. Smooth transition of Angelo to the society can be achieved by providing holistic care by
incorporating interventions for physical, physiological, pathological and psychological
condition of Angelo. Requirements of Angelo and his family members will be considered and
preference will be given to fulfil these requirements. Family members of Angelo should be
informed about all the aspects of Angelo. These aspects include, medical condition of
Angelo, diagnosis, schedule of medication administration, adherence to medication and
nutritional requirements of Angelo. Discharge planning for Angelo will be planned and
executed according to Nursing and Midwifery Council's (NMC) professional code of conduct
(2015). All the information related to Angelo will be kept confidential according to
guidelines of Data Protection Act (1998). Discharge planning foe Angelo should be initiated
since he got admitted to the hospital. Based on the, health status of Angelo discharge
planning can be changed to provide effective discharge to Angelo. Family members should
be educated about the care to be taken at the home. Prior to discharge, it should be sure that
Angelo is with improved medical condition and all the requirements for the discharge are
fulfilled. Continued care after discharge should be arranged for Angelo after discharge from
the hospital. Prepared discharge plan for Angelo should be person centred (Heath et al., 2015;
Orlu-Gul et al., 2014).
During preparation of discharge plan, patient should be assessed based on the current health
status and potential complications. Based on the assessment, some of the patients require
simple discharge plan. On the other hand, few patients require complex discharge plan.
Angelo requires complex discharge plan because he is associated with multiple health issues
like hypertension, hyperlipidaemia and Lewy body dementia. LBD patients are associated
with symptoms like visual hallucination, movement disorder, poor regulation of body
functions, cognitive problems, sleep difficulties and depression. Hence, Angelo should be
provided with care from multiple professionals like doctors, nurses, occupational therapist,
2
dietician and social worker. (Tochimoto et al., 2015). Anxiety in the Angelo can be reduced
by minimizing sensory stimulation. Angelo is going to be discharged from the hospital after
diagnosis of Lewy body dementia. Lewy body dementia is a pathological condition in which
there is deposition of alpha-synuclein proteins in the brain which are called as Lewy bodies.
It leads to problems in thinking, movement, behaviour, and mood. Lewy body dementia
patients exhibits progressive decline in the physical and mental abilities. These patients also
exhibit mental disturbance like hallucination, alteration in alertness and attention. (Kosaka,
2016). Angelo received all the necessary care, exhibiting acceptable discharge and exhibiting
satisfactory progress (Heenan and Birrell, 2017).
NMC Code of Professional Conduct (2015) 2.3 was followed for the enabling independence
and empowerment of Angelo. Due to this Angelo can participate in decision making for
treatment and care. Social support should be provided for Angelo to maintain his dignity and
to improve his morale (see table 1) (Burnard et al., 2004). Discharge planner should make an
account that antipsychotic drugs are not going to be helpful for LBD patients and should
make discharge planning accordingly after consultation with neurologist. Healthcare
providers should follow evidence-based information for care of Angelo and this information
should be shared with his family members. Evidence based information related to
unresponsiveness of antipsychotic drugs for LBD patients need to be provided to family
members (Boot et al., 2013). This information can be helpful in educating Angelo’s family
members. It is evident that, LBD patients can experience emergency situations like drastic
decrease in functioning and unfavourable behaviour. Hence, Angelo and his family members
should be educated with education use, food and medicine allergies and health insurance.
Even though caregiver and discharge planner need to provide person centred care to Angelo,
they need to be professional while providing care and preparing discharge plan. They need to
leave behind emotions while preparing discharge plan for Angelo. In LBD patients there
might be unacceptable behaviour and due to this behaviour care provider might have changed
perception about Angelo. Care provider should not take into account this emotional change
about Angelo while providing care to him (see table 2) (Raymond et al., 2014).
Assessment of mental condition is an important aspect in the patients with LBD patients.
Assessment can be performed by performing objective test. This can be useful in assessing
different tasks. MDT comprising of nurse, doctor, care manager, occupational therapist,
psychotherapist and discharge co-coordinators should work in coordination for effective
discharge of Angelo (see table 1) (Day et al., 2009). Discharge planning incorporates multiple
3
by minimizing sensory stimulation. Angelo is going to be discharged from the hospital after
diagnosis of Lewy body dementia. Lewy body dementia is a pathological condition in which
there is deposition of alpha-synuclein proteins in the brain which are called as Lewy bodies.
It leads to problems in thinking, movement, behaviour, and mood. Lewy body dementia
patients exhibits progressive decline in the physical and mental abilities. These patients also
exhibit mental disturbance like hallucination, alteration in alertness and attention. (Kosaka,
2016). Angelo received all the necessary care, exhibiting acceptable discharge and exhibiting
satisfactory progress (Heenan and Birrell, 2017).
NMC Code of Professional Conduct (2015) 2.3 was followed for the enabling independence
and empowerment of Angelo. Due to this Angelo can participate in decision making for
treatment and care. Social support should be provided for Angelo to maintain his dignity and
to improve his morale (see table 1) (Burnard et al., 2004). Discharge planner should make an
account that antipsychotic drugs are not going to be helpful for LBD patients and should
make discharge planning accordingly after consultation with neurologist. Healthcare
providers should follow evidence-based information for care of Angelo and this information
should be shared with his family members. Evidence based information related to
unresponsiveness of antipsychotic drugs for LBD patients need to be provided to family
members (Boot et al., 2013). This information can be helpful in educating Angelo’s family
members. It is evident that, LBD patients can experience emergency situations like drastic
decrease in functioning and unfavourable behaviour. Hence, Angelo and his family members
should be educated with education use, food and medicine allergies and health insurance.
Even though caregiver and discharge planner need to provide person centred care to Angelo,
they need to be professional while providing care and preparing discharge plan. They need to
leave behind emotions while preparing discharge plan for Angelo. In LBD patients there
might be unacceptable behaviour and due to this behaviour care provider might have changed
perception about Angelo. Care provider should not take into account this emotional change
about Angelo while providing care to him (see table 2) (Raymond et al., 2014).
Assessment of mental condition is an important aspect in the patients with LBD patients.
Assessment can be performed by performing objective test. This can be useful in assessing
different tasks. MDT comprising of nurse, doctor, care manager, occupational therapist,
psychotherapist and discharge co-coordinators should work in coordination for effective
discharge of Angelo (see table 1) (Day et al., 2009). Discharge planning incorporates multiple
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
stakeholders and effective communication among all the stakeholders is very important.
Effective communication among different stakeholders can be helpful for smooth and safe
discharge of Angelo. Effective communication among different stakeholders of MDT team
can be helpful in precise decision making. MDT should communicate with Angelo and
family members and enforce them to participate in the decision making (Pethybridge, 2004).
There can be impairment of communication in patients with dementia. Hence, special tools
need to be developed and implemented for communication in LOB patients. Communication
can be also be helpful in the educating Angelo and his family members about his health
condition. Angelo is claiming that he is experiencing presence of genomes. However, care
providers and psychiatrics should educate him that it is only hallucination due to his confused
state. As such, there would not be existence of such genomes. Other than Lewy body
dementia, Angelo is also suffering through hypertension and hyperlipidaemia. For these
health issues, he need to consume medicine consistently for the longer duration. Discharge
planner should make sure that he would consume medicines regularly by arranging stay of
nurse at his home (see table 2).
Patient participation is an important aspect in discharge planning because it can be helpful in
safe transition to society, improving patient fulfilment and lessening risk of readmissions.
Discharge planner should co-ordinate with Angelo and his family to improve their
participation in the discharge planning (Pearce, 2016). For providing holistic care for Angelo
in the regular basis his medical and social needs to be identified. By providing holistic care to
Angelo, his well-being can be effectively improved.
Long-term care (LTC) should be considered for Angelo because he is associated with
multiple conditions like hypertension, hyperlipidaemia and Lewy body dementia. LTC care
for patients usually decided based on the medical and social requirements of the individual
patients. Medical and social care to Angelo can be effectively provided by LTC. Activities of
daily living (ADL) should be incorporated in LTC of Angelo. Support for ADL to dress,
toilet use bath, to groom and to eat should be extended to Angelo. LTC in the form of ADL
can be helpful for Angelo to remain healthy, to improve wellbeing and to protect from
injuries because Angelo is being prone to fall (see table 2). LBD can produce slowed
reflexes, impaired reasoning and heightened risk-taking ability. These are the reasons
responsible for fall and injury in LBD patients. Access to care in case of Angelo can be
improved by LTC. Access to care can be improved with the help of community groups and
family members (Holland et al., 2013). LBD patients are usually isolated from the society
4
Effective communication among different stakeholders can be helpful for smooth and safe
discharge of Angelo. Effective communication among different stakeholders of MDT team
can be helpful in precise decision making. MDT should communicate with Angelo and
family members and enforce them to participate in the decision making (Pethybridge, 2004).
There can be impairment of communication in patients with dementia. Hence, special tools
need to be developed and implemented for communication in LOB patients. Communication
can be also be helpful in the educating Angelo and his family members about his health
condition. Angelo is claiming that he is experiencing presence of genomes. However, care
providers and psychiatrics should educate him that it is only hallucination due to his confused
state. As such, there would not be existence of such genomes. Other than Lewy body
dementia, Angelo is also suffering through hypertension and hyperlipidaemia. For these
health issues, he need to consume medicine consistently for the longer duration. Discharge
planner should make sure that he would consume medicines regularly by arranging stay of
nurse at his home (see table 2).
Patient participation is an important aspect in discharge planning because it can be helpful in
safe transition to society, improving patient fulfilment and lessening risk of readmissions.
Discharge planner should co-ordinate with Angelo and his family to improve their
participation in the discharge planning (Pearce, 2016). For providing holistic care for Angelo
in the regular basis his medical and social needs to be identified. By providing holistic care to
Angelo, his well-being can be effectively improved.
Long-term care (LTC) should be considered for Angelo because he is associated with
multiple conditions like hypertension, hyperlipidaemia and Lewy body dementia. LTC care
for patients usually decided based on the medical and social requirements of the individual
patients. Medical and social care to Angelo can be effectively provided by LTC. Activities of
daily living (ADL) should be incorporated in LTC of Angelo. Support for ADL to dress,
toilet use bath, to groom and to eat should be extended to Angelo. LTC in the form of ADL
can be helpful for Angelo to remain healthy, to improve wellbeing and to protect from
injuries because Angelo is being prone to fall (see table 2). LBD can produce slowed
reflexes, impaired reasoning and heightened risk-taking ability. These are the reasons
responsible for fall and injury in LBD patients. Access to care in case of Angelo can be
improved by LTC. Access to care can be improved with the help of community groups and
family members (Holland et al., 2013). LBD patients are usually isolated from the society
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
and unable to perform their own tasks. Hence, LTC should be incorporated in the care of
LBD patients to help them in ADL and to improve access to care. Provision of care to LBD
patients is associated with multiple factors, hence these patients face problems in receiving
care for the longer duration. Providing intervention to LBD patient can be more complicated
due to its manifold symptoms. Healthcare professionals should focus on the symptoms which
can disturb Angelo prominently (McKeith et al., 2009).
There can be disagreement between healthcare provider and Angelo for the potential or actual
symptoms of LBD (Popejoy et al., 2012). Hallucination experience of Angelo might not be
acceptable for healthcare provider as the prominent symptom for Angelo. At the same time,
Angelo might get ore disturbed due to his hallucination. Conversely, healthcare provider
might be considering loss of memory and confusion as the prominent symptoms for Angelo.
In LTC, exaggerating symptoms in the LBD patients might change over the period of time.
Hence, there should be open and healthy discussion between Angelo and healthcare provider
to focus on the particular symptom. It is evident that in psychiatric conditions including LBD,
treatment of one symptom can exaggerate another symptom. LBD patients need to consume
neuroleptics. Due to consumption of neuroleptics, there might be behavioural changes on the
LBD patients. These behavioural changes might be unacceptable to other people. Hence, it is
advisable not to provide LTC to the LBD patients in the hospital facility. Hence, Hospital
authorities try to avoid hospitalisation of LBD patients for the longer duration. Hospital
authorities need to make arrangements for LTC at home for Angelo and approachability of
outside healthcare professionals should be improved for Angelo to avoid unnecessary
hospitalisation (Kramberger et al., 2017).
Outcome of the discharge planning can be effectively improved by effective coordination
among the stakeholders engaged in the discharge planning. Nurse need to coordinate both at
the shift change and at the time of discharge from the hospital. Discharge coordinators can
perform their duties by effective communication among all the members of MDT. Potential
date of discharge should be declared on or before hours of admission of Angelo to the
hospital. Though, it is not feasible always to declare date before 48 hours of admission
because patient’s health status and requirements need to be considered while deciding
discharge date. For each patient, there might be different condition. Discharge date is also
depending on the hospital authorities and hospital policy. (Zurlo and Zuliani, 2018). Early
decision on discharge planning can be helpful in preparing effective discharge plan and its
operative implementation. There are varied aspects responsible influencing date of discharge.
5
LBD patients to help them in ADL and to improve access to care. Provision of care to LBD
patients is associated with multiple factors, hence these patients face problems in receiving
care for the longer duration. Providing intervention to LBD patient can be more complicated
due to its manifold symptoms. Healthcare professionals should focus on the symptoms which
can disturb Angelo prominently (McKeith et al., 2009).
There can be disagreement between healthcare provider and Angelo for the potential or actual
symptoms of LBD (Popejoy et al., 2012). Hallucination experience of Angelo might not be
acceptable for healthcare provider as the prominent symptom for Angelo. At the same time,
Angelo might get ore disturbed due to his hallucination. Conversely, healthcare provider
might be considering loss of memory and confusion as the prominent symptoms for Angelo.
In LTC, exaggerating symptoms in the LBD patients might change over the period of time.
Hence, there should be open and healthy discussion between Angelo and healthcare provider
to focus on the particular symptom. It is evident that in psychiatric conditions including LBD,
treatment of one symptom can exaggerate another symptom. LBD patients need to consume
neuroleptics. Due to consumption of neuroleptics, there might be behavioural changes on the
LBD patients. These behavioural changes might be unacceptable to other people. Hence, it is
advisable not to provide LTC to the LBD patients in the hospital facility. Hence, Hospital
authorities try to avoid hospitalisation of LBD patients for the longer duration. Hospital
authorities need to make arrangements for LTC at home for Angelo and approachability of
outside healthcare professionals should be improved for Angelo to avoid unnecessary
hospitalisation (Kramberger et al., 2017).
Outcome of the discharge planning can be effectively improved by effective coordination
among the stakeholders engaged in the discharge planning. Nurse need to coordinate both at
the shift change and at the time of discharge from the hospital. Discharge coordinators can
perform their duties by effective communication among all the members of MDT. Potential
date of discharge should be declared on or before hours of admission of Angelo to the
hospital. Though, it is not feasible always to declare date before 48 hours of admission
because patient’s health status and requirements need to be considered while deciding
discharge date. For each patient, there might be different condition. Discharge date is also
depending on the hospital authorities and hospital policy. (Zurlo and Zuliani, 2018). Early
decision on discharge planning can be helpful in preparing effective discharge plan and its
operative implementation. There are varied aspects responsible influencing date of discharge.
5
These include hospital capability, progress of clinical intervention and patient’s requirements.
Clinical progress of Angelo should be reviewed on daily basis by implementing review,
action, progress (RAP). Clinical progress should be updated on daily basis to MDT and
Angelo and his family members (Mortenson and Bishop, 2016).
Discharge checklist can be used as effective tool to assess effective implementation of
discharge planning. Success in discharge panning reflects in reduced hospital readmissions.
Checklist reflects excellence of discharge planning. Hospital readmissions can be prevented
by providing information related to diagnosis and medication consumption to the Angelo and
his family members. Discharge co-ordinator should ensure that Angelo is approachable to GP
post discharge and gratified with the discharge process. Discharge co-ordinator should also
ensure that Angelo and his family members are empowered to participate in decision making
in discharge planning. Patient empowerment is necessary to fulfil patient’s expectations and
to resolve their challenges. Patient empowerment in the discharge planning can be improved
by incorporation of both social and medical stakeholders (Russell et al., 2014). Discharge
coordinator should be bringing effective communication among Angelo. MDT and social
workers to improve Angelo’s empowerment in the discharge planning. Clinical referrals
should be made for Angelo, so that he can independently visit these healthcare facilities and
avoid hospital readmissions (see table 2) (Shepperd et al., 2013).
Approximately 48 hours before discharge, discharge checklist should be ready for Angelo.
However, it is not always feasible to prepare checklist before 48 hours discharge due to
varied conditions for different patients. Discharge checklist should comprise of all the
medical, social and personal needs of Angelo. All the aspects related to planning stage, pre-
discharge and important facets of actual discharge should be incorporated in the discharge
checklist (Soong et al., 2013).
Conclusion:
In case of complex discharge process, discharge planning requires more attention. In case of
Angelo, discharge planning is a complex process due to his multiple disease condition.
Appropriate discharge for Angelo can be achieved by incorporation of MDT which comprises
of stakeholders from both medical and social filed. Since, he is associated with multiple
disease for the longer duration, LTC should be considered for him. Coordination and
communication among different stakeholders can be helpful in reducing readmissions to the
6
Clinical progress of Angelo should be reviewed on daily basis by implementing review,
action, progress (RAP). Clinical progress should be updated on daily basis to MDT and
Angelo and his family members (Mortenson and Bishop, 2016).
Discharge checklist can be used as effective tool to assess effective implementation of
discharge planning. Success in discharge panning reflects in reduced hospital readmissions.
Checklist reflects excellence of discharge planning. Hospital readmissions can be prevented
by providing information related to diagnosis and medication consumption to the Angelo and
his family members. Discharge co-ordinator should ensure that Angelo is approachable to GP
post discharge and gratified with the discharge process. Discharge co-ordinator should also
ensure that Angelo and his family members are empowered to participate in decision making
in discharge planning. Patient empowerment is necessary to fulfil patient’s expectations and
to resolve their challenges. Patient empowerment in the discharge planning can be improved
by incorporation of both social and medical stakeholders (Russell et al., 2014). Discharge
coordinator should be bringing effective communication among Angelo. MDT and social
workers to improve Angelo’s empowerment in the discharge planning. Clinical referrals
should be made for Angelo, so that he can independently visit these healthcare facilities and
avoid hospital readmissions (see table 2) (Shepperd et al., 2013).
Approximately 48 hours before discharge, discharge checklist should be ready for Angelo.
However, it is not always feasible to prepare checklist before 48 hours discharge due to
varied conditions for different patients. Discharge checklist should comprise of all the
medical, social and personal needs of Angelo. All the aspects related to planning stage, pre-
discharge and important facets of actual discharge should be incorporated in the discharge
checklist (Soong et al., 2013).
Conclusion:
In case of complex discharge process, discharge planning requires more attention. In case of
Angelo, discharge planning is a complex process due to his multiple disease condition.
Appropriate discharge for Angelo can be achieved by incorporation of MDT which comprises
of stakeholders from both medical and social filed. Since, he is associated with multiple
disease for the longer duration, LTC should be considered for him. Coordination and
communication among different stakeholders can be helpful in reducing readmissions to the
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
hospital. Appropriate discharge planning is necessary for empowerment of Angelo and
permanency of care.
7
permanency of care.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Reference:
Burnard, P., Christine, M. C., and Susan, S. (2004). Professional and Ethical Issues in
Nursing. Baillière Tindall.
Day, M.R., McCarthy,G., and Coffey, A. (2009) Discharge planning: the role of the discharge
co-ordinator. Nursing Older People, 21, (1), pp. 26-31
Greenhalgh, T. (2013). Primary Health Care: Theory and Practice. John Wiley & Sons.
Heenan, D., and Birrell, D. (2017). The Integration of Health and Social Care in the UK:
Policy and Practice. Macmillan International Higher Education.
Heath, H., Sturdy, D. and Cheesly, A. (2010) Discharge planning: A summary of the
Department of Health’s guidance Ready to go. Planning the discharge and the transfer of
patients from hospital and intermediate care. Harrow: RCN Publishing Company Ltd.
Holland, D.E, Knafl, G.J., and Bowles, K.H. (2013). Targeting hospitalised patients for early
discharge planning intervention. Journal of Clinical Nursing, 22(19-20), pp. 2696-703.
Housley, W. (2017). Interaction in Multidisciplinary Teams. Routledge.
Kramberger, M.G., Auestad, B., Garcia-Ptacek, S., et al. (2017). Long-Term Cognitive
Decline in Dementia with Lewy Bodies in a Large Multicenter, International Cohort. Journal
of Alzheimer's Disease, 57(3), pp. 787-795.
McKeith, I. (2009). Top cited papers in International Psychogeriatrics: 1. Long-term use of
rivastigmine in patients with dementia with Lewy bodies: an open-label trial. International
Psychogeriatrics, 21(1), pp. 5-6.
Mortenson, W.B., and Bishop, A.M. (2016). Discharge Criteria and Follow-Up Support for
Dementia Care Units. Journal of Applied Gerontology, 35(3), pp. 321-30.
Orlu-Gul, M., Raimi-Abraham, B., Jamieson, E., Wei, L., Murray, M., Stawarz, K.,
Stegemann, S., Tuleu, C. and Smith, F.J. (2014) Public engagement workshop: How to
improve medicines for older people?. International journal of pharmaceutics, 459(1), pp.65-
69.
Pethybridge, J. How team working influences discharge planning from hospital: a study of
four multi-disciplinary teams in an acute hospital in England. Journal of Interprofessional
Care, 18(1), pp. 29-41.
Pearce, L. (2016). Ease the path from acute to community. Nursing Standard, 30(22), pp. 8-9.
Popejoy, L.L., Galambos, C., Moylan, K., and Madsen, R. (2012). Challenges to hospital
discharge planning for older adults. Clinical Nursing Research, 21(4), 431-49.
Raymond, M., Warner, A., Davies, N., Nicholas, N., Manthorpe, I. (2014). Palliative and end
of life care for people with dementia: lessons for clinical commissioners. Primary Health
Care Research & Development, 15(4), pp. 406-17.
Russell, P., Hewage, U., and Thompson, C. (2014). Method for improving the quality of
discharge summaries written by a general medical team. Internal Medicine Journal, 44(3),
pp.298-301.
8
Burnard, P., Christine, M. C., and Susan, S. (2004). Professional and Ethical Issues in
Nursing. Baillière Tindall.
Day, M.R., McCarthy,G., and Coffey, A. (2009) Discharge planning: the role of the discharge
co-ordinator. Nursing Older People, 21, (1), pp. 26-31
Greenhalgh, T. (2013). Primary Health Care: Theory and Practice. John Wiley & Sons.
Heenan, D., and Birrell, D. (2017). The Integration of Health and Social Care in the UK:
Policy and Practice. Macmillan International Higher Education.
Heath, H., Sturdy, D. and Cheesly, A. (2010) Discharge planning: A summary of the
Department of Health’s guidance Ready to go. Planning the discharge and the transfer of
patients from hospital and intermediate care. Harrow: RCN Publishing Company Ltd.
Holland, D.E, Knafl, G.J., and Bowles, K.H. (2013). Targeting hospitalised patients for early
discharge planning intervention. Journal of Clinical Nursing, 22(19-20), pp. 2696-703.
Housley, W. (2017). Interaction in Multidisciplinary Teams. Routledge.
Kramberger, M.G., Auestad, B., Garcia-Ptacek, S., et al. (2017). Long-Term Cognitive
Decline in Dementia with Lewy Bodies in a Large Multicenter, International Cohort. Journal
of Alzheimer's Disease, 57(3), pp. 787-795.
McKeith, I. (2009). Top cited papers in International Psychogeriatrics: 1. Long-term use of
rivastigmine in patients with dementia with Lewy bodies: an open-label trial. International
Psychogeriatrics, 21(1), pp. 5-6.
Mortenson, W.B., and Bishop, A.M. (2016). Discharge Criteria and Follow-Up Support for
Dementia Care Units. Journal of Applied Gerontology, 35(3), pp. 321-30.
Orlu-Gul, M., Raimi-Abraham, B., Jamieson, E., Wei, L., Murray, M., Stawarz, K.,
Stegemann, S., Tuleu, C. and Smith, F.J. (2014) Public engagement workshop: How to
improve medicines for older people?. International journal of pharmaceutics, 459(1), pp.65-
69.
Pethybridge, J. How team working influences discharge planning from hospital: a study of
four multi-disciplinary teams in an acute hospital in England. Journal of Interprofessional
Care, 18(1), pp. 29-41.
Pearce, L. (2016). Ease the path from acute to community. Nursing Standard, 30(22), pp. 8-9.
Popejoy, L.L., Galambos, C., Moylan, K., and Madsen, R. (2012). Challenges to hospital
discharge planning for older adults. Clinical Nursing Research, 21(4), 431-49.
Raymond, M., Warner, A., Davies, N., Nicholas, N., Manthorpe, I. (2014). Palliative and end
of life care for people with dementia: lessons for clinical commissioners. Primary Health
Care Research & Development, 15(4), pp. 406-17.
Russell, P., Hewage, U., and Thompson, C. (2014). Method for improving the quality of
discharge summaries written by a general medical team. Internal Medicine Journal, 44(3),
pp.298-301.
8
Shepperd, S., Lannin, N.A., Clemson, L.M., et al. (2013). Discharge planning from hospital
to home. Cochrane Database of Systematic Reviews, 31, (1):CD000313. doi:
10.1002/14651858.CD000313.
Soong, C., Daub, S., Lee, J., et al. (2013). Development of a checklist of safe discharge
practices for hospital patients. Journal of Hospital Medicine, 8(8), 444-9.
Tochimoto, S., Kitamura, M., Hino, S., and Kitamura, T. (2015). Predictors of home
discharge among patients hospitalized for behavioural and psychological symptoms of
dementia. Psychogeriatrics, 15(4), pp. 248-54.
Whitworth, H.B., and Whitworth, J. (2010). A Caregiver's Guide to Lewy Body Dementia.
Demos Medical Publishing.
Zun, L.S. (2013). Behavioral Emergencies for the Emergency Physician. Cambridge
University Press.
Zurlo, A., and Zuliani, G. (2018). Management of care transition and hospital discharge.
Aging Clinical and Experimental Research, 30(3), pp. 263-270.
9
to home. Cochrane Database of Systematic Reviews, 31, (1):CD000313. doi:
10.1002/14651858.CD000313.
Soong, C., Daub, S., Lee, J., et al. (2013). Development of a checklist of safe discharge
practices for hospital patients. Journal of Hospital Medicine, 8(8), 444-9.
Tochimoto, S., Kitamura, M., Hino, S., and Kitamura, T. (2015). Predictors of home
discharge among patients hospitalized for behavioural and psychological symptoms of
dementia. Psychogeriatrics, 15(4), pp. 248-54.
Whitworth, H.B., and Whitworth, J. (2010). A Caregiver's Guide to Lewy Body Dementia.
Demos Medical Publishing.
Zun, L.S. (2013). Behavioral Emergencies for the Emergency Physician. Cambridge
University Press.
Zurlo, A., and Zuliani, G. (2018). Management of care transition and hospital discharge.
Aging Clinical and Experimental Research, 30(3), pp. 263-270.
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
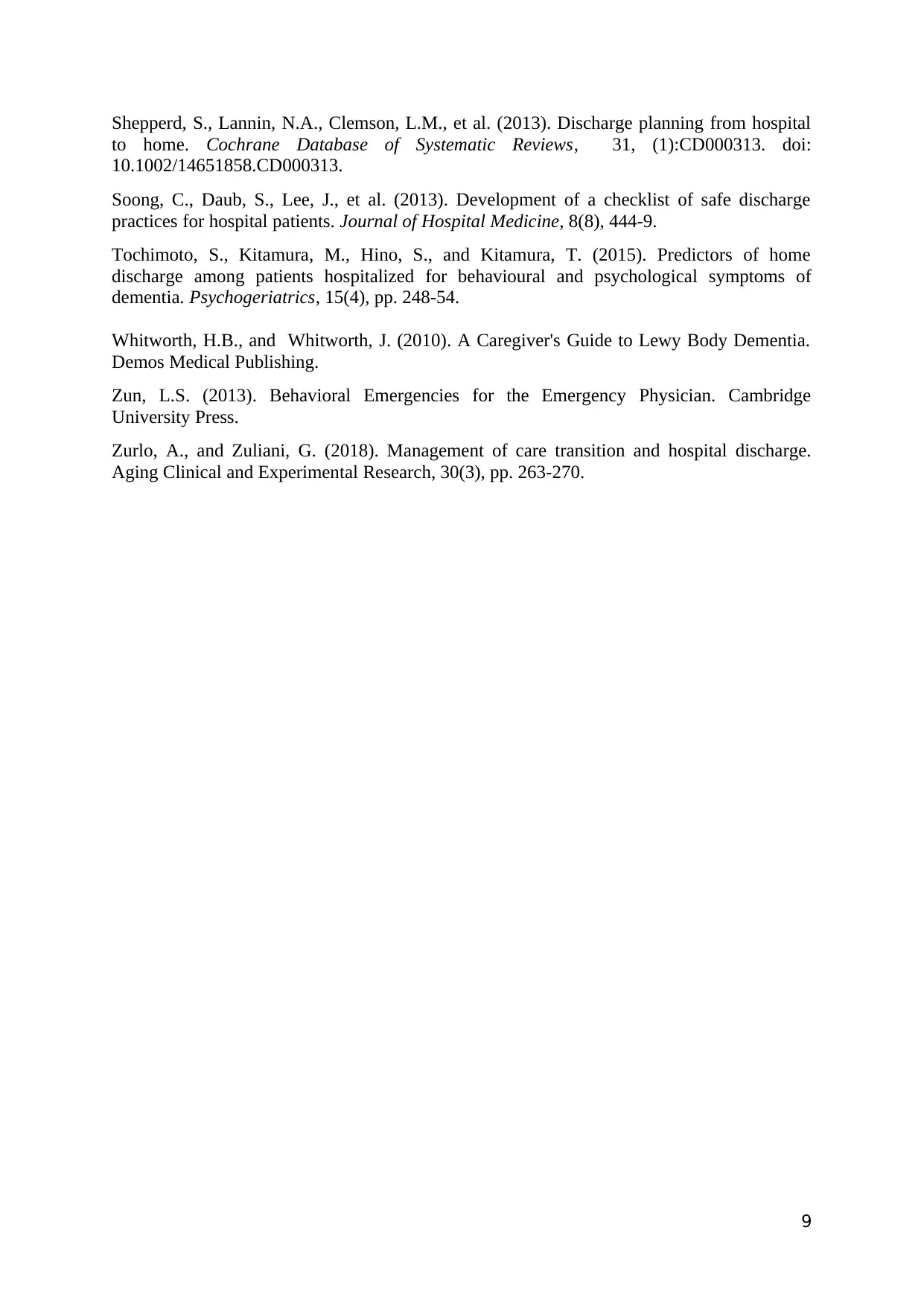
Appendix 1 :
Discharge Plan
Problem Outcome Intervention Rationale
Post discharge, there
should be smooth
discharge for Angelo
to the society.
Angelo should live
normal life post
discharge from the
hospital.
Nurse should make
sure that Angelo is
doing all his ADL.
Angelo is 75 years
old and living alone.
Due to this he might
not be able to do
ADL normally.
(Whitworth and
Whitworth, 2010;
Zun, 2013)
Management of
medication
consumption for
different health
conditions like
cardiovascular and
psychiatric
condition.
Nurse should make
sure, Angelo is
going to be consume
medication
according to
schedule.
Nurse should assure
that Angelo adheres
to the medication
consumption and
should encourage
him to adhere to it.
Nurse should
provide instructions
To Angelo about
medication
consumption in
written and verbal
form.
Angelo should be
educated by nurse
about the benefits
and adverse effects
of medication
consumption.
Angelo need to
know about the
benefits and adverse
effects of medication
consumption on
regular basis.
Angelo might not
know importance of
medication
consumption.
(Whitworth and
Whitworth, 2010;
Zun, 2013)
Referral for Angelo
after discharge.
All the information
should be provided
to Angelo about his
referrals.
Angelo should be
provided with all the
appointment letters
and contact numbers
of referrals from
both the medical and
social filled.
Medical and social
filed professionals
might not engage
with him without
prior appointment.
Hence, he might
need to wait for
10
Discharge Plan
Problem Outcome Intervention Rationale
Post discharge, there
should be smooth
discharge for Angelo
to the society.
Angelo should live
normal life post
discharge from the
hospital.
Nurse should make
sure that Angelo is
doing all his ADL.
Angelo is 75 years
old and living alone.
Due to this he might
not be able to do
ADL normally.
(Whitworth and
Whitworth, 2010;
Zun, 2013)
Management of
medication
consumption for
different health
conditions like
cardiovascular and
psychiatric
condition.
Nurse should make
sure, Angelo is
going to be consume
medication
according to
schedule.
Nurse should assure
that Angelo adheres
to the medication
consumption and
should encourage
him to adhere to it.
Nurse should
provide instructions
To Angelo about
medication
consumption in
written and verbal
form.
Angelo should be
educated by nurse
about the benefits
and adverse effects
of medication
consumption.
Angelo need to
know about the
benefits and adverse
effects of medication
consumption on
regular basis.
Angelo might not
know importance of
medication
consumption.
(Whitworth and
Whitworth, 2010;
Zun, 2013)
Referral for Angelo
after discharge.
All the information
should be provided
to Angelo about his
referrals.
Angelo should be
provided with all the
appointment letters
and contact numbers
of referrals from
both the medical and
social filled.
Medical and social
filed professionals
might not engage
with him without
prior appointment.
Hence, he might
need to wait for
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
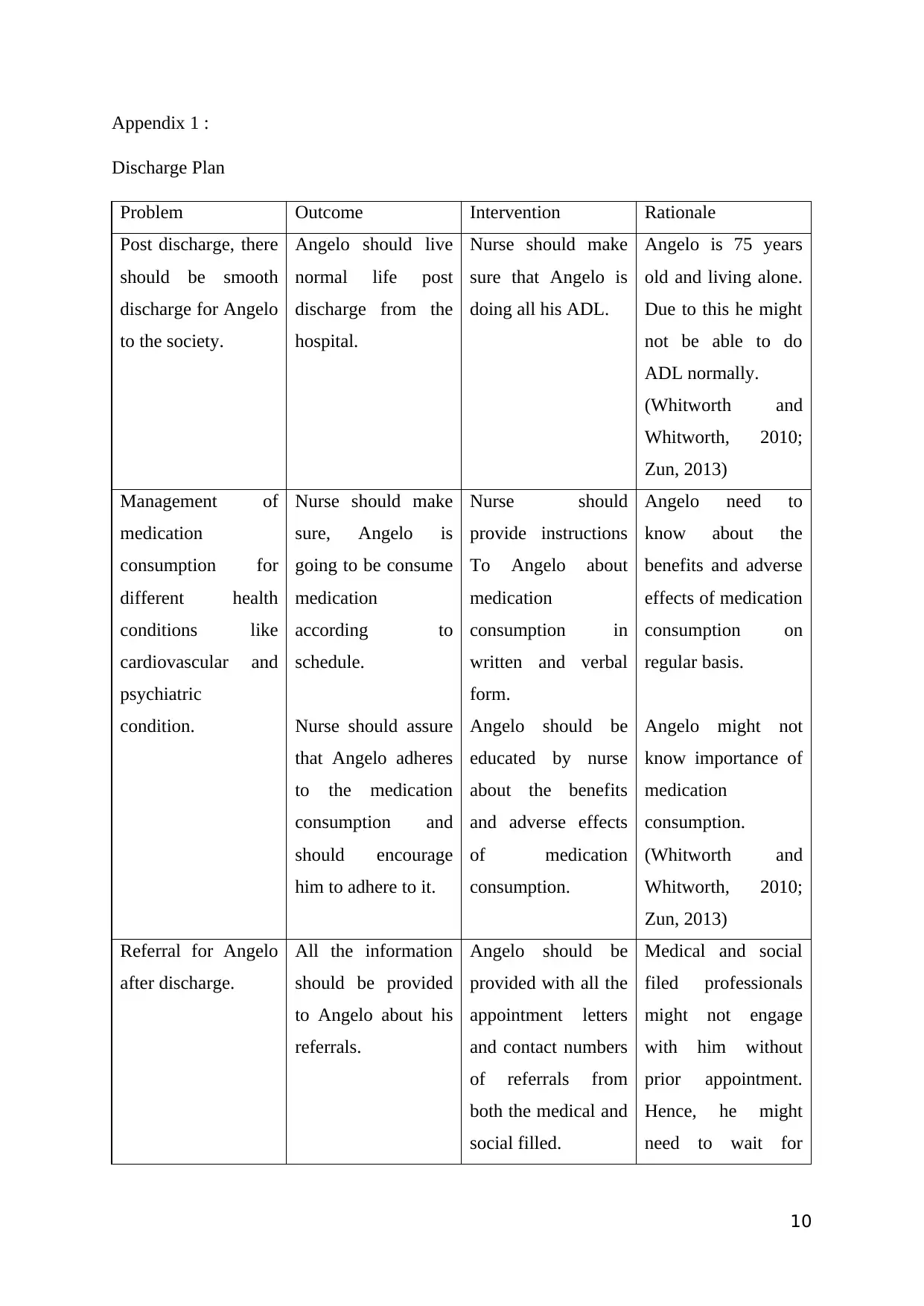
Appointment with
psychiatrist and
dietician should also
be provided to
Angelo.
longer duration.
Angelo is having
hypertension and
hyperlipidaemia for
the longer duration.
These conditions can
be effectively
managed with
proper diet along
with medications.
Dietician can
provide him with
suitable diet plan. In
Lewy body
dementia,
psychiatric
symptoms alter
frequently. Angelo
need to assess
behaviour and
psychiatric related
symptoms on the
regular basis.
(Whitworth and
Whitworth, 2010;
Zun, 2013)
Angelo’s
empowerment
through social
support.
He should be
empowered to fulfil
all his needs and
perform all his ADL
on his own.
Material for the
empowerment in the
form of information,
communication, and
education (IEC)
should be provided
Healthy lifestyle is
useful in improving
quality of life.
Acceptability in the
society can be
improved by living
11
psychiatrist and
dietician should also
be provided to
Angelo.
longer duration.
Angelo is having
hypertension and
hyperlipidaemia for
the longer duration.
These conditions can
be effectively
managed with
proper diet along
with medications.
Dietician can
provide him with
suitable diet plan. In
Lewy body
dementia,
psychiatric
symptoms alter
frequently. Angelo
need to assess
behaviour and
psychiatric related
symptoms on the
regular basis.
(Whitworth and
Whitworth, 2010;
Zun, 2013)
Angelo’s
empowerment
through social
support.
He should be
empowered to fulfil
all his needs and
perform all his ADL
on his own.
Material for the
empowerment in the
form of information,
communication, and
education (IEC)
should be provided
Healthy lifestyle is
useful in improving
quality of life.
Acceptability in the
society can be
improved by living
11
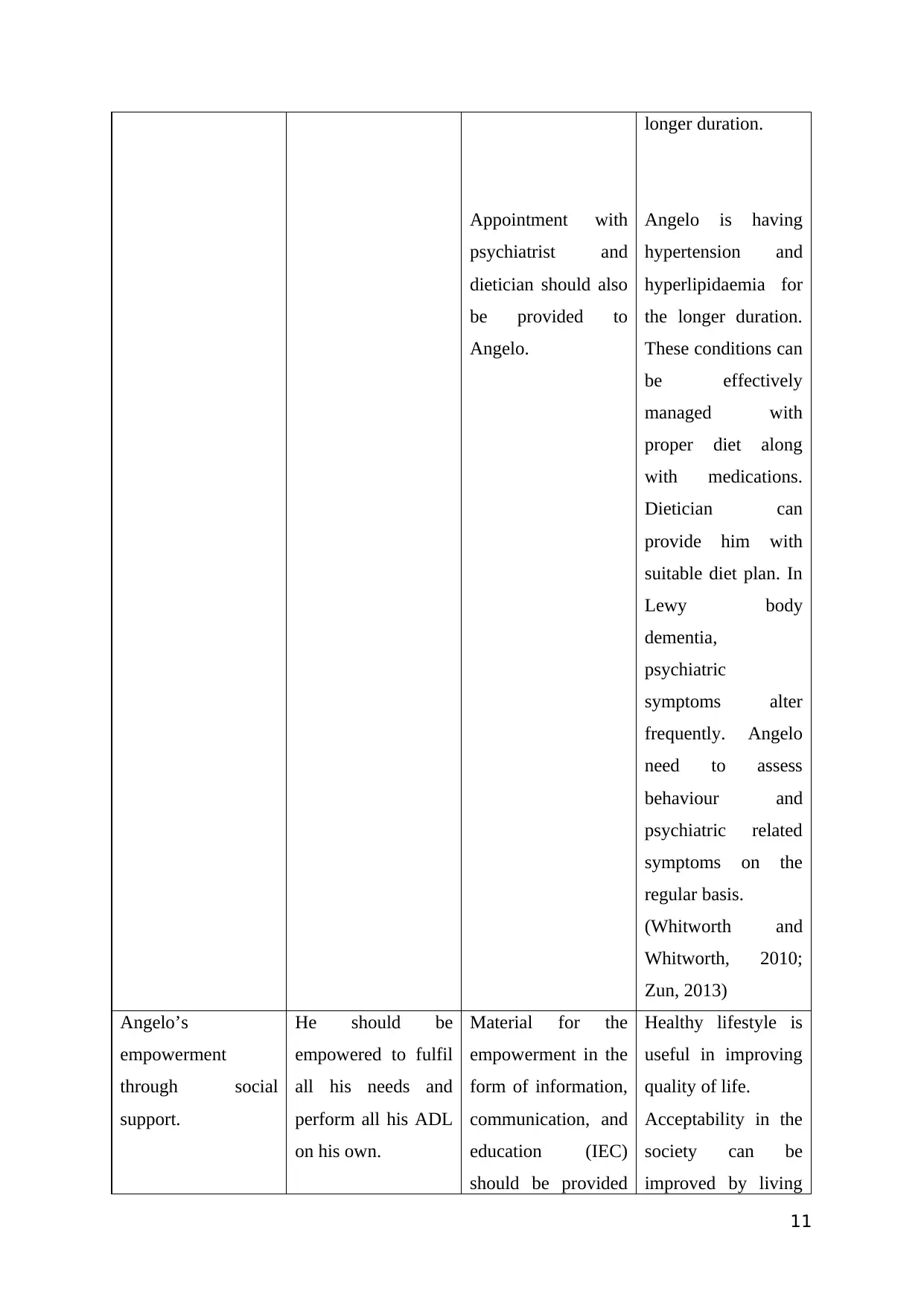
He should establish
effective
communication with
other members of
society and express
his thoughts and
feelings.
to him in printed
format.
Angelo should be
encouraged to
participate in various
social and cultural
activities and
connect to various
social groups.
It can be achieved
by adapting healthy
lifestyle by Angelo
which can be
acceptable for
groups of people.
healthy lifestyle and
improving quality of
life.
(Whitworth and
Whitworth, 2010;
Zun, 2013)
Appendix B : Multidisciplinary team (MDT)
The multidisciplinary team Responsibilities
Nurse Nurse is one of the most instrumental part
of MDT. Nurse should assess and provided
information related to health status prior to
admission, clinical progress during
admission and current health status of
Angelo.
Nurse should also participate in discussions
related to social status of Angelo.
Nurse can form special bond with Angelo
and improve his morale because nurse is the
primary source of contact for Angelo.
(Greenhalgh, 2013; Housley, 2017)
Doctor Doctor should perform clinical assessment
12
effective
communication with
other members of
society and express
his thoughts and
feelings.
to him in printed
format.
Angelo should be
encouraged to
participate in various
social and cultural
activities and
connect to various
social groups.
It can be achieved
by adapting healthy
lifestyle by Angelo
which can be
acceptable for
groups of people.
healthy lifestyle and
improving quality of
life.
(Whitworth and
Whitworth, 2010;
Zun, 2013)
Appendix B : Multidisciplinary team (MDT)
The multidisciplinary team Responsibilities
Nurse Nurse is one of the most instrumental part
of MDT. Nurse should assess and provided
information related to health status prior to
admission, clinical progress during
admission and current health status of
Angelo.
Nurse should also participate in discussions
related to social status of Angelo.
Nurse can form special bond with Angelo
and improve his morale because nurse is the
primary source of contact for Angelo.
(Greenhalgh, 2013; Housley, 2017)
Doctor Doctor should perform clinical assessment
12
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 19
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





