Care Planning Processes in Healthcare Practice: A Comprehensive Review
VerifiedAdded on 2023/01/03
|14
|4693
|68
Report
AI Summary
This report delves into the intricacies of care planning within the National Health Services (NHS) in the United Kingdom. It begins by comparing different assessment models, specifically the social and medical models of health, and their practical applications in healthcare settings. The report then discusses the application of theoretical perspectives, such as behavioral and sociological perspectives, to the care planning process. It emphasizes the importance of person-centered care and the responsibilities of healthcare professionals in promoting it, using examples of care plans to illustrate the process. The report also addresses the barriers to implementing care planning and highlights the benefits of using care plans to prioritize individual needs. Finally, it examines the ways in which individuals and families contribute to the evaluation of the care process and reviews the impact of care planning on all stakeholders involved, including practitioners, families, individuals, and carers. The report concludes by summarizing the key findings and their implications for improving healthcare practices.
Care Planning Processes in
Healthcare Practice
Healthcare Practice
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Contents
INTRODUCTION...........................................................................................................................3
TASK 1............................................................................................................................................3
P1 Compare the different models of assessment and their implementation in healthcare.....3
P2 Discuss the application of theoretical perspectives to the care planning process in a healthcare
setting.....................................................................................................................................5
TASK 2............................................................................................................................................6
P3 Discuss responsibilities and duties of own role in promoting person-centred care planning 6
P4 Demonstrate own contribution to the care planning process and use of care plans in the setting
................................................................................................................................................6
TASK 3............................................................................................................................................6
P5 Discuss the barriers to implementing care planning in the setting...................................6
P6 Review the benefits of the use of care plans in ensuring the needs of the individual are
prioritised...............................................................................................................................6
TASK 4............................................................................................................................................7
P7 Discuss the ways in which the individual and family contributes to evaluation of the care
process....................................................................................................................................7
P8 Review aspects of the care planning process and their impact upon the individual, family and
carers......................................................................................................................................8
CONCLUSION................................................................................................................................8
REFERENCES................................................................................................................................9
INTRODUCTION...........................................................................................................................3
TASK 1............................................................................................................................................3
P1 Compare the different models of assessment and their implementation in healthcare.....3
P2 Discuss the application of theoretical perspectives to the care planning process in a healthcare
setting.....................................................................................................................................5
TASK 2............................................................................................................................................6
P3 Discuss responsibilities and duties of own role in promoting person-centred care planning 6
P4 Demonstrate own contribution to the care planning process and use of care plans in the setting
................................................................................................................................................6
TASK 3............................................................................................................................................6
P5 Discuss the barriers to implementing care planning in the setting...................................6
P6 Review the benefits of the use of care plans in ensuring the needs of the individual are
prioritised...............................................................................................................................6
TASK 4............................................................................................................................................7
P7 Discuss the ways in which the individual and family contributes to evaluation of the care
process....................................................................................................................................7
P8 Review aspects of the care planning process and their impact upon the individual, family and
carers......................................................................................................................................8
CONCLUSION................................................................................................................................8
REFERENCES................................................................................................................................9
INTRODUCTION
In healthcare, the care planning is the process through which health care professionals or
practitioners and patient discuss, agree as well as review an action plan in order to accomplish the
goals or behaviour change relevance to the patient. In this report, the chosen organisation is National
Health Services which is a publicly funded healthcare system in United Kingdom. This report covers
influence of theoretical models and methods of planning and assessment in practice in workplace.
Apart from this, implement clear plan in workplace in order to mitigate desired outcomes for
individuals. In addition to this, the report also review the benefits and challenges of planning person
centred care in the workplace. At last, it reflects on the impact of planning of care on practitioners,
family, individuals and carers in relation to own practice.
TASK 1
P1 Compare the different models of assessment and their implementation in healthcare
Health can be defined as the state of complete mental, physical and social wellbeing and not
merely infirmity or disease absence. For every human being, the enjoyment of highest attainable
health standard is one of the fundamental right, without distinction of political beliefs, social
conditions, race, religion and economic condition. There are different models of health assessment
which can be executed by healthcare professionals in their practice. Some of the models along with
their comparison are discussed below:
The social model of health: it is the model which is emerged from social model of disability,
that has been strongly advocated through disability rights movement. The social model of health was
developed as reaction to traditional health model, i.e., medical model of health. The social health
model examines all the factors or elements that contributes to health including political, environment,
cultural and social factors. One of the example includes poor housing, low self-esteem and stress can
have adverse influence on health. Low self-esteem as well as low levels of autonomy are possibly to
relate to worse health. It is believed that the community know that the health of people being affected
by different issues. CDHN believes that communities can and must be actively involved in
determining, planning, designing as well as execute solutions to the issues associated with health and
unjust inequalities in health.
It is clearly recognised in the model that the health of a person is influenced through different
interpersonal, environmental, individual, economic, political and social factors. The senior carer in the
health care setting like National Health Services execute social model of health in order to determine
the interaction between the factors and other social influences on health of an individual. This leads to
dramatic differences in health among the various population groups. execution of social model of
health encourage the healthcare professionals to adopt a far ranging and deep perspective on health as
well as to address the political, cultural and social issues that impact on health in an effective way.
The social view regarding health implies that people must intervene to alter those aspects of
environment which promote ill health instead of continue to exhort people to alter their lifestyles and
In healthcare, the care planning is the process through which health care professionals or
practitioners and patient discuss, agree as well as review an action plan in order to accomplish the
goals or behaviour change relevance to the patient. In this report, the chosen organisation is National
Health Services which is a publicly funded healthcare system in United Kingdom. This report covers
influence of theoretical models and methods of planning and assessment in practice in workplace.
Apart from this, implement clear plan in workplace in order to mitigate desired outcomes for
individuals. In addition to this, the report also review the benefits and challenges of planning person
centred care in the workplace. At last, it reflects on the impact of planning of care on practitioners,
family, individuals and carers in relation to own practice.
TASK 1
P1 Compare the different models of assessment and their implementation in healthcare
Health can be defined as the state of complete mental, physical and social wellbeing and not
merely infirmity or disease absence. For every human being, the enjoyment of highest attainable
health standard is one of the fundamental right, without distinction of political beliefs, social
conditions, race, religion and economic condition. There are different models of health assessment
which can be executed by healthcare professionals in their practice. Some of the models along with
their comparison are discussed below:
The social model of health: it is the model which is emerged from social model of disability,
that has been strongly advocated through disability rights movement. The social model of health was
developed as reaction to traditional health model, i.e., medical model of health. The social health
model examines all the factors or elements that contributes to health including political, environment,
cultural and social factors. One of the example includes poor housing, low self-esteem and stress can
have adverse influence on health. Low self-esteem as well as low levels of autonomy are possibly to
relate to worse health. It is believed that the community know that the health of people being affected
by different issues. CDHN believes that communities can and must be actively involved in
determining, planning, designing as well as execute solutions to the issues associated with health and
unjust inequalities in health.
It is clearly recognised in the model that the health of a person is influenced through different
interpersonal, environmental, individual, economic, political and social factors. The senior carer in the
health care setting like National Health Services execute social model of health in order to determine
the interaction between the factors and other social influences on health of an individual. This leads to
dramatic differences in health among the various population groups. execution of social model of
health encourage the healthcare professionals to adopt a far ranging and deep perspective on health as
well as to address the political, cultural and social issues that impact on health in an effective way.
The social view regarding health implies that people must intervene to alter those aspects of
environment which promote ill health instead of continue to exhort people to alter their lifestyles and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

attitudes or continue to deal with illness after it appears when, in fact, the surroundings in which the
live as well as work provides them with little or no support or choice for making such alterations.
The medical model of health: this model was developed in 18th century, during age of
enlightenment, when traditional natural sciences initiate to dominate Medical and academia practice.
According to the medical model, the belief that science could cure the diseases and illness has
remained a core component of modern medicine. This health concept might be easy to understand the
model makes health an attribute that can measure simply through identifying if a disease or illness is
present or not. Yet, strong emphasis on the lack of disease or illness as a good health indicator as well
as the over dependence on impact of Medical Science on health, ignore the other important influence's
power. This model suggest that a disease is identified and detected by systematic process of
description, differentiation and observation, according to standard accepted procedures like medical
examinations, set of symptom descriptions or test. In this model, health is viewed as disease absence
and describes approach to illness that is dominant in western medicine. According to this model,
human body is treated as complex mechanism and through the use of medical procedures and
intervention, it advocates the treatment of symptom. The execution of medical model in healthcare
settings can help the health care professionals’ in treating the illness through medical intervention.
Comparison between social model of health and medical model of health
According to the above discussion, it can be said that the social model of health places
significance on changes which requires to be made through society by empowering individuals to be
in charge of on lifestyles and health in order to stay healthy. Whereas, according to medical model,
health is absence of disease. It informs the influential or powerful discourse about health. Apart from
this, the key components of social model of health include social, economic and environmental
factors. Whereas, the key elements of medical model include standard analytical format process. It is
broadly accepted that the social model of health focuses on alterations in society as well as way of
living of people to make the population healthy. In comparison, the medical model emphasizes on
eradication of illness by diagnosis as well as effective treatment. However, execution of both the
models will help health care professionals in improving the health outcomes of society or community
and enable people to live healthy lives.
P2 Discuss the application of theoretical perspectives to the care planning process in a healthcare
setting
In health care settings, there are some theoretical perspectives application of which can play a
crucial role in care planning process within a health care setting in organisation like National Health
Services. Some of the theoretical perspectives are discussed below:
1. Behavioural perspective: As per this perspective, behaviourism is distinct from other
approaches as they view individuals as controlled through the environment and particularly
that what the individual is, is the result of what they learnt from the environment. This
perspective is concerned with the way environmental forces affect observable behaviour. It
live as well as work provides them with little or no support or choice for making such alterations.
The medical model of health: this model was developed in 18th century, during age of
enlightenment, when traditional natural sciences initiate to dominate Medical and academia practice.
According to the medical model, the belief that science could cure the diseases and illness has
remained a core component of modern medicine. This health concept might be easy to understand the
model makes health an attribute that can measure simply through identifying if a disease or illness is
present or not. Yet, strong emphasis on the lack of disease or illness as a good health indicator as well
as the over dependence on impact of Medical Science on health, ignore the other important influence's
power. This model suggest that a disease is identified and detected by systematic process of
description, differentiation and observation, according to standard accepted procedures like medical
examinations, set of symptom descriptions or test. In this model, health is viewed as disease absence
and describes approach to illness that is dominant in western medicine. According to this model,
human body is treated as complex mechanism and through the use of medical procedures and
intervention, it advocates the treatment of symptom. The execution of medical model in healthcare
settings can help the health care professionals’ in treating the illness through medical intervention.
Comparison between social model of health and medical model of health
According to the above discussion, it can be said that the social model of health places
significance on changes which requires to be made through society by empowering individuals to be
in charge of on lifestyles and health in order to stay healthy. Whereas, according to medical model,
health is absence of disease. It informs the influential or powerful discourse about health. Apart from
this, the key components of social model of health include social, economic and environmental
factors. Whereas, the key elements of medical model include standard analytical format process. It is
broadly accepted that the social model of health focuses on alterations in society as well as way of
living of people to make the population healthy. In comparison, the medical model emphasizes on
eradication of illness by diagnosis as well as effective treatment. However, execution of both the
models will help health care professionals in improving the health outcomes of society or community
and enable people to live healthy lives.
P2 Discuss the application of theoretical perspectives to the care planning process in a healthcare
setting
In health care settings, there are some theoretical perspectives application of which can play a
crucial role in care planning process within a health care setting in organisation like National Health
Services. Some of the theoretical perspectives are discussed below:
1. Behavioural perspective: As per this perspective, behaviourism is distinct from other
approaches as they view individuals as controlled through the environment and particularly
that what the individual is, is the result of what they learnt from the environment. This
perspective is concerned with the way environmental forces affect observable behaviour. It
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
proposes two main processes where by individuals learn from environment including operant
conditioning and classical conditioning. It rejects the idea that individuals have free will as
well as believes that the environment is responsible for all behaviours of individuals.
Execution of behavioural perspective at the time of care planning by the healthcare
professionals within healthcare settings help in determining the impact of lifestyle behaviours
on health.
2. Sociological perspective: the perspective of health focuses that the behaviours, attitudes and
life chances of an individual is relying on their social background. As the sociology deals in
generalizations, individuals do not always think and behave in the patterns which sociologists
predict. Media, common sense and personal experience are the valuable knowledge sources
regarding different aspects of society. The theoretical perspective divided into micro and
macro views. The conflict theory emphasizes on conflict among distinct social, racial and
ethnic class as well as other groups and focuses on the way social institutions assist in
ensuring inequality. The functionalism perspective focuses on the functions which social
institutions serve to make sure the ongoing stability of society. Implementation of this
perspective in relation to healthcare assist care professionals during care planning to
emphasize on the influence of social backgrounds on behaviour and attitudes of people and
provide them with appropriate care and support.
TASK 2
P3 Discuss responsibilities and duties of own role in promoting person-centred care planning
The rising demand of healthcare often causes care providers to lose sight of the person behind
the condition they’re treating. This is why person-centred care is so important. It helps carers refocus
on a crucial aspect of care: fulfilling a patient’s needs beyond their disability or ailment. The health
and social care sector is increasingly adopting a person-centred care approach, and rightly so. Not
only does it help patients receive better quality care, but it also improves healthcare settings as a
whole.
Example of Person-Centred Care
Malcolm is a 27 year old inpatient who was recently in a car accident. He had to undergo
surgery for both his arms that suffered severe injuries during the crash. He needs to remain in hospital
for two more weeks before discharge, which means he will rely on others for a significant amount of
his daily care.
Care plan
PATIENTS MEDICAL INFORMATION
conditioning and classical conditioning. It rejects the idea that individuals have free will as
well as believes that the environment is responsible for all behaviours of individuals.
Execution of behavioural perspective at the time of care planning by the healthcare
professionals within healthcare settings help in determining the impact of lifestyle behaviours
on health.
2. Sociological perspective: the perspective of health focuses that the behaviours, attitudes and
life chances of an individual is relying on their social background. As the sociology deals in
generalizations, individuals do not always think and behave in the patterns which sociologists
predict. Media, common sense and personal experience are the valuable knowledge sources
regarding different aspects of society. The theoretical perspective divided into micro and
macro views. The conflict theory emphasizes on conflict among distinct social, racial and
ethnic class as well as other groups and focuses on the way social institutions assist in
ensuring inequality. The functionalism perspective focuses on the functions which social
institutions serve to make sure the ongoing stability of society. Implementation of this
perspective in relation to healthcare assist care professionals during care planning to
emphasize on the influence of social backgrounds on behaviour and attitudes of people and
provide them with appropriate care and support.
TASK 2
P3 Discuss responsibilities and duties of own role in promoting person-centred care planning
The rising demand of healthcare often causes care providers to lose sight of the person behind
the condition they’re treating. This is why person-centred care is so important. It helps carers refocus
on a crucial aspect of care: fulfilling a patient’s needs beyond their disability or ailment. The health
and social care sector is increasingly adopting a person-centred care approach, and rightly so. Not
only does it help patients receive better quality care, but it also improves healthcare settings as a
whole.
Example of Person-Centred Care
Malcolm is a 27 year old inpatient who was recently in a car accident. He had to undergo
surgery for both his arms that suffered severe injuries during the crash. He needs to remain in hospital
for two more weeks before discharge, which means he will rely on others for a significant amount of
his daily care.
Care plan
PATIENTS MEDICAL INFORMATION
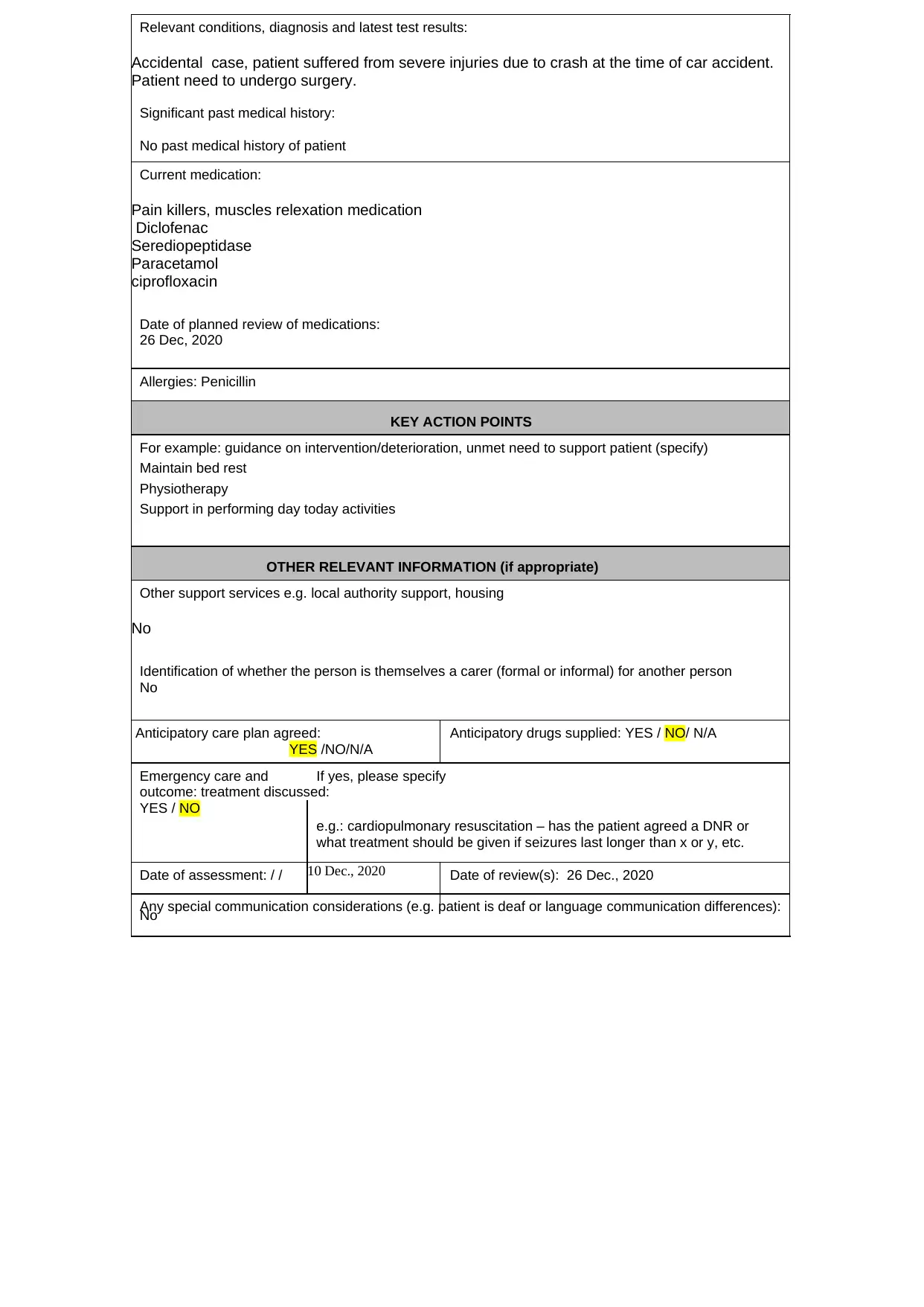
Relevant conditions, diagnosis and latest test results:
Accidental case, patient suffered from severe injuries due to crash at the time of car accident.
Patient need to undergo surgery.
Significant past medical history:
No past medical history of patient
Current medication:
Pain killers, muscles relexation medication
Diclofenac
Serediopeptidase
Paracetamol
ciprofloxacin
Date of planned review of medications:
26 Dec, 2020
Allergies: Penicillin
KEY ACTION POINTS
For example: guidance on intervention/deterioration, unmet need to support patient (specify)
Maintain bed rest
Physiotherapy
Support in performing day today activities
OTHER RELEVANT INFORMATION (if appropriate)
Other support services e.g. local authority support, housing
No
Identification of whether the person is themselves a carer (formal or informal) for another person
No
Anticipatory care plan agreed:
YES /NO/N/A
Anticipatory drugs supplied: YES / NO/ N/A
Emergency care and If yes, please specify
outcome: treatment discussed:
YES / NO
e.g.: cardiopulmonary resuscitation – has the patient agreed a DNR or
what treatment should be given if seizures last longer than x or y, etc.
Date of assessment: / / 10 Dec., 2020 Date of review(s): 26 Dec., 2020
Any special communication considerations (e.g. patient is deaf or language communication differences):
No
Accidental case, patient suffered from severe injuries due to crash at the time of car accident.
Patient need to undergo surgery.
Significant past medical history:
No past medical history of patient
Current medication:
Pain killers, muscles relexation medication
Diclofenac
Serediopeptidase
Paracetamol
ciprofloxacin
Date of planned review of medications:
26 Dec, 2020
Allergies: Penicillin
KEY ACTION POINTS
For example: guidance on intervention/deterioration, unmet need to support patient (specify)
Maintain bed rest
Physiotherapy
Support in performing day today activities
OTHER RELEVANT INFORMATION (if appropriate)
Other support services e.g. local authority support, housing
No
Identification of whether the person is themselves a carer (formal or informal) for another person
No
Anticipatory care plan agreed:
YES /NO/N/A
Anticipatory drugs supplied: YES / NO/ N/A
Emergency care and If yes, please specify
outcome: treatment discussed:
YES / NO
e.g.: cardiopulmonary resuscitation – has the patient agreed a DNR or
what treatment should be given if seizures last longer than x or y, etc.
Date of assessment: / / 10 Dec., 2020 Date of review(s): 26 Dec., 2020
Any special communication considerations (e.g. patient is deaf or language communication differences):
No
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Any special physical or medical considerations (e.g. specific postural or support needs or information
about medical condition – patient needs at least x mgs of drug before it works, etc.):
Timely medications
SIGNATORIES (if appropriate and / or possible)
Patient signature:
Date:
Carer (if applicable) signature:
Date:
Named accountable GP signature:
Date:
Care Coordinator signature (if applicable):
Date:
The care plan provided above for Malcolm helps in his early recovery and also helps in
treating his injury in an effective way. Apart from this, this plan assisted in make him able perform his
day to day activities appropriately. My duties and responsibilities in promoting care plan and person
centred approach is very important. I play the role of an educator in promoting care plan. I spend
much of the time with patient and administer him anticipatory guidance regarding safety, medications,
immunizations and nutrition. With the help of my skills and competencies, I provided patient with
proper care and safety. I also ensure that the patient is treated with dignity and respect and all the
personal information must be kept confidential while providing care to the patient.
Example 2:
Mrs. Landry is an old resident who was 80 years old and had a severe stroke yesterday. Mrs.
Linda is unconscious as well as receiving palliative care. During her admission two years ago, she and
her family discussed on her DNR status and requested a DNR order with comfort measures only.
Care plan:
about medical condition – patient needs at least x mgs of drug before it works, etc.):
Timely medications
SIGNATORIES (if appropriate and / or possible)
Patient signature:
Date:
Carer (if applicable) signature:
Date:
Named accountable GP signature:
Date:
Care Coordinator signature (if applicable):
Date:
The care plan provided above for Malcolm helps in his early recovery and also helps in
treating his injury in an effective way. Apart from this, this plan assisted in make him able perform his
day to day activities appropriately. My duties and responsibilities in promoting care plan and person
centred approach is very important. I play the role of an educator in promoting care plan. I spend
much of the time with patient and administer him anticipatory guidance regarding safety, medications,
immunizations and nutrition. With the help of my skills and competencies, I provided patient with
proper care and safety. I also ensure that the patient is treated with dignity and respect and all the
personal information must be kept confidential while providing care to the patient.
Example 2:
Mrs. Landry is an old resident who was 80 years old and had a severe stroke yesterday. Mrs.
Linda is unconscious as well as receiving palliative care. During her admission two years ago, she and
her family discussed on her DNR status and requested a DNR order with comfort measures only.
Care plan:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
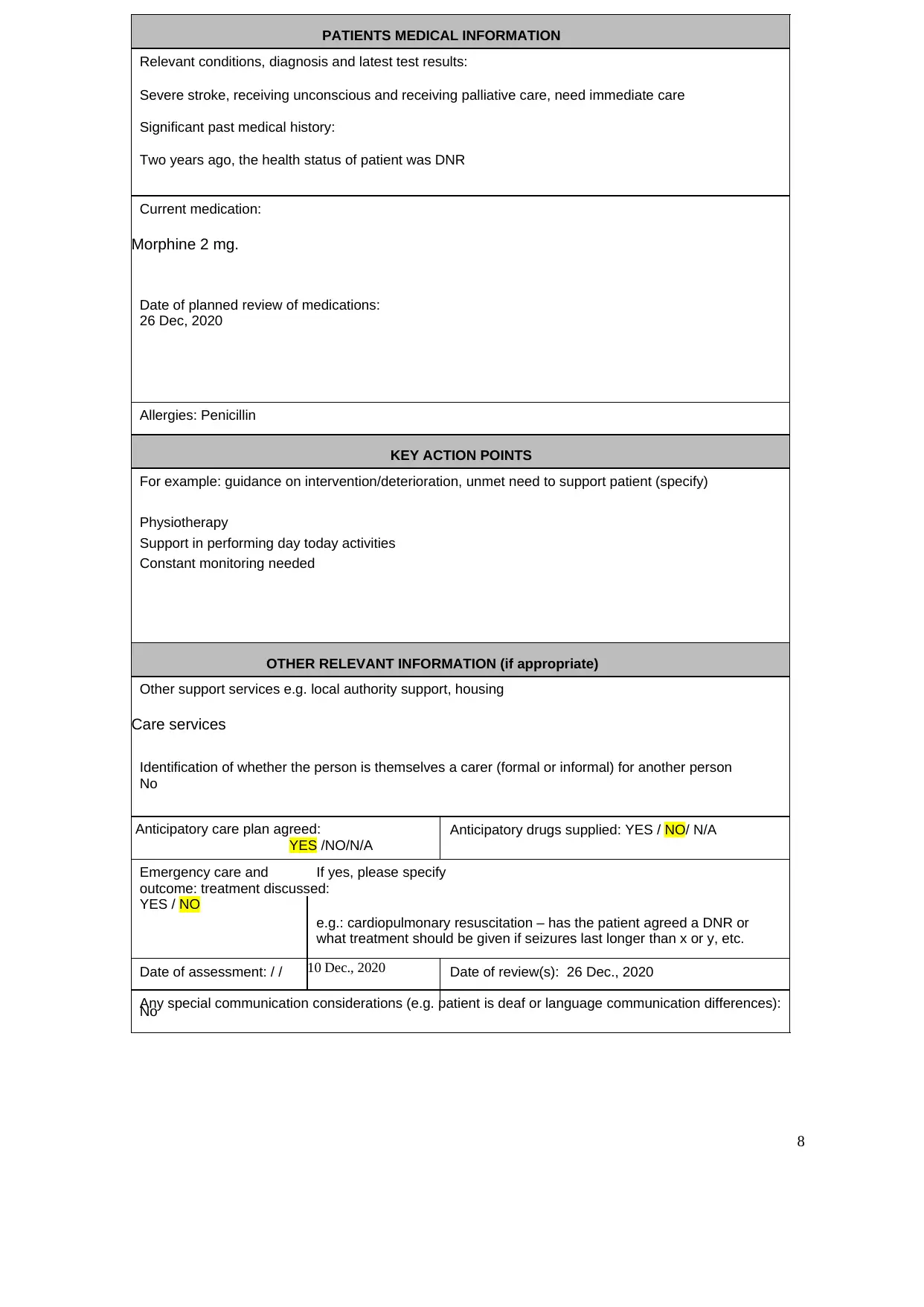
PATIENTS MEDICAL INFORMATION
Relevant conditions, diagnosis and latest test results:
Severe stroke, receiving unconscious and receiving palliative care, need immediate care
Significant past medical history:
Two years ago, the health status of patient was DNR
Current medication:
Morphine 2 mg.
Date of planned review of medications:
26 Dec, 2020
Allergies: Penicillin
KEY ACTION POINTS
For example: guidance on intervention/deterioration, unmet need to support patient (specify)
Physiotherapy
Support in performing day today activities
Constant monitoring needed
OTHER RELEVANT INFORMATION (if appropriate)
Other support services e.g. local authority support, housing
Care services
Identification of whether the person is themselves a carer (formal or informal) for another person
No
Anticipatory care plan agreed:
YES /NO/N/A
Anticipatory drugs supplied: YES / NO/ N/A
Emergency care and If yes, please specify
outcome: treatment discussed:
YES / NO
e.g.: cardiopulmonary resuscitation – has the patient agreed a DNR or
what treatment should be given if seizures last longer than x or y, etc.
Date of assessment: / / 10 Dec., 2020 Date of review(s): 26 Dec., 2020
Any special communication considerations (e.g. patient is deaf or language communication differences):
No
8
Relevant conditions, diagnosis and latest test results:
Severe stroke, receiving unconscious and receiving palliative care, need immediate care
Significant past medical history:
Two years ago, the health status of patient was DNR
Current medication:
Morphine 2 mg.
Date of planned review of medications:
26 Dec, 2020
Allergies: Penicillin
KEY ACTION POINTS
For example: guidance on intervention/deterioration, unmet need to support patient (specify)
Physiotherapy
Support in performing day today activities
Constant monitoring needed
OTHER RELEVANT INFORMATION (if appropriate)
Other support services e.g. local authority support, housing
Care services
Identification of whether the person is themselves a carer (formal or informal) for another person
No
Anticipatory care plan agreed:
YES /NO/N/A
Anticipatory drugs supplied: YES / NO/ N/A
Emergency care and If yes, please specify
outcome: treatment discussed:
YES / NO
e.g.: cardiopulmonary resuscitation – has the patient agreed a DNR or
what treatment should be given if seizures last longer than x or y, etc.
Date of assessment: / / 10 Dec., 2020 Date of review(s): 26 Dec., 2020
Any special communication considerations (e.g. patient is deaf or language communication differences):
No
8
Any special physical or medical considerations (e.g. specific postural or support needs or information
about medical condition – patient needs at least x mgs of drug before it works, etc.):
Timely medications
SIGNATORIES (if appropriate and / or possible)
Patient signature:
Date:
Carer (if applicable) signature:
Date:
Named accountable GP signature:
Date:
Care Coordinator signature (if applicable):
Date:
about medical condition – patient needs at least x mgs of drug before it works, etc.):
Timely medications
SIGNATORIES (if appropriate and / or possible)
Patient signature:
Date:
Carer (if applicable) signature:
Date:
Named accountable GP signature:
Date:
Care Coordinator signature (if applicable):
Date:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

In the case of Mrs. Landry, my role and responsibility in promoting care plan and person
centred care is to consistently work with the patient to prevent illness like stroke and other
diseases by educating them, preventing the risk factor and monitoring of safety hazards. I ensure
that patient receive holistic care which is required for optimal outcomes.
P4 Demonstrate own contribution to the care planning process and use of care plans in the setting
In the process of delivering care to the patients, families are considered as partners. Family
play a crucial role in providing treatment to patient, since it can render effective emotional and
psychological support to the patient who is undergoing treatment within health care settings.
Illness of patient can threaten the system. The outcome of threat of system can involve feeling of
weakness, lack of hope, fear and distress can lead to emotional and physical exhaustion. For this
cause, each intervention which declines the effect of the pressures, benefits family. The
reciprocal impact takes place due to family in social system that is constituted through people
interacting with each other. Therefore, any change in system impacts its stability. Since, system
is constituted by family; illness of patient has direct impact on all system. In the evaluation of
care process, individual and family play a significant role and contribute highly in developing
effective care services.
TASK 3
P5 Discuss the barriers to implementing care planning in the setting
There are several barriers which are faced by care professionals at the time of executing
care planning within the healthcare setting. Some of the barriers are discussed below:
1. Traditional practices and structures: this is one among the barrier which senior care face
in National Health Services while implementing care planning. The professionals work as
per the traditional care pathways limits the freedom to do things or provide care
differently than usual care. At the time of implementation of care planning, the ability to
work with flexibility and using different strategies is the prerequisite. But, the existing
power relationships developed around physicians invariably is perceived as barrier in
implementing care planning.
2. Lack of knowledge: in order to do care planning in proper manner, it is very necessary
for the senior care of National Health Services to have appropriate knowledge regarding
1
centred care is to consistently work with the patient to prevent illness like stroke and other
diseases by educating them, preventing the risk factor and monitoring of safety hazards. I ensure
that patient receive holistic care which is required for optimal outcomes.
P4 Demonstrate own contribution to the care planning process and use of care plans in the setting
In the process of delivering care to the patients, families are considered as partners. Family
play a crucial role in providing treatment to patient, since it can render effective emotional and
psychological support to the patient who is undergoing treatment within health care settings.
Illness of patient can threaten the system. The outcome of threat of system can involve feeling of
weakness, lack of hope, fear and distress can lead to emotional and physical exhaustion. For this
cause, each intervention which declines the effect of the pressures, benefits family. The
reciprocal impact takes place due to family in social system that is constituted through people
interacting with each other. Therefore, any change in system impacts its stability. Since, system
is constituted by family; illness of patient has direct impact on all system. In the evaluation of
care process, individual and family play a significant role and contribute highly in developing
effective care services.
TASK 3
P5 Discuss the barriers to implementing care planning in the setting
There are several barriers which are faced by care professionals at the time of executing
care planning within the healthcare setting. Some of the barriers are discussed below:
1. Traditional practices and structures: this is one among the barrier which senior care face
in National Health Services while implementing care planning. The professionals work as
per the traditional care pathways limits the freedom to do things or provide care
differently than usual care. At the time of implementation of care planning, the ability to
work with flexibility and using different strategies is the prerequisite. But, the existing
power relationships developed around physicians invariably is perceived as barrier in
implementing care planning.
2. Lack of knowledge: in order to do care planning in proper manner, it is very necessary
for the senior care of National Health Services to have appropriate knowledge regarding
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
issues faced by patients, their past medical history, current status of health etc. Lack of
knowledge is one of the key barrier in executing care planning in a proper way.
3. Insufficient time: this is the another barrier faced by senior care in National Health
Services as insufficient time constrained the delivery of care. In developing proper care
plan and executing it in an appropriate way, having sufficient time is very necessary. But,
not having sufficient time may increase the chances of errors and unable senior care to
execute the care planning in an effective and efficient way.
P6 Review the benefits of the use of care plans in ensuring the needs of the individual are
prioritised
The nursing care plan can be referred as the formal document which includes information
that easily defines supports and services that are being given to a person. It is a formal process
which involves correctly determining existing needs and recognising potential needs. It gives a
means of communication among patients, nurses and other health care providers to accomplish
effective outcomes of Health Care. Without proper care planning, consistency and quality in
patient care will be lost. There are several benefits of use of care plans in making sure that the
needs of individuals are prioritized. Some of the benefits of use of care plan by senior care of
National Health Services are provided below:
1. Care plan helps in ensuring and promoting evidence-based care and provide familiar and
pleasant conditions in health care centres.
2. It supports holistic care that includes full individual including psychological, spiritual,
physical and social in relation to management as well as prevention of disease.
3. The care planning works across diverse populations, therefore addressing the inequalities
in an appropriate way.
4. The care planning takes time in order to embed. Alterations in clinical indicators across
people might see after two of three cycles of care planning.
5. This improve the skills and knowledge of professionals reported, and ensure greater job
satisfaction.
6. Care plan also help in providing the patient with appropriate care so as to ensure positive
health outcomes.
7. Apart from this, it assists in ensuring that care is provided to individuals as per their
needs and preferences and prioritized accordingly.
2
knowledge is one of the key barrier in executing care planning in a proper way.
3. Insufficient time: this is the another barrier faced by senior care in National Health
Services as insufficient time constrained the delivery of care. In developing proper care
plan and executing it in an appropriate way, having sufficient time is very necessary. But,
not having sufficient time may increase the chances of errors and unable senior care to
execute the care planning in an effective and efficient way.
P6 Review the benefits of the use of care plans in ensuring the needs of the individual are
prioritised
The nursing care plan can be referred as the formal document which includes information
that easily defines supports and services that are being given to a person. It is a formal process
which involves correctly determining existing needs and recognising potential needs. It gives a
means of communication among patients, nurses and other health care providers to accomplish
effective outcomes of Health Care. Without proper care planning, consistency and quality in
patient care will be lost. There are several benefits of use of care plans in making sure that the
needs of individuals are prioritized. Some of the benefits of use of care plan by senior care of
National Health Services are provided below:
1. Care plan helps in ensuring and promoting evidence-based care and provide familiar and
pleasant conditions in health care centres.
2. It supports holistic care that includes full individual including psychological, spiritual,
physical and social in relation to management as well as prevention of disease.
3. The care planning works across diverse populations, therefore addressing the inequalities
in an appropriate way.
4. The care planning takes time in order to embed. Alterations in clinical indicators across
people might see after two of three cycles of care planning.
5. This improve the skills and knowledge of professionals reported, and ensure greater job
satisfaction.
6. Care plan also help in providing the patient with appropriate care so as to ensure positive
health outcomes.
7. Apart from this, it assists in ensuring that care is provided to individuals as per their
needs and preferences and prioritized accordingly.
2
TASK 4
P7 Discuss the ways in which the individual and family contributes to evaluation of the care
process
In the process of delivering care to the patients, families are considered as partners. Family
play a crucial role in providing treatment to patient, since it can render effective emotional and
psychological support to the patient who is undergoing treatment within health care settings.
Illness of patient can threaten the system. The outcome of threat of system can involve feeling of
weakness, lack of hope, fear and distress can lead to emotional and physical exhaustion. For this
cause, each intervention which decline the effect of the pressures, benefits family. The reciprocal
impact takes place due to family in social system, that is constituted through people interacting
with each other. Therefore, any change in system impacts its stability. Since, system is
constituted by family, illness of patient has direct impact on all system. In the evaluation of care
process, individual and family play a significant role and contribute highly in developing
effective care services.
Presence of family at the time of hospitalization of patient strengthened through the
perception of holistic care. The doctors, nurses, visitors and patient have expressed common
opinion regarding positive contribution a family on patient care in the hospital. The family
members of the patient constitute as an important source of emotional and psychological support
for patient. The family perform some crucial activities during the hospitalisation of patient which
contribute in evolution of care process. The family act as representation of patient as well as
informing them about subject concerning them. They participate in the planning of care of
patient and maintain communication of patient with family members and relatives. By providing
the appropriate support and information, family health care providers to deliver effective care
and accomplish positive responses from the patient.
P8 Review aspects of the care planning process and their impact upon the individual, family and
carers
Care planning is the process of developing a care plan for an individual by setting
patient-centric goals, developing strategies, outlining tasks and setting schedules in order to
accomplish the goals.
Here are four key steps to care planning:
3
P7 Discuss the ways in which the individual and family contributes to evaluation of the care
process
In the process of delivering care to the patients, families are considered as partners. Family
play a crucial role in providing treatment to patient, since it can render effective emotional and
psychological support to the patient who is undergoing treatment within health care settings.
Illness of patient can threaten the system. The outcome of threat of system can involve feeling of
weakness, lack of hope, fear and distress can lead to emotional and physical exhaustion. For this
cause, each intervention which decline the effect of the pressures, benefits family. The reciprocal
impact takes place due to family in social system, that is constituted through people interacting
with each other. Therefore, any change in system impacts its stability. Since, system is
constituted by family, illness of patient has direct impact on all system. In the evaluation of care
process, individual and family play a significant role and contribute highly in developing
effective care services.
Presence of family at the time of hospitalization of patient strengthened through the
perception of holistic care. The doctors, nurses, visitors and patient have expressed common
opinion regarding positive contribution a family on patient care in the hospital. The family
members of the patient constitute as an important source of emotional and psychological support
for patient. The family perform some crucial activities during the hospitalisation of patient which
contribute in evolution of care process. The family act as representation of patient as well as
informing them about subject concerning them. They participate in the planning of care of
patient and maintain communication of patient with family members and relatives. By providing
the appropriate support and information, family health care providers to deliver effective care
and accomplish positive responses from the patient.
P8 Review aspects of the care planning process and their impact upon the individual, family and
carers
Care planning is the process of developing a care plan for an individual by setting
patient-centric goals, developing strategies, outlining tasks and setting schedules in order to
accomplish the goals.
Here are four key steps to care planning:
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





