Improving Healthcare Quality and Safety in Western Australia: An Essay
VerifiedAdded on 2022/09/18
|21
|5950
|25
Essay
AI Summary
This essay delves into the critical issues of healthcare quality and safety within the Western Australian healthcare system, with a specific focus on hospital-acquired infections (HAIs) and their impact on geriatric patients. The essay highlights the prevalence of HAIs, particularly pneumonia and urinary tract infections, and their implications for patient outcomes, increased healthcare costs, and antimicrobial resistance. It examines the challenges posed by factors such as poor sanitation, inadequate staffing, and patient overcrowding. Furthermore, it explores various studies and programs aimed at addressing these issues, including pilot programs in residential aged care facilities (RACFs) and the importance of infection control measures. The essay underscores the need for improved management, hygiene practices, and preventative strategies to enhance patient safety and quality of care, advocating for solutions to mitigate the adverse effects of HAIs and promote better health outcomes for the elderly population in Western Australia.

Running Head: HEALTHCARE
0
[Type the company name]
Clinical Leadership and Management
Essay
Student
9/15/2019
0
[Type the company name]
Clinical Leadership and Management
Essay
Student
9/15/2019
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTHCARE
1
In-hospital care, numerous diseases affect the health of patients. In all the terminal
infections and injuries, healthcare-associated infections or hospital-acquired infection is
considered as one of the most rapid and challenging infection that are prevailing in the
environment of hospitals (Shiel Jr., 2019). This infection is developed during the provision of
health care in hospitals. The symptoms of the infection are observed within the 48 hours, after
the hospitalization, or in a month during the period of treatment. Many studies were conducted
in the context of this health problem in which it was identified, that the re-occurring infections or
diseases which are adversely impacting the health of the patients are HCAI and other
complexities appearing in the surgeries of patients. In the health terminology health-care,
infection is called as nosocomial ailment (Monegro & Regunath, 2019). It is occurred due to the
presence of harmful viruses and bacteria in the atmosphere of the health care facility. Such
infection can create a hazardous impact on the immune system of the patients (Stevens,
Hemmings, Scott, Lawler & White, 2014 ).
Every year about hundreds of patients lost their lives due to the infections caused due to
cardiovascular diseases and urinary infections occurring in the body. Pneumonia is also
considered as one of the major reasons of ill health of the patients. Such adverse events create
leads to huge monetary loss for health care organizations (World Health Organization , Health
care-associated infections: Fact Sheet, 2019). Besides this, every 7th nation out of advanced
nation and every 10th country from the emerging nations is suffering from the nosocomial
infection. It can be said that, unitary infections and Surgical site infection ailment, has a high
prevalence in developed countries (World Health Organization , Patient safety, 2019).
Infection can occur in any health care environment regardless of its location. These
infections can be developed can any age. However, its prevalence has been observed in the older
1
In-hospital care, numerous diseases affect the health of patients. In all the terminal
infections and injuries, healthcare-associated infections or hospital-acquired infection is
considered as one of the most rapid and challenging infection that are prevailing in the
environment of hospitals (Shiel Jr., 2019). This infection is developed during the provision of
health care in hospitals. The symptoms of the infection are observed within the 48 hours, after
the hospitalization, or in a month during the period of treatment. Many studies were conducted
in the context of this health problem in which it was identified, that the re-occurring infections or
diseases which are adversely impacting the health of the patients are HCAI and other
complexities appearing in the surgeries of patients. In the health terminology health-care,
infection is called as nosocomial ailment (Monegro & Regunath, 2019). It is occurred due to the
presence of harmful viruses and bacteria in the atmosphere of the health care facility. Such
infection can create a hazardous impact on the immune system of the patients (Stevens,
Hemmings, Scott, Lawler & White, 2014 ).
Every year about hundreds of patients lost their lives due to the infections caused due to
cardiovascular diseases and urinary infections occurring in the body. Pneumonia is also
considered as one of the major reasons of ill health of the patients. Such adverse events create
leads to huge monetary loss for health care organizations (World Health Organization , Health
care-associated infections: Fact Sheet, 2019). Besides this, every 7th nation out of advanced
nation and every 10th country from the emerging nations is suffering from the nosocomial
infection. It can be said that, unitary infections and Surgical site infection ailment, has a high
prevalence in developed countries (World Health Organization , Patient safety, 2019).
Infection can occur in any health care environment regardless of its location. These
infections can be developed can any age. However, its prevalence has been observed in the older
HEALTHCARE
2
generation as the immune system elderly patients are inclined to be more vulnerable to bacterial
infection. To justify the fact a research a study was conducted over 18469 patients. Through the
study, it was identified that 20.3% of aged patients are vulnerable to harmful and dangerous
infections. The probability of respiratory diseases like pneumonia, bacterial meningitis,
secondary bacteremia is higher in old age patients due to which mortality rates have been
increased in the aged people (Australian Government Department of Health and Agi, 2019).
Addition to the above statistics, it was examined that the treatment of Pneumonia in the elderly
people is of the critical challenge for the medical professionals as it weakens the immune system
of the body and increases the volume of mucus in the lungs (Russo , Cheng , Mitchell & Hall ,
2018). Along with Pneumonia, Urinary Tract Infection also has a high prevalence in aged
people. About 15% to 30% of the hospitalized senior populaces are detected to have UTI
whereas 25% to 50% women have a urinary infection (Australian Government Department of
Health and Agi, 2019).
In the list of developed countries, Australia has also witnessed the issues and challenges
in resolving the complication, which is occurring due to hospital-acquired infections. In the
hospitals, cases related to the urinary and respiratory have become common, due to which
treatment has become expensive and has increased the burden on the patients ( Willis ,
Reynolds , & Keleher, 2016). Out of the total hospitalized patients, approximately 48% with the
age above 65 are suffering from HAI (Australian Commission on Safety and Quality in Hea,
2019).
To justify the above discussion, two research experts undertook cross-sectional point
prevalence study in the 19 medical branches and about 2767 patients were included. All the
information was collected in the mid of the year (August-November) in which it was observed
2
generation as the immune system elderly patients are inclined to be more vulnerable to bacterial
infection. To justify the fact a research a study was conducted over 18469 patients. Through the
study, it was identified that 20.3% of aged patients are vulnerable to harmful and dangerous
infections. The probability of respiratory diseases like pneumonia, bacterial meningitis,
secondary bacteremia is higher in old age patients due to which mortality rates have been
increased in the aged people (Australian Government Department of Health and Agi, 2019).
Addition to the above statistics, it was examined that the treatment of Pneumonia in the elderly
people is of the critical challenge for the medical professionals as it weakens the immune system
of the body and increases the volume of mucus in the lungs (Russo , Cheng , Mitchell & Hall ,
2018). Along with Pneumonia, Urinary Tract Infection also has a high prevalence in aged
people. About 15% to 30% of the hospitalized senior populaces are detected to have UTI
whereas 25% to 50% women have a urinary infection (Australian Government Department of
Health and Agi, 2019).
In the list of developed countries, Australia has also witnessed the issues and challenges
in resolving the complication, which is occurring due to hospital-acquired infections. In the
hospitals, cases related to the urinary and respiratory have become common, due to which
treatment has become expensive and has increased the burden on the patients ( Willis ,
Reynolds , & Keleher, 2016). Out of the total hospitalized patients, approximately 48% with the
age above 65 are suffering from HAI (Australian Commission on Safety and Quality in Hea,
2019).
To justify the above discussion, two research experts undertook cross-sectional point
prevalence study in the 19 medical branches and about 2767 patients were included. All the
information was collected in the mid of the year (August-November) in which it was observed
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTHCARE
3
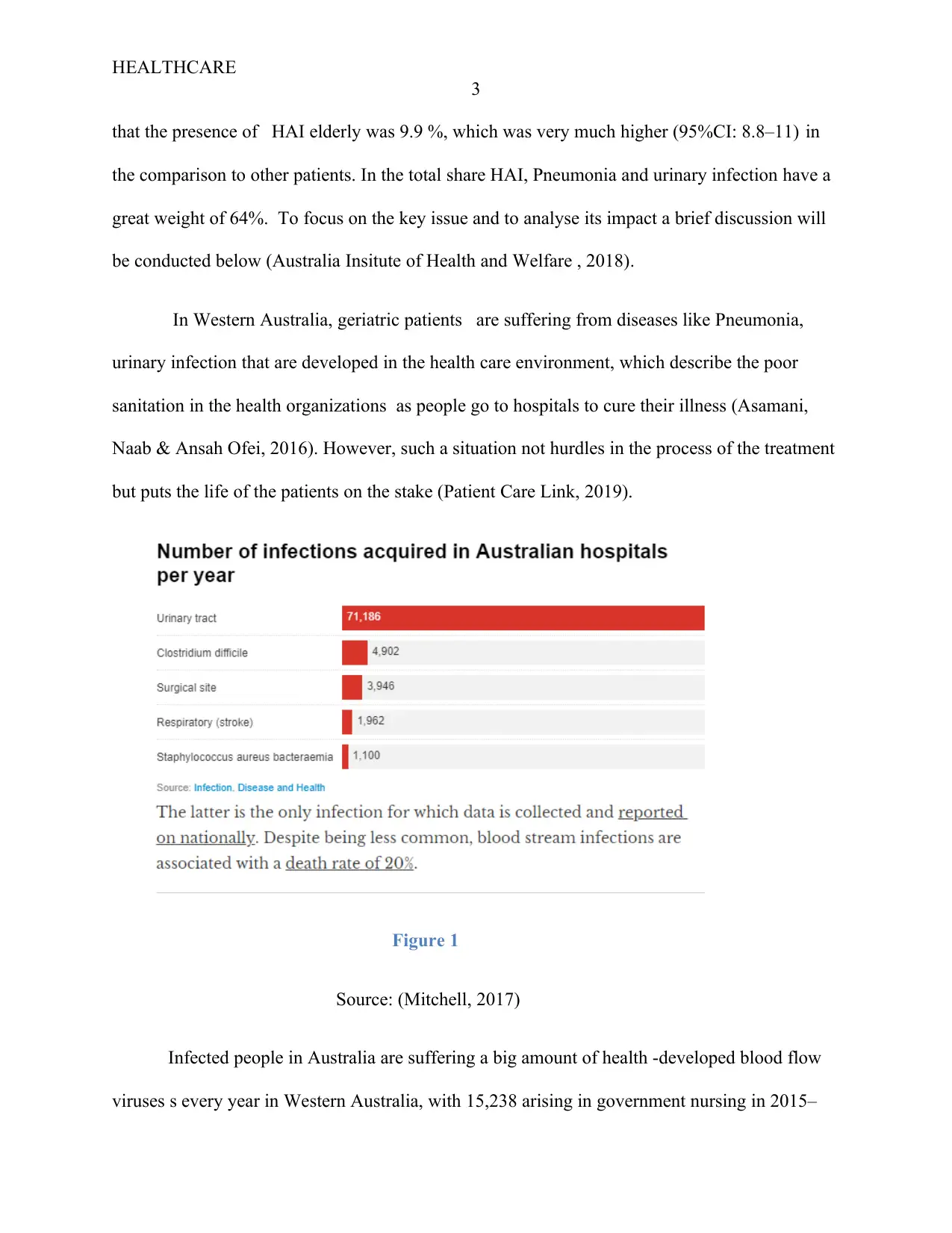
that the presence of HAI elderly was 9.9 %, which was very much higher (95%CI: 8.8–11) in
the comparison to other patients. In the total share HAI, Pneumonia and urinary infection have a
great weight of 64%. To focus on the key issue and to analyse its impact a brief discussion will
be conducted below (Australia Insitute of Health and Welfare , 2018).
In Western Australia, geriatric patients are suffering from diseases like Pneumonia,
urinary infection that are developed in the health care environment, which describe the poor
sanitation in the health organizations as people go to hospitals to cure their illness (Asamani,
Naab & Ansah Ofei, 2016). However, such a situation not hurdles in the process of the treatment
but puts the life of the patients on the stake (Patient Care Link, 2019).
Figure 1
Source: (Mitchell, 2017)
Infected people in Australia are suffering a big amount of health -developed blood flow
viruses s every year in Western Australia, with 15,238 arising in government nursing in 2015–
3
that the presence of HAI elderly was 9.9 %, which was very much higher (95%CI: 8.8–11) in
the comparison to other patients. In the total share HAI, Pneumonia and urinary infection have a
great weight of 64%. To focus on the key issue and to analyse its impact a brief discussion will
be conducted below (Australia Insitute of Health and Welfare , 2018).
In Western Australia, geriatric patients are suffering from diseases like Pneumonia,
urinary infection that are developed in the health care environment, which describe the poor
sanitation in the health organizations as people go to hospitals to cure their illness (Asamani,
Naab & Ansah Ofei, 2016). However, such a situation not hurdles in the process of the treatment
but puts the life of the patients on the stake (Patient Care Link, 2019).
Figure 1
Source: (Mitchell, 2017)
Infected people in Australia are suffering a big amount of health -developed blood flow
viruses s every year in Western Australia, with 15,238 arising in government nursing in 2015–
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTHCARE
4
16.2. Bloodstream infections can cause patients' important distress as they may experience
enhanced heart rate, tremors, fevers, dizziness, postural hypotension, extreme weakness and
lethargy, skin rash, impaired concentrate and agitation mental status (Abbott, 2014)
There is a high incidence of communicable diseases in Western Australia as it has the
potential to spread quickly in residential care facilities (RCF) environments as Australian citizens
reside nearby. There is a high level of interaction with employees, visitors, facilities can be
shared, and citizens may have hygiene-impact physical or mental disabilities. Residents may also
be more prone to infection in some environments, such as aged care, due to health circumstances
as it can weaken the immune system and increase the mortality rate. A study was conducted in
2010 to identify a variety of reasons, which indicates that a residential aged health care system is
extremely vulnerable to infection ( Russo, Stewardson, Cheng, Bucknall & Mitchell, 2019).
These factors involve advanced age for individual citizens of Western Australia, multiple acute-
illness like pre-morbidities (e.g., diabetes), mental disabilities immune destruction, enhanced
antibiotic exposure causing infection vulnerability, and utilization of sometimes permanent
invasive instruments (e.g., urinary tract catheters).
It has been observed that infections and viruses, which are present in the atmosphere of
the hospitals, are one of the major causes of acute illnesses in elderly patients. From the last 6
years, more than 3310 aged patients have been hospitalized. In all the above cases, the common
health issue is a health-acquired infection (Australian Government Department of Health and
Agi, 2019). During the medical diagnosis, it was identified out of the total hospitalized elderly
patients, 432 patients are were identified to be in contact with the viruses. The prevalence of
Pneumonia (5.6%) and urinary tract infections (UTI) (3.4%) were most commonly stated. To
monitor and control the impacts of infections a pilot program was adopted to investigate the
4
16.2. Bloodstream infections can cause patients' important distress as they may experience
enhanced heart rate, tremors, fevers, dizziness, postural hypotension, extreme weakness and
lethargy, skin rash, impaired concentrate and agitation mental status (Abbott, 2014)
There is a high incidence of communicable diseases in Western Australia as it has the
potential to spread quickly in residential care facilities (RCF) environments as Australian citizens
reside nearby. There is a high level of interaction with employees, visitors, facilities can be
shared, and citizens may have hygiene-impact physical or mental disabilities. Residents may also
be more prone to infection in some environments, such as aged care, due to health circumstances
as it can weaken the immune system and increase the mortality rate. A study was conducted in
2010 to identify a variety of reasons, which indicates that a residential aged health care system is
extremely vulnerable to infection ( Russo, Stewardson, Cheng, Bucknall & Mitchell, 2019).
These factors involve advanced age for individual citizens of Western Australia, multiple acute-
illness like pre-morbidities (e.g., diabetes), mental disabilities immune destruction, enhanced
antibiotic exposure causing infection vulnerability, and utilization of sometimes permanent
invasive instruments (e.g., urinary tract catheters).
It has been observed that infections and viruses, which are present in the atmosphere of
the hospitals, are one of the major causes of acute illnesses in elderly patients. From the last 6
years, more than 3310 aged patients have been hospitalized. In all the above cases, the common
health issue is a health-acquired infection (Australian Government Department of Health and
Agi, 2019). During the medical diagnosis, it was identified out of the total hospitalized elderly
patients, 432 patients are were identified to be in contact with the viruses. The prevalence of
Pneumonia (5.6%) and urinary tract infections (UTI) (3.4%) were most commonly stated. To
monitor and control the impacts of infections a pilot program was adopted to investigate the
HEALTHCARE
5
gravity of hospital-acquired disease over the patients. In this 12 hospital-associated health
services in the Grampians Rural Region, Victoria, Australia, participated in the research study of
RACFs (Residential Aged Care Facilities.)
This experimental program aimed to collect data that would guide the Australian
Infection Control Association taking and controlling the development of the virus in the
healthcare system, which implemented through the futuristic programs run by RACFs. Besides
this, 30 RACF participated (Dixit & Sambasivan, 2018 ).
During the program, Australian Government Aged Care Assessment Team (ACAT)
evaluated the probability of high-care residents who required assistance with most everyday
living actions. This activity was comprised of lodging, meals, laundry, and personal hygiene care
and, if required, medical care (Drager, 2013). They further analyzed the average life expectancy
of citizens in which the symptoms of the infections and viruses were detected in 84.9% of
Australian during the monitoring duration, whereas 68% of the females are suffering from such
kind of illness. In RACFs, the pilot program was conducted to gather knowledge and understand
the gravity of the diseases and to control and monitor HAI through effective programs. The
information gathered in the Grampians RACFs will assist the residential directs in the decisions
making the process to prevent HAI (J, 2016).
In the health care system, HAI and various other diseases not only create a hurdle in the
treatment of the patients but have become a burden on the facilities as many diseases require
special treatment and attention which also involves hiring medical experts. Such adverse events
increase the overall cost of treatment, which can overburden the patients and make them more
depressed. Moreover, due to the lack of efficient management the case of AMR case has been
5
gravity of hospital-acquired disease over the patients. In this 12 hospital-associated health
services in the Grampians Rural Region, Victoria, Australia, participated in the research study of
RACFs (Residential Aged Care Facilities.)
This experimental program aimed to collect data that would guide the Australian
Infection Control Association taking and controlling the development of the virus in the
healthcare system, which implemented through the futuristic programs run by RACFs. Besides
this, 30 RACF participated (Dixit & Sambasivan, 2018 ).
During the program, Australian Government Aged Care Assessment Team (ACAT)
evaluated the probability of high-care residents who required assistance with most everyday
living actions. This activity was comprised of lodging, meals, laundry, and personal hygiene care
and, if required, medical care (Drager, 2013). They further analyzed the average life expectancy
of citizens in which the symptoms of the infections and viruses were detected in 84.9% of
Australian during the monitoring duration, whereas 68% of the females are suffering from such
kind of illness. In RACFs, the pilot program was conducted to gather knowledge and understand
the gravity of the diseases and to control and monitor HAI through effective programs. The
information gathered in the Grampians RACFs will assist the residential directs in the decisions
making the process to prevent HAI (J, 2016).
In the health care system, HAI and various other diseases not only create a hurdle in the
treatment of the patients but have become a burden on the facilities as many diseases require
special treatment and attention which also involves hiring medical experts. Such adverse events
increase the overall cost of treatment, which can overburden the patients and make them more
depressed. Moreover, due to the lack of efficient management the case of AMR case has been
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTHCARE
6
increased. Higher the AMR (Antimicrobial resistance), longer the process of treatment and more
investment. The unhygienic attitude of the medical staff and carelessness in the maintenance of
the elderly patients has led to the perseverance of MRO as well as Clostridium which causes
major illnesses like diarrhea, Viral and abdominal discomfort. An estimation was made that there
were about more than 1,100 incidences of Staphylococcus aureus (golden staph) diseases that
were happening in the medical care facilities ( Auer, Schwendimann, MCommH, Geest &
Ausserhofer, 2014 ). Along with this issue, the occurrence and problematic side effects of
associated health care diseases (HAIs) have been well recognized in the medical history of the
nation. The development of HAI in the hospital environment has created an alarming situation
for the medical practitioners and staff. It is symptoms cannot be recognized at the begging of the
hospitalization as it started developing during the treatment and the doctors are not able to detect
it. Like HAI, other diseases not only weaken and stop the functioning of all body parts but also
makes the survival of the patients difficult which eventually lead to death, Such situations put
burden on the hospital care setting by keeping infective patients in hospital for longer and
consuming resources (Haque, Sartelli, McKimm & Bakar, 2018 ). In Australia, it has been
estimated that every year that health-related urinary tract infections use roughly 380,600
additional days of public hospital beds. However, there are many health care facilities, which can
prevent the development of HAI in the hospital environment.
A study was conducted in which it was identified that 65-70% of the blood related, and
urinary tract infections can be tracked and prevented by the providing premium provision of care
to the aged patients, as infections and virus occur and start multiplying when entering into the
blood of the hospitalized patients . It can be understood with the example, that when any kind of
germs present in the wound often can lead to the development of infection or illness. Bacteria
6
increased. Higher the AMR (Antimicrobial resistance), longer the process of treatment and more
investment. The unhygienic attitude of the medical staff and carelessness in the maintenance of
the elderly patients has led to the perseverance of MRO as well as Clostridium which causes
major illnesses like diarrhea, Viral and abdominal discomfort. An estimation was made that there
were about more than 1,100 incidences of Staphylococcus aureus (golden staph) diseases that
were happening in the medical care facilities ( Auer, Schwendimann, MCommH, Geest &
Ausserhofer, 2014 ). Along with this issue, the occurrence and problematic side effects of
associated health care diseases (HAIs) have been well recognized in the medical history of the
nation. The development of HAI in the hospital environment has created an alarming situation
for the medical practitioners and staff. It is symptoms cannot be recognized at the begging of the
hospitalization as it started developing during the treatment and the doctors are not able to detect
it. Like HAI, other diseases not only weaken and stop the functioning of all body parts but also
makes the survival of the patients difficult which eventually lead to death, Such situations put
burden on the hospital care setting by keeping infective patients in hospital for longer and
consuming resources (Haque, Sartelli, McKimm & Bakar, 2018 ). In Australia, it has been
estimated that every year that health-related urinary tract infections use roughly 380,600
additional days of public hospital beds. However, there are many health care facilities, which can
prevent the development of HAI in the hospital environment.
A study was conducted in which it was identified that 65-70% of the blood related, and
urinary tract infections can be tracked and prevented by the providing premium provision of care
to the aged patients, as infections and virus occur and start multiplying when entering into the
blood of the hospitalized patients . It can be understood with the example, that when any kind of
germs present in the wound often can lead to the development of infection or illness. Bacteria
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTHCARE
7
and viruses, which are a standard component of the human body, are often transmitted to
healthcare workers ' hands in healthcare environments and can be discovered in the patient
setting. Evidence indicates that patients admitted to a room earlier occupied by a drug-resistant
carrier have a considerably greater likelihood of obtaining that bacterium. Due to such frequent
complexities, the average stay of parents becomes longer which can even stretch 18.1 days.
According to healthcare Associated Infection detailed fact sheet presented by Australian
Commission on Safety and Quality in Health Care (2018), the expense of average night stay is
$2,074 and the cost of stay can be multiplied up to $ 37, 539, according to nature of treatment
(South Australia Health, 2019).
However, it is still unclear that how these are developed but lack of quality of services to
the aged patients, management in the clinical care setting and negligence in the process of the
treatment can be seen as major drivers of such issues.
In hospitals, high adverse outcome rates and outbreak interrogation have been associated
with the low and inexperienced nursing staff. Besides this patient overcrowding has also resulted
in poor adherence to hand hygiene. In the ICU setting, lack of sanitation on the part of nurses has
been shown to promote the spread of MRSA through stress-free consideration to fundamental
infection prevention measures. During the investigation, it was identified that the ratio of quality
and highly experienced nursing staff in the provision of care is very much less in comparison to
the hospitalized citizens, which has reduced the workload and increased the carelessness in the
treatment. It was evaluated many of the nurses avoid and give less consideration to the infection
control measures like the use of gloves and sanitizers before touching the patients. When there is
demand and the numbers of the hospitalized are very much higher, only at that time 25% of the
nurses wash their hands before coming in contact with the patients, which is further increased to
7
and viruses, which are a standard component of the human body, are often transmitted to
healthcare workers ' hands in healthcare environments and can be discovered in the patient
setting. Evidence indicates that patients admitted to a room earlier occupied by a drug-resistant
carrier have a considerably greater likelihood of obtaining that bacterium. Due to such frequent
complexities, the average stay of parents becomes longer which can even stretch 18.1 days.
According to healthcare Associated Infection detailed fact sheet presented by Australian
Commission on Safety and Quality in Health Care (2018), the expense of average night stay is
$2,074 and the cost of stay can be multiplied up to $ 37, 539, according to nature of treatment
(South Australia Health, 2019).
However, it is still unclear that how these are developed but lack of quality of services to
the aged patients, management in the clinical care setting and negligence in the process of the
treatment can be seen as major drivers of such issues.
In hospitals, high adverse outcome rates and outbreak interrogation have been associated
with the low and inexperienced nursing staff. Besides this patient overcrowding has also resulted
in poor adherence to hand hygiene. In the ICU setting, lack of sanitation on the part of nurses has
been shown to promote the spread of MRSA through stress-free consideration to fundamental
infection prevention measures. During the investigation, it was identified that the ratio of quality
and highly experienced nursing staff in the provision of care is very much less in comparison to
the hospitalized citizens, which has reduced the workload and increased the carelessness in the
treatment. It was evaluated many of the nurses avoid and give less consideration to the infection
control measures like the use of gloves and sanitizers before touching the patients. When there is
demand and the numbers of the hospitalized are very much higher, only at that time 25% of the
nurses wash their hands before coming in contact with the patients, which is further increased to
HEALTHCARE
8
70% during the absence of required nurses and when the need is very much higher. During the
monitoring, it was determined that a four-fold boosted the risk of obtaining an HAI was
associated with being hospitalized during this period (Australia Insitute of Health and Welfare ,
2018).
These studies illustrate that workload over the staff members , diseases, and microbial
are interrelated in the transmission from bad adherence to manual hygiene measures. Although
norms for hand hygiene procedures were released with evidence-based guidelines the “How-to-
Guide was created by professional collaborations: improving hygiene, there is no consistent
technique or instrument for assessing adherence to organizational policies ( Fernando , Gray &
Gottlieb, 2017 ).
Various methodologies for improving the quality and absence of agreement on how to
quantify compliance with the cleanness of the body have made it hard to regulate the efficacy of
expectations for hand sanitation in and across environments of the hospitals. Moreover,
prolonged antibiotic use in the absence of infection risk selecting for resistant organisms has
made did difficulty to treat the patients. This demonstrates the role of the hospital environment
in infection transmission and infers that current cleaning practices in hospital fail to reduce the
risk of infections. (Australian Commission on Safety and Quality in Hea, 2019)
The avoidance of Hospitalized-acquired Infection is considered as a top-priority problem
for the clinical doctor and nurses. For preventing its further development, the government has
introduced various reforms, like they has set certain standards in all Australian hospitals for
good clinical practice, and compliance is deemed compulsory for accreditation ( Lim , Stuart &
Kong , 2015). Over the last 40 years, the change in hospital-acquired infections has been
8
70% during the absence of required nurses and when the need is very much higher. During the
monitoring, it was determined that a four-fold boosted the risk of obtaining an HAI was
associated with being hospitalized during this period (Australia Insitute of Health and Welfare ,
2018).
These studies illustrate that workload over the staff members , diseases, and microbial
are interrelated in the transmission from bad adherence to manual hygiene measures. Although
norms for hand hygiene procedures were released with evidence-based guidelines the “How-to-
Guide was created by professional collaborations: improving hygiene, there is no consistent
technique or instrument for assessing adherence to organizational policies ( Fernando , Gray &
Gottlieb, 2017 ).
Various methodologies for improving the quality and absence of agreement on how to
quantify compliance with the cleanness of the body have made it hard to regulate the efficacy of
expectations for hand sanitation in and across environments of the hospitals. Moreover,
prolonged antibiotic use in the absence of infection risk selecting for resistant organisms has
made did difficulty to treat the patients. This demonstrates the role of the hospital environment
in infection transmission and infers that current cleaning practices in hospital fail to reduce the
risk of infections. (Australian Commission on Safety and Quality in Hea, 2019)
The avoidance of Hospitalized-acquired Infection is considered as a top-priority problem
for the clinical doctor and nurses. For preventing its further development, the government has
introduced various reforms, like they has set certain standards in all Australian hospitals for
good clinical practice, and compliance is deemed compulsory for accreditation ( Lim , Stuart &
Kong , 2015). Over the last 40 years, the change in hospital-acquired infections has been
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
HEALTHCARE
9
monitored by the health care system of Western Australia. To decrease its further development,
the health care association has adopted evidence-based infection prevention plans and policies.
Many factors affect the expansion of HAIs, including patient variables (e.g. acuity of disease and
general health status), hospitalized citizens’ carefulness variables (e.g. antibiotic use, invasive
use of medical devices). Besides this, they are an organizational factor (e.g. ratio of nurses to
patients, level of nursing learning, continuous or vocationally / float nurse), varying use by
hospital employees of aseptic methods (Government of Western Australia, 2019).
Aspects such as improved ambulatory acuteness of ailment, imbalance ratio nurse
staffing and patients, poor care-system and other requirements that have challenged the health
management to constantly to emphasis on evidence-based suggestions to maximize prevention of
infection which can influence such evolving trends. Despite these requirements on healthcare
workers and resources, it continues an imperative task to reduce preventable HAIs and enhances
maximizes the security of hospitalized citizens. There is another way of preventing the
significance of Health care infection is that the Australian government must take an active part in
avoiding reoccurrence by introducing the laws. Hospitals must provide training to their
employees so after attaining and skills, they must provide efficient treatment to the elderly
patients. Hospitals must conduct training programs, where through practical examples, the
importance of cleanness, sanitation in the medical facilities must be taught to the nurses so that
before meeting the illness of the patient's clinical nurses must take precautions. The hospital
must promote teamwork in the system, as Nurses are the prominent part of the health care system
as they play a significant role in avoiding hospital-acquired infections, not only by ensuring that
all aspects of their nursing practice are effectively achieved, but also through nursing research,
patient education, and infection control procedures being implemented. Moreover, the evidence-
9
monitored by the health care system of Western Australia. To decrease its further development,
the health care association has adopted evidence-based infection prevention plans and policies.
Many factors affect the expansion of HAIs, including patient variables (e.g. acuity of disease and
general health status), hospitalized citizens’ carefulness variables (e.g. antibiotic use, invasive
use of medical devices). Besides this, they are an organizational factor (e.g. ratio of nurses to
patients, level of nursing learning, continuous or vocationally / float nurse), varying use by
hospital employees of aseptic methods (Government of Western Australia, 2019).
Aspects such as improved ambulatory acuteness of ailment, imbalance ratio nurse
staffing and patients, poor care-system and other requirements that have challenged the health
management to constantly to emphasis on evidence-based suggestions to maximize prevention of
infection which can influence such evolving trends. Despite these requirements on healthcare
workers and resources, it continues an imperative task to reduce preventable HAIs and enhances
maximizes the security of hospitalized citizens. There is another way of preventing the
significance of Health care infection is that the Australian government must take an active part in
avoiding reoccurrence by introducing the laws. Hospitals must provide training to their
employees so after attaining and skills, they must provide efficient treatment to the elderly
patients. Hospitals must conduct training programs, where through practical examples, the
importance of cleanness, sanitation in the medical facilities must be taught to the nurses so that
before meeting the illness of the patient's clinical nurses must take precautions. The hospital
must promote teamwork in the system, as Nurses are the prominent part of the health care system
as they play a significant role in avoiding hospital-acquired infections, not only by ensuring that
all aspects of their nursing practice are effectively achieved, but also through nursing research,
patient education, and infection control procedures being implemented. Moreover, the evidence-
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
HEALTHCARE
10
based strategies have provided ample opportunities to the nurses to reduce the impacts of HAI
( Health Care Acquired Infection).
Through their experience and knowledge, the nurse can reduce the complexities, which
are arising in the treatment of the patient, thus assisting the medical professional in the recovery
of the aged patients. Attributing to these nurses has numerous tools, which are practiced by them
to minimize the impact of infection as well as to provide a safe and secure environment. They are
key areas of the nursing practice as by working upon them, midwives can control the prevalence
of viruses and various other infections like Pneumonia, urinary, and bloodstream infections.
Moreover, through the medium of these tools, nursing staff can understand the significance of
hand hygiene (Russo , Cheng , Mitchell & Hall , 2018).
Today many health service organizations are providing quality of services to patients so
that risk related hospital-acquired infection can be eliminated. It ensures the safety and quality of
the systems by preventing, detecting, managing and controlling hospital-acquired infections.
Many hospitals ensure that clinicians have access to appropriate domestic best practice
guidelines. Health care management supports medical practitioners and nurses in conducting
constant training which is crucial for the treatment and prevention of patients-acquired illnesses.
It ensures practical training which involves imparting the knowledge regarding the usage of
suitable equipment, devices, and goods which are necessary to minimize and efficiently handle
hospital-acquired infections ( Mohammadi, 2018 ). The training program should emphasize
the reusable equipment, tools, and devices that are reprocessed in a way consistent with
appropriate domestic and global norms. Health care organizations today are working according
to the standard so that the health of aged patients can be improved effectively in a systematic
way. Organizations are now adhering to the code of conduct (Monegro & Regunath, 2019).
10
based strategies have provided ample opportunities to the nurses to reduce the impacts of HAI
( Health Care Acquired Infection).
Through their experience and knowledge, the nurse can reduce the complexities, which
are arising in the treatment of the patient, thus assisting the medical professional in the recovery
of the aged patients. Attributing to these nurses has numerous tools, which are practiced by them
to minimize the impact of infection as well as to provide a safe and secure environment. They are
key areas of the nursing practice as by working upon them, midwives can control the prevalence
of viruses and various other infections like Pneumonia, urinary, and bloodstream infections.
Moreover, through the medium of these tools, nursing staff can understand the significance of
hand hygiene (Russo , Cheng , Mitchell & Hall , 2018).
Today many health service organizations are providing quality of services to patients so
that risk related hospital-acquired infection can be eliminated. It ensures the safety and quality of
the systems by preventing, detecting, managing and controlling hospital-acquired infections.
Many hospitals ensure that clinicians have access to appropriate domestic best practice
guidelines. Health care management supports medical practitioners and nurses in conducting
constant training which is crucial for the treatment and prevention of patients-acquired illnesses.
It ensures practical training which involves imparting the knowledge regarding the usage of
suitable equipment, devices, and goods which are necessary to minimize and efficiently handle
hospital-acquired infections ( Mohammadi, 2018 ). The training program should emphasize
the reusable equipment, tools, and devices that are reprocessed in a way consistent with
appropriate domestic and global norms. Health care organizations today are working according
to the standard so that the health of aged patients can be improved effectively in a systematic
way. Organizations are now adhering to the code of conduct (Monegro & Regunath, 2019).
HEALTHCARE
11
This standard includes maintaining hygiene before and after each patient touch, using
personal protective equipment when there is a danger of exposure to blood or body fluid. Besides
these nurses, sharp intramuscular injections should be used and disposed of immediately, and
environmental cleaning should be carried out, as well as reprocessing shared patient facilities.
Clinical managers and nursing employees are required to adopt respiratory hygiene and cough
labeling –use the aseptic technique–safe handling and disposal of waste and linen. Medical staff
measure the infection risk and implement transmission-based precautions in the process of the
treatment which curb the orientation of the dangerous infectious agents and diagnose
antimicrobial securely and efficiently following best practice guidelines ( Smith, Bull, Richards,
Woodburn & Bennet, 2011). For avoiding the risk of viruses, infection control staff play a
significant role in the prevention and prevention of medical errors by patients and health care
workers. Infection Control Practitioner (ICP) is being appointed for conducting a ward-specific
infection observation, so that information can be collected regarding the prevalence of infection
rates in the system. This is adopted to expose such information to the nursing staff so that staff
education and training can be conducted efficiently and effectively, react to and enforce outbreak
control measures, and consult on staff health problems.
Health care organizations hire specialist practitioners, as they are the experts who acquire
knowledge from science periodicals and learning programs provided by hospital care
organizations on the topics related which involves precise infection investigation theories,
infection control, and epidemiology. Besides, the above measures, visitors must take precautions
to avoid the risk of infection. There are certain suggestions, which must be followed by the
invitees ( Auer, MCommH & Ausserhofer, 2014). One of basic principle a visitors must follow
is the maintenance of hand hygiene before meeting the patients’ Bloodborne pathogens with
11
This standard includes maintaining hygiene before and after each patient touch, using
personal protective equipment when there is a danger of exposure to blood or body fluid. Besides
these nurses, sharp intramuscular injections should be used and disposed of immediately, and
environmental cleaning should be carried out, as well as reprocessing shared patient facilities.
Clinical managers and nursing employees are required to adopt respiratory hygiene and cough
labeling –use the aseptic technique–safe handling and disposal of waste and linen. Medical staff
measure the infection risk and implement transmission-based precautions in the process of the
treatment which curb the orientation of the dangerous infectious agents and diagnose
antimicrobial securely and efficiently following best practice guidelines ( Smith, Bull, Richards,
Woodburn & Bennet, 2011). For avoiding the risk of viruses, infection control staff play a
significant role in the prevention and prevention of medical errors by patients and health care
workers. Infection Control Practitioner (ICP) is being appointed for conducting a ward-specific
infection observation, so that information can be collected regarding the prevalence of infection
rates in the system. This is adopted to expose such information to the nursing staff so that staff
education and training can be conducted efficiently and effectively, react to and enforce outbreak
control measures, and consult on staff health problems.
Health care organizations hire specialist practitioners, as they are the experts who acquire
knowledge from science periodicals and learning programs provided by hospital care
organizations on the topics related which involves precise infection investigation theories,
infection control, and epidemiology. Besides, the above measures, visitors must take precautions
to avoid the risk of infection. There are certain suggestions, which must be followed by the
invitees ( Auer, MCommH & Ausserhofer, 2014). One of basic principle a visitors must follow
is the maintenance of hand hygiene before meeting the patients’ Bloodborne pathogens with
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 21
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





