NSG3NCR Project Part B: Clinical Project on Healthcare Communication
VerifiedAdded on 2020/11/23
|17
|3124
|53
Project
AI Summary
This project, part of the NSG3NCR course, presents a comprehensive analysis of healthcare communication standards, focusing on their impact on patient safety and clinical practices. The project begins with a literature review that examines the barriers and facilitators influencing changes in clinical practices, referencing the case of Ysabel Green to highlight the importance of patient involvement and communication. It explores factors like the gap between research and implementation, lack of cooperation, and information constraints as barriers, while identifying feedback, training, and resource availability as facilitators. The project then details a project plan, including the project outline, target audience (registered nurses), recommendations, presentation format (PowerPoint), and feedback approach (questionnaires). The presentation itself is included, followed by an evaluation of feedback using a questionnaire designed to gauge the audience's understanding of patient involvement in clinical decisions and the need for changes in clinical practices. The project emphasizes the need for healthcare professionals to prioritize patient communication, information sharing, and involvement in their care, to improve patient outcomes and safety.
Project part B
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TABLE OF CONTENTS
SECTION 1: Literature Review ......................................................................................................1
Introduction......................................................................................................................................1
Review.............................................................................................................................................1
Conclusion ......................................................................................................................................4
SECTION 2 : PROJECT PLAN .....................................................................................................4
Project outline: ...........................................................................................................................4
Target audience: .........................................................................................................................4
Recommendations and suggestions: ..........................................................................................5
Presentation format: ...................................................................................................................5
Feedback approach: ....................................................................................................................5
SECTION 3: PRESENTATION .....................................................................................................5
SECTION 4: EVALUATION OF FEEDBACK ..........................................................................12
REFERENCES .............................................................................................................................14
SECTION 1: Literature Review ......................................................................................................1
Introduction......................................................................................................................................1
Review.............................................................................................................................................1
Conclusion ......................................................................................................................................4
SECTION 2 : PROJECT PLAN .....................................................................................................4
Project outline: ...........................................................................................................................4
Target audience: .........................................................................................................................4
Recommendations and suggestions: ..........................................................................................5
Presentation format: ...................................................................................................................5
Feedback approach: ....................................................................................................................5
SECTION 3: PRESENTATION .....................................................................................................5
SECTION 4: EVALUATION OF FEEDBACK ..........................................................................12
REFERENCES .............................................................................................................................14
SECTION 1: Literature Review
Introduction
For regularly improving the quality of health care services and to meet the national safety
standards it is essential that clinical practices must involve the changes. According to Peterson &
et.al., (2015), advancements in the clinical practices leads to the better and desired output related
to health quality of individuals. In the case study of Ysabel Green it was observed that national
safety standard of partnering with consumer was not followed. Due to this Ysabel and her
husband both were very troubled and confused about the clinical procedures which were going
on. It affected the psychological state of the patient as well. This literature review will analyse
the barriers and facilitators involved in changing clinical practices for further improvement
(Clinton & LaCross, 2017). It will also evaluate the impact of these factors on clinical practices
in case of Ysabel's care.
Review
DiCenso, Guyatt & Ciliska (2014) states that, it is critical task for the healthcare
professionals to implement changes in their clinical practices. However, for sustaining the
quality healthcare it is required that these changes must be supported as per demand. For
instance, Ysabel and her husband were not included in any of the decision making during her
treatment. If they were also involved in decision making then, probably her health condition
would have been more qualitative.
In the given case study the quality of health services provided is not effective. It does not
follow the standards of national safety. To avoid such incidences in future it is necessary for
health care providers to consider the need for change in their clinical practices (Dang &
Dearholt, 2017). These changes will enable the health institutes to keep the patient safety at the
priority and to follow all necessary standards of safety and quality. In the view of Jun, Kovner &
Stimpfel (2016), changes in clinical practices will help professionals to identify the needs of their
patients so that appropriate treatment can be provided to them with minimum risks. However,
there are certain factors which influences the ways to implement changes in clinical practices.
Barriers of implementing changes in clinical practices: There are several factors which acts as
barriers to the changes.
Gap between research and implementation:
1
Introduction
For regularly improving the quality of health care services and to meet the national safety
standards it is essential that clinical practices must involve the changes. According to Peterson &
et.al., (2015), advancements in the clinical practices leads to the better and desired output related
to health quality of individuals. In the case study of Ysabel Green it was observed that national
safety standard of partnering with consumer was not followed. Due to this Ysabel and her
husband both were very troubled and confused about the clinical procedures which were going
on. It affected the psychological state of the patient as well. This literature review will analyse
the barriers and facilitators involved in changing clinical practices for further improvement
(Clinton & LaCross, 2017). It will also evaluate the impact of these factors on clinical practices
in case of Ysabel's care.
Review
DiCenso, Guyatt & Ciliska (2014) states that, it is critical task for the healthcare
professionals to implement changes in their clinical practices. However, for sustaining the
quality healthcare it is required that these changes must be supported as per demand. For
instance, Ysabel and her husband were not included in any of the decision making during her
treatment. If they were also involved in decision making then, probably her health condition
would have been more qualitative.
In the given case study the quality of health services provided is not effective. It does not
follow the standards of national safety. To avoid such incidences in future it is necessary for
health care providers to consider the need for change in their clinical practices (Dang &
Dearholt, 2017). These changes will enable the health institutes to keep the patient safety at the
priority and to follow all necessary standards of safety and quality. In the view of Jun, Kovner &
Stimpfel (2016), changes in clinical practices will help professionals to identify the needs of their
patients so that appropriate treatment can be provided to them with minimum risks. However,
there are certain factors which influences the ways to implement changes in clinical practices.
Barriers of implementing changes in clinical practices: There are several factors which acts as
barriers to the changes.
Gap between research and implementation:
1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
There are instances when health professionals find it difficult to adopt the changes. For
example in case of Ysabel nurses assumed that there is no need to involve patient and her family
in decision making to provide them information regarding the treatment procedure. Such
approach always prohibits the demand to implement changes in the clinical practices. According
to Williams, Perillo & Brown (2015), clinical practice provides the standards for design,
performance, analysis and monitoring of clinical trials. It is very complex process for the
individuals to adopt changes which can be implemented in all the above processes. The cost
limitations and feasibility servers as important barriers before implementing changes. For
instance clinical trials may require informing decisions and status of patient but they may not
have system or application for supporting it (Edvardsson, Watt & Pearce, 2017). The new
implementation will require budget consideration as well as approval from the management.
Lack of cooperation from top management and fellow members:
Whenever some changes are proposed they are highly criticised by the peer groups or
other health organisations. It is usually considered that these changes are not required or will
bring risk and are not useful. Hence, health groups discourage these clinical changes and does
not show positive response towards their implementation. Chamberlain, Pollock & Fulbrook,
(2018) states that the innovations and changes cannot be helpful in achieving goals if they are not
accomplished by all participants with same efforts. When clinical practices require amendments
then it is necessary that all associated groups such as patients, nurses and other health carers
equally cooperate with it. For instance when patients want to participate in decision making of
clinical trials but if nurses does not allow them or guide them with information then patient will
not be able to participate and hence no clinical changes will be observed (Tobiano & et.al.,
2015).
Information constraints: As per the discussion in Trevena & et.al., (2017) nurses maywant to
provide information to patients but they do not have much information. Hence, they are unable to
follow healthcare standards. Thus changes must be made in clinical approaches so that nurses
also have awareness regarding the health status of their patient.
Barriers related to management and decision making within health organisations: This is
significant barrier related to the above mentioned issue. Health organisation are satisfied with
their structure and procedures. They believe that there is no need to implement these changes and
2
example in case of Ysabel nurses assumed that there is no need to involve patient and her family
in decision making to provide them information regarding the treatment procedure. Such
approach always prohibits the demand to implement changes in the clinical practices. According
to Williams, Perillo & Brown (2015), clinical practice provides the standards for design,
performance, analysis and monitoring of clinical trials. It is very complex process for the
individuals to adopt changes which can be implemented in all the above processes. The cost
limitations and feasibility servers as important barriers before implementing changes. For
instance clinical trials may require informing decisions and status of patient but they may not
have system or application for supporting it (Edvardsson, Watt & Pearce, 2017). The new
implementation will require budget consideration as well as approval from the management.
Lack of cooperation from top management and fellow members:
Whenever some changes are proposed they are highly criticised by the peer groups or
other health organisations. It is usually considered that these changes are not required or will
bring risk and are not useful. Hence, health groups discourage these clinical changes and does
not show positive response towards their implementation. Chamberlain, Pollock & Fulbrook,
(2018) states that the innovations and changes cannot be helpful in achieving goals if they are not
accomplished by all participants with same efforts. When clinical practices require amendments
then it is necessary that all associated groups such as patients, nurses and other health carers
equally cooperate with it. For instance when patients want to participate in decision making of
clinical trials but if nurses does not allow them or guide them with information then patient will
not be able to participate and hence no clinical changes will be observed (Tobiano & et.al.,
2015).
Information constraints: As per the discussion in Trevena & et.al., (2017) nurses maywant to
provide information to patients but they do not have much information. Hence, they are unable to
follow healthcare standards. Thus changes must be made in clinical approaches so that nurses
also have awareness regarding the health status of their patient.
Barriers related to management and decision making within health organisations: This is
significant barrier related to the above mentioned issue. Health organisation are satisfied with
their structure and procedures. They believe that there is no need to implement these changes and
2
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
current practices are effective enough. When nurses, patients and other members encourage the
clinical changes but if these organisations does not sanction budgets or management does not
provide team to do so then goals cannot be achieved. When hospital management will permit the
changes only then, they can be implemented in clinical practices.
The above mentioned barriers are critical and greatly affect the clinical changes and
advancements.
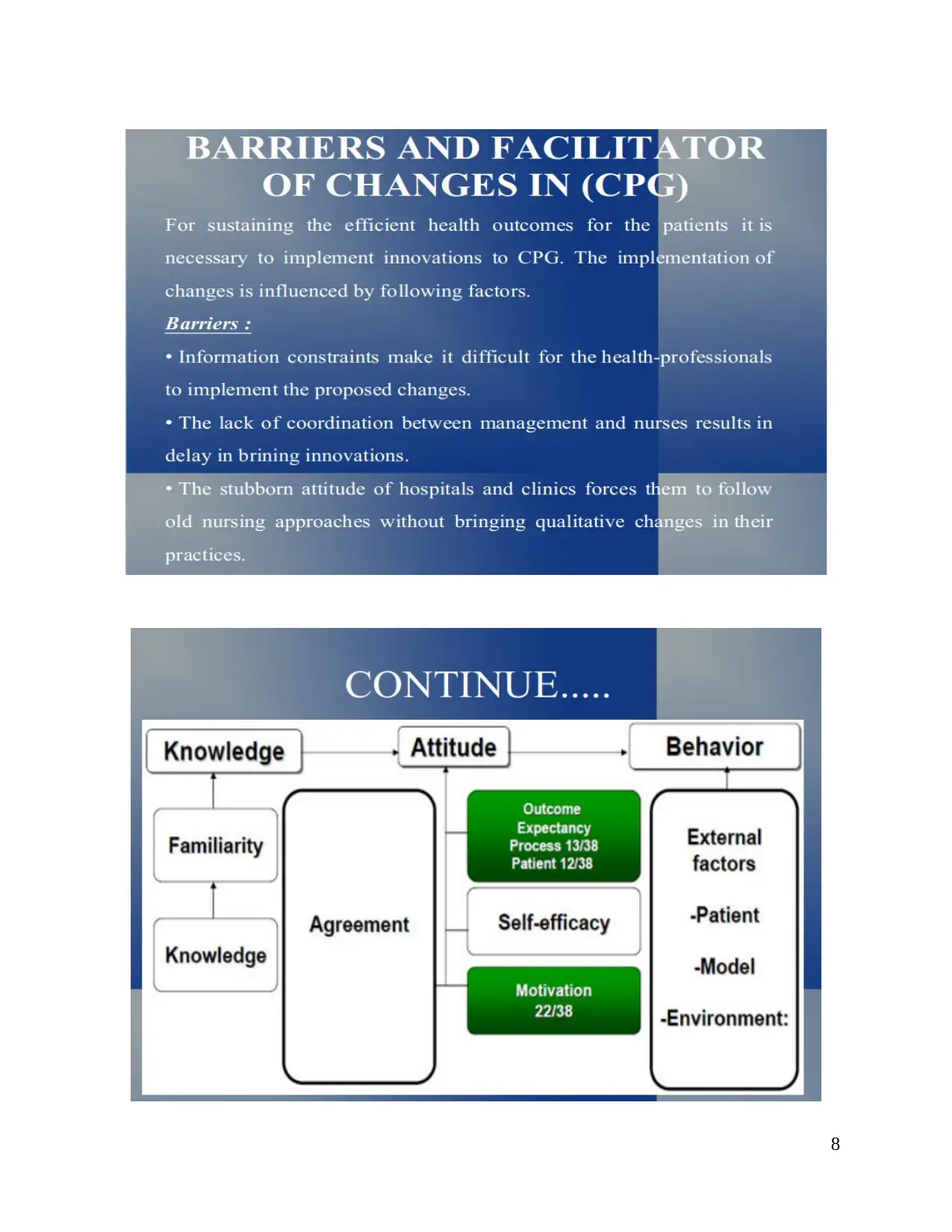
Facilitators to amendments in clinical practices:
There are various facilitators which promotes and encourages the need of clinical practice
amendments. According to Zanello & et.al., (2016), Rogers' Diffusion of innovation model,
adoption of new guidelines for clinical practices has following facilitators:
Feedbacks and flexible suggestions: At the persuasion stage nurses follow certain steps to
maintain the quality of practices. The quality can be assured by providing feedbacks and
suggestions. It promotes the clinical advancements so that quality of services can be sustained.
Empowerment and training sessions: When health service providers are trained regarding their
practices and duties they take more initiatives to improve the clinical practices. Like in case of
Ysabel if front line nurses were trained enough and were provided with adequate information of
patient then they would have able to properly communicate with the Ysabel's husband.
Resource availability and acceptance of innovation: Clinical practice guidelines (CPG) is
facilitated by availability of technical tools. Lúanaigh & Hughes, (2016) states that when health
organisations have sufficient resources then, it is easy for them to implement new changes.
Along with this the evidence-based strategies are more likely to bring productive results. The
changes in clinical practices as per CPG states the mandates and are encouraged by innovations.
Impact of barriers and facilitators on implementation of clinical changes:
As per discussion in Kadu & Stolee (2015), communication for safety standard is one of
the important safety standard. It states that health organisations must implement effective system
to communicate with patient, families and other multidisciplinary teams so that safety of patient
is not compromised. The feedbacks and empowerment will assure that nursing care providers are
liable to communicate with the patients and carers so that collective decision can be taken.
Ysabel and her husband were not informed about any complication or treatment approach. But if
3
clinical changes but if these organisations does not sanction budgets or management does not
provide team to do so then goals cannot be achieved. When hospital management will permit the
changes only then, they can be implemented in clinical practices.
The above mentioned barriers are critical and greatly affect the clinical changes and
advancements.
Facilitators to amendments in clinical practices:
There are various facilitators which promotes and encourages the need of clinical practice
amendments. According to Zanello & et.al., (2016), Rogers' Diffusion of innovation model,
adoption of new guidelines for clinical practices has following facilitators:
Feedbacks and flexible suggestions: At the persuasion stage nurses follow certain steps to
maintain the quality of practices. The quality can be assured by providing feedbacks and
suggestions. It promotes the clinical advancements so that quality of services can be sustained.
Empowerment and training sessions: When health service providers are trained regarding their
practices and duties they take more initiatives to improve the clinical practices. Like in case of
Ysabel if front line nurses were trained enough and were provided with adequate information of
patient then they would have able to properly communicate with the Ysabel's husband.
Resource availability and acceptance of innovation: Clinical practice guidelines (CPG) is
facilitated by availability of technical tools. Lúanaigh & Hughes, (2016) states that when health
organisations have sufficient resources then, it is easy for them to implement new changes.
Along with this the evidence-based strategies are more likely to bring productive results. The
changes in clinical practices as per CPG states the mandates and are encouraged by innovations.
Impact of barriers and facilitators on implementation of clinical changes:
As per discussion in Kadu & Stolee (2015), communication for safety standard is one of
the important safety standard. It states that health organisations must implement effective system
to communicate with patient, families and other multidisciplinary teams so that safety of patient
is not compromised. The feedbacks and empowerment will assure that nursing care providers are
liable to communicate with the patients and carers so that collective decision can be taken.
Ysabel and her husband were not informed about any complication or treatment approach. But if
3

nurses were empowered and trained to provide information then they might have informed her
husband.
Similarly, lack of resources can affect the clinical practices. The MRI of Ysabel was due
to shortage of staff on public holiday. It was possible to avoid such incidents if health institute
was aware regarding the prior arrangements of resources so that procedures were not delayed.
The postponed MRI leads to delay in treatment procedure and hence her situation degraded.
There must be a proper coordination between staff members so that carers are not confused and
well aware about procedures. As per the view of Tobiano & et.al., (2015) empowerment and
training session will make the clinical practices transparent and more effective. The patients will
also find it easy to manage the situation with ease.
Conclusion
The literature review has highlighted the importance of clinical practice guidelines. It has
also evaluated the different facilitators and barriers which affects the process of clinical changes.
Thus, it can be concluded from the literature review that for delivering the quality health care
services the national standards of health must be followed. In order to achieve this objective
changes must be implemented in practice guidelines of health-professionals.
SECTION 2 : PROJECT PLAN
Project outline:
The project will focus on the health standard of communication for safety. For providing
quality and accurate services it is essential that patient and carers must have knowledge about
treatment methods and its impact (Gill & et.al., 2015). Ysabel and her husband were not
informed about any of the safety consideration. The nursing staff gave her discharge after
providing medications without informing them about after discharge precautions or possible
risks. It resulted in more critical condition. If they both were informed about the situation then,
probably Ysabel's condition could have been improved. The presentation will highlight the
impact of the standard and how it can be crucial in health deterioration cases.
Target audience:
The project will be presented to health professionals especially registered nurses. It will
help them to understand the need and significance of the above quoted standard.
4
husband.
Similarly, lack of resources can affect the clinical practices. The MRI of Ysabel was due
to shortage of staff on public holiday. It was possible to avoid such incidents if health institute
was aware regarding the prior arrangements of resources so that procedures were not delayed.
The postponed MRI leads to delay in treatment procedure and hence her situation degraded.
There must be a proper coordination between staff members so that carers are not confused and
well aware about procedures. As per the view of Tobiano & et.al., (2015) empowerment and
training session will make the clinical practices transparent and more effective. The patients will
also find it easy to manage the situation with ease.
Conclusion
The literature review has highlighted the importance of clinical practice guidelines. It has
also evaluated the different facilitators and barriers which affects the process of clinical changes.
Thus, it can be concluded from the literature review that for delivering the quality health care
services the national standards of health must be followed. In order to achieve this objective
changes must be implemented in practice guidelines of health-professionals.
SECTION 2 : PROJECT PLAN
Project outline:
The project will focus on the health standard of communication for safety. For providing
quality and accurate services it is essential that patient and carers must have knowledge about
treatment methods and its impact (Gill & et.al., 2015). Ysabel and her husband were not
informed about any of the safety consideration. The nursing staff gave her discharge after
providing medications without informing them about after discharge precautions or possible
risks. It resulted in more critical condition. If they both were informed about the situation then,
probably Ysabel's condition could have been improved. The presentation will highlight the
impact of the standard and how it can be crucial in health deterioration cases.
Target audience:
The project will be presented to health professionals especially registered nurses. It will
help them to understand the need and significance of the above quoted standard.
4
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Recommendations and suggestions:
The project aims at providing message to nurses that communication for safety standard
must be integral part of their clinical practices. When carers and family members are not
involved in decision making patients may feel anxious and worried. This psychological effect
affects the quality of nursing to a great extent. Thus, health service providers must ensure that
they must regularly inform the status and need of procedures to the patients and carers (Dang &
Dearholt, 2017). It will help them to relax and better recovery will be observed. Another point of
consideration is that individuals have the right to know about their well beings and risks related
to the clinical approaches. Hence, nurses must acknowledge them with adequate information.
Presentation format:
The power point format has been intended to use for presenting this project. The
presentation format highlights the key issues and provides a chance to audience to question or
comment. When their questions are addressed orally in front of them then, it gives better
understanding to them and message is delivered successfully (Pereira & et.al., 2014).
Feedback approach:
For evaluating the effectiveness of the presentation it is necessary to evaluate the
feedbacks from the audience. For obtaining feedback from the users the various evaluation tools
can be used. For this purpose surveys such as questionnaires can be used. This evaluation tool
will help to analyse the perspective of audience and their opinion on the belief. The questions
will provide an accurate analysis of the understanding developed through the presentation
(Runciman, Merry & Walton, 2017).
SECTION 3: PRESENTATION
5
The project aims at providing message to nurses that communication for safety standard
must be integral part of their clinical practices. When carers and family members are not
involved in decision making patients may feel anxious and worried. This psychological effect
affects the quality of nursing to a great extent. Thus, health service providers must ensure that
they must regularly inform the status and need of procedures to the patients and carers (Dang &
Dearholt, 2017). It will help them to relax and better recovery will be observed. Another point of
consideration is that individuals have the right to know about their well beings and risks related
to the clinical approaches. Hence, nurses must acknowledge them with adequate information.
Presentation format:
The power point format has been intended to use for presenting this project. The
presentation format highlights the key issues and provides a chance to audience to question or
comment. When their questions are addressed orally in front of them then, it gives better
understanding to them and message is delivered successfully (Pereira & et.al., 2014).
Feedback approach:
For evaluating the effectiveness of the presentation it is necessary to evaluate the
feedbacks from the audience. For obtaining feedback from the users the various evaluation tools
can be used. For this purpose surveys such as questionnaires can be used. This evaluation tool
will help to analyse the perspective of audience and their opinion on the belief. The questions
will provide an accurate analysis of the understanding developed through the presentation
(Runciman, Merry & Walton, 2017).
SECTION 3: PRESENTATION
5
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
6

7
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
8
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
9
10
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




