Healthcare Systems: Australia and South Africa Comparison Report
VerifiedAdded on 2023/04/08
|14
|3369
|280
Report
AI Summary
This report provides a comparative analysis of the healthcare systems in Australia and South Africa, addressing key aspects such as financing mechanisms, the role of the private sector, and the populations facing limited access to healthcare services. The report explores the financing systems in both countries, highlighting the contributions towards universal healthcare, including the involvement of public and private funding. It also examines the role of the private sector in both systems, including the availability of private health insurance and its impact on healthcare access and delivery. Furthermore, the report identifies population groups with restricted access to healthcare in both Australia and South Africa, along with the barriers they face, such as geographical limitations, financial constraints, and socioeconomic disparities. The analysis draws on data and insights from various sources, including government reports, academic literature, and healthcare organizations, to provide a comprehensive overview of the healthcare landscapes in both countries. The report is structured to address the specific questions outlined in the HEAL6010 assignment brief, offering a detailed comparison and contrast of the two healthcare systems.

Running head: ORGANISATION OF HEALTHCARE SYSTEMS
Organisation of Healthcare Systems
Name of the Student
Name of the University
Author note
Organisation of Healthcare Systems
Name of the Student
Name of the University
Author note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1ORGANISATION OF HEALTHCARE SYSTEMS
Question 1
Financing system of Australia and the contribution towards the universal healthcare
To understand the funding system of healthcare in Australia the involvement of public
and government funding in healthcare and associated system have to be identified to examine
their contribution towards the Universal healthcare system. In Australia, the governing
system of universal healthcare comprises three levels of government: federal and state,
territorial and local government. The federal government offers financial supports and several
indirect supports along with the healthcare professionals. The federal government also
subsidises primary care providers under the process of Medicare Benefits Scheme or MBS
and the Pharmaceutical Benefits Scheme or PBS (Aihw.gov.au. 2016). The federal
government also provides funding for state healthcare services. In direct service delivery it
only has a limited role. On the other hand, the chief responsibility of the of the State
government are associated with the public hospitals, ambulance services, dental services,
public health and mental health services. In addition to the funding provided by the federal
government, the state government has to also contribute their own funding for these
healthcare services in state level (Morgan, Leopold and Wagner 2017).
In Australian financial system for healthcare, for providing the Community health
services such as vaccines and food-standard regulation as well preventive health programs,
the local governments plays a major role. According to annual report of 2014-2015, total
health spending in local and state level on healthcare and related services was 10.0% of GDP,
which is a 2.8% boost from the annual expenditure of 2013–2014. The government has
funded the 67% of the total expenditure of the health system (Schmidt, Gostin and Emanuel,
2015). In this regards it has to be mentioned that the visitors of Australia cannot access the
general Medicare system. Medicare is partially financed by a particular taxation system under
Question 1
Financing system of Australia and the contribution towards the universal healthcare
To understand the funding system of healthcare in Australia the involvement of public
and government funding in healthcare and associated system have to be identified to examine
their contribution towards the Universal healthcare system. In Australia, the governing
system of universal healthcare comprises three levels of government: federal and state,
territorial and local government. The federal government offers financial supports and several
indirect supports along with the healthcare professionals. The federal government also
subsidises primary care providers under the process of Medicare Benefits Scheme or MBS
and the Pharmaceutical Benefits Scheme or PBS (Aihw.gov.au. 2016). The federal
government also provides funding for state healthcare services. In direct service delivery it
only has a limited role. On the other hand, the chief responsibility of the of the State
government are associated with the public hospitals, ambulance services, dental services,
public health and mental health services. In addition to the funding provided by the federal
government, the state government has to also contribute their own funding for these
healthcare services in state level (Morgan, Leopold and Wagner 2017).
In Australian financial system for healthcare, for providing the Community health
services such as vaccines and food-standard regulation as well preventive health programs,
the local governments plays a major role. According to annual report of 2014-2015, total
health spending in local and state level on healthcare and related services was 10.0% of GDP,
which is a 2.8% boost from the annual expenditure of 2013–2014. The government has
funded the 67% of the total expenditure of the health system (Schmidt, Gostin and Emanuel,
2015). In this regards it has to be mentioned that the visitors of Australia cannot access the
general Medicare system. Medicare is partially financed by a particular taxation system under
2ORGANISATION OF HEALTHCARE SYSTEMS
the control of government. In the 2013–2014 fiscal year the funding in Medicare system
raised up to AUD 10.3 trillion (Stigler et al. 2016). The fund was further expanded in July
2014 to improve the financial capability for the disability care system. Public policies
encourage PHI enrolment with a tax discount and, over and above some income, a penalty
payment for not having PHI (Medicare Levy supplement).
Financing system of Africa and the contribution towards the universal healthcare
In South Africa, a combination of private and public funding system is used for
providing the financial support to national level healthcare system. The financial contribution
of this mixed funding mechanism can be clearly seen in the reported funding of the year
2005, where the funding from general tax allocation was around 40%, whereas around 45%
of the total health care funding was from private healthcare scheme and around 14% from
out-of-pocket payments (Rao et al. 2014). It is critical that households finance healthcare
according to their ability to pay and if risk is pooled to improve their prepayment for
healthcare in this context. Accordingly, universal coverage requires considerable social
solidarity, often enshrined in African cultures. Solidarity enables the rich (income cross-
subsidies), and the healthy (risk cross-subsidies) to cross-subsidize the poor. Like many other
developing countries, South Africa coexists in both private and public health. In comparison
with the public system, the private healthcare system currently accounts for the largest
portion, including both medical and private out - of-pocket payments, of all funding for
healthcare (Fusheini and Eyles 2016).
The highest total per capita level of health care expenditure is found in Africa in South Africa
(i.e. from public and private sources). This means, after the Commission on macroeconomics
and the estimates on health resource requirements from the Commission, that there is a
relatively sufficient amount of health care per capita to provide everyone with more than a
the control of government. In the 2013–2014 fiscal year the funding in Medicare system
raised up to AUD 10.3 trillion (Stigler et al. 2016). The fund was further expanded in July
2014 to improve the financial capability for the disability care system. Public policies
encourage PHI enrolment with a tax discount and, over and above some income, a penalty
payment for not having PHI (Medicare Levy supplement).
Financing system of Africa and the contribution towards the universal healthcare
In South Africa, a combination of private and public funding system is used for
providing the financial support to national level healthcare system. The financial contribution
of this mixed funding mechanism can be clearly seen in the reported funding of the year
2005, where the funding from general tax allocation was around 40%, whereas around 45%
of the total health care funding was from private healthcare scheme and around 14% from
out-of-pocket payments (Rao et al. 2014). It is critical that households finance healthcare
according to their ability to pay and if risk is pooled to improve their prepayment for
healthcare in this context. Accordingly, universal coverage requires considerable social
solidarity, often enshrined in African cultures. Solidarity enables the rich (income cross-
subsidies), and the healthy (risk cross-subsidies) to cross-subsidize the poor. Like many other
developing countries, South Africa coexists in both private and public health. In comparison
with the public system, the private healthcare system currently accounts for the largest
portion, including both medical and private out - of-pocket payments, of all funding for
healthcare (Fusheini and Eyles 2016).
The highest total per capita level of health care expenditure is found in Africa in South Africa
(i.e. from public and private sources). This means, after the Commission on macroeconomics
and the estimates on health resource requirements from the Commission, that there is a
relatively sufficient amount of health care per capita to provide everyone with more than a
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3ORGANISATION OF HEALTHCARE SYSTEMS
basic level of care. In the field of health policy, the NHI proposal by ANC has generated
considerable debate among key health stakeholders and academics. It is anticipated that the
proposed scheme would pool its funds into one single unit or NHIF. However, the budget
share in the health sector has declined from approximately 11.5% in 2000/2001 to about
10.9% in 2007/2008, as opposed to the Abuja declaration by the African Heads of State in
2001 that requires countries to allocate to the health sector up to 15% of the overall budget in
the Government (Fusheini and Eyles 2016).
Question 2
Role of the private sector in both Australian healthcare systems
The PHI is readily available and provides more options for providers (mainly
hospitals), faster access to non-emergency services, and discounts on the services selected.
The Lifetime Health Coverage program is a reduction in the premium for life when
participants sign up before the age of 31 (Jakovljevic, Groot and Souliotis 2016). The
government policy encourages PHI registration by tax discounts or by penalty, in excess of
certain incomes. PHI does not have a Medicare levy charge. There is a 2% increase in
baseline premiums for people who do not sign up after 30 years of age each year. As a result,
the absorption of 30 people is higher and below but rapidly decreases with age, with an opt-
out trend starting at 50 years. Almost half of the people in Australia (47%) have private
hospital coverage and almost 56% in 2016 received general treatment. Insurers are a
combination of profits and non-profits (Mayosi and Benatar 2014). Private health expenses
accounted for 8.7% of all health expenditures in 2014–2015. Private health insurance may
include hospital, general or ambulance treatment coverage. Private health insurance
providing a more flexible range of suppliers (especially in hospitals), speedier access to non-
emergency services and discounts on selected services is now readily available. Nearly half
basic level of care. In the field of health policy, the NHI proposal by ANC has generated
considerable debate among key health stakeholders and academics. It is anticipated that the
proposed scheme would pool its funds into one single unit or NHIF. However, the budget
share in the health sector has declined from approximately 11.5% in 2000/2001 to about
10.9% in 2007/2008, as opposed to the Abuja declaration by the African Heads of State in
2001 that requires countries to allocate to the health sector up to 15% of the overall budget in
the Government (Fusheini and Eyles 2016).
Question 2
Role of the private sector in both Australian healthcare systems
The PHI is readily available and provides more options for providers (mainly
hospitals), faster access to non-emergency services, and discounts on the services selected.
The Lifetime Health Coverage program is a reduction in the premium for life when
participants sign up before the age of 31 (Jakovljevic, Groot and Souliotis 2016). The
government policy encourages PHI registration by tax discounts or by penalty, in excess of
certain incomes. PHI does not have a Medicare levy charge. There is a 2% increase in
baseline premiums for people who do not sign up after 30 years of age each year. As a result,
the absorption of 30 people is higher and below but rapidly decreases with age, with an opt-
out trend starting at 50 years. Almost half of the people in Australia (47%) have private
hospital coverage and almost 56% in 2016 received general treatment. Insurers are a
combination of profits and non-profits (Mayosi and Benatar 2014). Private health expenses
accounted for 8.7% of all health expenditures in 2014–2015. Private health insurance may
include hospital, general or ambulance treatment coverage. Private health insurance
providing a more flexible range of suppliers (especially in hospitals), speedier access to non-
emergency services and discounts on selected services is now readily available. Nearly half
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4ORGANISATION OF HEALTHCARE SYSTEMS
of the Australian population (47%) had private hospital coverage and nearly 56 percent had
general treatment coverage in 2016 (Asante et al. 2016).
Patients can opt for treatment with full fees (with full fee coverage) as a public patient
or a private patient (with 75% fee coverage) when accessing hospital services. Insurance
covers MBS fees for private patients (Hall 2015). The consumer will bear the costs of the
difference, if a provider charges above the MBS fee, unless it has gaps. Costs for hospital
accommodation, operational fees (implants and theater fees) and diagnostic trials can also be
charged to the patient. The coverage includes dental, physiotherapy, chiropractic, podiatry,
home nursing and optometry insurance. The amount or number of services covered may be
limited by dollars. The socio-economic status of private health insurance varies. PHI only
includes one out of five (22,1%) of the poorest 20% of the population, up to more than 57,2%
for the most advantaged quintile population (Asante et al. 2016). This difference is partly due
to the surcharge for higher-income payers from Medicare levies.
Role of the private sector in both African healthcare systems
The national health minister once again said at a press conference on South Africa's
National Health Insurance that private health care only serves 16 percent of the population.
About 18% of the population in South Africa belong to medical schemes that give them
privacy. In 1997 there were 161, in 2004 there were 200. The number of private hospitals is
rapidly increasing. Netcare, with approximately 43 hospitals and 18 day clinics in the whole
of South Africa, and Medi-clinic (www.netcare.co.za), with around 53 hospitals, are two of
the leading private healthcare providers. In 2012, private health care providers provided
primary health care services for 28 percent, an estimated 38 percent of the South African
people, due to the relative extent of this demand and the resulting growth and development in
of the Australian population (47%) had private hospital coverage and nearly 56 percent had
general treatment coverage in 2016 (Asante et al. 2016).
Patients can opt for treatment with full fees (with full fee coverage) as a public patient
or a private patient (with 75% fee coverage) when accessing hospital services. Insurance
covers MBS fees for private patients (Hall 2015). The consumer will bear the costs of the
difference, if a provider charges above the MBS fee, unless it has gaps. Costs for hospital
accommodation, operational fees (implants and theater fees) and diagnostic trials can also be
charged to the patient. The coverage includes dental, physiotherapy, chiropractic, podiatry,
home nursing and optometry insurance. The amount or number of services covered may be
limited by dollars. The socio-economic status of private health insurance varies. PHI only
includes one out of five (22,1%) of the poorest 20% of the population, up to more than 57,2%
for the most advantaged quintile population (Asante et al. 2016). This difference is partly due
to the surcharge for higher-income payers from Medicare levies.
Role of the private sector in both African healthcare systems
The national health minister once again said at a press conference on South Africa's
National Health Insurance that private health care only serves 16 percent of the population.
About 18% of the population in South Africa belong to medical schemes that give them
privacy. In 1997 there were 161, in 2004 there were 200. The number of private hospitals is
rapidly increasing. Netcare, with approximately 43 hospitals and 18 day clinics in the whole
of South Africa, and Medi-clinic (www.netcare.co.za), with around 53 hospitals, are two of
the leading private healthcare providers. In 2012, private health care providers provided
primary health care services for 28 percent, an estimated 38 percent of the South African
people, due to the relative extent of this demand and the resulting growth and development in
5ORGANISATION OF HEALTHCARE SYSTEMS
the sector. In addition, an estimated 37% of GPs, 59% of experts and 38% of nurses were
involved in the private sector in South Africa (Mayosi, and Benatar 2014).
It is further estimated that in 2013 the private health services sector accounted for
35% of hospitals and 28% of hospital beds. Between 2007/08 and 2011/12 the average health
outlay in South Africa was 50% and 3%, respectively, for the public, private and donor sector
and NGOs. All of these figures show the size and importance of private healthcare in
accessing quality treatment in South Africa (Jakovljevic, Groot and Souliotis 2016). On the
Johannesburg Stock Exchange (JSE), the 3 largest private hospital groups are listed and have
a significant effect on local investment and taxation.
Question 3
Population group in Australia that has limited access and the barriers
Australians living in rural and remote areas tend to have shorter lives, higher levels of
illness and injury, and poorer access to and use of health services compared to people living
in metropolitan areas. Poor health outcomes in rural and remote areas could be driven by a
variety of factors, including the degree of disadvantage of education and opportunities for
employment, income, and access to services. Individuals living in remote parts of Australia
may need to travel long distances or move to health care or receive specialized treatment
(Australian Institute of Health and Welfare. 2018). For example, 57 percent of those living in
Very Remote Sites at the beginning of their treatment with end-stage kidney disease moved
within 1 year from combined data for 2005–2010. In 2013–14, the highest rate for emergency
hospital surgery admissions in Very remote regions was (22 per 1,000 population) and the
lowest rate of admissions in major cities was declining (12 out of 1,000) (Aihw.gov.au.
2016). Access to health services contributes significantly to health and well-being. In view of
the overall poorness of their health and the need for healthcare more strongly than non-
the sector. In addition, an estimated 37% of GPs, 59% of experts and 38% of nurses were
involved in the private sector in South Africa (Mayosi, and Benatar 2014).
It is further estimated that in 2013 the private health services sector accounted for
35% of hospitals and 28% of hospital beds. Between 2007/08 and 2011/12 the average health
outlay in South Africa was 50% and 3%, respectively, for the public, private and donor sector
and NGOs. All of these figures show the size and importance of private healthcare in
accessing quality treatment in South Africa (Jakovljevic, Groot and Souliotis 2016). On the
Johannesburg Stock Exchange (JSE), the 3 largest private hospital groups are listed and have
a significant effect on local investment and taxation.
Question 3
Population group in Australia that has limited access and the barriers
Australians living in rural and remote areas tend to have shorter lives, higher levels of
illness and injury, and poorer access to and use of health services compared to people living
in metropolitan areas. Poor health outcomes in rural and remote areas could be driven by a
variety of factors, including the degree of disadvantage of education and opportunities for
employment, income, and access to services. Individuals living in remote parts of Australia
may need to travel long distances or move to health care or receive specialized treatment
(Australian Institute of Health and Welfare. 2018). For example, 57 percent of those living in
Very Remote Sites at the beginning of their treatment with end-stage kidney disease moved
within 1 year from combined data for 2005–2010. In 2013–14, the highest rate for emergency
hospital surgery admissions in Very remote regions was (22 per 1,000 population) and the
lowest rate of admissions in major cities was declining (12 out of 1,000) (Aihw.gov.au.
2016). Access to health services contributes significantly to health and well-being. In view of
the overall poorness of their health and the need for healthcare more strongly than non-
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6ORGANISATION OF HEALTHCARE SYSTEMS
indigenous populations, it influences particularly the health status of indigenous and Torres
Strait Islanders. Around 203 indigenous primary healthcare organizations reported data on the
total number of their clients, contacts and care episodes in 2014–15. Services were provided
by more than 5 million contacts to 434,600 clients, with a mean of 12 customers per person
(Aihw.gov.au. 2016). Aboriginals and Torres Strait Islanders are over three-quarters (79 %)
of those clients. Over time, health care episodes have almost tripled to customers in these
organizations, from 1.2 million in 1999–2000 to 3.5 million in 2014-15 (AIHW 2016b)
(Australian Institute of Health and Welfare. 2018). GP services were 10 per cent more than
that for non-Indigenous Australians per 1,000 Indigenous Australians, but the claims for
specialist services for indigenous Australians were 43 per cent less.
Population group in Africa that has limited access and the barriers
In South Africa, access to healthcare is constitutionally enshrined in South Africa;
however considerable inequity still exists, mainly due to distortions in the allocation of
resources. Over one thousand people, mainly in LMICs, are unable to access the needed
healthcare services. They are inexpensive. The barriers to access include large distances and
high travel costs in rural areas in particular; high out - of-pocket (OOP) care payment; long
queues; and disabled patients. The hurdles of access experienced elsewhere in LMIC's
resonate with uneven social power relations (Mayosi and Benatar 2014). The achievement of
a fair UHC requires accessible, necessary services(' dependence') for the whole population('
breadth'), while adapting the disadvantaged groups to' different needs' and financial
constraints(' height'). The differences in health outcomes from racial and socio-economic to
rural and urban to private sectors are still challenging. There were 21 159 of the 4668
households sampled. Four-fifths were black Africans, almost half had primary or minor
education, and 39.9% were rural (Crush and Tawodzera 2014).
indigenous populations, it influences particularly the health status of indigenous and Torres
Strait Islanders. Around 203 indigenous primary healthcare organizations reported data on the
total number of their clients, contacts and care episodes in 2014–15. Services were provided
by more than 5 million contacts to 434,600 clients, with a mean of 12 customers per person
(Aihw.gov.au. 2016). Aboriginals and Torres Strait Islanders are over three-quarters (79 %)
of those clients. Over time, health care episodes have almost tripled to customers in these
organizations, from 1.2 million in 1999–2000 to 3.5 million in 2014-15 (AIHW 2016b)
(Australian Institute of Health and Welfare. 2018). GP services were 10 per cent more than
that for non-Indigenous Australians per 1,000 Indigenous Australians, but the claims for
specialist services for indigenous Australians were 43 per cent less.
Population group in Africa that has limited access and the barriers
In South Africa, access to healthcare is constitutionally enshrined in South Africa;
however considerable inequity still exists, mainly due to distortions in the allocation of
resources. Over one thousand people, mainly in LMICs, are unable to access the needed
healthcare services. They are inexpensive. The barriers to access include large distances and
high travel costs in rural areas in particular; high out - of-pocket (OOP) care payment; long
queues; and disabled patients. The hurdles of access experienced elsewhere in LMIC's
resonate with uneven social power relations (Mayosi and Benatar 2014). The achievement of
a fair UHC requires accessible, necessary services(' dependence') for the whole population('
breadth'), while adapting the disadvantaged groups to' different needs' and financial
constraints(' height'). The differences in health outcomes from racial and socio-economic to
rural and urban to private sectors are still challenging. There were 21 159 of the 4668
households sampled. Four-fifths were black Africans, almost half had primary or minor
education, and 39.9% were rural (Crush and Tawodzera 2014).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7ORGANISATION OF HEALTHCARE SYSTEMS
The richer quintiles concentrated surgical visits in the private sector. Private
outpatient care (including general practitioners, private dentists and pharmacies) has been
steadily increasing in consumption, from 15.7% to 60.8% of the wealthy; a group which also
used outpatients in private hospitals four times more than in private hospitals. The total
utilization of hospital-private facilities for rural residents and those living in informal urban
areas was only 10% (33,6 admissions) (van Rensburg 2014). Private admissions in the more
poor, rural provinces of Limpopo, Mpumalanga, and Eastern Cape also produced widespread
differences.
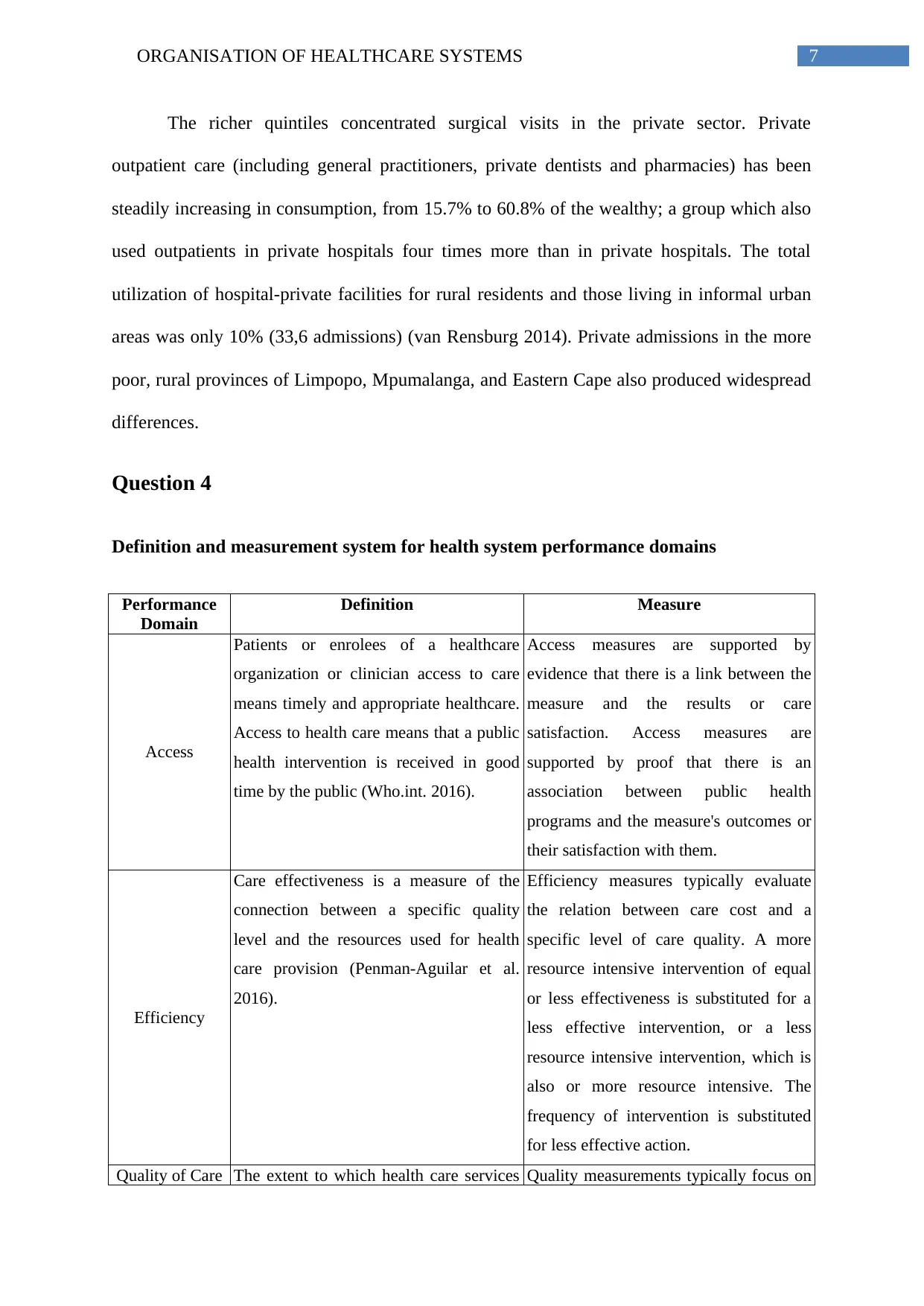
Question 4
Definition and measurement system for health system performance domains
Performance
Domain
Definition Measure
Access
Patients or enrolees of a healthcare
organization or clinician access to care
means timely and appropriate healthcare.
Access to health care means that a public
health intervention is received in good
time by the public (Who.int. 2016).
Access measures are supported by
evidence that there is a link between the
measure and the results or care
satisfaction. Access measures are
supported by proof that there is an
association between public health
programs and the measure's outcomes or
their satisfaction with them.
Efficiency
Care effectiveness is a measure of the
connection between a specific quality
level and the resources used for health
care provision (Penman-Aguilar et al.
2016).
Efficiency measures typically evaluate
the relation between care cost and a
specific level of care quality. A more
resource intensive intervention of equal
or less effectiveness is substituted for a
less effective intervention, or a less
resource intensive intervention, which is
also or more resource intensive. The
frequency of intervention is substituted
for less effective action.
Quality of Care The extent to which health care services Quality measurements typically focus on
The richer quintiles concentrated surgical visits in the private sector. Private
outpatient care (including general practitioners, private dentists and pharmacies) has been
steadily increasing in consumption, from 15.7% to 60.8% of the wealthy; a group which also
used outpatients in private hospitals four times more than in private hospitals. The total
utilization of hospital-private facilities for rural residents and those living in informal urban
areas was only 10% (33,6 admissions) (van Rensburg 2014). Private admissions in the more
poor, rural provinces of Limpopo, Mpumalanga, and Eastern Cape also produced widespread
differences.
Question 4
Definition and measurement system for health system performance domains
Performance
Domain
Definition Measure
Access
Patients or enrolees of a healthcare
organization or clinician access to care
means timely and appropriate healthcare.
Access to health care means that a public
health intervention is received in good
time by the public (Who.int. 2016).
Access measures are supported by
evidence that there is a link between the
measure and the results or care
satisfaction. Access measures are
supported by proof that there is an
association between public health
programs and the measure's outcomes or
their satisfaction with them.
Efficiency
Care effectiveness is a measure of the
connection between a specific quality
level and the resources used for health
care provision (Penman-Aguilar et al.
2016).
Efficiency measures typically evaluate
the relation between care cost and a
specific level of care quality. A more
resource intensive intervention of equal
or less effectiveness is substituted for a
less effective intervention, or a less
resource intensive intervention, which is
also or more resource intensive. The
frequency of intervention is substituted
for less effective action.
Quality of Care The extent to which health care services Quality measurements typically focus on
8ORGANISATION OF HEALTHCARE SYSTEMS
increase the probability of health
outcomes for individuals and populations
and comply with current professional
know – how (Saver et al. 2015).
care structures or processes that are
linked with positive health outcomes and
controlled by the health system.
Measurements of quality as a mechanism
by comparison of criterion to assign
quantities to quality of care (Wong, et al.
2014).
Equity
The absence, whether these groups are
socially or economically,
demographically, geographical or
otherwise stratified, of avoidable, unfair,
or remediable differences between groups
of persons is equality (Wong, et al. 2014)
At a minimum, the measurement of
health equity requires population-based
information on health status, health care
and social determinants of health to be
divided into different socio-economic
standards, ethnic group, and gender (with
adequate sample size to reliable
estimates) (Who.int. 2016).
Health Status
WHO has defined health as a "state of
total physical, mental and social
goodness rather than simply a lack of
illness." Health can be taken into account
in terms of structure and function of a
person's body and the presence or
absence of disease or signs (health
status), symptoms and the extent of the
condition that affects the person's normal
life (quality of life) (Who.int. 2016).
Clinical and pathological medicine can
also measure health status and clinics or
measure instruments are normally
observed by clinicians including: sign
(blood pressure, temperature, x - ray,
tumour size), symptoms (disease specific
checklists). co- morbidity (Charlson
Index) (Charlson Index, ICED index of
co - existent illnesses) (Saver et al.
2015).
Health
Determinations
The range of personal, social, economic,
and environmental factors that influence
health status are known as determinants
of health (Wong, et al. 2014).
The measurement of determinants of the
health comprises several factors such as
Policymaking, Social factors, Health
services, Individual behaviour, Biology
and genetics.
Question 5
Benefits associated with the health system performance measurement:
increase the probability of health
outcomes for individuals and populations
and comply with current professional
know – how (Saver et al. 2015).
care structures or processes that are
linked with positive health outcomes and
controlled by the health system.
Measurements of quality as a mechanism
by comparison of criterion to assign
quantities to quality of care (Wong, et al.
2014).
Equity
The absence, whether these groups are
socially or economically,
demographically, geographical or
otherwise stratified, of avoidable, unfair,
or remediable differences between groups
of persons is equality (Wong, et al. 2014)
At a minimum, the measurement of
health equity requires population-based
information on health status, health care
and social determinants of health to be
divided into different socio-economic
standards, ethnic group, and gender (with
adequate sample size to reliable
estimates) (Who.int. 2016).
Health Status
WHO has defined health as a "state of
total physical, mental and social
goodness rather than simply a lack of
illness." Health can be taken into account
in terms of structure and function of a
person's body and the presence or
absence of disease or signs (health
status), symptoms and the extent of the
condition that affects the person's normal
life (quality of life) (Who.int. 2016).
Clinical and pathological medicine can
also measure health status and clinics or
measure instruments are normally
observed by clinicians including: sign
(blood pressure, temperature, x - ray,
tumour size), symptoms (disease specific
checklists). co- morbidity (Charlson
Index) (Charlson Index, ICED index of
co - existent illnesses) (Saver et al.
2015).
Health
Determinations
The range of personal, social, economic,
and environmental factors that influence
health status are known as determinants
of health (Wong, et al. 2014).
The measurement of determinants of the
health comprises several factors such as
Policymaking, Social factors, Health
services, Individual behaviour, Biology
and genetics.
Question 5
Benefits associated with the health system performance measurement:
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9ORGANISATION OF HEALTHCARE SYSTEMS
The healthcare system performance measurement can offer a broad assessment of
system performance as well as can also stimulate better data collection and analytic
efforts across health systems and nations.
The healthcare system performance measurement enables the authority to place the
healthcare system performance measurement at the centre of the governmental policy
where policy-makers at all levels can have the freedom to concentrate on areas where
improvements are most readily secured, in contrast to piecemeal performance
indicators (Wong, et al. 2014).
The healthcare system performance measurement offers a clear indication which
systems represent the best overall performance and improvement efforts. As a result,
it enables more accurate and effective judgement and cross-national comparison in
order to improve the health system efficiency
Challenges associated with health system performance measurement:
One of the major limitation of health system performance measurement is that it May
disguise failings in specific parts of the health care system, which can lead to making
individual measures under a contentious and hidden dataset while statistically
calculating the aggregation of the obtained data. Sometimes the performance
measurement ignores some aspects of performance that are difficult to measure,
leading to adverse behavioural effects (Penman-Aguilar et al. 2016).
The health system performance measurement can make the whole measurement
system difficult to determine where poor performance is occurring and, consequently,
may make policy and planning more difficult and less effective.
The healthcare system performance measurement can offer a broad assessment of
system performance as well as can also stimulate better data collection and analytic
efforts across health systems and nations.
The healthcare system performance measurement enables the authority to place the
healthcare system performance measurement at the centre of the governmental policy
where policy-makers at all levels can have the freedom to concentrate on areas where
improvements are most readily secured, in contrast to piecemeal performance
indicators (Wong, et al. 2014).
The healthcare system performance measurement offers a clear indication which
systems represent the best overall performance and improvement efforts. As a result,
it enables more accurate and effective judgement and cross-national comparison in
order to improve the health system efficiency
Challenges associated with health system performance measurement:
One of the major limitation of health system performance measurement is that it May
disguise failings in specific parts of the health care system, which can lead to making
individual measures under a contentious and hidden dataset while statistically
calculating the aggregation of the obtained data. Sometimes the performance
measurement ignores some aspects of performance that are difficult to measure,
leading to adverse behavioural effects (Penman-Aguilar et al. 2016).
The health system performance measurement can make the whole measurement
system difficult to determine where poor performance is occurring and, consequently,
may make policy and planning more difficult and less effective.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10ORGANISATION OF HEALTHCARE SYSTEMS
Health system performance measurement often can lead to double counting, because
of high positive correlation May use feeble data when seeking to cover many areas,
which may make the methodological soundness of the entire indicator questionable.
As a result, sometime it only reflects certain preferences when inadequately
developed methods for applying weights to composite indicators are used.
Health system performance measurement often can lead to double counting, because
of high positive correlation May use feeble data when seeking to cover many areas,
which may make the methodological soundness of the entire indicator questionable.
As a result, sometime it only reflects certain preferences when inadequately
developed methods for applying weights to composite indicators are used.
11ORGANISATION OF HEALTHCARE SYSTEMS
Reference
Aihw.gov.au. 2016. how-does-australias-health-system-work. [online] Available at:
https://www.aihw.gov.au/getmedia/f2ae1191-bbf2-47b6-a9d4-1b2ca65553a1/ah16-2-1-how-
does-australias-health-system-work.pdf.aspx [Accessed 8 Apr. 2019].
Aihw.gov.au. 2016. Indigenous Australians’ access to health services. [online] Available at:
https://www.aihw.gov.au/getmedia/01d88043-31ba-424a-a682-98673783072e/ah16-6-6-
indigenous-australians-access-health-services.pdf.aspx [Accessed 8 Apr. 2019].
Asante, A., Price, J., Hayen, A., Jan, S. and Wiseman, V., 2016. Equity in health care
financing in low-and middle-income countries: a systematic review of evidence from studies
using benefit and financing incidence analyses. PloS one, 11(4), p.e0152866.
Australian Institute of Health and Welfare. 2018. Rural & remote health, Access to health
services - Australian Institute of Health and Welfare. [online] Available at:
https://www.aihw.gov.au/reports/rural-health/rural-remote-health/contents/access-to-health-
services [Accessed 8 Apr. 2019].
Crush, J. and Tawodzera, G., 2014. Medical xenophobia and Zimbabwean migrant access to
public health services in South Africa. Journal of Ethnic and Migration Studies, 40(4),
pp.655-670.
Fusheini, A. and Eyles, J., 2016. Achieving universal health coverage in South Africa
through a district health system approach: conflicting ideologies of health care
provision. BMC health services research, 16(1), p.558.
Gauld, R., Burgers, J., Dobrow, M., Minhas, R., Wendt, C., B. Cohen, A. and Luxford, K.,
2014. Healthcare system performance improvement: a comparison of key policies in seven
high-income countries. Journal of health organization and management, 28(1), pp.2-20.
Reference
Aihw.gov.au. 2016. how-does-australias-health-system-work. [online] Available at:
https://www.aihw.gov.au/getmedia/f2ae1191-bbf2-47b6-a9d4-1b2ca65553a1/ah16-2-1-how-
does-australias-health-system-work.pdf.aspx [Accessed 8 Apr. 2019].
Aihw.gov.au. 2016. Indigenous Australians’ access to health services. [online] Available at:
https://www.aihw.gov.au/getmedia/01d88043-31ba-424a-a682-98673783072e/ah16-6-6-
indigenous-australians-access-health-services.pdf.aspx [Accessed 8 Apr. 2019].
Asante, A., Price, J., Hayen, A., Jan, S. and Wiseman, V., 2016. Equity in health care
financing in low-and middle-income countries: a systematic review of evidence from studies
using benefit and financing incidence analyses. PloS one, 11(4), p.e0152866.
Australian Institute of Health and Welfare. 2018. Rural & remote health, Access to health
services - Australian Institute of Health and Welfare. [online] Available at:
https://www.aihw.gov.au/reports/rural-health/rural-remote-health/contents/access-to-health-
services [Accessed 8 Apr. 2019].
Crush, J. and Tawodzera, G., 2014. Medical xenophobia and Zimbabwean migrant access to
public health services in South Africa. Journal of Ethnic and Migration Studies, 40(4),
pp.655-670.
Fusheini, A. and Eyles, J., 2016. Achieving universal health coverage in South Africa
through a district health system approach: conflicting ideologies of health care
provision. BMC health services research, 16(1), p.558.
Gauld, R., Burgers, J., Dobrow, M., Minhas, R., Wendt, C., B. Cohen, A. and Luxford, K.,
2014. Healthcare system performance improvement: a comparison of key policies in seven
high-income countries. Journal of health organization and management, 28(1), pp.2-20.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 14
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




